Abstract
Background
We tested whether an educational video on the goals of care in advanced cancer (life-prolonging, basic or comfort care) can help patients understand these goals and impact preferences for resuscitation.
Methods
Survey of 80 advanced cancer patients before and after viewing the video. Outcomes included changes in goals-of-care preference and knowledge, and consistency of preferences with code status.
Results
Before viewing the video, 10 patients (13%) preferred life-prolonging care; 24 (30%) basic care; and 29 (36%) comfort care; 17 (21%) were unsure. Preferences did not change after the video: 9 (11%) chose life-prolonging care; 28 (35%) basic care; 29 (36%) comfort care; and, 14 (18%) were unsure (p=0.28). Compared to baseline, after the video presentation more patients did not want CPR (71 vs 61%, p=0.03) or ventilation (79 vs 67%, p=0.008). Knowledge about goals of care and likelihood of resuscitation increased post-video (p<.001). Of the patients who did not want CPR or ventilation after the video augmentation, only 4 (5%) had a documented DNR order in the medical record (kappa statistic −0.01; 95% CI −0.06 – 0.04). Acceptability of the video was high.
Conclusion
Patients with advanced cancer did not change care preferences after viewing the video, but fewer wanted CPR or ventilation. Documented code status was inconsistent with patient preferences. Patients were more knowledgeable after the video, found the video acceptable, and would recommend it to others. Video may enable visualization of “goals of care,” enriching patient understanding of worsening health states and better informing decision-making.
Keywords: Decision-Making, video decision aids, end-of-life decision-making, advanced cancer, advance care planning, code status, resuscitation, preferences
Introduction
Advance care planning (ACP) involves planning with patients for future medical care in situations where the patient may not be able to imagine future health states and medical care.1, 2 ACP usually includes a conversation regarding future health states and elucidation of the goals of care, which may lead to documentation of patient preferences in the medical record or the completion of an advance directive (e.g., a living will or designating a health care proxy).1, 2 The flaws of current methods of ACP are well documented3, 4, including concerns regarding the fundamental premise of ACP, which is that patients can accurately imagine future disease states that are often troubling.5
The current ACP model entails clinicians verbally communicating information about a condition and then asking patients what they would want in the given scenario.6 Central to this process is the ability to imagine oneself as a part of that scenario and use one’s value system to develop preferences for care. Patients are encouraged to document whether they would want mechanical ventilation or other life-prolonging interventions, but most patients have little knowledge of what these interventions entail.5 Thus, there is growing recognition that a new model of ACP is needed to more effectively elicit a patient’s goals of care in particular future health states. One potential remedy is the use of decision aids.
Over the last decade, decision support tools have been developed to help patients make more informed decisions by clarifying benefits and risks for a wide variety of medical interventions.7–10 More than 500 decision support tools have been developed, including 12 videos.10 An increasingly utilized healthcare information technology, video can improve decision-making by providing visual information that captures complex medical and emotional scenarios.11, 12 Video can help patients understand their medical options and clarify their preferences by reinforcing the goals-of-care discussion with the use of realistic images, something that is lacking in verbal descriptions.7–10, 13–15 However, to the best of our knowledge, few video support tools have focused on end-of-life communication in advanced cancer.10
In our previous work, we demonstrated that a video of the goals of care in advanced cancer improved understanding and decision-making in a small group of patients with advanced brain cancer.16 This work was limited by studying only one type of cancer, and it did not compare patients’ stated preferences to their documented code status. We were interested in extending this work to: 1. see the influence of the video on patients with a diversity of advanced cancers; 2. explore the effect of reinforcing a verbal description with the video on overall knowledge and CPR/ventilation preferences; and, 3. compare patients’ stated preferences after watching the video to their documented code status.
We hypothesized that supplementing verbal discussions with visual images would change the choices for overall care of patients with advanced cancer in the event they were critically ill. Additionally we hypothesized that reinforcing discussions with visual images would improve overall knowledge regarding the decision-making process and would lead to preferences against the use of CPR and ventilation. Finally, we were also interested in comparing patients’ stated preferences regarding CPR/ventilation after watching the video to their documented code status in the medical record. We completed a before and after trial to study whether a goals-of-care video would shape the choices made by patients with advanced cancer about their preferences for future medical care.
