Abstract
AIM
Age-related macular degeneration (AMD) is the leading cause of blindness in the developed world and complement factor H (CFH) polymorphism has been found to associate with the AMD. To investigate whether the Y402H variant in CFH is associated with AMD in Chinese populations, a systematic review and meta-analysis were performed to estimate the magnitude of the gene effect and the possible mode of action.
METHODS
A meta-analysis was performed using data available from ten case-control studies assessing association between the CFH Y402H polymorphism and AMD in Chinese populations involving 1538 AMD. Data extraction and study quality assessment were performed in duplicate. Summary odds ratios (ORs) and 95% confidence intervals (CIs) an allele contrast and genotype contrast were estimated using fixed- effects models. The Q-statistic test was used to assess heterogeneity, and Funnel plot was used to evaluate publication bias.
RESULTS
Seven of ten case-control studies were neovascular AMD, and few studies came from west and north of China. There was strong evidence for association between CFH and AMD in Chinese population, with those having risk allele C 2.35 times more likely to have AMD than subjects with T allele. Evidence of publication bias was not observed in our meta-analysis.
CONCLUTION
This meta-analysis summarizes the strong evidence for an association between CFH and AMD in Chinese and indicates each C allele increasing the odds of AMD by 2.33-fold.But more evidences about the relation between CFH polymorphism and different type of Chinese AMD from various district were needed.
Keywords: age-related macular degeneration, complement factor H polymorphism, meta-analysis, Chinese population
INTRODUCTION
Age-related macular degeneration (AMD) is the leading cause of blindness in the developed world, accounting for half of all new cases of registered blindness[1]-[4]. AMD is a common multifactorial and heterogeneous disorder. Owing to an expected demographic shift towards ageing populations, the prevalence of AMD is expected to double in the coming decades[5] and the burden of AMD is set to grow. It was traditionally thought that Asians, including Chinese, have relatively lower prevalence rates for AMD compared with whites[6]-[10]. Although the precise cause of AMD remains elusive, recent genetic studies have provided significant insights into the molecular basis of AMD. Recent genetic association studies have demonstrated that the complement factor H (CFH) gene is a major risk factor for the development of AMD in various ethnicities[11]-[14]. A common allele Y402H of CFH which is characterized by a substitution of histidine for tyrosine at codon 402 on the long arm of chromosome 1, region 31 (rs1061170), alters the binding of the CFH protein to sulfated polysaccharides. The Y402H coding variant in CFH has been extensively studied via genetic and molecular method, which provides strong statistical evidence for disease association and a plausible biological context supporting this variant as an attractive candidate for a causal polymorphism leading to the development of AMD. However, most of these studies came from western countries, and the compelling association between Y402H and AMD observed in European cohorts is not as relevant to the disease risk in populations of Asian ancestry. Multiple independent studies have been performed to assess the association between Y402H and AMD in Asian populations[15]-[26], but most of these studies reported a lack of association in Korean, Japanese and Chinese. The Chinese population consists of 56 ethnicities with very diverse genetic backgrounds. Several studies are now emerging from various geographic areas of China, and three independent studies from Beijing[21] and Nantong[20] and Hongkong[25] reported no significant association between Y402H and Neovascular AMD. The low frequencies of variant alleles and small sample sizes in studies have hindered reliable assessment of the association between CFH Y402H and AMD in Chinese populations. To overcome these barriers, we performed a robust systematic meta-analysis of 10 case-control studies involving 1538 patients and 1605 normal controls of Chinese ancestry to assess the association between the Y402H variant and AMD in Chinese populations.
MATERIALS AND METHODS
Materials
MEDLINE (from January 1966 to October 9, 2011) was searched using the PubMed search engine. The search strategy was “macular degeneration” or “AMD” AND “complement factor H” OR “CFH”. Results were limited to English language papers. The literature search was performed in duplicate by two authors (Y.L. and A.Y.). Studies included in the meta-analysis had to fulfill the following criteria: (1) The study must be unrelated case control, representing an assessment of the association between the CFH Y402Hvariant and AMD in Chinese populations; (2) the study must present available data on allele and genotype distributions for case and control subjects; (3) the study must be written in English and published in peer-reviewed journals. For duplicate publications, the largest dataset was chosen for meta-analysis.
