Abstract
Introduction
The gastrointestinal stromal tumor (GIST) is the most common mesenchymal tumor of the intestinal tract, known to be refractory to conventional chemotherapy or radiation. Its pathogenesis is defined by mutations within the KIT and PDGFRA gene, which constitutively activate KIT and PDGFRA oncoproteins, and serve as crucial diagnostic and therapeutic targets.
Discussion
Besides surgery, therapy with imatinib mesylate, which inhibits KIT kinase activity, represents the other cornerstone for the treatment of GIST. Still, the only curative option for GIST is given after complete surgical removal even in a metastatic setting, but recurrence is common, and the risk can be defined by surgical factors like incomplete resection, intraperitoneal rupture, or bleeding and tumor associated factors like tumor size, mitotic index, or localization.
Conclusion
Consequently, adjuvant therapy with imatinib mesylate or other tyrosine kinase inhibitors is recommended for high-risk patients after complete resection. For unresectable and advanced GIST, a partial response or stable disease can be achieved in about 80% of patients with imatinib mesylate.
Keywords: Gastrointestinal stromal tumor, Imatinib mesylate, Surgical resection
Introduction
Gastrointestinal stromal tumors (GISTs) represent a wide clinical spectrum of tumors with different dignity, which may arise throughout the entire gastrointestinal tract. They are located typically in the submucosa of the stomach and the small and large intestines, although cases arising in the esophagus, greater omentum, and mesenterial adipose tissue have been described. In the early literature, these tumors used to be classified as leiomyomas, cellular leiomyomas, leiomyoblastomas, and leiomyosarcomas [1], but in the 1960s, electron microscopic studies revealed the lack of typical smooth muscle differentiation in some of these gastric tumors [2]. Subsequently, leiomyomas, which did not exhibit ultrastructural characteristics of smooth muscle cells and lacked immunohistochemical features of Schwann cells (i.e., no expression of S-100 protein), were classified as “gastric stromal tumors” by Mazur and Clark in 1983 [3]. Since it has been demonstrated that GIST arise from the interstitial cells of Cajal [4], which are located in the submucosal and myenteric plexus of the gastrointestinal tract, the term GIST is applied to these mesenchymal tumors arising in the submucosa of the gastrointestinal tract marking the beginning of a new era. Consequently, reports published before 1993 dealing with gastric and intestinal smooth muscle tumors largely describe GIST [5–7]. The genetic basis of GIST growth is a mutation of the KIT or PDGFRA gene leading to constitutional activation of receptor tyrosine kinases, which is the driving force behind tumor development. In the following review, the definition, epidemiology, pathogenesis, morphologic and genetic findings, treatment, and prognostic factors of GIST will be discussed.
Literature search and data extraction
First, a PubMed search using different search terms including “gastrointestinal stromal tumors/GIST[S],”was conducted. All available English written articles were read in full length. References were then cross-checked to achieve—to the best of our knowledge—completeness of the reports to be included in this review.
Definition
GISTs usually present as round, sharply demarcated mass lesions arising in the submucosal layer of the gastrointestinal (GI) tract (Fig. 1). They are defined as tumors of the GI tract that are composed of spindle cells, epithelioid, or occasionally pleomorphic mesenchymal cells and mostly express the KIT (CD117, stem cell factor receptor) protein (Fig. 2). GIST have been described to originate from interstitial cells of Cajal [4] or a stem cell-like subset of KIT-positive spindle cells around the myenteric plexus [4, 8, 9]. Most of these tumors are strongly and nearly uniformly KIT positive (70%) and can be histologically subclassified into eight subtypes, mainly of spindle cell, epithelioid, or mixed-type differentiation [10]. Although other tumor entities, such as metastatic melanoma, pulmonary small cell carcinoma, and other types of carcinoma, angiosarcoma, Ewing sarcoma, mastocytoma, and seminoma, may show positive expression of KIT, they are not classified as GIST [11–14]. Furthermore, true smooth muscle tumors (leiomyomas and leiomyosarcomas), schwannomas, and neurofibromas are excluded by the above-mentioned definition. However, some tumors, which apply to the morphological criteria for GIST, do not express KIT. They also typically lack all other marker proteins employed in the differential diagnosis of GIST [CD34, PDGFRA, smooth muscle actin (SMA), desmin and S-100 protein], and the classification of these tumors with a “null-phenotype” is still being discussed. In case of lacking KIT expression, immunohistochemical staining with PKC theta [15], PDGFRA [16], or DOG-1 [17] can be of additional help.
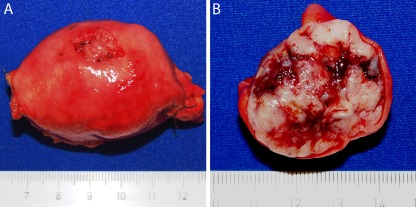
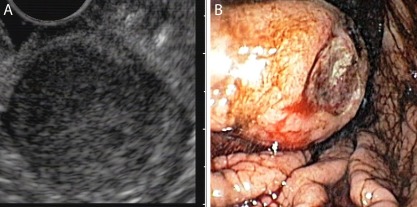
Fig. 1.
Grossly, gastrointestinal stromal tumors (GIST) usually present as round and sharply demarcated submucosal mass lesions throughout the gastrointestinal tract, as in this case, in the wall of the stomach (a). They exhibit a solid, sometimes cystic, fleshy, tan white cut surface with occasional areas of hemorrhage (b) and sometimes ulcerations of the overlying mucosa
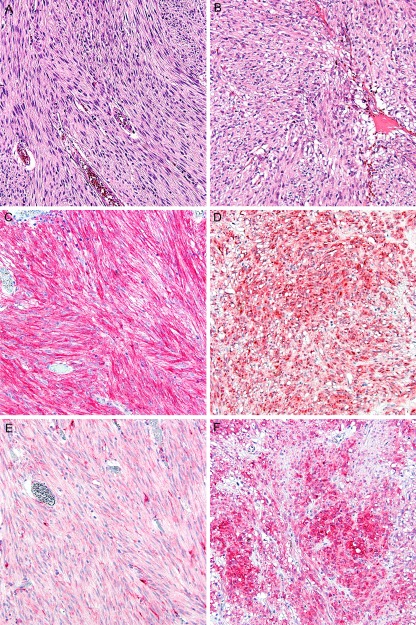
Fig. 2.
On microscopic view, GIST either show spindle cell [a hematoxylin–stain (HE)] or epithelioid differentiation (b), HE, the latter of which being most frequent in gastric GIST. Immunostaining with CD117 (KIT) is characteristically positive in GIST of either differentiation (c spindle cell, d epithelioid). Immunostaining with PDGFRA is typically weaker in spindle cell GIST (e) than in epithelioid GIST (f) (×100)
Epidemiology
The annual incidence of GIST is estimated at 10–20/million, with 20–30% of cases presenting features of metastasis upon first diagnosis. GISTs typically occur in individuals above 50 years of age [18–21] at a median age ranging between 55 and 65 years, including all locations. GIST is very infrequent in children and only rarely develops before the age of 40 years. Some series show equal gender distribution, but others propose a male predominance [14, 18, 22, 23].
GIST are most commonly located in the stomach (60–70%), followed by the small intestine (20–30%), colon and rectum (5%), and esophagus (<5%). Rare cases of primary GIST located in the greater omentum and mesentery have also been reported [24], but in these cases of extragastrointestinal GIST with extensive involvement of the abdominal cavity, the primary site of origin may simply be impossible to determine. GIST may occur sporadically in pediatric cases, but population-based figures on the incidence of GIST in children are not available [25–27]. Only few cases with familial GIST have been reported so far since its first description in 1998 [28–32], and the inheritance is autosomal dominant. In addition to germ line KIT mutations, germ line mutations encoding the succinate dehydrogenase (SDH) subunits B, C, D (SDHB, SDHC, and SDHD) have been identified in familial GIST recently [33].
Furthermore, GIST rarely occurs in association with other tumor syndromes such as neurofibromatosis type 1 [34–36]. Neurofibromatosis-associated GIST are often multiple within the small intestine [34–36]. Aidan Carney first described the association of gastric leiomyosarcoma, extra-adrenal paraganglioma, and pulmonary chondroma, which was subsequently termed Carney triad [37]. In addition, adrenocortical tumors and esophageal leiomyoma were considered components of the triad [38–40] recently. Furthermore, it was suggested to distinguish an inherited tumor syndrome comprising GIST and paragangliomas (Carney–Stratakis syndrome or Carney–Stratakis dyad) from the classic Carney triad [41].
