Abstract
AIM
To evaluate the corneal endothelial cell density and morphology in Chinese patients with pseudoexfoliation syndrome (PEX).
METHODS
Medical records of 16 patients (20 eyes) with PEX who presented to our institution between July 2008 and June 2010 were retrospectively reviewed. Thirteen eyes had combined glaucoma. The information of five apparently normal fellow eyes in these patients was also recorded. Left eyes of 20 patients with bilateral senile cataracts but no other eye disease were included as controls. Specular microscopy was performed in all eyes to analyze for corneal endothelial cell density and morphology. Cell density, coefficient of variation in cell size, and percentage of hexagonal cells in corneal endothelium were evaluated.
RESULTS
The mean corneal endothelial cell density in the PEX eyes was 2298±239 cells/mm2, significantly lower than that in the cataract eyes (2652±18 cells/mm2, P=0.026), but there were no significant differences in coefficient of variation of cell size and frequency of hexagonality between these two groups. No significant differences in the three parameters were found between the apparently normal fellow eyes and the PEX eyes or the cataract eyes, or between the PEX eyes with and without glaucoma.
CONCLUSION
Corneal endothelial cell density may decrease in Chinese patients with PEX. The development of glaucoma in PEX eyes does not seem to be related with the change in corneal endothelial cell density or morphology.
Keywords: corneal endothelial cell density, pseudoexfoliation syndrome, corneal morphology
INTRODUCTION
Pseudoexfoliation syndrome (PEX) is a common age-related disease clinically diagnosed by the formation or deposition of abnormal fibrillar material upon some intraocular structures[1]. Deposition of pseudoexfoliative material on corneal endothelium, anterior lens surface, iris, trabecular meshwork, zonula, and ciliary body[2],[3] may lead to various ocular complications, such as chronic open-angle glaucoma, lens subluxation, poor mydriasis[4],[5], and zonular dehiscence, capsular rupture or vitreous loss at the time of cataract extraction[2]. Corneal endothelial changes have also been reported, including decreased cell density, higher coefficient of variation in cell size, and lower percentage of hexagonal cells[6]-[8]. On the other hand, some studies reported no such significant changes in eyes with PEX[9].
By far, the characteristics of corneal endothelium in Chinese patients with PEX have been unclear. This study aimed to evaluate the corneal endothelial cell density and morphology in eyes diagnosed with this syndrome at our institution.
PATIENTS AND METHODS
Materials
This study conformed to the guidelines of the Declaration of Helsinki. PEX was diagnosed if abnormal fibrillar material was present on the anterior lens capsule and/or pupillary margin. The diagnosis of pseudoexfoliative glaucoma was based on the findings of an elevated intraocular pressure (>21mmHg), typical glaucomatous cupping of the optic nerve head, and visual field defects. Twenty consecutive PEX eyes in nine men (ten eyes) and seven women (ten eyes) who visited our institution between July 2008 and June 2010 were included(Table 1). Mean patient age was 69.1±17.7 years (range 53-78 years). Among them, 13 eyes developed glaucoma. Five apparently normal fellow eyes from the same 16 patients were also examined.
Table 1. Clinicial data of patients with PEX.
| Patient | Sex | Age | Eye | Glaucoma | Cell density (cells/mm2) | Coefficient of variation in cell size (%) | Hexagonal cells (%) |
| 1 | F | 68 | OD | P | 2312 | 36 | 42 |
| OS | P | 2505 | 32 | 60 | |||
| 2 | M | 74 | OD | P | 2457 | 24 | 65 |
| OS | P | - | - | - | |||
| 3 | M | 78 | OD | P | - | - | - |
| OS | P | 2723 | 30 | 33 | |||
| 4 | F | 77 | OD | P | - | - | - |
| OS | P | 812 | 37 | 52 | |||
| 5 | M | 53 | OD | P | 1923 | 35 | 54 |
| OS | P | 2048 | 36 | 69 | |||
| 6 | M | 63 | OD | P | - | - | - |
| OS | P | 669 | 34 | 63 | |||
| 7 | M | 65 | OD | P | 2695 | 26 | 72 |
| OS | P | - | - | - | |||
| 8 | F | 68 | OD | P | 3105 | 34 | 47 |
| OS | P | 2500 | 43 | 63 | |||
| 9 | M | 75 | OD | P | 2754 | 40 | 32 |
| OS | P | - | - | - | |||
| 10 | M | 63 | OD | P | 1926 | 44 | 49 |
| OS | P | - | - | - | |||
| 11 | F | 53 | OD | N | - | - | - |
| OS | N | 2664 | 36 | 77 | |||
| 12 | F | 72 | OD | N | 2762 | 29 | 63 |
| OS | N | - | - | - | |||
| 13 | M | 75 | OD | N | - | - | - |
| OS | N | 17 | 2722 | 26 | |||
| 14 | F | 67 | OD | N | 14 | 2293 | 23 |
| OS | N | - | - | - | |||
| 15 | OD | N | 10 | 2253 | 50 | ||
| OS | N | 11 | 2583 | 45 | |||
| 16 | M | 78 | OD | N | - | - | - |
| OS | N | 11 | 2262 | 25 |
P: Positive(with glaucoma); N: Negative(without glaucoma); -: Excluded because of previous intraocular surgery.
