Abstract
Alternate-level-of-care (ALC) days represent hospital beds that are taken up by patients who would more appropriately be cared for in other settings. ALC days have been found to be costly and may result in worse functional outcomes, reduced motor skills and longer lengths of stay in rehabilitation. This study examines the factors that are associated with acute care ALC days among patients with acquired brain injury (ABI). We used the Discharge Abstract Database to identify patients with ABI using International Classification of Disease-10 codes. From fiscal years 2007/08 to 2009/10, 17.5% of patients with traumatic and 14% of patients with non-traumatic brain injury had at least one ALC day. Significant predictors include having a psychiatric co-morbidity, increasing age and length of stay in acute care. These findings can inform planning for care of people with ABI in a publicly funded healthcare system.
Abstract
Les niveaux de soins alternatifs (NSA) correspondent aux lits d'hôpital qui sont occupés par des patients qui recevraient des soins plus appropriés dans un autre type d'établissement. Les jours NSA peuvent être coûteux et donner lieu à de moindres résultats sur le plan fonctionnel, à une motricité réduite et à de plus longs séjours pour la réadaptation. Cette étude examine les facteurs associés aux jours NSA pour les soins de courte durée chez les patients qui présentent une lésion cérébrale acquise (LCA). À l'aide de la Base de données sur les congés des patients, nous avons répertorié les patients qui ont présenté une LCA, en fonction des codes de la Classification internationale des maladies-10. Pour les exercices financiers de 2007/08 à 2009/10, 17,5 pour cent des patients qui ont présenté une lésion cérébrale traumatique et 14 pour cent des patients qui ont souffert d'une lésion cérébrale non traumatique ont présenté au moins un jour pour un NSA. Les facteurs de prédiction significatifs comprennent la présence d'une comorbidité psychiatrique, un age avancé et la durée du séjour dans un établissement de soins de courte durée. Ces résultats peuvent servir à renseigner la planification des soins pour les personnes souffrant d'une LCA dans un système de santé financé par les deniers publics.
Delays in discharge from the healthcare system are designated as alternate-level-of-care (ALC) days. In Ontario, the Ministry of Health and Long-Term Care defines an ALC day as follows:
When a patient is occupying a bed in a hospital and does not require the intensity of resources/services provided in this care setting… the patient must be designated Alternate Level of Care (ALC) at that time by the physician or her/his delegate. (MOHLTC 2008)
The cost of delaying discharge is high for both the healthcare system and for patients. In a national audit, Worthington and Oldham (2006) estimated that delays in discharges from hospitals cost the UK healthcare system over £1 million per day. Other studies have found that delays to rehabilitation negatively affect patients' functional outcomes, motor skills and length of stay in rehabilitation (Kunik et al. 2006). These concerns, in addition to increasingly tight healthcare budgets, have raised delayed discharges as a high-priority policy issue in Canada.
Studies examining the factors for delayed discharge have identified lack of healthcare or social care resources (or both); clinicians' lack of knowledge of patient conditions, and lack of communication between doctors (Hammond et al. 2009); and patients who are older (DeCoster et al. 1997; Flintoft et al. 1998; CIHI 2009), have a nervous system diagnosis (DeCoster et al. 1997), require diagnostic testing, have multiple co-morbidities and live at a distance from hospital (Flintoft et al. 1998). A brief report by the Canadian Institute for Health Information (2011) on ALC in Canada found that ALC patients were more likely to begin their hospitalization in the emergency department and were more than twice as likely to have co-morbid conditions compared to non-ALC patients. Also, the most common reasons for ALC admission were waiting for palliative care (33%), for admission to another adequate facility (27%) and for physiotherapy (11%).
Of equal concern are acquired brain injuries (ABIs), which are the leading cause of death and disability worldwide (Greenwald et al. 2003; WHO 2006). The Toronto Acquired Brain Injury Network (2012) has defined ABI as damage to the brain that occurs no fewer than seven days after birth and can occur due to traumatic and non-traumatic causes. Traumatic brain injury (TBI) is more common than breast cancer, HIV/AIDS, spinal cord injury and multiple sclerosis combined (Colantonio et al. in press). While fewer studies have investigated non-traumatic brain injury (nTBI) as a group, studies demonstrate that individuals with nTBI experience consequences similar to those found in patients with brain injury due to trauma (Cullen et al. 2008). The physical, cognitive, psycho-social and long-term impacts of ABI are also well documented (Tagliaferri et al. 2006; WHO 2006).
