Abstract
In 2001, we described an autosomal dominant myopathy characterized by neuromuscular ventilatory failure in ambulant patients. Here we describe the underlying genetic basis for the disorder, and we define the neuromuscular, respiratory and radiological phenotype in a study of 31 mutation carriers followed for up to 31 years. A combination of genome-wide linkage and whole exome sequencing revealed the likely causal genetic variant in the titin (TTN) gene (g.274375T>C; p.Cys30071Arg) within a shared haplotype of 2.93 Mbp on chromosome 2. This segregated with the phenotype in 21 individuals from the original family, nine subjects in a second family with the same highly selective pattern of muscle involvement on magnetic resonance imaging and a third familial case with a similar phenotype. Comparing the mutation carriers revealed novel features not apparent in our original report. The clinical presentation included predominant distal, proximal or respiratory muscle weakness. The age of onset was highly variable, from early adulthood, and including a mild phenotype in advanced age. Muscle weakness was earlier onset and more severe in the lower extremities in nearly all patients. Seven patients also had axial muscle weakness. Respiratory function studies demonstrated a gradual deterioration over time, reflecting the progressive nature of this condition. Cardiomyopathy was not present in any of our patients despite up to 31 years of follow-up. Magnetic resonance muscle imaging was performed in 21 affected patients and revealed characteristic abnormalities with semitendinosus involvement in 20 of 21 patients studied, including 3 patients who were presymptomatic. Diagnostic muscle histopathology most frequently revealed eosinophilic inclusions (inclusion bodies) and rimmed vacuoles, but was non-specific in a minority of patients. These findings have important clinical implications. This disease should be considered in patients with adult-onset proximal or distal myopathy and early respiratory failure, even in the presence of non-specific muscle pathology. Muscle magnetic resonance imaging findings are characteristic and should be considered as an initial investigation, and if positive should prompt screening for mutations in TTN. With 363 exons, screening TTN presented a major challenge until recently. However, whole exome sequencing provides a reliable cost-effective approach, providing the gene of interest is adequately captured.
Keywords: hereditary myopathy with early respiratory failure, cytoplasmic body, titin, exome sequencing, distal myopathy
Introduction
Respiratory muscle weakness is a common late feature of many neuromuscular disorders, but usually develops after the onset of significant limb or axial weakness. Defects of neuromuscular transmission and motor neuron disease (amyotrophic lateral sclerosis) occasionally require immediate ventilation on presentation (Qureshi et al., 2004; Gautier et al., 2010), as can α-glucosidase deficiency (acid maltase deficiency, type II glycogenosis) (Mellies and Lofaso, 2009) and rare presentations of other inherited, metabolic, inflammatory or toxic myopathies (Hutchinson and Whyte, 2008). However, in general, respiratory failure is unusual in ambulant patients. In contrast, several European families have been described where affected individuals developed significant ventilatory weakness early in the disease course (Patel et al., 1983; Chapon et al., 1989; Edstrom et al., 1990; Abe et al., 1993; Chinnery et al., 2001; Birchall et al., 2005). Sporadic cases with similar clinical and pathological features have also been described (Kinoshita et al., 1975; Jerusalem et al., 1979; Winter et al., 1986; Bertini et al., 1990; Baeta et al., 1996; Evangelista et al., 2009; Tasca et al., 2010). Differences in the neuromuscular phenotype led to several different names for the clinical syndromes, including hereditary myopathy with early respiratory failure (OMIM #603689), hereditary cytoplasmic body myopathy with early respiratory failure (Jerusalem et al., 1979; Patel et al., 1983; Chapon et al., 1989; Abe et al., 1993), hereditary inclusion body myopathy with early respiratory failure (Chinnery et al., 2001) and myopathy with respiratory failure and myofibrillar aggregates (Kinoshita et al., 1975; Edstrom et al., 1990). All reported cases shared in common the presence of early respiratory muscle involvement, and predominantly proximal and/or distal muscle weakness with pathological features including eosinophilic inclusions on muscle histopathology and Z-disc abnormalities with cytoplasmic bodies on electron microscopy. A mutation in the kinase domain of titin was identified as the cause in three Swedish families (Lange et al., 2005), but the genetic cause of the disease in all the other patients remained elusive.
In 2001, we described a family with an autosomal dominant myopathy associated with early respiratory failure (Chinnery et al., 2001). The disorder presented in mid-adult life in 11 individuals with predominantly distal weakness and preferential diaphragmatic involvement in some patients. Hip and shoulder girdle weakness developed later in the disease course. The absence of axial weakness distinguished the family from other clinical descriptions, and the disease did not link to genetic loci known to be relevant at the time. Subsequent studies defined the lower-limb muscle magnetic resonance imaging (MRI) phenotype, with prominent semitendinosis and obturator externus involvement, which was detectable in clinically unaffected individuals at risk of inheriting the disorder (Birchall et al., 2005). Here, we report the genetic basis of this disease and confirm our clinical suspicion that two other families have the same disorder. This allowed us to define the clinical spectrum of the disease in 31 patients.