Methods
Participants
Study participants were recruited from the ambulatory oncology practices affiliated with Memorial Sloan-Kettering Comprehensive Cancer Center, a quaternary academic medical center specializing in the care of patients with cancer. All English-speaking patients with advanced cancer returning to see an oncologist were eligible to participate. Patients were eligible if they had terminal, progressive cancer with poor prognosis and limited/poor response to usual treatment algorithms, and whose treatment intent is palliative. The terms terminal, progressive, poor prognosis, palliative intent and limited/poor response were judged by the patient’s oncologist (and not by the research assistant or consenting professional).
Oncologists were contacted by e-mail during each week of the study to identify patients meeting the above eligibility criteria. Once a potential subject was identified, the oncologist would introduce the study to the patient after the patient’s visit. Patients who agreed to participate were then referred to the study research assistant who further explained the study and obtained informed consent. If family members were present with the patient, they were allowed to remain during the interview and view the video, but were asked not to make decisions for the patient.
Potential participants were screened with the Folstein mini-mental state examination (MMSE)17, which has possible score range of 0–30, with scores less than 25 indicative of cognitive impairment. Patients were ineligible if they scored < 25 on the MMSE or were deemed to be in a psychological state not appropriate for end-of-life discussions by the treating clinician. Interviews were conducted primarily by A.N.B. from July 1, 2009-June 30, 2010. The hospital’s institutional review board approved the study and all participants provided written informed consent.
Design
A structured verbal questionnaire was designed following a review of the ACP and oncology literature and in consultation with experts in oncology, palliative care, medical ethics and decision-making. An overview of the study design is shown in Figure 1.
Figure 1.
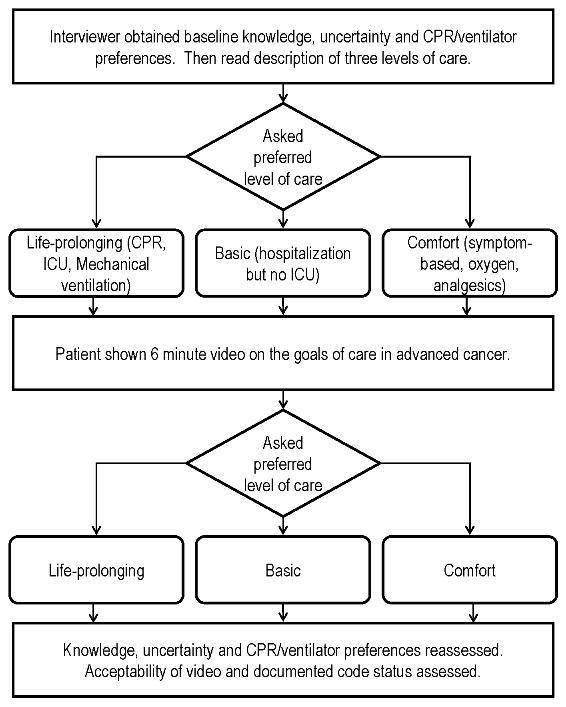
Overview of the study design.
After informed consent was obtained, participants had a baseline assessment to gather socio-demographic data, knowledge about goals-of-care choices, and individual choices for CPR and ventilation. The socio-demographic data included age, race, gender, religion, level of education, marital status, and self-reported completion of an advance directive. The knowledge measurement included six questions, five true/false queries and one multiple-choice item, that were intended to measure the participants’ understanding of the various choices of health care in the advanced stages of cancer (Table 1). Overall scores ranged from 0–6, with higher scores representing more knowledge of the choices of medical care, and were used in our previous work.16 Participants were queried regarding whether or not they wished to have CPR attempted or to be placed on a breathing machine.
Table 1.
