Abstract
Obesity is associated with impaired health-related quality of life (QoL) and reduced productivity; less is known about the effect of dietary factors. This study investigated how dietary behaviors, physical activity, and Body Mass Index (BMI) relate to weight-specific QoL and work productivity. The study was conducted in 31 small blue-collar and service industry worksites in Seattle. Participants were 747 employees (33.5% non-White). Measures included self-reported servings of fruits and vegetables, dietary behaviors such as fast food consumption, Godin free-time physical activity scores, measured height and weight, Obesity and Weight Loss Quality of Life (OWLQOL) scores, and Work Limitations Questionnaire (WLQ) scores. Baseline data were analyzed using linear mixed models separately for men (n=348) and women (n=399), since gender modified the effects. BMI was negatively associated with OWLQOL in both women (p<0.001) and men (p<0.001). The linear effect estimate for OWLQOL score associated with one-category increase in BMI was 30% (95% CI: 25%, 44%) for women and 14% (95% CI: 10%, 17%) for men. BMI was positively associated with productivity loss only in women (exp(slope)=1.46, 95% CI: 1.02, 2.11, p=0.04). Eating while doing another activity was negatively associated with OWLQOL scores in men (p=0.0006, independent of BMI) and with productivity in women (p=0.04, effect diminished when adjusting for BMI). Fast food meals were associated with decreased productivity for men (p=0.038, independent of BMI). Results suggest the obesogenic dietary behaviors and higher BMI are associated with decreased QoL and productivity variously in women and men.
Keywords: Dietary behaviors, Obesity, Quality of Life, Work productivity
INTRODUCTION
Obesity has become a major public health problem. In the United States, the prevalence of obesity (Body Mass Index of 30 or higher) has increased drastically, from 15% in 1985 to the current 34.3%(1). It is well-established that obesity is associated with a number of adverse health outcomes including hypertension, Type II diabetes, heart disease, stroke, respiratory problems, and certain types of cancer(2). Often overlooked are the equally important relationships between obesity and non-physical health outcomes, such as well-being, productivity, and psychosocial functioning.
To accommodate this oversight, Healthy People 2010(3) expanded its 2000 goal of longevity to include increased quality of life and overall well-being(4), researchers have started collecting such data, and the body of literature concerning obesity and outcomes such as quality of life and productivity is rapidly growing. Health-related quality of life (HRQOL) has been defined variously, but most often concerns concepts of physical, psychological, and social functioning and well-being. Measures of perceived quality of life are confined to those aspects of life known only to the person and are perceptions about how a specific condition affects a person’s life in relation to their goals, standards, and concerns(5).
Several studies have found that obesity is associated with a diminished HRQOL(6, 7), and higher Body Mass Indexes (BMIs) have been shown to be associated with physical, social, and emotional domains of HRQOL(4). Recently, researchers have also examined obesity-specific subscales of HRQOL. Kolotkin et al.(7), using the Impact of Weight on Quality of Life-Lite (IWQOL-Lite) instrument, showed that individuals with higher BMIs were more likely to report impaired obesity-specific HRQOL. Similar impairments in energy and vitality, in addition to increased body pain, have been observed in obese patients(6).
Obesity is also associated with reduced productivity(8), with an estimated $73.1 billion in productivity losses due to obesity among full-time employees(9). While some of this effect may be due to co-morbid conditions such as diabetes and hypertension, evidence suggests that lower productivity is exacerbated by the presence of obesity(10). BMI appears to independently predict absenteeism, with obese employees missing more days of work than their normal-weight counterparts(11). With high estimated costs lost due to sickness or disability related to obesity, the prevalence of obesity is a serious economic concern.
Evidence suggests HRQOL and productivity are modifiable by targeting diet and exercise. Randomized controlled trials (RCTs) have shown that a diet rich in fruits and vegetables is associated with higher HRQOL(12). Data also suggest physical activity is associated with improved HRQOL(13) and fewer physical and mental unhealthy days(14, 15). In addition, data from the longitudinal Swedish Obesity Study (SOS), which used the SOS Quality of Life Survey, showed that weight loss was associated with improved scores on the obesity-related problems (OP) subscale(4). Worksite interventions have proven successful in increasing fruit and vegetable consumption and physical activity(16) and may indirectly increase HRQOL and productivity.
The Move and Moderate in Balance (MOVE `M) study is a worksite-randomized trial to encourage healthy dietary choices and physical activity and maintain or reduce the weight of employees at the worksites. This paper explores baseline associations between BMI, fruit and vegetable consumption, physical activity and weight-related quality of life and proxy measures for productivity among employees of small South Seattle worksites.
METHODS
Recruitment
Worksites in South Seattle were recruited from a defined geographical area and were identified using U.S. Standard Industrial Classification (SIC) two-digit codes(17), including construction, manufacturing, transportation, and service industries. Worksites with between 15 and 80 employees were recruited. During a screening call, additional criteria were checked: a high proportion of employees with sedentary or stationary occupations (>50%), a low turnover rate (<30%), a low proportion of non-English speaking employees (<30%), and a breakdown of ≤33% management/professional staff and ≥30% in blue or pink collar positions.
Eligible interested worksites were involved in a run-in phase that required letter of intent to participate, employee list for survey administration, and high baseline survey response rate. Worksites were recruited on a rolling basis, constituting four waves with 32 worksites from 2006–2008. Each wave contains six to ten worksites (three to five pairs) randomized to either intervention or control arms. This manuscript includes data from 31 worksites (one worksite was not randomized) at baseline only.
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Institutional Review Boards at the University of Washington and the Fred Hutchinson Cancer Research Center. Written informed consent was obtained from all participants.
