Abstract
HBV vaccination rates for incarcerated adults remain low despite their high risk for infection. This study determined predictors of vaccine completion in homeless adults (N=297) who reported histories of incarceration and participated in one of three nurse-led hepatitis programs of different intensity. Moreover time since release from incarceration was also considered. Just over half of the former prisoners completed the vaccine series. Older age (≥ 40), having a partner, and chronic homelessness were associated with vaccine completion. Recent research has documented the difficulty in providing vaccine services to younger homeless persons and homeless males at risk for HBV. Additional strategies are needed to achieve HBV vaccination completion rates greater than 50% for formerly incarcerated homeless men. Keywords: Hepatitis B, former prisoners, homeless, men, vaccine completion
Introduction
The Centers for Disease Control and Prevention (CDC, 2009) reported that as of 2007, within the United States (U.S.), the incidences of hepatitis A virus (HAV) and B virus (HBV) infection were 1.0 case per 100,000 and 1.5 cases per 100,000, respectively. HAV infection has been highly associated with poor water sanitation and poor standard of living (Lugoboni, Quaglio, Civitelli, & Mezzelani, 2009). Risk factors for HBV infection include injection drug use (IDU), unprotected sex (Nyamathi et al., 2009a), poverty, marginalized living conditions, and limited access to education and health care (Badiaga, Raoult, & Brouqui, 2008; Hudson et al., 2009; Vahdani, Hosseini-Moghaddam, Family, & Moheb-Dezfouli, 2009).
Among the previously incarcerated and homeless population in particular, risk factors are commonly experienced and can result in HBV infection. While HBV seroprevalence is high in homeless groups (Poulos, et al., 2007), within the correctional population, HBV infection is five times greater than in the general population (Gupta & Altice, 2009; Hennessey et al., 2009). Formerly incarcerated adults also face challenges in the community due to their high rates of substance use and abuse - 65% of prison inmates reported being regular drug users (US Department of Justice, 2006) and have limited access to drug treatment, housing and critical structural services (Freudenberg, Daniels, Crum, Perkins, & Richie, 2005; Kushel, Hahn, Evans, Bangsberg, & Moss, 2005; Narevic et al., 2006; Nelson, Deess, & Allen, 1999). In addition, formerly incarcerated individuals experience higher rates of mental illness, such as depression, post-traumatic stress disorder, bipolar disorder and schizophrenia, than the general population (Massoglia, 2008; McNiel, Binder, & Robinson, 2005); which may mediate high risk behaviors once released (Greenberg & Rosenheck, 2008).
HAV/HBV Compliance Among High-Risk Groups
Vaccination is considered to be the most effective way to prevent hepatitis infection (Motta-Castro et al., 2009). Despite vaccine availability, coverage has remained low among high-risk groups such as homeless persons (Nyamathi et al., 2009a) and persons who are either incarcerated (Sneller et al., 2008) or have a history of incarceration (Devasia et al., 2006). Among a sample of homeless individuals, those who reported a history of incarceration were less likely to complete the HAV/HBV vaccine series compared to the never incarcerated population (Nyamathi et al., 2009b). Moreover, in a study of jail inmates in three cities, only 12% of the study inmates had serologic evidence of hepatitis B immunization, compared with 25% self-reported hepatitis B vaccination among the general U.S. population (Hennessey et al., 2009). In particular, with persons with chronic Hepatitis C virus (HCV) infection, the need for HAV and HBV immunization to prevent co-infection of HAV and HBV is timely. Yet, only 62% of HCV infected individuals who received the combined HAV/HBV vaccine completed all three doses (Hernandez, Hasson, & Cheung, 2009). In fact, a compliance rate as low as 28% for all three HBV doses has been reported (Motta-Castro et al., 2009). As previously incarcerated homeless persons engage in high rates of behaviors that place them at risk for HAV (Latimer et al., 2007) and HBV infections (Devasia et al., 2006); this population should be targeted for prevention efforts upon their release from jail or prison.
Nurse-Led Hepatitis Vaccination Interventions
The existing literature supports the effectiveness of offering HAV/HBV risk reduction education along with HAV/HBV vaccination to high-risk groups such as homeless persons and those with a history of incarceration. Gunn and colleagues (2007) found that offering hepatitis vaccination along with education resulted in a 3-dose compliance rate of 62%, among attendees of an urban sexually transmitted infection clinic. Wolfers and colleagues (2009) showed that a counseling-plus-vaccination intervention resulted in a 3-dose HBV completion rate of 77%, among high-risk clinic attendees, while Hagedorn et al. (2007) reported a 60% 3-dose HAV/HBV completion rate among participants attending a substance use disorder clinic, following an intervention of group education and individual counseling. Nurse case management plus participant tracking has been correlated with significantly increased adherence to the HAV/HBV vaccination series (3-dose completion rate of 68%), among homeless adults (Nyamathi et al., 2009a).
Currently, there is a lack of literature on whether levels of intensity of nurse-led hepatitis programs predict successful vaccination completion among the formerly incarcerated population. The purpose of this study is to assess the effect of nurse-led hepatitis education programs of varying intensity on HAV/HBV vaccine completion among homeless persons with a history of incarceration. Understanding the impact of these programs targeting homeless adults with a history of incarceration can help in the planning and delivery of care to this vulnerable group.