Materials and methods
Clinical assessments
Ethical approval was granted by the Newcastle University and Hospitals Local Research Ethics Committee. All assessments and clinical investigations were carried out in the Newcastle upon Tyne Hospitals NHS Foundation Trust. Clinical data were available for 31 affected individuals. A structured history and examination was performed on 22 subjects (P.F.C., R.H. and G.P.), along with routine haematological, biochemical, immunological and endocrine blood tests, including serum creatine kinase. Clinical neurophysiology (electromyography and nerve conduction studies, n = 13), muscle MRI (n = 21) and skeletal muscle biopsy (n = 15) were performed on a subgroup of affected individuals.
Muscle biopsy analysis
Diagnostic skeletal muscle biopsies were snap frozen on site for histopathological and histochemical examination on cryostat sections (15 biopsies) and western blot analysis (7 biopsies). Diagnostic immunocytochemistry was performed using the following commercially available antibodies. Dystrophin: Dy10/12B2 (N-terminus), Dy4/6 D3 (rod), Dy8/6C5 (C-terminus). Associated glycoproteins: Ad1/20A6 (α-sarcoglycan), βSarc1/5B1 (β-sarcoglycan), 35DAG/21B5 (γ-sarcoglycan), δSarc3/12C1 (δ-sarcoglycan), 43DAG/8D5 (β-dystroglycan). β-Spectrin: RBC2/3D5 (to monitor membrane integrity on sections). Laminins: commercial anti-laminin α5 (Chemicon MAB 1924), β1 (Chemicon MAB 1921) and γ1 chain (Chemicon MAB 1920), Mer3/22B2 (equivalent to 300 kDa α2 chain fragment) on sections; commercial α2 (Chemicon MAB 1922) (80 kDa fragment) on blots. Caveolin 3, Emerin and lamin A/C: commercial antibodies (Transduction Labs C38320 and Novocastra NCL-LAM-A/C, respectively). Calpain 3: Calp3d/2C4 (exon1), Calp3c/12A2 (exon 8) on blots only. Dysferlin: NCL-hamlet (exon 53) on blots and sections, Ham3/17B2 (at exon 11-12 junction) on sections. Telethonin (G-11), neonatal myosin heavy chain (NCL-MHCn), on sections only. Titin antibody m10-1 (Hackman et al., 2008) was used on western blots.
Pathological analysis of muscles from post-mortem examination
Immunohistochemistry
Post-mortem samples (quadriceps, gastrocnemius, diaphragm, cardiac) obtained from Patient A-IV:17 were analysed. Control skeletal muscle was obtained during orthopaedic surgical intervention in individuals not suffering from neuromuscular diseases. A standard immunohistochemistry protocol was used on 6 -µm frozen sections with antibodies against desmin (Dako D33, 1:400), myotilin (Novocastra NCL-Myotilin, 1:50) and P62 (Abcam ab56416, 1:150). Labelling for calpain 3 (Novocastra NCL-CALP-2C4, 1:50) and valosin-containing protein (BD Biosciences, 1:2000) was carried out with a sensitive detection protocol (X-Cell-Plus HRP Detection, Menapath) as previously described (Charlton et al., 2009).
Sodium dodecyl sulphate polyacrylamide gel electrophoresis and western blotting
Sections (30 × 10 µm) were cut for each sample and quickly dissolved in loading buffer (0.05 M dithiothreitol, 0.1 M EDTA, 0.125 M Tris, 4% sodium dodecyl sulphate, 10% glycerol, 0.005% bromophenol blue, pH 8), boiled for 3 min and centrifuged. Gel electrophoresis and transfer were carried out as described (Anderson et al., 1999). After transfer, nitrocellulose membrane sheets were labelled with monoclonal anti-calpain antibodies (Novocastra NCL-CALP-2C4 and NCL-CALP-2A12, both 1:60) that detect the full size calpain 3 at 94 kDa and degradation fragments of the protein at 60 or 30 kDa or rabbit polyclonal m10-1 at 1:500, raised against the most C-terminal titin doman M10 (Hackman et al., 2008). Antibody detection was performed using an enhanced chemiluminescence detection system (Thermo Scientific SuperSignal® West Pico Chemiluminescent Substrate). Proteins on gel were stained with Coomassie Brilliant Blue after transfer. Dried blots and gels were used for densitometric analysis with AlphaView™ Q Software (Alpha Innotech).
Genome-wide linkage analysis
A total of 28 individuals (of which 21 were affected) were genotyped at 1170 microsatellite markers derived from the Applied Biosciences HD Marker linkage set and deCODE designed markers derived from the Marshfield genetic map. The average marker distance was 4 cM, with 95% of the gaps <6 cM and none >10 cM. Proprietary deCODE Allele Caller software was used for automated allele calling. CEPH family DNA samples were used as quality controls. Markers (93.7%) were successfully genotyped.