Knowledge assessment questionnaire used at baseline and after viewing the video (one point per correct answer, score range 0–6).
| Knowledge Assessment Questionnaire |
|---|
| True or False: |
| 1. Cardiopulmonary resuscitation or CPR is a medical procedure that is done on patients whose heart stops beating in an attempt to restart their heart. (True) |
| 2. Most cancer patients that get CPR in the hospital survive and get to leave the hospital. (False) |
| 3. Most cancer patients who survive CPR and being placed on a breathing machine have very few complications from these procedures. (False) |
| 4. Comfort care is a type of medical care that can only be provided for cancer patients living in hospice. (False) |
| 5. Once you tell your doctor what kind of medical care you want if your cancer becomes very advanced, you cannot change your wishes in the future. (False) |
|
Multiple Choice: 6. How many cancer patients that get CPR in the hospital survive and get to leave the hospital?
|
All participants were then read a verbal description of the three choices of health care available in advanced cancer: life-prolonging care, basic medical care, and comfort care. The choices of medical care were created by reviewing the ACP literature and then critiqued by ten oncologists in a systematic review process. Explanations for each of the choices for medical care were provided as follows: life-prolonging care attempts to sustain life regardless of cost and features all potential medical interventions including CPR, breathing machines, and medical care in the ICU. Basic medical care proposes to sustain physical and cognitive functions and features interventions such as hospitalization and intravenous medicines, but does not include CPR, breathing machines, and medical care in the ICU. Comfort care intends to maximize comfort and relieve symptoms, and usually involves medicines to ease symptoms but would not normally include being admitted to the hospital.
Participants were then asked to select which level of care (life-prolonging, basic, or comfort care) they would prefer if they became critically ill. Participants unable to choose a category were recorded as “not sure.”
Participants then viewed a six-minute video portraying the three choices of health care in advanced cancer. The video was displayed on a laptop computer. The definitions of the three levels of health care were the same as those used in the verbal description, but also included visual images of the choices. For example, life-prolonging care scenes included an ICU with a patient on a ventilator being tended to by nursing staff. Additional images included a simulated code with physicians depicting CPR and intubation, and physicians administering various intravenous medicines. Visual scenes to portray basic medical care included a patient receiving oral medicines, scenes from an inpatient ward service, and a patient receiving oxygen. The video portrayal of comfort care used images of a patient on home hospice care receiving medicines for pain, a patient at home receiving supplemental oxygen with a nasal cannula, and a medical assistant helping a patient with self-care.
The creation of the video followed a systematic approach, starting with a review of the ACP literature in advanced cancer. The video’s overall design was reviewed for appropriateness and accuracy by ten doctors specializing in cancer, three ICU physicians, three experts in palliative medicine, three experts in bioethics and two decision-making experts using an iterative process. The film was created without using stage directions or special effects to impart a realistic film style known as cinema verite.18 The overall designing and creation of the film was done by the principal investigator (A.E.V.) using standardized filming criteria.19
After viewing the video, all participants were again asked to choose which category of care they would prefer if they became critically ill with advanced cancer (life-prolonging, basic, or comfort care). Participants unable to choose a level of medical care were recorded as “not sure.”
Participants were again asked the knowledge questions as well as whether they would want CPR or ventilation attempted. Finally, we measured the perceived value of the video by asking subjects to rate on a four-point scale whether they were comfortable viewing the video, if they would recommend the video to others, and if they found the video helpful in their understanding of their choices. All data were collected in a private quiet room with the aid of a structured script.
For all subjects, whether or not they had a DNR order documented in their medical record prior to viewing the video was determined by chart abstraction.
Analysis
Participant characteristics and outcomes were described using proportions for categorical variables, and means and standard deviations (SD) for continuous variables. The primary outcome measure was change in the level of care chosen. Additional measures included change in knowledge compared to baseline and change in CPR/ventilator preferences compared to baseline. We were also interested in subjects’ ratings of the visual aid in terms of comfort, utility, and helpfulness. Finally, we compared stated preferences for CPR/ventilator after viewing the video to the code status documented in the medical record prior to viewing the video.
Changes in levels of care elected by participants before and after viewing the video were analyzed with McNemar’s test for situations involving more than a binary outcome.20 Changes in knowledge scores from baseline to post-intervention were compared between the two groups using two-sample t-tests. Preferences for pre-intervention CPR/ventilation compared to baseline were compared using exact χ2 tests.
Finally, kappa statistics were used to summarize the agreement between a stated post intervention preference regarding CPR/ventilation and documentation of DNR orders in the medical record prior to viewing the video. A two-sided p value <.05 was considered statistically significant for all analyses. Data were analyzed using SAS software, version 9.2 (SAS Institute Inc., Cary, NC).
