Abstract
Adolescent health researchers and practitioners are frequently interested in assessing depression as part of student screening and for school-wide prevention and intervention planning. However, this task is challenging given the lack of free, brief assessments of depressive symptoms in youth. This study evaluated the psychometric properties of an adapted version of the Modified Depression Scale (MDS). Data came from a school-based survey of 9th-12th graders in Boston (N=1,657). We assessed internal consistency reliability and known-groups validity, in addition to the feasibility of establishing a dichotomous cut-point to classify adolescents as having high versus low depressive symptoms. We also evaluated the validity of the adapted MDS as a school-wide measure. At the student-level, the adapted MDS demonstrated acceptable internal consistency. Students engaging in risk behaviors (e.g., substance use) or who were victimized (e.g., bullied) had significantly higher depressive symptom scores. Students who endorsed four or five MDS symptoms often or always had a heightened risk of suicidal ideation, substance use, and failing grades when compared to students who endorsed three or fewer symptoms often or always. At the school-level, higher mean levels of depressive symptoms in a school were associated with higher mean levels of suicidal ideation and failing grades. Results of this study suggest that the adapted MDS is a promising measurement tool that could be useful to school-based professionals and researchers to evaluate depressive symptoms in adolescents and ascertain the prevalence of depressive symptoms in schools.
Keywords: Depressive symptoms, Population health, Adolescents, Reliability, Validity
Depression is one of the most common mental health problems among adolescents. As many as 30% of adolescents report experiencing symptoms of depression, such as feeling sad or hopeless, that interfere with their functioning (Eaton et al., 2008). Adolescents who experience depressive symptoms are more likely than their non-depressed peers to engage in a variety of risk behaviors, including unsafe sexual activity (Lehrer, Shrier, Gortmaker, & Buka, 2006), cigarette, alcohol, and drug use (Saban & Flisher, 2010), disordered eating (Fulkerson, Sherwood, Perry, Neumark-Sztainer, & Story, 2004), and suicidality (Hallfors et al., 2004). Students who experience depressive symptoms or engage in these risky behaviors are also more likely to have difficulties with learning and meeting the demands of the school environment (Eccles & Roeser, 2011; Hawkins, 1997). These findings suggest that preventing depression among students should be a priority for schools and local or state education authorities.
Recognition of the link between depression, risk behaviors, and academic functioning has led to a growing interest in school-wide or population-based prevention and intervention activities focused on both educational and mental health outcomes among all students in a school (Jones, Brown, & Aber, 2011). These efforts are referred to as universal prevention in that they target the entire school population, rather than individual students, as in the case of a selected or indicated intervention (Mrazek & Haggerty, 1994). To track the progress of these school-wide prevention efforts, and identify the need for them in the first place, schools must monitor the level of depressive symptoms in the entire school (Dowdy, Ritchey, & Kamphaus, 2010). Tracking the prevalence of depressive symptoms among all students in a school is in keeping with a coordinated school health program, which emphasizes not only the provision of counseling, psychological, and social services, but also the assessment of mental, emotional, and social health problems in schools (McKenzie, Pinger, & Kotecki, 2008). Population-based assessments of whole school health are also important given that there is variation across schools in the prevalence of depression. For example, a study using data from the National Longitudinal Study of Adolescent Health found that approximately 5% of the variation in student’s reports of depressive symptoms was due to differences across schools (Dunn & Masyn, 2011). While this level of variation may seem small, when considered from a population-based perspective it suggests that in addition to identifying students who experience depressive symptoms, districts will also benefit from identifying differential school need for interventions.
To engage in school-wide prevention and intervention activities, schools have traditionally used measures that focus on individual students. These include diagnostic assessments, which seek to determine the nature of individual student emotional problems, and screening assessments, which seek to identify individual students who are at-risk for emotional problems and who may therefore benefit from intervention (Glover & Albers, 2007). To complement these tools, schools also need population-based measures, which go beyond classification of individual students and allow schools to engage in: (a) surveillance, to monitor trends in levels of symptoms and associated risk factors among the school population (Dowdy et al., 2010); (b) prediction, to estimate schools at the greatest risk for poor outcomes; and (c) evaluation, to assess the efficacy of a given school-wide prevention or intervention program. For any measure to be practical for school-based researchers or school professionals, whether for use with individual students or entire schools, it must be inexpensive and easy to administer.
Currently, there are few measurement tools focusing on depressive symptoms that are ideally suited to researchers working with schools. As described in review articles (see for example Brooks & Kutcher, 2001; Myers & Winters, 2002), the most widely-used self-report measures of child and adolescent depressive symptoms, such as the Beck Depression Inventory, include more than 20 items (and frequently more than 25), a length that discourages many school-based researchers and those interested in health behaviors from assessing depressive symptoms altogether, particularly when resources are limited. Moreover, most instruments cannot be shortened or modified due to copyright restrictions and must be purchased from publishers, making them too costly for school-based researchers. At the same time, existing low-cost measures used for public health surveillance often fail to capture comprehensive information about depressive symptoms. For instance, the Youth Risk Behavior Surveillance System (YRBS) survey includes only one item to measure depressive symptoms (i.e. “During the past 12 months, did you ever feel so sad or hopeless almost every day for two weeks or more in a row that you stopped doing some usual activities?”) (Centers for Disease Control and Prevention, 2005). Thus, there is a need for a brief and publicly-available tool that: (a) could be easily administered to a large number of students; (b) provides information about the levels of depressive symptoms within a school; and (c) can be used for school-wide planning activities.
After reviewing the literature, we located the Modified Depression Scale (MDS)1 in the Centers for Disease Control and Prevention’s (CDC) compendium of assessment tools for youth violence research (Dahlberg, Toal, Swahn, & Behrens, 2005). The MDS is a self-administered six-item scale designed to assess the frequency of depressive symptoms (e.g., sadness, irritability, hopelessness, sleep disturbance, and concentration difficulties) among adolescents. It is based on the Roberts 26-item DSM Scale for Depression (Kelder et al., 2001; Roberts, Roberts, & Chen, 1997) and was adapted by Bosworth (1996) and published in the Compendium in its adapted form. The MDS is comparable in length to other measures, including the nine-item Patient Health Questionnaire (PHQ) that was also developed based on DSM criteria (Kroenke, Spitzer, & Williams, 2001). Although the PHQ assesses many of the same symptoms as the MDS, it has been primarily used with people older than age 18. Importantly, it does not assess irritability, which is one of the core features of depression in adolescents (American Psychiatric Association, 2000). The MDS is neither a diagnostic nor a classification tool, but instead can be used to identify students at risk of depression.
