Abstract
Background: There is continued debate as to the optimal strategy for diagnosis and management of primary hyperparathyroidism (PHPT).
Aim: To compare the strategies used for the diagnosis and management of PHPT by physicians in five European countries.
Design: Questionnaire-based survey.
Methods: Physicians in France, Germany, the UK, Italy and Spain were invited to participate in the survey which was conducted using a web-based interface and were included in the evaluation if they had treated a minimum of four patients suffering from PHPT in the past year.
Results: A total of 421 physicians completed the survey. The majority of respondents were endocrinologists (68%) but other specialities included rheumatologists (10.9%), internists (11.8%) and urologists (9.2%). Diagnostic methods were similar across different countries and specialities but there were significant differences in the proportion of physicians who recommended parathyroidectomy in asymptomatic patients with indications for surgery according to the 2002 National Institutes of Health (NIH) consensus conference statement (χ2 = 26.1, P < 0.001). The proportion of patients referred for surgery ranged from 32% in Italy to 66% in Spain with intermediate values in Germany (64%), France (55%) and the UK (53%). Conversely, pharmacological therapy was used most frequently for these patients in Italy (32%) and least frequently in Spain (14%).
Conclusion: Significant differences exist in the management of patients with asymptomatic PHPT in countries across Europe who have accepted indications for surgery according to the NIH consensus statement. Further research will be required to explore the reasons for this and to determine if these differences affect the clinical outcome of PHPT.
Introduction
Primary hyperparathyroidism (PHPT) is a common disease which affects 0.1–2% of populations, with a 3:1 female preponderance.1 The clinical presentation of PHPT has changed dramatically over the past 30 years from a symptomatic disorder associated with severe hypercalcaemia, renal stones and bone disease to a condition that is often asymptomatic, which is picked up as an ‘incidental’ finding on biochemical screening. Nonetheless, patients with mild PHPT can progress to develop symptoms and complications, and epidemiological studies have suggested that untreated PHPT may be associated with an increased risk of cardiovascular disease.2
The optimal strategy for the diagnosis and management of PHPT has been the subject of several position statements, including those which emerged from National Institutes of Health (NIH) Consensus Development Conferences in 20023 and the third international workshop on primary hyperparathyroidism in 20094–8 and that published by the American Association of Clinical Endocrinologists and Endocrine Surgeons in 2005.9 Although these statements have been endorsed by some European organizations, including the European Calcified Tissues Society (www.ectsoc.org), it is unclear to what extent European physicians adhere to these recommendations for the diagnosis and management of PHPT. In view of this, the aim of the present study was to evaluate to what extent physicians in Europe who regularly manage PHPT follow these guidelines and to determine if there is variation across Europe in the management of this disease. To achieve this aim we conducted a web-based survey of the clinical strategies used by endocrinologists, rheumatologists, internists and urologists to diagnose and manage PHPT in France, Germany, the UK, Italy and Spain in 2009.
Methods
Participants
Potential participants in this study were recruited to a panel by various methods including telephone, face-to-face and referral recruitment processes. Panel members were then verified as registered physicians. For the purposes of this study, specifically endocrinologists, rheumatologists, internist or urologists in the countries of interest (France, Germany, the UK, Italy and Spain) were invited by an email to participate in a survey on the diagnosis and management of PHPT. Respondents were only included in the evaluation if they had been practising for ≥3 years, had treated a minimum of four PHPT patients a year, and had spent >50% of their time treating patients. Respondents were excluded if they had taken part in any market research of a similar topic in the last 3 months. The survey was conducted online between 12 and 30 June 2009. The aim was to collect data from 80 clinicians per country to provide a reasonable sample size for analysis although we did not perform any specific power calculations before deciding upon the sample size.