Pathogenesis and genetics
The central events in the pathogenesis of GIST are the exclusive mutations of the KIT and PDGFRA gene. The KIT gene encodes a protein that serves as a receptor for the growth factor stem cell factor, and the intracellular domain contains a tyrosine kinase enzyme, which activates a cascade of activities ultimately causing mitosis. Mutations in the KIT gene lead to uncontrolled activation of the tyrosine kinase site and therefore enhanced cell proliferation [4].
Mutations can be subdivided into primary (i.e., original) and secondary mutations, the latter developing during the treatment with tyrosine kinase inhibitors and causing secondary drug resistance. The most common primary mutations (deletions, point mutations, and duplications) are being observed in exon 11 (juxtamembrane domain) of the KIT gene (Fig. 3). The most common mutations in gastric GIST are duplications in the 3′ region of KIT exon 11, whereas tumors with deletions behave more aggressively than those with point mutations [42]. Furthermore, patients with KIT mutations involving codons 557–558 have an unfavorable prognosis [43]. In gastric GIST, PDGFR-alpha mutations are found in up to 20% [25]. Mutations of the KIT kinase domains (i.e., exon 13, 14, and 17) are very rare, and GIST with such mutations show variable sensitivity to imatinib. Interestingly, secondary mutations usually occur in these KIT kinase domains in patients during or after imatinib treatment and lead to secondary drug resistance. In GIST without KIT mutations, PDGFRA mutations occur with a frequency of approximately 30–40%, predominantly in gastric GIST often leading to primary imatinib resistance [44].
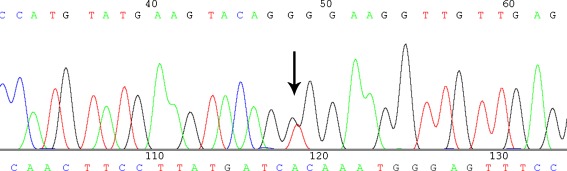
Fig. 3.
Mutational analysis of the KIT and PDGFRA genes has become an important prognostic tool with therapeutic impact as the exemplary point mutation at codon 557 at KIT exon 11, causing the replacement of the amino acid tryptophan by glycine (c.1669T >G;p.W557G) (arrow)
Furthermore, these tumors display typical patterns of chromosomal gains and losses, including losses at 1p, 14q, 15q, and 22q. Tumor site is associated with distinct chromosomal imbalances; for instance, gastric GIST show predominantly losses of 14q, whereas intestinal GIST more frequently exhibit losses of 15q [45].
Taken together, mutational analysis of GIST serves as an important tool not only in the diagnostic procedure but also in the assessment of potential sensitivity and response to the application of tyrosine kinase inhibitors [42, 46, 47].
Biological behavior and prognostic factors
In general, the risk of progression in completely resected primary GIST can be predicted by the combination of mitotic rate, tumor size, and localization (Table 1) [48, 49]. In 2002, Fletcher et al. [49] first proposed a classification for the estimation of the risk of progression taking into account mitotic rate and tumor size (centimeters). This classification was then extended by Miettinen et al. [48] who recognized that also the tumor site played an important role and included this criterion in the risk stratification of GIST in 2006 leading to the current Union for International CancerControl (UICC) classification (Table 2). However, the Miettinen–Lasota classification has been validated in a large dataset, whereas this is not the case for the UICC classification, thus limiting the clinical applicability of the latter.
Table 1.
Risk stratification of malignant GIST according to Miettinen et al. [27]
| Risk of progressiona | |||||
|---|---|---|---|---|---|
| Mitotic rate | Tumor size (cm) | Stomach | Jejunum or leum | Duodenum | Rectum |
| ≤ 5/50 HPF | ≤2 | None | None | None | None |
| >2 ≤ 5 | Very low | Low | Low | Low | |
| >5 ≤ 10 | Low | Moderate | Highc | Highbc | |
| >10 | Moderate | High | |||
| > 5/50 HPF | ≤2 | Noneb | Highb | n.a. | High |
| >2 ≤ 5 | Moderate | High | High | High | |
| >5 ≤ 10 | High | High | Highc | Highc | |
| >10 | High | High | |||
HPF high power fields, n.a. not available due to small number of patients
aDefined as rates of metastases or tumor related death in GIST
bVery small number of cases
cCombined due to small number of cases
Table 2.
UICC classification, seventh edition (2010)
| Mitotic rate | Tumor size (cm) | T | N | M | UICC stage | |
|---|---|---|---|---|---|---|
| Gastric GIST | Intestinal GIST | |||||
| Lowa | ≤2 | 1 | 0 | 0 | IA | I |
| >2 ≤ 5 | 2 | 0 | 0 | IA | I | |
| >5 ≤ 10 | 3 | 0 | 0 | IB | II | |
| >10 | 4 | 0 | 0 | II | IIIA | |
| Highb | ≤2 | 1 | 0 | 0 | II | IIIA |
| >2 ≤ 5 | 2 | 0 | 0 | II | IIIB | |
| >5 ≤ 10 | 3 | 0 | 0 | IIIA | IIIB | |
| >10 | 4 | 0 | 0 | IIIB | IIIB | |
| Any | Any | 1 | 0 | IV | IV | |
| Any | Any | 1 | IV | IV | ||
Staging for intestinal GIST can be applied to GISTs in less common sites, such as oesophagus, colon, rectum and mesentery
a≤5/50 HPF
b>5/50 HPF
GIST arising in the esophagus are very rare [19, 50] and are typically localized in the lower third of the esophagus. The majority of tumors excide 5 cm in size and display >5 mitoses per 50 high power fields (HPF), but due to the limited number of cases with documented long-term follow-up, a definitive risk stratification cannot be defined yet.
In contrast to esophageal GIST, gastric GIST represent a large clinic-pathologically complex group and make up the majority of GIST [21, 51]. Reported tumor size varies from a few millimeters to >40 cm with a mean size of 6 cm in the largest reported series [25]. Gastric GIST often shows a higher frequency of epithelioid morphology and positive immunostaining for PDGFRA than non-gastric GIST [10]. Interestingly, gastric GIST exhibits a better prognosis than small intestinal GIST of comparable size and mitotic rate. Thus, gastric GIST with ≤5 mitoses per 50 HPF and a size of ≤10 cm have a low risk of distant metastases with <5% compared to small and large intestinal GIST, which already show a high risk of progression at the same mitotic rate and size [25]. GIST of 2 to ≤5 cm size and >5 mitoses per 50 HPF located in the stomach show progression in 10–15%, similar to tumors >10 cm but with mitotic rates ≤5/50 HPF.
Only 4–5% of GIST are located in the duodenum [52, 53]. Most of these tumors feature spindle cell differentiation and the prognosis of tumors ≤2 cm with ≤5 mitoses per 50 HPF is excellent. Tumors with a size from >2 to ≤5 cm have a high risk of clinical progression even with ≤5 mitoses per 50 HPF. Patients with duodenal GIST exceeding 5 cm or >5 mitoses per 50 HPFs have a high tumor-related mortality.
The small intestine harbors the second largest group of GIST with a tumor-related mortality up to 50% [27] and a higher rate of malignant behavior than gastric GIST [27]. Small intestinal GIST occur at a median age of 59 years with a male predominance of 55%. In contrast to gastric GIST, intestinal GIST are mostly spindle cell tumors with only 5% of epithelioid morphology. Remarkably, the epithelioid GIST of the small intestine is significantly linked to a bad prognosis and differs morphologically and clinically from gastric epithelioid GIST [27]. Whether this difference results from a different histological subtype or reflects the morphological manifestation of tumor progression is not yet defined.
Only 1–2% of GIST are located in the colon. The prognosis of these tumors can be classified based on mitotic rates into a favorable and unfavorable group [54–56]. GIST of the rectum vary from incidental small tumors to huge tumors, which occupy almost the entire pelvis, and represent 4% of all GIST. Prognosis is again estimated by tumor size and mitotic rate. Only small tumors (<2 cm) with low mitotic rate (<5 per 50 HPF) do not show evidence of clinical progression. A mitotic rate of >5 per HPFs results in a metastatic rate of >50% [57].
