Abstract
AIM
To present the results of implantation of Iakymenko keratoprosthesis in five patients with vascularized corneal leukoma caused by severe ocular injury.
METHODS
Iakymenko keratoprosthesis was implanted into 5 eyes of 5 patients: 4 patients were suffered from chemical burns and 1 patient from explosive injury. The preoperative visual acuity ranged from light perception to hand motion. The implantation surgery was composed of two-stage procedures. The follow-up period was from 9 months to 11 years. The outcome measures were visual acuity, retention, and complications of the keratoprosthesis.
RESULTS
Vision improvements were achieved in most patients. All keratoprosthesis were retained within the follow-up period. Corneal melting occurred in one patient and fibrous closure in another patient, both of which were successfully treated. Retinal detachment occurred in one patient after surgery.
CONCLUSION
Iakymenko keratoprosthesis seems to be a promising alternative for the patients with severe corneal injury, but further investigation is needed to evaluate the role of Iakymenko keratoprosthesis.
Keywords: Iakymenko keratoprosthesis, visual rehabilitation, complications
INTRODUCTION
Corneal disease is one of the most important causes of blindness. For many corneal diseases such as corneal scar, keratoconus and endothelial failure, penetrating keratoplasty yields acceptable results. However, some complicated corneal lesions with limbal stem cell deficiency, severe neovascularization or repeated corneal graft failure, are poor candidates for penetrating keratoplasty. Implantation of a synthetic corneal replacement, namely keratoprosthesis, has been developed for treatment of such diseases. Now many types of keratoprostheses have been designed and applied in the clinical practice, from the totally synthetic Boston keratoprothesis, to the combined synthetic optic and biological frame of the osteo-odonto keratoprothesis (OOKP) and the entirely biological tissue engineered cornea. The indications for this procedure have been expanded for more corneal diseases including Stevens–Johnson syndrome, chemical burns, disorders with limbal stem cell deficiency, ocular cicatricial pemphigoid, and severe corneal vascularization.
The Iakymenko keratoprosthesis(I-KPro) was developed in Filatov Institute of Eye Disease & Tissue Therapy, Ukraine[1],[2]. We learned the surgical skill from Dr. Iakymenko and introduced it into China. From 1999, we performed I-KPro implantation in 5 patients with vascularized corneal leukoma caused by severe chemical injury or explosive injury. We now present the result of I-KPro implantation with follow-up of up to 11 years.
MATERIALS AND METHODS
Materials
Inclusion criteria for this study were severe corneal diseases with poor prognosis for keratoplasty including chemical injury, allograft failure and deep corneal vascularization, visual acuity not better than 20/500, potential for significant visual improvement, blindness in the contralateral eye and age older than 18 years. Patients with active inflammation, uncontrolled raised intraocular pressure, cicatrizing ocular diseases such as ocular cicatricial pemphigoid or Stevens-Johnson syndrome, and ultrasound evidence of significant posterior segment pathology were excluded. Ethics board committee approval was obtained for the study. All patients provided written informed consent. Five patients with severe vascularized corneal leucoma were included in this study. The keratoprothesis implantation was performed from 1999 and follow-up duration ranged from 9 months to 11 years.