Questionnaire
The survey topics and the available answer options are summarized in Supplementary Table 1. They included questions regarding the methods used for the diagnosis of PHPT, the respondents' preferred management strategy for symptomatic and asymptomatic PHPT, and if diagnosis and management strategies were in accordance with current guidelines.3–9 Additional questions were aimed at excluding ineligible participants according to the criteria mentioned previously (data not shown).
Statistical analysis
Differences in management strategies employed by respondents in different groups were analysed by chi-square test.
Results
Demographics of respondents
A total of 1269 physicians initially responded to an email invitation to participate. Responses to the questionnaire were obtained from 421 eligible physicians from five European countries as summarized in Table 1. The main reasons for this difference were that the physicians did not fulfil the inclusion criteria (82%) or did not complete the questionnaire (9%). The majority of respondents were endocrinologists and the distribution of specialities represented in the survey was similar across all countries. The average number of patients seen per year varied across countries, with the lowest number in France [mean ± standard deviation, 26 ± 35; median (Q1, Q3), 20 (10, 30)] and the highest in the UK [mean ± SD, 67 ± 65; median (Q1, Q3), 45 (25, 81)].
Table 1.
Respondents by speciality and country
| Total | France | Germany | UK | Italy | Spain | |
|---|---|---|---|---|---|---|
| Endocrinologist | 286 (67.9) | 55 (68.8) | 52 (65.0) | 65 (69.9) | 61 (69.3) | 53 (66.3) |
| Rheumatologist | 46 (10.9) | 10 (12.5) | 8 (10.0) | 10 (10.8) | 10 (11.4) | 10 (12.5) |
| Internist | 50 (11.9) | 10 (12.5) | 10 (12.5) | 10 (10.8) | 11 (12.5) | 10 (12.5) |
| Urologist | 39 (9.3) | 5 (6.3) | 10 (12.5) | 8 (8.6) | 6 (6.8) | 10 (8.8) |
| Total | 421 (100) | 80 (100) | 80 (100) | 93 (100) | 88 (100) | 80 (100) |
Values shown are number (%) of respondents.
Diagnosis of PHPT
The diagnostic tests used in patients suspected to have PHPT were similar across Europe. The vast majority of respondents (98%) reported that parathyroid hormone (PTH) was measured as part of the diagnostic work up with no significant difference between countries. Other tests used frequently were serum calcium (85%), serum creatinine (96%) and 24-h urinary excretion of calcium (85%).
Adherence to guidelines
Approximately a third of respondents in each country (34–44%) reported that they adhered to the NIH 2002 guidelines3 when treating PHPT (Table 2), with no significant difference between countries. The majority of the remaining respondents followed other guidelines and only a very limited number of respondents in each country did not always follow any guidelines when making treatment decisions.
Table 2.
Do your treatment decisions always follow guidelines?
| France | Germany | UK | Italy | Spain | |
|---|---|---|---|---|---|
| NIH | 50 (43.9) | 51 (41.2) | 44 (37.6) | 42 (35.0) | 39 (33.9) |
| AACE/AAES | 26 (22.8) | 24 (19.8) | 16 (13.7) | 30 (25.0) | 34 (29.6) |
| 3rd Int. Workshop | 6 (5.3) | 14 (11.6) | 14 (12.0) | 25 (20.8) | 24 (20.9) |
| National | 6 (5.3) | 19 (15.7) | 24 (20.5) | 14 (11.7) | 13 (11.3) |
| Other | 23 (20.2) | 10 (8.3) | 18 (15.4) | 9 (7.5) | 4 (3.5) |
| No | 3 (2.6) | 3 (2.5) | 1 (0.9) | 0 (0) | 1 (0.9) |
Values are numbers (%) of respondents who followed guidelines. AACE/AAES, American Society of Clinical Endocrinologists/American Society of Endocrine Surgeons.
