Abstract
Purpose
Anastomotic leakage is a serious complication after colorectal surgery. Pre- and intraoperative factors may contribute to failure of colorectal anastomosis. In this study we have tried to determine risk factors for anastomotic leakage, with special emphasis on intraoperative blood pressure changes.
Methods
During a 24-month period, patients receiving a colorectal anastomosis were prospectively evaluated. For each patient preoperative characteristics, intraoperative adverse events and surgical outcome data were collected. Blood pressure changes were calculated as a relative decrease (>25% and >40%) from preoperative baseline values.
Results
During the study period, 285 patients underwent colorectal surgery with an anastomosis. Fifteen patients developed an anastomotic leakage (5.3%). All patients who developed a leakage had a left-sided procedure (P < 0.001). When blood loss was more than 250 mL (P = 0.003) or an intraoperative adverse event occurred (P = 0.050), the risk for developing an anastomotic leakage was significantly increased. A preoperative high diastolic blood pressure of ≥90 mmHg (P = 0.008) and severe intraoperative hypotension [>40% decrease in diastolic blood pressure (P = 0.049)] were identified as univariate risk factors for anastomotic leakage.
Conclusions
The development of an anastomotic leakage after colorectal surgery is related to surgical, patient and anaesthetic risk factors. A high preoperative diastolic blood pressure and profound intraoperative hypotension combined with complex surgery, marked by a blood loss of ≥250 mL and the occurrence of intraoperative adverse events, is associated with an increased risk of developing anastomotic leakage.
Keywords: Anastomotic leakage, Blood pressure, Colorectal surgery
Introduction
Anastomotic leakage is a serious complication occurring in gastrointestinal surgery. Morbidity and mortality increase considerably after the development of an anastomotic leakage. Several factors such as obesity [1], ASA score, emergency surgery [2], lower anastomotic level [3], male gender [4], smoking or alcohol abuse [5, 6] and perioperative fluid management have been identified as independent risk factors for anastomotic failure.
Tissue ischemia at the site of the anastomosis is frequently cited and implicated as a cause for anastomotic breakdown [7, 8]. During anaesthesia, the blood pressure tends to decrease due to a variety of factors, including direct effects of the anaesthetic, inhibition of the sympathetic nervous system and loss of baroreceptor reflex control of arterial pressure. These changes can result in episodes of intraoperative hypotension and microvascular ischemia.
Although hypertension is not considered to be an independent risk factor for the development of cardiovascular complications [9], patients with pre-existing hypertension are more likely to experience intraoperative blood pressure variability [10]. This has led to a renewed interest in the association between intraoperative hemodynamic variability and adverse postoperative outcomes such as stroke, slow graft function after organ transplantation [11, 12], anastomotic leakage [13] and even 1-year mortality [14].
The influence of aberrant preoperative and intraoperative hemodynamic status on an adverse outcome following colorectal surgery has not been extensively studied. Our objective was to identify pre- and intraoperative predictive factors contributing to the failure of colorectal anastomoses, with a special emphasis on intraoperative blood pressure changes.
Methods
Patients
This prospective observational study was approved by the hospital ethics committee. During a 24-month period, 285 consecutive patients undergoing elective or emergency colorectal surgery with large bowel anastomoses in our institution were evaluated. The procedures included in this study were open or laparoscopic resections of colon or rectum. The reversal of a stoma was categorised as other. Past medical history and demographic data such as age, gender, body mass index (BMI), American Society of Anesthesiologists (ASA) risk classification, smoking and alcohol consumption were also collected. Physical examination and vital signs such as blood pressure and heart rate were recorded preoperatively in the outpatient clinic.