Methods
Study Design
Data for this paper came from a larger study that used a longitudinal, randomized, quasi-experimental design to evaluate the effectiveness of one of three types of programs of varying intensity on HAV/HBV completion among homeless adults (Nyamathi et al., 2009a). These programs included two intervention programs: Nurse Case Managed Program with Incentives and Tracking (NCMIT), and a Standard plus Incentives and Tracking (SIT). The Control group was the Standard plus Incentives program only (SI).
In the parent study, all participants were offered the three-series Twinrix Hepatitis A (Inactivated) and Hepatitis B (Recombinant) Vaccine over a six-month period by a study nurse blinded to the group assignment. Study sites were stratified by the type of site and size and eligible individuals were randomized by site to one of the three programs. Independent nurse/outreach teams worked exclusively with participants in the same study condition, so that the team that worked with the nurse case managed group did not work with the standard education groups and vice versa. A team of outreach workers who were not involved in the intervention activities provided tracking and follow-up on all participants in the managed group and the standard education groups with tracking for the six-month follow-up questionnaire.
Recruitment sites included homeless shelters, residential recovery programs, and streets in the Skid Row area of Los Angeles. The University of California Los Angeles Human Subject Protection Committee approved the study, all measures utilized and all related materials. The Comprehensive Health Seeking and Coping Paradigm (CHSCP) (Nyamathi, 1989) provided the framework for the study and focused on the implementation of strategies relating to coping, communication skills, and promotion of health-seeking behavior. The current study was designed to assess predictors of vaccine completion among homeless adults who have a history of prior incarceration.
Participants
This sample included 297 male participants selected from the original sample of 854 and who reported a history of imprisonment. As a subgroup at risk for hepatitis B and C viruses as well as HIV, these assays were conducted. Persons eligible for the original study met the following criteria: a) aged 18–65, residing in one of the participating homeless sites; b) willingness to undergo hepatitis A virus (HAV), hepatitis B virus (HBV), hepatitis C virus (HCV) and HIV antibody testing at baseline and at six-month follow-up; and c) no history of HBV vaccination. In the total sample, 88% of participants completed the six-month follow-up. Among the participants who reported a history of incarceration, 90% completed the six-month follow-up. As previous incarceration rate among females in the parent study was low, only males were selected for the present study.
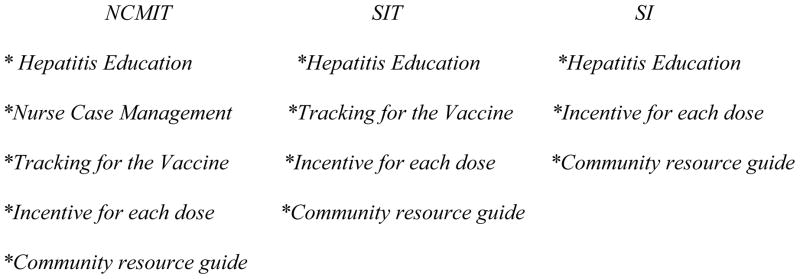
Nurse-led Hepatitis Programs – Three Levels
Nurse-led hepatitis programs are defined as targeted programs led by nurses which can vary in intensity – the highest level of intensity focuses on hepatitis health promotion, nurse case management, tracking for completion of the vaccine, and provision of incentives. The least intensive is also nurse-run, but offers primarily brief hepatitis education and incentive only. The three levels are described below and depicted in Figure 1.
Figure 1.
Levels of Nurse-led Hepatitis Programs
Nurse Case Managed with Incentives and Tracking (NCMIT)
Participants in the NCMIT program received the following from a trained research nurse: a) targeted hepatitis educational session during the first session that incorporated information about hepatitis and HIV infection, diagnosis, prevention and transmission; HAV/HBV vaccination, and the importance of adherence to the vaccine series; b) Nurse Case Management which included seven sessions focused on enhancement of self esteem, social and behavioral coping skills; self-management and communications competencies necessary for overcoming barriers to completion of the HBV vaccination series, and competencies to reducing risky substance use and sexual practices; c) Client Tracking by outreach workers; d) Incentives for receiving each dose of the vaccine ($5); and e) a Local Community Resource Guide.
Standard with Incentives and Tracking (SIT) Program
Participants in the SIT group received a 20-minute targeted hepatitis education session similar to the NCMIT group, as well as tracking, incentives and a local community resource guide.
Standard with Incentives (SI) Program
The SI group received the brief targeted hepatitis education session, and incentives, but no tracking. For all groups, the incentive for receiving each dose of the vaccine was $5. Additional financial incentives were provided equally to all participants for blood draw and return for test results, and completion of the baseline and six-month follow-up questionnaires.
Procedure
The research protocol and consent form were approved by the UCLA Human Subjects Protection committee. At each recruitment site, homeless adults who had signed an informed consent were administered a brief screener assessing basic socio-demographic characteristics and a hepatitis-related health history designed to evaluate eligibility for the HAV/HBV vaccination study. Those who were potentially eligible and completed a second written informed consent received pretest counseling and a provided a blood sample for HAV, HBV, HCV and HIV assays. Subsequent to the blood draw, the potential participants were referred to one of the research nurses stationed at the site two-weeks later for posttest counseling and test results. Homeless adults found to be HBV negative at the two-week follow-up (regardless of their HAV/HCV/HIV status), and who were interested in participating in the study were then provided final written informed consent for the study. Subsequent to administration of the baseline survey by the research staff, participants were informed of their randomization group and received one of the three programs over a six-month period.