Moreover, left eyes of 20 patients (11 men and nine women) with bilateral senile cataracts were evaluated as controls. Mean patient age was 69.5±19.1 years (range 52-79 years). All 20 eyes had been examined with dilated pupil and no other disorders or pseudoexfoliative material was observed.
Methods
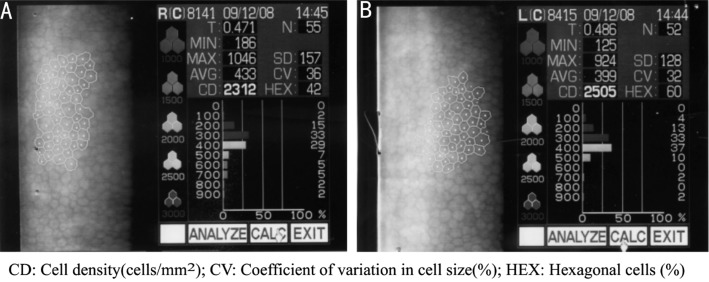
All eyes in this study had no previous intraocular surgery. Their central corneal endothelial cells were detected by specular microscopy (Topcon, Tokyo, Japan) and photographed for analysis of cell density and hexagonality, and coefficient of variation in cell size(Figure 1). The unpaired t-test was used to compare differences between any two groups among the PEX eyes, their apparently normal fellow eyes, and the cataract eyes, as well as between the PEX eyes with and without glaucoma. P<0.05 was considered statistically significant.
Figure 1. Results of corneal endothelium test in patient No.1.
A: OD; B: OS.
RESULTS
The data of corneal endothelial cells in all eyes are listed in Tables 2 and 3. The mean endothelial cell density in the PEX eyes (2298±239 cells/mm2) was significantly lower than that in the cataract eyes (2652±18 cells/mm2) (P =0.026). However, neither the coefficient of variation in cell size nor the percentage of hexagonal cells was significantly different between these two groups. In addition, there were no statistically significant differences in the three parameters between the apparently normal fellow eyes and the PEX eyes or the cataract eyes, or between the PEX eyes with and without glaucoma.
Table 2. Data of corneal endothelium in PEX, cataract, and apparently normal fellow eyes.
| Cell density (cells/mm2) | Coefficient of variation in cell size (%) | Hexagonal cells (%) | |
| Pseudoexfoliation syndrome (n=20) | 2298±239* | 34.7±7.1 | 54.5±2.8 |
| Apparently normal fellow eyes (n=5) | 2568±172 | 34.6±1.4 | 59.4±9.9 |
| Cataract (n=20) | 2652±18 | 36±1.4 | 56.1±10.6 |
*P<0.05 compared with the cataract eyes
(mean±standard deviation)
Table 3. Data of corneal endothelium in PEX eyes with and without glaucoma.
| With glaucoma (n=13) | Without glaucoma (n=7) | P | |
| Cell density (cells/mm2) | 2186±2 | 2505±284 | 0.278 |
| Coefficient of variation in cell size (%) | 34.7±6.4 | 33.4±7.8 | 0.777 |
| Hexagonal cells (%) | 53.9±3.5 | 55.1±19.1 | 0.847 |
(mean ± standard deviation)
DISCUSSION
The prevalence rate of PEX in different populations is various: 9.6% in Iran[10], 3.8% in India[11], 3.4% in Japan[12], and 0.32% in Singapore[13]. Young et al[14] reported a rate of 0.4% in Chinese patients aged 60 or above in a hospital based epidemiology study.