Anaesthetic procedure
Preoperative beta blockers were continued until surgery. All patients were premedicated with diazepam 10 mg orally 60 min before induction. After arrival in the operating theatre, electrocardiogram tracing from leads II and V5 were displayed continuously. An intravenous drip and radial arterial line were inserted. The urinary bladder was catheterized in all patients. Unless contraindicated, all patients received an epidural catheter, at a level between T6 and T10. Before induction, all patients received an epidurally administered bolus injection of a mixture of levobupivacaine 0.5% and sufentanil 5 μg/mL. Following induction of general anaesthesia with intravenously administered propofol, sufentanil and rocuronium, endotracheal intubation was performed. Controlled ventilation was adjusted to maintain end tidal CO2 between 35 and 45 mmHg. Anaesthesia was maintained with sevoflurane and 70% nitrous oxide in oxygen, muscle relaxation was preserved with incremental doses of rocuronium. A nasogastric tube was inserted and subsequently removed at the end of surgery. Central venous lines were only inserted on indication. Blood losses were accurately assessed and replaced by blood (packed cells) and fresh frozen plasma when the haemoglobin level fell under 8 g/dL (5.0 mmol/L). Initial blood losses were substituted with intravenous colloids. A base infusion of Ringer’s lactate, 2–4 mL/kg/h was administered throughout the operation. Blood and intravenous fluids were warmed before administration. A heated forced air blanket was used to prevent a significant fall in body temperature. In the presence of insufficient analgesia (increased heart rate and blood pressure and/or signs of lacrimation and sweating), a bolus of sufentanil (10 μg) was administered intravenously. Intraoperative blood pressure changes were calculated as a relative decrease (>25% and >40%) in systolic and diastolic blood pressure from preoperative baseline values. If mean blood pressure decreased under 65 mmHg, an intravenous vasopressive agent was administered. Postoperatively an epidural patient controlled analgesia pump was used to provide analgesia.
Surgical procedure
Surgical factors such as previous abdominal surgery, preoperative radiotherapy, the indication for surgery, duration of surgery, complications during surgery and postoperative data were prospectively collected and recorded. All included patients, whether with benign or malignant pathology, entered a multi-modal rehabilitation program. Prior to surgery all patients were informed in detail about the perioperative enhanced recovery protocol, and were given an estimated length of stay. Families were also encouraged to participate, and to motivate the patient during the postoperative recovery.
Patients particularly at risk for respiratory complications received a preoperative consultation by a physiotherapist. Patients received carbohydrate-loaded drinks until 2 h before surgery, and received no bowel preparation. In cases of surgery on the left-sided colon or rectum, patients received an enema on the morning of the day of surgery. Perioperative antibiotics were given as a single intravenous shot of 2 g of cefazolin and 500 mg of metronidazole. The trans-urethral urinary catheter was removed when patients could adequately mobilize. All patients were encouraged to be ambulant on the first postoperative day.
The decision to operate laparoscopically was based on patient characteristics (previous surgery, co-morbidity) and tumour characteristics (size, complexity, involvement of surrounding structures). Drains were only used on indication and in case of surgery in the lower pelvis.
All anastomoses were handsewn, except for colorectal anastomoses, which were achieved using a circular stapler. Gastric tubes were removed postoperatively before leaving the recovery room. Oral fluid intake was commenced on the same day as surgery. Oral food intake was commenced the day after surgery.
Anastomotic leakage
Anastomotic leakage was suspected on clinical indications such as fever, tachycardia, pain, tenderness, peritonitis or purulent/faecal discharge from a drain. All suspected anastomotic leaks were proven by CT scan, ultrasound or after operative evidence was obtained.
Variables and risk factors
Various independent clinical variables were analysed. Patient age and body mass index were evaluated as continuous variables. Gender, smoking, co-morbidity and physical status (ASA ≤2 or ≥3) were evaluated as categorical variables. The use of alcohol was analysed as a categorical variable (≤2 or ≥3 units a day). Indication for operation was categorised as carcinoma, benign or other. The occurrence of an intraoperative complication such as lesion of the spleen, bladder, ureter or ileum, severe bleeding or positive air bubble test was analysed as a categorical variable. Duration of surgery was evaluated as a continuous variable. Blood loss was evaluated as a continuous and categorical variable (<250 and ≥250 mL). Preoperative diastolic (<90 and ≥90 mmHg) and systolic (<150 and ≥150 mmHg) blood pressures were evaluated as continuous and categorical variable. The relative decrease in systolic and diastolic blood pressure from baseline values (preoperative measurements) during the operation were evaluated as continuous (in minutes) and categorical (>25% and >40%) variables.
Statistical analysis
The main object of this study was to identify potential predictors for anastomotic leakage. To identify these potential risk factors, univariate tests were performed using Fisher’s exact test (on categorical variables) and the Wilcoxon–Mann–Whitney test (on continuous variables), both with the binary outcome of anastomotic leakage. The analysis was done using the R-project statistical package (R Foundation for Statistical Computing, 2010, Vienna, Austria). P values of less than 0.05 were considered to be significant. But at this relatively low number of events, variables with P values below 0.3 may still be considered potential predictors and should where possible be included in further studies.