Methods
Surgical technique
The I-KPro was composed of a central rigid polymethyl methacrylate (PMMA) optical cylinder and a titanium-tantalum frame. The optic cylinder had a diameter of 3.5 mm in the anterior part and 2.6mm in the posterior part (Figure 1). The I-KPro implantation surgery was composed of two stage procedures, both of which were performed under local anesthesia. In stage I procedure, after exposing the ocular surface with lid retraction suture, a superior, 270 degree of conjunctival peritomy and recession were performed to make a conjunctival flap. Flieringa fixation ring was fixed with 6-0 black silk, then a superior 270° scleral incision at approximately 1.0 mm posterior to the limbus was performed and extended into the cornea to divide the cornea into two layers at maximal possible depth, superficial and deep, using a lamellar dissecting blade. The dissection was then extended into the inferior cornea so that a central corneal pocket was created. For preparation of the auricular cartilage, the ear skin was incised to expose the underlying cartilage after infiltration anesthesia, and then a cartilage graft was obtained using a 9mm trephine followed by clearance of the superficial connective tissues. A trephine with similar diameter of the optic cylinder of I-KPro, 3.3 mm, was used to make a hole in the center of the cartilage graft. After that, the optic cylinder of Iakymenko keratoprosthesis was fixed in the hole of auricular cartilage, and placed in gentamycin-containing saline for use. The superficial corneal flap was then reflected inferiorly to expose the deep cornea, to allow trephination of the central posterior lamella with a 2.5 mm trephine to enter the anterior chamber. The piece of posterior lamella was removed. Cataract extraction (2 patients) was performed through the trephination hole in central posterior cornea after anterior capsulorhexis (1 case), in the 2nd case cataract was removed in the capsule through additional 180° limbal incision of posterior corneal layers. Then the I-KPro with auricular cartilage was placed between the two layers within the pocket, the optic cylinder in the posterior lamellar opening. The superficial corneal flap was then replaced and sutured at the limbus with pre-placed absorbable suture, and the conjunctival flap was placed over the cornea.
Figure 1. Photograph of Iakymenko keratoprosthesis.

Stage II procedure was performed at about 6 months after the stage I procedure. Care was taken to determine the position of optic cylinder. Trephination of the tissues superficial to I-KPro including conjunctiva and anterior corneal lamella using a 3.5mm trephine was performed to expose the optic cylinder.
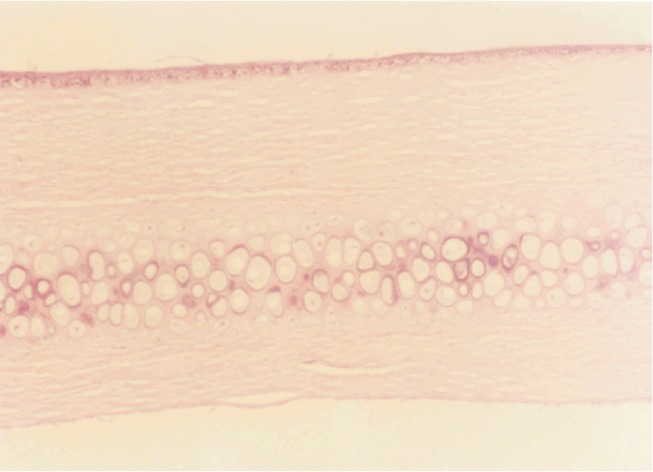
To examine the biocompatibility of auricular cartilage with cornea, we previously performed animal experiments. The autologous auricular cartilage was obtained from the rabbit ear and then implanted into its corneal stroma. After 4 weeks, tissue section was prepared and HE staining was performed to observe the biocompatibility of auricular cartilage. The results showed that the auricular cartilage was completely integrated into cornea without any space between the two different tissues, indicating a satisfactory compatibility of auricular cartilage with corneal stroma (Figure 2).
Figure 2. Microphotograph showing the good compatibility of auricular cartilage with corneal stroma 4 weeks after the implantation of auricular cartilage into corneal stroma. The tissue section was stained with haematoxylin and eosin. No obvious border between auricular cartilage and corneal stroma was found, and the collagen layers was arranged in order without infiltration of inflammatory cells (×100).
Postoperative medication
After stage I procedure, systemic antibiotics (cefradine 2g once daily) and systemic steroid (Dexamethasone 15mg daily) was administered intravenously for a week. Multiple vitamins were taken orally. Topical Ofloxacin and dexamethasone eyedrops were administered three times daily. 1% atropine eye ointment and tetracycline ointment were administered once daily. Two weeks after the stage I implantation, basic fibroblast growth factor (bFGF) eyedrops was given to promote the epithelial growth. After stage II procedure, Ofloxacin and Dexamethasone eyedrops were administered three times daily, tetracycline ointment once daily. Dexamethasone eyedrops administration was stopped one week later. Artificial tears were applied for patients with dry eye.