Methods
Data extraction
Data were extracted independently and in duplicate by two reviewers (Y.L. and A.Y.) using a standardized data extraction form. Any disagreement was adjudicated by a third author (Z.H.). The following variables were extracted from each study: the name of the first author, year of publication, institution of the study, geographic region, phenotype of cases evaluated, sample size, mean age and gender ratio of study participants, and allele and genotype distributions in cases and controls.
Statistical Analysis
For each study, deviations from the Hardy–Weinberg equilibrium (HWE) in control subjects were tested using the exact test. Between-study heterogeneity was assessed by the Q-statistic test and I2 statistic. P <0.1 was considered statistically significance for the Q-statistic test. I2 ranges between 0% and 100% (where a value of 0% represents no heterogeneity) and larger values represent increasing heterogeneity. Meta-analysis was performed to evaluate the evidence on the association between CFH Y402H and AMD in Chinese populations using the Mantel–Haenszel fixed-effects model. Publication bias was assessed by funnel plot. All meta-analyses were performed using RevMan software (version 5.0). All tests were 2-tailed. P<0.05 was considered statistically significance except for the test of between-study heterogeneity.
RESULTS
Eligibility of Studies
A total of 316 publications were identified in the initial PubMed search, of which 11 met our inclusion criteria. 2 eligible studies were the same cohorts. Table 1 lists the studies included in the meta-analysis together with summary characteristics of study subjects. All studies were case–control designs with subjects of Chinese ancestry, of these half were age matched or age and sex matched healthy controls[17],[20],[24]-[26]; mean age ranged from 57.5 to 76.1 years; percent males ranged from 44.8 to 81.8%. The quality of studies ranged from 5 to 9, out of a best possible score of 12. The combined sample size for this meta-analysis was 1538. We estimated summary odds ratios (ORs) and 95% confidence intervals (CIs).
Table 1. General characteristic of studies included in the review.
| Study | Year | Sample size Case/control | Institution | Subjects origin | Phenotype of cases | Mean age | Male% | Genotyping Method |
| Lau[16] | 2006 | 163/232 | National Yang-Ming University, Taipei | Taiwan | Neovascular AMD | 76.1 | 81.8 | PCR-RFLP |
| Chu[17] | 2008 | 144/126 | Peking Union Medical College Hospital | Beijing | Neovascular AMD | 67.2 | 54.8 | PCR-RFLP |
| Lin[19] | 2008 | 133/180 | China Medical University Hospital | Taichung, Taiwan | Early AMD | NA | NA | Real-time PCR-based (melting curve analysis) |
| Ng[20] | 2008 | 163/155 | Chinese University of Hong Kong | Hong Kong | Neovascular AMD | 74.3 | 50.3 | Direct sequencing |
| Xu[21] | 2008 | 121/132 | Beijing Tongren Hospital | Beijing | Neovascular AMD | 66.1 | 54.9 | PCR-RFLP |
| Pei[22] | 2009 | 123/130 | Peking University People's Hospital | Beijing | Neovascular AMD | 69.9 | 53.0 | Direct sequencing |
| Gao[23] | 2010 | 208/140 | Beijing Tongren Hospital | Beijing | Soft drusen | 57.5 | 44.8 | PCR-RFLP |
| Liu[24] | 2010 | 158/220 | Sichuan Provincial People's Hospital | Sichuan | Mixed (neovascular/soft drusen) | 64.2 | 54.6 | Direct sequencing |
| 80/220 | ||||||||
| Yang[25] | 2010 | 109/150 | Affiliated Hospital of Nantong University | Nantong | Neovascular AMD | 64.8 | 46.7 | PCR-RFLP |
| Dong[26] | 2011 | 136/140 | Qilu Hospital of Shandong University | Shandong | Neovascular AMD | 70.4 | 59.0 | PCR-RFLP |
AMD= age-related macular degeneration; PCR= polymerase chain reaction; RFLP=restriction fragment length polymorphism. NA =not available.