Instruments
All instruments have been previously tested and validated for impoverished and/or homeless African-American, Latino, and White adults (Nyamathi et al., 2008; 2011; Sherbourne & Stewart, 1991; Simpson & Chatham, 1995; Stewart, Hays, & Ware, 1988).
Socio-demographic Characteristics
Socio-demographic information, which included age, gender, ethnicity, education, homeless history, partnership and veteran status, number of lifetime and recent sexual partners, public assistance, and history of incarceration was collected using a structured questionnaire.
Drug and Alcohol Use Behaviors
The TCU Drug History form measured Drug and Alcohol Use (Simpson & Chatham, 1995). This questionnaire records lifetime and past six-month use of 16 drugs, and elicits information about current frequency of non-injection and injection use. This instrument has been validated with men and women with a history of drug addiction, prostitution, and homelessness and revealed two-week test-retest reliabilities in an acceptable range of .63 to .71 (Anglin et al., 1996). The four-item CAGE screener (Ewing, 1984) and 2 additional items measured problem drinking. Sharing/Cleaning Needles and Other Drug Paraphernalia was measured by six items modified from the LA Seroprevalence Study (Ford, 1992); these items elicited data on needle sharing and cleaning, sharing other drug equipment, and sharing straws for cocaine and methamphetamine use. Binge drinking was defined as consumption of five or more drinks in a day. Respondents were also asked about their history of smoking cigarettes.
Mental and Physical Health
Mental Health was assessed with the Center for Epidemiological Studies Depression (CES-D) scale (Radloff, 1977) and the five-item mental health index (MHI-5) (Stewart, Hays, & Ware, 1988). The 20-item self-report CES-D is designed to measure depressive symptomology in the general population and has been validated for use in homeless populations (Ritchey, LaGory, Fitzpatrick, & Mullis, 1990). Each item measures the frequency of a symptom on a four-point response scale from 0 “Rarely or none of the time (Less than 1 day)” to 3 “Most of the time (5–7 days)”. Examples of CES-D items are “I felt depressed,” and “I felt fearful.” Item scores were summed giving an overall scale that could range from 0 to 60. Higher scores indicate more depression. The scale was dichotomized at the customary value of 16 (Radloff, 1977). The internal reliability in this sample was 0.90.
The MHI-5 has well-established reliability and validity (Stewart, Hays, & Ware, 1988) and is frequently scored on a scale of 0–100. An established cut-point of 66 (Rubenstein et al., 1989) was used to identify participants’ poor emotional well being. Cronbach’s alpha was 0.80.
Perceived Health status was measured by asking participants to rate their general health on a five-point scale from “excellent” to “poor”. Health status was dichotomized at fair or poor versus better health.
Statistical Analyses
Chi-square and two-sample t tests were used to assess group differences in socio-demographic characteristics, including homelessness (having been homeless for a year or more), time since discharge (being discharged from prison less than or one year or longer), substance use, depressive symptoms, emotional well-being and public benefits, depending on whether the variable of interest was categorical or continuous with an approximately normal distribution. This broad array of variables were selected to consider factors that may have biased the regression findings. Multiple logistic regression analysis was used to assess the relative effects of the programs on six-month HBV vaccine completion controlling for potential confounders. Initially, variables that were associated with HBV vaccine completion were used in a backward selection procedure at the .15 level in the multiple logistic regression to identify independent correlates. The retention level was .10. Final predictors in the models were examined for multi-collinearity and the Hosmer-Lemeshow test was used to assess goodness of fit of the model (p = .271), indicating the hypothesis that the model fits would not be rejected.. Statistical analyses were performed with SAS/STAT (http://www.sas.com).
Results
Socio-demographic Characteristics
The sample was composed of 297 eligible homeless males, who were a subsample of the parent study participants and were categorized as having been discharged from prison more than 1 year ago (n = 164) or more recently (≤ 1 year) (n = 133). As depicted in Table 1, this sample came primarily from the NCMIT and SIT groups (n = 140 and 108, respectively), with fewer in the SI group (n = 49). The majority of study participants were African American (70%), and over half were 40 years of age or older. Over two-thirds of the participants had completed high school and approximately two-thirds had been homeless for more than one year.
Table 1.