Two-point and multipoint linkage analysis was performed using ALLEGRO v1.2c (incorporated into the EasyLINKAGE Plus package) (Gudbjartsson et al., 2000; Lindner and Hoffmann, 2005). An autosomal dominant mode of inheritance and a parametric model-based assumption with complete penetrance and a disease allele frequency of 0.1% were used for analysis.
Fine mapping
A further nine markers were used to fine-map the linked locus: two markers were proximal to D2S335 (D2S2380 and D2S399) and seven were distal to this marker (D2S2257, D2S148, D2S2173, D2S324, D2S1574E, D2S385 and D2S2310). One oligonucleotide from each pair was fluorescently labelled (sequences available on request). In addition to 50 ng DNA, 1 × GoTaq® buffer (Promega), 0.33 µM of each oligonucleotide, 2.5 mM dNTPs (Roche) and 0.5 U Taq polymerase (Promega) were added, to a final volume of 15 µl. Amplification was initiated by denaturation at 95°C for 2 min, followed by 30 cycles of denaturation at 95°C for 1 min, annealing at 57–61°C for 1 min and extension at 72°C for 1 min. Finally, there was a further extension at 72°C for 3 min before the samples were cooled to 4°C. Amplicons (3 µl) were utilized for downstream analysis of microsatellite sizes by using a CEQ8000™ Genetic analysis system (Beckman Coulter) according to manufacturer’s instructions. Analysis was conducted using Beckman Coulter Fragment Analysis v2.2.1 software.
Array comparative genomic hybridization
Array comparative genomic hybridization was performed on an affected individual (Patient A-IV:12) by using a whole genome 4 × 44k oligo array (ISCA version 2.0), analysed with Bluefuse Multi v2.4 software, with expected resolution of ∼0.25 Mb.
Whole exome sequencing and bioinformatics
Whole exome sequencing was initially performed on two subjects (Patients A-III:6 and A-IV:12) by using the Agilent SureSelect Human All Exon (38 Mb) capture system, and subsequently on another affected individual (Patient A-IV:10) by using the Illumina TruSeq™ Exome Enrichment (62 Mb) capture system. Genomic DNA was fragmented, hybridized and exonic sequences were enriched according to manufacturer’s protocol. The captured DNA fragments were purified and sequenced on an Illumina Genome Analyser IIx using 75 bp reads (single and paired-end, respectively) for Patients A-III:6 and A-IV:12, and an Illumina Hiseq2000 platform using 100 bp paired-end reads for Patient A-IV:10. Sequence reads were aligned to the human reference genome (UCSC hg19) using BWA (Li and Durbin, 2010) and the aligned sequence files were reformatted using SAMtools (Li et al., 2009). Single base variants were identified using Varscan v2.2 (Koboldt et al., 2009) and indels were identified using Dindel v1.01 (Albers et al., 2011). The raw lists of variants were filtered using in-house Perl scripts to identify variants within target regions that were not present in dbSNP132 or in the exome sequences of 50 unrelated and unaffected individuals. Putative ‘disease causing’ mutations were identified using MutationTaster (Schwarz et al., 2010) with the intention to screen any mutations causing amino acid substitutions and/or were predicted as deleterious.
Segregation analysis
Detection of the candidate mutations was performed by direct sequencing. The details of the specific primer sequences are available in the Supplementary material. Polymerase chain reaction was performed with Immolase (Bioline) according to manufacturer’s protocol, using ∼50 ng of DNA, 0.25 mM of each oligonucleotide and 0.75–4 mM MgCl2, for 30 cycles with annealing temperature of 57–65°C. Sequencing was performed using BigDye® (Applied Biosystems) according to the manufacturer’s protocol with an ABI 3130XL sequencer. Additional single nucleotide variants flanking the disease mutation identified by exome sequencing were Sanger sequenced to further define the disease haplotype for between-family comparisons.
Analysis of titin protein expression
Western blot analysis was carried out using the rabbit polyclonal antibody m10-1 (Hackman et al., 2008) to the C-terminus of titin on Patient A-III:6, compared to normal control muscle and muscle from patients with tibial muscular dystrophy and LGMD2J. The titin C-terminus is fragmented, and we use the pattern and intensity of the fragments to assess the integrity of titin C-terminus.