Allele Frequency
Data from control groups were used for pooling allele prevalence (Table 2). All studies were observed Hardy–Weinberg equilibrium (HWE) and were included in pooling. The pooled prevalence for the risk allele C was 5.50% (95% CI: 3.97, 7.75).
Table 2. Estimation of the pooled prevalence of the CFH Y402H allele.
| Study | HWE P-value | N | T Frequency | % Allele | C Frequency | % Allele |
| Lau[16] | 0.66 | 464 | 219 | 97.20 | 13 | 2.80 |
| Chu[17] | 0.23 | 252 | 239 | 94.84 | 13 | 5.16 |
| Lin[19] | 0.53 | 360 | 344 | 95.56 | 16 | 4.44 |
| Ng[20] | 0.71 | 310 | 301 | 97.10 | 9 | 2.90 |
| Xu[21] | 0.32 | 264 | 243 | 92.05 | 21 | 7.95 |
| Pei[22] | 0.58 | 260 | 248 | 95.38 | 12 | 4.62 |
| Gao[23] | 0.50 | 280 | 265 | 94.64 | 15 | 5.36 |
| Liu[24] | 0.66 | 440 | 416 | 94.55 | 24 | 5.45 |
| Yang[25] | 0.37 | 300 | 194 | 88.99 | 24 | 11.01 |
| Dong[26] | 0.36 | 280 | 255 | 91.07 | 25 | 8.93 |
| Pooled prevalence (%) | 94.50 (95% CI: 92.2, 96.0) | 5.50 (95% CI: 3.97, 7.75) | ||||
Quantitative Synthesis
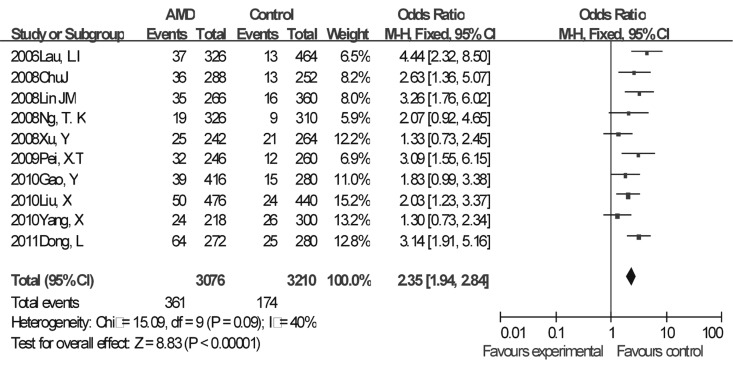
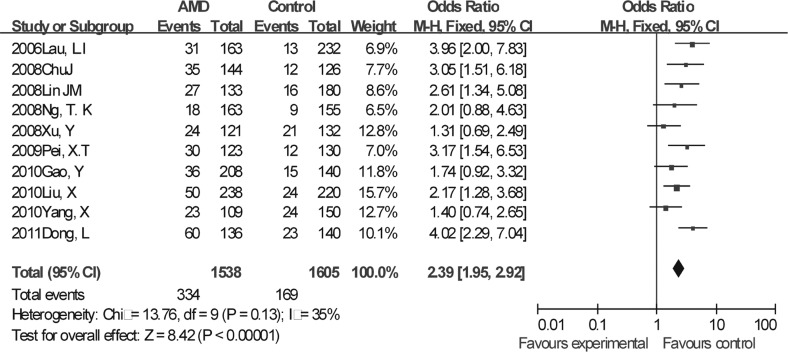
We performed a meta-analysis based on an allele contrast model. The Y402H variant showed a significant summary OR of 2.35 (95% CI, 1.94-2.84; fix-effects P<0.001; Figure 1). The Q-statistic test indicated no significant between-study heterogeneity across the 10 studies (Q =15.09, df = 9, P =0.09, I2 = 40%; Figure 1). We also calculated a summary OR based on genotype contrast. For this analysis, we considered a dominant genetic model, which compares a combination of C/C and C/T genotypes with the homozygous T/T, because of the rarity of the CC genotype. The summary OR was 2.39 (95%CI, 1.95-2.92) for carriers of the risk allele C (fixed-effects, P<0.001) with no evidence of heterogeneity (Q =13.76, df=9, P = 0.13, I2 = 35%; Figure 2), The population attribute risk for carrying at least 1 risk allele was 8.8% (95% CI, 5.9-12.1). Next, we performed a stratified analysis according to the sub-phenotype of AMD. The summary ORs for neovascular AMD risk were 2.37 (95% CI, 1.92-2.93) and summary ORs for soft drusen were 2.20 (95% CI, 1.53-3.17) in the allelic contrast.
