Abstract
AIM
To evaluate the efficacy of intralesional radiofrequency ablation in the treatment of periorbital syringomas.
METHODS
We tried the intralesional radiofrequency ablation for 64 patients with periorbital syringomas from 2007 to 2011. The operation was performed under 2.5 loupe magnifications. The handpiece was assembled with a needle electrode and connected to the radiofrequency ablation apparatus. The electrode was then inserted into the target lesions in dermis and delivering injury to the base of these tumors. Results were assessed clinically by comparing pre- and post-treatment photographs and patient satisfaction rates.
RESULTS
Clinical improvement increased with each subsequent treatment session. The percent of patients whose clinic improvement grade were≥3 after each session was respectively 71.9%(Session1), 83.3%(Session2), and 100%(Session3). The statistical results indicated the concordance of the clinical assessment and the satisfaction level of patients (kappa=0.78 of the session1; kappa=0.82 of the session2). The majority of patients had good or excellent cosmetic results. Postoperatively, there were no permanent side effects or recurrences.
CONCLUSION
As a new technique of minimally invasion, the intralesional radiofrequency ablation was found to be an effective, inexpensive, highly precise and safe way of treating periorbital syringomas.
Keywords: periorbital syringomas, radiofrequency ablation, treatment
INTRODUCTION
Syringomas are common benign adnexal tumors derived from intradermal eccrine ducts. They mainly appear in the periorbital areas, and cause significant and awkward cosmetic problems. Histologically, syringomas consist of dermal tumors with epidermal cysts. The bulk of the abnormal tissue can extend as far down as the upper reticular dermis, making these tumors resistant to superficial surgical destruction[1]. For delicate periobital skin, a prerequisite for the optimal treatment for periorbital syringomas is the complete destruction of the lesions with minimal adverse effects. Previously different treatment modalities have been described for these lesions including surgical excision, cryotherapy, chemical peeling, electrodesiccation, laser therapy, and nonablative fractional photothermolysis. Although most treatments have shown some degree of efficacy, all therapies have the potential for scarring, pigmentary changes and tumor recurrence. The radiofrequency ablation technique has been widely used in the ablation of some types of tumor[2]-[5]. As a technique of minimally invasion, it has the advantage of deep and precise tissue penetration, causing separately and thoroughly eliminate target tissues. Since syringomas are present in the papillary layer and deeply embedded within the dermis, the destructive method used must be capable of penetrating to this depth and have little injury to the normal tissue. The objective of the present study was to carry out intralesional radiofrequency ablation, which allowed for the selective destruction of dermal lesions with little damage to the surrounding normal epidermis, to treat periorbital syringomas.
MATERIALS AND METHODS
Subjects
The Institutional Review Board of PLA General Hospital, Beijing, China, approved this study. The study was started in July 2007 and carried out over a period of 4 years. After obtaining informed consent, we treated the periorbital syringomas of 64 Asian patients (62 women and 2 men; mean age 42 years, range 21–60 years; Fitzpatrick skin type: III-IV) with intralesional radiofrequency ablation. All of the patients had been diagnosed with syringomas for at least 2 years. Patients were excluded if they had experienced treatment within the previous 6 months, had a propensity for keloids or were immunosuppressed.
Methods
Local anesthesia was achieved with injection of 2% lidocaine solution into the involved areas of the eyelids and upper cheeks. The treatment was performed under 2.5 loupe magnifications. The handpiece was assembled with a sharp steel syringe needle of 0.33mm diameter and connected to the radiofrequency ablation apparatus (40.0MHz, 30W) (RASXL-II Tian-ding-kang, Corporation, Beijing, China). The needle electrode was then inserted directly into the center of each lesion at a depth of 0.5 to 1.0mm. At the same time, high frequency current was delivered to the needle for about 1 to 2 seconds to ablate the abnormal tissue. Then the needle electrode was rapidly withdrawn. For isolated lesions the operation was carried out only once. Furthermore, for confluent or conglomerate lesions, the needle was repeatedly inserted into plaque-type lesions at intervals 1 to 3 mm. Depending on the severity of the lesions they were treated for one to three sessions. The intervals between treatment sessions were about 8 weeks. Immediately after treatment, mild swelling and erythema with tiny crusting were seen in the treated lesions. All of the patients tolerated the treatment without undue problems. Postoperatively, patients were instructed to apply a topical antibiotic ointment during the first 3 to 5 days after treatment, to lessen the swelling and minimize any risk of infection.
