Abstract
Background:
Fight against human immunodeficiency virus (HIV) is incomplete without addressing problems associated with difficult diagnosis of tuberculosis in HIV-Tuberculosis coinfected patients. Chest X-ray is a primary tool to evaluate tuberculosis in HIV.
Aim:
To assess and compare various radiological patterns of pulmonary tuberculosis in HIV patients and compare these patterns in relation to CD4 counts.
Materials and Methods:
Prospective cohort study was conducted in a tertiary hospital in South India from September 2009 to July 2011 with 200 HIV positive patients. WHO guidelines were used for diagnosis of HIV and tuberculosis.
Results:
27% of the patients had sputum positive pulmonary tuberculosis, with higher incidence (33%) among CD4 less than 200 as compared to CD4 more than 200 (14%). Infiltration (39%) followed by consolidation (30%), cavity (11%), and lymphadenopathy (9%) seen with CD4 less than 200. Infiltration (37.5%) followed by cavity (25%) and miliary (25%) with CD4 above 200. Bilateral (68.5%) and mid and lower zones or all zone involvement more commonly seen.
Conclusion:
In patients with CD4 lower than 200 noncavitory infiltration and consolidation predominated. Involvement of lungs was atypical; diffuse or mid and lower zone involvement than classical upper lobe involvement. A high index of suspicion is necessary for the accurate and timely diagnosis of tuberculosis in HIV positive patients.
Keywords: CD4, HIV/AIDS, tuberculosis
Introduction
India is home to approximately 2.5 million people living with human immunodeficiency virus (HIV), the third largest number of cases of any country in the world, and is recognized as the source of increasing HIV prevalence among its South Asian neighbors. Recently released national HIV prevalence estimates for India indicate that 0.22% of women and 0.36% of men aged 15–49 years are infected.[1–3]
About 70% of the individuals affected with HIV usually have one or more respiratory illnesses during the course of their HIV disease.[4] Pulmonary complications of the HIV infection study demonstrated that respiratory symptoms are a common complaint among the HIV-infected individual and increasingly frequent as CD4 counts declined to less than 200 cells/mm3.[5] Respiratory symptoms may result from a wide spectrum of pulmonary illness that includes HIV-related opportunistic infections and neoplasm.
Chest radiography is the corner stone of the diagnostic evaluation of respiratory symptoms in HIV infected patients, because each of the HIV-related opportunistic infections and neoplasm has a characteristic radiographic presentation, the radiograph (combined with information delivered from history and physical examination and selected lab tests) can narrow the diagnostic possibilities and suggest a diagnostic approach. Tuberculosis can present with a variety of chest radiographic findings, including upper lung zone infiltrates often with cavitations, middle or lower zone consolidation mimicking bacterial pneumonia, miliary, nodule(s), pleural effusion, and intrathoracic adenopathy. In case of tuberculosis, noncavitory infiltrates and intrathoracic adenopathy increased as the CD4 counts decreased.[5,6]
A wide clinicoradiological spectrum of tuberculosis was seen among HIV patients, in consonance with their varying immune status. With the conventional sputum positivity and tuberculin test not providing an adequate diagnostic help, familiarity with the clinicoradiological spectrum of tuberculosis and coexisting opportunistic infections is absolutely necessary.[7] This study makes an attempt to correlate the chest X-ray and CD4 counts as it will help in better understanding this deadly duo of HIV and tuberculosis.
Materials and Methods
Confidentiality of the data collected was maintained. Written consent was taken from the patient to be a part of the study. Ethical clearance was obtained from time bound ethics committee.
The present study was done as a prospective cohort study in a tertiary care hospital of South India from August 2009 to July 2011. 100 HIV-positive female patients and 100 HIV-positive males, who satisfy the inclusion criteria, were the subjects of the study. All patients above the age of 18 with confirmed HIV infection as per NACO guidelines were the subjects of the study.
All the HIV-positive patients satisfying the inclusion criteria were registered in the study group. These individuals were subsequently assessed thoroughly as per the protocol. This included detailed clinical history including presenting symptoms, past history, disease diagnosis, and complete physical examination followed by appropriate baseline and specific laboratory tests. The chest radiography was taken for all the patients and detailed evaluation of the radiograph was done. CD4 count was estimated at the same point of time. Sputum AFB stain was carried out to look for pulmonary tuberculosis. Special staining techniques were used when clinically indicated.
Results
Mean age among males was 37.4 years and among females was 35.3 years, respectively. Maximum number of patients belonged to age group of 31–40 years in both males and females, 55% in males and 63% in females, respectively. In the age group of 26–30, females were more compared to males (22% females and 13% males), whereas in the age group of 41–50 males were more in number as compared to females – 26% males and 11% females.