Results
A total of 179 eligible patients were screened for participation in the study of whom 86 (48.0%) agreed to participate. The most often cited reason for non-participation was lack of interest. Four participants withdrew due to lack of time to complete the survey. Two participants were disqualified, one due to a recruitment error and another at the request of a spouse, leaving a total of 80 participants. The characteristics of this group are shown in Table 2. Most of the patients were male (72.5%), white (91.3%), highly educated (83.7% some college or higher), and had an advance directive (75.0%). Prostate cancer was the most common type of cancer (45% of participants), followed by melanoma (18.8%). The average knowledge score at baseline was 2.8 (range 0–6).
Table 2.
Baseline characteristics of subjects
| Characteristics | Total N = 80 |
|---|---|
| No. (%) | |
|
| |
| Age, years | |
| Mean (SD) | 65 (12) |
| Range | 36–89 |
|
| |
| Gender | |
| Female | 22 (27.5) |
|
| |
| Race | |
| White | 73 (91.3) |
| Black | 5 (6.3) |
| Other | 2 (2.4) |
|
| |
| Education | |
| High School or lower | 13 (16.3) |
| Some college / tech.school or higher | 67 (83.7) |
|
| |
| Religious Affiliation | |
| Christian (non-Catholic) | 14 (17.6) |
| Catholic | 34 (42.5) |
| Jewish | 13 (16.3) |
| Other | 19 (23.6) |
|
| |
| Marital Status | |
| Never married | 5 (6.3) |
| Married / with partner | 66 (82.5) |
| Divorced | 2 (2.5) |
| Widowed | 5 (6.3) |
| Missing | 2 (2.4) |
|
| |
| Advance Directive* | |
| Yes | 60 (75.0) |
|
| |
| Type of Cancer | |
| Prostate | 36 (45.0) |
| Melanoma | 15 (18.8) |
| Pancreatic | 8 (10.0) |
| Breast | 6 (7.5) |
| Lymphoma | 4 (5.0) |
| Leiomyosarcoma | 2 (2.5) |
| Other | 9 (11.3) |
|
| |
| Desire CPR at baseline | |
| No | 49 (61.3) |
|
| |
| Desire Ventilation at baseline | |
| No | 54 (67.5) |
|
| |
| Knowledge Score at baseline** | |
| Mean (SD) | 2.8 (0.9) |
Abbreviations: CPR – Cardiopulmonary resuscitation.
Advance Directive included those subjects having designated a health-care proxy or having completed a living will, or both.
Knowledge score range (0–6), higher score indicates more knowledge.
After hearing a verbal description of the three levels of medical care in advanced cancer, 10 (13%) participants desired life-prolonging care; 24 (30%) chose basic care; 29 (36%) preferred comfort care; and 17 (21%) were unsure of their preferences. Subject preferences did not change significantly after viewing the video: 9 (11%) subjects desired life-prolonging care; 28 (35%) chose basic care; 29 (36%) of the subjects chose comfort care; and, 14 (18%) were unsure of their preferences (p=0.28) (Figure 2).
Figure 2.
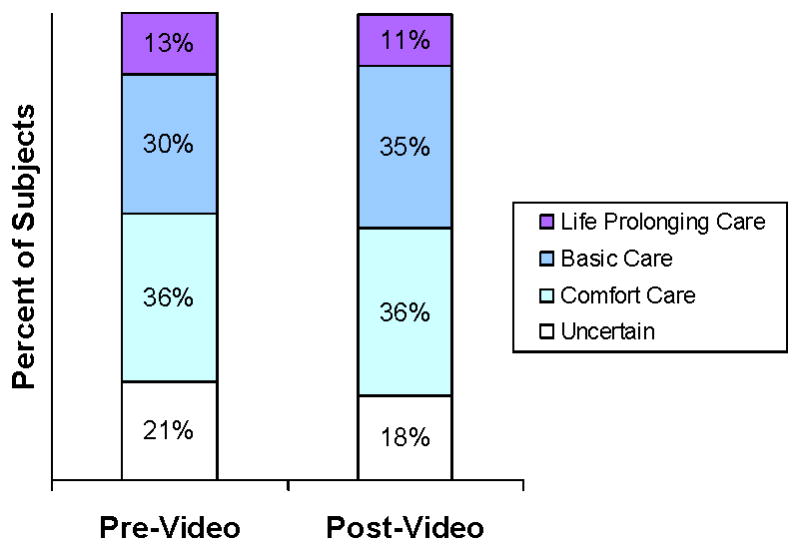
Distribution of patient preferences for goals of care after hearing a verbal description (pre-video) and after viewing the video (post-video).