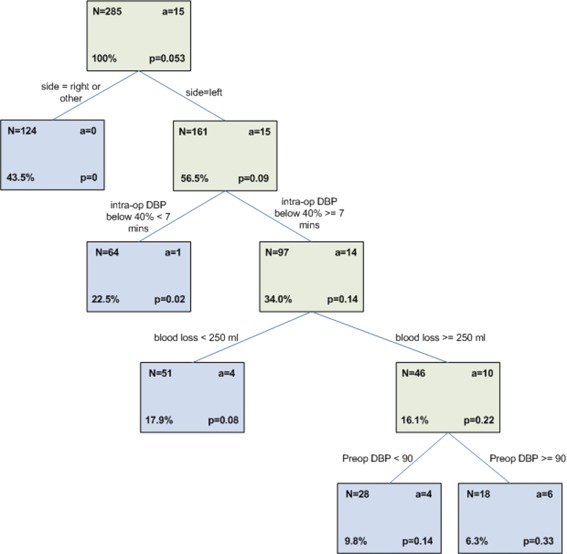
A decision tree was created to identify subgroups with an increased risk of anastomotic leakage. As the statistics are low, the resulting tree should not be used as a predictive model for clinical use. Recursive partitioning using the CHAID algorithm (chi-squared automatic interaction detector) was used to build the decision tree, furthermore the Chordiant Predictive Analytics software (Chordiant Software, 2010, Cupertino, USA) was used.
Results
During the study period of 24 months, 285 ASA I–III patients underwent colorectal surgery with large bowel anastomoses. Of these 285 patients, 263 patients were scheduled for elective and 22 for emergency surgery. The patient characteristics are shown in Table 1 and the surgical history of patients in Table 2. Over 61% (175) of the patients had a malignancy, and in 14% of the patients (40) there was an ‘other’ indication for surgery such as reversal of a stoma.
Table 1.
Patient characteristics
| Variable | Total cohort (n = 285) | Cases with leakage (n = 15) | Cases without leakage (n = 270) | P value |
|---|---|---|---|---|
| Age (mean ± SD), years | 67 ± 14 | 64 ± 11 | 67 ± 14 | 0.395 |
| Age ≥80 years | 50 (17.5%) | 1 (6.7%) | 49 (18.1%) | 0.483 |
| Gender | ||||
| Male | 149 (52.3%) | 9 (60%) | 140 (51.9%) | 0.603 |
| Female | 136 (47.7%) | 6 (40%) | 130 (48.1%) | |
| BMI (mean ± SD) | 25.5 ± 3.8 | 26.6 ± 3.2 | 25.4 ± 3.9 | 0.141 |
| Pts with severe co-morbidity (ASA ≥3) | 27 (9.5%) | 1 (6.7%) | 26 (9.6%) | >0.999 |
| MET ≤4 | 30 (10.5%) | 1 (6.7%) | 29 (10.7%) | >0.999 |
Data expressed as mean ± SD or number (percentage)
BMI body mass index. ASA physical status classification system according to the American Society of Anesthesiologists. MET metabolic equivalent of the task [20]
Table 2.
Surgical history
| Variable | Total cohort (n = 285) | Cases with leakage (n = 15) | Cases without leakage (n = 270) | P value |
|---|---|---|---|---|
| Smoking | 99 (34.7%) | 8 (53.3%) | 91 (33.7%) | 0.262 |
| Alcohol ≥3 glasses/day | 14 (4.9%) | 2 (13.3%) | 12 (4.4%) | 0.114 |
| Indication | ||||
| Carcinoma | 175 (61.4%) | 12 (80%) | 163 (60.4%) | 0.234 |
| Benign | 70 (24.6%) | 3 (20%) | 67 (24.8%) | |
| Other | 40 (14.0%) | 0 | 40 (14.8%) | |
| Previous abdominal surgery | 126 (44.2%) | 3 (20%) | 123 (45.6%) | 0.642 |
| Preoperative radiotherapy | 20 (7.0%) | 3 (20%) | 17 (6.3%) | 0.078 |
In Table 3 the univariate analysis of the risk factors for anastomotic leakage is shown. In 17 cases (6%), an intraoperative adverse event (such as a lesion of the spleen, ureter, bladder or ileum, torsion of the anastomosis, acute massive bleeding or positive air bubble test) occurred. The anastomotic leak rate was 5.3% (15 out of 285).
Table 3.