Baseline Sample Characteristics of Former Inmates by Program
| Characteristics | NCMIT++ (N = 140) | SIT++ (N = 108) | SI++ (N = 49) | Total (N = 297) |
|---|---|---|---|---|
| Background | % | % | % | % |
| Age ≥ 40* | 57.9 | 57.4 | 77.6 | 60.9 |
| Ethnicity: | ||||
| Black | 70.7 | 63.0 | 83.7 | 70.0 |
| White | 15.7 | 13.0 | 8.2 | 13.5 |
| Hispanic | 11.4 | 22.2 | 6.1 | 14.5 |
| Other | 2.1 | 1.9 | 2.0 | 2.0 |
| High School Grad* | 67.1 | 64.8 | 83.7 | 69.0 |
| Partnered | 26.4 | 21.3 | 34.7 | 25.9 |
| Recruitment Site*** | ||||
| Homeless Shelter | 25.2 | 20.4 | 18.4 | 22.3 |
| Drug Recovery Shelter | 49.6 | 62.0 | 18.4 | 49.0 |
| Street | 25.2 | 17.6 | 63.3 | 28.7 |
| Employed | 8.6 | 8.3 | 18.4 | 10.1 |
| Homeless ≥ 1 year | 64.8 | 64.5 | 65.3 | 64.8 |
| Recently discharged from jail/prison** | 42.1 | 56.5 | 26.5 | 44.8 |
| Government assistance*** | 41.4 | 50.0 | 79.6 | 50.8 |
| Lifetime IDUb | 22.1 | 28.7 | 18.4 | 23.1 |
| Recent+ IDU | 7.1 | 9.3 | 10.2 | 8.4 |
| Recent Non IDU | 53.6 | 50.0 | 51.0 | 51.9 |
| Daily Alcohol Use | 15.0 | 8.3 | 22.5 | 13.8 |
| Daily Drug Use | 32.1 | 25.9 | 42.9 | 31.7 |
| Binge drinking | 17.3 | 12.0 | 16.3 | 15.2 |
| Psychological Resources | ||||
| Depressive Symptoms | 46.4 | 45.4 | 40.8 | 45.1 |
| Poor Emotional Well Being | 47.9 | 38.9 | 40.8 | 43.4 |
| Support from Primary Substance Users | 3.8 | 7.5 | 11.4 | 6.3 |
| Support Primarily from Non Substance Users | 74.4 | 65.4 | 59.1 | 68.7 |
recent refers to past six-month period
NCMIT = Nurse Case Managed Program with Incentives and Tracking
SIT = Standard plus Incentives and Tracking;
SI = Standard plus Incentives program only
= Men Having Sex with Men;
= Injection Drug Use
p < .05, chi-square or t test for program differences
p < .01, chi-square or t test for program differences
p < .001, chi-square or t test for program differences
In comparing previously incarcerated by treatment group, no differences were found at baseline with respect to ethnicity, partnership status, or employment. However, differences were found with age, education, and recruitment site. Participants in the SI group were older, and more likely to have completed high school, received public assistance, and resided on the streets before the study when compared to participants in the other two groups. In addition, recently discharged inmates were underrepresented in the SI program. No differences were noted in reports of depressive symptoms, social support, or poor emotional well-being.
As shown in Table 1, nearly a quarter of the sample reported a history of lifetime injection drug use, with more than two-thirds reporting a history of inhaling cocaine or methamphetamine. Over half of the participants reported use of non-injection drugs in the past six months. Daily drug use was most prevalent in the SI group, while ex-inmates in the SIT group were more likely to report attending recent self-help programs.
Correlates of Vaccine Completion
In terms of completion of the HBV vaccine series, no differences were found with respect to time since release from jail/prison (Table 2). In addition, no differences were found in terms of type of program, ethnicity, education, recruitment site, recent self-help group attendance and drug use. Completing the vaccine was quite challenging for ex-inmates as only 61% of the NCMIT participants completed, with somewhat fewer in the SIT and SI programs (55% and 53%, respectively; data not shown). Completers were more likely to be older than 40 years of age (67%) compared to non-completers (53%), and more likely to have been homeless for one year or longer. Non-completers were more likely than completers to have engaged in binge drinking. Depressive symptomology was found to be high for both groups.
Table 2.
Associations Between Baseline Characteristics and Vaccine Completion
| Characteristic | Percent, or Mean (SD) | |
|---|---|---|
| Did not Complete Vaccine (N = 127) | Completed Vaccine (N = 170) | |
| Background | % | % |
| Age ≥ 40* | 52.8 | 67.1 |
| Ethnicity | ||
| African American | 67.7 | 71.8 |
| White | 16.6 | 11.2 |
| Hispanic | 14.2 | 14.7 |
| Other | 1.6 | 2.4 |
| High School Grad | 63.0 | 73.5 |
| Employed | 10.2 | 10.0 |
| Homeless ≥ 1 year* | 57.9 | 69.8 |
| Recently Discharged from Jail/Prison | 48.0 | 42.4 |
| Substance Use | ||
| Lifetime IDU | 22.8 | 24.7 |
| Recent + IDU | 8.7 | 8.2 |
| Recent Non-IDU | 52.0 | 51.8 |
| Daily Alcohol Use | 11.0 | 15.9 |
| Daily Drug Use | 33.9 | 30.0 |
| Recent Binge drinking** | 21.4 | 10.6 |
| Psychosocial Resources | ||
| Depressive Symptoms | 47.2 | 43.5 |
| Poor Emotional Well-Being | 46.5 | 41.2 |
| Multiple Sexual Partners Past 6 months | 24.4 | 26.5 |
recent refers to past six-month period
Score of 16 or more on 20-item CES-D
p < .05, chi-square or t test for differences between treatment completers and non-completers
p < .01, chi-square or t test for differences between treatment completers and non-completers
Multivariate Findings
Adjusting for potential confounders, older homeless individuals, those who have been homeless over one year and those who were partnered had almost 2 times greater odds completing the HBV vaccine series than younger homeless persons, and those without significant others (Table 3). Type of program was not a significant factor. Ex-inmates who attended a self-help program and those who reported binge drinking were significantly less likely to complete the vaccine than those not reporting these activities.
Table 3.