Baseline Measurements
Baseline surveys were solicited from all employees at participating worksites on an index date agreed with the company. Each site was given an additional two weeks to collect surveys from those who were not present at the proctored group meeting on the index date. If a site did not reach the 70% enrollment goal, two additional attempts were made to collect surveys from non-responders. The third and final attempt to collect survey data used a shorter version of the survey containing 15 vital information questions. Additional measures (i.e. blood draw and pedometer assessment) were taken on a randomly-selected sub-sample of about 20 individuals who had agreed on the survey to be re-contacted (or a minimum of 50% of survey respondents).
Assessment of BMI
BMI (kg/m2) was calculated using measured height and weight and was grouped according to standard categories: “underweight”, “normal”, “overweight”, and “obese”(18). Measurements were conducted at the baseline survey administration for everyone who completed a survey, and at the date of a blood draw at the site for those missing these objective measures.
Assessment of Dietary Behaviors
Daily servings of fruits and vegetables were assessed via the survey, which provided pictorial representations of typical fruit and vegetable servings. Summary fruit and vegetable questions in a Food Frequency Questionnaire (FFQ) format(19) assessed consumption of fruit, 100% fruit juice, other fruit juice, non French-fried potatoes, non-potato vegetables, and green salad. Fruit and vegetable consumption has consistently been shown to be associated with reduced BMI(20). Several eating behaviors have been shown to be associated with risk of obesity, including consumption of fast food(21) and soft drinks(22), TV viewing(22), and eating while doing other activities(22). The questionnaire included items on frequency of eating at fast food restaurants, frequency of drinking sodas, and eating while doing another activity such as watching television.
Assessment of Physical Activity
Physical activity was quantified as free-time physical activity of at least 10 minutes and was assessed using a modified Godin Leisure-Time Exercise Questionnaire(23), which used a cut-point of 15 minutes. The change, made in common with other centers in the Obesity Prevention in Worksites consortium, is consistent with the new recommendations(24). Godin and Shephard(25) established its reliability (test-retest correlation coefficient ranging from 0.48 for light activity to 0.94 for strenuous activity) and validity in relation to maximal oxygen consumption. At least one additional study has confirmed reliability and validity(26). Their published composite free-time exercise score was computed for each individual.
Assessment of Obesity-specific Quality of Life
Obesity-specific quality of life (HRQOL) was measured using the Obesity and Weight Loss Quality of Life (OWLQOL) Questionnaire(27, 28). The OWLQOL is a 17-item self-administered questionnaire that was developed cross-culturally to address shortcomings of preexisting instruments that focus on functional status or behaviors associated with obesity. The theoretical foundation for this instrument is the Maslow’s needs hierarchy(29). All items tap unobservable needs such as freedom from stigma and attainment of culturally-appropriate goals. For example, respondents are asked the degree to which weight affects their energy with statements such as “I feel frustrated that I have less energy because of my weight” and “My weight prevents me from doing what I want to do”. Reliability and validity are well-established and have exceeded recommended minimums within obese populations(28). The Guttman-Cronbach’s α was 0.96, indicating a high internal consistency, and factor analyses supported an overall score(28). Although a Cronbach’s α of 0.96 is very high, it refers to the total scale and 6,000 data points indicated a high α for each of many combinations of items, but the 17 that were chosen reflected the best content(30). Excluding several items reduced the α below 0.90, indicating reduced internal consistency(30). The composite OWLQOL score was computed for each individual and used as the obesity-specific quality of life outcome.
Assessment of Productivity
Productivity was assessed using the 8-item short-form of the Work Limitations Questionnaire (WLQ)(31). The WLQ is a self-administered questionnaire designed to measure the degree to which health problems may interfere with performing job functions(31). For instance, respondents are asked “In the past two weeks, how much of the time did your physical health or emotional problems make it difficult for you to do the following? 1) Get going easily at the beginning of the workday, 2) Handle the workload”. The reliability and validity of the WLQ are well-established(32). The WLQ is considered to be a good measure of self-reported work productivity, as self-reported work limitations have been shown to be significantly (p<0.0001) associated with employee work productivity(32). The overall WLQ Productivity Loss Score(33) was computed, where a higher score indicates greater limitations in work productivity.
Statistical Methods
Baseline demographic characteristics of the study subjects with no missing values for gender were computed. Associations betwee the log-transformed outcomes (OWLQOL scores and productivity loss scores) and the predictors were assessed. Predictors included log transformed BMI, physical activity (Godin score), daily servings of fruits and vegetables, doing something while eating, fast food restaurant meals per month, and soft drink consumption. Multiplicative interaction terms were generated by creating a cross-product term between each predictor and gender and tested for significance in a univariate model using a likelihood ratio test. Gender was found to modify the relationship between OWLQOL and all six predictors (each p<0.001), and between some predictors and WLQ productivity scores, so the OWLQOL and WLQ scores were analyzed by gender. For both outcomes, adjusted geometric means and 95% confidence intervals were obtained using linear mixed model for fixed age, race, education, and income effects and random worksite effects. The geometric mean is a common alternative way of presenting an average with an emphasis on central tendency, and is the appropriate choice when an outcome is log-transformed. It is similar to the arithmetic mean but is calculated by multiplying the numbers together (not summing, as in the arithmetic mean), then dividing the resulting product by the nth root (where n is the count of numbers in the set). Regression analyses were based on individuals with complete data on age, race, education, income, and the predictor and outcome of interest for each regression; thus the number of individuals varied for each analysis. The outcomes were log-transformed to reduce skewness and back transformed for comparison.