Objective and Subjective Evaluations
Before their operation, each patient underwent digital photography. After a period of 8 weeks from each session, photographs were taken again. Two dermatologists blinded to the treatments performed objective clinical assessments of the syringomas. They counted the number of lesions and compared the before and after photos in none chronological order, using a global improvement scale (grade 0, worsened; grade 1, minimal improvement of 0-25% or steady state; grade 2, moderate improvement of 26-50%; grade 3, marked improvement of 51–75%; and grade 4, near total improvement of >75%,)[6]. Patients were asked to rate their overall satisfaction level with the treatment at 8 weeks after each session. (Grade 0: worsened; Grade 1: poor; Grade 2: slightly satisfied; Grade 3: satisfied; and Grade 4: very satisfied).
Statistical Analysis
The Kappa statistic test with SPSS 16.0 was used to evaluate the concordance of clinical assessment scores and patient satisfaction rates. The concordance of assessment were considered statistically significant when the kappa value was 0.75<K≤1.
RESULTS
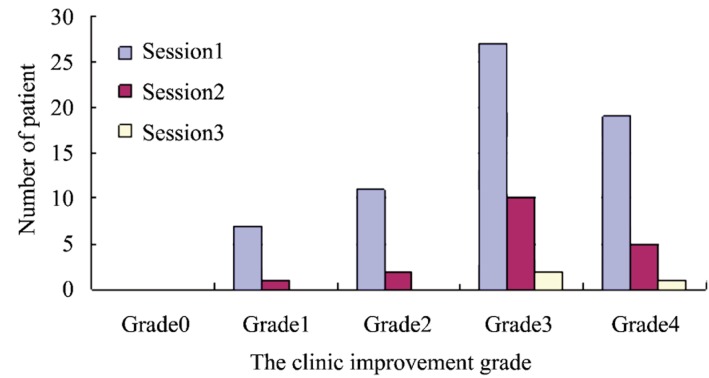
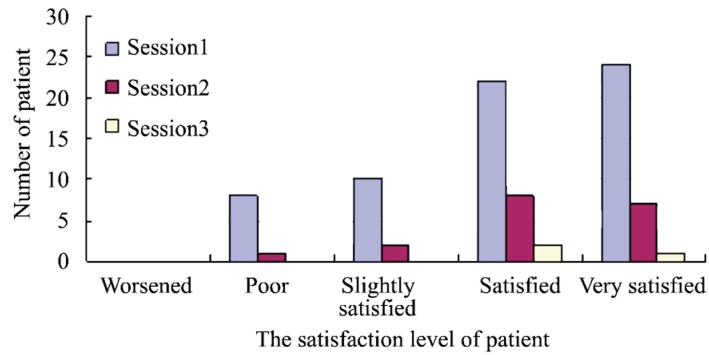
All patients accepted being followed-up for 1 to 12 months. Most of the patients were treated in only one session (46 patients, 71.9%). The patients with multiple lesions needed 2-3 sessions to completely eliminate the benign tumors (15 patients received two sessions, 23.4%; 3 patients received three sessions, 4.7%). The clinic improvement and satisfaction level of patients were evaluated at 8 weeks after each session and detailed in the Figure 1 and Figure 2. Along the subsequent treatment sessions, the percent of patients whose clinic improvement grade were≥3 after each session was respectively 71.9%(Session1), 83.3%(Session2) and 100%(Session3). The mean clinical improvement grade was respectively 2.9±0.9(Session1), 3.0±0.8(Session2) and 3.3±0.5(Session3). The statistical results indicated the concordance of the clinical assessment and the satisfaction level of patients (Table 1 and Table 2). Postoperatively in all patients, the scab was formed in the focal areas and the time of decrustation was 1 to 5 days. Temporary erythema and hyper pigmentation occurred in the majority of patients and then cleared spontaneously in 2 to 3 months. After 6 months from the termination of the treatment session, most patients were pleased with the results, complained of no major adverse effects and remained free of recurrence (Figure 3-5).