Given the importance of delayed discharge and the impact of ABI, it is crucial to examine ALC days among ABI patients and the impact of delayed discharge on them. The long-term impact of ABI, and the need for rehabilitation and complex support following discharge from acute care, are known to result in longer lengths of stay (LOS) and ALC days in the ABI population. A report by the GTA Rehabilitation Network (2004) stated that 10% of patients waiting for rehabilitation in ALC were ABI patients, making them one of the most prevalent groups. Moreover, a study by Colantonio and colleagues (2010) found that the availability of and access to appropriate services for persons with ABI is a growing concern. Identified gaps include a lack of facilities that address age-appropriate needs of persons with ABI, lack of training about the cognitive and behavioural needs of these patients, and lack of resources for and poor coordination of services.
Using a population-based approach, this study describes the number of ALC days in the ABI population and identifies the predictors of ALC days among these patients. The study leverages the administrative collection of healthcare data in all hospitals in Ontario, which informs program planning and policy for patients with ABI.
Methods
Data sources
Ontario hospital administrative data, collected for the purposes of payment and funding, were used for this study. These data were provided by the Ontario Ministry of Health and Long-Term Care (MOHLTC) from CIHI holdings, and specific variables were requested from the Discharge Abstract Database (DAD), which documents all publicly funded acute care hospitalizations in Ontario. We examined three fiscal years of discharges – April 1, 2007 to March 31, 2010 – among those that have met the ABI case definition. A large chart re-abstraction study using the DAD showed perfect or near-perfect agreement for non-clinical variables and moderate to substantial agreement for the most responsible diagnoses, and good specificity of TBI codes (Juurlink et al. 2006).
Case definition
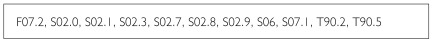
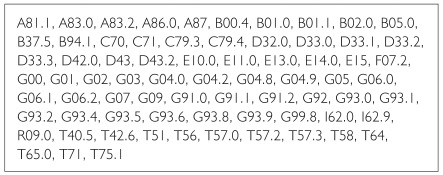
ABI cases were identified using International Classification of Diseases 10th Revision (ICD-10) codes and included both TBI and nTBI causes in all diagnosis positions. The definition used for TBI was based on a recently published conservative definition derived from a literature review and stakeholder consultation in the Canadian context (Chen and Colantonio 2011). nTBI included anoxia, vascular insults (excluding stroke), brain tumours, encephalitis, metabolic encephalopathies, brain infections and toxic effects. See Figures 1 and 2 for the ICD-10 codes used to define TBI and nTBI.
FIGURE 1.
ICD-10 codes used to define traumatic brain injury (TBI)
FIGURE 2.
ICD-10 codes used to define non-traumatic brain injury (nTBI)
All hospital separations were grouped into episodes of care using a 24-hour rule (i.e., admissions that occurred within 24 hours of a previous discharge were considered part of the same episode of care). Only the last admission in the episode was considered. Patients 18 years of age and younger were excluded owing to a very low frequency of ALC patients in this population.
Predictor variables of interest
Our study primarily focused on demographic and clinical characteristics of patients in relation to ALC. Demographic information collected included patient age and gender. These variables in the DAD have been shown to be very accurate and reliable in re-abstraction studies (Juurlink et al. 2006). Age was categorized using the following groupings: 19–54, 55–64, 65–74, 75–84 and 85+. The fiscal year of admission was also considered to examine time trends in ALC propensity.
Clinical characteristics included the most responsible diagnosis (MRDx, the diagnosis most responsible for the patient's stay in a facility), measures of severity of condition (e.g., LOS, special-care days) and co-morbidities. The most responsible diagnosis was dichotomized based on whether the brain injury code was in the MRDx position. Length of stay in acute care was defined as the number of days between admission and discharge from acute care, excluding the number of ALC days (calculated as LOS – ALC days). Special-care days were defined as the cumulative number of days spent in all intensive care units (e.g., medical intensive nursing care units, neonatal intensive care units). Finally, co-morbidities were analyzed using the Charlson Co-morbidity Index. This index, developed in the 1980s, is widely accepted as a useful tool for measuring co-morbidity disease status and has shown a consistent correlation to in-hospital mortality (Sundararajan et al. 2004). Psychiatric co-morbidities, defined as any mental health or behavioural disorder diagnosis (ICD-10 F chapter heading) anywhere in the abstract, were also considered in this study because they have been identified as among the most common co-morbidities for ABI and have an impact on outcomes (Colantonio et al. 2011c). Thus, psychiatric co-morbidities were considered in any diagnosis position.
Treatment location was considered in the context of whether patients were treated in the same region or local health integration network (LHIN) where they resided. This geographic measure gives some indication of whether geography presents any barriers to treatment. Finally, the cause of injury was considered and dichotomized for patients with a TBI into those with an external cause of injury of motor vehicle collision (MVC) and those who were not in a MVC. Previous studies in Ontario have examined MVC as a proxy for the presence of additional resources through supplemental insurance for this type of injury, which was found to be associated with more discharges to home (Kim et al. 2006).