Even though the MDS could be useful to school-based researchers and practitioners, and has already been used in a number of studies, limited information exists about its psychometric properties. Studies using the MDS with adolescents in locations throughout the US and Canada (Almeida, et al., 2009; Bosworth, et al., 1999; Edwards, et al., 2006; Goldstein, et al., 2007; Tandon & Solomon, 2009), including the World Health Organization-funded Health Behavior in School Age Children Study (Wang, Iannotti, Luk, & Nansel, 2010), have reported the scale demonstrates good internal consistency reliability, with Cronbach’s alpha coefficients of 0.74 or higher. However, detailed information about MDS reliability and validity is lacking. Specifically, little is known about: the underlying factor structure of the MDS, whether MDS scores are associated with risk behaviors, and if it is appropriate as a population-based tool.
The current study was designed to examine the psychometric properties of an adapted version of the MDS in a school-based sample of adolescents for use as a tool to measure depressive symptoms at the level of students and schools. Our research questions were as follows: To what extent is the adapted MDS a reliable measure of depressive symptoms? To what degree are depressive symptoms scores, measured by the adapted MDS, associated with violence and educational outcomes that are known to be related to experiences of depression? Is it feasible to establish a dichotomous cut-point that could be used by schools to identify the percent of students with high levels of depressive symptoms? We explored this last question based on our interest in providing schools with a concise and easily understandable metric (i.e., a percentage) to describe the pervasiveness of depressive symptoms within a school. In evaluating the adapted MDS, we hypothesized that the scale would be a valid and reliable measure, capable of identifying both individual students and schools with high levels of depressive symptoms.
Methods
Subjects
Data came from the 2008 administration of the Boston Youth Survey (BYS), a biennial paper-and-pencil survey of high school students (9th–12th graders) in Boston Public Schools (BPS; Azrael et al., 2009). The BYS 2008 data collection instrument covered a range of topics (e.g., demographic characteristics, health behaviors, use of school and community resources, developmental assets, and risk factors) and had a particular emphasis on violence. Thirty-two eligible public high schools within the BPS system were invited to participate. Additional schools that were considered ineligible for participation were those that served adults (i.e., “night schools”), students transitioning back to school after incarceration, students on suspension, and students who were primarily living outside of Boston (i.e., schools for children with special needs). Twenty-two eligible schools participated in the survey, for a school participation rate of 69%. Among schools considered eligible, we did not observe any statistically significant differences in key school indicators (e.g., drop-out rates, racial composition of students, scores on standardized tests) between participating and non-participating schools.
To acquire a random sample of students within participating schools, we generated a list of unique humanities classrooms within each school. Classrooms were then stratified by grade and selected randomly for survey administration. Every student within the selected classrooms was invited to participate. Selection of classrooms continued until the total number of students to be surveyed ranged from 100–125 per school. In two schools with total enrollments close to 100, all classrooms in the school were invited to participate. An average of 85.4 students per school completed the survey (range: 40–132).
Instruments
Depressive Symptoms
We used an adapted version of the MDS to assess symptoms of depression. Students were asked to report the frequency of five symptoms in the past month: “In the past month, how often …(a) “Were you very sad?”; (b) “Were you grouchy or irritable, or in a bad mood?”; (c) “Did you feel hopeless about the future?”; (d) “Did you sleep a lot more or less than usual?”; and (e) “Did you have difficulty concentrating on your school work?”. They used a five-point response scale: (1) never, (2) rarely, (3) sometimes, (4) often, and (5) always. (The original option of “seldom” was replaced with “rarely” based on feedback from students who participated in pilot testing; they were unfamiliar with the word seldom.). The BYS research team omitted the sixth MDS item on appetite disturbance (“How often did you feel like not eating or eating more than usual?”) to conserve space, with the assumption that the item would be the least discriminating. We derived total scores by summing items among youth who had complete responses for all five items (range: 5–25). We also created a set of categorical variables denoting the percentages of youth who responded “often” or “always” to each survey item as a way of capturing more severe symptoms.
Related Behaviors and Indicators
In addition to the adapted MDS, we measured four indicators of youth well-being: (a) mental health and suicidality; (b) substance use; (c) victimization; and (d) school performance. To assess mental health and suicidality, students were asked whether they had, within the 12 months preceding survey administration, considered suicide, attempted suicide, cut or injured themselves, and visited a mental health professional. We assessed substance use by asking if students used alcohol, tobacco, or marijuana in the past 30 days. We assessed victimization through a series of questions asking about being bullied, physical victimization by peers (e.g., punched, kicked by other kids), and family violence (e.g., punched, grabbed, by an adult in the home). School performance was assessed by asking respondents about their grades and truancy. Students who reported having “mostly D’s” or “mostly F’s” were classified as having failing grades and those who reported skipping school one or more times in the past month were classified as truant. Items related to suicidal ideation, suicide attempts, and substance use were adapted from the 2005 Youth Risk Behavioral Surveillance System questionnaire (Centers for Disease Control and Prevention, 2005). Items related to physical victimization from parents and peers were modified from the Conflict Tactics Scales (CTS Straus, 2007). The item on bullying was adapted from Rigby (1998). All other items were developed by the BYS research team. For school-level analyses, we created adapted MDS school-level means by taking the average MDS total score within each school.
Demographic Characteristics
The BYS also measured student’s grade in school, sex, Hispanic ethnicity, nativity (i.e., US or foreign-born), and race. We used a race/ethnicity variable with five levels: (a) Hispanic/Latino; (b) Non-Hispanic, Black/African American; (c) Non-Hispanic, White; and (d) Non-Hispanic, Asian, and (e) Other, which includes those who were bi- or multi-racial, Native Hawaiian or other Pacific Islander, American Indian, or Alaska Native. We also created school-level means for three of these variables, representing the proportion of students in the school who were female, Non-Hispanic White, and foreign-born.
Procedure
The paper-and-pencil survey was administered to students by trained staff between January and April of 2008. Prior to survey administration, we obtained passive consent from students’ parents. Survey administrators also read a statement on informed consent before each survey was distributed. Students were given 50 minutes to complete the survey. Of the 2,725 students enrolled in the classrooms selected for participation, 1,878 completed a survey (response rate = 68.9%). Students who did not complete a survey either (a) chose not to participate (n = 99), (b) were not permitted by their parent to take the survey (n = 24), or (c) were absent from school on the day of survey administration (n = 724).