Logistic Regression Results for Completion of HBV Vaccination (n =294)
| Adjusted Odds Ratio | 95% CI | P Value | |
|---|---|---|---|
| Intervention Programs (vs Control Program) | |||
| NCMIT | 1.65 | 0.81, 3.32 | 0.165 |
| SIT | 1.61 | 0.77, 3.38 | 0.201 |
| Age ≥ 40 | 1.85 | 1.12, 3.07 | 0.017 |
| Homeless ≥ 1 year | 1.81 | 1.08, 3.03 | 0.025 |
| Fair/Poor Health | 1.51 | 0.77, 2.95 | 0.23 |
| Partnereda | 1.98 | 1.10, 3.58 | 0.023 |
| Recent+ Binge Drinking | 0.47 | 0.24, 0.92 | 0.029 |
| Recent + AA/NAb | 0.48 | 0.28, 0.81 | 0.006 |
recent refers to past six-month period
compared to not having a current partner
compared to no recent attendance at informal substance abuse treatment meetings
Discussion
Among our sample of homeless adults with a history of incarceration, findings revealed that intensity of nurse-led hepatitis programs was not a significant predictor of HAV/HBV vaccine completion among formerly incarcerated homeless persons. Depending on treatment group assignment, HAV/HBV vaccination completion rates varied (61%, 55% and 53% for NCMIT, SIT, and SI groups, respectively); there were no significant differences between the NCMIT and the other two groups. While rates of HBV vaccination completion among homeless populations have ranged from 47% (Lum, Ochoa, Hahn, Shafer & Moss, 2003) to 62% (Nyamathi et al., 2009a), strategies used to date have not resulted in acceptable vaccination rates among former prisoners who are homeless. However, incentives and careful follow-up may reveal a trend for increasing completion rates in this vulnerable group.
While we expected a stronger vaccination completion outcome among participants who participated in the NCMIT program, it is possible that if this study had been designed for ex-inmates, there may have been better outcomes for the NCMIT participants. Hence, this study points out while the risk in this population is great, more work needs to be done to understand the complex needs of, and multiple differences within, homeless, drug-using, and formerly incarcerated populations. Moreover, increased program and policy efforts and financial commitment are required to more effectively engage these individuals in preventive health services that have lasting effects, like HBV vaccination.
We found that older homeless participants were nearly twice as likely to complete the vaccination series, compared with younger participants. This is in accord with findings from a study by Wouters and colleagues (2007), which showed that among Belgian sex workers, persons over 40 had significantly higher compliance rates than those under 21. Altice and colleagues (2005) also found that among syringe exchange site attendees, older age was correlated with vaccination completion. Ompad and colleagues (2004) provides further evidence that older age is associated with vaccination completion.
We also found that time since incarceration was not significantly related to HAV/HBV vaccination completion among this vulnerable subgroup. While heavy use of drugs and alcohol by former inmates has been well documented in recent literature (Braithwaite & Arriola, 2003; Freudenberg et al., 2005; Hiller et al., 2005; Hudson et al., 2009; Kushel et al., 2005; Kushel, Vittinghoff, & Haas, 2001; Narevic et al., 2006; Nyamathi et al., 2009b), regardless of time since release, only about half of formerly incarcerated homeless men completed the HAV/HBV vaccine series. Further research is needed to investigate access-related issues parolees and other former inmates face once released into the community. Further research should also focus on increasing the interest of this group in engaging in activities that may promote life skills and providing support and guidance in seeking employment and partnerships with positive role models, while slowly engaging them in health promoting behaviors.
Nevertheless, findings also revealed that former inmates who were homeless for a longer period of time were more likely to complete the vaccine series. Those who had been homeless for over one year had a significantly greater likelihood of completing the vaccination series than did recently homeless persons. Longer duration of homelessness may have reflected a greater knowledge level of resources in the community for health protection. Participants who had been homeless longer may have also been more familiar and comfortable with taking advantage of available programs and services, such as the HBV vaccine series offered via this study.
Our study is the first to report the relationship between duration of homelessness and vaccination compliance. However, the concept that duration of homelessness has an impact on health behavior has been documented. Persons who have been homeless for more than a year have been found to have greater AIDS knowledge, and to engage in more risky sexual practices, compared with newly homeless persons (Rew, Grady, Whittaker, & Bowman, 2008).
Social support was also related to vaccination completion. Participants who had a support system were significantly more likely to complete the vaccination series than those without significant others. To date, there have been no published findings relating social support to hepatitis vaccination completion. However, there have been studies showing that higher social support predicts medication adherence with HIV medication regimens among high-risk youth (MacDonnell, Naar-King, Murphy, Parsons & Harper, 2009). Social support has also been shown to be a predictor of drug treatment completion among parole violators. (Zanis, Coviello, Lloyd, & Nazar, 2009).
Future research is warranted on the benefit of accelerated HBV vaccine schedules as well. A number of studies have been conducted to evaluate whether the provision of the hepatitis vaccine on an accelerated dosing schedule improves compliance among high-risk groups, with mixed results. HBV vaccination delivered on a 0, 1 month, and 4 month schedule did not result in significantly greater compliance than the usual 0, 1 month and 6 month schedule (compliance rates for the 3rd dose were 59% and 54%, respectively; Wouters et al., 2007). While Christensen et al. (2004) found that completion of the 3-week (0, 7-day, 14-day) HBV vaccine was significantly higher among prisoners (63%) versus those treated using the standard 6-month schedule (20%), others found that HBV vaccination resulted in very low completion rates for both the three week (29%) or the six month (57%) month schedule (Ramasami, Abu-Rajab, Sarkar, & Baguley, 2009). Additionally, a 12-month booster is also required with the 0, 7 day and 14 dosing schedule (Van Herck, Leuridan, & Van Damme, 2007).
