Abstract
AIM
To study the distribution of ocular higher-order aberrations(HOAs) and mesopic pupil size in individuals screened for refractive surgery.
METHODS
Ocular HOAs and mesopic pupil size were studied in 2 458 eyes of 1 240 patients with myopia, myopic astigmatism and compound myopic astigmatism and 215 eyes of 110 patients with hyperopia, hyperopic astigmatism and compound hyperopic astigmatism using the Zywave aberrometer (Busch& Lomb). All patients had correctable refractive errors without a history of refractive surgery or underlying diseases. Root-mean-square values of HOAs, total spherical aberration, total coma and mesopic pupil size were analyzed. Ocular HOAs were measured across a ≥ 6.0 mm pupil, and pupil size measurements were performed under the mesopic condition.
RESULTS
The mean values of HOAs, total spherical aberration and total coma in the myopic group were 0.369µm, ±0.233, 0.133± 0.112µm and 0.330±0.188µm, respectively. In the hyperopic group the mean values of HOAs, total spherical aberration and total coma were 0.418µm ±0.214, 0.202±0.209µm and 0.343±0.201µm, respectively. Hyperopes showed greater total HOAs (P<0.01) and total spherical aberration (P<0.01) compared to myopes. In age-matched analysis, only the amount of total spherical aberration was higher in the hyperopic group (P=0.05). Mesopic pupil size in the myopic group was larger (P≤0.05).
CONCLUSION
The results suggested that significant levels of HOAs were found in both groups which are important for planning refractive surgeries on Iranians. There were significantly higher levels of total spherical aberration in hyperopes compared to myopes. Mesopic pupil size was larger in myopic group.
Keywords: corneal wavefront aberration, pupil, mesopic vision, race, myopia, hyperopia
INTRODUCTION
Ocular aberrations may play a major role in the image formation in the ocular optical system. Lower order aberrations such as astigmatism and defocus can easily be corrected and may be less problematic, however higher order aberrations (HOAs) can cause more degradation of the visual performance[1]-[5].
Customized corneal ablation has been successfully used to address wavefront aberrations of the eye. Given increasing interest in the management of ocular aberrations, performing preoperative aberrometry is more usual than the past. Higher order aberrations cannot be corrected by sphero-cylindric lenses which make them very important in clinical practice. The pupil size can affect the results of refractive surgeries due to its role in post operative visual symptoms such as glare and halo. The larger pupil size may also produce greater HOAs[1],[4]. Thus the pupil diameter is an important factor to consider especially for those patients who are candidates for refractive surgery.
In this study we investigated the distribution of HOAs and mesopic pupil size (MPS) in individuals screened for refractive surgery.
MATERIALS AND METHODS
Materials
Totally 2458 eyes of 1240 patients with myopia, myopic astigmatism and compound myopic astigmatism and 215 eyes of 110 patients with hyperopia, hyperopic astigmatism and compound hyperopic astigmatism were enrolled in our study. Subjects were selected from patients referred for refractive surgery to our center from September 2006 to November 2008 who participated in a cross sectional study.
Methods
Wave front aberrometry
The present study used the Zywave aberrometer developed by Busch& Lomb based on the Hartmann-Shack principle. All wavefront measurements were performed by the same examiner.
All wavefront measurements were repeated 3 times for each eye. The best image was included in the study based on the image quality. If the wavefront refraction of the patient was consistent with the subjective refraction (differences between spherical diopter: ±0.75D, cylindrical diopter: ±0.5D and astigmatic axis: ±15°), it would be included in the study and then HOAs and root mean square (RMS) values were documented. At first we performed pupillometry under mesopic condition (5 cd/m2) and then a pupillary diameter of at least 6.0 mm using tropicamide 0.5% eye drop was used for the analysis in this study.
All patients were examined to exclude other contributing factors such as previous ocular or corneal diseases, cataract, corneal scar or other media opacities and surgery or trauma which could alter wavefront measurements. Patients with a best-corrected visual acuity (BCVA) of less than 20/40 were excluded.