Results
Patients
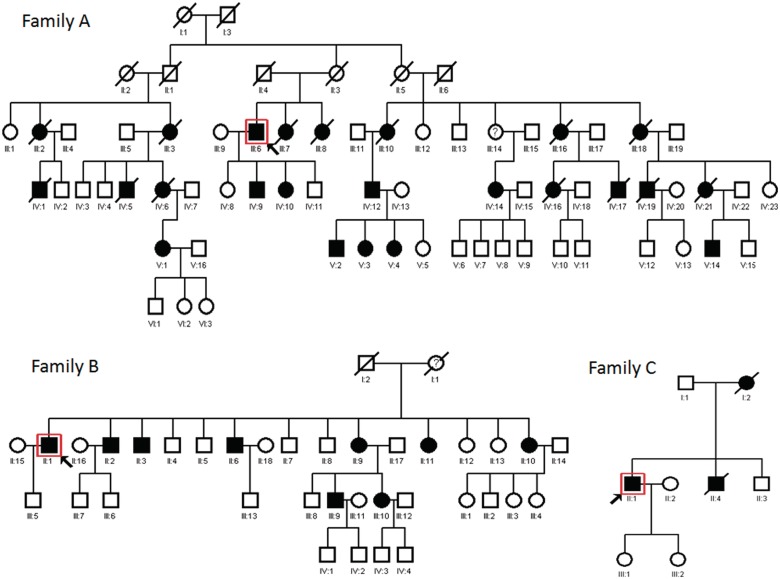
Pedigrees for the three families are represented in Fig. 1. There were no genealogical links between the three families, although all are based in the North East of England. The clinical features of all affected individuals are summarized in Table 1, and serial pulmonary function testing results are presented in Fig. 2. A key identifying previously published patients is included in Appendix A.
Figure 1.
Pedigrees of the three families with hereditary myopathy with early respiratory failure. Part of Families A and B have been published previously (Appendix A). Surrounding box and arrow indicate the proband in each pedigree. Open symbols represent unaffected family members, filled symbols are affected by hereditary myopathy with early respiratory failure.
Table 1.
Clinical features at the time of initial clinical assessment in three families (22 affected individuals)a
| Patient ID | Onset age | Onset symptom | Proximal versus distal predominant | Weakness pattern at presentation |
Pulmonary function percentage predicted |
CK (u/l)b | NCS/EMG | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Distal | Proximal | Axial | Respiratory | FEV1 | VC | ||||||
| Family A | |||||||||||
| A-III:3 | 71 | Proximal and distal wk | Proximal = distal | ADF/APF 4 | D 4+, HF 4 | Normal | 88 | ||||
| A-III:6 | 47 | Drop foot | Distal | ADF (R) 4-, (L) 1, AI 4- | HF (R) 4-, (L) 3, KF 4 | Normal | 72 | 68 | 218 | ||
| A-III:7 | 55 | Dyspnoea | Proximal | Normal | D 4+, HF 4+ | NF 4+ | Symptomatic on exertion | 56 | 62 | 185 | |
| A-III:8 | 61 | Dyspnoea | N/A | Normal | Normal | Normal | Dyspnoea, orthopnoea | 73 | 77.5 | 112 | Normal |
| A-III:16 | 54 | Falls | Proximal = distal | FF/FE 3, WF/WE 4, ADF 4, APF 4+ | D 3, EF/EE 4, HF 2, HE 3, KF/KE 4- | NF 4, NE 4+ | |||||
| A-IV:4 | 45 | Dyspnoea | N/A | Normal | Normal | Normal | Dyspnoea | 77 | Myopathic (proximal) | ||
| A-IV:6 | 48 | Proximal wk | Proximal | ADF 4 | D 4+, HF 3, KE 4 | NF 4+ | Symptomatic on exertion | 107 (83 sup) | 100 (80 sup) | 94 | |
| A-IV:10 | 38 | Proximal wk | Proximal | Normal | D 4+, HF/HE 4+ | Normal | 327 | ||||
| A-IV:12 | 44 | Drop foot and dyspnoea | Distal | ADF 3 | HF 4 | Normal | 40 | 43 | 237 | Myopathic | |
| A-V:14 | 36 | Drop foot | Distal | FF/FE 4, WF/WE 4, ADF 3, AE 4 | HF 4 | Normal | 56 | 67 | 549 | Necrotizing myopathy | |
| A-IV:16 | 33 | Drop foot | Proximal | WE/WF 4+ | D 4-, EF/EE 4, HF 3, HE 4-, ADF 4 | NF 4+ | Symptomatic on exertion | 63 | 61 (53 sup) | 303 | Necrotizing myopathy |
| A-IV:20 | 42 | Unknown | Proximal | WF 4+, ADF 4 | D 4, EF/EE 4, HF 2, HE/HA 3, KF 4, KE 4- | NF 4, NE 4+ | 35 | 38 | |||
| A-V:1 | 22 | Proximal wk and orthopnoea | Proximal | All 4 | D 4 -, EF/EE 4, HF 4-, HE 4 | Normal | 48 | Normal | |||
| Family B | |||||||||||
| B-II:1 | 30 | Drop foot | Distal | WF 4+, ADF 3, AI 4-, AE 4, APF 5 | Normal | 102 | 92 | 966 | Necrotizing myopathy (distal predominant) | ||
| B-II:2 | 44 | Drop foot | Distal | ADF 4 | D 4+, EE 4+, HF 4+ | Normal | 67 | 63 | 242 | Necrotizing myopathy (distal predominant) | |
| B-II:3 | 40 | Drop foot | Distal | ADF/AI/AE 4- | FE/WE 4 | NF 4 | 566 | Myopathic | |||
| B-II-6 | 42 | Drop foot | Distal | ADF 4 | Normal | 620 | Necrotizing myopathy | ||||
| B-II:9 | 41 | Proximal wk | Proximal | ADF 4, APF 4 | D 4, HF 3, HE 4, KE/KF 4 | Normal | 70 | 76 | 312 | Necrotizing myopathy | |
| B-II:10 | 45 | Drop foot | Distal | FE 4+, ADF/AE/AI 3, APF 4+ | HF 4+, KE 4+ | NF 4 | |||||
| B-II:11 | 55 | Proximal wk and orthopnoea | Proximal = distal | ADF 4 | HF 4+ | Normal | 66 | 68 | |||
| B-III:9 | 43 | Exertional dyspnoea | Distal | ADF 4+ | Normal | Normal | Symptomatic on exertion | 59 | 66 | 398 | Necrotizing myopathy |
| Family C | |||||||||||
| C-II:1 | 45 | Drop foot | Distal | WE/WF 4-, FE/FF 4-, ADF 2, APF 4- | EE 4+, HF 3, KE/KF 4 | Normal | 47 | 46 | 167 | Myopathic | |
a All muscles not reported are MRC strength 5/5 (normal).