Data Analysis
Given that we were interested in evaluating the adapted MDS for the use as both an individual and school-level tool to evaluate levels of depressive symptoms, we conducted our analyses at both the individual and school levels. We began by conducting univariate analyses to describe the distribution of each item and the total MDS scale in this sample and among males and females. We calculated an intraclass correlation coefficient (ICC) to determine the proportion of variation in depressive symptoms that was due to difference across schools (rather than differences within schools, across students). Next, we conducted bivariate analyses to determine whether mean scores and proportions significantly varied across subgroups. To assess reliability, we conducted a categorical factor analysis, a type of analysis designed for ordinal data. In contrast to a continuous factor analysis, a categorical factor analysis does not require that data are continuous or that any distributional assumptions, such as normality, are met (Flora & Curran, 2004). We also used tetrachoric correlations, designed for categorical data, to examine the strength, direction, and magnitude of the associations between each MDS item. We then estimated the internal consistency reliability of the total MDS score by calculating Cronbach’s alpha coefficients for the total sample and separately for males and females. We also examined item-to-total score correlations, Cronbach’s alpha coefficients when specific items of the scale were deleted, and evaluated whether floor or ceiling effects were present (Terwee et al., 2007). We sought to provide information for known-groups validity, a type of convergent construct validity (DeVellis, 2003), by comparing risk behavior and victimization status on the basis of MDS total scores, because youth who engage in risk behaviors or experience violence are more likely to have higher levels of depressive symptoms. We also examined, at the school level, the association between average MDS scores and rates of engagement in risk behaviors. Based on our interest in determining whether the adapted MDS could be used as a binary indicator to differentiate youth with high levels of depressive symptoms from those with lower levels of depression or no symptoms, we created a set of binary variables indicating the number of youth who endorsed “often” or “always” to each MDS item. We calculated odds ratios denoting the risk of experiencing each risk behavior or type of violence based on the number of items where youth reported high levels of depressive symptoms (e.g., endorsed often/always).
We conducted analyses with SAS Version 9.2 (alpha < 0.05 was the level of statistical significance). We stratified some analyses by sex based on well-documented sex differences in depression (Nolen-Hoeksema & Hilt, 2009), and restricted analyses to students who completed all five items on the adapted MDS scale. For individual-level descriptive statistics and tests of validity, in which standard errors were estimated, we accounted for the correlated nature of the observations or clustering of students within school by using generalized estimating equations (GEE) (Hanley, Negassa, deB. Edwardes, & Forrester, 2003). All individual-level tests of validity controlled for sex, age, and race/ethnicity. All school-level tests of validity were conducted using multiple linear regression models that were adjusted for the percentage of students in the school who were female and non-Hispanic White. We conducted analyses for the categorical factor analysis in Mplus version 6.1, which accounted for clustering of students in schools. Acceptable model fit was determined by a non-significant chi-square test, CFI and TLI values greater than 0.95, and RMSEA and SRMR values below 0.05 (Kline, 2010).
Results
Sample
To conduct psychometric analyses using a complete case analysis, we removed 221 youth (11.8%) missing data on any of the five MDS items, creating an analytic sample of 1,657. Missingness ranged from 10.3% on the sleep disturbance item to 8.8% on the sadness item. More than half of respondents in the analytic sample were female (54.0%). The sample was ethnically diverse, with 42.4% of students identifying as non-Hispanic Black, 33.4% Hispanic/Latino, 9.3% non-Hispanic White, 8.1% Asian, and 6.7% Other or Multiracial. Respondents ranged in age from 13 to 19 years (8.0% were ≤14 years; 19.0% were 15; 27.7% were 16; 26.8% were 17; and 18.5% were ≥18 years), and were distributed almost equally across grades (24.4% from 9th grade; 27.2% from 10th grade; 26.8% from 11th grade; 21.5% from 12th grade). Nearly one-third were born outside of the US. Participants excluded from the analytic sample were not significantly different from those in the analytic sample with respect to race/ethnicity or age, though a greater percentage of excluded participants were male (58.4% vs. 46.1%, z = 0.002). With respect to the school-level characteristics, the average school consisted of half males and females (M = 52.61; range 22.0% – 69.0% female), a majority of students who were non-White (M = 7.34; range 0% – 47.3% non-Hispanic White), and almost a third of students who were foreign-born (M = 31.08; range 10.3% – 61.8% foreign born).
Student-Level Descriptive Statistics
Table 1 describes the distribution of adapted MDS scores in the total sample and stratified by sex. Items corresponding to irritability and sleep problems had the highest mean values (M = 2.9 for each), and the item related to feeling hopeless had the lowest (M = 2.1). Females had significantly higher mean total scores (z = 8.81, p < 0.0001) as well as higher scores on each of the five items. Females more often reported experiencing MDS items often/always.
Table 1.
Descriptive Statistics for the Modified Depression Scale (MDS) by Each Item and the Total Score
| Survey Item In the past 30 days, how often: | Total Sample (n=1657) | Females (n=891) | Males (n=762) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | (SE) | % Reporting Often/Always | M | (SE) | % Reporting Often/Always | M | (SE) | % Reporting Often/Always | z-statistic for means | z-statistic for proportions | |
| Were you very sad? (Sadness) | 2.6 | (0.04) | 20.0 % | 2.9 | (0.03) | 27.6 % | 2.2 | (0.05) | 11.3 % | 12.91*** | 9.10*** |
| Were you grouchy, irritable, or in a bad mood? (Irritability) | 2.9 | (0.05) | 26.7 % | 3.1 | (0.05) | 33.5 % | 2.7 | (0.06) | 18.6 % | 7.91*** | 8.60*** |
| Did you feel hopeless about the future? (Hopelessness) | 2.1 | (0.04) | 15.6 % | 2.3 | (0.05) | 18.7 % | 2.0 | (0.06) | 11.9 % | 3.94*** | 3.24** |
| Did you sleep a lot more or a lot less than usual? (Sleep problems) | 2.9 | (0.04) | 31.6 % | 3.0 | (0.06) | 36.0 % | 2.7 | (0.04) | 26.4 % | 4.65*** | 3.77*** |
| Did you have difficulty concentrating on your school work? (Concentration difficulties) | 2.8 | (0.04) | 28.5 % | 2.9 | (0.06) | 30.9 % | 2.7 | (0.05) | 25.6 % | 3.39*** | 3.53*** |
| Total Score | 13.3 | (0.17) | 55.9 % | 14.2 | (0.17) | 62.6% | 12.2 | (0.19) | 47.8% | 8.81*** | 6.89*** |
Cell entries are estimates of the mean, adjusted standard errors (adjusted for clustering), the percentage of respondents who reported often/always for each item and on every item (total score), as well as t-statistics and χ2 statistics for analyses comparing females and males. Results derived from generalized estimating equations (GEE).