Statistical Analysis
RMS values of HOAs and MPS were analyzed. Data were analyzed using the Statistical Program for Social Sciences (SPSS) (Version 15, SPSS Inc., Chicago, Illinois, USA). To evaluate normal distribution of quantitative data, we employed Kolmogorov-Smirnov test. Based on this test, we used T- test to compare myopic and hyperopic subjects after the design effect of bilateral cases had been adjusted. P values of equal or less than 0.05 were considered to be statistically significant.
RESULTS
Myopic spherical equivalent (SE) was in the range of -0.75 to -16.0D with a mean±SD of -3.76D±2.94 and a cylinder of -1.24D±1.75. In the hyperopic group hyperopic spherical equivalent (SE) was in the range of +0.50 to +8.25D with a mean±SD of +3.26D±2.57 and a cylinder of -1.56D±1.87. The mean age was 28.31±7.32 and 37.69±10.09 for myopic and hyperopic patients, respectively (Table 1).
Table 1. Patient demography.
| Number | Myopia 2458 eyes of 1240 patients | Hyperopia 215 eyes of 110 patients | |
| Refraction | Mean±SD | -3.76±2.94 | +3.26±2.57 |
| Range | -16.00 to -0.75 | +0.50 to +8.25D | |
| Cylinder | Mean±SD | -1.24±1.75 | -1.56±1.87 |
| Range | -7.00 to 0.0 | -6.80 to 0.0 | |
| Age | Mean±SD | 28.3±7.32 | 37.69±10.09 |
| Range | 18 to 56 | 20 to 64 | |
| Gender | 70% (1707) | 60% (128) | |
| 30% (741) | 40% (85) | ||
The mean MPS in myopic group was 6.17mm±1.35mm (range: 2.80mm to 8.90mm), and in hyperopic group was 5.60mm±1.30mm (range: 2.80mm to 8.00mm). MPS was larger in myopic patients (P<0.01, Table 2).
Table 2. Refractive error, higher order aberration and mesopic pupil size.
| Myopia | Hyperopia | P | ||
| Mesopic pupil size | Mean±SD | 6.17 ± 1.35 | 5.60 ± 1.30 | <0.01 |
| Range | 2.8 to 8.9 | 2.8 to 8.0 | ||
| Ho-RMS* | Mean±SD | 0.37 ± 0.23 | 0.42 ± 0.21 | <0.01 |
| Range | 0.10 to 0.99 | 0.16 to 0.97 | ||
| Total Coma | Mean±SD | 0.33 ±0.19 | 0.34 ±0.20 | 0.48 |
| Range | 0.08 to 0.96 | 0.13 to 0.95 | ||
| Total spherical aberration | Mean±SD | 0.13 ± 0.11 | 0.20 ±0.21 | <0.01 |
| Range | 0.0 to 0.65 | 0.0 to 0.56 |
*Ho-RMS: Higher order RMS.
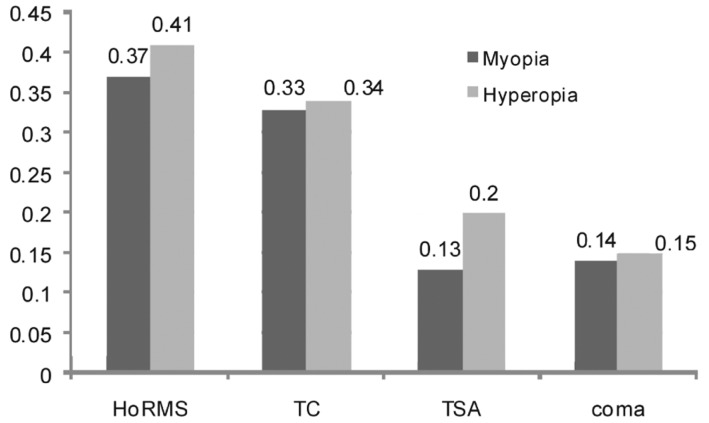
The mean value of HOAs in myopic group was 0.369µm±0.233 (range 0.100µm to 0.990µm). The mean total spherical aberration (TSA) was 0.133±0.112µm and the mean total coma was (TC) 0.330±0.188µm in this group. In hyperopic group the mean value of HOAs was 0.418µm±0.214 (range: 0.160µm to 0.970µm). The mean TSA was 0.202±0.209µm and the mean TC was 0.343±0.201µm for hyperopic group. Compared to myopic patients, hyperopic patients had significantly higher total HOAs and TSAs (P<0.01) in both cases. In age-matched analysis, only TSA was higher in hyperopic eyes (P=0.05). The majority of higher order aberrations were related to the third and fourth order aberrations (Figure 1, Table 2).