b The reference range for creatine kinase is 10–190 u/l at our centre.
ADF = ankle dorsiflexion; AE = ankle eversion; AI = ankle inversion; APF = ankle plantarflexion; CK = creatine kinase; D = deltoid; EE = elbow extension; EF = elbow flexion; FE = finger extension; FF = finger flexion; KE = knee extension; KF = knee flexion; HA = hip adduction; HE = hip extension; HF = hip flexion; NCS = nerve conduction studies; NE = neck extension; NF = neck flexion; sup = supine; WE = wrist extension; WF = wrist flexion; wk = weakness; FEV1 = forced expiratory volume in 1 second; VC = vital capacity; EMG = electromyography; R = right; L = left.
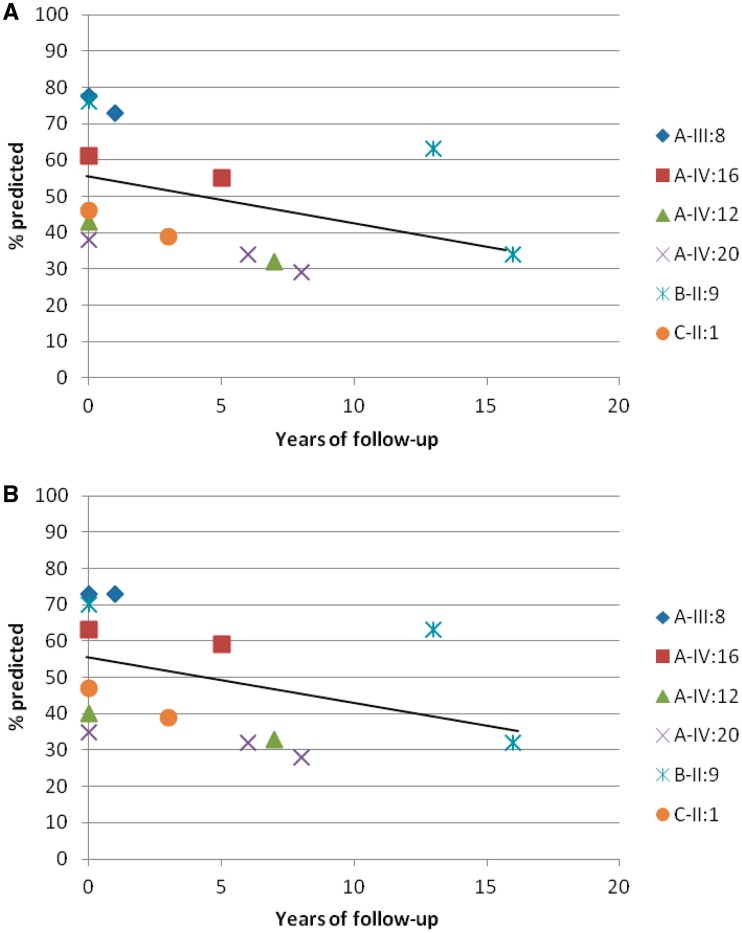
Figure 2.
Pulmonary function testing results showing a gradual decline over time for (A) forced vital capacity and (B) forced expiratory volume. Results expressed as the percentage of expected values for height, gender and weight. Unique identifiers are shown for individual patients. A solid line indicates the line of best fit.