80% of males and 88% of females had education up to high school or less. Maximum number of the study population had education up to high school (45% among males and 69% among females). In this study, maximum number of patients belonged to unskilled work group (49% among males and 54% among females), most of them were manual laborers. 25% of females were house wives. Skilled workers included drivers, clerks, and others and males dominate over females in this group, 34% males and 18% females.
Loss of appetite and weight was present among 82% in both groups. 69% of males and 72% of females had fever at the time of presentation. 68% of males and 69% of females also had cough as a predominant symptom.
CD4 at the time of diagnosis: 11% of females had CD4 count of less than 50 in comparison with 1% of males who had CD4 of less than 50. Among CD4 range of 100-150, males (31%) were more compared to females (17%). 71% of males had CD4 less than 200, whereas 65% of females had CD4 less than 200 at the time of diagnosis [Figure 1].
Figure 1.
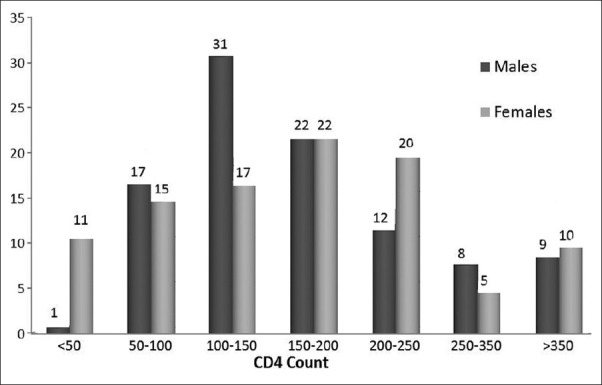
CD4 count at the time of diagnosis
HIV and Pulmonary Tuberculosis
Pulmonary tuberculosis was diagnosed with sputum AFB in 54 patients (29 males and 25 females). Various patterns of chest X-ray presentations with respect to CD4 counts as follows. In patients with CD4 of less than 200, infiltration [Figure 2] was seen among 18 (39%) followed by consolidation in 14 (30%). Cavity and cardiomegaly were present in 5 (11%) each. Lymphadenopathy [Figure 3] 4 (9%), Pleural effusion 4 (9%), COPD 4 (9%), and miliary 3 (7%) also seen in lesser number. CD4 of above 200 had infiltration in 3 (37.5%), miliary in 2 (25%), and cavity in 2 (25%) chest radiographs.
Figure 2.
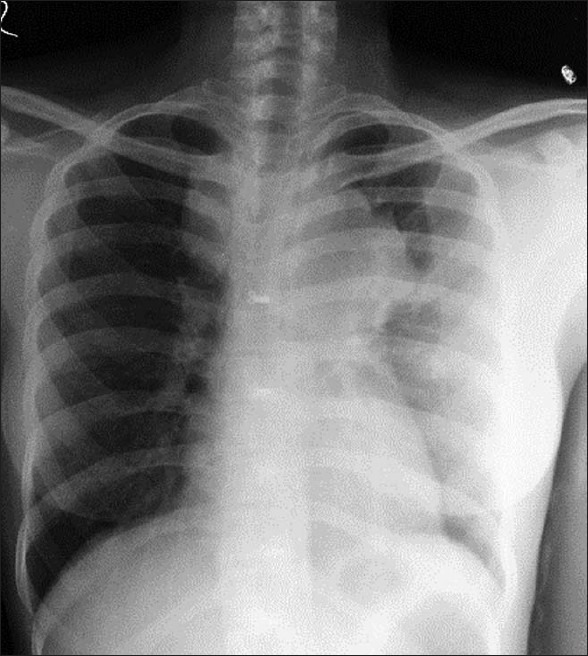
Generalized lymphadenopathy with TB lymphadenitis-CD4 count 110
Figure 3.

Diffuse nodular infiltration in HIV-TB coinfection
Females with sputum-positive pulmonary TB with HIV with CD4 of less than 200 had following findings. Infiltration was seen in 11 (55%), cardiomegaly in 5 (25%), lymphadenopathy in 4 (20%). Consolidation was observed in 3 (15%) and 2 (10%) had cavity. Normal X-ray was seen in one patient. CD4 of above 200 had 2 (40%) cavitatory and infiltration lesion each in chest X-ray. Pleural effusion and miliary mottling was seen among 1 (20%) each. In males with CD4 count of less than 200 with pulmonary TB showed consolidation in 11 (42%) followed by infiltration in 5 (19%). COPD was observed in 5 (15%). cavity, miliary, and pleural effusion were 3 (12%) each in number. CD4 of more than 200 had one (33%) each of consolidation, miliary, infiltration, and pneumothorax each [Figure 4].