Figure 1. Higher order aberrations and refractive error.
TC: total coma; TSA: total spherical aberration.
DISCUSSION
In this study, we investigated ocular HOAs and MPS in both myopic and hyperopic patients. Aberrometry is a valuable method to detect eyes with an abnormal optical condition. Consistent with previous studies, ocular wavefront aberrations differed widely between subjects, with a mean SD of approximately 0.10µm for the total HOAs. The mean total higher-order RMS value is 0.33µm for a 6.0-mm pupil[6]-[10]. RMS values can be calculated from aberration coefficients and represent a summary of optical quality. In the present study, HOAs in myopic patients (average: 0.369µm) were lower than those in hyperopic patients (average: 0.418µm). This might be because of the confounding role of the age in our study, since the mean age of hyperopic subjects was significantly higher than myopic subjects and as other studies have shown HOAs increase with age[11]-[14]. In age-matched analysis, only TSA was higher in hyperopic patients. Liorente et al[15] also have reported greater spherical aberration in hyperopia compared to myopia. Bisneto et al[16] suggested that hyperopic patients with less than -0.75D astigmatism show greater amount of spherical aberration and hyperopic patients with more than -0.75D astigmatism show a greater amount of other HOAs (other than coma and spherical aberration) and also high-order RMS aberrations. HOAs may be more common in ammetropic eyes than emmetropic eyes, as He et al[17] proposed that myopic patients may present with greater HOAs compared to emmetropes. On the other hand, there are some studies that propose no relationship or even an opposite relationship between myopia or hyperopia and higher order aberrations[15]-[21]. Kirwan et al[22] reported greater higher order aberrations in myopes compared to hyperopes, however they studied on children, a population different from our study. In our study, the most significant components of HOAs were third order aberrations and fourth order aberrations respectively and the fifth order RMS value was the smallest among the three which is supported by other studies[1]-[4].
There were higher amounts of ocular HOAs in our subjects compared to Caucasian population[23]. Higher amounts of HOAs In Chinese population have also been reported compared to Caucasian population[24],[25]. Wei et al[19] postulated that one reason may be the differences in the precorneal tear film stability. The variation in the ocular tear film may cause differences in the local thickness and refractive index and cause optical path differences and different wavefront aberrations; thus there are higher levels of aberrations in patients with dry eyes[26]. Evidences show that tear films in Asian eyes are less stable than those in Caucasian and Indonesian eyes[27]-[29]. It may be the reason for more prevalent wavefront aberrations in our population.