~p<0.10,
p<0.05,
p<0.001,
p<0.0001
We examined the distribution of adapted MDS scores across groups expected to differ in their levels of depressive symptoms. Average MDS scores were significantly higher among older students (z-statistic = 2.58, p = 0.01) and differed by race/ethnicity (z-statistic = 0.06, p = 0.02). However, there were no statistically significant differences in MDS scores among those born in the US compared to those born in another country (z-statistic = −1.11, p = 0.27).
School-Level Descriptive Statistics
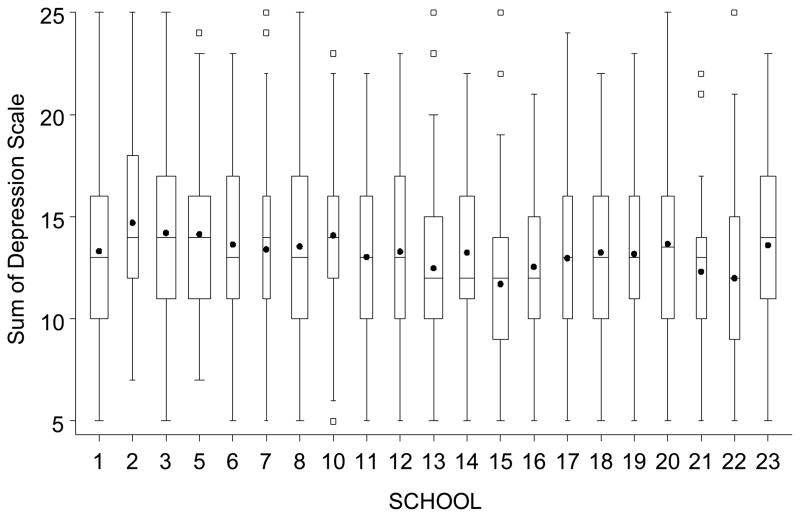
Figure 1 presents the distribution of MDS scores by schools. Mean depressive symptoms scores across schools ranged from 11.7 to 14.7, with the average depression score across schools being 13.2 (SE = 0.16, p < 0.0001). Although the variation within schools was greater than the variation across schools, there was significant between-school variation in depressive symptoms (σ2between = 0.30, p= 0.03). Specifically, the ICC showed that 1.6% of the variability in depressive symptoms could be attributed to differences across schools.
Figure 1. Distribution of MDS scores within and between schools (n=21).
The figure presents box plots depicting the distribution of MDS scores within each school and across all of schools in the sample. Dots represent the mean adapted MDS scores within the school. Horizontal lines in the boxes, for each school, represent the first quartile, the median, and the third quartile of the distribution of adapted MDS total scores within each school. Vertical lines depict the range of total scores (minimum to maximum values) in each school. Squares depict outlying values.
Factor Structure and Correlations
The adapted MDS was unidimensional (unrotated eigenvalues=2.96, 0.72); this one factor had good overall fit (χ2=242.77; CFI=0.94; TLI=0.88; RMSEA=0.17; SRMR=0.05). The proportion of variance in each item (or observed variable) that was explained by the factors ranged from 40% for sleep to 57% for sad. There were high and consistent factor loadings for all items (0.63–0.75). Factor loadings were highest for items measuring intrapsychic depressive symptoms, such as sadness and irritability (0.75 and 0.73, respectively), and lowest for items assessing somatic symptoms, such as sleep disturbance and difficulty with concentration (0.63 and 0.66, respectively). Tetrachoric correlation coefficients indicated that MDS items were moderately and significantly correlated (r = 0.40 – 0.62). The intrapsychic symptoms of sadness, irritability, and hopelessness were most strongly correlated with one another. Sleep disturbance had the weakest correlation with other items (r = 0.44 – 0.40).
Floor or Ceiling Effects
The adapted MDS did not have floor or ceiling effects, that is no more than 15% of the sample had the lowest or highest possible score. Total adapted MDS scores were normally distributed, with 4.5% of students having the lowest score (5) and 0.9% having the highest (25).
Internal Consistency Reliability
The adapted MDS displayed acceptable internal consistency reliability in the total sample (Cronbach’s α = 0.79; Table 2). The Cronbach’s alpha coefficient did not increase with the deletion of any individual items; it decreased the least with the deletion of sleep problems. Findings from sex-stratified analyses were similar to the total sample. However, for females, the items corresponding to sadness and hopelessness correlated most strongly with the total score, whereas hopelessness and irritability were most strongly correlated to the total score for males.
Table 2.
Internal Consistency Reliability Values of the Modified Depression Scale (MDS) in the BYS Sample
| Survey Item | Total Sample (n=1657) | Females (n=891) | Males(n=762) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| r to Total Score | α | α if Item Deleted | r to Total Score | α | α if Item Deleted | r to Total Score | α | α if Item Deleted | |
| Sadness | 0.60 | 0.74 | 0.60 | 0.72 | 0.57 | 0.74 | |||
| Irritability | 0.59 | 0.74 | 0.57 | 0.73 | 0.58 | 0.74 | |||
| Hopelessness | 0.59 | 0.74 | 0.59 | 0.72 | 0.59 | 0.73 | |||
| Sleep problems | 0.51 | 0.77 | 0.47 | 0.76 | 0.52 | 0.76 | |||
| Concentration difficulties | 0.55 | 0.76 | 0.55 | 0.74 | 0.55 | 0.75 | |||
| Total Score | 0.79 | 0.78 | 0.78 | ||||||
Cell entries are raw Pearson’s r correlation coefficients between individual items and the total MDS score, Cronbach’s alpha coefficient, and Cronbach’s alpha coefficient if the individual item were deleted.
Known-Groups Validity
Table 3 presents the result of analyses examining the association between victimization and risk behaviors with MDS scores. Odd ratios (Ors) refer to the odds of each risk status for each one unit difference in the MDS symptom total score. The adapted MDS significantly differentiated youth who had engaged in risk behavior or who had been victimized from those who had not (Ors ranged from 1.07–1.31, all p < 0.001). The strongest association was between the MDS and reports of suicidal ideation.
Table 3.