Participants significantly improved their knowledge scores after the video compared to baseline (mean change 1.6, SD 0.95; p<.001).
Preferences regarding CPR and ventilation also changed significantly after the video augmentation. At baseline, 49 (61%) participants did not want CPR; after the video augmentation, 57 (71%) preferred not to have CPR (p=0.03) (Figure 3). In regards to ventilation, 54 participants (67%) did not want ventilation at baseline; 64 (79%) did not want ventilation after hearing the verbal description and watching the video (p=0.008) (Figure 4).
Figure 3.
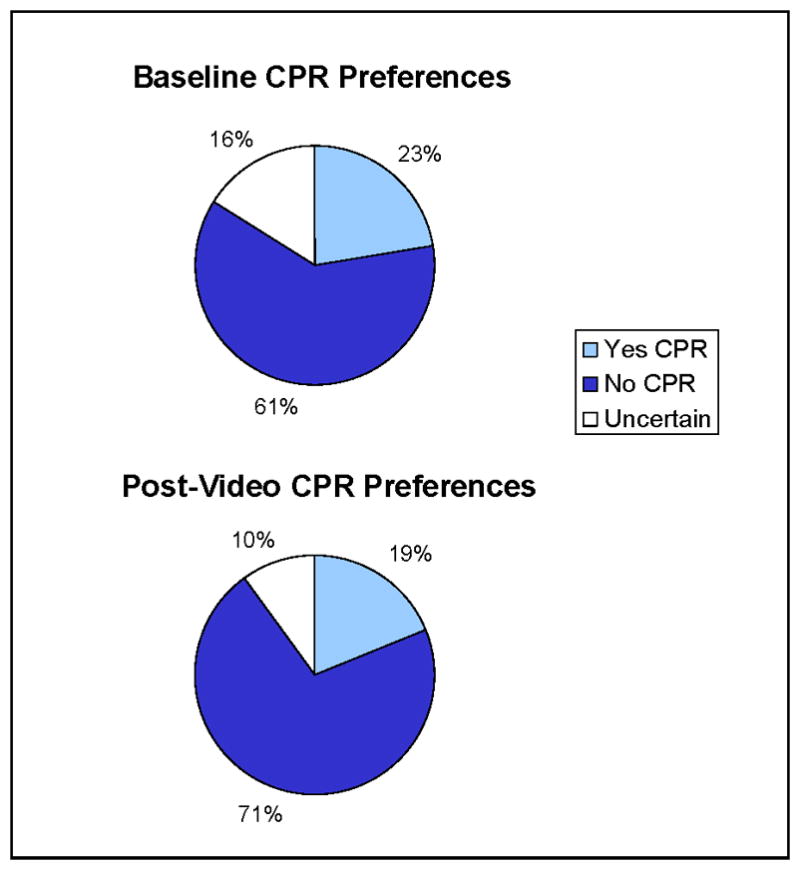
Distribution of preferences regarding CPR after hearing a verbal description (pre-video) and after viewing the video (post-video) (p=.03).
Figure 4.
