Abstract
The ratio of patients to physicians has long been used as a tool for measuring and planning healthcare resources in Canada. Some current changes in primary care, such as enrolment of patients with physicians, make this ratio easier to calculate, while others, such as changing practice structure, make it more complex to interpret. Based on information gleaned from a review of the literature, we argue that before panel size can be used as an accountability measure for individual physicians or practices in primary care, we must understand its relationship to quality and outcomes at individual and population levels, as well as the contextual factors that affect it.
Abstract
Le ratio patients–médecins a longtemps été utilisé comme outil pour les mesures et la planification des ressources humaines de la santé au Canada. Certains changements actuels dans les soins primaires, tels que l'inscription des patients auprès des médecins, facilitent le calcul de ce ratio, tandis que d'autres, tels que les changements dans la structure de la pratique, les rendent plus complexes à interpréter. Selon l'information recueillie par une revue de la littérature, nous stipulons qu'avant d'utiliser le nombre de patients comme mesure de comptabilisation pour les médecins ou les établissements de soins primaires, il faut comprendre la relation entre cette mesure et la qualité ou les résultats aux niveaux individuel et populationnel, de même que les facteurs contextuels qui l'affectent.
Politicians and healthcare funders in Canada are increasingly recognizing the importance of primary healthcare (PHC)1 to the healthcare system and health. Substantial reforms have taken place in many provinces, resulting in a shift from an uncoordinated system of private, autonomous fee-for-service primary care providers to systems comprising complex and varied delivery models, with payment structures designed to encourage the provision of high-priority services, processes and outcomes of care (Hutchison et al. 2011).
Many factors have driven PHC reform, among them cost control and improved access to primary care services (Hutchison et al. 2011). To achieve these goals, some tools previously used for planning health human resources, such as the ratio of family physicians to population (and the related concept of the number of patients per physician) are now also being used as accountability measures for individual practices and providers. For example, several jurisdictions have established panel size targets for physicians based on the desired increase in accessibility that elements of their reforms (e.g., interprofessional teams) afford (Rosser et al. 2011; Canada's Health Newsweekly 2011). The methods by which these targets were derived have not been made public.
The ratio of patients to providers is easier to calculate than ever in systems where PHC reform has led to a requirement for patient enrolment to individual physicians. But contemporaneous changes to the PC workforce have complicated its interpretation. It appears considerably more difficult to understand patient-to-physician ratios in the context of part-time practice, “focused practice” family physicians (who practise in a single clinical area), rural practices that may be required to provide a larger number of services because of the lack of neighbouring resources or practices that host non-physician PC providers, such as nurse practitioners and physician assistants. Despite these complexities of interpretation, it remains important to establish the “optimal” panel size in PC. Having a defined, appropriately sized patient panel at the provider level improves continuity and thus patient satisfaction with care; defines workload; permits prediction of patient demand; reveals provider issues; and helps improve outcomes (Murray et al. 2007). But “optimal” may be in the eye of the beholder, reflecting diverse priorities, values and incentives. Politicians and decision-makers who wish to ensure that every member of the population has a PC provider might prefer larger panel sizes, while those wishing to improve care delivery might advocate smaller numbers. Healthcare providers are affected by the financial incentives inherent to different funding models: if larger numbers pay more (as under capitation), then providers may seek to enrol more patients. Salaried providers working without productivity inducements might have no incentive to maximize their panel size. Practice context is also important. Family doctors practising in remote areas or mainly seeing high-needs patients might have more difficulty coping with a large panel than those in well-resourced urban centres or with healthier, less resource-dependent patients. In this paper, we explore the complexity of using panel size as an accountability measure in PC. To do so, we examine what is known about the relationship between panel size and healthcare quality measures, describe some of the contextual factors that affect this relationship and critique the methods currently in use to determine panel size. We draw from the academic and grey literature from the Netherlands, United Kingdom, United States and Canada.
“Panel Size” Defined
Panel size is generally defined as “the number of patients (regularly) under the care of a full time equivalent (FTE) PC physician” (Murray et al. 2007). Related to, but distinct from, panel size are “workload” – the amount of time that activities consume or the frequency at which activities take place (Groenewegen and Hutten 1991) – and “productivity” – production of an output per unit of effort. In health systems where all patients are required to register with a particular PC physician, panel size is equivalent to the number of registered patients (adjusted for FTE). Various methods have been proposed to calculate panel size in non-rostered systems. A commonly used method calculates panel size by counting the number of patients who receive the majority of their care from an individual physician over a two-year period (Menec et al. 2000).