Univariate analysis of the risk factors for anastomotic leakage
| Variable | Total cohort (n = 285) | Cases with leakage (n = 15) | Cases without leakage (n = 270) | P value |
|---|---|---|---|---|
| Surgery | ||||
| Elective | 263 (92.3%) | 14 (93.3%) | 249 (92.2%) | >0.999 |
| Acute | 22 (7.7%) | 1 (6.7%) | 21 (7.8%) | >0.999 |
| Laparotomy | 182 (63.9%) | 10 (66.7%) | 172 (63.7%) | >0.999 |
| Laparoscopy | 103 (36.1%) | 5 (33.3%) | 98 (36.3%) | >0.999 |
| Of which conversion | 28 (27.2%) | 2 (40%) | 26 (26.5%) | 0.649 |
| Anastomosis, right | 84 (29.5%) | 0 | 84 (31.1%) | >0.999 |
| Anastomosis, left | 161 (56.5%) | 15 (100%) | 146 (4.1%) | <0.001 |
| Other | 40 (14.0%) | 0 | 40 (14.8%) | >0.999 |
| Duration of surgery (min) | 241 ± 82 | 252 ± 67 | 240 ± 82 | 0.306 |
| Intraoperative adverse eventa | 17 (6.0%) | 3 (20%) | 14 (5.2%) | 0.050 |
| Total intraoperative fluid intake (mL) | 3513 ± 1315 | 3523 ± 1040 | 3513 ± 1331 | 0.915 |
| Blood loss (mL) | 387 ± 437 | 423 ± 296 | 384 ± 446 | 0.015 |
| Blood loss ≥250 mL | 87 (30.5%) | 10 (66.7%) | 77 (28.5%) | 0.003 |
| Neuraxial technique | 250 (87.7%) | 13 (86.7%) | 237 (87.8%) | 0.390 |
| Preoperative DBP (mmHg) | 81 ± 12 | 87 ± 10 | 81 ± 13 | 0.019 |
| DBP ≥90 mmHg | 79 (27.7%) | 9 (60%) | 70 (25.9%) | 0.008 |
| Preoperative SBP (mmHg) | 141 ± 20 | 136 ± 17 | 142 ± 20 | 0.398 |
| SBP ≥150 mmHg | 92 (32.3%) | 4 (26.7%) | 88 (32.6%) | 0.780 |
| DBP: intraoperative ↓ >25% (yes or no) | 267 (93.7%) | 15 (100%) | 252 (93.3%) | >0.999 |
| Duration (min), mean ± SD | 112 ± 84 | 137 ± 92 | 111 ± 84 | 0.278 |
| Intraoperative ↓ DBP >40% (yes or no) | 209 (73.3%) | 14 (93.3%) | 195 (72.2%) | 0.127 |
| Duration (min), mean ± SD | 38 ± 57 | 51 ± 57 | 37 ± 57 | 0.049 |
| SBP: intraoperative ↓ >25% (yes or no) | 263 (92.3%) | 15 (100%) | 248 (91.9%) | >0.999 |
| Duration (min), mean ± SD | 93 ± 71 | 86 ± 58 | 93 ± 72 | 0.862 |
| Intraoperative ↓ SBP >40% (yes or no) | 205 (71.9%) | 13 (86.7%) | 192 (71.1%) | 0.368 |
| Duration (min), mean ± SD | 27 ± 43 | 22 ± 34 | 28 ± 43 | 0.923 |
| Intraoperative use of vasoactive drugs | 213 (74.7%) | 12 (80%) | 201 (74.4%) | 0.768 |
aIntraoperative adverse events reported: lesion spleen, ureter, bladder or ileum, torsion of the anastomosis, acute massive bleeding, positive air bubble test
A left side anastomosis (P < 0.001) and blood loss as a continuous (P = 0.015) and as a categorical variable of 250 mL or more (P = 0.003) were statistically significant risk factors for developing anastomotic leakage. A preoperative high diastolic blood pressure (P = 0.019) or as categorical variable of more than 90 mmHg (P = 0.008) was also statistically associated with a higher incidence of anastomotic leakage. In 209 cases (73%) the maximum decrease in diastolic blood pressure from baseline was greater than 40%. The median duration of such a decrease in diastolic blood pressure was 13 min. From these procedures, 14 cases of anastomotic leakage resulted (P = 0.127 for the categorical test and P = 0.049 for the continuous test of the duration of the decrease).