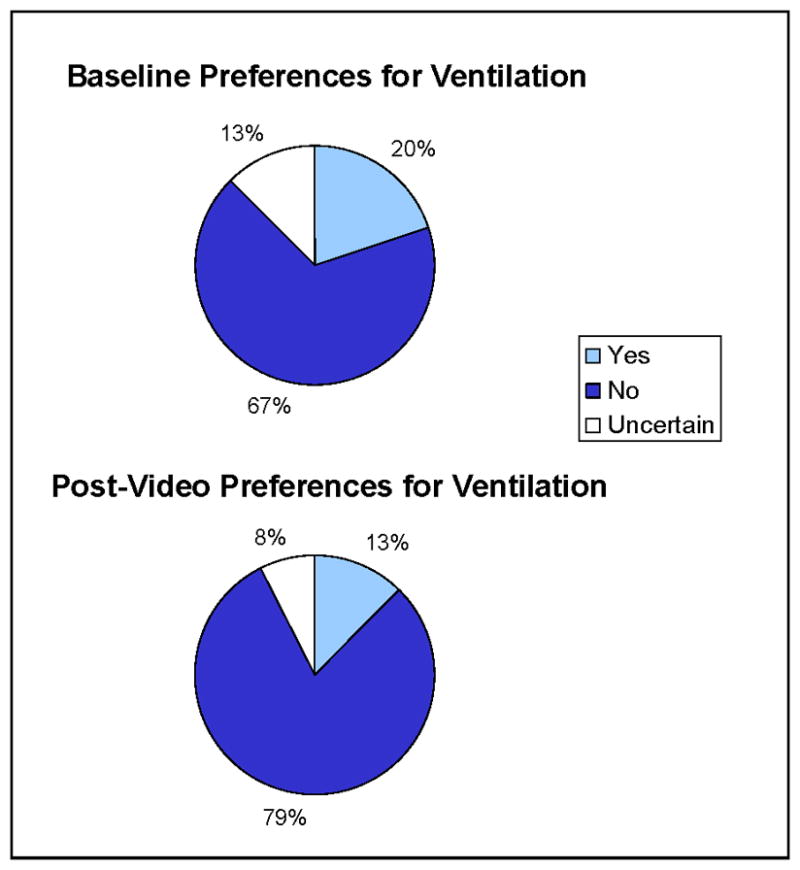
Distribution of preferences regarding ventilation after hearing a verbal description (pre-video) and after viewing the video (post-video) (p=.008).
The video was highly acceptable to the participants: 64 (80%) were either “very” or “somewhat” comfortable watching the video; 61 (76%) would “definitely” or “probably” recommend the video to other cancer patients; and, 51 (64%) found the video either “very” or “somewhat” helpful.
Discrepancy existed between participants’ stated preferences against CPR or ventilation after the video augmentation and their documented code status prior to the survey. Of the participants who did not want CPR or ventilation after the video augmentation, only 4 (5%) had a documented DNR order in the medical record (kappa statistic −0.01; 95% CI −0.06 – 0.04).
Discussion and conclusion
Discussion
Participants with advanced cancer did not significantly change their preferences for life-prolonging, basic medical or comfort care after watching the video compared to a verbal description of these goals of care. Participants did, however, change their preferences for CPR and ventilation after watching the video augmentation, and were more knowledgeable about advance care planning. Notably, participants who stated a preference against CPR or ventilation after the video were highly unlikely to have a DNR order in the medical record. Overwhelmingly, participants were comfortable watching the video and would recommend it to others. Video decision aids supplementing advance care planning discussions may play a significant role in helping patients with advanced cancer make more informed end-of-life decisions.
An important factor in ACP is the patient’s ability to realistically imagine and comprehend future goals of care. This usually requires envisioning a health state that may be difficult to imagine for some patients, such as being attached to a ventilator in the last moments of life. Watching a video may provide details not necessarily communicated by a provider’s verbal discussion. At baseline, a significant number of patients were uncertain about their preferences for CPR or ventilation. After viewing the video and compared to baseline, many subjects had more knowledge about their decision and were more likely to prefer not to have CPR or ventilation. Comparing knowledge and preferences after the video augmentation simulates how video decision support tools are intended to reinforce and supplement patient-doctor discussions. The fact that many subjects would recommend the video to others and found the video helpful lends support for the informational value of visual media.
Often, ACP conversations rely solely on oral communication to provide information regarding future health states. The supplementing of ACP discussions with visual images may have significant clinical implications since patients sometimes incorrectly imagine future health states.21 Innovative models of ACP must make sure that the media used to educate patients about their options correctly depict future health states and interventions. A more thorough comprehension of future health states with visual images allows patients to visualize and better understand their options.
Delivery of end-of-life medical care to patients with advanced cancer that is consistent with their stated preferences is a critical component of high-quality medical care. Our study suggests that the present modality of ACP discussions for complex decision-making at the end of life is often inadequate and may leave patients with inaccurate impressions. Tools such as video decision aids can empower and inform patients with advanced cancer as they deliberate about complicated issues at a vulnerable time in their medical trajectories.
Our study examined the expressed wishes of patients and compared them to documented code status and found a profound lack of correlation. Video decision aids may be a feasible and effective approach towards ascertaining the goals of care; however, our findings also demonstrate that ascertainment of goals of care may not be enough, as steps must also be taken to translate those wishes into a medical order (e.g. DNR orders). Lack of correlation between patients’ desires for comfort-oriented care at the end of life and their documented orders in the medical record should be considered a medical error no different from missing documentation of allergies since this lack of correlation may lead to unwanted and tragic outcomes.