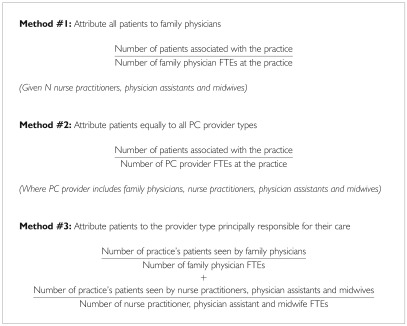
The definition of panel size is more complex in an interprofessional setting. The American literature notes the importance of all PC professionals on a team but uses only three types of “associated PC providers” in panel size calculations: nurse practitioners, physician assistants and midwives. There are three methods of calculating panel size in interprofessional settings (see Box 1). Calculations based on the physician alone (method #1) require additional information about the number and type of associated providers. Method #2 estimates the proportion of patients per primary care provider and implies that all providers contribute equally to managing the panel, while method #3 attributes patients to individual provider types, but does not provide guidance about where to attribute shared patients.
Box 1.
Calculation of panel size in primary care
The Relationship between Panel Size and Quality Measures
Large panel size has been linked with reductions in access by individuals (Stefos et al. 2011) and in other key dimensions of PC service delivery, in particular relational continuity (Murray et al. 2007), comprehensiveness (Butler and Calnan 1987) and patient satisfaction with care (Stefos et al. 2011). Higher panel sizes have also been associated with poorer PC performance process measures in prevention (Dahrouge et al. 2011), health promotion (Hogg et al. 2009) and chronic disease management (Russell et al. 2009), though in a large observational study in the US Veterans Health Administration, effect on measured clinical processes was small and largely insignificant (Stefos et al. 2011). The relationship between panel size and quality measures may not be linear, and there may be thresholds at high or low ratios of patients to physician where quality changes more rapidly. At a population level, larger patient panels presumably reduce the need for a larger PC workforce; however, it is possible that large patient panels may cause reductions in important dimensions, such as practice accessibility, continuity and technical quality of care for individuals, shifting costs to other parts of the healthcare system. There is no information on the effect of different panel sizes on equity – that is, providing the same quality of care to people regardless of who they are or where they live (Health Quality Ontario 2011), a current system priority.
Contextual Influences on Capacity to Care for Patients
Numerous practitioner, practice and contextual factors have been linked with productivity or panel size. Providers newly in practice tend to have smaller panels (VHA 2004). Part-time providers seem to be as or more productive than full-time providers (Fairchild et al. 2001). Providers paid by fee for service produce more services per unit of time than those paid by capitation or salary (Sarma et al. 2010). Watson and colleagues (2005) documented very different workloads and patterns of service provision among physicians in different age cohorts. It is recognized that physicians have an individual “style,” a factor that may lead to differences in caring for patients with the same condition (Geraghty et al. 2007). While it is accepted that clinical teaching has an impact on the productivity of preceptors, the variability of learners and of teaching practices does not permit adjustment of panel size through the use of a simple formula (Mayo-Smith and Frisbee 2003).
At the level of the practice, an increased ratio of clerical and nursing staff (who provide direct assistance in the delivery of PC) to PC providers and a higher number of exam rooms per provider have each been independently associated with increased physician panel size (VHA 2004). On the other hand, panel sizes tend to be smaller in isolated practices (Ricketts et al. 2007) or those caring for patient populations with medical (VHA 2004) or socio-economic (Ricketts et al. 2007) complexity, presumably attributable to the reduced resources in isolated practices and greater time requirements for complex patients.
Many current PC reforms assume that interprofessional teams and the use of non-physician PC providers allow physician panel size to be increased (Wetmore 2009). Indeed, when new team members “substitute” for the physician with some tasks and patients, they may free the physician to work on other activities, potentially allowing for increases in panel size. Much of what these team members do may instead “supplement” the physician's work, performing new tasks that the physician was unable to do when working alone, thereby providing more comprehensive services (Laurant et al. 2005), but not necessarily increases in panel size.