Finally, we found that participants who attended a self-help program, and those who reported binge drinking, were significantly less likely to complete the vaccination series, compared with persons who did not attend self-help programs, or non-binge drinkers. We have not found any published clinical trials corroborating these findings, although there has been a relationship found between alcohol abuse and a history of incarceration (Hudson et al., 2009).
Clinical Implications
This study has clinical implications for forensic nursing. Findings revealed that both intensive and brief nursing interventions, coupled with incentives and detailed tracking can support HBV/HAV vaccine completion rates in formerly incarcerated, homeless adults, a marginalized and hard-to-reach population. The NCMIT and the SIT provide frameworks to develop programs that can offer critical health care services while addressing the multiple barriers facing this population including substance use disorders, mental health problems, limited access to housing and employment, and poor social support. A nurse-case managed program that approaches these barriers in a multifaceted way will promote health and ensure these individuals develop stable lives in their communities. Nurses serving this population could consider partnering with public health departments, nursing schools, treatment centers, and/or housing programs to develop nurse-led interventions and programs that provide not only HBV/HAV vaccines but essential services as well.
Study Limitations
This study has a couple of limitations. First, the sample included only male participants, recruited from the Skid Row area of Los Angeles. Consequently, the external generalizability of our findings to other homeless groups including women and those living in other cities may be limited. Second, there may have been inherent biases in our study design because self-report was used to evaluate the effect of control variables such as duration of homelessness, and substance use.
Conclusion
Homeless persons with a history of incarceration have higher rates of infectious disease than those without this history (Hudson et al., 2009). HAV and HBV infection continues to be a problem in this population and this has been attributed to several factors including poor medication adherence (Nyamathi et al., 2009b). This study was designed to assess predictors of HAV/HBV vaccination among formerly incarcerated homeless adults. Time since release had no bearing on HAV/HBV vaccination rates. Nevertheless, our compliance rates were similar to those reported in other studies undertaken to improve hepatitis vaccination compliance among high risk groups. Our most intense nursing intervention (NCMIT) was not significantly more effective at promoting compliance than were the other lesser intense groups (SIT and SI).
Homeless former prisoners often face barriers which limit their abilities to access health services (Hudson et al., 2009) and this may jeopardize vaccination compliance. Our participants were recruited from shelters, residential recovery programs, and from the streets of Los Angeles. It has been suggested that provision of hepatitis interventions should take place in controlled settings such as correctional facilities (Devasia et al., 2006). We believe that studies of the effect of nurse-led hepatitis intervention should be carried out within the correctional facility, in an attempt to evaluate whether prevention prior to release results in HAV/HBV infection reduction. Further research is also warranted on accelerated vaccine dosing schedules.
Acknowledgments
This study was supported by funds from the National Institute of Drug Abuse DA016147-01
Contributor Information
Adeline M. Nyamathi, University of California, Los Angeles.
Elizabeth Marlow, University of California, San Francisco.
Catherine Branson, University of California, Los Angeles.
Mary Marfisee, University of California, Los Angeles.
Karabi Nandy, University of California, Los Angeles.
References
- Altice FL, Bruce R, Walton M, Buitrago MI. Adherence to hepatitis B virus vaccination at syringe exchange sites. Journal of Urban Health. 2005;82(1):151–161. doi: 10.1093/jurban/jti016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anglin MD, Longshore D, Turner S, McBride D, Inciardi J, Prendergast M. Studies of the functioning and effectiveness of treatment alternatives to street crime (TASC) programs. Los Angeles: UCLA Drug Abuse Research Center; 1996. [Google Scholar]
- Badiaga S, Raoult D, Brouqui P. Preventing and controlling emerging and reemerging transmissible diseases in the homeless. Emerging Infectious Diseases. 2008;14(9):1353–1359. doi: 10.3201/eid1409.082042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braithwaite RL, Arriola KRJ. Male prisoners and HIV prevention: A call for action ignored. American Journal of Public Health. 2003;93(5):759–763. doi: 10.2105/ajph.93.5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Surveillance for acute viral hepatitis-United States, 2007. MMWR. 2009;58(SS-3):1–27. [PubMed] [Google Scholar]
- Christensen PB, Fisker N, Krarup HB, Liebert E, Jaroslavtsev N, Christensen K, Georgsen J. Hepatitis B vaccination in prison with a 3-week schedule is more efficient than the standard 6-month schedule. Vaccine. 2004;22:3897–3901. doi: 10.1016/j.vaccine.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Devasia RA, Jones T, Kainer M, Halford S, Sheeler LL, Swift J, Schaffer W. Two community hepatitis B outbreaks: an argument for vaccinating incarcerated persons. Vaccine. 2006;24(9):1354–1358. doi: 10.1016/j.vaccine.2005.09.023. [DOI] [PubMed] [Google Scholar]