In patients with a dilated pupil, total HOAs increase[30] and also the quality of image may decrease as the pupil diameter increases[31],[32]. Despite the controversy about the role of pupil diameter in night vision problems after refractive surgery, the ablation zone should ideally be larger than the pupil size in each level of ambient light[33]-[35]. Also the pupil size can affect our surgical plan for implanting a multifocal IOL[36]; thus knowing the pupil size under low levels of ambient light such as mesopic conditions, and also probable determinant factors of MPS would be invaluable. In this study, the pupil sizes under the mesopic conditions in myopic eyes and hyperopic eyes were 6.17 and 5.60, respectively. Thus, MPS in the myopic group was larger. Despite the relatively large number of hyperopic cases in our study, the number of myopic cases was significantly higher than hyperopic cases and there was a statistically significant age difference between myopic and hyperopic subjects participating in the study (P<0.01). Several studies have shown that pupil size decreases with the age under different illumination states[36]-[42], thus age may be a confounding factor causing the difference of MPS between myopic and hyperopic subjects in our study. In age-matched analysis, MPS was still larger in myopic group. Hashemi et al. reported an inverse relationship between refractive error and pupil size in univariable analysis, but not in the multivariable analysis, supported by other studies[43]-[45]. They reported smaller pupil sizes among hyperopic patients compared to the myopes probably because of more accommodation in hyperopic subjects[46]. However some studies have reported no relationship between the pupil diameter and refraction among patients with hyperopia and myopia[47],[48]. There are not any organized data about mesopic pupil sizes in different races and different iris colors. Kokh et al[49] reported that brown iris colors may be associated with larger pupil sizes. Schnitzler et al[50] have proposed that the pupil diameter in eyes with blue and brown irises is larger than green iris, however other studies did not support this hypothesis[36],[47],[51]-[53]. There were larger pupil sizes in our Iranian patients having darker iris colours.
The existing knowledge concerning the clinical significance of HOAs and MPS, their relationship to the visual function, and the potential effectiveness of correcting HOAs in refractive surgery encouraged us to study HOAs and MPS in our population. We think that our findings are important to assess their clinical significance and role in laser refractive surgery especially among Iranian population because of higher amounts of HOAs and larger pupil sizes.
REFERENCES
- 1.de Castro LE, Sandoval HP, Bartholomew LR, Vroman DT, Solomon KD. High-order aberrations and preoperative associated factors. Acta Ophthalmol Scand. 2007;85:106–110. doi: 10.1111/j.1600-0420.2006.00757.x. [DOI] [PubMed] [Google Scholar]
- 2.Wang L, Koch DD. Ocular higher-order aberrations in individuals screened for refractive surgery. J Cataract Refract Surg. 2003;29:1896–1903. doi: 10.1016/s0886-3350(03)00643-6. [DOI] [PubMed] [Google Scholar]
- 3.Carkeet A, Leo SW, Khoo BK, Au Eong KG. Modulation transfer functions in children: pupil size dependence and meridional anisotropy. Invest Ophthalmol Vis Sci. 2003;44:3248–3256. doi: 10.1167/iovs.02-1064. [DOI] [PubMed] [Google Scholar]