Next, OWLQOL scores and productivity loss scores were examined for a linear trend within each of the ordered categorical predictor variables described above, adjusting for age, race, education, and income. Race was collapsed into five categories (non-Hispanic White, Hispanic, Asian, Black or African American, and Other) when used as an adjustment variable. Logarithmically transformed slope estimates and their corresponding standard errors were obtained then back-transformed by taking the exponential of the slopes and corresponding 95% confidence intervals. The exponential of the slope represented the relative change of the outcome when the predictor increased one unit. Finally, the effects of physical activity and obesogenic dietary behaviors were assessed when controlling for BMI, which was logarithmically transformed to reduce the effect of skewness.
All statistical tests were two-sided. Statistical analyses were conducted using Statistical Analysis System software (version 9.1; SAS Institute, Inc.).
RESULTS
Results include all four randomization waves of MOVE `M (31 worksites). The average worksite had 27 employees, similar to the non-randomized companies in the recruiting pool. The most common worksite size was 15–24 employees for randomized companies and 10–14 for non-randomized companies. Randomized worksites reflected the SIC code distribution of the underlying recruiting pool.
The original dataset of employees in randomized companies who completed the baseline questionnaire (n=753) was restricted to individuals with non-missing values for gender (n=747, 99.2% of original dataset). A slightly greater proportion of males had a college degree whereas slightly greater proportion of females had a postgraduate or professional degree (Table 1). The majority of both female and male employees were non-Hispanic White (65.4% and 66.8% and respectively), reflecting the general population composition in the Pacific Northwest. Approximately 61% (n=459) of employees were either overweight (25.8%) or obese (35.6%). The average BMI, servings of fruits and vegetables, free-time physical activity scores, and WLQ Scores were similar between males and females; however, a higher proportion of men were overweight as compared to women. Males had a slightly higher average OWLQOL score (86.0) than females (69.5).
Table 1.
Baseline demographic characteristics of employees at Move'M worksites
| Females (n=399) |
Males (n=348) |
|||
|---|---|---|---|---|
| n | %a | n | %a | |
| Age (yrs) | ||||
| < 25 | 30 | 7.5 | 32 | 9.2 |
| 25 to 39 | 154 | 38.6 | 132 | 37.9 |
| 40 to 54 | 157 | 39.4 | 116 | 33.3 |
| 55+ | 58 | 14.5 | 67 | 19.3 |
| Race | ||||
| Non-Hispanic White | 261 | 65.4 | 233 | 67.0 |
| Hispanic | 32 | 8.0 | 28 | 8.1 |
| Black or African American | 40 | 10.0 | 25 | 7.2 |
| Asian | 37 | 9.3 | 36 | 10.3 |
| Otherb | 27 | 6.8 | 22 | 6.3 |
| Education | ||||
| Less than high school | 18 | 4.5 | 9 | 2.6 |
| High school graduate or GED | 194 | 48.6 | 159 | 45.7 |
| Technical college | 24 | 6.0 | 22 | 6.3 |
| College | 105 | 26.3 | 127 | 36.5 |
| Postgraduate or professional degree | 57 | 14.3 | 28 | 8.1 |
| Household income | ||||
| <$25,000 | 24 | 6.0 | 21 | 6.0 |
| $25,000 to 49,000 | 108 | 27.1 | 62 | 17.8 |
| $50,000 to 74,999 | 78 | 19.6 | 82 | 23.6 |
| $75,000 to 100,000 | 73 | 18.3 | 45 | 12.9 |
| >$100,000 | 65 | 16.3 | 82 | 23.6 |
| BMI (kg/m2) | ||||
| <18.5 ("underweight") | 5 | 1.3 | 0 | 0.0 |
| 18.5 to 24.99 ("normal") | 122 | 30.6 | 62 | 17.8 |
| 25 to 29.99 ("overweight") | 80 | 20.1 | 113 | 32.5 |
| 30+ ("obese") | 147 | 36.8 | 119 | 34.2 |
| Daily servings fruits/vegetables | ||||
| <1 | 11 | 2.8 | 7 | 2.0 |
| 1 to 2 | 167 | 41.9 | 194 | 55.8 |
| 3 to 4 | 164 | 41.1 | 107 | 30.8 |
| 5+ | 56 | 14.0 | 37 | 10.6 |
| Soft drink/soda (diet or regular) consumption | ||||
| Never | 91 | 22.8 | 41 | 11.8 |
| Less than once a week | 96 | 24.1 | 60 | 17.2 |
| About once a week | 40 | 10.0 | 36 | 10.3 |
| 2–5 times per week | 81 | 20.3 | 84 | 24.1 |
| About once a day | 52 | 13.0 | 76 | 21.8 |
| 2 or more times per day | 38 | 9.5 | 48 | 13.8 |
| Eating while doing another activity | ||||
| Never | 16 | 4.0 | 21 | 6.0 |
| Seldom | 59 | 14.8 | 79 | 22.7 |
| Sometimes | 161 | 40.4 | 137 | 39.4 |
| Most of the time/Always | 162 | 40.6 | 108 | 31.0 |
| Meanc | SD | Meanc | SD | |
| BMI | 29.7 | 8.1 | 29.8 | 6.0 |
| Servings fruits/vegetables | 3.0 | 1.8 | 2.6 | 1.8 |
| Fast food meals per month | 5.3 | 6.8 | 6.8 | 7.8 |
| Free time physical activity score | 25.1 | 20.6 | 31.3 | 28.9 |
| Obesity and Weight-Loss Quality of Life total score | 69.5 | 24.7 | 86.0 | 16.3 |
| Work Limitations Productivity Loss Score | 6.8 | 6.4 | 6.2 | 6.0 |
Move'M, Move and Moderate in Balance; GED, General Equivalency Diploma
Percents may not sum to 100% due to rounding or missing data
Other includes Native American or Alaskan Native, Hawaiian or Pacific Islander, or self-specified
Arithmetic mean
Examining OWLQOL as the outcome of interest, for all predictors, there were significant interactions with gender (each p<0.0001). Thus, all OWLQOL analyses were presented as gender-specific (Table 2). OWLQOL scores were negatively associated with BMI for both females (p<0.0001) and males (p<0.0001). The negative impact of obesity on OWLQOL scores was more pronounced for women. An additional unit in BMI was associated 30% lower (95% CI: 25%, 34%) geometric mean OWLQOL for women and a 14% lower (95% CI: 10%, 17%) geometric mean OWLQOL for men.