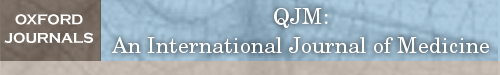
Management of symptomatic PHPT
The preferred management strategies for symptomatic PHPT are summarized in Figure 1. Parathyroidectomy was the preferred treatment option for 72% of UK respondents and 73.8% of German respondents, whereas this was less favoured by Italian respondents: only 42% recommended parathyroidectomy as first-line treatment. Intermediate values were found for France (63.8%) and Spain (60.0%) and the differences between countries was statistically significant (χ2 = 23.8, P < 0.001). In keeping with these observations, pharmacologic treatment for symptomatic patients was the most favoured first-line option for Italian respondents (44.3%), but this was less favoured by German respondents (16.3%), UK respondents (22.6%), French respondents (25.0%) and Spanish respondents (30.0%) (χ2 = 19.4, P = 0.001).
Figure 1.
Preferred management strategies for symptomatic PHPT. Values (%) are respondents’ answers to the multi-choice Question 11 ‘When a PHPT patient is symptomatic do you … ?’ Respondents chose a single answer from a multi-choice list.
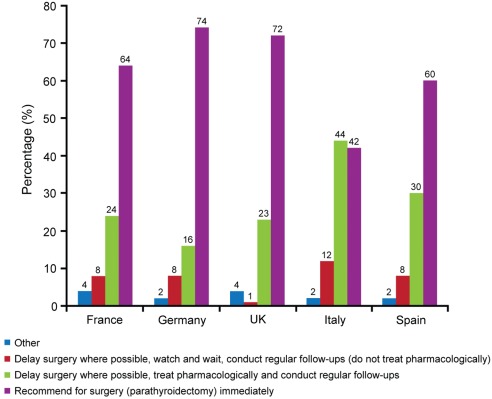
Management of asymptomatic PHPT
The preferred management strategies for a patient with asymptomatic PHPT in different countries are summarized in Figure 2. Asymptomatic PHPT is defined as elevated serum levels of PTH in combination with high or normal serum levels of calcium, all causes of secondary hyperparathyroidism being ruled out, in a patient without symptoms that have been related to this condition.3–9 Few respondents selected parathyroidectomy as the first-line option, but this was more favoured in an asymptomatic patient who had complications such as significant hypercalcaemia [serum calcium >1.0 mg/dl (>0.25 mmol/l) above normal]; hypercalciuria [>400 mg/day (>10 mmoL/day)], impaired renal function or osteoporosis. Between 48.0% and 66.0% of respondents in most countries favoured parathyroidectomy in these patients with the exception of Italy where only 32% would have considered parathyroidectomy as first line. The difference between countries was significant (χ2 = 26.0, P < 0.001). Follow-up with monitoring of serum calcium values, with and without pharmacological treatment, were reasonably popular options for these patients in the UK and Italy, but were less popular in Germany, France and Spain.
Figure 2.
Preferred management strategies for asymptomatic PHPT. Values (%) are respondents’ answers to the multi-choice Question 12 ‘When a PHPT patient is asymptomatic do you … ?’ aRecommendation based on 2002 NIH Consensus Development Guidelines.3
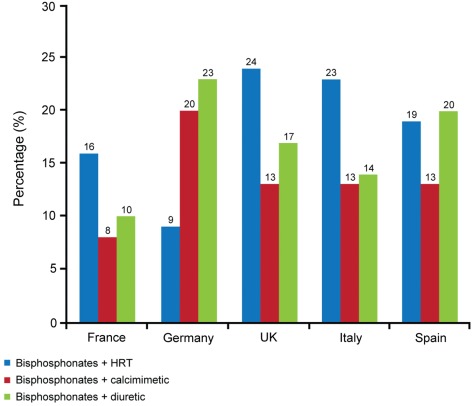
Pharmacologic therapies used in the medical management of PHPT
Respondents were asked about their preferred medical management options when used as an alternative to surgery. Treatment options include bisphosphonate therapy, calcimimetics, diuretics and hormone-replacement therapy (HRT) which includes both oestrogen and oestrogen receptor agonists.