- Ewing JA. Detecting alcoholism: The CAGE questionnaire. JAMA. 1984;252:1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- Ford WL. Risk assessment for IV drug users not in treatment. AIDS Epidemiology Program, Dept. of Health Services; Los Angeles, California: 1992. Unpublished Instrument. [Google Scholar]
- Freudenberg N, Daniels J, Crum M, Perkins T, Richie BE. Coming home from jail: The social and health consequences of community reentry for women, male adolescents, and their families and communities. American Journal of Public Health. 2005;95:1725–1736. doi: 10.2105/AJPH.2004.056325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg G, Rosenheck A. Jail incarceration, homelessness, and mental health: A national study. Psychiatric Services. 2008;59(2):170–177. doi: 10.1176/ps.2008.59.2.170. [DOI] [PubMed] [Google Scholar]
- Gunn RA, Lee MA, Murray PJ, Gilchick RA, Margolis S. Hepatitis B vaccination of men who have sex with men attending an urban STD clinic: Impact of an ongoing vaccination program, 1998–2003. Sexually Transmitted Diseases. 2007;54(9):663–668. doi: 10.1097/01.olq.0000258306.20287.a7. [DOI] [PubMed] [Google Scholar]
- Gupta S, Altice FL. Hepatitis B virus infection in US correctional facilities: A review of diagnosis, management, and public health implications. Journal of Urban Health. 2009;86:263–279. doi: 10.1007/s11524-008-9338-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagedorn H, Dieperink E, Dingmann D, Durfee J, Ho S, Isenhart C, Rettman N, et al. Integrating hepatitis prevention services into a substance use disorder clinic. Journal of Substance Abuse Treatment. 2007;32:391–398. doi: 10.1016/j.jsat.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Hennessey KA, Kim AA, Griffin V, Collins NT, Weinbaum CM, Sabin K. Prevalence of infection with hepatitis B and C viruses and co-infection with HIV in three jails: a case for viral hepatitis prevention in jails in the United States. Journal of Urban Health: Bulletin of the New York Academy of Medicine. 2009;86(1):93–105. doi: 10.1007/s11524-008-9305-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez B, Hasson NK, Cheung R. Hepatitis C performance measure on hepatitis A and B vaccination: Missed opportunities? The American Journal of Gastroenterology. 2009;104:1961–1967. doi: 10.1038/ajg.2009.252. [DOI] [PubMed] [Google Scholar]
- Hiller ML, Webster JM, Garrity TF, Leukefeld CG, Narevic E, Staton M. Prisoners with substance abuse and mental health problems: Use of health and health services. The American Journal of Drug and Alcohol Abuse. 2005;1:1–20. [PubMed] [Google Scholar]
- Hudson AL, Nyamathi A, Bhattacharya D, Shoptaw S, Marfisee M, Leake B. Impact of prison status on HIV-related risk behaviors. AIDS & Behavior. 2009 May 10; doi: 10.1007/s10461-009-9570-x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushel MB, Hahn JA, Evans JL, Bangsberg DR, Moss AR. Revolving doors: Imprisonment among the homeless and marginally housed population. American Journal of Public Health. 2005;95:1747–1752. doi: 10.2105/AJPH.2005.065094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285(2):200–6. doi: 10.1001/jama.285.2.200. [DOI] [PubMed] [Google Scholar]
- Latimer WW, Moleko A, Melnikov A, Mitchell M, Severtson SG, von Thomsen S, Graham C. Prevalence and correlates of hepatitis A among adult drug users: The significance of incarceration and race/ethnicity. Vaccine. 2007;25:7125–7131. doi: 10.1016/j.vaccine.2007.07.041. [DOI] [PubMed] [Google Scholar]
- Lugoboni F, Quaglio G, Civitelli P, Mezzelani P. Bloodborne viral hepatitis infections among drug users: the role of vaccination. International Journal of Environmental Research & Public Health. 2009;6:400–413. doi: 10.3390/ijerph6010400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lum PL, Ochoa KC, Hahn JA, Shafer KP, Moss AR. Hepatitis B virus immunization among young injection drug users in San Francisco, Calif: The UFO Study. American Journal of Public Health. 2003;93(6):919–923. doi: 10.2105/ajph.93.6.919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonnell KE, Naar-King S, Murphy D, Parsons J, Harper G. Predictors of medication adherence in high risk youth of color living with HIV. Journal of Pediatric Psychology. 2009:1–9. doi: 10.1093/jpepsy/jsp080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massoglia M. Incarceration as exposure: The prison, infectious disease, and other stress-related illnesses. Journal of Health & Social Science Behavior. 2008;49:56–71. doi: 10.1177/002214650804900105. [DOI] [PubMed] [Google Scholar]
- McNiel DE, Binder RL, Robinson JD. Incarceration associated with homelessness, mental disorder, and co-occurring substance abuse. Psychiatric Services. 2005;56:840–846. doi: 10.1176/appi.ps.56.7.840. [DOI] [PubMed] [Google Scholar]
- Motta-Castro A, Gomes SA, Yoshida C, Miguel JC, Teles SA, Martins RM. Compliance with and response to hepatitis B vaccination in remaining quilombo communities in Central Brazil. Cad Saude Publica. 2009;25(4):738–742. doi: 10.1590/s0102-311x2009000400004. [DOI] [PubMed] [Google Scholar]