Figure 1. Grades of clinical improvement reported after each treatment session with intralesional radiofrequency ablation compared with the baseline.
Figure 2. Patient satisfaction levels after each treatment session with intralesional radiofrequency ablation.
Table 1. Curative effect evaluation from dermatologists and patients of the first session.
| No. of patients for the each satisfaction level | No. of patients of the each clinic improvement grade |
Total | ||||
| Grade0 | Grade1 | Grade2 | Grade3 | Grade4 | ||
| Worsened | 0 | 0 | 0 | 0 | 0 | 0 |
| Poor | 0 | 6 | 2 | 0 | 0 | 8 |
| Slightly satisfied | 0 | 1 | 8 | 1 | 0 | 10 |
| Satisfied | 0 | 0 | 1 | 21 | 0 | 22 |
| Very satisfied | 0 | 0 | 0 | 5 | 19 | 24 |
| Total | 0 | 7 | 11 | 27 | 19 | 64 |
Kappa =0.78
Table 2. Curative effect evaluation from dermatologists and patients of the second session.
| No. of patients for the each satisfaction level | No. of patients of the each clinic improvement grade |
Total | ||||
| Grade0 | Grade1 | Grade2 | Grade3 | Grade4 | ||
| Worsened | 0 | 0 | 0 | 0 | 0 | 0 |
| Poor | 0 | 1 | 0 | 0 | 0 | 1 |
| Slightly satisfied | 0 | 0 | 2 | 0 | 0 | 2 |
| Satisfied | 0 | 0 | 0 | 8 | 0 | 8 |
| Very satisfied | 0 | 0 | 0 | 2 | 5 | 7 |
| Total | 0 | 1 | 2 | 10 | 5 | 18 |
Kappa =0.82
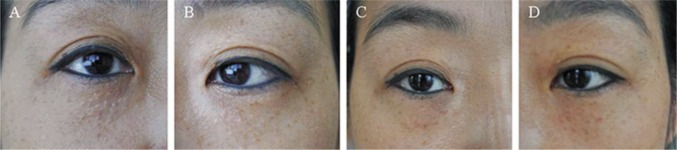
Figure 3. A 43-year-old Chinese woman presented with syringomas on her upper and lower eyelids (A and B). After one session of intralesional radiofrequency ablation the clinical improvement of the periorbital syringomas was grade 4 (C and D).
Figure 5. A 28-year-old Chinese woman presented with syringomas mostly on her upper eyelids (A). After one session of intralesional radiofrequency ablation the clinical improvement of the periorbital syringomas was grade 4 (B).

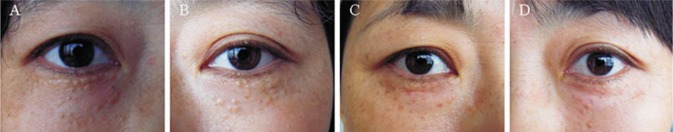
Figure 4. A 52-year-old Chinese woman presented with syringomas mostly on her lower eyelids (A and B). After two sessions of intralesional radiofrequency ablation the clinical improvement of the periorbital syringomas was grade 3 (C and D).
DISCUSSION
The unsightly appearance of periorbital syringomas has been a cosmetically debilitating problem. There are strong demands for treatment to achieve an aesthetic improvement. Features of syringomas from skin biopsies include the existence of epithelial funiculars that indicate the structure of lumen formation in the upper dermis through to the intercellular layer of the dermis[7]. Due to the deep embedment of syringomas within the dermis, complete removal is often unsuccessful and recurrence frequently takes place[8]. There are various traditional methods for treating syringomas such as excision[9], cryosurgery[10], electrosurgery[11], topical atropine or tretinoin applications[12],[13], chemical peeling[14],[15] and laser ablation[16],[17]. However, all of the established treatment modalities have proved to be not only nonspecific to the target tissue but also destructive to the neighboring normal tissue. So the risk of postoperative complications such as erythema, pigmentary changes and scarring was increased. Some other treatments such as the Q-switched Nd:YAG laser treatment after temporary tattooing of the lesions[18], the multiple drilling method using a super pulse mode CO2 laser[6],[19] and nonablative fractional photothermolysis[20] were introduced. However, little improvement was reported in relation to the cosmetic problems from epidermal injury, or in the low efficacy rate due to incomplete destruction of deep dermal lesions[21]. The optimal treatment for periorbital syringomas is selective ablation of the dermal target lesions in the intercellular layer of the dermis, with little damage to normal epidermal tissue. In addition, due to the presence of delicate periorbital skin, the requirement for high precision in the application of the ablating technique is very strict. In our study, we treated patients with the intralesional radiofrequency ablation technique and obtained successful results.