Outcome variable
The outcome variable in this study is the occurrence of a hospital admission with at least one ALC day. The patient is classified as ALC when the physician or designated other indicates that the patient no longer requires acute care or is awaiting placement in a complex continuing care unit, home for the aged, nursing home, free-standing rehabilitation facility, other extended care institution or home care program.
Analyses
Descriptive statistics such as the number, average and standard deviation of ALC days per year are presented here. A multivariable logistic regression analysis was performed to identify predictors of ALC days. To control for patients with multiple hospitalizations, generalized estimating equations (GEE) were employed with an exchangeable correlation structure and the log link. Because the two ABI subpopulations are different, we analyzed TBI and nTBI separately. All variables were forced into the model regardless of statistical significance. Multicollinearity of the independent variables was tested using a variation inflation factor.
Encrypted data were received on a compact disc in fixed-width text format. Data were imported into SAS format and stored on a secure computer system at the Toronto Rehabilitation Institute. This study was approved by the Toronto Rehabilitation Institute Research Ethics Board. All analyses were conducted in SAS v.9.1.
Results
The total number of ALC days increased among TBI and nTBI patients from fiscal years 2007/08 to 2009/10 from 15,606 to 22,637 days and 39,918 to 48,267 days, respectively. In 2009, TBI and nTBI patients contributed a total of 70,904 ALC days. Overall, nTBI patients had more ALC days (48,267 days vs. 22,637 days), and on average, TBI patients had longer ALC stays (23.9 days vs. 19.6 days) (Table 1).
TABLE 1.
Total and average number of ALC days for TBI and nTBI by fiscal year, 2007/08–2009/10
| Fiscal Year | Number of ALC Episodes | Total ALC Days | Mean (Standard Deviation) of ALC Stay (Days)a | Median ALC Stay (Days)a |
|---|---|---|---|---|
| TBI | ||||
| 2007 | 770 | 15,606 | 20.3 (30.5) | 11 |
| 2008 | 836 | 20,230 | 24.2 (40.9) | 11 |
| 2009 | 949 | 22,637 | 23.9 (40.6) | 10 |
| nTBI | ||||
| 2007 | 1,937 | 39,918 | 20.6 (35.7) | 11 |
| 2008 | 2,156 | 46,701 | 21.7 (36.6) | 10 |
| 2009 | 2,463 | 48,267 | 19.6 (40.5) | 8 |
Note: a Includes only patients with one or more ALC day
Table 2 presents the characteristics of TBI patients with ALC days and multivariate analysis of factors on the propensity of ALC days. Overall, 17.5% of TBI patients had at least one ALC day during their acute care stay. The majority had a TBI diagnosis in the MRDx field (61.4%), were aged 65 years and older (66.8%) and were male (58%). Examination of the clinical characteristics revealed that the majority of patients (53.7%) stayed in acute care for 12 days or more (excluding ALC days); 23.1% had a Charlson Co-morbidity Index score of 2 or more; 31.4% had a psychiatric diagnosis; and 37.7% had at least one special-care day. Approximately one-fifth of patients received treatment outside their LHIN of residence, and 15.3% were involved in a MVC (percentages are not shown in the table).
TABLE 2.