Results of Student-Level Analyses Estimating the Log Odds of Behavior/Victimization Status based on MDS Total Score
| OR | 95% CI | |
|---|---|---|
| Mental Health and Suicidality | ||
| Considered suicide (n=197) | 1.31 | 1.26–1.37 |
| Attempted suicide (n=66) | 1.27 | 1.20–1.34 |
| Cut/injured self (n=141) | 1.21 | 1.16–1.25 |
| Visited professional (n=382) | 1.14 | 1.11–1.17 |
| Substance Use | ||
| Drank alcohol (n=621) | 1.10 | 1.07–1.13 |
| Used tobacco (n=205) | 1.16 | 1.10–1.21 |
| Used marijuana (n=320) | 1.07 | 1.03–1.11 |
| Victimization | ||
| Bullied by Peers (n=677) | 1.12 | 1.09–1.15 |
| Victimized by Peers (n=370) | 1.10 | 1.07–1.12 |
| Experienced Family Violence (n=263) | 1.14 | 1.09–1.20 |
| School Performance | ||
| Failing Grades (n=243) | 1.11 | 1.08–1.15 |
| Truant (n=588) | 1.08 | 1.05–1.11 |
Cell entries are adjusted odds ratios (adjusted for clustering) and 95% CI (Confidence Interval). All OR were statistically significant at p<0.0001. Cell sizes across analyses may not sum to total N due to missing data. All analyses controlled for sex, age, and race/ethnicity.
Table 4 presents the results of the school-level analyses examining the association between school-level depressive symptoms and school-level risk behavior problems. The adapted MDS significantly differentiated schools with a high prevalence of students who considered suicide and received failing grades. Specifically, we found that each one unit difference in the average MDS score within a school was associated, on average, with a 5.3% difference in the proportion of students who had received failing grades and an 8.2% difference in the proportion of students who had considered suicide. However, MDS scores were not significantly associated with any other school-level risk factors.
Table 4.
Results of School-Level Analyses Estimating the Prevalence of Behavior/Victimization Status based on MDS Total Score
| Beta (s.e.) | p-value | |
|---|---|---|
| Mental Health and Suicidality | ||
| Considered suicide (12.2) | 8.21 (2.75) | 0.01 |
| Attempted suicide (4.6) | 5.50 (3.63) | 0.15 |
| Cut/injured self (8.7) | 6.45 (3.95) | 0.12 |
| Visited professional (24.3) | 1.11 (1.73) | 0.53 |
| Substance Use | ||
| Drank alcohol (38.9) | −0.16 (1.45) | 0.91 |
| Used tobacco (13.0) | 0.35 (2.06) | 0.87 |
| Used marijuana (20.4) | −0.73 (1.85) | 0.70 |
| Victimization | ||
| Bullied by Peers (41.5) | 1.59 (1.39) | 0.27 |
| Victimized by Peers (23.8) | 0.72 (1.85) | 0.70 |
| Experienced Family Violence (16.5) | 2.17 (2.50) | 0.40 |
| School Performance | ||
| Failing Grades (16.3) | 5.30 (1.56) | 0.01 |
| Truant (38.0) | 0.76 (1.11) | 0.50 |
Cell entries are beta coefficients and standard errors (S.E.). Parentheses next to each risk factor indicator refer to the average level of each indicator across all schools (i.e. the average school-wide percent). All analyses controlled for percentage of students in the school who were female and White.
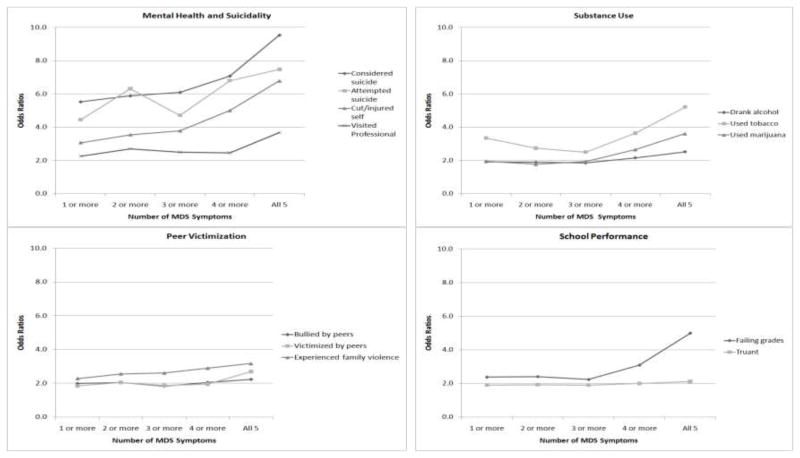
In examining frequent depressive symptoms, we found that 55.9% reported experiencing at least one MDS symptom often or always (last row of Table 1). Moreover, 34.1% of the total sample reported experiencing two or more symptoms at this frequency, 18.3% reported three or more symptoms, 9.6% reported four or more symptoms, and 4.4% endorsed all five MDS items often/always. Figure 2 presents the results of analyses investigating whether there was an appropriate cut-point to differentiate youth with high depressive symptoms from all others. The figure is organized according to the number of items youth endorsed as often/always, with adjusted odds ratios that compare the log odds of each risk behavior among those with a score of one or more, two or more, three or more, four or more, or five on the MDS (versus youth with fewer symptoms). Results of these analyses suggest that several outcomes increased considerably among youth who endorsed four or five (vs. three or fewer) MDS symptoms: considered suicide, attempted suicide, cut/injured self, drank alcohol, used tobacco, reported failing grades. However, this pattern was not consistent across other outcomes, which either increased linearly and did not have a clear cut-point (e.g., family violence) or were unrelated to MDS scores (e.g., used marijuana, bullied, truant). The odds of experiencing each outcome increased from 1.90 to 5.53-fold among those reporting one or more symptoms of depression (compared to those reporting no symptoms) to between 2.12 and 9.54-fold among those reporting all five symptoms (compared to those reporting fewer).
Figure 2. Results of Generalized Estimating Equation (GEE) Analyses Estimating the Log Odds of Each Behavior/Victimization Status by MDS Category Score.
Cell entries are adjusted odds ratios (adjusted for clustering) and 95% CI. All OR were statistically significant at p<0.0001. The referent group for each comparison (i.e. OR) is youth with a fewer number of symptoms (e.g., 1 or more symptoms compared to zero; 2 or more symptoms compared to zero or 1 symptoms). Analyses controlled for sex, age, and race/ethnicity. Sample sizes for each MDS score were: n = 926 endorsed 1 or more MDS symptoms, n = 565 endorsed 2 or more MDS symptoms, n = 304 endorsed 3 or more MDS symptoms, n = 159 endorsed 4 or more MDS symptoms, n = 73 endorsed all 5 symptoms.