There may also be other methods to improve practice efficiency – group visits (Jaber et al. 2006), advanced access scheduling (Murray et al. 2003), use of electronic health records (Black et al. 2011), collaboration with community resources for chronic disease management and non–visit-based care delivered by telephone or electronically, ensuring that all staff work to their full scope of practice, or improving patient self-management. These approaches could potentially be employed to increase physicians' panel size without compromising quality of care; however, the evidence is indirect at best.
Current Approaches to Calculating Optimal Panel Size
The “workload formula”
The most commonly cited approach to calculate an appropriate panel size for an individual PC physician is to examine availability of physician services (supply) in relation to patient usage of services (demand), an approach known as the “workload formula” (Murray et al. 2007).
Therefore, in order to increase panel size, a provider has to increase the number of available visits by working longer hours or offering shorter appointments (leading to more visits per day), working more days per year or reducing the average number of visits per patient per year. Unfortunately, this workload formula represents a post hoc analysis of past usage patterns and hence does not take into account quality of care or efficient use of resources. For example, past usage may conceal problems with access, resulting in patients seeking care elsewhere (reducing continuity of care). The formula also ignores newer “non–office-visit” approaches to the provision of PC. Thus, while useful to provide an overview of the mechanics of panel size, the workload formula clearly should not be used alone to determine appropriate panel size.
“Target” panel size
Acknowledging that contextual factors affect panel size, the US Veterans Health Administration (VHA) uses a target panel size for individual practices based on average panels across its fully capitated primary care system. Review of the literature and VHA data revealed that two structural factors (number of clerical and nursing support staff assisting directly in PC delivery per PC provider and number of clinic rooms available per provider) and a clinical patient “intensity” score (largely based on medical co-morbidity and insurance status) are linked to panel size (US Department of Health and Human Services 2008). The VHA provides a target panel size for an ideal “reference” practice, and adjusts it for individual practices by up to +/− 10% for varying levels of support staff, +/− 5% for varying numbers of rooms and +/− 10% for variations in patient “intensity.” The VHA approach addresses some practice-level efficiency issues and acknowledges that more intense or complicated patients use more resources, but bases its panel size targets on past and current utilization patterns, without addressing quality measures. Such an approach requires the existence of other mechanisms to monitor and improve quality, which the VHA health system has implemented separately.
Panel size for planning purposes
Refining crude physician-to-population ratios, the US Health Resources and Services Administration (HRSA) uses a calculation based on the ratio of the healthcare needs of the population of a region to the number of health professionals already serving it (expressed as a panel size) in order to designate medically underserved areas. Population healthcare need is derived from data from a variety of sources and includes age, sex, race, employment status, poverty, population-level health indicators (such as low birth weight, standardized mortality rate and infant mortality rate) and population density (which correlates with available services and is related to the rural or urban nature of a place). Poverty contributes the most to healthcare need, followed by population density and unemployment. In very poor areas, the rate of poverty alone can decrease recommended population-to-PC-provider ratio by up to 50% (US Department of Health and Human Services 2007). Though based on existing usage patterns, this method highlights the necessity of understanding the healthcare needs of the population related to both health and social factors to determine a target panel size, even at a community level.
Putting it all together
The relationship between panel size and quality of care seems to be modified by contextual factors. A given panel size may lead to acceptable care in one setting, but may cause problems in another. Current panel size calculation methods are fairly primitive and based on historical utilization patterns, failing to account for quality of service delivery, technical quality of care and innovative service delivery processes. Little consideration is given to the relationship of the PC practice or provider with the in-office team or the surrounding healthcare system. Only the large-scale planning method incorporates important patient and community characteristics that predict the demand for care, but it has little applicability for an individual provider or practice. Unfortunately, published evidence is insufficient at present to produce a “formula” to describe context and its modifying effect on the relationship between panel size and quality.
Conclusion
Policy makers and professional organizations need – and in a sense, deserve – guidance from health service researchers on appropriate panel sizes for primary care practices. As it stands, evidence can inform us only about the myriad factors influencing panel sizes. In a changing and complex PHC environment, this is the best we can do. As ever in healthcare, the context needs to be understood before the prescription is written. How many patients should a family physician have? International policy experience and emerging literature discourage “one size fits all” target panel size for PC physicians and allied providers, their practices and their communities. Unfortunately, methods to adjust or weight panel size based on contextual factors are in their infancy, and the current mix of PC providers and funding models across the country adds complexity to the task. Further large-scale work is required to explore the relationship between panel size and quality-of-care dimensions for individuals and populations, examining community and practice contextual factors and downstream costs.