Respondents from all countries selected bisphosphonate therapy as the first-line option they found most suitable (mean ranking) followed by calcimimetics as the second option and the diuretic furosemide as the third. Combination therapy, oestrogen treatment and oestrogen receptor agonists were found to be the less suitable options [in varying order of preference depending on country (Table 3)].
Table 3.
Preferred pharmacological treatment for PHPT
| Ranking, 1–6 (mean) |
|||||
|---|---|---|---|---|---|
| France | Germany | UK | Italy | Spain | |
| Bisphosphonate | 1 (1.91) | 1 (1.88) | 1 (1.68) | 1 (1.99) | 1 (1.90) |
| Calcimimetics | 2 (2.53) | 2 (2.63) | 2 (3.24) | 2 (3.24) | 2 (3.01) |
| Furosemide | 3 (3.91) | 3 (3.61) | 3 (3.89) | 3 (3.89) | 3 (3.83) |
| Combination | 6 (4.41) | 4 (3.79) | 4 (3.94) | 5 (3.94) | 6 (4.11) |
| Oestrogen receptor agonists | 4 (4.04) | 5 (4.39) | 6 (4.19) | 6 (4.01) | 4 (4.10) |
| Oestrogen treatment | 5 (4.20) | 6 (4.71) | 5 (4.05) | 4 (3.93) | 5 (4.05) |
Values are rankings (1 representing the most frequently preferred treatment and 6 the least preferred treatment) based on the median ranking of each treatment modality by country. The mean ranking is provided in parentheses.
As reflected by the mean rankings, it was apparent that most respondents tried three to four individual treatments before trying combination therapy; however, those individual respondents who recorded combination therapy as ranking from 1–3 were required to state the most common combination drug treatments used in the medical management of PHPT along with the percentage of patients that received this combination. These percentages are shown in Figure 3. The three most commonly used combination treatments were bisphosphonate therapy with either HRT, calcimimetic or diuretic therapy.
Figure 3.
Patients receiving preferred combination pharmacological therapies for the treatment of PHPT. Values are estimate percentages of the number of patients with PHPT receiving combination therapy given by those physicians ranking combination therapy from 1–3 (1, most suitable; 6, least suitable).
Differences between specialities
There were no differences between specialities in the approaches to the diagnosis and management of PHPT with one exception: the management of patients with asymptomatic PHPT. For this group of patients, parathyroidectomy was favoured as the first choice treatment by 204/286 endocrinologists (71.3%), compared with 20/51 internists (39.2%), 21/48 rheumatologists (43.7%) and 17/36 urologists (47.2%), a difference that was significant (χ2 = 31.9, P < 0.001).
Discussion
The optimal strategy for the management of PHPT continues to be a subject of considerable debate, probably reflecting the fact that there have been no large-scale randomized studies addressing the long-term effects of surgical versus conservative management for this condition. In the absence of these studies, several reviews, clinical guidelines and position statements have been published by expert groups to help physicians decide upon how best to manage the individual patient.3–9 In the present survey, we did not ask physicians if they were aware of guidelines but only if they managed patients with PHPT according to specific guidelines (Supplementary Table 1). However, most respondents in each country reported that they adhered to a guideline when treating PHPT. The majority of the physicians across the five countries used the 2002 NIH guideline and not the updated 2009 guideline that was the result of the third international workshop on primary hyperparathyroidism. This may, at least in part, be explained by the fact that the present survey was conducted in 2009 at the time of publication of the updated 2009 guideline.
It is generally agreed that parathyroidectomy should be the treatment of first choice for patients with symptomatic PHPT and this was the option favoured by physicians in most European countries, with the notable exception of Italy where only 42% of physicians favoured parathyroidectomy as the treatment of first choice for symptomatic patients. The lack of enthusiasm for surgery in Italy was counterbalanced by a relatively increased preference for pharmacological options: 44% of physicians favoured medical treatment with follow-up.