Characteristics of TBI patients with ALC days and multivariate analysis of factors on propensity of ALC days, Ontario, 2007/08–2009/10 (total number of hospital episodes = 14,586)
| Characteristics | Any ALC Days | ||||
|---|---|---|---|---|---|
| ALC | Odds Ratio | 95% Confidence Interval | |||
| N | % | ||||
| Overall | 2,555 | 17.5 | - | - | |
| Age | |||||
| 19–54 | 580 | 10.3 | 1.00 | - | - |
| 55–64 | 267 | 14.9 | 1.45*** | 1.22 | 1.71 |
| 65–74 | 407 | 19.7 | 2.05*** | 1.75 | 2.39 |
| 75–84 | 690 | 22.6 | 2.50*** | 2.17 | 2.87 |
| 85+ | 611 | 29.7 | 3.67*** | 3.17 | 4.26 |
| Sex | |||||
| Male | 1,481 | 15.8 | 1.00 | - | - |
| Female | 1,074 | 20.7 | 1.13** | 1.03 | 1.25 |
| Charlson Co-morbidity Indexa | |||||
| 0–1 (low) | 1,965 | 15.6 | 1.09*** | 1.05 | 1.14 |
| 2–3 | 446 | 28.7 | |||
| 4+ (high) | 144 | 32.2 | |||
| Local Health Integration Network (LHIN) Concordance | |||||
| Yes | 2,013 | 18.1 | 0.97 | 0.86 | 1.09 |
| No | 542 | 15.7 | |||
| Special-Care Days (days)a | |||||
| None | 1,593 | 15.8 | 0.99 | 0.98 | 1.00 |
| 1–2 | 179 | 10.4 | |||
| 3–5 | 234 | 19.8 | |||
| 6–11 | 214 | 27.5 | |||
| 12+ | 335 | 40.1 | |||
| Psychiatric Co-morbidity | |||||
| Yes | 801 | 26.2 | 1.73*** | 1.56 | 1.92 |
| No | 1,754 | 15.2 | |||
| Length of Stay (excluding ALC days)a | |||||
| <1 | - | - | 1.04*** | 1.04 | 1.05 |
| 1–2 | 132 | 4.9 | |||
| 3–5 | 334 | 7.9 | |||
| 6–11 | 717 | 18.7 | |||
| 12+ | 1,372 | 36.2 | |||
| TBI Diagnosis in MRDx | |||||
| Yes | 1,569 | 15.4 | 0.72*** | 0.65 | 0.80 |
| No | 986 | 22.3 | |||
| Fiscal Year of Admission | |||||
| 2007 | 770 | 16.8 | 1.00 | - | - |
| 2008 | 836 | 17.6 | 1.04 | 0.93 | 1.17 |
| 2009 | 949 | 18.1 | 1.08 | 0.97 | 1.22 |
| Motor Vehicle Collision | |||||
| Yes | 392 | 17.7 | 1.35*** | 1.17 | 1.56 |
| No | 2,163 | 17.5 | |||
Notes: a Odds ratio represents an increase in relative odds per 1 unit change in the variable
p <.05;
p <.01;
p <.001
Multivariate analyses showed that the odds of having an ALC day increased significantly with increasing age. The odds of having an ALC day also increased among females (OR=1.13), patients with a psychiatric co-morbidity (OR=1.73) and those involved in a MVC (OR=1.35). Each increase in the Charlson Co-morbidity Index category increased the odds of having an ALC day by 9%, and each increase in the length of stay in acute care (excluding ALC days) increased the odds by 4%.
Table 3 presents the characteristics of nTBI patients with ALC days and multivariate analysis of factors on the propensity of ALC days. Among nTBI patients with any ALC days, 38.5% had a nTBI diagnosis in the MRDx field, and the majority were aged 65 years and older (64.4%) and male (51.2%). Clinical characteristics revealed that the majority of patients stayed in acute care for 12 days or more (excluding ALC days) (52.8%) and had a Charlson Co-morbidity Index score of 2 or more (69%); 23.3% had psychiatric co-morbidities, and 26.8% had at least one special-care day. Approximately 15% of patients received their treatment outside their LHIN of residence (percentages are not shown in the table).
TABLE 3.
Characteristics of nTBI patients with ALC days and multivariate analysis of factors on propensity of ALC days, Ontario, 2007/08–2009/10 (total number of hospital episodes = 46,893)
| Characteristics | Any ALC Days | |||||
|---|---|---|---|---|---|---|
| ALC | Odds Ratio | 95% Confidence Interval | ||||
| N | % | |||||
| Overall | 6,556 | 14.0 | - | - | ||
| Age | ||||||
| 19–54 | 1,152 | 7.4 | 1.00 | - | - | |
| 55–64 | 1,184 | 12.3 | 1.59*** | 1.45 | 1.74 | |
| 65–74 | 1,520 | 15.7 | 2.08*** | 1.90 | 2.27 | |
| 75–84 | 1,893 | 21.8 | 3.12*** | 2.87 | 3.40 | |
| 85+ | 807 | 24.5 | 3.77*** | 3.40 | 4.18 | |
| Sex | ||||||
| Male | 3,356 | 14.1 | 1.00 | - | - | |
| Female | 3,200 | 13.9 | 1.02 | 0.96 | 1.08 | |
| Charlson Co-morbidity Indexa | ||||||
| 0–1 (low) | 2,031 | 10.3 | 1.08*** | 1.07 | 1.10 | |
| 2–3 | 1,873 | 16.3 | ||||
| 4+ (high) | 2,652 | 17.0 | ||||
| Local Health Integration Network (LHIN) Concordance | ||||||
| Yes | 5,552 | 14.8 | 1.22*** | 1.13 | 1.32 | |
| No | 1,004 | 10.8 | ||||
| Special-Care Days (days)a | ||||||
| None | 4,797 | 14.8 | 0.99** | 0.99 | 1.00 | |
| 1–2 | 360 | 5.5 | ||||
| 3–5 | 361 | 10.5 | ||||
| 6–11 | 423 | 17.8 | ||||
| 12+ | 615 | 28.1 | ||||
| Psychiatric Co-morbidity | ||||||
| Yes | 1,525 | 20.5 | 1.85*** | 1.73 | 1.99 | |
| No | 5,031 | 12.8 | ||||
| Length of Stay (excluding ALC days)a | ||||||
| <1 | <5 | - | 1.02*** | 1.02 | 1.02 | |
| 1–2 | 406 | 6.2 | ||||