In our cohort only 20 out of 285 patients (7%) underwent preoperative radiotherapy, with 3 out of 20 patients developing an anastomotic leak (P = 0.078). Four other factors may be considered potential predictors (P < 0.30), suggesting that they might be related to anastomotic failure: BMI (P = 0.141), smoking (P = 0.262), severe alcohol consumption (≥3 units a day, P = 0.114), and the surgical indication being a carcinoma (P = 0.234, see Tables 1 and 2).
Recursive partitioning using the CHAID algorithm resulted in the decision tree shown in Fig. 1. Notably, this tree identifies a subgroup of patients with a high incidence of leakage that has a high preoperative diastolic blood pressure combined with a significant decrease in diastolic blood pressure during the operation. The subgroup consists of patients with left-sided resection, blood loss of more than 250 mL, preoperative diastolic blood pressure of more than 90 mmHg and a long (more than 7 min) period of relative decrease in diastolic blood pressure of more than 40% from baseline during the operation. This subgroup consists of 18 patients of which 6 developed an anastomotic leakage.
Fig. 1.
Decision tree: The overall risk of developing an anastomotic leak is 5.3% in our population. The subgroup of patients after left-sided resection had an increased risk of 9%. The patients who had a relative decrease in DBP of more than 40% during the operation had an increased risk of 14%, and their risk further increased to 22% if intraoperative blood loss was ≥250 mL. Patients in this subgroup who had a preoperative DBP of ≥90 mmHg had a 33% increased risk of developing an anastomotic leak
Most patients received epidural analgesia (253 out of 285). In four patients the epidural failed to provide adequate analgesia and was removed on the day of surgery (day 0). The median duration of continuation of patient controlled epidural analgesia was 2 (1–10) days, with a mean of 2.59 days. The median duration of hospital stay was 6 (1–105) days. Postoperative complications ranging from pneumonia to wound infection occurred in 101 patients (35%). Of the patients with anastomotic leakage, 93% also developed a second complication (14 out of 15). The mortality rate associated with anastomotic leak was 13% (2 out of 15). The overall mortality rate in the group of patients without anastomotic failure was 0.7% (2 out of 270, see Table 4).
Table 4.
Outcome
| Total cohort (n = 285) | Cases with leakage (n = 15) | Cases without leakage (n = 270) | P value | |
|---|---|---|---|---|
| Development complicationsa | 101 (35.4%) | 14 (93.3%) | 87 (32.2%) | <0.001 |
| Hospital stay (days) | 10 ± 11 | 29 ± 24 | 9 ± 9 | <0.001 |
| Mortality | 4 (1.4%) | 2 (13.3%) | 2 (0.7%) | 0.015 |
aOther than anastomotic leak: pneumonia, anaphylactic or septic shock, bleeding, wound infection, abscesses, oedema, bladder dysfunction, gastric perforation
Discussion
There are numerous reports over the association between surgical procedures and surgical outcome such as anastomotic leakage. However, aberrant preoperative and intraoperative hemodynamic status and their influence on adverse outcome after colorectal surgery have not been analysed in detail. Our current study investigates associations between adverse surgical outcome, in particular anastomotic leakage, and intraoperative hemodynamic aberrations. The occurrence of preoperative diastolic hypertension, defined as DBP ≥90 mmHg was independently associated with the occurrence of anastomotic leakage, possibly indicating a higher susceptibility for microvascular ischemia due to hypotension at the site of anastomosis. Also severe intraoperative relative hypotension (a relative decrease in diastolic blood pressure of more than 40%) was associated with an increased incidence of anastomotic leakage. Although the decrease in diastolic blood pressure was accompanied by a decrease in systolic blood pressure, this drop was less severe and was not of statistical significance. This is probably due to the relatively small population size in our study. The identification of high diastolic blood pressure as a risk factor in our small cohort could be a stimulation to find confirmation in a larger study and in other hospital populations. This outcome may have important consequences when deciding which patient deserves a covering ileostomy and which patient has such a limited risk for anastomotic failure that defunctioning of the anastomotic site is not necessary. Furthermore, an increased awareness of the importance of intraoperative blood pressure control may be necessary.
Besides the vital signs used in the current study, biochemical indicators such as systemic arterial hyperlactatemia may also be important to correctly interpret microcirculation. The systemic concentrations of lactate, however, may vary widely due to overall hemodynamic state and liver function. It has been demonstrated by Deeba et al. [15] that rapid intraluminal sampling microdialysis of glucose and lactate were important parameters for detection of bowel ischemia. Therefore, in a future prospective trial it might be interesting to add intraluminal glucose and lactate measurements.