Few physicians favoured surgery as the first choice treatment option for asymptomatic PHPT without complications, but this was the most popular option in most countries where patients with PHPT had complications such as impaired renal function, hypercalciuria, low bone mineral density (BMD) and more severe hypercalcaemia. A notable exception was Italy, however, where the proportion of physicians who favoured surgery for such patients was only 32.0%.
Medical management of symptomatic PHPT with follow-up was considered to be the treatment of choice by between 16.3% and 44.3% of respondents with the lowest proportion in Germany and the highest in Italy. This approach was favoured less for asymptomatic patients in all countries, with values ranging from 13.0% in Germany to 32.0% in Italy.
Relatively few randomized trials have been conducted to determine how surgery compares with conservative management of patients with PHPT. It has been reported that many patients with asymptomatic PHPT actually suffer from undiagnosed neurocognitive symptoms,10 and a small randomized controlled trial showed that some of these symptoms improved following surgery.11 In an epidemiological study it was reported that mortality is increased in patients with mild hypercalcaemia,12 but this could not be confirmed in another epidemiological study where mortality only was increased among the quartile of patients with the highest serum levels of calcium.13 It has been suggested that conservative treatment should be abandoned for the management of PHPT14 although there is no evidence to suggest that lowering calcium values in these patients, either medically or by parathyroidectomy, is effective in reducing the increased mortality of these subjects.
At the present time several medical therapies are used for the treatment of osteoporosis associated with PHPT, including HRT, raloxifene and bisphosphonates. These drugs have been shown to be effective in increasing BMD values in patients with PHPT but they do not reduce serum calcium values significantly. The calcimimetic cinacalcet has also become available for the treatment of PHPT. This lowers PTH and serum calcium levels significantly but does not increase BMD values.15 In the present survey, bisphosphonates were the most widely used treatments for PHPT and when used in combination were generally combined with HRT, diuretics or cinacalcet. Although diuretics were quite commonly used in this survey, presumably in an attempt to lower serum calcium values in PHPT because of their calciuric effect, we are not aware of any evidence from randomized trials to suggest that they are actually effective in this condition.
There are limitations associated with the use of survey data. Perhaps most significantly, there is the inherent potential for bias in responding, such as giving an affirmative answer to a question because it is the perceived ‘correct answer’. The format of the questionnaire, designed to maximize response rate, led to a relatively closed selection choice possibly influencing responses.
In summary, the present survey has shown that substantial variation exists in clinicians' approach to the management of PHPT in different European countries. This emphasizes the need for further research to fully explore the long-term efficacy of different management strategies.
Supplementary Data
Supplementary Data are available at QJMED Online.
Funding
This study was funded by Amgen (Europe) GmbH.
Conflict of interest: B. L. L. has spoken at a speakers' bureau supported by Amgen and has consulted for Amgen, Eli Lilly, MSD, Novartis, Nycomed and Servier. She has also received research grants from Amgen, Eli Lilly, MSD, Novartis, Nycomed and Pfizer. S. H. R. has received research grants from Eli Lilly and has consulted for MSD, Novartis and Amgen.
Supplementary Material
Acknowledgements
Editorial assistance was provided by ApotheCom ScopeMedical Ltd funded by Amgen (Europe) GmbH and by Dr Caterina Hatzifoti of Amgen (Europe) GmbH.