RESULTS
Preoperative Characteristics
A total of five I-KPros were implanted in 5 eyes of 5 patients. All the patients were male, with a mean age of 35 years (range, 27-41 years). All the five patients suffered from severe vascularized corneal leucoma, of which 4 patients were secondary to chemical burns and one patient caused by explosive injury. The time after injury ranged from 1.4 to 4 years. Allograft keratoplasty was performed in 3 patients previously but failed to improve visual acuity due to graft rejection. Cataract extraction was performed in 3 patients before keratoprosthesis. The preoperative best spectacle-corrected visual acuity ranged from counting fingers to light perception; preoperatively the contralateral eye had no light perception.
Visual Acuity
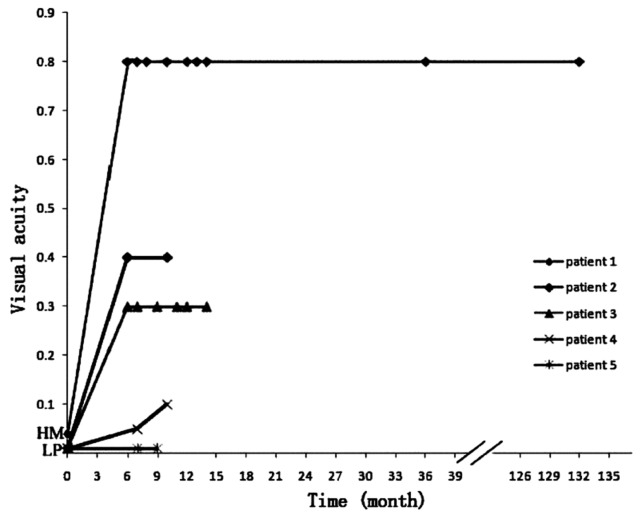
The keratoprosthesis dramatically improved the vision in most patients. At 6 month after keratoprosthesis, the best uncorrected visual acuity (BUVA) of 20/200 or better was achieved in four patients, and only one patient had no significant improvement in BUVA who was found to have retinal detachment in the operated eye. The BUVA remained almost unchanged within the follow-up period, except an improvement from 10/200 to 20/200 in one patient. The visual outcomes are summarized Figure 3.
Figure 3. Graph showing the preoperative and postoperative visual acuity of the 5 patients over the follow-up period. For each patient, the preoperative visual acuity is showed at 0 of time axis, and the posterative corrected visual acuity is showed at the point of each visit.
HM: Hand movement; LP: Light perception.
Retention
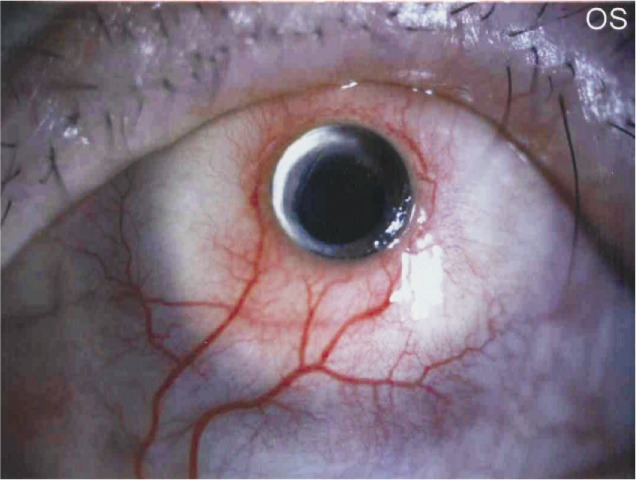
In all the five cases, the prosthesis was retained without dislocation or extrusion within the follow-up duration. A longest retention was obtained in one patient with a follow-up of 11 years (Figure 4). The retention duration for some patients was not updated for lost of follow-up.
Figure 4. Anterior segment photograph obtained 11 years after Iakymenko keratoprosthesis implantation.