Over the last two decades, great progress has been made in the treatment of diseases using radiofrequency ablation technology, because of its distinguishing characteristic of only inducing tissue microtrauma due to effective targeting with almost no side-effects. The use of radiofrequency ablation in treating solid tumors and benign diseases of solid organs has gradually increased, and is now widely used in almost every system of the body. It has been successfully used in the treatment of intervertebral disc protrusion[22], the prostatic hypertrophy[23], the rosacea[24] and so on. The radiofrequency ablation device transfers electromagnetic waves to the target tissues via a treatment electrode. The electrical resistance of human tissue helps convert this electromagnetic energy into molecular energy, which causes denaturation of intracellular and extracellular proteins resulting in coagulation effects[25]. The radiofrequency ablation technique has many advantages, such as high precision, no bleeding and less damage to other surrounding tissues.
In studies by Karam and Benedetto, syringomas were treated with short bursts of high frequency low voltage delivered with an epilating needle electrode that was inserted into the center of the lesions causing electrodesiccation[1],[26]. However, it is well known that electrodesiccation (from the Latin desiccare, to dry up) causes superficial damage due to low tissue penetration, and electrofulguration (from the Latin fulgur, lightening) also induces superficial tissue damage. In contrast, electrocoagulation has the advantage of deeper tissue penetration and effective tissue destruction, thus providing longer therapeutic effects[27]. In a study by Al Aradi IK, syringomas were treated with a dual-frequency 4 MHz radiofrequency device in which the electrode was only contacted superficially to the area of lesions[28]. Therefore, deep seated tumors could not be removed effectively using this approach.
In this study, we tried the intralesional radiofrequency ablation as a new technique of the minimally invasion for patients with periorbital syringomas. We used a sharp steel syringe needle attached to the handpiece of the radiofrequency ablation apparatus. The needle was inserted deeply enough into each lesion to deliver injury to the base of these tumors. The operation was performed under 2.5 loupe magnification and the electrode was a sharp steel needle of 0.33mm diameter. This made the visual field clearer, the operation process more convenient, the ablation accuracy easier to control and further enhanced the precision of the treatment. The radiofrequency ablation technique is an approach in which the electromagnetic wave is transmitted via an electrode to vibrate the molecules of the tissues with which it comes into contact[29]. Because only the contacted tissues are ablated, virtually little harm is done to adjacent tissues that are not in contact with the electrode, and thermal conduction to the normal skin is reduced. Another advantage of the intralesional radiofrequency ablation method is that each deep seated lesion can be removed effectively, and the unharmed adjacent normal tissues between each lesion are helpful in achieving a good recovery. This method also can remove confluent or conglomerate lesions with little normal tissue injury, but requires several treatment sessions in exchange for the lower risk of side effects. The operating frequency of this device was 40 MHz and the power output was 30 W. This setting of frequency and power resulted in safe, precise and rapid tumor ablation. A drawback of the method is that due to the necessity of inserting the needle into each lesion, each session took a long time to achieve complete removal of the tumor. However, the clinical efficacy and cosmetic outcome from the intralesional radiofrequency ablation method were excellent.
In conclusion, intralesional radiofrequency ablation is an effective, inexpensive, highly precise and safe way of treating periorbital syringomas. However, further study of the histological features of the local area treated with this therapy is required. As more experience with intralesional radiofrequency ablation of periorbital syringomas is gained, it is essential to give more thought to the treatment of syringomas at other sites using this method.