Figure 1. Forest plot of fixed effects meta-analysis of the association between Y402H and AMD based on allelic contrast.
Odds ratios (black squares) and 95% CIs (bars) are given for each study. Also shown are the shaded diamonds of the summary ORs based on the Mantel–Haenszel fixed-effects model. CI =confidence interval; OR = odds ratio.
Figure 2. Forest plot of fixed effects meta-analysis of the association between Y402H and AMD based on genotype contrast.
Odds ratios (black squares) and 95% CIs (bars) are given for each study. Also shown are the shaded diamonds of the summary ORs based on the Mantel–Haenszel fixed-effects model. CI =confidence interval; OR = odds ratio.
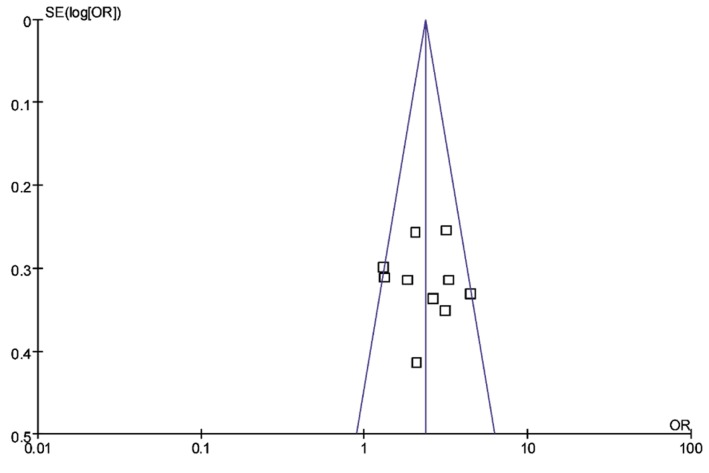
Publication Bias
We assessed publication bias using funnel plot with pseudo of 95% confidence limits of 10 references including in the meta-analysis (Figure 3). No statistically significant evidence of publication bias was detected for the allelic contrast model and dominant model.
Figure 3. Funnel plot with pseudo of 95% confidence limits of 10 references including in the meta-analysis.
DISCUSSION
Past studies have indicated that inflammation plays a role in the initiation and progression of AMD. The association between the Y402H polymorphism and AMD is consistently reported in Northern American and European populations. The magnitude of CFH Y402H and AMD association appears to become lower when studies move from the West to the East. A Russian study reported an OR in patients homozygous for the 402H variant to be only 2.45[27], whereas ORs higher than 3 have been reported in Western populations[28]. Most studies on Eastern Asian populations have shown no evidence of 402H association with AMD, including some studies from Chinese population. This meta-analysis reported a summary allele OR of 2.35 (P<0.001) and strongly supported the notion that the Y402H variant is a risk factor for AMD in Chinese populations. In individuals carrying at least 1 copy of the risk C allele, disease risk is increased by approximately 2-fold. And evidence of publication bias was not observed in our meta-analysis.