Various articles describe an increased chance of anastomotic leakage in males because of the smaller pelvis; however, no significant difference was found in our study group. In our cohort colonic surgery and rectal surgery was combined which may be the reason for the lack of difference. Furthermore, in this study, the use of steroids is not evaluated.
All anastomoses were handsewn, except for colorectal anastomoses, which were achieved using a circular stapler. Stapled anastomosis with a circular device is a well-established technique for anastomosis after sigmoid resection or low anterior resection. Results of stapled anastomoses are not inferior to handsewn methods, and therefore, the rate of left-sided anastomotic leak is probably not a result of the use of stapling devices [16, 17].
In our study population, most patients (88%) received (patient controlled) epidural analgesia. We did not control for possible severe sympathicolysis caused by the neuraxial blockade, but by using patient controlled analgesia and avoiding motor blockade, it was our intention to minimize the influence on postoperative blood pressure. With patients undergoing laparoscopic resections, a neuraxial technique might not be necessary and with regards to blood pressure control has to be used with caution.
In contrast to findings in previous studies, we did not find long operation duration as a risk factor for anastomotic leakage. But, the occurrence of intraoperative adverse events (P = 0.050) was an indicator for the development of anastomotic leakage. Intraoperative adverse events could be an indication of more complex surgery. Acute massive bleeding was not specifically mentioned as a complication in the leakage group (see Table 5 and 6), but blood loss of 250 mL or more proved to be a significant independent risk factor for anastomotic failure. The cutoff point of 250 mL for this continuous variable of blood loss was arbitrary. A recent study from Telem et al. [18] pointed out that blood loss of more than 200 mL is an independent risk factor. Arbitrarily chosen or not, there are indications that subsequent blood loss during operation is a strong predictor for the development of anastomotic leakage. In our study only 12 out of 285 patients (4.2%) needed a blood transfusion of which 1 patient developed an anastomotic leak. Despite the difference in blood loss between the groups who developed anastomotic leakage, blood transfusion-associated immunosuppression is presumably not an obvious explanation.
Table 5.
Characteristics of patients with anastomotic leakage
| ID | Procedure | Indication | M/F | Age | BMI | ASA | MET | Alcohol | RT |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Low anterior resection | Malignancy | F | 74 | 23 | 3 | ≤4 | <3 | Yes |
| 2 | High anterior resection | Malignancy | M | 73 | 29 | 1 | 5 to 8 | None | No |
| 3 | Hemicolectomy | Malignancy | F | 85 | 27 | 2 | 5 to 8 | <3 | No |
| 4 | High anterior resection (conversion) | Diverticulitis | M | 68 | 25 | 1 | 5 to 8 | <3 | No |
| 5 | Low anterior resection | Malignancy | M | 50 | 28 | 2 | ≥9 | >6 | No |
| 6 | High anterior resection | Diverticulitis | F | 77 | 29 | 2 | 5 to 8 | None | No |
| 7 | High anterior resection | Stenosis | M | 73 | 24 | 1 | 5 to 8 | <3 | No |
| 8 | Low anterior resection | Malignancy | M | 54 | 24 | 1 | 5 to 8 | <3 | Yes |
| 9 | Colectomy (conversion) | Malignancy | M | 63 | 26 | 1 | 5 to 8 | <3 | Yes |
| 10 | Low anterior resection | Malignancy | M | 67 | 25 | 1 | 5 to 8 | 3 to 6 | No |
| 11 | High anterior resection | Malignancy | F | 66 | 28 | 2 | 5 to 8 | None | No |
| 12 | High anterior resection | Malignancy | F | 57 | 32 | 1 | 5 to 8 | <3 | No |
| 13 | Low anterior resection | Malignancy | M | 44 | 21 | 2 | 5 to 8 | <3 | No |
| 14 | Low anterior resection | Malignancy | F | 76 | 30 | 2 | ≥9 | <3 | No |
| 15 | Low anterior resection | Malignancy | M | 55 | 30 | 2 | ≥9 | <3 | No |
Table 6.