Table 2.
Mean Obesity and Weight Loss Quality of Life (OWLQOL) scores by baseline reported dietary behaviors, physical activity, and BMI
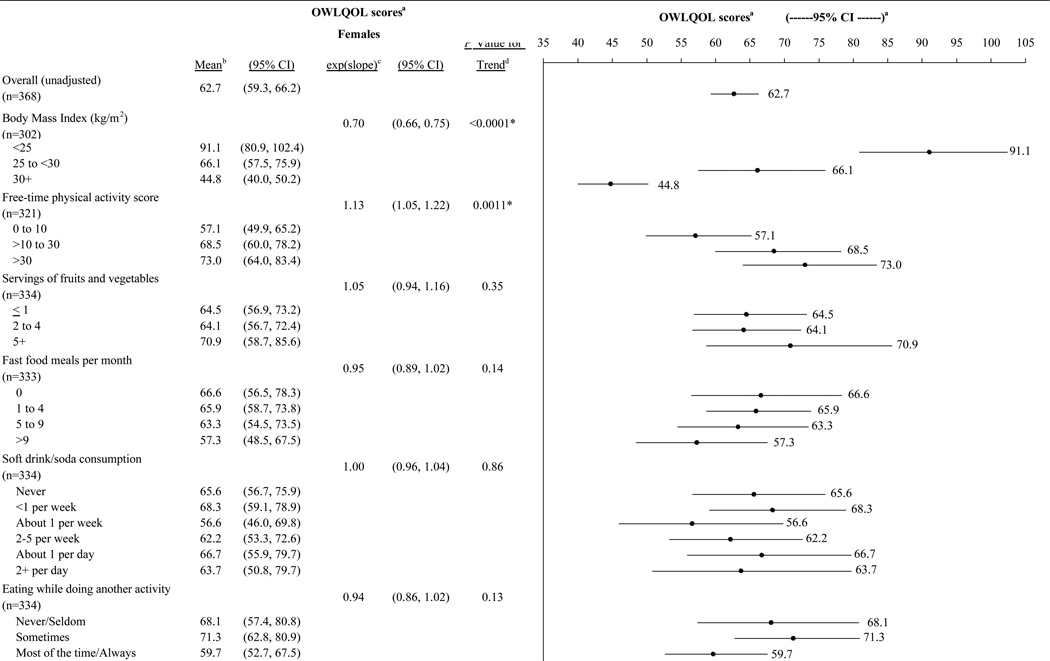
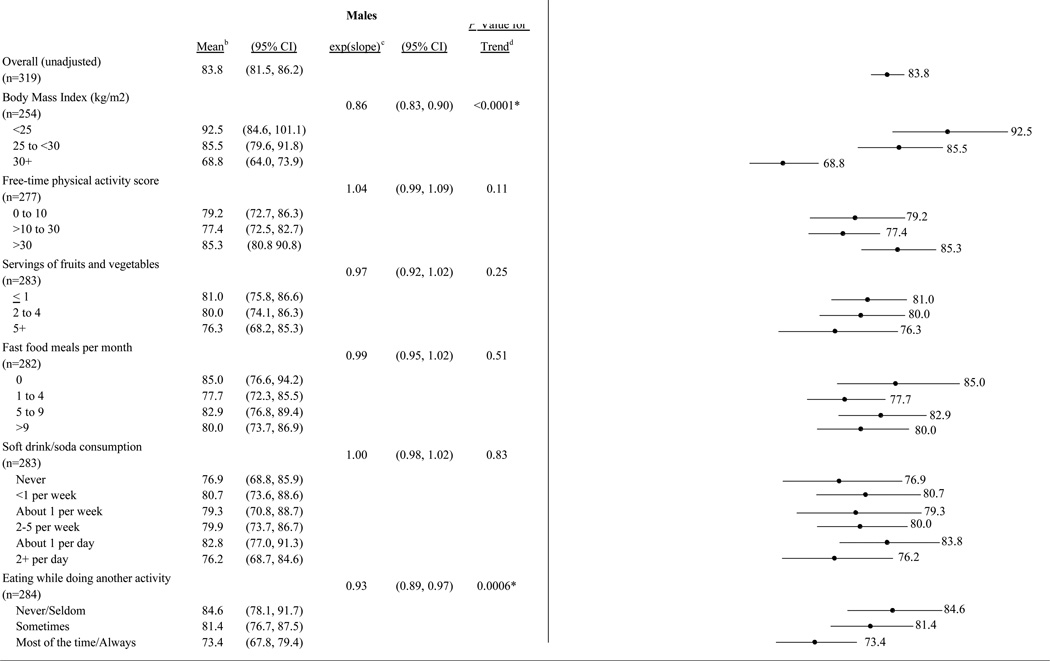
|
Linear mixed model adjusted for age (continuous), race (collapsed into 4 categories), education, and income
Geometric mean
Exponential transform of slope estimate: slope coefficients were obtained from log-transformed data, but have been back-transformed for presentation here
Trend tested with Wald Test
Significant at the 0.05 level
Physical activity was positively associated with OWLQOL only in women (p=0.0011). An additional unit in free-time physical activity score was associated with 13% positive difference (95% CI: 5%, 22%) in geometric mean OWLQOL score. However, this effect became insignificant when controlling for BMI. Servings of fruits and vegetables, soda consumption, and fast food consumption were not significantly associated with OWLQOL scores for males or females. Eating while doing other activities was significantly associated with the OWLQOL in men only (p=0.0006). Comparing two men, the geometric mean OWLQOL score for the man who ate more frequently while doing other activities was 7% lower (95% CI: 3%, 11%) than the man who ate while doing other activities less frequently. This association remained significant after controlling for BMI but became attenuated (exp(slope)=0.95, 95% CI: 0.92, 0.98, p=0.0028). All other effects remained the same when controlling for BMI. All associations and effect sizes persisted after controlling for age, race, education, and income.