The mechanism involved in the pathobiology of this syndrome remains obscure. A “protein sink model” was proposed to explain the formation of the pseudoexfoliative material. It speculates that there is an aberrant nucleation protein or nucleation protein complex binding to other proteins. These proteins form a more complex unstable protein matrix in the aqueous humor of the eye, which eventually develops into the pseudoexfoliative material that deposits upon some intraocular structures[15]. When the corneal endothelium is affected, the cornea becomes irregular, discontinuous and edematous, and may result in corneal endothelial decompensation[16],[17].
In the current study, the difference was statistically significant in corneal endothelial cell density, but not in coefficient of variation of cell size and percentage of hexagonal cells between the PEX eyes and the cataract eyes. This is similar to the results reported by Inoue et al[18], who made comparisons between the eyes with PEX and those with senile cataract or refractive error. Miyanke et al[6], however, observed not only decreased cell density but also reduced cell hexagonality and increased coefficient of variation in cell size in the PEX eyes compared to the cataract eyes. They also reported statistically significant differences in coefficient of variation of cell size and percentage of hexagonal cells between the apparently normal fellow eyes of PEX eyes and the cataract eyes, which is different from the findings in our series that neither of the parameters between the two groups of eyes was significantly different.
It was reported that the endothelial cell density was not correlated with the severity of glaucoma[19]. Morphologic changes of corneal endothelium can occur in PEX eyes even with normal intraocular pressure[20]. In this study, corneal endothelial cell density, coefficient of variation in cell size, and percentage of hexagonal cells in eyes with pseudoexfoliative glaucoma had no significant differences compared to those without glaucoma. This is consistent with the outcomes of the investigations by Hattori[8], Päivi et al[9], and Inoue et al[18]. According to Seitz et al[21], however, the cell density in PEX eyes with glaucoma was significantly lower than those without glaucoma.
Moreover, changes of corneal endothelium in PEX eyes may cause trouble when patients need intraocular surgery. Quiroga et al[7] reported that PEX increased the risk of corneal endothelial decompensation after cataract surgery. In their study, endothelial cell density in 21.87% of PEX eyes was less than 2000 cells/mm2 and considered to be risky. In the current study, we also found a high prevalence of low endothelial cell density in PEX eyes (20%). Therefore, evaluation of preoperative corneal endothelium is suggested for PEX patients who are scheduled for intraocular surgery to help with the selection of surgical approach. The small sample size in this study, which can be attributed to the low prevalence of PEX in Chinese people, may lead to bias. Further investigations with much more samples are needed so as to provide more information for eye doctors.
REFERENCES
- 1.Schlötzer-Schrehardt U, Naumann GO. Ocular and systemic pseudoexfoliation syndrome. Am J Ophthalmol. 2006;141:921–937. doi: 10.1016/j.ajo.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 2.Ritch R. Exfoliation Syndrome. Surv Ophthalmol. 2001;45:265–315. doi: 10.1016/s0039-6257(00)00196-x. [DOI] [PubMed] [Google Scholar]
- 3.Ritch R. Exfoliation syndrome and occludable angles. Trans Am Ophthalmol Soc. 1994;92:845–944. [PMC free article] [PubMed] [Google Scholar]
- 4.Ritch R, Schlötzer-Schrehardt U. Exfoliation syndrome. Surv Ophthalmol. 2001;45:265–315. doi: 10.1016/s0039-6257(00)00196-x. [DOI] [PubMed] [Google Scholar]