Intraoperative and postoperative complications of patients with anastomotic leakage
| ID | Blood pressure (mmHg) | Time ↓ SBP >40% (min) | Time ↓ DBP > 40% (min) | Intraoperative adverse events | Duration of surgery (min) | Blood loss (mL) | Postoperative complication | Hospital stay (days) |
|---|---|---|---|---|---|---|---|---|
| 1 | 128/85 | 11 | 42 | 211 | 300 | Wound infection | 25 | |
| 2 | 151/90 | 126 | 109 | 317 | 600 | Pneumonia, wound infection | 34 | |
| 3 | 158/61 | 47 | 7 | 297 | 250 | Stomach perforation | 9 | |
| 4 | 130/95 | 5 | 8 | 306 | 300 | 5 | ||
| 5 | 122/75 | 0 | 0 | 298 | <150 | Multiple abcesses | 60 | |
| 6 | 110/90 | 3 | 128 | Lesion bladder | 393 | 1,180 | Septic shock | 27 |
| 7 | 165/95 | 1 | 26 | Lesion ureter | 181 | 400 | Double J catheter ureter | 15 |
| 8 | 140/80 | 0 | 15 | Torsion anastomosis | 158 | 250 | Pneumonia | 6 |
| 9 | 144/99 | 55 | 89 | 305 | 300 | Abdominal compartment syndrome, pneumonia | 4 | |
| 10 | 105/80 | 5 | 49 | 215 | 200 | Wound infection | 49 | |
| 11 | 136/92 | 29 | 42 | 299 | 200 | Wound infection | 28 | |
| 12 | 120/90 | 6 | 20 | 234 | <150 | Wound infection | 30 | |
| 13 | 130/95 | 2 | 204 | 366 | 800 | Wound infection | 33 | |
| 14 | 154/87 | 37 | 7 | 315 | 300 | Wound dehiscence | 94 | |
| 15 | 145/95 | 10 | 25 | 329 | <150 | Cardiac arrythmias | 19 |
Patients 3 and 9 died during the study, see also Table 4 (Outcome)
Patients were evaluated up until 14 days post-discharge. Since anastomotic leakages are detected anywhere from 3 to 40 days postoperatively [19], it is possible that some of the anastomotic leakages were not evaluated. Clinically significant leaks would however almost certainly have been identified, since all patients received follow-up in our surgical outpatient clinic.
The sample size of 285 procedures with 15 anastomotic leakages does not allow the use of multivariate logistic regression. Therefore, this study has focused on a univariate identification of potential risk factors. The risk factors appointed in this study need further evaluation in a large prospective trial. We should be cautious with the interpretation of the results of this small study, but we can point out the potential importance of intraoperative blood pressure control.
Conclusion
In our study several preoperative and intraoperative factors were demonstrated to be associated with the postoperative development of an anastomotic leak. In particular, high preoperative diastolic blood pressure and longer episodes of severe intraoperative hypotension, combined with complex surgery (marked by blood loss of ≥250 mL) and the occurrence of intraoperative adverse events, resulted in a significant increase in the development of anastomotic leakage. This could be an indication that hypotension should be avoided, particularly in patients with high preoperative blood pressures.
Proximal diversion does not prevent anastomotic leakage and leads in its own right to morbidity. In patients with multiple risk factors for the development of an anastomotic leak, however, one can imagine that a proximal diversion could lessen the dreaded sequelae should a leak occur.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Biondo S, Pares D, Kreisler E, et al. Anastomotic dehiscence after resection and primary anastomosis in left-sided colonic emergencies. Dis Colon Rectum. 2005;48:2272–2280. doi: 10.1007/s10350-005-0159-9. [DOI] [PubMed] [Google Scholar]
- 2.Choi HK, Law WL, Ho JW. Leakage after resection and intraperitoneal anastomosis for colorectal malignancy: analysis of risk factors. Dis Colon Rectum. 2006;49:1719–1725. doi: 10.1007/s10350-006-0703-2. [DOI] [PubMed] [Google Scholar]
- 3.Yeh CY, Changchien CR, Wang J-Y, et al. Pelvic drainage and other risk factors for leakage after elective anterior resection in rectal cancer patients: a prospective study of 978 patients. Ann Surg. 2005;241:9–13. doi: 10.1097/01.sla.0000150067.99651.6a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lipska MA, Bisset IP, Parry BR, Merrie AE, et al. Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ J Surg. 2006;76:579–585. doi: 10.1111/j.1445-2197.2006.03780.x. [DOI] [PubMed] [Google Scholar]