- Narevic E, Garrity TF, Schoenberg NE, Hiller ML, Webster JM, Leukefeld CG, Staton Tindall M. Factors predicting unmet health services needs among incarcerated substance users. Substance Use & Misuse. 2006;41:1077–1094. doi: 10.1080/10826080600692167. [DOI] [PubMed] [Google Scholar]
- Nelson M, Deess P, Allen C. The first month out: Post-incarceration experiences in New York City. New York: Vera Institute of Justice; 1999. [Google Scholar]
- Nyamathi A. Comprehensive health seeking and coping paradigm. Journal of Advanced Nursing. 1989;14:281–290. doi: 10.1111/j.1365-2648.1989.tb03415.x. [DOI] [PubMed] [Google Scholar]
- Nyamathi A, de Castro V, McNeese-Smith D, Nyamathi K, Shoptaw S, Marfisee M, Khalilifard F, Cohen A. Alcohol use reduction program in methadone maintained individuals with hepatitis C virus infection. Journal of Addictive Diseases. 2008;27(4):27–33. doi: 10.1080/10550880802324499. [DOI] [PubMed] [Google Scholar]
- Nyamathi AM, Liu Y, Marfisee M, Shoptaw S, Gregerson P, Saab S, Leake B, et al. Effects of a nurse-managed program on hepatitis A and B vaccine completion among homeless adults. Nursing Research. 2009a;58(1):13–22. doi: 10.1097/NNR.0b013e3181902b93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi AM, Sinha K, Saab S, Marfisee M, Greengold B, Leake B, Tyler D. Feasibility of completing an accelerated vaccine series for homeless adults. Journal of Viral Hepatitis. 2009b;16:666–673. doi: 10.1111/j.1365-2893.2009.01114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi AM, Nandy K, Greengold B, Marfisee M, Khalilifard F, Cohen A, Leake B. Effectiveness of intervention on improvement of drug use among methadone maintained adults. Journal of Addictive Diseases. 2011;30:6–16. doi: 10.1080/10550887.2010.531669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ompad DC, Galea S, Wu Y, Fuller CM, Latka M, Koblin B, Vlahov D. Acceptance and completion of hepatitis B vaccination among drug users in New York City. Communicable Disease & Public Health. 2004;7(4):294–300. [PubMed] [Google Scholar]
- Poulos R, Ferson M, Orr K, Lucy A, Botham S, McCarthy M, Stern J, et al. Risk factors and seroprevalence of markers for hepatitis A, B and C in persons subject to homelessness in inner Sydney. Australian & New Zealand Journal of Public Health. 2007;31(3):247–251. doi: 10.1111/j.1467-842x.2007.00056.x. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ramasami S, Abu-Rajab K, Sarkar P, Baguley S. Audit of hepatitis B vaccination of men who have sex with men attending Scottish genitourinary medicine clinics. International Journal of STD & AIDS. 2009;20:575–576. doi: 10.1258/ijsa.2008.008447. [DOI] [PubMed] [Google Scholar]
- Rew L, Grady M, Whittaker TA, Bowman K. Interaction of duration of homelessness and gender on adolescent sexual health indicators. Journal of Nursing Scholarship. 2008;40(2):109–15. doi: 10.1111/j.1547-5069.2008.00214.x. [DOI] [PubMed] [Google Scholar]
- Ritchey FJ, La Gory M, Fitzpatrick KM, Mullis J. A comparison of homeless, community-wide, and selected distressed samples on the CES-Depression Scale. American Journal of Public Health. 1990;80:1384–1386. doi: 10.2105/ajph.80.11.1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubenstein LV, Calkins DR, Young RY, Cleary P, Fink A, Kosecoff J, Jette A, et al. Improving patient function: A randomized trial of functional disability screening. Annals of Internal Medicine. 1989;111:836–842. doi: 10.7326/0003-4819-111-10-836. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Simpson D, Chatham L. TCU/DATAR forms manual. Ft. Worth, TX: Institute of Behavioral Research, Texas Christian University; 1995. [Google Scholar]
- Sneller V, Fishbein DB, Weinbaum C, Lombard A, Murray P, McLaurin JA, Friedman L. Vaccinating adolescents in high-risk settings: Lessons learned from experiences with hepatitis B vaccine. Pediatrics. 2008;121(Suppl 1):S55–S62. doi: 10.1542/peds.2007-1115G. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Hays RD, Ware JE., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Medical Care. 1988;26:724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- US Department of Justice; Bureau of Justice Statistics. Drug Use and Dependence, State and Federal Prisoners 2004. 2006. [Google Scholar]
- Vahdani P, Hosseini-Moghaddam S, Family A, Moheb-Dezfouli R. Prevalence of HBV, HCV, HIV, and syphilis among homeless subjects older than fifteen years in Tehran. Archives of Iranian Medicine. 2009;12(5):483–487. [PubMed] [Google Scholar]
- Van Herck K, Leuridan E, Van Damme P. Schedules for hepatitis B vaccination of risk groups: balancing immunogenicity and compliance. Sexually Transmitted Infections. 2007;83:426–432. doi: 10.1136/sti.2006.022111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfers M, de Wit J, Hospers HJ, Richardus JH, de Zwart O. Effects of a short individually tailored counseling session for HIV prevention in gay and bisexual men receiving hepatitis B vaccination. BMC Public Health. 2009;9:1–11. doi: 10.1186/1471-2458-9-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wouters K, Leuridan E, Van Herck K, Van Ardenne N, Roelofs I, Mak R, Prevost C, et al. Compliance and immunogenicity of two hepatitis B vaccination schedules in sex workers in Belgium. Vaccine. 2007;25:1893–1900. doi: 10.1016/j.vaccine.2006.09.073. [DOI] [PubMed] [Google Scholar]
- Zanis DA, Coviello DM, Lloyd JJ, Nazar BL. Predictors of drug treatment completion among parole violators. Journal of Psychoactive Drugs. 2009;41(2):173–180. doi: 10.1080/02791072.2009.10399910. [DOI] [PubMed] [Google Scholar]