Interactions were again present when examining the Work Limitations Questionnaire score as the outcome, so these analyses were also presented as gender-specific (Table 3). BMI was positively associated with WLQ scores only in women (p=0.04). A one-category difference in BMI was associated with a 1.46-fold (95% CI: 1.02, 2.11) positive difference in geometric mean WLQ score. The association between BMI and WLQ scores was insignificant in men (p=0.06). Eating while doing another activity was positively associated with WLQ scores only in women (p=0.04). A one-category difference was associated with a 1.59-fold (95% CI: 1.01, 2.50) positive difference in geometric mean WLQ score; however, this effect diminished when controlling for BMI. Fast food consumption was significantly positively related to WLQ score in men (p=0.038). A one-category difference was associated with a 1.56-fold (95% CI: 1.03, 2.37) positive difference in geometric mean WLQ score. This association remained significant when controlling for BMI. None of the remaining predictors were associated with productivity loss scores for males or females. All other effects remained the same when controlling for BMI, and all associations and effect sizes persisted after controlling for age, race, education, and income.
Table 3.
Mean Work Limitations Questionnaire (WLQ) Productivity Loss Score by baseline reported dietary behaviors, physical activity, and BMI
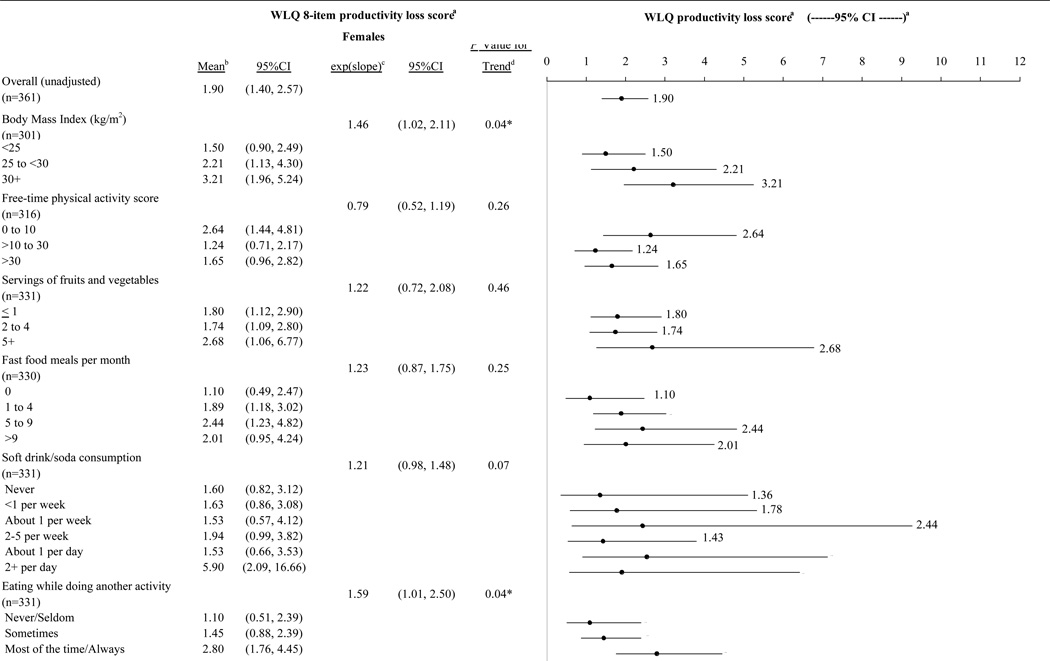 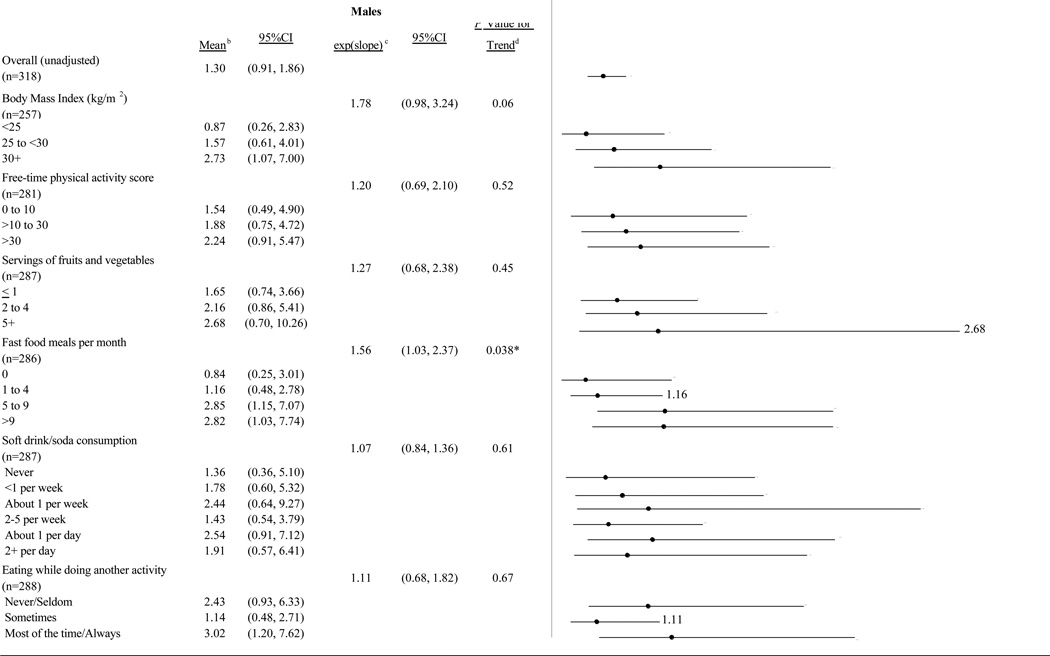
|
Linear mixed model adjusted for gender, age (continuous), race (collapsed into 4 categories), education, and income
Geometric mean
Exponential transform of slope estimate: slope coefficients were obtained from log-transformed data, but have been back-transformed for presentation here
Trend tested with Wald Test
Significant at the 0.05 level
DISCUSSION
Results from this study suggest that BMI is inversely associated with self-reported obesity-specific HRQOL and work productivity. Certain obesogenic behaviors were also related to obesity-specific HRQOL and productivity. For women, free-time physical activity was associated with higher obesity-specific quality of life, and eating while doing another activity was associated with lower productivity, but these associations appeared to operate through BMI. For men, eating while doing another activity was inversely associated with obesity-specific quality of life and fast food meals were inversely associated with productivity; however, unlike in women, these effects did not appear to operate through BMI.