Outside the gastrointestinal tract, GIST tumors are rare (<1%), and most of them might represent metastases of GIST located primarily in the gastrointestinum [58]. These tumors are commonly designated as extragastrointestinal GIST (EGIST) [24, 59, 60] and exhibit an overall favorable prognosis [59, 60], which contradicts the view that they might be metastases. However, the available data regarding the prognosis of EGIST are still rather limited. Apart from the greater omentum, the mesenteric tissue and retroperitoneum, few cases of EGIST in the rectovaginal space, urinary bladder, pharynx, and the gallbladder have been reported [61–64].
In summary, the rate of clinical progression, including risk of metastases and relapse and tumor-related death in GIST, can be estimated by mitotic rate, size, and location (Table 1) [25, 27, 48, 52, 57].
Diagnostics
Initial patient evaluation should include a computed tomography (CT) scan (Fig. 4) of the abdomen and pelvis without chest CT because lung metastases are extraordinarily rare. CT scan of primary GIST typically display exophytic tumors, which are >5 cm and enhance inhomogeneously [65]. Endoscopic ultrasound might be of additional value, but biopsy is not mandatory prior to surgery, except to rule out differential diagnoses like lymphoma or other malignant or benign neoplasms. Establishing a histological diagnosis is essential when planning neoadjuvant therapy and in the metastatic setting, where surgery is not the first treatment of choice. Biopsies can either be taken endoscopically (deep biopsy reaching the muscularis layer) or as core needle biopsies (ultrasound or CT guided). With endoscopic techniques, GIST can be visualized as a submucosal protruberance, commonly with a central ulceration [66]. Especially in gastric GIST, endoscopic ultrasound (Fig. 5) is of additional value in the diagnostics of GIST because it differentiates the different layers of the gastric wall allowing the GIST to be assigned to the muscle layer.
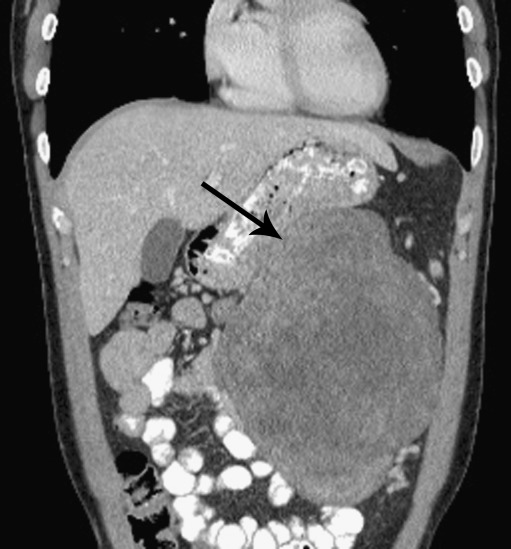
Fig. 4.
Abdominal CT scan displaying a gastric GIST
Fig. 5.
Endosonography for a gastric GIST (a) with the corresponding gastroscopic view of the tumor (b)
Priciples of therapy
Role of surgery
Still, only complete surgical resection of GIST is curative. GIST rarely metastasize to lymph nodes [67–70] and therefore regional lymphadenectomy is generally not required. Furthermore, organ-sparing resection (segmental resection, etc.) is oncologically appropriate and should thus be aimed for. The primary goal is to remove the tumor with tumor free margins since 5-year overall survival in GIST patients with complete gross resection has been estimated at 42% compared to only 9% overall survival if the excision was incomplete [70]. GIST can usually be lifted away from surrounding structures, rarely spread into adjacent organs and therefore offer an excellent opportunity for laparoscopic tumor resection with efficacy and recurrence rates similar or superior to historical open surgical controls [71–74]. When the tumor attaches to other organs, en bloc resection is appropriate. Intraperitoneal rupture or bleeding is associated with a high risk of postoperative recurrence of nearly 100% [43, 75, 76]. Therefore, it is of critical importance that the GIST, which is soft and fragile in nature, does not rupture intraoperatively demanding special care while handling the tumor.
Tyrosine kinase inhibitors
Within the KIT and PDGFRA gene, the mutations are clustered in four (exons 9, 11, 13, and 17) or three exons (exons 12, 14, and 18), respectively [77] resulting in constitutive tyrosine kinase activity. Tyrosine kinase inhibitors are able to occupy the active site of the enzyme and thus prevent the activation and subsequent cell division [78]. This offers the opportunity of a targeted treatment of GIST by tyrosine kinase inhibitors, such as imatinib mesylate (IM, Gleevec®, Novartis, Basel, Switzerland) or others. Beside imatinib mesylate several other tyrosine kinase inhibitors like sunitinib, nilotinib, masatinib, mosetanib, sorafenib, regorafinib, and dasatinib [79] are available. These substances differ in their ability to inhibit one or several tyrosine kinases.
Side effects
Generally, therapy with tyrosine kinase inhibitors is well-tolerated and safe. However, one has to be aware of some side effects and enzymatic interactions, which are listed in the information and direction of use provided by the manufacturer. Plasma levels can be influenced by drugs that are metabolized by the cytochrome P-450 isoform 3A4. In our experience, clinical side effects mainly include edema (mostly periorbital), muscle cramps, and gastrointestinal side effects. Hematologic side effects include decreases in hemoglobin levels and leukocyte count. Generally, therapy does not have to be interrupted, and treatment is mostly symptomatic [66].
Neoadjuvant therapy
Neoadjuvant therapy with tyrosine kinase inhibitors should be considered to facilitate R0 resection and allow for a less morbid operation, especially in duodenal GIST in which complete surgical resection is sometimes difficult to achieve [80]. Tumor size and vascularization may be reduced resulting in a decreased risk of intraoperative tumor rupture and peritoneal seeding [81–83].
In several studies, the effect of preoperative application of imatinib mesylate in patients with primary GIST of different sites was examined. While some authors report tumor shrinkage in all patients with a median size reduction of 34% and conclude that, in unresectable or locally advanced GIST, preoperative imatinib mesylate can be useful to improve resectability and reduce surgical morbidity [84], others classify the response clinically into three groups: (1) early responders (up to 70% [80, 85]), (2) those with stable disease, and (3) those with progressive disease while on targeted therapy [85]. The impact of preoperative imatinib therapy depends on the primary KIT and PDGFRA mutation status. Therefore, early and regular response control with PET is essential during neoadjuvant treatment, as non-responders (wild type, unfavorable mutation in KIT or PDGFRA) must be recognized early. Accordingly, patients with early radiographic response to imatinib therapy seem to have a greater probability of R0 resection and prolonged disease-free survival [85]. In another study, primary and recurrent metastatic GIST were treated with preoperative imatinib mesylate, and the 2-year progression free survival was 83% and 77%, respectively [82].
The duration of neoadjuvant treatment is not completely defined yet. Eisenberg et al. [81] recommend that the response of neoadjuvant imatinib mesylate in resectable GIST should be evaluated early and continuously, and surgical resection should be offered within 3–6 month to avoid tumor progression. It is necessary to keep in mind that secondary mutations may emerge, which may interfere with drug binding and lead to secondary drug resistance during the course of therapy [80, 85].
According to the 2011 NCCN guidelines, neoadjuvant therapy is recommended for GIST that are marginally resectable or resectable with risk of significant morbidity (NCCN). The duration for neoadjuvant treatment is currently discussed, and in therapy responders, a treatment of 4–6 months has been proposed [86]. Cases that show progress under preoperative therapy should be treated following the below-mentioned guidelines for progressive disease.
Adjuvant therapy
The risk of postoperative recurrence is fairly high in tumors with the above-stated high-risk features (Table 1) [48]. Without tyrosine kinase inhibitor treatment, the overall 5-year disease-specific survival rate has been reported as 35% after surgical resection [26]. Even after complete surgical resection, the overall 5-year survival rate was only 54% in metastasized and non-metastasized patients with a median survival of 19 months in metastatic disease and 12 months in those with local recurrence [26]. As stated above, high-risk GIST [48] have a risk of tumor recurrence of up to 66% [51], making it obvious that surgery alone is not sufficient to provide long-term survival for a vast number of GIST patients.