The CFH Y402H polymorphism is located within a binding site for heparin and C-reactive protein (CRP), a systemic inflammatory marker associated with AMD. Therefore, changes in this region of the protein may result in a malfunctioning CFH that is not able to inhibit the complement cascade properly. The variation of CFH may in part explain the differences in the prevalence of late AMD in various ethnicities and geographic regions and the different treatment response of AMD to photodynamic therapy (PDT) or intravitreal bevacizumab[12],[29]-[32]. But so far, to our knowledge there was no evidence from Chinese about the CHF polymorphisms and PDT treatment response association or a pharmacogenetic effect of the CFH Y402H variations with ranibizumab in Chinese AMD.
In summary, this meta-analysis summarizes the strong evidence for an association between CFH and AMD in Chinese population, and indicates a potentially multiplicative model with each C allele, increasing the odds of AMD by 2.3-fold. But China has broad area and a great variety of ethnicities with very diverse genetic backgrounds. Most vidences including in this reviews came from limited geographical position and genetic backgrounds. So much evidence and further additional prospective studies of larger sample populations are needed to understand the role of genetic factors on the prevalence and treatment response for this blinding eye disease from China.
REFERENCES
- 1.Klein R, Klein BE, Linton KL. Prevalence of age-related maculopathy. The Beaver Dam Eye Study. Ophthalmology. 1992;99(6):933–943. doi: 10.1016/s0161-6420(92)31871-8. [DOI] [PubMed] [Google Scholar]
- 2.Klein R, Klein BE, Moss SE. Age-related eye disease and survival. The Beaver Dam Eye Study. Arch Ophthalmol. 1995;113(3):333–339. doi: 10.1001/archopht.1995.01100030089026. [DOI] [PubMed] [Google Scholar]
- 3.Klein R, Klein BE, Jensen SC, Meuer SM. The five-year incidence and progression of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology. 1997;104(1):7–21. doi: 10.1016/s0161-6420(97)30368-6. [DOI] [PubMed] [Google Scholar]
- 4.Klein R, Cruickshanks KJ, Nash SD, Krantz EM, Javier Nieto F, Huang GH, Pankow JS, Klein BE. The prevalence of age-related macular degeneration and associated risk factors. Arch Ophthalmol. 2010;128(6):750–758. doi: 10.1001/archophthalmol.2010.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedman DS, O'Colmain BJ, Munoz B, Tomany SC, McCarty C, de Jong PT, Nemesure B, Mitchell P, Kempen J. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol. 2004;122(4):564–572. doi: 10.1001/archopht.122.4.564. [DOI] [PubMed] [Google Scholar]
- 6.Michon JJ, Lau J, Chan WS, Ellwein LB. Prevalence of visual impairment, blindness, and cataract surgery in the Hong Kong elderly. Br J Ophthalmol. 2002;86(2):133–139. doi: 10.1136/bjo.86.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng CL, Saw SM, Pang CE, Chee C. Age-related macular degeneration in Singapore. Singapore Med J. 2009;50(2):126–131. [PubMed] [Google Scholar]
- 8.Xu L, Li YB, Wang YX, Jonas JB. Age-related macular degeneration and mortality: the Beijing eye study. Ophthalmologica. 2008;222(6):378–379. doi: 10.1159/000151468. [DOI] [PubMed] [Google Scholar]