We should not discard panel size as an accountability measure, but we should not use it without adjustment or to achieve isolated objectives. To do so may risk untoward consequences related to the equity and quality of PC, and costs across the healthcare system. While we wait for more evidence to guide us in answering the question posed in the title of this paper – “How many patients should a family physician have?” – our glib answer is, “as many as possible without leading to poor outcomes.”
Acknowledgements
Funding for this research was provided by Community Health Centres of the Champlain and South East Local Health Integration Networks of Ontario. The views expressed in this report are the views of the authors and do not necessarily reflect those of the Community Health Centres or the Local Health Integration Networks.
NOTES
We acknowledge the important distinction between primary healthcare (PHC) and primary care (PC). This paper principally addresses PC, in which services are provided to individuals (Muldoon et al. 2006). There is no reason PC could not exist within a broader framework of PHC.
Contributor Information
Laura Muldoon, Department of Family Medicine, University of Ottawa, Somerset West Community Health Centre, Ottawa, ON.
Simone Dahrouge, Department of Family Medicine, University of Ottawa, C.T. Lamont Primary Health Care Research Centre, Bruyère Research Institute, Ottawa, ON.
Grant Russell, Monash University Primary Care Research Unit, Melbourne, Australia.
William Hogg, Department of Family Medicine, University of Ottawa, C.T. Lamont Primary Health Care Research Centre, Bruyère Research Institute, Ottawa, ON.
Natalie Ward, C.T. Lamont Primary Health Care Research Centre, Bruyère Research Institute, Department of Sociology and Anthropology, University of Ottawa, Ottawa, ON.
REFERENCES
- Black A.D., Car J., Pagliari C., Anandan C., Cresswell K., Bokun T., et al. 2011. “The Impact of eHealth on the Quality and Safety of Health Care: A Systematic Overview.” PLoS Medicine 8. Retrieved March 6, 2012. <http://www.plosmedicine.org/article/info%3Adoi%2F10.1371%2Fjournal.pmed.1000387>. [DOI] [PMC free article] [PubMed]
- Butler J.R., Calnan M.W. 1987. “List Sizes and Use of Time in General Practice.” British Medical Journal (Clinical Research Edition) 295: 1383–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canada's Health Newsweekly 2011. (July 8). “Some Doctors in PEI Are Being Told to Increase Their Caseloads.” Health Edition 15(27). Retrieved March 6, 2012. <http://www.healthedition.com/article.cfm?articleID=9562>. [Google Scholar]
- Dahrouge S., Hogg W., Russell G., Tuna M., Geneau R., Muldoon L., et al. 2011. “The Impact of Remuneration and Organizational Factors on Prevention Activity in Primary Care: A Cross-Sectional Study.” Canadian Medical Association Journal. Retrieved March 6, 2012. <http://www.cmaj.ca/content/184/2/E135.full>. [DOI] [PMC free article] [PubMed]
- Department of Veterans Affairs & Veterans Health Administration (VHA) 2004. “Guidance on Primary Care Panel Size.” (VHA Directive 2004-031.) Retrieved March 6, 2012. <http://VA-247-07-RP-0210-016.pdf>.
- Fairchild D.G., McLoughlin K.S., Gharib S., Horsky J., Portnow M., Richter J., et al. 2001. “Productivity, Quality, and Patient Satisfaction: Comparison of Part-Time and Full-Time Primary Care Physicians.” Journal of General Internal Medicine 16: 663–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geraghty E.M., Franks P., Kravitz R.L. 2007. “Primary Care Visit Length, Quality, and Satisfaction for Standardized Patients with Depression.” Journal of General Internal Medicine 22: 1641–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groenewegen P.P., Hutten J.B.F. 1991. “Workload and Job Satisfaction among General Practitioners: A Review of the Literature.” Social Science & Medicine 32(2): 1111–19 [DOI] [PubMed] [Google Scholar]
- Health Quality Ontario 2011. Quality Monitor: Report on Ontario's Health System. Retrieved March 6, 2012. <http://www.ohqc.ca/pdfs/2011_report_-_english.pdf>.