- 4.Wang Y, Zhao K, Jin Y, Niu Y, Zuo T. Changes of higher order aberration with various pupil sizes in the myopic eye. J Refract Surg. 2003;19:S270–S274. doi: 10.3928/1081-597X-20030302-21. [DOI] [PubMed] [Google Scholar]
- 5.Villa C, Gutiérrez R, Jiménez JR, Gonzáz-Méijome JM. Night vision disturbances after successful LASIK surgery. Br J Ophthalmol. 2007;91:1031–1037. doi: 10.1136/bjo.2006.110874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Castejón-Mochón JF, López-Gil N, Benito A, Artal P. Ocular wave-front aberration statistics in a normal young population. Vision Res. 2002;42:1611–1617. doi: 10.1016/s0042-6989(02)00085-8. [DOI] [PubMed] [Google Scholar]
- 7.Cerviño A, Hosking SL, Ferrer-Blasco T, Montes-Mico R, Gonzalez-Meijome JM. A pilot study on the differences in wavefront aberrations between two ethnic groups of young generally myopic subjects. Ophthalmic Physiol Opt. 2008;28:532–537. doi: 10.1111/j.1475-1313.2008.00592.x. [DOI] [PubMed] [Google Scholar]
- 8.Ramamirtham R, Kee C.S, Hung L. F, Qiao-Grider Y, Huang J, Roorda A, Smith E. L. Wave aberrations in rhesus monkeys with vision-induced ametropias. Vision Res. 2007;47:2751–2756. doi: 10.1016/j.visres.2007.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santodomingo-Rubido J, Mallen E. A, Gilmartin B, Wolffsohn J. S. A new non-contact optical device for ocular biometry. Br J Ophthalmol. 2002;86:458–462. doi: 10.1136/bjo.86.4.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smirnov MS. Measurement of the wave aberration of the human eye. Biophysics J. 1962;7:766–795. [Google Scholar]
- 11.Applegate RA, Thibos LN, Hilmantel G. Optics of aberroscopy and super vision. J Cataract Refract Surg. 2001;27:1093–1107. doi: 10.1016/s0886-3350(01)00856-2. [DOI] [PubMed] [Google Scholar]
- 12.McLellan JS, Marcos S, Burns SA. Age-related changes in monochromatic wave aberrations of the human eye. Invest Ophthalmol Vis Sci. 2001;42:1390–1395. [PubMed] [Google Scholar]
- 13.Guirao A, Redondo M, Artal P. Optical aberrations of the human cornea as a function of age. J Opt Soc Am A Opt Image Sci Vis. 2000;17:1697–1702. doi: 10.1364/josaa.17.001697. [DOI] [PubMed] [Google Scholar]
- 14.Porter J, Guirao A, Cox IG, Williams DR. Monochromatic aberrations of the human eye in a large population. J Opt Soc Am A Opt Image Sci Vis. 2001;18:1793–1803. doi: 10.1364/josaa.18.001793. [DOI] [PubMed] [Google Scholar]
- 15.Llorente L, Barbero S, Cano D, Dorronsoro C, Marcos S. Myopic versus hyperopic eyes: axial length, corneal shape and optical aberrations. J Vis. 2004;22:288–298. doi: 10.1167/4.4.5. [DOI] [PubMed] [Google Scholar]
- 16.Bisneto OS, Temporini ER, Arieta CE, Moreira H. Relationship between high-order aberrations and age and between high-order aberrations and refraction errors. Arq Bras Oftalmol. 2007;70:290–297. doi: 10.1590/s0004-27492007000200019. [DOI] [PubMed] [Google Scholar]
- 17.He JC, Sun P, Held R, Thorn F, Sun X, Gwiazda JE. Wavefront aberrations in eyes of emmetropic and moderately myopic school children and young adults. Vision Res. 2002;42:1063–1070. doi: 10.1016/s0042-6989(02)00035-4. [DOI] [PubMed] [Google Scholar]
- 18.Howland HC, Howland B. A subjective method for the measurement of monochromatic aberrations of the eye. J Opt Soc Am. 1977;67:1508–1518. doi: 10.1364/josa.67.001508. [DOI] [PubMed] [Google Scholar]
- 19.Wei RH, Lim L, Chan WK, Tan DT. Higher order ocular aberrations in eyes with myopia in a Chinese population. J Refract Surg. 2006;22:695–702. doi: 10.3928/1081-597X-20060901-11. [DOI] [PubMed] [Google Scholar]