- 9.Cackett P, Yeo I, Cheung CM, Vithana EN, Wong D, Tay WT, Tai ES, Aung T, Wong TY. Relationship of smoking and cardiovascular risk factors with polypoidal choroidal vasculopathy and age-related macular degeneration in Chinese persons. Ophthalmology. 2011;118(5):846–852. doi: 10.1016/j.ophtha.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 10.Nonyane BA, Nitsch D, Whittaker JC, Sofat R, Smeeth L, Chakravarthy U, Fletcher AE. An ecological correlation study of late age-related macular degeneration and the complement factor H Y402H polymorphism. Invest Ophthalmol Vis Sci. 2010;51(5):2393–2402. doi: 10.1167/iovs.09-4228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edwards AO, Ritter R. Complement factor H polymorphism and age-related macular degeneration. Science. 2005;308(5720):421–424. doi: 10.1126/science.1110189. [DOI] [PubMed] [Google Scholar]
- 12.Donoso LA, Vrabec T, Kuivaniemi H. The role of complement Factor H in age-related macular degeneration: a review. Surv Ophthalmol. 2010;55(3):227–246. doi: 10.1016/j.survophthal.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Delcourt C, Delyfer MN, Rougier MB, Amouyel P, Colin J, Le Goff M, Malet F, Dartigues JF, Lambert JC, Korobelnik JF. Associations of Complement Factor H and Smoking with Early Age-Related Macular Degeneration: The ALIENOR Study. Invest Ophthalmol Vis Sci. 2011;52(8):5955–5962. doi: 10.1167/iovs.10-6235. [DOI] [PubMed] [Google Scholar]
- 14.Wegscheider BJ, Weger M, Renner W, Steinbrugger I, Marz W, Mossbock G, Temmel W, El-Shabrawi Y, Schmut O, Jahrbacher R, Haas A. Association of complement factor H Y402H gene polymorphism with different subtypes of exudative age-related macular degeneration. Ophthalmology. 2007;114(4):738–742. doi: 10.1016/j.ophtha.2006.07.048. [DOI] [PubMed] [Google Scholar]
- 15.Chen LJ, Liu DT, Tam PO, Chan WM, Liu K, Chong KK, Lam DS, Pang CP. Association of complement factor H polymorphisms with exudative age-related macular degeneration. Mol Vis. 2006;12:1536–1542. [PubMed] [Google Scholar]
- 16.Lau LI, Chen SJ, Cheng CY, Yen MY, Lee FL, Lin MW, Hsu WM, Wei YH. Association of the Y402H polymorphism in complement factor H gene and neovascular age-related macular degeneration in Chinese patients. Invest Ophthalmol Vis Sci. 2006;47(8):3242–3246. doi: 10.1167/iovs.05-1532. [DOI] [PubMed] [Google Scholar]
- 17.Chu J, Zhou CC, Lu N, Zhang X, Dong FT. Genetic variants in three genes and smoking show strong associations with susceptibility to exudative age-related macular degeneration in a Chinese population. Chin Med J (Engl) 2008;121(24):2525–2533. [PubMed] [Google Scholar]
- 18.Lee KY, Vithana EN, Mathur R, Yong VH, Yeo IY, Thalamuthu A, Lee MW, Koh AH, Lim MC, How AC, et al. Association analysis of CFH, C2, BF, and HTRA1 gene polymorphisms in Chinese patients with polypoidal choroidal vasculopathy. Invest Ophthalmol Vis Sci. 2008;49(6):2613–2619. doi: 10.1167/iovs.07-0860. [DOI] [PubMed] [Google Scholar]
- 19.Lin JM, Tsai YY, Wan L, Lin HJ, Tsai Y, Lee CC, Tsai CH, Tsai FJ, Tseng SH. Complement factor H variant increases the risk for early age-related macular degeneration. Retina. 2008;28(10):1416–1420. doi: 10.1097/IAE.0b013e318184661d. [DOI] [PubMed] [Google Scholar]
- 20.Ng TK, Chen LJ, Liu DT, Tam PO, Chan WM, Liu K, Hu YJ, Chong KK, Lau CS, Chiang SW, et al. Multiple gene polymorphisms in the complement factor h gene are associated with exudative age-related macular degeneration in Chinese. Invest Ophthalmol Vis Sci. 2008;49(8):3312–3317. doi: 10.1167/iovs.07-1517. [DOI] [PubMed] [Google Scholar]