Discussion
In response to the need for a brief, reliable, and inexpensive measure of depressive symptoms for researchers in schools, we set out to assess the psychometric properties of an adapted Modified Depression Scale (MDS) for use with adolescents. Results demonstrate that the adapted MDS has good reliability and validity. Consistent with other studies of the MDS (Bosworth, et al., 1999; Edwards, et al., 2006; Goldstein, et al., 2007), we found that – in a school-based sample of Boston youth – the adapted MDS had acceptable internal consistency reliability (α=0.79). It also did not have floor or ceiling effects. We extend previous work on the MDS by showing the adapted version had a clear unidimensional structure with highest factor loadings for items that characterize intrapsychic symptoms of depression (sadness, irritability, and hopelessness). This is in keeping with current thinking regarding the nosology of depression in youth, as the DSM-IV identifies sadness and irritability (in children and adolescents) as core symptoms of depression (American Psychiatric Association, 2000). By comparison, the somatic symptoms measured by the MDS (sleep problems and concentration difficulties) had lower factor loadings and reduced correlations with other items. Although somatic symptoms are listed as indicators of depression in the DSM-IV, they can also be markers of a number of other psychological problems (e.g., anxiety, attention-deficit/hyperactivity disorder, substance use); it is therefore not surprising that they were less strongly associated with the total score.
This study also shows that the adapted MDS demonstrated strong known-groups validity, as it differentiated both youth and schools on the basis of several risk factors. Consistent with current literature on risk factors associated with depression, those with higher MDS total scores were more likely to: be female (Nolen-Hoeksema & Hilt, 2009), have experienced peer victimization and bullying (Klomek, Marrocco, Kleinman, Schonfeld, & Gould, 2007), have recently used alcohol, tobacco, and marijuana (Armstrong & Costello, 2002; Kandel et al., 1997), and display other indicators of psychological distress, including suicidal ideation, self-injury, and receipt of psychological services (Alexandre, Dowling, Stephens, Laris, & Rely, 2008; Fergusson, Beautrais, & Horwood, 2003; Hallfors, et al., 2004; Osman, Kopper, Barrios, Gutierrez, & Bagge, 2004). Odds ratios for these effects were high (range: 1.07–1.31), especially as they represented the odds of each risk status for just a one unit difference in the MDS score. These findings suggest that the adapted MDS is useful for predictive purposes in that it can effectively serve as an indicator of depressive symptoms that increase adolescents’ risk for a number of poor psychosocial outcomes. Based on these results, school researchers should co-administer the MDS with other brief measures of psychosocial functioning in an effort to understand predictors or correlates of depressive symptoms at both the level of students and schools (Dowdy, et al., 2010). These types of comprehensive measurement tools have been used with other mental health outcomes in youth, including eating disorders (Shisslak et al., 1999), and would enable schools to understand school-wide levels of these co-occurring experiences.
We also found that schools with high average MDS scores also have, on average, higher levels of students who considered suicide and received failing grades. These findings suggest that the MDS may be able to detect not just individual students in need, but also schools in need of global prevention and intervention services. The finding that the adapted MDS was more strongly associated with psychosocial risk factors at the student-level, compared to risk factors at the school-level, suggests that the MDS may be a better predictor of student need rather than school need. However, our study may not have been powered to the same degree at both levels of analysis (i.e. at the student-level and school-level). That is, although we included a large number of students in this sample, we included a relatively small number of schools and only had modest levels of between-school variation in depressive symptoms (even though this level was statistically significant). Thus, the finding that school levels of considering suicide and receiving failing grades was associated with school levels of depressive symptoms suggests these associations are quite robust. Indeed, just a one unit difference in the average MDS score within a school was associated, on average, with a 5.3% difference in the proportion of students who had received failing grades and an 8.2% difference in the proportion of students who had considered suicide and received failing grades. Future studies that include a larger number of schools will be better able to detect more moderate associations.
Further research is also needed on the most effective application of the MDS to estimating school-wide risk for depression and informing prevention and intervention planning. More detailed school-level analyses of the association between the related risk factors and MDS scores, as well as school-level demographic features (e.g., school demographic composition; teacher training and tenure) could identify important between-school differences that have relevance for program implementation. These types of analyses will be important for determining the applicability of the MDS for mental health services planning and determining the schools most in need of prevention and intervention efforts.
Analyses to determine whether the adapted MDS could be used with a dichotomous cut-point suggest that adolescents who experienced any of the MDS symptoms often/always had significantly increased risk for most of the psychosocial outcomes we considered. Endorsing four or five MDS symptoms heightened risk for suicidality, substance use, and failing grades. These findings were not surprising, as the association between these risk factors and depression is well-established. In contrast, the cut-point did not distinguish between adolescents with high and low levels of depressive symptoms on more distal outcomes (e.g., peer victimization, truancy). Rather than being linked directly, these indicators may represent mediating pathways (e.g., depressive symptoms causes weight gain, which in turn leads to being bullied by peers). We also found that the proportion of students endorsing four or more depressive symptoms often/always (9.6%) was consistent with existing epidemiological research on the prevalence of major depression in adolescents (Green, McGinnity, Meltzer, Ford, & Goodman, 2005; Merikangas et al., 2010). Based on these findings, we think researchers interested in the MDS as a binary indicator (depressed/not depressed) may find the ≥4 cut-point useful.
Limitations and Future Directions
This study had several limitations. First, the BYS research team omitted the item measuring appetite disturbance from the MDS. This was done to shorten the data collection instrument so as to reduce respondent burden and keep the instrument short enough to be completed within a class period. This decision was made on the basis of familiarity with the instrument, rather than empirical and psychometric data. Given our finding that the MDS somatic items (i.e., sleep problems and concentration difficulties) had lower factor loadings than the intrapsychic items, and consistent with other studies (Ward, 2006), we suspect that appetite disturbance would have also had a reduced association with other items and thus provided less information about depressive symptoms. Second, all measures included in this study are based on self-report of adolescents and it is possible that associations between the MDS and other risk factors were artificially inflated by common method variance. Although it is often difficult for schools to collect data from multiple informants (e.g., teachers, parents), conducting a multi-informant analysis could provide additional information about the validity of the MDS. Third, although our results indicate that the adapted MDS is strongly associated with risk factors related to depression, without a co-administered “gold standard” assessment of depressive symptoms, it is difficult to fully ascertain the validity of the MDS. Future research on the MDS should include a co-administered depressive symptoms measure.