- 20.Collins MJ, Wildsoet CF. Atchison DA. Monochromatic aberrations and myopia. Vision Res. 1995;35:1157–1163. doi: 10.1016/0042-6989(94)00236-f. [DOI] [PubMed] [Google Scholar]
- 21.Carkeet A, Luo HD, Tong L, Saw SM, Tan DT. Refractive error and monochromatic aberrations in Singaporean children. Vision Res. 2002;42:1809–1824. doi: 10.1016/s0042-6989(02)00114-1. [DOI] [PubMed] [Google Scholar]
- 22.Kirwan C, O'Keefe M, Soeldner H. Higher-order aberrations in children. Am J Ophthalmol. 2006;141:67–70. doi: 10.1016/j.ajo.2005.08.031. [DOI] [PubMed] [Google Scholar]
- 23.Cheng X, Bradley A, Hong X, Thibos LN. Relationship between refractive error and monochromatic aberrations of the eye. Optom Vis Sci. 2003;80:43–49. doi: 10.1097/00006324-200301000-00007. [DOI] [PubMed] [Google Scholar]
- 24.Lim KL, Fam HB. Ethnic differences in higher-order aberrations:Spherical aberration in the South East Asian Chinese eye. J Cataract Refract Surg. 2009;35:2144–2148. doi: 10.1016/j.jcrs.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 25.Montés-Micó R, Cáliz A, Alió JL. Wavefront analysis of higher order aberrations in dry eye patients. J Refract Surg. 2004;20:243–247. doi: 10.3928/1081-597X-20040501-08. [DOI] [PubMed] [Google Scholar]
- 26.Lee AJ, Lee J, Saw SM, Gazzard G, Koh D, Widjaja D, Tan DT. Prevalence and risk factors associated with dry eye symptoms: a population based study in Indonesia. Br J Ophthalmol. 2002;86:1347–1351. doi: 10.1136/bjo.86.12.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am J Ophthalmol. 2003;136:318–326. doi: 10.1016/s0002-9394(03)00218-6. [DOI] [PubMed] [Google Scholar]
- 28.Lin PY, Tsai SY, Cheng CY, Liu JH, Chou P, Hsu WM. Prevalence of dry eye among an elderly Chinese population in Taiwan: the Shihpai Eye Study. Ophthalmology. 2003;110:1096–1101. doi: 10.1016/S0161-6420(03)00262-8. [DOI] [PubMed] [Google Scholar]
- 29.Albietz JM, Lenton LM, McLennan SG. Dry eye after LASIK: comparison of outcomes for Asian and Caucasian eyes. Clin Exp Optom. 2005;88:89–96. doi: 10.1111/j.1444-0938.2005.tb06673.x. [DOI] [PubMed] [Google Scholar]
- 30.Liang J, Williams DR. Aberrations and retinal image quality of the normal human eye. J Opt Soc Am A Opt Image Sci Vis. 1997;14:2873–2883. doi: 10.1364/josaa.14.002873. [DOI] [PubMed] [Google Scholar]
- 31.Oshika T, Klyce SD, Applegate RA, Howland HC. Changes in corneal wavefront aberrations with aging. Invest Ophthalmol Vis Sci. 1999;40:1351–1355. [PubMed] [Google Scholar]
- 32.Campbell FW, Gubisch RW. Optical quality of the human eye. J Physiol. 1966;186:558–578. doi: 10.1113/jphysiol.1966.sp008056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pop M, Payette Y. Risk factors for night vision complaints after LASIK for myopia. Ophthalmology. 2004;111:3–10. doi: 10.1016/j.ophtha.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 34.Salz JJ, Trattler W. Pupil size and corneal laser surgery. Curr Opin Ophthalmol. 2006;17:373–379. doi: 10.1097/01.icu.0000233958.96133.02. [DOI] [PubMed] [Google Scholar]
- 35.Holladay JT, Lynn MJ, Waring GO, III, Gemmill M, Keehn GC, Fielding B. The relationship of visual acuity, refractive error, and pupil size after radial keratotomy. Arch Ophthalmol. 1991;109:70–76. doi: 10.1001/archopht.1991.01080010072036. [DOI] [PubMed] [Google Scholar]
- 36.Nakamura K, Bissen-Miyajima H, Oki S, Onuma K. Pupil sizes in different Japanese age groups and the implications for intraocular lens choice. J Cataract Refract Surg. 2009;35:134–138. doi: 10.1016/j.jcrs.2008.10.020. [DOI] [PubMed] [Google Scholar]