Our study has some limitations. Visual images may be edited to steer patients toward a particular decision. We attempted to avoid bias in the creation of the video by including a variety of experts in the review of the film and using the cinema verité style of documentary film-making that favors realistic scenery over staged directions.18 Nevertheless, using a visual medium such as film can introduce aesthetic biases.
Our trial did not study additional film clips that changed characteristics of the people filmed, such as gender or race. Additionally, our before and after study design did not study the influence of the film in isolation. We also did not include longer versions of the oral description of the choices of medical care. Rather, we hoped to simulate realistic ACP conversations that occur in practice, which focus on brevity and the broad levels of medical care.
Additionally, our participants were recruited from one quaternary medical center in New York City that specializes in the care of patients with cancer and included primarily highly educated male patients with prostate cancer, a unique population reflective of the large numbers of patients with prostate cancer referred to Memorial Sloan-Kettering Comprehensive Cancer Center. Our patients did not include two of the leading causes of death from cancer, lung or colon cancer. Attitudes towards the use of video and preferences of patients with advanced cancer may differ by cancer type, geographic location, education and type of institution. Finally, the majority of participants already had an advance directive and had likely considered questions regarding their overall goals of care prior to seeking help at a highly specialized institution that focuses on cancer care. A greater impact might have been seen had the intervention been presented to patients who had not yet formulated an advance directive.
Our use of visual images to depict the goals of medical care may enhance patients’ understanding of their options beyond that provided by oral ACP discussions. Future studies using the visual medium for ACP include trials that study whether patients actually document their choices in advance directives after watching the video, as well as following the stability of patients’ preferences longitudinally since many of the patients exposed to the video may make very different decisions in the future as a result of the video. Additional studies might also include use of the video earlier in the disease process since ACP discussions are ongoing and not simply a one-time discussion.
The visual medium offers a powerful aid for providers to ground ACP discussions. Issues surrounding the creation of these films, such as how to design them and who should approve them, must be carefully examined prior to the routine use of visual decision aids to other diseases. Deliberation among patients, families, doctors, and film-makers is an initial step towards addressing these important factors.
Conclusion
Involving cancer patients in ACP discussions surrounding care at the end of life respects their autonomy, but requires that providers offer patients the tools with which to make fully informed decisions. The use of video decision aids to supplement verbal descriptions of the goals of care is one powerful means to better inform patients. The use of video decision aids is palatable to patients, increases their understanding of their options, and has the potential to improve the quality of end-of-life care.
Acknowledgments
We would like to thank Patricia Agre, RN, EdD, Susan Holland, MA, Matthew Fury, MD, David Solit, MD, Dana Rathkopf, MD, Ethan Basch, MD, Heather Landau, MD and David Kissane, MD of the Memorial Sloan Kettering Cancer Center for their contributions to patient recruitment.
Funding: The project described was supported by Award Number R21CA139121 from the National Cancer Institute. Dr. Volandes was also supported by grant number K08HS018780 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, the Agency for Healthcare Research and Quality, or the National Institutes of Health.
Footnotes
Financial disclosures statement: Dr. Volandes is on the Board of the Nous Foundation, Inc., a non-profit foundation that disseminates educational videos. Dr. Volandes has no financial interest in and receives no payment from the Foundation. No financial disclosures were reported by the other authors.