Family A
Originally described with 11 affected and 13 unaffected individuals (Chinnery et al., 2001), the family now has 21 affected and 20 unaffected individuals. The phenotype was variable within the members of this family. Age of onset varied from 33 to 71 years. The most common presenting symptom was foot drop in 5/12 patients, exertional dyspnoea and/or orthopnoea in 4/12 patients and proximal weakness in 3/12 patients. Despite the common initial presentation of distal weakness, on clinical examination we judged the myopathy to be predominantly proximal in 5/12 patients, predominantly distal in 3/12 patients and both in the remainder. Weakness was generally more severe in the lower extremities, particularly for hip flexion and ankle dorsiflexion. Weakness was symmetrical in all patients except one (Patient A-III:6), although as his condition progressed his weakness became symmetric (particularly of ankle dorsiflexion 0/5 and hip flexion 2/5). Neck flexor weakness was present in 5/12 patients. Evidence of respiratory muscle weakness was indicated by decreased forced vital capacity and forced expiratory volume in 8/12 of the patients, and when recorded pulmonary function decreased in the supine position. Five of 12 patients eventually required nocturnal non-invasive ventilatory support for respiratory muscle weakness, and in these patients this occurred between 5 and 8 years after the time of initial assessment in our clinic. One of these patients has been receiving nocturnal ventilation for 18 years and continues to live at home. Walking aids were eventually required by most of the patients in this family, most commonly ankle-foot orthoses for foot drop, which became necessary between 1 and 4 years after initial presentation. Two of 12 patients became wheelchair-bound after an interval of 7–8 years. Mild to moderate elevations of creatine kinase were present in 7/12 patients. Neurophysiology revealed myopathy with spontaneous activity in 2/5 patients, myopathic changes in 2/5 patients and was normal in one mildly affected individual.
Family B
Based in a different region of the North East of England, Family B was identified on clinical grounds and shared distinctive MRI features with Family A (Birchall et al., 2005). Since then we have identified nine affected family members, and at present 19 family members are unaffected. Detailed clinical records were available for all nine affected family members. Age of onset varied from 22 to 55 years, and again we observed heterogeneous phenotype. Five patients presented with drop foot, three patients with symptoms of proximal weakness and three with respiratory symptoms. On clinical examination we judged that six of the patients had predominantly distal muscle involvement, particularly of ankle dorsiflexion; two of these patients had atrophy in the anterior compartment of the distal lower extremity (Patients B-II:1 and B-II:3). Mild to moderate elevations of creatine kinase were present in six patients. Neurophysiology demonstrated myopathy with spontaneous activity in 5/7 patients and was normal in one patient.
Family C
Living in the same region as Family B, the index case presented with drop foot at the age of 45 years. His mother had been wheelchair-bound since he was a child and had a diagnosis of muscular dystrophy on her death certificate. His brother had difficulty with strength in his arms and legs but died at age 47 years from unrelated causes (liver cirrhosis). On initial assessment, the proband had pronounced weakness of ankle dorsiflexion and less so of hip flexion. Calf hypertrophy was present. He also had milder grade weakness of the proximal and distal upper extremities. He was referred for ankle-foot orthoses upon our initial assessment, and became wheelchair-bound 10 years after his initial presentation. He required nocturnal continuous positive airway pressure ventilation 11 years following initial assessment. Despite having a forced vital capacity <40% for the last seven years, with nocturnal ventilation the patient has continued to live at home with assistance.
Muscle histology and protein analysis
Diagnostic muscle biopsy results from 15 subjects
We present a summary of the pathological findings from 15 affected members from all three families, which includes seven previously reported subjects (Table 2). The most common findings were eosinophilic inclusions (‘inclusion bodies’) and blue-rimmed vacuoles. Inclusions were found in a small minority of muscle fibres (typically <5%), even in severely affected individuals. However, affected fibres typically contained multiple inclusions. Inclusions had absent staining on NADH, succinyl dehydrogenase, periodic acid-Schiff and myophosphorylase assays, but intense staining with Gomori trichrome. Other non-specific myopathic features were variably present, including fibre size variability (up to 20-fold). Immunocytochemistry excluded known dystrophinopathies, limb-girdle muscular dystrophies (LGMD) and myofibrillar myopathies as a diagnosis. Staining of calpain 3 (CAPN3) was normal or mildly decreased in muscle biopsies taken from quadriceps, gastrocnemius or deltoid muscle. The reduction was more marked in muscle biopsies from tibialis anterior. Three patients had mild, non-specific abnormalities on muscle biopsy that (in the absence of the family history and later genetic testing) would not have permitted a diagnosis of hereditary myopathy with early respiratory failure. Electron microscopy was only performed on biopsies from Family A and has been reported previously (Chinnery et al., 2001).
Table 2.