Figure 4.
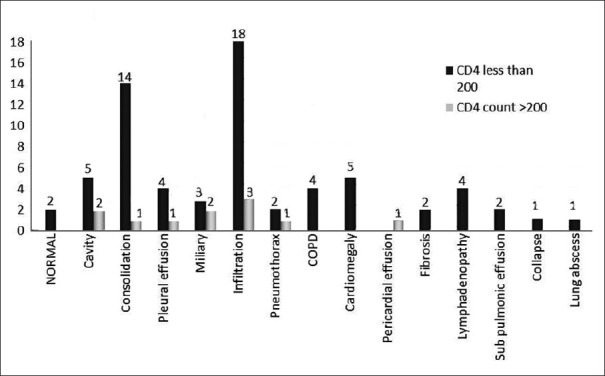
CD4 and chest X-ray correlation of HIV with TB
Tuberculosis-atypical involvement of lungs in HIV
On the right side, all-zone involvement was observed in 18 (42%) of them, whereas middle and lower lobe involvements were observed in 15 (35%) of the chest radiographs. Upper lobe involvement was seen in 2 (0.05%). On left side, all-zone involvement was seen among 22 (50%) middle and lower were seen in 13 (29.5%) of them. Upper zone involvement was seen in 2 (0.05%).
Among patients with HIV and pulmonary TB coinfection, bilateral lung involvement was observed among 37 (68.5%) of the chest radiographs.
Among patients with CD4 count less than 200, Oral candidiasis was observed among 55.9% patients, pulmonary tuberculosis in 33%, CMV retinitis in 8%, and TB lymphadenitis among 7% of them. Patients with CD4 more than 200 had 14% incidence of pulmonary tuberculosis. Pneumocystis carinii pneumonia was diagnosed among 16% of patients and all had CD4 count less than 200.
Discussion
Tuberculosis, unlike other HIV-associated opportunistic infections, may occur at relatively high levels of CD4 counts, although its frequency markedly increases in patients with more severe immunosuppression HIV-TB cases have been observed to have severe immunosuppression at presentation, with several studies reporting CD4 counts of less than 200.[4] In patients with mild immunosuppression, chest X-ray typically shows upper lobe and/or bilateral infiltrates, cavitation, pulmonary fibrosis, and shrinkage. The clinical picture often resembles postprimary pulmonary tuberculosis, and the sputum smear is usually positive. In severely immunosuppressed patients, the features of the disease are atypical, resembling those of primary tuberculosis. The sputum smear can often be negative and chest X-ray shows interstitial infiltrates, especially in the lower zones, with no features of cavitation and fibrosis. Unilateral or bilateral infiltrates are seen more often in the lower lobes than in the upper lobes and typical cavities are seen in only 25% of patients.[6–8]
In our study, pulmonary tuberculosis was diagnosed with sputum AFB in 54 patients (29 males and 25 females). Various patterns of chest X-ray presentations with respect to CD4 counts as follows. In patients with CD4 of less than 200, infiltration was seen among 18 (39%), followed by consolidation in 14 (30%). Cavity and cardiomegaly were present in 5(11%) each. Lymphadenopathy 4 (9%), pleural effusion 4 (9%), COPD 4 (9%), and miliary 3 (7%) were also seen in lesser number. In a study by Pearlman et al.[9] infiltrates were seen among 52%, lymphadenopathy in 30%, interstitial disease in 27%, pulmonary nodule in 18%, cavity in 7%, and pleural effusion in 7%. Normal X-ray was seen in 9%.
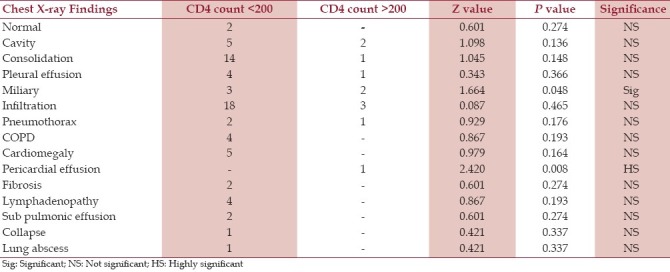
CD4 of above 200 had infiltration in 3 (37.5%), miliary in 2 (25%), and cavity in 2 (25%) chest radiographs. In a study by Pearlman et al.,[9] infiltrates were seen among 67%, lymphadenopathy in 7%, interstitial disease in 17%, pulmonary nodule in 20%, cavity in 20%, and pleural effusion in 10%. Normal X-ray was seen in 3% [Table 1].
Table 1.
Correlation analysis of chest X-ray findings with CD4 count
In another study by Maniar et al.,[10] infiltration was seen among 62.5%, hilar lymphadenopathy in 17.5%, pleural effusion in 16.5%, and consolidation in 7.5%. Pericardial effusion was seen among 3% and miliary shadows in 1.5%.