Footnotes
Foundation item: Supported by Military Medical Specialized Research Fund in the 11th Five-Year Period, China (No. 200626Z000058)
REFERENCES
- 1.Karam P, Benedetto AV. Intralesional electrodesiccation of syringomas. Dermatol Surg. 1997;23(10):921–924. doi: 10.1111/j.1524-4725.1997.tb00749.x. [DOI] [PubMed] [Google Scholar]
- 2.de Baere T. Radiofrequency ablation of liver and lung tumors. J Radiol. 2011;92(9):825–834. doi: 10.1016/j.jradio.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Kim JH, Kim TH, Kim SD, Lee KS, Sung GT. Radiofrequency ablation of renal tumors: our experience. Korean J Urol. 2011;52(8):531–537. doi: 10.4111/kju.2011.52.8.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Vilsteren FG, Pouw RE, Seewald S, Alvarez Herrero L, Sondermeijer CM, Visser M, Ten Kate FJ, Yu Kim Teng KC, Soehendra N, Rosch T, Weusten BL, Bergman JJ. Stepwise radical endoscopic resection versus radiofrequency ablation for Barrett's oesophagus with high-grade dysplasia or early cancer: a multicentre randomised trial. Gut. 2011;60(6):765–773. doi: 10.1136/gut.2010.229310. [DOI] [PubMed] [Google Scholar]
- 5.Ilaslan H, Schils J, Joyce M, Marks K, Sundaram M. Radiofrequency ablation: another treatment option for local control of desmoid tumors. Skeletal Radiol. 2010;39(2):169–173. doi: 10.1007/s00256-009-0807-6. [DOI] [PubMed] [Google Scholar]
- 6.Cho SB, Kim HJ, Noh S, Lee SJ, Kim YK, Lee JH. Treatment of syringoma using an ablative 10,600-nm carbon dioxide fractional laser: a prospective analysis of 35 patients. Dermatol Surg. 2011;37(4):433–438. doi: 10.1111/j.1524-4725.2011.01915.x. [DOI] [PubMed] [Google Scholar]
- 7.Elder D ER, Jaworsky C, Johnson B., Jr . 8th ed. Philadelphia: Lippincott-Raven; 1997. Lever's histopathology of the skin; pp. 778–779. [Google Scholar]
- 8.Cho SB, Lee SH, Lee SJ, Lee JE, Kim DH. Syringoma treated with pinhole method. J Eur Acad Dermatol Venereol. 2009;23(7):852–853. doi: 10.1111/j.1468-3083.2008.03051.x. [DOI] [PubMed] [Google Scholar]
- 9.Stevenson TR, Swanson NA. Syringoma: removal by electrodesiccation and curettage. Ann Plast Surg. 1985;15(2):151–154. doi: 10.1097/00000637-198508000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Belardi MG, Maglione MA, Vighi S, di Paola GR. Syringoma of the vulva. A case report. J Reprod Med. 1994;39(12):957–959. [PubMed] [Google Scholar]
- 11.Langtry JA, Carruthers A. Electrocautery for treating periorbital syringomas. Dermatol Surg. 1998;24(6):691–692. [PubMed] [Google Scholar]
- 12.Sanchez TS, Dauden E, Casas AP, Garcia-Diez A. Eruptive pruritic syringomas: treatment with topical atropine. J Am Acad Dermatol. 2001;44(1):148–149. doi: 10.1067/mjd.2001.109854. [DOI] [PubMed] [Google Scholar]
- 13.Gomez MI, Perez B, Azana JM, Nunez M, Ledo A. Eruptive syringoma: treatment with topical tretinoin. Dermatology. 1994;189(1):105–106. doi: 10.1159/000246803. [DOI] [PubMed] [Google Scholar]
- 14.Kang WH, Kim NS, Kim YB, Shim WC. A new treatment for syringoma. Combination of carbon dioxide laser and trichloroacetic acid. Dermatol Surg. 1998;24(12):1370–1374. [PubMed] [Google Scholar]