- 21.Xu Y, Guan N, Xu J, Yang X, Ma K, Zhou H, Zhang F, Snellingen T, Jiao Y, Liu X, et al. Association of CFH, LOC387715, and HTRA1 polymorphisms with exudative age-related macular degeneration in a northern Chinese population. Mol Vis. 2008;14:1373–1381. [PMC free article] [PubMed] [Google Scholar]
- 22.Pei XT, Li XX, Bao YZ, Yu WZ, Yan Z, Qi HJ, Qian T, Xiao HX. Association of c3 gene polymorphisms with neovascular age-related macular degeneration in a chinese population. Curr Eye Res. 2009;34(8):615–622. doi: 10.1080/02713680903003484. [DOI] [PubMed] [Google Scholar]
- 23.Gao Y, Li Y, Xu L, Zhang HT, Jonas JB, Sun BC. Complement factor H polymorphism in age-related maculopathy in the Chinese population: the Beijing Eye Study. Retina. 2010;30(3):443–446. doi: 10.1097/IAE.0b013e3181c2e086. [DOI] [PubMed] [Google Scholar]
- 24.Liu X, Zhao P, Tang S, Lu F, Hu J, Lei C, Yang X, Lin Y, Ma S, Yang J, et al. Association study of complement factor H, C2, CFB, and C3 and age-related macular degeneration in a Han Chinese population. Retina. 2010;30(8):1177–1184. doi: 10.1097/IAE.0b013e3181cea676. [DOI] [PubMed] [Google Scholar]
- 25.Yang X, Hu J, Zhang J, Guan H. Polymorphisms in CFH, HTRA1 and CX3CR1 confer risk to exudative age-related macular degeneration in Han Chinese. Br J Ophthalmol. 2010;94(9):1211–1214. doi: 10.1136/bjo.2009.165811. [DOI] [PubMed] [Google Scholar]
- 26.Dong L, Qu Y, Jiang H, Dai H, Zhou F, Xu X, Bi H, Pan X, Dang G. Correlation of complement factor H gene polymorphisms with exudative age-related macular degeneration in a Chinese cohort. Neurosci Lett. 2011;488(3):283–287. doi: 10.1016/j.neulet.2010.11.048. [DOI] [PubMed] [Google Scholar]
- 27.Fisher SA, Rivera A, Fritsche LG, Babadjanova G, Petrov S, Weber BH. Assessment of the contribution of CFH and chromosome 10q26 AMD susceptibility loci in a Russian population isolate. Br J Ophthalmol. 2007;91(5):576–578. doi: 10.1136/bjo.2006.105577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Souied EH, Leveziel N, Richard F, Dragon-Durey MA, Coscas G, Soubrane G, Benlian P, Fremeaux-Bacchi V. Y402H complement factor H polymorphism associated with exudative age-related macular degeneration in the French population. Mol Vis. 2005;11:1135–1140. [PubMed] [Google Scholar]
- 29.Nischler C, Oberkofler H, Ortner C, Paikl D, Riha W, Lang N, Patsch W, Egger SF. Complement factor H Y402H gene polymorphism and response to intravitreal bevacizumab in exudative age-related macular degeneration. Acta Ophthalmol. 2011;89(4):e344–349. doi: 10.1111/j.1755-3768.2010.02080.x. [DOI] [PubMed] [Google Scholar]
- 30.Feng X, Xiao J, Longville B, Tan AX, Wu XN, Cooper MN, McAllister IL, Isaacs T, Palmer LJ, Constable IJ. Complement factor H Y402H and C-reactive protein polymorphism and photodynamic therapy response in age-related macular degeneration. Ophthalmology. 2009;116(10):1908–1912 e1901. doi: 10.1016/j.ophtha.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 31.Xing C, Sivakumaran TA, Wang JJ, Rochtchina E, Joshi T, Smith W, Mitchell P, Iyengar SK. Complement factor H polymorphisms, renal phenotypes and age-related macular degeneration: the Blue Mountains Eye Study. Genes Immun. 2008;9(3):231–239. doi: 10.1038/gene.2008.10. [DOI] [PubMed] [Google Scholar]
- 32.Grassi MA, Fingert JH, Scheetz TE, Roos BR, Ritch R, West SK, Kawase K, Shire AM, Mullins RF, Stone EM. Ethnic variation in AMD-associated complement factor H polymorphism p.Tyr402His. Hum Mutat. 2006;27(9):921–925. doi: 10.1002/humu.20359. [DOI] [PubMed] [Google Scholar]