The suggestion of a gender difference appears to be supported by the research in this area. As was expected from the literature(28, 34–36), women in this study were more likely to report lower obesity-specific quality of life. In addition, the results presented agree with previous studies that found the impact of obesity on HRQOL to be more severe for women than men(34, 37). Similarly, prior results have found an effect of physical activity on HRQOL for both men and women(14, 15), and within women alone(38). The findings also complement a study by Muenning etl al.(39) who found the desire to lose weight was a stronger predictor of unhealthy days for women than men, concluding that negative body image contributes to the morbidity of obesity, particularly for women. Indeed, one potential explanation for this gender difference is body image. The social acceptability of body size can vary between women and men; at least one study has shown that overweight men are significantly more likely to report that their body size was socially acceptable than overweight women(40). Women also tend to be more heavily impacted by body image psychologically than men, associating body dissatisfaction with self-esteem(41), and by selecting body images thinner than their own as being more desirable to the opposite sex(42). Thus, it is possible that the positive effects of healthier dietary and physical activity behaviors on quality of life and productivity are conditional on body size perceptions only among women.
The evidence presented, combined with current economic evidence, may help to convince management to invest in the health of their employees. In particular, the findings may have important implications for companies and organizations, which may want to consider offering healthier choices and lunch breaks for employees in order to maintain or increase productivity. It is especially important for the MOVE `M study, as this could provide incentive for worksites to join the study if they believe decreasing employees’ BMIs as a result of the intervention’s effort may increase productivity.
The present study has several limitations. All variables, with the exception of BMI, were assessed using self-report survey data. However, it is important to note that quality of life can only be measured by reports by the individual and perceived productivity may be an equally or more important measure compared to productivity measures such as absenteeism, lost wages, and replacement staff from the employer. Due to the cross-sectional nature of these data, one cannot draw conclusions concerning causality. Thus, it is unclear whether BMI and physical activity may influence obesity-specific QOL, or if this relationship is reversed. Weight-related quality of life could well be a predictor of weight-related behaviors. Due to the small number of underweight individuals, the data could not be used to verify previous research(43, 44) suggesting individuals at either end of the spectrum, underweight or overweight/obese, tend to have compromised self-reported HRQOL. Nonetheless, whereas current studies have focused on general HRQOL, this study confirms a similar negative impact of obesity on obesity-specific HRQOL. Finally, although the most common worksite size of randomized companies was slightly larger than non-randomized companies, this is unlikely to affect the generalizability of these results.
The study has several noteworthy strengths. The large sample size allows us to draw strong conclusions. In addition, height and weight were directly measured for all employees, resulting in BMI calculations that are more accurate than those obtained from self-reported height and weight. Using linear mixed models, worksite-level effects were controlled for in order to examine individual-level associations. Finally, the study design will allow us to evaluate the effect of the intervention, particularly in relation to the measures described in this manuscript. The hypothesis is that the intervention will increase fruit and vegetable consumption and physical activity and decrease BMI, and that a related improvement in OWLQOL and productivity scores will be observed. Nonetheless, this determination cannot be made based on cross-sectional data, and evaluation of these outcomes at two-year follow-up may shed more light on this potential mediating mechanism.
These results suggest that obesity-specific HRQOL and productivity may be particularly impaired in obese men and women, with the impact being more pronounced in women. Physical activity and obesogenic behaviors may operate through BMI to affect obesity-specific quality of life and productivity in women, but obesogenic behaviors appear to affect obesity-specific quality of life and productivity independent of BMI in men. The implication gender differences in the effects of obesity, physical activity, and obesogenic behaviors on obesity-specific HRQOL and productivity is important and should be further researched. Such information may prove useful in addressing the mental health and overall well-being of obese women and men.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the employees at the worksites who took the time to complete the baseline survey and physical measurements for the MOVE `M study. Their voluntary participation made this investigation possible. The work presented here was supported by funding from the US National Cancer Institute as part of U54 CA116847. All authors contributed to this manuscript. SAW conceived the study and wrote the majority of the manuscript. SAAB is the Principle Investigator of the MOVE ‘M project, wrote the protocol, guided the assessment development, and monitored the research process for this paper from its inception by providing methodological and statistical guidance and participating in manuscript revisions. JAH assisted in writing the methods section, particularly concerning the recruitment of worksites. AM edited the manuscript and acted as the Principle Investigator of the collection of studies of which this study was a part. LX conducted all analyses and assisted in the write-up of the statistical analyses section. CYW contributed to the statistical analyses section and aided in analyses. DLP provided guidance on patient reported outcomes and assisted in writing the sections on the measurement of obesity-related quality of life (the OWLQOL) and the discussion and interpretation of results.