Complications
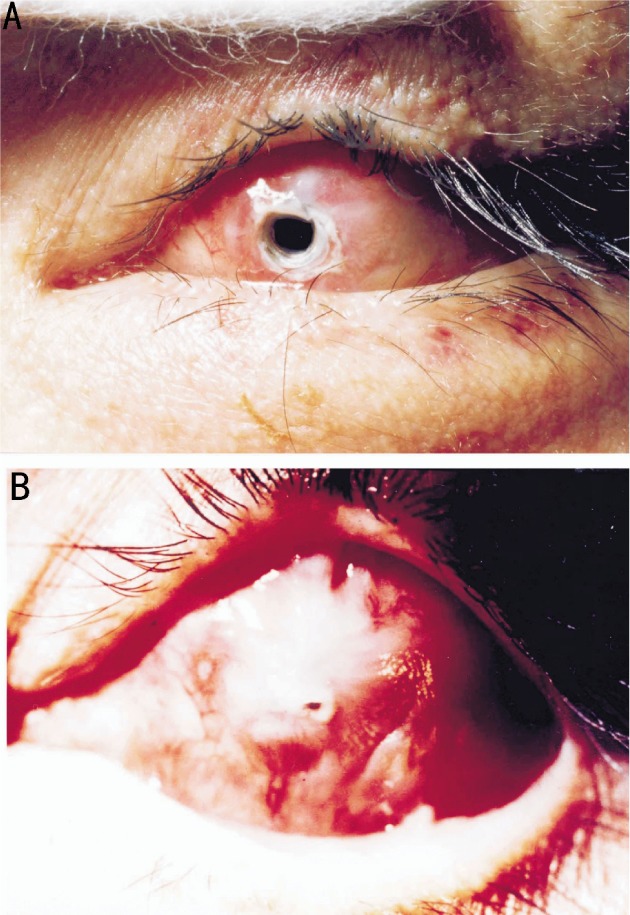
Corneal melting was observed in one patient 2.5 months after stage I procedure, without obvious aqueous humor leakage. After administration of bFGF eyedrops four times daily, the I-KPro was covered by epithelium and the underlying connective tissues one month later (Figure 5). Fibrous reclosure of the anterior opening occurred in one case. Excision of the fibrous membrane and cauterization of the peripheral tissue was performed to regain a clear visual axis. Retinal detachment was found in one patient 7 months after surgery. Other complications reported in other studies such as surface infection, endophthalmitis, intractable glaucoma were not found in our study.
Figure 5. A: Corneal melting occurred 2.5 months after stage I procedure; B: After treatment with bFGF eyedrops for 3 weeks, connective tissues grew on the surface of keratoprosthesis, with a pinhole-like defect in the center.
DISCUSSION
As the last resort of ophthalmologists for many refractory corneal diseases, keratoprosthesis has achieved great progresses in device design and postoperative management, which in turn increase the number of implantation and expand the indications. Moreover, the keratoprothesis is considered to be highly cost-effective compared with corneal transplantation[3]. However, keratoprosthesis did not develop so rapidly in China as in those developed countries. Few studies on keratoprosthesis from China have been published over the past decades[4],[5]. We performed I-KPro implantation on several patients and the follow-up period ranged from 9 months to 11 years.
Presently several types of keratoprostheses are applied in clinical use. Boston KPro is the most commonly used keratoprosthesis, with more than 3,000 being implanted worldwide[6]. Many clinical trials have demonstrated satisfactory retention rate and visual improvement, with the most common complications of retroprosthetic membrane formation and raised intraocular pressure[7]-[9]. The osteo-odonto-keratoprosthesis (OOKP) uses the patient's own tooth root and surrounding alveolar bone to support a centrally cemented optical cylinder and it requires a two-stage procedure. It is theoretically reasonable that the biological material might increase the tissue integration and reduce extrusion rate. OOKP has wider application compared with other KPros and it can even be used for patients with sever dry eye caused by Stevens–Johnson syndrome, ocular cicatricial pemphigoid, etc. The results of several studies on OOKP proved it to be well retained and the complications rate were generally low[10]-[12]. Alphacor keratoprosthesis is made from a single biocompatible polymer and involves a two-stage procedure. However, the results of clinical studies showed a relatively low retention rate due to corneal stromal melting and a high incidence of complications in cases with a history of herpetic eye disease[13]-[16]. Additionally, many other types of Kpro were developed but the clinical studies have not extended enough to draw a definite conclusion[17]-[19]. The I-KPro is different from the above mentioned keratoprosthesis, but it shares much common characteristics. The optic cylinder is made of PMMA, which is also used in Boston keratoprosthesis. Auricular cartilage is used for increasing tissue integration of I-KPro, just as the role of bone and tooth used in OOKP. The surgical procedure of I-KPro implantation is similar to that of AlphaCor, both composed of two stages and characterized by placing the device in the pocket between anterior and posterior corneal lamella. More than 1000 I-KPro implantations were performed in the Filatov Institute since 1966[20].