Summary of muscle histopathology findings in 15 patients
| Patient ID | Eosinophilic inclusions | Rimmed vacuoles | Fibre splitting/ fragmentation | Atrophy | Internal nuclei | Type I fibre predominance | Fibre size variation | Other |
|---|---|---|---|---|---|---|---|---|
| A-III:6 | + (minimal) | + (minimal) | + | + | ||||
| A-III:16 | ++ | + | ++ | + | ++ | ++ | ||
| A-IV:1 | ++ | +++ | + | |||||
| A-IV:4 | ++ | + | + | + | + | + | ||
| A-IV:6 | + | ++ | +++ | +++ | ||||
| A-IV:16 | + | + | ++ | +++ | + | ++ | 50% replacement by fat and fibrous tissue | |
| A-IV:17 | +++ | + | +++ | ++ | ++ | ++ | ||
| A-IV:19 | + | + | + | ++ | + | ++ | ||
| A-IV:20 | +++ | + | ++ | + | ++ | ++ | Internal nuclei fragmentation atrophy | |
| B-II:1 | + | +++ | ++ | ++ | +++ | Massive variation of fibre size up to 20-fold | ||
| B-II:2 | + | ++ | +++ | +++ | + | |||
| B-II-6 | ++ | + | ++ | |||||
| B-II:9 | + | ++ | ++ | ++ | ++ | Muscle fibre hypertrophy | ||
| B-III:9 | + | Myopathic features | ||||||
| C-II:1 | +++ | End-stage muscle, mostly type 2 fibres |
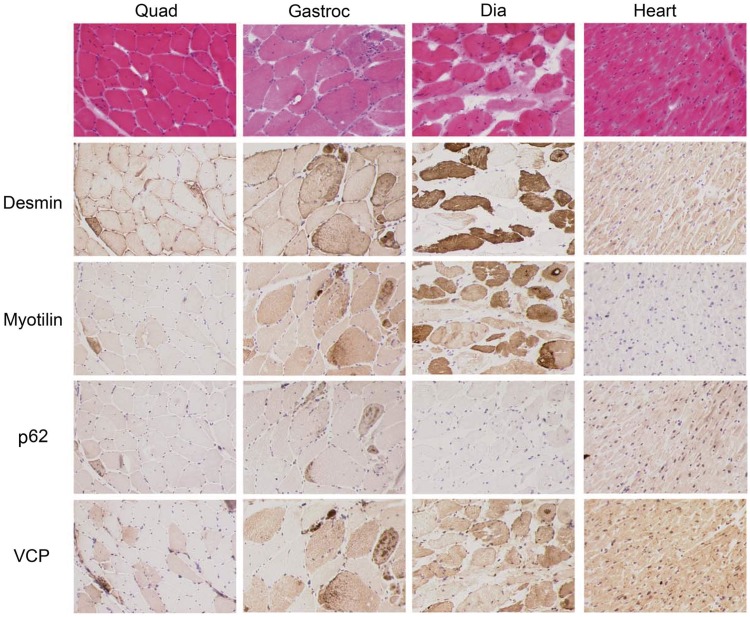
Analysis of diaphragm, gastrocnemius, quadriceps and cardiac muscle from a post-mortem examination
The different muscle samples showed common pathological features of varying severity. Some degree of fibre size variation, internal nucleation, fibrosis and fat replacement was observed in all muscles analysed, but these features were more marked in the diaphragm and milder in the quadriceps. Necrosis, regeneration and inflammation were not seen. A predominant feature of the gastrocnemius was the presence of fibre fragmentation and eosinophilic inclusions, while the diaphragm was predominantly affected by fibrosis and fat replacement. Normal expression of sarcolemmal proteins such as dystrophin and components of the dystrophin glycoprotein complex had earlier been confirmed on this patient (Chinnery et al., 2001). To investigate the nature of the inclusions and possible myofibrillar changes secondary to the defect in titin, we stained the sections with antibodies against desmin, myotilin, p62 and valosin-containing protein (Fig. 3). In all samples, most inclusions were positive for desmin, myotilin and valosin-containing protein, while only a sub-population of fibres showed reactivity to p62, indicating that ubiquitinated multi-protein aggregates containing p-tau are present in some of the cytoplasmic bodies (Nogalska et al., 2009). Heart histology was normal, and protein inclusions were not observed with any of the antibodies in myocardium (Fig. 3).
Figure 3.
Post-mortem muscle pathology. Haematoxylin and eosin staining of quadriceps (quad), gastrocnemius (gastroc), diaphragm (dia) and cardiac muscle (heart) from Patient IV-12. Consecutive sections of muscles labelled with antibodies for desmin, myotilin, p62 and valosin-containing protein (VCP). The inclusions are positive for desmin, myotilin and valosin-containing protein, and some inclusions bound p62.