Conclusions
Results of this study provide good preliminary evidence to document the reliability and validity of the MDS, which is increasingly being used in large school-based studies to measure depressive symptoms among youth (e.g. Wang, et al., 2010). The MDS fills an important need for school researchers as a brief, inexpensive, and publicly-available tool for evaluating depressive symptoms in adolescents and ascertaining the prevalence of depressive symptoms in schools. By surveying student depressive symptoms, schools can determine the level of need of their students, detect trends over time, and select appropriate prevention and intervention programs. This type of surveillance is critical for reducing depressive symptoms, monitoring associated risk behaviors, and ultimately improving the health and well-being of school children. The brevity of the MDS, combined with its psychometric properties, make it well-suited for survey activities that are limited in their resources or space. The MDS is therefore a very good option for both schools who want to conduct epidemiological activities and school-based researchers interested in incorporating a measure of depression into their study.
Acknowledgments
Funding: This work was supported by a grant from the Center for Disease Control and Prevention (CDC) National Center for Injury Prevention and Control (NCIPC) (U49CE00740) to the Harvard Youth Violence Prevention Center (David Hemenway, Principal Investigator) and a pre-doctoral training grant from the National Institute of Mental Health (F31MH088074) to Erin C. Dunn. This work was also supported by a grant from the Robert Wood Johnson Foundation through the New Connections Program to Renee M. Johnson. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health, the National Institutes of Health, or the Robert Wood Johnson Foundation.
The Boston Youth Survey (BYS) was conducted in collaboration with the Boston Public Health Commission (Barbara Ferrer, Director), Boston’s Office of Human Services (Larry Mayes, Chief), Boston Public Schools (Carol Johnson, Superintendent) and the Office of The Honorable Mayor Thomas M. Menino. The survey would not have been possible without the participation of the faculty, staff, administrators, and students of Boston Public Schools. We also acknowledge the work of Daria Fanelli, Alicia Savannah, Angela Browne, Dan Dao, Beth Molnar and all those who participated in survey administration. We give special thanks to Mary Vriniotis, MSPH and Deborah Azrael, PhD for their contributions to the project that made these analyses possible and to Gheorghe Doros, PhD and Janice Weinberg, ScD for assisting with statistical analysis.
Footnotes
The CDC Compendium inaccurately attributed the MDS to Pamela Orpinas rather than Kris Bosworth (personal communication, Dr. Linda Dahlberg, Centers for Disease Control and Prevention, 9/21/2009)
Contributor Information
Erin C. Dunn, Email: erindunn@hsph.harvard.edu, Department of Society, Human Development, and Health, Harvard School of Public Health. 677 Huntington Avenue, Boston, MA 02115. phone: 617-935-1290
Renee M. Johnson, Email: rjohnson@bu.edu, Department of Community Health Sciences, Boston University School of Public Health, Boston, MA
Jennifer G. Green, Email: jggreen@bu.edu, Jennifer G. Green, Special Education Program, Boston University School of Education, Boston, MA
References
- Alexandre PK, Dowling K, Stephens RN, Laris AS, Rely K. Predictors of outpatient mental health service use by American youth. Psychological Services. 2008;5:251–261. doi: 10.1037/1541-1559.5.3.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida J, Johnson RM, Corliss HL, Molnar BE, Azrael D. Emotional distress among LGBT youth: The influence of perceived discrimination based on sexual orientation. Journal of Youth and Adolescence. 2009;38:1001–1014. doi: 10.1007/s10964-009-9397-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. text revision ed. [Google Scholar]
- Armstrong TD, Costello EJ. Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology. 2002;70:1224–1239. doi: 10.1037//0022-006x.70.6.1224. [DOI] [PubMed] [Google Scholar]
- Azrael D, Johnson RM, Molnar BE, Vriniotis M, Dunn EC, Duncan DT, Hemenway D. Creating a youth violence data system for Boston, Massachusetts. Australian and New Zealand Journal of Criminology. 2009;43(3):406–421. [Google Scholar]
- Bosworth K, Espelage D, DuBay T, Dahlberg LL, Daytner G. Using multimedia to teach conflict-resolution skills to young adolescents. American Journal of Preventive Medicine. 1996;12(5):65–74. [PubMed] [Google Scholar]
- Bosworth K, Espelage DL, Simon TR. Factors associated with bullying behavior in middle school students. Journal of Early Adolescence. 1999;19(3):341–362. [Google Scholar]
- Brooks SJ, Kutcher S. Diagnosis and measurement of adolescent depression: A review of commonly utilized instruments. Journal of Child and Adolescent psychopharmacology. 2001;11(4):341–376. doi: 10.1089/104454601317261546. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2005 National Youth Risk Behavior Surveillance (YRBS) Data Users Manual. Atlanta, GA: 2005. [Google Scholar]
- Dahlberg LL, Toal SB, Swahn M, Behrens CB. Measuring Violence-Related Attitudes, Behaviors, and Influences Among Youths: A Compendium of Assessment Tools. 2. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2005. [Google Scholar]
- DeVellis RF. Scale development: theory and applications. 2. Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]
- Dowdy E, Ritchey K, Kamphaus RW. School-based screening: A population-based approach to inform and monitor children’s mental health needs. School Mental Health. 2010;2:166–176. doi: 10.1007/s12310-010-9036-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EC, Masyn KE. Using multi-level factor analysis to capture features of youth and their experiences of context: An illustration focusing on schools. Paper presented at the Society for Prevention Research Meeting; Washington, DC. 2011. [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Weschsler H. Morbidity and Mortality Weekly: Surveillance Summaries. 2008. Youth Risk Behavior Surveillance - United States, 2007. [PubMed] [Google Scholar]
- Eccles JS, Roeser RW. School and community influences on human development. In: Bornstein MH, Lamb ME, editors. Developmental science: An advanced textbook. 6. New York, NY: Psychology Press; 2011. pp. 571–643. [Google Scholar]
- Edwards MC, Green C, Perkins UE. Teen dating violence, ethnic identity, and depression in inner city african american youths and young adults. Journal of Knowledge and Best Practice in Juvenile Justice and Psychology. 2006;1(1):41–50. [Google Scholar]