The first adjuvant treatment trial was the phase II open-label, single-arm trial of the American College of Surgeons Oncology Group (ACOSOG) Z9000 [87]. Patients in this trial underwent complete gross resection of a KIT-expressing primary GIST that was at high risk of recurrence (≥10 cm, tumor rupture, or <5 peritoneal metastases). The patients with exon 9 mutations of the KIT gene quickly experienced recurrence once imatinib was stopped (0% recurrence-free survival at 2 years), and patients with exon 11 mutations showed about 62% recurrence-free survival at 3 years. PDGFRA-mutant patients had the most favorable results, with about 90% recurrence-free at 3 years. Patients without detectable mutations (wild type) showed about 77% recurrence-free survival at 3 years. Taken together, this trial led to the conclusion that imatinib prolongs recurrence-free survival and is associated with improved overall survival compared with historical controls [87].
The trial was followed by the phase III double-blind and placebo-controlled ACOSOG Z9001 trial [88]. Patients had complete resection of a (c-kit positiv) primary GIST of at least 3 cm in size, followed by a 1-year adjuvant imatinib treatment (400 mg). Recurrence-free survival with imatinib was 98% versus 83% in the placebo group [88]. Although adjuvant imatinib therapy was shown to be safe and seemed to prolong recurrence-free survival compared to placebo treatment, the overall survival was not different at this time [89]. This study has led to the accelerated approval by the Food and Drug Administration (FDA, 12/2008).
In Europe, two other phase III trials are ongoing, and analyses are awaited for the end of 2011 and 2012. The EORTC 62024 intergroup trial was designed for patients with intermediate and high-risk GIST treated with imatinib (400 mg) or placebo for 2 years with overall survival as the primary end point. The German-Scandinavian SSG XVIII/AIO trial was designed for adjuvant treatment (imatinib 400 mg) of high-risk GIST with a treatment duration of 3 or 1 year and recurrence-free survival as the primary end point. Some data suggest that when interrupted at either 1 or 3 years, relapse consistently can be observed at a median of 6 months [90]. However, it is still being debated whether adjuvant treatment will prevent relapse or only delay [90], and the unknown long-term efficacy and safety profile of adjuvant imatinib have to be considered in the decision [91]. The optimal duration of adjuvant imatinib still has to be determined, and the only available data show the efficacy of 1-year treatment vs. placebo on progression-free survival, although 1 year of treatment in view of the ACOSOG Z9001 and preliminary results of the SSG XVIII trial may not suffice. Concerning the development of imatinib resistance in adjuvant treated GIST, interesting findings within the BFR14 trial suggest that the time to resistance to imatinib begins to elapse on the first day of imatinib administration and is not stopped at imatinib interruption [90]. However, further studies are being done to examine this observation and define possible consequences.
The current clinical practice guidelines [92] recommend surgical resection for limited disease and adjuvant imatinib therapy as an option for patients with a substantial risk of relapse (see Table 1). Rupture and intraperitoneal hemorrhage have to be considered as metastatic GIST until proven otherwise.
The optimal duration of adjuvant therapy with tyrosine kinase inhibitors is still being debated [93]. To define the patient group that profits most from adjuvant imatinib treatment, tumor size, mitotic count, mutation type and site, and the quality of surgery will have to be taken into account [90]. Furthermore, mutational analysis may select patients who are more likely to benefit from the treatment. KIT exon 11 mutations show the greatest benefit from adjuvant treatment with 400 mg imatinib. Of note, KIT exon 11 codon 557/558 deletion/insertion mutations have a more aggressive clinical behavior [94]. Regarding KIT exon 9 mutations, it has been demonstrated that KIT exon 9 mutated GIST profit from a higher imatinib dosage in view of recurrence-free survival [95, 96]. In addition, sunitinib is beneficial for exon 9 mutated-GIST [97]. Wild-type patients do not seem to benefit from adjuvant imatinib [47]; however, in vivo studies evaluating sunitinib [98] and in vitro studies for nilotinib and dasatinib [79] are promising. As for PDGFRA-mutated GIST, PDGFRA exon 18 generally benefits from adjuvant imatinib therapy, with the exception of PDGFRA exon 18 D842V-mutated GIST [44].
However, all patients in the above-mentioned studies were treated in a palliative setting, and currently, there is no published evidence on the different effects of adjuvant imatinib in GISTs with different mutations.
Palliative therapy
Existing clinical practice guidelines (NCCN, ESMO) recommend the administration of imatinib for patients with metastases in the liver or the peritoneum. In the year 2000, the application of the tyrosine kinase inhibitors imatinib mesylate was first studied in the palliative setting for patients with advanced and non-resectable GIST [99].
According to the NCCN guidelines, patients with progressive disease under imatinib treatment can be re-assessed for surgery. If surgery is not an option, limited and generalized progression should be distinguished. Limited progression should be treated either with imatinib at the same or increased dose; if possible, radiofrequency ablation can be considered. With further or generalized progress, imatinib at increased dose or sunitinib (37.5 mg) [97, 100, 101] should be considered. If the disease progresses despite prior imatinib or sunitinib therapy, participation in a clinical study, other options, or best supportive care are advised. Other options include novel substances such as nilotinib [102], the oral multikinase inhibitors sorafenib [103, 104], masatinib, dasatinib [105], and AMG706, the oral antiangiogenic molecule vatalanib [106], the mTOR-inhibitor RAD 001 and rapamycin [107], and the protein kinase C-inhibitor PKC 412 [108]. These substances do not have a label for GIST and can thus be used only off-label or in a clinical trials. Additionally, re-exposal to imatinib can be discussed after treatment interruption or progression under other treatment schedules.
In the future, combination therapies will be discussed. This might include tyrosine inhibitor combinations as well as chemotherapy combinations. A recent article showed promising activity of the combination doxorubicin with imatinib in heavily pretreated gastrointestinal stromal tumors [109].
The role of surgery in the setting of metastatic GIST is still being discussed, and data to guide surgical decision making, such as timing for intervention, are very limited [93, 110–113]. Some authors propose a positive effect of surgical debulking for limited progression on kinase inhibitor therapy in selected cases and in residual disease upon best clinical response compared with patients treated with imatinib alone [93, 110, 111]. However, in the setting of generalized progression, the role of surgical treatment is very limited and usually not indicated [93, 111].
Follow-up
According to the ESMO guidelines from 2010, there are no published data for the optimal routine follow-up policy of surgically treated patients with localized disease [92]. Metastases are mostly observed in the peritoneum or the liver [92]. The speed at which relapses take place is probably influenced by the mitotic rate of the tumor. Therefore, risk assessment based on mitotic count, size, and localization can be helpful in choosing the individualized follow-up [92]. Since patients with high risk GIST generally relapse within 2–3 years, and patients with low-risk may relapse later, the follow-up should be adapted to tumor criteria [92]. According to the NCCN guidelines, in the setting of localized disease, contrast-enhanced abdominal and pelvic CT scan is the technique of choice for staging and follow-up [114]. In rectal GIST, MRI should be used, and additional PET or PET-CT/MRI but may be useful for early detection of tumor response during neoadjuvant treatment [114]. Even though in Germany, regular ultrasound exams help to extend the CT intervals, the ESMO guidelines mention exemplary follow-up schemes: For intermediate–high-risk patients, a CT routine follow-up can be done every 3–4 months for 3 years, then every 6 months until 5 and yearly afterwards [92]; for low-risk tumors, every 6 months for 5 years; and very low-risk GIST probably do not deserve routine follow-up [92]. We would however recommend CT intervals of 6 months for high-risk GIST, with an ultrasound exam at 3 months. After 5 years, with non-detectable or stable disease, a yearly CT scan should be sufficient. In our experience, while liver metastases are well-detected by imaging techniques, peritoneal metastases become apparent with sub-ileus or ileus symptoms, before they are depicted in routine imaging. PET-CT might help to detect the development of early metastases and to distinguish active tumors from hyaline tumor remnants and facilitates the planning of surgical interventions [115].