| 3–5 | 855 | 6.8 | ||||
| 6–11 | 1,829 | 13.6 | ||||
| 12+ | 3,464 | 24.2 | ||||
| nTBI Diagnosis in MRDx | ||||||
| Yes | 2,527 | 12.8 | 1.12*** | 1.06 | 1.19 | |
| No | 4,029 | 14.8 | ||||
| Fiscal Year of Admission | ||||||
| 2007 | 1,937 | 12.8 | 1.00 | - | - | |
| 2008 | 2,156 | 14.0 | 1.07* | 1.00 | 1.15 | |
| 2009 | 2,463 | 15.1 | 1.19*** | 1.12 | 1.28 | |
Notes: a Odds ratio represents an increase in relative odds per 1 unit change in the variable
p <.05;
p <.01;
p <.001
Multivariate analyses showed that the odds of having an ALC day increased significantly with increasing age. The odds of having an ALC day also increased among patients with psychiatric co-morbidities (OR=1.85), those who received treatment within their LHIN of residence (OR=1.22) and those with a nTBI diagnosis in the MRDx field (OR=1.12). Each increase in Charlson Co-morbidity category increased the odds of having an ALC day by 8%, and each increase in the length of stay in acute care outside of ALC days increased the odds by 2%. Conversely, each increase in the number of special-care days decreased the odds of having an ALC day by 1%. Finally, the odds of having an ALC day among nTBI patients in 2009 increased by 19% compared to patients in 2007.
Discussion
This paper is the first to our knowledge that analyzes predictors of ALC days in the ABI population. From fiscal years 2007/08 to 2009/10, the number of ABI episodes and total number of ALC days increased substantially. The average length of ALC stays among TBI patients increased from 20.3 days in 2007 to 23.9 days in 2009 and remained relatively stable among nTBI patients, from 20.6 days to 19.6 days. Significant predictors for ALC days in this population include increasing age, Charlson Co-morbidity Index, length of stay and presence of psychiatric co-morbidity.
Findings from this study demonstrate that predictors of delayed discharge among the ABI population are similar to those found in other patient populations (e.g., increasing age, presence of co-morbidities). In the ABI population, compared to patients aged 19–54 years, the odds of having an ALC day increased by 105% among TBI patients aged 65–74 years of age and by 267% among TBI patients aged 85 years and older. Similar findings were observed among nTBI patients. While the older adult population (≥65 years) comprises 13% of the Canadian population, they represent 60% of the hospital days (MOHLTC 2010). In addition, it is projected that the older adult population will double in the next 20 years (MOHLTC 2010). The highest rates of TBI and nTBI are among older adults (≥65 years), and they increase with increasing age (Colantonio et al. 2011a). As such, it is important that policy makers prepare for and address the anticipated increase in the number of ALC days by older ABI patients in the future.
Having a psychiatric co-morbidity also increased the odds of having an ALC day among TBI and nTBI patients by 73% and 85%, respectively. Similarly, increasing Charlson Co-morbidity Index category increased the odds of having an ALC day by 9% in the TBI population and by 8% in the nTBI population. This finding is particularly important because studies have demonstrated that co-morbidities are common in the ABI population and play a major role in the outcome of these patients. For example, in a study by Bombardier and colleagues (2010), 53.1% of their participants met criteria for major depressive disorder at least once in their follow-up period. Similarly, Colantonio and colleagues (2011c) found that the ABI in-patient rehabilitation population had a high number of co-morbidities, with the top three involving the circulatory system (38.8%), nervous system (36.1%) and mental health (30.5%). Studies examining the outcome of patients with co-morbidities found that older adults with a major depression in the first months after TBI had persisting adverse effects on outcome (Rapoport et al. 2006). Across the lifespan, major depression is also a common complication of TBI and is associated with poorer functional outcome and lower social integration (Rogers and Read 2007). Thus, given the prevalence and impact of co-morbidities among patients with ABI, and the significantly increased odds of having an ALC day with the presence of psychiatric co-morbidities and increasing co-morbidity scores, strategies to target this high-risk group are encouraged. A possible way to address this issue could be to expand services within available facilities to include mental health services as well as physical care.