- 37.Birren JE, Casperson RC, Botwinick J. Age changes in pupil size. J Gerontol. 1950;5:216–221. doi: 10.1093/geronj/5.3.216. [DOI] [PubMed] [Google Scholar]
- 38.Kadlecova V, Peleska M, Vasko A. Dependence on age of the diameter of the pupil in the dark. Nature. 1958;182:1520–1521. doi: 10.1038/1821520a0. [DOI] [PubMed] [Google Scholar]
- 39.Scha fer WD, Weale RA. The influence of age and retinal illumination on the pupillary near reflex. Vision Res. 1970;10:179–91. doi: 10.1016/0042-6989(70)90114-8. [DOI] [PubMed] [Google Scholar]
- 40.Said FS, Sawires WS. Age dependence of changes in pupil diameter in the dark. Optica Acta. 1972;19:359–361. [Google Scholar]
- 41.Lowenfeld IE. Pupillary changes related to age. In: Thompson HS, Daroff R, Frisén L, Glaser JS, Sanders MD, editors. Topics in Neuro-Ophthalmology. Baltimore, MD, Williams& Wilkins; 1979. pp. 124–150. [Google Scholar]
- 42.Kohnen EM, Zubcov AA, Kohnen T. Scotopic pupil size in a normal pediatric population using infrared pupillometry. Graefes Arch Clin Exp Ophthalmol. 2004;242:18–23. doi: 10.1007/s00417-003-0735-4. [DOI] [PubMed] [Google Scholar]
- 43.Chaidaroon W, Juwattanasomran W. Colvard pupillometer measurement of scotopic pupil diameter in emmetropes and myopes. Jpn J Ophthalmol. 2002;46:640–644. doi: 10.1016/s0021-5155(02)00556-7. [DOI] [PubMed] [Google Scholar]
- 44.Hsieh YT, Hu FR. The correlation of pupil size measured by Colvard pupillometer and Orbscan II. J Refract Surg. 2007;23:789–795. doi: 10.3928/1081-597X-20071001-08. [DOI] [PubMed] [Google Scholar]
- 45.Netto MV, Ambrosio R, Jr, Wilson SE. Pupil size in refractive surgery candidates. J Refract Surg. 2004;20:337–342. doi: 10.3928/1081-597X-20040701-06. [DOI] [PubMed] [Google Scholar]
- 46.Hashemi H, Yazdani K, Khabazkhoob M, Mehravaran S, Mohammad K, Fotouhi A. Distribution of photopic pupil diameter in the Tehran eye study. Curr Eye Res. 2009;34:378–385. doi: 10.1080/02713680902853327. [DOI] [PubMed] [Google Scholar]
- 47.Winn B, Whitaker D, Elliott DB, Phillips NJ. Factors affecting light-adapted pupil size in normal human subjects. Invest Ophthalmol Vis Sci. 1994;35:1132–1137. [PubMed] [Google Scholar]
- 48.Robl C, Sliesoraityte I, Hillenkamp J, Prahs P, Lohmann CP, Helbig H, Herrmann WA. Repeated pupil size measurements in refractive surgery candidates. J Cataract Refract Surg. 2009;35:2099–2102. doi: 10.1016/j.jcrs.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 49.Koch DD, Samuelson SW, Haft EA, Merin LM. Pupillary size and responsiveness; implications for selection of a bifocal intraocular lens. Ophthalmology. 1991;98:1030–1035. [PubMed] [Google Scholar]
- 50.Schnitzler EM, Baumeister M, Kohnen T. Scotopic measurement of normal pupils: Colvard versus Video Vision Analyzer infrared pupillometer. J Cataract Refract Surg. 2000;26:859–866. doi: 10.1016/s0886-3350(00)00486-7. [DOI] [PubMed] [Google Scholar]
- 51.Vaswani RS, Mudgil AV, Gleicher D. Correlation of pupil size to iris color in children. J Refract Surg. 2002;18:189. doi: 10.3928/1081-597X-20020301-15. [DOI] [PubMed] [Google Scholar]
- 52.Dain SJ, Cassimaty VT, Psarakis DT. Differences in FM100-Hue test performance related to iris colour may be due to pupil size as well as presumed amounts of macular pigmentation. Clin Exp Optom. 2004;87:322–325. doi: 10.1111/j.1444-0938.2004.tb05061.x. [DOI] [PubMed] [Google Scholar]
- 53.Bradley JC, Bentley KC, Mughal AI, Bodhireddy H, Young RS, Brown SM. The effect of gender and iris color on the dark-adapted pupil diameter. J Ocul Pharmacol Ther. 2010;26:335–340. doi: 10.1089/jop.2010.0061. [DOI] [PubMed] [Google Scholar]