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Appelman HD. Mesenchymal tumors of the gut: historical perspectives, new approaches, new results, and does it make any difference? Monogr Pathol. 1990;31:220–246. [PubMed] [Google Scholar]
- 2.Walker P, Dvorak AM. Gastrointestinal autonomic nerve (GAN) tumor. Ultrastructural evidence for a newly recognized entity. Arch Pathol Lab Med. 1986;110(4):309–316. [PubMed] [Google Scholar]
- 3.Mazur MT, Clark HB. Gastric stromal tumors. Reappraisal of histogenesis. Am J Surg Pathol. 1983;7(6):507–519. doi: 10.1097/00000478-198309000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279(5350):577–580. doi: 10.1126/science.279.5350.577. [DOI] [PubMed] [Google Scholar]
- 5.Robinson TL, Sircar K, Hewlett BR, et al. Gastrointestinal stromal tumors may originate from a subset of CD34-positive interstitial cells of Cajal. Am J Pathol. 2000;156(4):1157–1163. doi: 10.1016/S0002-9440(10)64984-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Evans HL. Smooth muscle tumors of the gastrointestinal tract. A study of 56 cases followed for a minimum of 10 years. Cancer. 1985;56(9):2242–2250. doi: 10.1002/1097-0142(19851101)56:9<2242::aid-cncr2820560918>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 7.Akwari OE, Dozois RR, Weiland LH, Beahrs OH. Leiomyosarcoma of the small and large bowel. Cancer. 1978;42(3):1375–1384. doi: 10.1002/1097-0142(197809)42:3<1375::aid-cncr2820420348>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 8.Miettinen M, Lasota J. Gastrointestinal stromal tumors (GISTs): definition, occurrence, pathology, differential diagnosis and molecular genetics. Pol J Pathol. 2003;54(1):3–24. [PubMed] [Google Scholar]
- 9.Kindblom LG, Remotti HE, Aldenborg F, Meis-Kindblom JM. Gastrointestinal pacemaker cell tumor (GIPACT): gastrointestinal stromal tumors show phenotypic characteristics of the interstitial cells of Cajal. Am J Pathol. 1998;152(5):1259–1269. [PMC free article] [PubMed] [Google Scholar]
- 10.Miettinen M, Lasota J, Sobin LH. Gastrointestinal stromal tumors of the stomach in children and young adults: a clinicopathologic, immunohistochemical, and molecular genetic study of 44 cases with long-term follow-up and review of the literature. Am J Surg Pathol. 2005;29(10):1373–1381. doi: 10.1097/01.pas.0000172190.79552.8b. [DOI] [PubMed] [Google Scholar]
- 11.Arber DA, Tamayo R, Weiss LM. Paraffin section detection of the c-kit gene product (CD117) in human tissues: value in the diagnosis of mast cell disorders. Hum Pathol. 1998;29(5):498–504. doi: 10.1016/s0046-8177(98)90066-1. [DOI] [PubMed] [Google Scholar]
- 12.Miettinen M, Sarlomo-Rikala M, Lasota J. KIT expression in angiosarcomas and fetal endothelial cells: lack of mutations of exon 11 and exon 17 of C-kit. Mod Pathol. 2000;13(5):536–541. doi: 10.1038/modpathol.3880093. [DOI] [PubMed] [Google Scholar]
- 13.Montone KT, van Belle P, Elenitsas R, Elder DE. Proto-oncogene c-kit expression in malignant melanoma: protein loss with tumor progression. Mod Pathol. 1997;10(9):939–944. [PubMed] [Google Scholar]
- 14.Miettinen M, Sobin LH, Sarlomo-Rikala M. Immunohistochemical spectrum of GISTs at different sites and their differential diagnosis with a reference to CD117 (KIT) Mod Pathol. 2000;13(10):1134–1142. doi: 10.1038/modpathol.3880210. [DOI] [PubMed] [Google Scholar]
- 15.Motegi A, Sakurai S, Nakayama H, et al. PKC theta, a novel immunohistochemical marker for gastrointestinal stromal tumors (GIST), especially useful for identifying KIT-negative tumors. Pathol Int. 2005;55(3):106–112. doi: 10.1111/j.1440-1827.2005.01806.x. [DOI] [PubMed] [Google Scholar]
- 16.Sevinc A, Camci C, Yilmaz M, Buyukhatipoglu H. The diagnosis of C-kit negative GIST by PDGFRA staining: clinical, pathological, and nuclear medicine perspective. Onkologie. 2007;30(12):645–648. doi: 10.1159/000109978. [DOI] [PubMed] [Google Scholar]
- 17.West RB, Corless CL, Chen X, et al. The novel marker, DOG1, is expressed ubiquitously in gastrointestinal stromal tumors irrespective of KIT or PDGFRA mutation status. Am J Pathol. 2004;165(1):107–113. doi: 10.1016/S0002-9440(10)63279-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miettinen M, Sarlomo-Rikala M, Lasota J. Gastrointestinal stromal tumors: recent advances in understanding of their biology. Hum Pathol. 1999;30(10):1213–1220. doi: 10.1016/s0046-8177(99)90040-0. [DOI] [PubMed] [Google Scholar]
- 19.Kim KM, Kang DW, Moon WS, et al. Gastrointestinal stromal tumors in Koreans: it’s incidence and the clinical, pathologic and immunohistochemical findings. J Korean Med Sci. 2005;20(6):977–984. doi: 10.3346/jkms.2005.20.6.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goettsch WG, Bos SD, Breekveldt-Postma N, et al. Incidence of gastrointestinal stromal tumours is underestimated: results of a nation-wide study. Eur J Cancer. 2005;41(18):2868–2872. doi: 10.1016/j.ejca.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Tryggvason G, Gislason HG, Magnusson MK, Jonasson JG. Gastrointestinal stromal tumors in Iceland, 1990–2003: the icelandic GIST study, a population-based incidence and pathologic risk stratification study. Int J Cancer. 2005;117(2):289–293. doi: 10.1002/ijc.21167. [DOI] [PubMed] [Google Scholar]
- 22.Ueyama T, Guo KJ, Hashimoto H, et al. A clinicopathologic and immunohistochemical study of gastrointestinal stromal tumors. Cancer. 1992;69(4):947–955. doi: 10.1002/1097-0142(19920215)69:4<947::aid-cncr2820690419>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 23.Lerma E, Oliva E, Tugues D, Prat J. Stromal tumours of the gastrointestinal tract: a clinicopathological and ploidy analysis of 33 cases. Virchows Arch. 1994;424(1):19–24. doi: 10.1007/BF00197388. [DOI] [PubMed] [Google Scholar]
- 24.Miettinen M, Monihan JM, Sarlomo-Rikala M, et al. Gastrointestinal stromal tumors/smooth muscle tumors (GISTs) primary in the omentum and mesentery: clinicopathologic and immunohistochemical study of 26 cases. Am J Surg Pathol. 1999;23(9):1109–1118. doi: 10.1097/00000478-199909000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1,765 cases with long-term follow-up. Am J Surg Pathol. 2005;29(1):52–68. doi: 10.1097/01.pas.0000146010.92933.de. [DOI] [PubMed] [Google Scholar]
- 26.DeMatteo RP, Lewis JJ, Leung D, et al. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000;231(1):51–58. doi: 10.1097/00000658-200001000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miettinen M, Makhlouf H, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the jejunum and ileum: a clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up. Am J Surg Pathol. 2006;30(4):477–489. doi: 10.1097/00000478-200604000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Nishida T, Hirota S, Taniguchi M, et al. Familial gastrointestinal stromal tumours with germline mutation of the KIT gene. Nat Genet. 1998;19(4):323–324. doi: 10.1038/1209. [DOI] [PubMed] [Google Scholar]
- 29.Wozniak A, Rutkowski P, Sciot R, et al. Rectal gastrointestinal stromal tumors associated with a novel germline KIT mutation. Int J Cancer. 2008;122(9):2160–2164. doi: 10.1002/ijc.23338. [DOI] [PubMed] [Google Scholar]
- 30.Kleinbaum EP, Lazar AJ, Tamborini E, et al. Clinical, histopathologic, molecular and therapeutic findings in a large kindred with gastrointestinal stromal tumor. Int J Cancer. 2008;122(3):711–718. doi: 10.1002/ijc.23137. [DOI] [PubMed] [Google Scholar]