Geography was also associated with the odds of having an ALC day among ABI patients. We found that the odds of having an ALC day increased by 22% among nTBI patients receiving care within their LHIN of residence. This finding is important because recent data demonstrate that LHIN concordance in acute care varies across Ontario, with concordance in Erie St. Clair LHIN and North West LHIN almost 100% and in Toronto Central, 38% (Colantonio et al. 2011b). This finding suggests that planning of services and strategies to reduce ALC should be at the local level and that the capacity of the LHINs to provide facilities required by the ABI population should be evaluated.
Finally, our finding that having a nTBI as the main diagnosis increased the odds of having an ALC day is in line with DeCoster and colleagues' (1997) finding that having a nervous system diagnosis is associated with delayed discharge and CIHI's (2009) finding that a nervous system diagnosis disproportionately contributes to ALC days. Having a main diagnosis of brain injury indicates that the brain injury requires the greatest amount of acute care and speaks to the complexity of this condition and the need for community resources on discharge from acute care. Interestingly, in this study, having a TBI as the main diagnosis decreased the odds of having an ALC day by 28%. This finding suggests that TBI and nTBI patients are distinct populations, and certain heterogeneity exists within ABI subtypes as well. Further, co-morbidities as well as complications associated with TBI might be driving longer lengths of stay and delayed discharge. Therefore, policy makers should not view ABI patients as a homogeneous group when aiming to reduce ALC days in this population.
A limitation of this study is that it relies on administrative data for estimates on ALC days. In a re-abstraction study, CIHI (2010) found that ALC days were 100% reliable, but questions remain on the consistency of ALC designation. The same findings also show that there is wide variation of ALC days reported among hospitals. While many acute care patients would be expected to have ALC days based on their discharge destination to in-patient rehabilitation or long-term care, many are not designated with ALC days in the DAD. Therefore, it is likely that the ALC measure underestimates actual ALC days experienced by all patients and, in the case of this paper, patients with ABI. Efforts to increase the quality of ALC data will allow better trend analysis in the future. Also, we did not directly compare our findings to data on Ontario ALC days and thus could not determine the proportion of total Ontario ALC days in the DAD sample that comprises patients with an ABI.
Nonetheless, data from the DAD are comprehensive and include all acute care hospitalizations in Ontario (CIHI 2010). Moreover, the data are rich in the variables collected and are universal. Given that Ontario is the most populous province, representing approximately 40% of the Canadian population, trends in Ontario can inform other provinces in Canada (Statistics Canada 2010).
This study presents a compelling argument for attention to costly ALC days among ABI patients. From fiscal years 2007/08 to 2009/10, the total number of ALC days among ABI patients in Ontario increased substantially by 7,031 days among TBI patients and by 8,349 days among nTBI patients. The increase of 15,380 ALC days among ABI patients alone calls for attention to this population, which has been identified as one of the most prevalent groups in ALC awaiting rehabilitation (GTA Rehabilitation Network 2004). This elevated number of ALC days could translate into increased revenue for other services, such as community services. More recently, the Ministry of Health and Long-Term Care began to provide the LHINs with resources and investments to support patients' transition from hospitals to appropriate community services and home care. This initiative was specifically designed to ensure that patients receive the appropriate care in the most appropriate setting (MOHLTC 2011). Thus, we suggest that the amount and type of services offered by home care be expanded to address patients capable of living independently at home while awaiting a bed in a facility.
Future research should identify the specific barriers in accessing services following discharge from acute care in order to inform policies aiming to reduce ALC days. Moreover, research into the unique and common predictors of having an ALC day among different patient populations may assist in providing a more targeted strategy to reduce the number of ALC days overall. Finally, in a recent report on addressing ALC in the aging population, Dr. David Walker, the Provincial ALC Lead in Ontario, recommended that the primary care system be improved to identify patients in the community who are at risk of frailty and deterioration. This will reduce “the likelihood of a crisis situation that may require an ED visit and/or subsequent hospital admission” (Walker 2011: 13). Thus, studies should be conducted to identify high-risk groups. Dr. Walker's recommendation can also be expanded to the general patient population. With the rising costs of healthcare, research into strategies to reduce the number and cost of ALC days, in both the ABI and general patient population, is crucial.
Acknowledgements
Funding for this study was obtained from the Ontario Neurotrauma Foundation, The Toronto Rehabilitation Institute, and a grant from the Ministry of Health and Long-Term Care to Toronto Rehabilitation Institute. We would like to thank the Ministry of Health and Long-Term Care for providing us with data, and the Canadian Institute for Health Information for advice on data quality and codes. We thank Sandra Sokoloff for administrative support.
Contributor Information
Chen Amy, Toronto Rehabilitation Institute, UHN, Toronto, ON.