- 5.Alfaiate M, Leite E, Mira J, Cunha-Vaz J. G. Prevalence and surgical complications of pseudoexfoliation syndrome in Portuguese patients with senile cataract. J Cataract Refract Surg. 1996;22:972–976. doi: 10.1016/s0886-3350(96)80202-1. [DOI] [PubMed] [Google Scholar]
- 6.Miyake K, Matsuda M, Inaba M. Corneal endothelial changes in pseudoexfoliation syndrome. Am J Ophthalmol. 1989;108:49–52. doi: 10.1016/s0002-9394(14)73259-3. [DOI] [PubMed] [Google Scholar]
- 7.Quiroga L, Lansingh VC, Samudio M, Pena FY, Cater MJ. Characteristics of the corneal endothelium and pseudoexfoliation syndrome in patients with senile cataract. Clin Exp Ophthalmol. 2010;38:449–455. doi: 10.1111/j.1442-9071.2010.02313.x. [DOI] [PubMed] [Google Scholar]
- 8.Hattori Y. Corneal endothelial examination of pseudoexfoliation syndrome. Nippon Ganka Gakkai Zasshi. 1990;94:957–963. [PubMed] [Google Scholar]
- 9.Päivi P, Vasara K, Harju M, Setälä K. Corneal thickness and corneal endothelium in normotensive subjects with unilateral exfoliation syndrome. Graefes Arch Clin Exp Ophthalmol. 2000;238:659–663. doi: 10.1007/s004170000159. [DOI] [PubMed] [Google Scholar]
- 10.Nouri-Mahdavi K, Nosrat N, Sahebghalam R, Jahanmard M. Pseudoexfoliation syndrome in central Iran: a population-based survey. Acta Ophthalmol Scand. 1999;77:581–584. doi: 10.1034/j.1600-0420.1999.770521.x. [DOI] [PubMed] [Google Scholar]
- 11.Arvind H, Raju P, Paul PG, Baskaran M, Ve Ramesh S, George RJ, McCarty C, Vijaya L. Pseudoexfoliation in south India. Br J Ophthalmol. 2003;87(11):1321–1323. doi: 10.1136/bjo.87.11.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miyazaki M, Kubota T, Kubo M, Kiyohara Y, Iida M, Nose Y, Ishibashi T. The prevalence of pseudoexfoliation syndrome in a Japanese population: the Hisayama study. J Glaucoma. 2005;14(6):482–484. doi: 10.1097/01.ijg.0000185436.15675.b3. [DOI] [PubMed] [Google Scholar]
- 13.Sumasri K, Raju P, Aung T, Wong TY. Prevalence of pseudoexfoliation in Malay population in Singapore. Am J Ophthalmol. 2008;145:766–7. doi: 10.1016/j.ajo.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 14.Young AL, Tang WW, Lam DS. The prevalence of pseudoexfoliation syndrome in Chinese people. Br J Ophthalmol. 2004;88:193–5. doi: 10.1136/bjo.2003.021816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee RK. The molecular pathophysiology of pseudoexfoliation glaucoma. Curr Opin Ophthalmol. 2008;19:95–101. doi: 10.1097/ICU.0b013e3282f49cda. [DOI] [PubMed] [Google Scholar]
- 16.Naumann GO, Schlötzer-Schrehardt U, Küchle M. Pseudoexfoliation syndrome for the comprehensive ophthalmologist. Intraocular and systemic manifestations. Ophthalmology. 1998;105:951–968. doi: 10.1016/S0161-6420(98)96020-1. [DOI] [PubMed] [Google Scholar]
- 17.Schlötzer-Schrehardt UM, Dörfler S, Naumann GOH. Corneal endothelial involvement in pseudoexfoliation syndrome. Arch Ophthalmol. 1993;111:666–674. doi: 10.1001/archopht.1993.01090050100038. [DOI] [PubMed] [Google Scholar]
- 18.Inoue K, Okugawa K, Oshika T, Amano S. Morphological study of corneal endothelium and corneal thickness in pseudoexfoliation syndrome. Jpn J Ophthalmol. 2003;47:235–239. doi: 10.1016/s0021-5155(03)00022-4. [DOI] [PubMed] [Google Scholar]
- 19.Vannas A, Setala K, Ruusuvaara P. Endothelial cells in capsular glaucoma. Acta Ophthalmol (Copenh) 1977;55:951–958. doi: 10.1111/j.1755-3768.1977.tb05676.x. [DOI] [PubMed] [Google Scholar]
- 20.Wang L, Yamasita R, Hommura S. Corneal endothelial changes and aqueous flare intensity in pseudoexfoliation syndrome. Ophthalmologica. 1999;213:387–391. doi: 10.1159/000027460. [DOI] [PubMed] [Google Scholar]
- 21.Seitz B, Müller EE, Langenbucher A, Kus MM, Naumann GOH. Endothelial keratopathy in pseudoexfoliation syndrome: quantitative and qualitative morphometry using automated video image analysis. Klin Monatsbl Augenheilkd. 1995;207:167–175. doi: 10.1055/s-2008-1035363. [DOI] [PubMed] [Google Scholar]