Footnotes
Conflict of Interest Statement: The authors declare that they have no competing interests.
REFERENCES
- 1.Overweight and Obesity: Introduction. 2010 [updated November 20, 2009; cited 2010 February 22]; Available from: http://www.cdc.gov/obesity/data/trends.html.
- 2.Overweight and Obesity: Health Consequences. 2010 [updated August 19, 2009; cited 2010 February 22] Available from: http://www.cdc.gov/obesity/causes/health.html.
- 3.Healthy People 2010: Understanding and Improving Health. Washington, DC: 2001. [Google Scholar]
- 4.Karlsson J, Taft C, Ryden A, et al. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes (Lond) 2007 Aug;31(8):1248–1261. doi: 10.1038/sj.ijo.0803573. [DOI] [PubMed] [Google Scholar]
- 5.Patrick DL, Erickson P. Health status and health policy: quality of life in health care evaluation and resource allocation. New York: Oxford University Press; 1993. [Google Scholar]
- 6.Fontaine KR, Cheskin LJ, Barofsky I. Health-related quality of life in obese persons seeking treatment. J Fam Pract. 1996 Sep;43(3):265–270. [PubMed] [Google Scholar]
- 7.Kolotkin RL, Crosby RD, Williams GR. Health-related quality of life varies among obese subgroups. Obes Res. 2002 Aug;10(8):748–756. doi: 10.1038/oby.2002.102. [DOI] [PubMed] [Google Scholar]
- 8.Wolf AM, Colditz GA. Current estimates of the economic cost of obesity in the United States. Obes Res. 1998 Mar;6(2):97–106. doi: 10.1002/j.1550-8528.1998.tb00322.x. [DOI] [PubMed] [Google Scholar]
- 9.Finkelstein EA, Dibonaventura MD, Burgess SM, et al. The Costs of Obesity in the Workplace. Journal of occupational and environmental medicine / American College of Occupational and Environmental Medicine. 2010 Sep 25; doi: 10.1097/JOM.0b013e3181f274d2. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan PW, Ghushchyan V, Ben-Joseph RH. The Effect of Obesity and Cardiometabolic Risk Factors on Expenditures and Productivity in the United States. Obesity. 2008 doi: 10.1038/oby.2008.325. 26 June 2008. [DOI] [PubMed] [Google Scholar]
- 11.Bungum T, Satterwhite M, Jackson AW, et al. The relationship of body mass index, medical costs, and job absenteeism. American journal of health behavior. 2003 Jul-Aug;27(4):456–462. doi: 10.5993/ajhb.27.4.17. [DOI] [PubMed] [Google Scholar]
- 12.Plaisted CS, Lin PH, Ard JD, et al. The effects of dietary patterns on quality of life: a substudy of the Dietary Approaches to Stop Hypertension trial. J Am Diet Assoc. 1999 Aug;99(8 Suppl):S84–S89. doi: 10.1016/s0002-8223(99)00421-6. [DOI] [PubMed] [Google Scholar]
- 13.Vuillemin A, Boini S, Bertrais S, et al. Leisure time physical activity and health-related quality of life. Prev Med. 2005 Aug;41(2):562–569. doi: 10.1016/j.ypmed.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 14.Brown DW, Balluz LS, Heath GW, et al. Associations between recommended levels of physical activity and health-related quality of life. Findings from the 2001 Behavioral Risk Factor Surveillance System (BRFSS) survey. Prev Med. 2003 Nov;37(5):520–528. doi: 10.1016/s0091-7435(03)00179-8. [DOI] [PubMed] [Google Scholar]
- 15.Brown DW, Brown DR, Heath GW, et al. Associations between physical activity dose and health-related quality of life. Med Sci Sports Exerc. 2004 May;36(5):890–896. doi: 10.1249/01.mss.0000126778.77049.76. [DOI] [PubMed] [Google Scholar]
- 16.Beresford SA, Thompson B, Feng Z, et al. Seattle 5 a Day worksite program to increase fruit and vegetable consumption. Prev Med. 2001 Mar;32(3):230–238. doi: 10.1006/pmed.2000.0806. [DOI] [PubMed] [Google Scholar]
- 17. [[cited 2008 July 4]];1987 SIC Matched to 1997 NAICS Major Groups (2-Digit) Available from: http://www.census.gov/epcd/naics/nsic2ndx.htm#S3.
- 18.How is BMI calculated and interpreted? 2008 [updated June 20, 2008; cited 2008 July 28] Available from: http://www.cdc.gov/nccdphp/dnpa/healthyweight/assessing/bmi/adult_BMI/about_adult_BMI.htm#Interpreted.