Chest X-ray abnormalities are even more non-specific in HIV-infected patients than in HIV-negative patients, which may result in under diagnosis. Radiological patterns depend on the level of immunity in the host. Typical pulmonary lesions are seen only in about one third of the HIV-infected patients with clinical tuberculosis.[11] Among patients with HIV and pulmonary TB, we observed that tuberculosis involvement of lungs was atypical as there was all-zone involvement in most of them or middle and lower lobe involvement in the remaining majority.
On the right side, all-zone involvement was observed in 18 (42%) of them, whereas middle and lower lobe involvement in 15 (35%) of the chest radiographs. Upper lobe involvement was seen in 2 (0.05%). On left side, all-zone involvement seen among 22 (50%), middle and lower lobe involvement in 13 (29.5%) of them. Upper zone involvement seen in 2 (0.05%).
Tuberculosis classically involves the upper lobes usually unilaterally. Among patients with HIV and pulmonary tuberculosis coinfection, bilateral lung involvement was observed among 37 (68.5%) of the chest radiographs, suggesting that diffuse involvement is more common in patients with HIV and TB coinfection. In a study by Maniar et al.,[10] in patients with HIV and TB coinfection, upper zone involvement was seen among 3.7%, middle zone involvement among 62.5%, lower zone involvement in 33.8%. Unilateral disease seen among 71.8% and bilateral in 28.2%.
Conclusion
In our study, most common radiological presentation of tuberculosis was parenchymal infiltration followed by consolidation, cavity, cardiomegaly, lymphadenopathy, pleural effusion, COPD, and miliary shadows. In males, consolidation was more common than infiltration. Involvement of lung field in tuberculosis was atypical as evidenced by bilateral lung involvement; middle and lower zone or diffuse involvement. Comparison of CD4 count with chest X-ray revealed miliary shadows and pericardial effusion significantly increased among CD4 less than 200.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Silverman JG, Decker MR, Saggurti N, Balaiah D, Raj A. Intimate partner violence and HIV infection among married Indian women. JAMA. 2008;300:703–10. doi: 10.1001/jama.300.6.703. [DOI] [PubMed] [Google Scholar]
- 2.Summary of findings of the 3rd National Family Health Survey. India NFHS-3. International Institute for Population Sciences and Macro international Inc. 2005-06. [st Accessed on 2011 Dec 15]. Available from: http://www.nfhsindia.org/nfhs3.html .
- 3.Ramachandran R, Swaminathan S, Somasundaram S. Mycobacteremia in tuberculosis patients with HIV infection. Indian J Tuberc. 2002;50:29. [Google Scholar]
- 4.Arora VK. HIV and respiratory system - with special reference to tuberculosis-Indian perspective. J Intern Med. 1997;8:125–7. [Google Scholar]
- 5.Huang L. HIV In site knowledge base chapter. University of California San Francisco. 2009. Jan, [Last Accessed on 2011 Dec 15]. Available from: http://www.hivinsite.ucsf.edu .
- 6.Haung L. Respiratory disease. In: Dolin R, Masur H, Saag MS, editors. AIDS Therapy. 2nd ed. Philadelphia: Churchill Livingstone; 2003. pp. 827–52. [Google Scholar]
- 7.Gold JA, Rom WN, Harkin TJ. Significance of abnormal chest radiograph findings in patients with HIV-1 infection without respiratory symptoms. Chest. 2002;121:1472–7. doi: 10.1378/chest.121.5.1472. [DOI] [PubMed] [Google Scholar]
- 8.Swaminathan S. Clinical presentation and treatment of HIV-TB. Indian J Tuberc. 2002;49:11–16. [Google Scholar]
- 9.Perlman DC, el-Sadr WM, Nelson ET, Matts JP, Telzak EE, Salomon N, et al. Variation of chest radiographic patterns in pulmonary tuberculosis by degree of human immunodeficiency virus-related immunosuppression. Clin Infect Dis. 1997;25:242–6. doi: 10.1086/514546. [DOI] [PubMed] [Google Scholar]
- 10.Maniar JK, Kamath RR, Mandalia S, Shah K, Maniar A. HIV and tuberculosis: Partners in crime. Indian J Dermatol Venereol Leprol. 2006;72:276–82. doi: 10.4103/0378-6323.26723. [DOI] [PubMed] [Google Scholar]
- 11.Sircar AR, Tripathi AK, Choudhary SK, Misra R. Clinical profile of AIDS: A study at a referral hospital. J Assoc Physicians India. 1998;46:775–8. [PubMed] [Google Scholar]