References
- 1.Emanuel LL, Danis M, Pearlman RA, Singer PA. Advance care planning as a process: structuring the discussions in practice. J Am Geriatr Soc. 1995;43:440–446. doi: 10.1111/j.1532-5415.1995.tb05821.x. [DOI] [PubMed] [Google Scholar]
- 2.Gillick MR. Advance care planning. N Engl J Med. 2004;350:7–8. doi: 10.1056/NEJMp038202. [DOI] [PubMed] [Google Scholar]
- 3.Hahn ME. MSJAMA. Advance directives and patient-physician communication. JAMA. 2003;289:96. doi: 10.1001/jama.289.1.96. [DOI] [PubMed] [Google Scholar]
- 4.Hawkins NA, Ditto PH, Danks JH, Smucker WD. Micromanaging death: process preferences, values, and goals in end-of-life medical decision making. Gerontologist. 2005;45:107–117. doi: 10.1093/geront/45.1.107. [DOI] [PubMed] [Google Scholar]
- 5.Tulsky JA, Fischer GS, Rose MR, Arnold RM. Opening the black box: how do physicians communicate about advance directives? Ann Intern Med. 1998;129:441–449. doi: 10.7326/0003-4819-129-6-199809150-00003. [DOI] [PubMed] [Google Scholar]
- 6.Finucane TE, Shumway JM, Powers RL, D’Alessandri RM. Planning with elderly outpatients for contingencies of severe illness: a survey and clinical trial. J Gen Intern Med. 1988;3:322–325. doi: 10.1007/BF02595788. [DOI] [PubMed] [Google Scholar]
- 7.Barry MJ. Involving patients in medical decisions: how can physicians do better? Jama. 1999;282:2356–2357. doi: 10.1001/jama.282.24.2356. [DOI] [PubMed] [Google Scholar]
- 8.Barry MJ. Health decision aids to facilitate shared decision making in office practice. Ann Intern Med. 2002;136:127–135. doi: 10.7326/0003-4819-136-2-200201150-00010. [DOI] [PubMed] [Google Scholar]
- 9.Woolf SH, Chan EC, Harris R, et al. Promoting informed choice: transforming health care to dispense knowledge for decision making. Ann Intern Med. 2005;143:293–300. doi: 10.7326/0003-4819-143-4-200508160-00010. [DOI] [PubMed] [Google Scholar]
- 10.O’Connor AM, Stacey D, Entwistle V, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2003:CD001431. doi: 10.1002/14651858.CD001431. [DOI] [PubMed] [Google Scholar]
- 11.Volandes AE, Paasche-Orlow MK, Barry MJ, et al. Video decision support tool for advance care planning in dementia: randomised controlled trial. BMJ. 2009;338:b2159. doi: 10.1136/bmj.b2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Volandes AE, Lehmann LS, Cook EF, Shaykevich S, Abbo ED, Gillick MR. Using video images of dementia in advance care planning. Arch Intern Med. 2007;167:828–833. doi: 10.1001/archinte.167.8.828. [DOI] [PubMed] [Google Scholar]
- 13.Entwistle V. The potential contribution of decision aids to screening programmes. Health Expect. 2001;4:109–115. doi: 10.1046/j.1369-6513.2001.00141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Molenaar S, Sprangers MA, Postma-Schuit FC, et al. Feasibility and effects of decision aids. Med Decis Making. 2000;20:112–127. doi: 10.1177/0272989X0002000114. [DOI] [PubMed] [Google Scholar]
- 15.Estabrooks C, Goel V, Thiel E, Pinfold P, Sawka C, Williams I. Decision aids: are they worth it? A systematic review. J Health Serv Res Policy. 2001;6:170–182. doi: 10.1258/1355819011927431. [DOI] [PubMed] [Google Scholar]
- 16.El-Jawahri A, Podgurski LM, Eichler AF, et al. Use of video to facilitate end-of-life discussions with patients with cancer: a randomized controlled trial. Journal of Clinical Oncology. 2010;28:305–310. doi: 10.1200/JCO.2009.24.7502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 18.Grant BK, Sloniowski J. Documenting the documentary: close readings of documentary film and video. Detroit: Wayne State University Press; 1998. [Google Scholar]
- 19.Gillick MR, Volandes AE. The Psychology of Using and Creating Video Decision Aids for Advance Care Planning. In: Lynch TE, editor. Psychology of Decision Making in Medicine and Health Care. New York, NY: Nova Science Publishers; 2007. pp. 193–206. [Google Scholar]
- 20.Bowker AH. Bowker’s test for symmetry. J Am Stat Assoc. 1995;43:572–574. doi: 10.1080/01621459.1948.10483284. [DOI] [PubMed] [Google Scholar]
- 21.Ubel PA, Loewenstein G, Schwarz N, Smith D. Misimagining the unimaginable: the disability paradox and health care decision making. Health Psychol. 2005;24:S57–62. doi: 10.1037/0278-6133.24.4.S57. [DOI] [PubMed] [Google Scholar]