- 19.Thompson FE, Byers T. Dietary assessment resource manual. J Nutr. 1994 Nov;124(11 Suppl):2245S–2317S. doi: 10.1093/jn/124.suppl_11.2245s. [DOI] [PubMed] [Google Scholar]
- 20.Lin BH, Morrison RM. Higher Fruit Consumption Linked WIth Lower Body Mass Index. Food Review. 2002;25(3):28–32. [Google Scholar]
- 21.French SA, Harnack L, Jeffery RW. Fast food restaurant use among women in the Pound of Prevention study: dietary, behavioral and demographic correlates. Int J Obes Relat Metab Disord. 2000 Oct;24(10):1353–1359. doi: 10.1038/sj.ijo.0801429. [DOI] [PubMed] [Google Scholar]
- 22.Liebman M, Pelican S, Moore SA, et al. Dietary intake, eating behavior, and physical activity-related determinants of high body mass index in rural communities in Wyoming, Montana, and Idaho. Int J Obes Relat Metab Disord. 2003 Jun;27(6):684–692. doi: 10.1038/sj.ijo.0802277. [DOI] [PubMed] [Google Scholar]
- 23.Godin G, Shephard RJ. Godin Leisure-Time Exercise Questionnaire. Medicine and Science in Sports and Exercise. 1997 Jun 29;(Supplement):S36–S38. June. [Google Scholar]
- 24. [cited 2008 August 1];Inside the Pyramid: How much physical activity is needed? 2008 Available from: http://www.mypyramid.gov/pyramid/physical_activity_amount.html.
- 25.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985 Sep;10(3):141–146. [PubMed] [Google Scholar]
- 26.Jacobs DR, Jr, Ainsworth BE, Hartman TJ, et al. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993 Jan;25(1):81–91. doi: 10.1249/00005768-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Niero M, Martin M, Finger T, et al. A new approach to multicultural item generation in the development of two obesity-specific measures: the Obesity and Weight Loss Quality of Life (OWLQOL) questionnaire and the Weight-Related Symptom Measure (WRSM) Clin Ther. 2002 Apr;24(4):690–700. doi: 10.1016/s0149-2918(02)85144-x. [DOI] [PubMed] [Google Scholar]
- 28.Patrick DL, Bushnell DM, Rothman M. Performance of two self-report measures for evaluating obesity and weight loss. Obes Res. 2004 Jan;12(1):48–57. doi: 10.1038/oby.2004.8. [DOI] [PubMed] [Google Scholar]
- 29.Maslow AH. A Theory of Human Motivation. Psychological Review. 1943;50(4):370–396. [Google Scholar]
- 30.Patrick D. Whisnant S, editor. Personal communication via e-mail. 2010.
- 31.Lerner D, Amick BC, 3rd, Rogers WH, et al. The Work Limitations Questionnaire. Med Care. 2001 Jan;39(1):72–85. doi: 10.1097/00005650-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Lerner D, Amick BC, 3rd, Lee JC, et al. Relationship of employee-reported work limitations to work productivity. Med Care. 2003 May;41(5):649–659. doi: 10.1097/01.MLR.0000062551.76504.A9. [DOI] [PubMed] [Google Scholar]
- 33.Lerner D, Rogers WH, Chang H. Technical Report: Scoring the Work Limitations Questionnaire (WLQ) Scales and the WLQ Index for Estimating Work Productivity Loss. 2005 [Google Scholar]
- 34.Kolotkin RL, Head S, Hamilton M, et al. Assessing Impact of Weight on Quality of Life. Obes Res. 1995 Jan;3(1):49–56. doi: 10.1002/j.1550-8528.1995.tb00120.x. [DOI] [PubMed] [Google Scholar]
- 35.Katz DA, McHorney CA, Atkinson RL. Impact of obesity on health-related quality of life in patients with chronic illness. J Gen Intern Med. 2000 Nov;15(11):789–796. doi: 10.1046/j.1525-1497.2000.90906.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kolotkin RL, Crosby RD, Kosloski KD, et al. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001 Feb;9(2):102–111. doi: 10.1038/oby.2001.13. [DOI] [PubMed] [Google Scholar]
- 37.Larsson U, Karlsson J, Sullivan M. Impact of overweight and obesity on health-related quality of life--a Swedish population study. Int J Obes Relat Metab Disord. 2002 Mar;26(3):417–424. doi: 10.1038/sj.ijo.0801919. [DOI] [PubMed] [Google Scholar]
- 38.Brown WJ, Mishra G, Lee C, et al. Leisure time physical activity in Australian women: relationship with well being and symptoms. Res Q Exerc Sport. 2000 Sep;71(3):206–216. doi: 10.1080/02701367.2000.10608901. [DOI] [PubMed] [Google Scholar]
- 39.Muennig P, Jia H, Lee R, et al. I think therefore I am: perceived ideal weight as a determinant of health. Am J Public Health. 2008 Mar;98(3):501–506. doi: 10.2105/AJPH.2007.114769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rand CS, Resnick JL. The "good enough" body size as judged by people of varying age and weight. Obes Res. 2000 Jul;8(4):309–316. doi: 10.1038/oby.2000.37. [DOI] [PubMed] [Google Scholar]
- 41.Furnham A, Badmin N, Sneade I. Body image dissatisfaction: gender differences in eating attitudes, self-esteem, and reasons for exercise. J Psychol. 2002 Nov;136(6):581–596. doi: 10.1080/00223980209604820. [DOI] [PubMed] [Google Scholar]
- 42.Demarest J, Allen R. Body image: gender, ethnic, and age differences. J Soc Psychol. 2000 Aug;140(4):465–472. doi: 10.1080/00224540009600485. [DOI] [PubMed] [Google Scholar]
- 43.Ford ES, Moriarty DG, Zack MM, et al. Self-reported body mass index and health-related quality of life: findings from the Behavioral Risk Factor Surveillance System. Obes Res. 2001 Jan;9(1):21–31. doi: 10.1038/oby.2001.4. [DOI] [PubMed] [Google Scholar]
- 44.Jia H, Lubetkin EI. The impact of obesity on health-related quality-of-life in the general adult US population. J Public Health (Oxf) 2005 Jun;27(2):156–164. doi: 10.1093/pubmed/fdi025. [DOI] [PubMed] [Google Scholar]