- 31.Thalheimer A, Schlemmer M, Bueter M, et al. Familial gastrointestinal stromal tumors caused by the novel KIT exon 17 germline mutation N822Y. Am J Surg Pathol. 2008;32(10):1560–1565. doi: 10.1097/PAS.0b013e318172ce6f. [DOI] [PubMed] [Google Scholar]
- 32.Chompret A, Kannengiesser C, Barrois M, et al. PDGFRA germline mutation in a family with multiple cases of gastrointestinal stromal tumor. Gastroenterology. 2004;126(1):318–321. doi: 10.1053/j.gastro.2003.10.079. [DOI] [PubMed] [Google Scholar]
- 33.Matyakhina L, Bei TA, McWhinney SR, et al. Genetics of Carney triad: recurrent losses at chromosome 1 but lack of germline mutations in genes associated with paragangliomas and gastrointestinal stromal tumors. J Clin Endocrinol Metab. 2007;92(8):2938–2943. doi: 10.1210/jc.2007-0797. [DOI] [PubMed] [Google Scholar]
- 34.Takazawa Y, Sakurai S, Sakuma Y, et al. Gastrointestinal stromal tumors of neurofibromatosis type I (von Recklinghausen’s disease) Am J Surg Pathol. 2005;29(6):755–763. doi: 10.1097/01.pas.0000163359.32734.f9. [DOI] [PubMed] [Google Scholar]
- 35.Miettinen M, Fetsch JF, Sobin LH, Lasota J. Gastrointestinal stromal tumors in patients with neurofibromatosis 1: a clinicopathologic and molecular genetic study of 45 cases. Am J Surg Pathol. 2006;30(1):90–96. doi: 10.1097/01.pas.0000176433.81079.bd. [DOI] [PubMed] [Google Scholar]
- 36.Kang DY, Park CK, Choi JS, et al. Multiple gastrointestinal stromal tumors: clinicopathologic and genetic analysis of 12 patients. Am J Surg Pathol. 2007;31(2):224–232. doi: 10.1097/01.pas.0000213318.66800.94. [DOI] [PubMed] [Google Scholar]
- 37.Carney JA, Sheps SG, Go VL, Gordon H. The triad of gastric leiomyosarcoma, functioning extra-adrenal paraganglioma and pulmonary chondroma. N Engl J Med. 1977;296(26):1517–1518. doi: 10.1056/NEJM197706302962609. [DOI] [PubMed] [Google Scholar]
- 38.Carney JA. Gastric stromal sarcoma, pulmonary chondroma, and extra-adrenal paraganglioma (Carney Triad): natural history, adrenocortical component, and possible familial occurrence. Mayo Clin Proc. 1999;74(6):543–552. doi: 10.4065/74.6.543. [DOI] [PubMed] [Google Scholar]
- 39.Diment J, Tamborini E, Casali P, et al. Carney triad: case report and molecular analysis of gastric tumor. Hum Pathol. 2005;36(1):112–116. doi: 10.1016/j.humpath.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 40.Knop S, Schupp M, Wardelmann E, et al. A new case of Carney triad: gastrointestinal stromal tumours and leiomyoma of the oesophagus do not show activating mutations of KIT and platelet-derived growth factor receptor alpha. J Clin Pathol. 2006;59(10):1097–1099. doi: 10.1136/jcp.2005.029801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carney JA, Stratakis CA. Familial paraganglioma and gastric stromal sarcoma: a new syndrome distinct from the Carney triad. Am J Med Genet. 2002;108(2):132–139. doi: 10.1002/ajmg.10235. [DOI] [PubMed] [Google Scholar]
- 42.Martin J, Poveda A, Llombart-Bosch A, et al. Deletions affecting codons 557–558 of the c-KIT gene indicate a poor prognosis in patients with completely resected gastrointestinal stromal tumors: a study by the Spanish Group for Sarcoma Research (GEIS) J Clin Oncol. 2005;23(25):6190–6198. doi: 10.1200/JCO.2005.19.554. [DOI] [PubMed] [Google Scholar]
- 43.Hohenberger P, Ronellenfitsch U, Oladeji O, et al. Pattern of recurrence in patients with ruptured primary gastrointestinal stromal tumour. Br J Surg. 2010;97(12):1854–1859. doi: 10.1002/bjs.7222. [DOI] [PubMed] [Google Scholar]
- 44.Corless CL, Schroeder A, Griffith D, et al. PDGFRA mutations in gastrointestinal stromal tumors: frequency, spectrum and in vitro sensitivity to imatinib. J Clin Oncol. 2005;23(23):5357–5364. doi: 10.1200/JCO.2005.14.068. [DOI] [PubMed] [Google Scholar]
- 45.Gunawan B, von Heydebreck A, Sander B, et al. An oncogenetic tree model in gastrointestinal stromal tumours (GISTs) identifies different pathways of cytogenetic evolution with prognostic implications. J Pathol. 2007;211(4):463–470. doi: 10.1002/path.2128. [DOI] [PubMed] [Google Scholar]
- 46.Heinrich MC, Corless CL, Demetri GD, et al. Kinase mutations and imatinib response in patients with metastatic gastrointestinal stromal tumor. J Clin Oncol. 2003;21(23):4342–4349. doi: 10.1200/JCO.2003.04.190. [DOI] [PubMed] [Google Scholar]
- 47.Heinrich MC, Owzar K, Corless CL, et al. Correlation of kinase genotype and clinical outcome in the North American Intergroup Phase III Trial of imatinib mesylate for treatment of advanced gastrointestinal stromal tumor: CALGB 150105 Study by Cancer and Leukemia Group B and Southwest Oncology Group. J Clin Oncol. 2008;26(33):5360–5367. doi: 10.1200/JCO.2008.17.4284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol. 2006;23(2):70–83. doi: 10.1053/j.semdp.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 49.Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Int J Surg Pathol. 2002;10(2):81–89. doi: 10.1177/106689690201000201. [DOI] [PubMed] [Google Scholar]
- 50.Miettinen M, Sarlomo-Rikala M, Sobin LH, Lasota J. Esophageal stromal tumors: a clinicopathologic, immunohistochemical, and molecular genetic study of 17 cases and comparison with esophageal leiomyomas and leiomyosarcomas. Am J Surg Pathol. 2000;24(2):211–222. doi: 10.1097/00000478-200002000-00007. [DOI] [PubMed] [Google Scholar]
- 51.Nilsson B, Bumming P, Meis-Kindblom JM, et al. Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era—a population-based study in western Sweden. Cancer. 2005;103(4):821–829. doi: 10.1002/cncr.20862. [DOI] [PubMed] [Google Scholar]
- 52.Miettinen M, Kopczynski J, Makhlouf HR, et al. Gastrointestinal stromal tumors, intramural leiomyomas, and leiomyosarcomas in the duodenum: a clinicopathologic, immunohistochemical, and molecular genetic study of 167 cases. Am J Surg Pathol. 2003;27(5):625–641. doi: 10.1097/00000478-200305000-00006. [DOI] [PubMed] [Google Scholar]
- 53.Goldblum JR, Appelman HD. Stromal tumors of the duodenum. A histologic and immunohistochemical study of 20 cases. Am J Surg Pathol. 1995;19(1):71–80. doi: 10.1097/00000478-199501000-00009. [DOI] [PubMed] [Google Scholar]
- 54.Tworek JA, Goldblum JR, Weiss SW, et al. Stromal tumors of the anorectum: a clinicopathologic study of 22 cases. Am J Surg Pathol. 1999;23(8):946–954. doi: 10.1097/00000478-199908000-00013. [DOI] [PubMed] [Google Scholar]
- 55.Tworek JA, Goldblum JR, Weiss SW, et al. Stromal tumors of the abdominal colon: a clinicopathologic study of 20 cases. Am J Surg Pathol. 1999;23(8):937–945. doi: 10.1097/00000478-199908000-00012. [DOI] [PubMed] [Google Scholar]
- 56.Miettinen M, Sarlomo-Rikala M, Sobin LH, Lasota J. Gastrointestinal stromal tumors and leiomyosarcomas in the colon: a clinicopathologic, immunohistochemical, and molecular genetic study of 44 cases. Am J Surg Pathol. 2000;24(10):1339–1352. doi: 10.1097/00000478-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 57.Miettinen M, Furlong M, Sarlomo-Rikala M, et al. Gastrointestinal stromal tumors, intramural leiomyomas, and leiomyosarcomas in the rectum and anus: a clinicopathologic, immunohistochemical, and molecular genetic study of 144 cases. Am J Surg Pathol. 2001;25(9):1121–1133. doi: 10.1097/00000478-200109000-00002. [DOI] [PubMed] [Google Scholar]