Brandon Zagorski, University of Toronto, Faculty of Medicine, Health Policy Management and Evaluation, Toronto, ON.
Vincy Chan, University of Toronto, Faculty of Medicine, Public Health Sciences, Toronto, ON.
Daria Parsons, Toronto Rehabilitation Institute, UHN, Toronto, ON.
Rika Vander Laan, Toronto Rehabilitation Institute, UHN, Toronto, ON.
Angela Colantonio, Saunderson Family Chair in Acquired Brain Injury Research, Toronto Rehabilitation Institute – UHN, Professor, Department of Occupational Science & Occupational Therapy, Faculty of Medicine, University of Toronto, Toronto, ON.
REFERENCES
- Bombardier C.H., Fann J.R., Tempkin N.R., Esselman P.C., Barber J., Dikmen S.S. 2010. “Rates of Major Depressive Disorder and Clinical Outcomes Following Traumatic Brain Injury.” Journal of the American Medical Association 303(19): 1938–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brain Injury Association of America 2004. “A Comparison of Traumatic Brain Injury and Leading Injuries or Diseases.” Retrieved February 27, 2012. <http://www.braininjurygeorgia.org/articles/tbi_incidence.pdf>.
- Canadian Institute for Health Information (CIHI) 2009. “Alternate Level of Care in Canada.” Retrieved February 27, 2012. <http://secure.cihi.ca/cihiweb/products/ALC_AIB_FINAL.pdf>.
- Canadian Institute for Health Information (CIHI) 2010. Discharge Abstract Database. Retrieved February 27, 2012. <http://www.cihi.ca/cihi-ext-portal/internet/en/document/types+of+care/hospital+care/rehabilitation/services_dad>.
- Canadian Institute for Health Information (CIHI) 2011. “Alternate Level of Care in Atlantic Canada, 2009–2010.” Retrieved February 27, 2012. <http://secure.cihi.ca/cihiweb/products/ALC_AIB_FINAL.pdf>.
- Cancer Care Ontario 2009. “Alternate Level of Care.” Retrieved February 27, 2012. <http://www.cancercare.on.ca/cms/One.aspx?portalId=1377&pageId=43214>.
- Chen A.Y., Colantonio A. 2011. “Defining Neurotrauma in Administrative Data Using the International Classification of Diseases Tenth Revision.” Emerging Themes in Epidemiology 8: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colantonio A., Chase S., Ratcliff G., Vernich L., Al-Sukhni E., Yasseen B. In press. Preventive Health Practices and Behavioral Risk Factors in Women Surviving Traumatic Brain Injury. Health Care for Women International; [DOI] [PubMed] [Google Scholar]
- Colantonio A., Howse D., Kirsh B., Chiu T., Zulla R., Levy C. 2010. “Living Environments for People with Moderate to Severe Acquired Brain Injury.” Healthcare Policy 5(4): e120–e138 [PMC free article] [PubMed] [Google Scholar]
- Colantonio A., Chan V., Chen A., Zagorski B., Parsons D., Vander Laan R. 2011a. “ABI Dataset Project – Older Adult Report.” Report submitted September 2011 to Ontario Neurotrauma Foundation. [Google Scholar]
- Colantonio A., Chan V., Zagorski B., Parsons D., Vander Laan R. 2011b. “Ontario ABI Dataset Project – LHIN Fact Sheet.” Report submitted December 2011 to Ontario Neurotrauma Foundation. [Google Scholar]
- Colantonio A., Gerber G., Bayley M., Deber R., Yin J., Kim H. 2011c. “Differential Profiles for Patients with Traumatic and Non-Traumatic Brain Injury.” Journal of Rehabilitation Medicine 43: 311–15 [DOI] [PubMed] [Google Scholar]
- Cullen N.K., Park Y., Bayley M.T. 2008. “Functional Recovery Following Traumatic vs. Non-Traumatic Brain Injury: A Case-Controlled Study.” Brain Injury 22(13–14): 1013–20 [DOI] [PubMed] [Google Scholar]
- DeCoster C., Roos N.P., Carriere K.C., Peterson S. 1997. “Inappropriate Hospital Use by Patients Receiving Care for Medical Conditions: Targeting Utilization Review.” Canadian Medical Association Journal 157(7): 889–96 [PMC free article] [PubMed] [Google Scholar]
- Flintoft V.F., Williams J.I., Williams R.C., Basinski A.S., Blackstien-Hirsch P., Naylor C.D. 1998. “The Need for Acute, Subacute and Nonacute Care at 105 General Hospital Sites in Ontario. Joint Policy and Planning Committee Non-Acute Hospitalization Project Working Group.” Canadian Medical Association Journal 158(10): 1289–96 [PMC free article] [PubMed] [Google Scholar]
- Greater Toronto Area (GTA) Rehabilitation Network 2004. Analysis of Alternate Level of Care (ALC) Snapshots: Patients Awaiting Rehabilitation in ALC and Inpatient Rehabilitation Capacity. Retrieved February 27, 2012. <http://www.gtarehabnetwork.ca/reports>.