- Hogg W., Dahrouge S., Russell D., Tuna M., Geneau R., Muldoon L., et al. 2009. “Health Promotion Activity in Primary Care: Performance of Models and Associated Factors.” Open Medicine 3: 165–73 [PMC free article] [PubMed] [Google Scholar]
- Hutchison B., Levesque J.F., Strumpf E., Coyle N. 2011. “Primary Health Care in Canada: Systems in Motion.” Milbank Quarterly 89: 256–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaber R., Braksmajer A., Trilling J.S. 2006. “Group Visits: A Qualitative Review of Current Research.” Journal of the American Board of Family Medicine 19: 276–90 [DOI] [PubMed] [Google Scholar]
- Laurant M., Reeves D., Hermens R., Braspenning J., Grol R., Sibbald B. 2005. (April 18). “Substitution of Doctors by Nurses in Primary Care.” Cochrane Database of Systematic Reviews 2: CD001271. Retrieved March 6, 2012. <http://www.ncbi.nlm.nih.gov/pubmed/15846614>. [DOI] [PubMed]
- Mayo-Smith M., Frisbee K. 2003. Advisory Group on VHA Physician Productivity and Staffing. Report of the Primary Care Subcommittee. Washington, DC: US Department of Veterans Affairs [Google Scholar]
- Menec V., Black C., Roos N., Bogdanovic B., Reid R. 2000. Defining Practice Populations for Primary Care: Methods and Issues. Winnipeg: Manitoba Centre for Health Policy and Evaluation, University of Manitoba [Google Scholar]
- Muldoon L., Hogg W., Levitt M. 2006. “Primary Care (PC) and Primary Health Care (PHC): What Is the Difference?” Canadian Journal of Public Health 97(5): 409–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray M., Bodenheimer T., Rittenhouse D., Grumbach K. 2003. “Improving Timely Access to Primary Care: Case Studies of the Advanced Access Model.” Journal of the American Medical Association 289: 1042–46 [DOI] [PubMed] [Google Scholar]
- Murray M., Davies M., Boushon B. 2007. “Panel Size: How Many Patients Can One Doctor Manage?” Family Practice Management 14: 44–51 Retrieved March 6, 2012. <http://www.aafp.org/fpm/2007/0400/p44.html>. [PubMed] [Google Scholar]
- Ricketts T.C., Goldsmith L.J., Holmes G.M., Randolph R.M., Lee R., Taylor D.H., et al. 2007. “Designating Places and Populations as Medically Underserved: A Proposal for a New Approach.” Journal of Health Care for the Poor & Underserved 18: 567–89 [DOI] [PubMed] [Google Scholar]
- Rosser W.W., Colwill J.M., Kasperski J., Wilson L. 2011. “Progress of Ontario's Family Health Team Model: A Patient-Centered Medical Home.” Annals of Family Medicine 9: 165–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell G., Dahrouge S., Hogg W., Geneau R., Muldoon L., Tuna M. 2009. “Delivering Chronic Disease Management: Results from the Comparison of Models of Primary Health Care in Ontario Study.” Annals of Family Medicine 7: 309–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarma S., Devlin R.A., Hogg W. 2010. “Physicians' Production of Primary Care in Ontario, Canada.” Health Economics 19: 14–30 [DOI] [PubMed] [Google Scholar]
- Stefos T., Burgess J., Mayo-Smith M., Frisbee K., Harvey H., Lehner L., Lo S., Moran E. 2011. “The Effect of Physician Panel Size on Health Care Outcomes.” Health Services Management Research 24: 96–105 [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services 2007. Health Resources and Services Administration. Bureau of Primary Health Care Section 330 Grantees – Uniform Data System. Region 1 – Rollup Report. [Google Scholar]
- US Department of Health and Human Services 2008. “Designation of Medically Underserved Populations and Health Professional Shortage Areas”: in Federal Register 73(41): 11232–52 Retrieved March 8, 2012. <http://www.gpo.gov/fdsys/pkg/FR-2008-02-29/pdf/E8-3643.pdf>. [Google Scholar]
- Watson D.E., Reid R., Roos N., Heppner P. 2005. “Growing Old Together: The Influence of Population and Workforce Aging on Supply and Use of Family Physicians.” Canadian Journal of Aging 24 (Suppl. 1): 37–45 [DOI] [PubMed] [Google Scholar]
- Wetmore S. 2009. More on Family Health Teams. Toronto: Ontario College of Family Physicians; Retrieved March 8, 2012. <http://www.ocfp.on.ca/docs/communications/april-08-2009.pdf?Status=Master#8b3447b0-755a-489a-9826-6e80760a5b84>. [Google Scholar]