- 58.Agaimy A, Wunsch PH. Gastrointestinal stromal tumours: a regular origin in the muscularis propria, but an extremely diverse gross presentation. A review of 200 cases to critically re-evaluate the concept of so-called extra-gastrointestinal stromal tumours. Langenbecks Arch Surg. 2006;391(4):322–329. doi: 10.1007/s00423-005-0005-5. [DOI] [PubMed] [Google Scholar]
- 59.Yamamoto H, Oda Y, Kawaguchi K, et al. c-kit and PDGFRA mutations in extragastrointestinal stromal tumor (gastrointestinal stromal tumor of the soft tissue) Am J Surg Pathol. 2004;28(4):479–488. doi: 10.1097/00000478-200404000-00007. [DOI] [PubMed] [Google Scholar]
- 60.Reith JD, Goldblum JR, Lyles RH, Weiss SW. Extragastrointestinal (soft tissue) stromal tumors: an analysis of 48 cases with emphasis on histologic predictors of outcome. Mod Pathol. 2000;13(5):577–585. doi: 10.1038/modpathol.3880099. [DOI] [PubMed] [Google Scholar]
- 61.Zhang W, Peng Z, Xu L. Extragastrointestinal stromal tumor arising in the rectovaginal septum: report of an unusual case with literature review. Gynecol Oncol. 2009;113(3):399–401. doi: 10.1016/j.ygyno.2009.02.019. [DOI] [PubMed] [Google Scholar]
- 62.Nasu K, Ueda T, Kai S, et al. Gastrointestinal stromal tumor arising in the rectovaginal septum. Int J Gynecol Cancer. 2004;14(2):373–377. doi: 10.1111/j.1048-891x.2004.014230.x. [DOI] [PubMed] [Google Scholar]
- 63.Peerlinck ID, Irvin TT, Sarsfield PT, Harington JM. GIST (gastro-intestinal stromal tumour) of the gallbladder: a case report. Acta Chir Belg. 2004;104(1):107–109. doi: 10.1080/00015458.2003.11978406. [DOI] [PubMed] [Google Scholar]
- 64.Mekni A, Chelly I, Azzouz H, et al. Extragastrointestinal stromal tumor of the urinary wall bladder: case report and review of the literature. Pathologica. 2008;100(3):173–175. [PubMed] [Google Scholar]
- 65.Sandrasegaran K, Rajesh A, Rushing DA, et al. Gastrointestinal stromal tumors: CT and MRI findings. Eur Radiol. 2005;15(7):1407–1414. doi: 10.1007/s00330-005-2647-7. [DOI] [PubMed] [Google Scholar]
- 66.Cameron S, Ramadori G. Gastrointestinal stromal tumors: diagnostics, therapy and beyond? Minerva Gastroenterol Dietol. 2009;55(4):409–423. [PubMed] [Google Scholar]
- 67.Gold JS, Gonen M, Gutierrez A, et al. Development and validation of a prognostic nomogram for recurrence-free survival after complete surgical resection of localised primary gastrointestinal stromal tumour: a retrospective analysis. Lancet Oncol. 2009;10(11):1045–1052. doi: 10.1016/S1470-2045(09)70242-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gold JS, Dematteo RP. Combined surgical and molecular therapy: the gastrointestinal stromal tumor model. Ann Surg. 2006;244(2):176–184. doi: 10.1097/01.sla.0000218080.94145.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Autelitano F, Santeusanio G, Mauriello A, et al. Latent pathology of the thyroid: an epidemiological and statistical study of thyroids sampled during 507 consecutive autopsies. Ann Ital Chir. 1992;63(6):761–781. [PubMed] [Google Scholar]
- 70.Pierie JP, Choudry U, Muzikansky A, et al. The effect of surgery and grade on outcome of gastrointestinal stromal tumors. Arch Surg. 2001;136(4):383–389. doi: 10.1001/archsurg.136.4.383. [DOI] [PubMed] [Google Scholar]
- 71.Novitsky YW, Kercher KW, Sing RF, Heniford BT. Long-term outcomes of laparoscopic resection of gastric gastrointestinal stromal tumors. Ann Surg. 2006;243(6):738–745. doi: 10.1097/01.sla.0000219739.11758.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nguyen SQ, Divino CM, Wang JL, Dikman SH. Laparoscopic management of gastrointestinal stromal tumors. Surg Endosc. 2006;20(5):713–716. doi: 10.1007/s00464-005-0435-8. [DOI] [PubMed] [Google Scholar]
- 73.Matthews BD, Walsh RM, Kercher KW, et al. Laparoscopic vs open resection of gastric stromal tumors. Surg Endosc. 2002;16(5):803–807. doi: 10.1007/s00464-001-8319-z. [DOI] [PubMed] [Google Scholar]
- 74.Bedard EL, Mamazza J, Schlachta CM, Poulin EC. Laparoscopic resection of gastrointestinal stromal tumors: not all tumors are created equal. Surg Endosc. 2006;20(3):500–503. doi: 10.1007/s00464-005-0287-2. [DOI] [PubMed] [Google Scholar]
- 75.Demetri GD, Antonia S, Benjamin RS, et al (2010) Soft tissue sarcoma. J Natl Compr Canc Netw 8(6):630–674 [DOI] [PubMed]
- 76.Rutkowski P, Nowecki ZI, Michej W, et al. Risk criteria and prognostic factors for predicting recurrences after resection of primary gastrointestinal stromal tumor. Ann Surg Oncol. 2007;14(7):2018–2027. doi: 10.1245/s10434-007-9377-9. [DOI] [PubMed] [Google Scholar]
- 77.Lasota J, Miettinen M. KIT and PDGFRA mutations in gastrointestinal stromal tumors (GISTs) Semin Diagn Pathol. 2006;23(2):91–102. doi: 10.1053/j.semdp.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 78.Rubin BP, Fletcher JA, Fletcher CD. Molecular insights into the histogenesis and pathogenesis of gastrointestinal stromal tumors. Int J Surg Pathol. 2000;8(1):5–10. doi: 10.1177/106689690000800105. [DOI] [PubMed] [Google Scholar]
- 79.Agaram NP, Laquaglia MP, Ustun B, et al. Molecular characterization of pediatric gastrointestinal stromal tumors. Clin Cancer Res. 2008;14(10):3204–3215. doi: 10.1158/1078-0432.CCR-07-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lopes LF, Bacchi CE. Imatinib treatment for gastrointestinal stromal tumour (GIST) J Cell Mol Med. 2010;14(1–2):42–50. doi: 10.1111/j.1582-4934.2009.00983.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Eisenberg BL, Smith KD. Adjuvant and neoadjuvant therapy for primary GIST. Cancer Chemother Pharmacol. 2011;67(Suppl 1):S3–S8. doi: 10.1007/s00280-010-1516-5. [DOI] [PubMed] [Google Scholar]
- 82.Eisenberg BL, Harris J, Blanke CD, et al. Phase II trial of neoadjuvant/adjuvant imatinib mesylate (IM) for advanced primary and metastatic/recurrent operable gastrointestinal stromal tumor (GIST): early results of RTOG 0132/ACRIN 6665. J Surg Oncol. 2009;99(1):42–47. doi: 10.1002/jso.21160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Catania V, Consoli A, Cavallaro A, et al. The neo-adjuvant treatment in gastrointestinal stromal tumor. Eur Rev Med Pharmacol Sci. 2010;14(8):727–730. [PubMed] [Google Scholar]
- 84.Fiore M, Palassini E, Fumagalli E, et al. Preoperative imatinib mesylate for unresectable or locally advanced primary gastrointestinal stromal tumors (GIST) Eur J Surg Oncol. 2009;35(7):739–745. doi: 10.1016/j.ejso.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 85.Dudeja V, Armstrong LH, Gupta P, et al. Emergence of imatinib resistance associated with downregulation of c-kit expression in recurrent gastrointestinal stromal tumor (GIST): optimal timing of resection. J Gastrointest Surg. 2010;14(3):557–561. doi: 10.1007/s11605-009-1121-2. [DOI] [PubMed] [Google Scholar]
- 86.Hohenberger P, Wardelmann E. Surgical considerations for gastrointestinal stroma tumor. Chirurg. 2006;77(1):33–40. doi: 10.1007/s00104-005-1125-8. [DOI] [PubMed] [Google Scholar]
- 87.DeMatteo RP, Owzar K, Antonescu CR, et al. (2008) Efficacy of adjuvant imatinib mesylate following complete resection of localized, primary gastrointestinal stromal tumor (GIST) at high risk of recurrence: the US Intergroup phase II trial ACOSOG Z9000. Gastrointestinal Cancers Symposium 2008