- 5.Sorensen LT, Jorgensen T, Kirkeby LT, Skovdal J, Vennits B, Wille-Jorgensen P. Smoking and alcohol abuse are major risk factors for anastomotic leakage in colorectal surgery. Br J Surg. 1999;86:927–931. doi: 10.1046/j.1365-2168.1999.01165.x. [DOI] [PubMed] [Google Scholar]
- 6.Kingham TP, Pachter HL. Colonic anastomotic leak: risk factors, diagnosis and treatment. J Am Coll Surg. 2009;208(2):269–278. doi: 10.1016/j.jamcollsurg.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 7.Boyle NH, Manifold D, Jordan MH, Mason RC. Intraoperative assessment of colonic perfusion using scanning laser Doppler flowmetry during colonic resection. J Am Coll Surg. 2000;191:504–510. doi: 10.1016/S1072-7515(00)00709-2. [DOI] [PubMed] [Google Scholar]
- 8.Vignali A, Gianotti L, Braga M, et al. Altered microperfusion at the rectal stump is predictive for rectal anastomotic leak. Dis Colon Rectum. 2000;43:76–82. doi: 10.1007/BF02237248. [DOI] [PubMed] [Google Scholar]
- 9.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Struijker Boudier HA, Zanchetti A. The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2007;28:1462–1536. doi: 10.1093/eurheartj/ehm236. [DOI] [PubMed] [Google Scholar]
- 10.Goldman L, Caldera DL. Risks of general anesthesia and elective operation in the hypertensive patient. Anesthesiology. 1979;50:285. doi: 10.1097/00000542-197904000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Reich DL, Wood RK, Jr, Emre S, Bodian CA, Hossain S, Krol M, Feierman D. Association of intraoperative hypotension and pulmonary hypertension with adverse outcomes after orthoptopic liver transplantation. J Cardiothorac Vasc Anesth. 2003;17(6):699–702. doi: 10.1053/j.jvca.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Sandid MS, Assi MA, Hall S. Intraoperative hypotension and prolonged operative time as risk factors for slow graft function in kidney transplant recipients. Clin Transplant. 2006;20:762–768. doi: 10.1111/j.1399-0012.2006.00567.x. [DOI] [PubMed] [Google Scholar]
- 13.Zakrison T, Nascimento BA, Jr, Tremblay LN, Kiss A, Rizoli SB. Perioperative vasopressors are associated with an increased risk of gastrointestinal anastomotic leakage. World J Surg. 2007;31:1627–1634. doi: 10.1007/s00268-007-9113-4. [DOI] [PubMed] [Google Scholar]
- 14.Bijker JB, van Klei WA, Vergouwe Y, Eleveld DJ, van Wolfswinkel L, Moons KG, Kalkman CJ. Intraoperative hypotension and 1-year mortality after noncardiac surgery. Anesthesiology. 2009;111:1217–1226. doi: 10.1097/ALN.0b013e3181c14930. [DOI] [PubMed] [Google Scholar]
- 15.Deeba S, Corcoles EP, Hanna BG, Pareskevas P, Azis O, Boutelle MG, Darzi A. Use of rapid sampling microdialysis for intraoperative monitoring of bowel ischemia. Dis Colon Rectum. 2008;51:1408–1413. doi: 10.1007/s10350-008-9375-4. [DOI] [PubMed] [Google Scholar]
- 16.Lustosa SA, Matos D, Atallah AN, Castro AA (2001) Stapled versus handsewn methods for colorectal anastomosis surgery. Cochrane Database Syst Rev 2001;(3):CD003144 [DOI] [PubMed]
- 17.MacRae HM, McLeod RS. Handsewn versus stapled anastomoses in colon and rectal surgery: a meta-analysis. Dis Colon Rectum. 1998;41(2):180–189. doi: 10.1007/BF02238246. [DOI] [PubMed] [Google Scholar]
- 18.Telem DA, Chin EH, Nguyen SQ, Divino CM. Risk factors for anastomotic leak following colorectal surgery. Arch Surg. 2010;145(4):371–376. doi: 10.1001/archsurg.2010.40. [DOI] [PubMed] [Google Scholar]
- 19.Hyman N, Manchester TL, Osler T, Burns B, Cataldo PA. Anastomotic leaks after intestinal anastomosis: it’s later than you think. Ann Surg. 2007;245:254–258. doi: 10.1097/01.sla.0000225083.27182.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jette M, Sidney K, Blumchen G. Metabolic equivalents (METs) in exercise testing, exercise prescription and evaluation of functional capacity. Clin Cardiol. 1990;13:555–565. doi: 10.1002/clc.4960130809. [DOI] [PubMed] [Google Scholar]