- Fergusson DM, Beautrais AL, Horwood LJ. Vulnerability and resiliency to suicidal behaviours in young people. Psychological Medicine. 2003;33:61–73. doi: 10.1017/s0033291702006748. [DOI] [PubMed] [Google Scholar]
- Flora DB, Curran PJ. An empirical evaluation of alternative methods of estimation for confirmatory factor analysis with ordinal data. Psychological Methods. 2004;9(4):466–491. doi: 10.1037/1082-989X.9.4.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulkerson JA, Sherwood NE, Perry CL, Neumark-Sztainer D, Story M. Depressive symptoms and adolescent eating and health behaviors: a multifaceted view in a population-based sample. Preventive Medicine. 2004;38(6):867–875. doi: 10.1016/j.ypmed.2003.12.028. [DOI] [PubMed] [Google Scholar]
- Glover TA, Albers CA. Considerations for evaluating universal screening assessments. Journal of School Psychology. 2007;45:117–135. [Google Scholar]
- Goldstein AL, Walton MA, Cunningham RM, Trowbridge MJ, Maio RF. Violence and substance use as risk factors for depressive symptoms among adolescents in an urban emergency department. Journal of Adolescent Health. 2007;40:276–279. doi: 10.1016/j.jadohealth.2006.09.023. [DOI] [PubMed] [Google Scholar]
- Green H, McGinnity A, Meltzer H, Ford T, Goodman R. Mental health of children and young people in Great Britain, 2004. Office of National Statistics; 2005. [Google Scholar]
- Hallfors DD, Waller MW, Ford CA, Halpern CT, Brodish PH, Iritani B. Adolescent depression and suicide risk: Association with sex and drug behavior. American Journal of Preventive Medicine. 2004;27(3):224–230. doi: 10.1016/j.amepre.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Hanley JA, Negassa A, deB Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: An orientation. American Journal of Epidemiology. 2003;157(4):364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- Hawkins JD. Academic performance and school success: Sources and consequences. In: Weissberg RP, Gullotta TP, Hampton RL, Ryan BA, Adams GR, editors. Enhancing children’s wellness. Healthy Children 2010. Issues in Children’s and Families’ Lives. Vol. 8. Thousand Oaks, CA: Sage Publications; 1997. pp. 278–305. [Google Scholar]
- Jones SM, Brown JL, Aber JL. Two-year impacts of a universal school-based social-emotional and literacy intervention: An experiment in translational developmental research. Child Development. 2011;82(2):533–554. doi: 10.1111/j.1467-8624.2010.01560.x. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Johnson JG, Bird HR, Canino G, Goodman SH, Lahey BB, Schwab-Stone M. Psychiatric disorders associated with substance use among children and adolescents: Findings from the Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study. Journal of Abnormal Child Psychology. 1997;25:121–132. doi: 10.1023/a:1025779412167. [DOI] [PubMed] [Google Scholar]
- Kelder SH, Murray NG, Orpinas P, Prokhorov A, McReynolds L, Zhang Q, Roberts R. Depression and substance use in minority middle-school students. American Journal of Public Health. 2001;91(5):761–766. doi: 10.2105/ajph.91.5.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 3. New York, NY: Guilford Press; 2010. [Google Scholar]
- Klomek AB, Marrocco F, Kleinman M, Schonfeld IS, Gould MS. Bullying, depression, and suicidality in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:40–49. doi: 10.1097/01.chi.0000242237.84925.18. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehrer JA, Shrier LA, Gortmaker S, Buka S. Depressive symptoms as a longitudinal predictor of sexual risk behaviors among US middle and high school students. Pediatrics. 2006;118(1):189–200. doi: 10.1542/peds.2005-1320. [DOI] [PubMed] [Google Scholar]
- McKenzie JF, Pinger RR, Kotecki JE. An introduction to community health. Sudbury, MA: Jones and Bartlett Publishers; 2008. The school health program: A component of community health; pp. 145–170. [Google Scholar]
- Merikangas KM, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrazek PJ, Haggerty RJ, editors. Reducing risks for mental disorders: Frontiers for preventive research. Washington, DC: National Academy Press; 1994. [PubMed] [Google Scholar]
- Myers K, Winters NC. Ten-year review of rating scales II: Scales for internalizing disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(6):634–659. doi: 10.1097/00004583-200206000-00004. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Hilt LM, editors. Gender differences in depression. 2. New York, NY: The Guilford Press; 2009. [Google Scholar]
- Osman A, Kopper BA, Barrios F, Gutierrez PM, Bagge CL. Reliability and validity of the Beck Depression Inventory-II with adolescent psychiatric inpatients. Psychological Assessment. 2004;16:120–132. doi: 10.1037/1040-3590.16.2.120. [DOI] [PubMed] [Google Scholar]
- Rigby K. The relationship between problems among male and female secondary school children. Journal of Health Psychology. 1998;3:465–479. doi: 10.1177/135910539800300402. [DOI] [PubMed] [Google Scholar]
- Roberts R, Roberts CR, Chen YR. Ethnocultural differences in prevalence of adolesent depression. American Journal of Community Psychology. 1997;25(1):95–110. doi: 10.1023/a:1024649925737. [DOI] [PubMed] [Google Scholar]
- Saban A, Flisher AJ. The association between psychopathology and substance use in young people: A review of the literature. Journal of Psychoactive Drugs. 2010;42(1):37–47. doi: 10.1080/02791072.2010.10399784. [DOI] [PubMed] [Google Scholar]
- Shisslak CM, Renger R, Sharpe T, Crago M, McKnight KM, Gray N, Taylor CB. Development and evaluation of the McKnight Risk Factor Survey for assessing potential risk and protective factors for disordered eating in preadolescent and adolescent girls. International Journal of Eating Disorders. 1999;25:195–214. doi: 10.1002/(sici)1098-108x(199903)25:2<195::aid-eat9>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Straus MA. Conflict tactic scales. In: Jackson NA, editor. Encyclopedia of Domestic Violence. New York, NY, Routledge: Taylor and Francis Group; 2007. pp. 190–197. [Google Scholar]
- Tandon DS, Solomon BS. Risk and protective factors for depressive symptoms in urban african american adolescents. Youth and Society. 2009;41(1):80–99. [Google Scholar]
- Terwee CB, Bot SDM, de Boer MR, van der Windt DAWM, Knol DL, Dekker J, de Vet HCW. Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology. 2007;60:34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Wang J, Iannotti RJ, Luk JW, Nansel TR. Co-occurrence of victimization from five subtypes of bullying: Physical, verbal, social exclusion, spreading rumors, and cyber. Journal of Pediatric Psychology. 2010:1–10. doi: 10.1093/jpepsy/jsq048. [DOI] [PMC free article] [PubMed] [Google Scholar]