- 88.Corless CL, Ballman KV, Antonescu C, et al. Relation of tumor pathologic and molecular features to outcome after surgical resection of localized primary gastrointestinal stromal tumor (GIST): results of the intergroup phase III trial ACOSOG Z9001. J Clin Oncol. 2010;28(15):100006. [Google Scholar]
- 89.Dematteo RP, Ballman KV, Antonescu CR, et al. Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: a randomised, double-blind, placebo-controlled trial. Lancet. 2009;373(9669):1097–1104. doi: 10.1016/S0140-6736(09)60500-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gronchi A, Judson I, Nishida T, et al. Adjuvant treatment of GIST with imatinib: solid ground or still quicksand? A comment on behalf of the EORTC Soft Tissue and Bone Sarcoma Group, the Italian Sarcoma Group, the NCRI Sarcoma Clinical Studies Group (UK), the Japanese Study Group on GIST, the French Sarcoma Group and the Spanish Sarcoma Group (GEIS) Eur J Cancer. 2009;45(7):1103–1106. doi: 10.1016/j.ejca.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 91.Essat M, Cooper K. Imatinib as adjuvant therapy for gastrointestinal stromal tumors: a systematic review. Int J Cancer. 2010;128(9):2202–2214. doi: 10.1002/ijc.25827. [DOI] [PubMed] [Google Scholar]
- 92.Casali PG, Blay JY. Gastrointestinal stromal tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21(Suppl 5):v98–v102. doi: 10.1093/annonc/mdq208. [DOI] [PubMed] [Google Scholar]
- 93.Deshaies I, Cherenfant J, Gusani NJ, et al. Gastrointestinal stromal tumor (GIST) recurrence following surgery: review of the clinical utility of imatinib treatment. Ther Clin Risk Manag. 2010;6:453–458. doi: 10.2147/TCRM.S5634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kontogianni-Katsarou K, Dimitriadis E, Lariou C, et al. KIT exon 11 codon 557/558 deletion/insertion mutations define a subset of gastrointestinal stromal tumors with malignant potential. World J Gastroenterol. 2008;14(12):1891–1897. doi: 10.3748/wjg.14.1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Patel S, Zalcberg JR. Optimizing the dose of imatinib for treatment of gastrointestinal stromal tumours: lessons from the phase 3 trials. Eur J Cancer. 2008;44(4):501–509. doi: 10.1016/j.ejca.2007.11.021. [DOI] [PubMed] [Google Scholar]
- 96.Debiec-Rychter M, Sciot R, Le Cesne A, et al. KIT mutations and dose selection for imatinib in patients with advanced gastrointestinal stromal tumours. Eur J Cancer. 2006;42(8):1093–1103. doi: 10.1016/j.ejca.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 97.Demetri GD, van Oosterom AT, Garrett CR, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. 2006;368(9544):1329–1338. doi: 10.1016/S0140-6736(06)69446-4. [DOI] [PubMed] [Google Scholar]
- 98.Janeway KA, Albritton KH, Van Den Abbeele AD, et al. Sunitinib treatment in pediatric patients with advanced GIST following failure of imatinib. Pediatr Blood Cancer. 2009;52(7):767–771. doi: 10.1002/pbc.21909. [DOI] [PubMed] [Google Scholar]
- 99.Joensuu H, Roberts PJ, Sarlomo-Rikala M, et al. Effect of the tyrosine kinase inhibitor STI571 in a patient with a metastatic gastrointestinal stromal tumor. N Engl J Med. 2001;344(14):1052–1056. doi: 10.1056/NEJM200104053441404. [DOI] [PubMed] [Google Scholar]
- 100.George S, Blay JY, Casali PG, et al. Clinical evaluation of continuous daily dosing of sunitinib malate in patients with advanced gastrointestinal stromal tumour after imatinib failure. Eur J Cancer. 2009;45(11):1959–1968. doi: 10.1016/j.ejca.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 101.Winer JH, Raut CP (2011) Management of recurrent gastrointestinal stromal tumors. J Surg Oncol 104:915–920 [DOI] [PubMed]
- 102.Demetri GD, Casali PG, Blay JY, et al. A phase I study of single-agent nilotinib or in combination with imatinib in patients with imatinib-resistant gastrointestinal stromal tumors. Clin Cancer Res. 2009;15(18):5910–5916. doi: 10.1158/1078-0432.CCR-09-0542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Guo T, Agaram NP, Wong GC, et al. Sorafenib inhibits the imatinib-resistant KITT670I gatekeeper mutation in gastrointestinal stromal tumor. Clin Cancer Res. 2007;13(16):4874–4881. doi: 10.1158/1078-0432.CCR-07-0484. [DOI] [PubMed] [Google Scholar]
- 104.Huynh H, Lee JW, Chow PK, et al. Sorafenib induces growth suppression in mouse models of gastrointestinal stromal tumor. Mol Cancer Ther. 2009;8(1):152–159. doi: 10.1158/1535-7163.MCT-08-0553. [DOI] [PubMed] [Google Scholar]
- 105.Shah NP, Lee FY, Luo R, et al. Dasatinib (BMS-354825) inhibits KITD816V, an imatinib-resistant activating mutation that triggers neoplastic growth in most patients with systemic mastocytosis. Blood. 2006;108(1):286–291. doi: 10.1182/blood-2005-10-3969. [DOI] [PubMed] [Google Scholar]
- 106.Joensuu H, De Braud F, Coco P, et al. Phase II, open-label study of PTK787/ZK222584 for the treatment of metastatic gastrointestinal stromal tumors resistant to imatinib mesylate. Ann Oncol. 2008;19(1):173–177. doi: 10.1093/annonc/mdm419. [DOI] [PubMed] [Google Scholar]
- 107.Schoffski P, Reichardt P, Blay JY, et al (2010) A phase I-II study of everolimus (RAD001) in combination with imatinib in patients with imatinib-resistant gastrointestinal stromal tumors. Ann Oncol 21(10):1990–1998 [DOI] [PubMed]
- 108.Weisberg E, Wright RD, Jiang J, et al. Effects of PKC412, nilotinib, and imatinib against GIST-associated PDGFRA mutants with differential imatinib sensitivity. Gastroenterology. 2006;131(6):1734–1742. doi: 10.1053/j.gastro.2006.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Maurel J, Martins AS, Poveda A, et al (2010) Imatinib plus low-dose doxorubicin in patients with advanced gastrointestinal stromal tumors refractory to high-dose imatinib: a phase I–II study by the Spanish Group for Research on Sarcomas. Cancer 116(15):3692–3701 [DOI] [PubMed]
- 110.Mussi C, Ronellenfitsch U, Jakob J, et al. Post-imatinib surgery in advanced/metastatic GIST: is it worthwhile in all patients? Ann Oncol. 2010;21(2):403–408. doi: 10.1093/annonc/mdp310. [DOI] [PubMed] [Google Scholar]
- 111.Raut CP, Posner M, Desai J, et al. Surgical management of advanced gastrointestinal stromal tumors after treatment with targeted systemic therapy using kinase inhibitors. J Clin Oncol. 2006;24(15):2325–2331. doi: 10.1200/JCO.2005.05.3439. [DOI] [PubMed] [Google Scholar]
- 112.Rutkowski P, Nowecki Z, Nyckowski P, et al. Surgical treatment of patients with initially inoperable and/or metastatic gastrointestinal stromal tumors (GIST) during therapy with imatinib mesylate. J Surg Oncol. 2006;93(4):304–311. doi: 10.1002/jso.20466. [DOI] [PubMed] [Google Scholar]
- 113.Bonvalot S, Eldweny H, Pechoux CL, et al. Impact of surgery on advanced gastrointestinal stromal tumors (GIST) in the imatinib era. Ann Surg Oncol. 2006;13(12):1596–1603. doi: 10.1245/s10434-006-9047-3. [DOI] [PubMed] [Google Scholar]
- 114.Reichardt P, Blay JY, Mehren M. Towards global consensus in the treatment of gastrointestinal stromal tumor. Expert Rev Anticancer Ther. 2010;10(2):221–232. doi: 10.1586/era.09.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Goerres GW, Stupp R, Barghouth G, et al. The value of PET, CT and in-line PET/CT in patients with gastrointestinal stromal tumours: long-term outcome of treatment with imatinib mesylate. Eur J Nucl Med Mol Imaging. 2005;32(2):153–162. doi: 10.1007/s00259-004-1633-7. [DOI] [PMC free article] [PubMed] [Google Scholar]