References
- 1.Fraser WD. Hyperparathyroidism. Lancet. 2009;374:145–58. doi: 10.1016/S0140-6736(09)60507-9. [DOI] [PubMed] [Google Scholar]
- 2.Vestergaard P, Mollerup CL, Frokjaer VG, Christiansen P, Blichert-Toft M, Mosekilde L. Cardiovascular events before and after surgery for primary hyperparathyroidism. World J Surg. 2003;27:216–22. doi: 10.1007/s00268-002-6541-z. [DOI] [PubMed] [Google Scholar]
- 3.Bilezikian JP, Potts JT, Jr, Fuleihan G, Kleerekoper M, Neer R, Peacock M, et al. Summary statement from a workshop on asymptomatic primary hyperparathyroidism: a perspective for the 21st century. J Bone Miner Res. 2002;17(Suppl. 2):N2–11. [PubMed] [Google Scholar]
- 4.Bilezikian JP, Khan AA, Potts JT., Jr Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J Clin Endocrinol Metab. 2009;94:335–9. doi: 10.1210/jc.2008-1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eastell R, Arnold A, Brandi ML, Brown EM, D'Amour P, Hanley DA, et al. Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the third international workshop. J Clin Endocrinol Metab. 2009;94:340–50. doi: 10.1210/jc.2008-1758. [DOI] [PubMed] [Google Scholar]
- 6.Khan AA, Bilezikian JP, Potts JT., Jr The diagnosis and management of asymptomatic primary hyperparathyroidism revisited. J Clin Endocrinol Metab. 2009;94:333–4. doi: 10.1210/jc.2008-1757. [DOI] [PubMed] [Google Scholar]
- 7.Udelsman R, Pasieka JL, Sturgeon C, Young JE, Clark OH. Surgery for asymptomatic primary hyperparathyroidism: proceedings of the third international workshop. J Clin Endocrinol Metab. 2009;94:366–72. doi: 10.1210/jc.2008-1761. [DOI] [PubMed] [Google Scholar]
- 8.Silverberg SJ, Lewiecki EM, Mosekilde L, Peacock M, Rubin MR. Presentation of asymptomatic primary hyperparathyroidism: proceedings of the third international workshop. J Clin Endocrinol Metab. 2009;94:351–65. doi: 10.1210/jc.2008-1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.AACE/AAES Task Force on Primary Hyperparathyroidism. The American Association of Clinical Endocrinologists and the American Association of Endocrine Surgeons position statement on the diagnosis and management of primary hyperparathyroidism. Endocr Pract. 2005;11:49–54. doi: 10.4158/EP.11.1.49. [DOI] [PubMed] [Google Scholar]
- 10.Perrier ND. Asymptomatic hyperparathyroidism: a medical misnomer? Surgery. 2005;137:127–31. doi: 10.1016/j.surg.2004.06.037. [DOI] [PubMed] [Google Scholar]
- 11.Perrier ND, Balachandran D, Wefel JS, Jimenez C, Busaidy N, Morris GS, et al. Prospective, randomized, controlled trial of parathyroidectomy versus observation in patients with ‘asymptomatic’ primary hyperparathyroidism. Surgery. 2009;146:1116–22. doi: 10.1016/j.surg.2009.09.034. [DOI] [PubMed] [Google Scholar]
- 12.Palmer M, Adami HO, Bergstrom R, Jakobsson S, Akerstrom G, Ljunghall S. Survival and renal function in untreated hypercalcaemia. Population-based cohort study with 14 years of follow-up. Lancet. 1987;1:59–62. doi: 10.1016/s0140-6736(87)91906-4. [DOI] [PubMed] [Google Scholar]
- 13.Wermers RA, Khosla S, Atkinson EJ, Grant CS, Hodgson SF, O'Fallon WM, et al. Survival after the diagnosis of hyperparathyroidism: a population-based study. Am J Med. 1998;104:115–22. doi: 10.1016/s0002-9343(97)00270-2. [DOI] [PubMed] [Google Scholar]
- 14.Stevenson JC, Lynn JA. Time to end a conservative treatment for mild hyperparathyroidism. Br Med J (Clin Res Ed) 1988;296:1016–7. doi: 10.1136/bmj.296.6628.1016-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peacock M, Bolognese MA, Borofsky M, Scumpia S, Sterling LR, Cheng S, et al. Cinacalcet treatment of primary hyperparathyroidism: biochemical and bone densitometric outcomes in a five-year study. J Clin Endocrinol Metab. 2009;94:4860–7. doi: 10.1210/jc.2009-1472. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.