- 15.Frazier CC, Camacho AP, Cockerell CJ. The treatment of eruptive syringomas in an African American patient with a combination of trichloroacetic acid and CO2 laser destruction. Dermatol Surg. 2001;27(5):489–492. doi: 10.1046/j.1524-4725.2001.00167.x. [DOI] [PubMed] [Google Scholar]
- 16.Wang JI, Roenigk HH., Jr Treatment of multiple facial syringomas with the carbon dioxide (CO2) laser. Dermatol Surg. 1999;25(2):136–139. doi: 10.1046/j.1524-4725.1999.08111.x. [DOI] [PubMed] [Google Scholar]
- 17.Kopera D, Soyer HP, Cerroni L. Vulvar syringoma causing pruritus and carcinophobia: treatment by argon laser. J Cutan Laser Ther. 1999;1(3):181–183. doi: 10.1080/14628839950516850. [DOI] [PubMed] [Google Scholar]
- 18.Park HJ, Lim SH, Kang HA, Byun DG, Houh D. Temporary tattooing followed by Q-switched alexandrite laser for treatment of syringomas. Dermatol Surg. 2001;27(1):28–30. [PubMed] [Google Scholar]
- 19.Park HJ, Lee DY, Lee JH, Yang JM, Lee ES, Kim WS. The treatment of syringomas by CO(2) laser using a multiple-drilling method. Dermatol Surg. 2007;33(3):310–313. doi: 10.1111/j.1524-4725.2007.33065.x. [DOI] [PubMed] [Google Scholar]
- 20.Akita H, Takasu E, Washimi Y, Sugaya N, Nakazawa Y, Matsunaga K. Syringoma of the face treated with fractional photothermolysis. J Cosmet Laser Ther. 2009;11(4):216–219. doi: 10.3109/14764170903352860. [DOI] [PubMed] [Google Scholar]
- 21.Hong SK, Lee HJ, Cho SH, Seo JK, Lee D, Sung HS. Syringomas Treated by Intralesional Insulated Needles without Epidermal Damage. Ann Dermatol. 2010;22(3):367–369. doi: 10.5021/ad.2010.22.3.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kapural L. Intervertebral disk cooled bipolar radiofrequency (intradiskal biacuplasty) for the treatment of lumbar diskogenic pain: a 12-month follow-up of the pilot study. Pain Med. 2008;9(4):407–408. doi: 10.1111/j.1526-4637.2008.00464.x. [DOI] [PubMed] [Google Scholar]
- 23.Savoie PH, Lopez L, Simonin O, Loubat M, Bladou F, Serment G, Karsenty G. Two-years follow-up of radiofrequency thermotherapy for urination disorders due to benign prostatic hyperplasia. Prog Urol. 2009;19(7):501–506. doi: 10.1016/j.purol.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 24.Erisir F, Isildak H, Haciyev Y. Management of mild to moderate rhinophyma with a radiofrequency. J Craniofac Surg. 2009;20(2):455–456. doi: 10.1097/SCS.0b013e31819b9830. [DOI] [PubMed] [Google Scholar]
- 25.Hainer BL. Electrosurgery for the skin. Am Fam Physician. 2002;66(7):1259–1266. [PubMed] [Google Scholar]
- 26.Karam P, Benedetto AV. Syringomas: new approach to an old technique. Int J Dermatol. 1996;35(3):219–220. doi: 10.1111/j.1365-4362.1996.tb01647.x. [DOI] [PubMed] [Google Scholar]
- 27.Pollack SV. 1st ed. New York: Churchill Livingstone; 1991. Electrosurgery of the skin; pp. 37–50. [Google Scholar]
- 28.Al Aradi IK. Periorbital syringoma: a pilot study of the efficacy of low-voltage electrocoagulation. Dermatol Surg. 2006;32(10):1244–1250. doi: 10.1111/j.1524-4725.2006.32284.x. [DOI] [PubMed] [Google Scholar]
- 29.Jiang TY, Wang XL, Suo W, He QH, Xiao HY. Radiofrequency ablation technique eradicating palpebral margin neoplasm. Int J Ophthalmol. 2011;4(2):186–189. doi: 10.3980/j.issn.2222-3959.2011.02.16. [DOI] [PMC free article] [PubMed] [Google Scholar]