Appropriate patients selection is of great importance for the prognosis of the surgery. The indications for different types of keratoprostheses vary. As reported in previous studies, Boston keratoprosthesis and AlphaCor keratoprosthesis are not suitable for patients with abnormal lid function or severe dry eye, while OOKP has much wider application. Our preliminary results suggest chemical injury and corneal graft failure might be indications for I-KPro. However, our study is limited by the number of patients included, and it may be expanded to more corneal diseases by future clinical researches.
It is difficult to compare Iakymenko keratoprosthesis with other types of keratoprostheses because the patients' situation and surgeons' skill vary in different studies. Poor tissue integration is a major problem for keratoprosthesis, which leads to failure of retention. In our study, no device extrusion was found within the follow-up period. We think many factors contributed to this result. First, the use of autologous cartilage significantly enforced the mechanical strength and biological compatibility of the I-KPro. Second, postoperative administration of tetracycline reduced the activity of collagenase and inhibited tissue degradation. Third, the application of bFGF successfully promoted tissue growth and prevented corneal melting. Retinal detachment occurred in one patient, but we did not definitely know the reason. We supposed it might be related with the fragile retina of the patient and the impact of cataract extraction.
In conclusion, despite the small sample size in our study, the preliminary result of I-KPro was acceptable. All of the five patients achieved a middle-term to long-term visual improvement and implant stability. No severe complication was found in these patients except retinal detachement in one patient. So I-KPro implantation seems to be a promising alternative for the patients with severe corneal scar or opacity, which is no suitable for keratoplasty. Our experience with I-KPro might be helpful for consideration of improvement in the keratoprosthesis design and surgical skills.
Footnotes
Foundation items: Supported by National Natural Science Foundation of China (No. 81000368); Medical Scientific Research Foundation of Guangdong Province, China (B2008091, A2011327)
REFERENCES
- 1.Iakymenko SA. Optic penetrating keratoprosthesis using new models of corneal prostheses. Oftalmol Zh. 1981;36(2):102–104. [PubMed] [Google Scholar]
- 2.Iakymenko SA. Results of PMMA/Titanium keratoprosthesis in 502 eyes. Refract Corneal Surg. 1993;9:197–198. [Google Scholar]
- 3.Ament JD, Stryjewski TP, Ciolino JB, Todani A, Chodosh J, Dohlman CH. Cost-effectiveness of the Boston keratoprosthesis. Am J Ophthalmol. 149(2):221–8 e2. doi: 10.1016/j.ajo.2009.08.027. [DOI] [PubMed] [Google Scholar]
- 4.Yu J, Huang Y. Keratoprosthesis in China. Am J Ophthalmol. 150(2):291. doi: 10.1016/j.ajo.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 5.Huang Y, Yu J, Liu L, Du G, Song J, Guo H. Moscow Eye Microsurgery Complex in Russia Keratoprosthesis in Beijing. Ophthalmology. 2011;118(1):41–46. doi: 10.1016/j.ophtha.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 6.Gomaa A, Comyn O, Liu C. Keratoprostheses in clinical practice - a review. Clin Experiment Ophthalmol. 2010;38(2):211–224. doi: 10.1111/j.1442-9071.2010.02231.x. [DOI] [PubMed] [Google Scholar]