- Greenwald B.D., Burnett D.M., Miller M.A. 2003. “Congenital and Acquired Brain Injury. 1. Brain Injury: Epidemiology and Pathophysiology.” Archives of Physical Medicine and Rehabilitation 84(3 Suppl. 1): S3–S7 [PubMed] [Google Scholar]
- Hammond C.L., Pinnington L.L., Phillips M.F. 2009. “A Qualitative Examination of Inappropriate Hospital Admissions and Lengths of Stay.” BMC Health Services Research 9: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juurlink D., Preyra C., Croxford R., Chong A., Austin P., Tu J., et al. 2006. Canadian Institute for Health Information Discharge Abstract Database: A Validation Study. Toronto: Institute for Clinical Evaluative Sciences [Google Scholar]
- Kim H., Colantonio A., Deber R., Vernich L. 2006. “Discharge Destination from Acute Care After Traumatic Brain Injury.” Canadian Journal of Neurological Sciences 33(1): 48–52 [DOI] [PubMed] [Google Scholar]
- Kunik C.L., Flowers L., Kazanjian T. 2006. “Time to Rehabilitation Admission and Associated Outcomes for Patients with Traumatic Brain Injury.” Archives of Physical Medicine and Rehabilitation 87(12): 1590–96 [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Long-Term Care (MOHLTC) 2008. Ontario Wait Times. “Alternate Levels of Care (ALC) Patient Definition.” Retrieved February 27, 2012. <http://www.health.gov.on.ca/en/pro/programs/waittimes/edrs/alc_definition.aspx>.
- Ministry of Health and Long-Term Care (MOHLTC) 2010. “Discharge of Hospital Patients.” Toronto: Office of the Auditor General of Ontario [Google Scholar]
- Ministry of Health Long-Term Care (MOHLTC) 2011. Caring for Our Aging Population and Addressing Alternate Level of Care. Ministry Reports. Retrieved February 27, 2012. <http://www.health.gov.on.ca/en/public/publications/ministry_reports/walker_2011/walker_2011.aspx>.
- Rapoport M.J., Kiss A., Feinstein A. 2006. “The Impact of Major Depression on Outcome Following Mild-to-Moderate Traumatic Brain Injury in Older Adults.” Journal of Affective Disorders 92: 273–76 [DOI] [PubMed] [Google Scholar]
- Rogers J.M., Read C.A. 2007. “Psychiatric Comorbidity Following Traumatic Brain Injury.” Brain Injury 21(13–14): 1321–33 [DOI] [PubMed] [Google Scholar]
- Statistics Canada 2010. “Population by Year, by Province and Territory.” Retrieved February 27, 2012. <http://www40.statcan.gc.ca/l01/cst01/demo02a-eng.htm>.
- Sundararajan V., Henderson T., Perry C., Muggivan A., Quan H., Ghali W.A. 2004. “New ICD-10 Version of the Charlson Comorbidity Index Predicted In-Hospital Mortality.” Journal of Clinical Epidemiology 57(12): 1288–94 [DOI] [PubMed] [Google Scholar]
- Tagliaferri F., Compagnone C., Korsic M., Servadei F., Kraus J. 2006. “A Systematic Review of Brain Injury Epidemiology in Europe.” Acta Neurochirurgica 148(3): 255–68; discussion 268. [DOI] [PubMed] [Google Scholar]
- Toronto Acquired Brain Injury Network 2012. “Definition of Acquired Brain Injury.” Retrieved February 27, 2012. <http://www.abinetwork.ca/downloads/abidefinition.pdf>.
- Walker D. 2011. “Caring for Our Aging Population and Addressing Alternate Level of Care.” Retrieved February 27, 2012. <http://www.health.gov.on.ca/en/public/publications/ministry_reports/walker_2011/walker_2011.pdf>.
- World Health Organization (WHO) 2006. “Traumatic Brain Injuries.” In Neurological Disorders: Public Health Challenges (pp. 164–76). Geneva: Author; Retrieved February 27, 2012. <http://www.who.int/mental_health/neurology/neurodiso/en/>. [Google Scholar]
- Worthington A.D., Oldham J.B. 2006. “Delayed Discharge from Rehabilitation After Brain Injury.” Clinical Rehabilitation 20(1): 79–82 [DOI] [PubMed] [Google Scholar]