- 7.Aquavella JV, Qian Y, McCormick GJ, Palakuru JR. Keratoprosthesis: the Dohlman-Doane device. Am J Ophthalmol. 2005;140(6):1032–1038. doi: 10.1016/j.ajo.2005.06.041. [DOI] [PubMed] [Google Scholar]
- 8.Zerbe BL, Belin MW, Ciolino JB. Results from the multicenter Boston Type 1 Keratoprosthesis Study. Ophthalmology. 2006;113(10):1779 e1–7. doi: 10.1016/j.ophtha.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 9.Aldave AJ, Kamal KM, Vo RC, Yu F. The Boston type I keratoprosthesis: improving outcomes and expanding indications. Ophthalmology. 2009;116(4):640–651. doi: 10.1016/j.ophtha.2008.12.058. [DOI] [PubMed] [Google Scholar]
- 10.Falcinelli G, Falsini B, Taloni M, Colliardo P. Modified osteo-odonto-keratoprosthesis for treatment of corneal blindness: long-term anatomical and functional outcomes in 181 cases. Arch Ophthalmol. 2005;123(10):1319–1329. doi: 10.1001/archopht.123.10.1319. [DOI] [PubMed] [Google Scholar]
- 11.Liu C, Okera S, Tandon R, Herold J, Hull C, Thorp S. Visual rehabilitation in end-stage inflammatory ocular surface disease with the osteo-odonto-keratoprosthesis: results from the UK. Br J Ophthalmol. 2008;92(9):1211–1217. doi: 10.1136/bjo.2007.130567. [DOI] [PubMed] [Google Scholar]
- 12.Tan DT, Tay AB, Theng JT, Lye KW, Parthasarathy A, Por YM, et al. et al. Keratoprosthesis surgery for end-stage corneal blindness in asian eyes. Ophthalmology. 2008;115(3):503–10 e3. doi: 10.1016/j.ophtha.2007.04.065. [DOI] [PubMed] [Google Scholar]
- 13.Hicks CR, Crawford GJ, Lou X, Tan DT, Snibson GR, Sutton G, Downie N, Werner L, Chirila TV, Constable IJ. Corneal replacement using a synthetic hydrogel cornea, AlphaCor: device, preliminary outcomes and complications. Eye (Lond) 2003;17(3):385–392. doi: 10.1038/sj.eye.6700333. [DOI] [PubMed] [Google Scholar]
- 14.Hicks CR, Crawford GJ, Dart JK, Grabner G, Holland EJ, Stulting RD, Tan DT, Bulsara M. AlphaCor: Clinical outcomes. Cornea. 2006;25(9):1034–1042. doi: 10.1097/01.ico.0000229982.23334.6b. [DOI] [PubMed] [Google Scholar]
- 15.Crawford GJ, Hicks CR, Lou X, Vijayasekaran S, Tan D, Mulholland B, Chirila TV, Constable IJ. The Chirila Keratoprosthesis: phase I human clinical trial. Ophthalmology. 2002;109(5):883–889. doi: 10.1016/s0161-6420(02)00958-2. [DOI] [PubMed] [Google Scholar]
- 16.Holak SA, Holak HM, Bleckmann H. AlphaCor keratoprosthesis: postoperative development of six patients. Graefes Arch Clin Exp Ophthalmol. 2009;247(4):535–539. doi: 10.1007/s00417-008-0964-7. [DOI] [PubMed] [Google Scholar]
- 17.Kim MK, Lee SM, Lee JL, Chung TY, Kim YH, Wee WR, Lee JH. Long-term outcome in ocular intractable surface disease with Seoul-type keratoprosthesis. Cornea. 2007;26(5):546–551. doi: 10.1097/ICO.0b013e3180415d35. [DOI] [PubMed] [Google Scholar]
- 18.Ghaffariyeh A, Honarpisheh N, Karkhaneh A, Abudi R, Moroz ZI, Peyman A, Faramarzi A, Abasov F. Fyodorov-Zuev keratoprosthesis implantation: long-term results in patients with multiple failed corneal grafts. Graefes Arch Clin Exp Ophthalmol. 2011;249(1):93–101. doi: 10.1007/s00417-010-1493-8. [DOI] [PubMed] [Google Scholar]
- 19.Hollick EJ, Watson SL, Dart JK, Luthert PJ, Allan BD. Legeais BioKpro III keratoprosthesis implantation: long term results in seven patients. Br J Ophthalmol. 2006;90(9):1146–1151. doi: 10.1136/bjo.2006.092510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iakymenko SA. Keratoprosthesis - 40-years experience of study and application in the Filatov Institute (analysis of 1000 operations) Abstract Book of World Ophthalmology Congress; Berlin. 2010;2010:41. [Google Scholar]