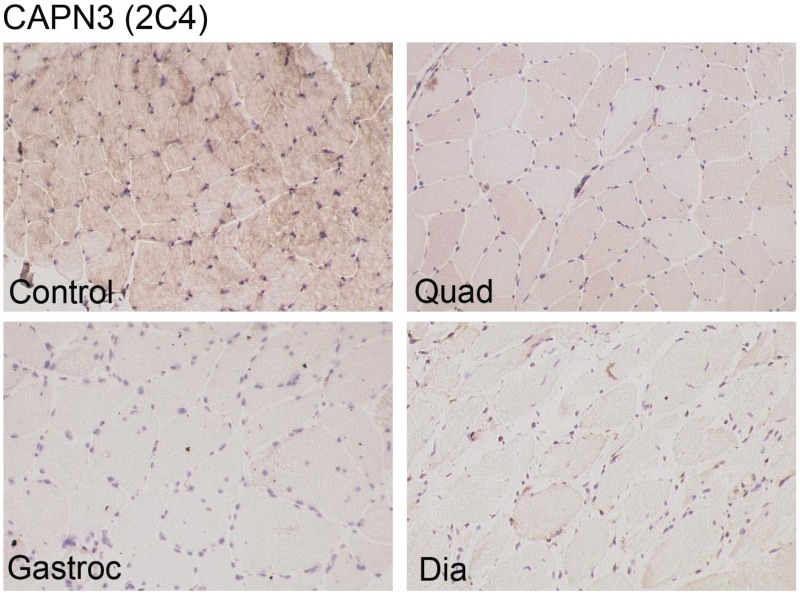
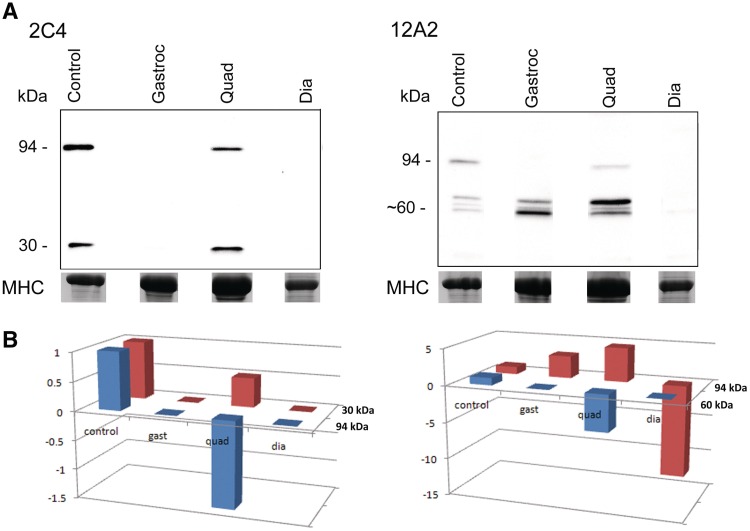
Calpain 3 is a known binding partner of titin (Sorimachi et al., 1995), and muscle biopsies of tibial muscular dystrophy and LGMD type 2J (LGMD2J) patients show variable secondary reduction in calpain 3 (Haravuori et al., 2001). To investigate whether this reduction may correlate with the severity of the involvement of different muscle groups, we performed calpain 3 labelling on sections and immunoblot. In control muscle, the NCL-CALP-2C4 antibody showed diffuse cytoplasmic labelling (Charlton et al., 2009). Fainter labelling was detected in the patient’s quadriceps, gastrocnemius and diaphragm labelled with much reduced intensity (Fig. 4). The same antibody used on western blot showed reduced calpain 3 in the quadriceps and no labelling in gastrocnemius and diaphragm. Labelling with NCL-CALP-2A12 revealed a similar reduction, although calpain 3 degradation bands at ∼60 kDa were still detected in the gastrocnemius (Fig. 5A). Calpain 3 can undergo exhaustive autolysis but it is usually stable (8 h) in human muscle. When freezing or storage artefacts occur, the intensity of the 94 kDa band may be reduced on immunoblot, while an increase in abundance of degradation bands at 60 and 30 kDa is observed. Given that the samples were collected post-mortem, some degree of protein degradation should be taken into account. Indeed, densitometric data normalized to the myosin content in each lane showed that the 60-kDa degradation bands detected in quadriceps and gastrocnemius were stronger in intensity than control (Fig. 5B). Calpain 3 was not detected in the diaphragm with either antibody.
Figure 4.
Calpain 3 immunocytochemistry. Control and patient muscle [quadriceps (quad), gastrocnemius (gastroc) and diaphragm (dia)] labelled with NCL-CALP-2C4 antibody against epitopes encoded by CAPN3 exon 1. Calpain 3 expression is decreased in gastrocnemius compared with quadriceps, and not detected in diaphragm, corresponding to the severity of weakness in these muscles.
Figure 5.
Western blot analysis of calpain 3. (A) Immunoblot of control and patient muscle samples [quadriceps (quad), gastrocnemius (gastroc) and diaphragm (dia)] labelled with NCL-CALP-2C4 and NCL-CALP-2A12 antibodies, directed against epitopes encoded by exons 1 and 8 of CAPN3, respectively. Myosin heavy chain (MHC) from post-blotted gel indicates the amount of protein loaded. (B) Densitometric analysis of calpain 3. y-axis = fold change in intensity.
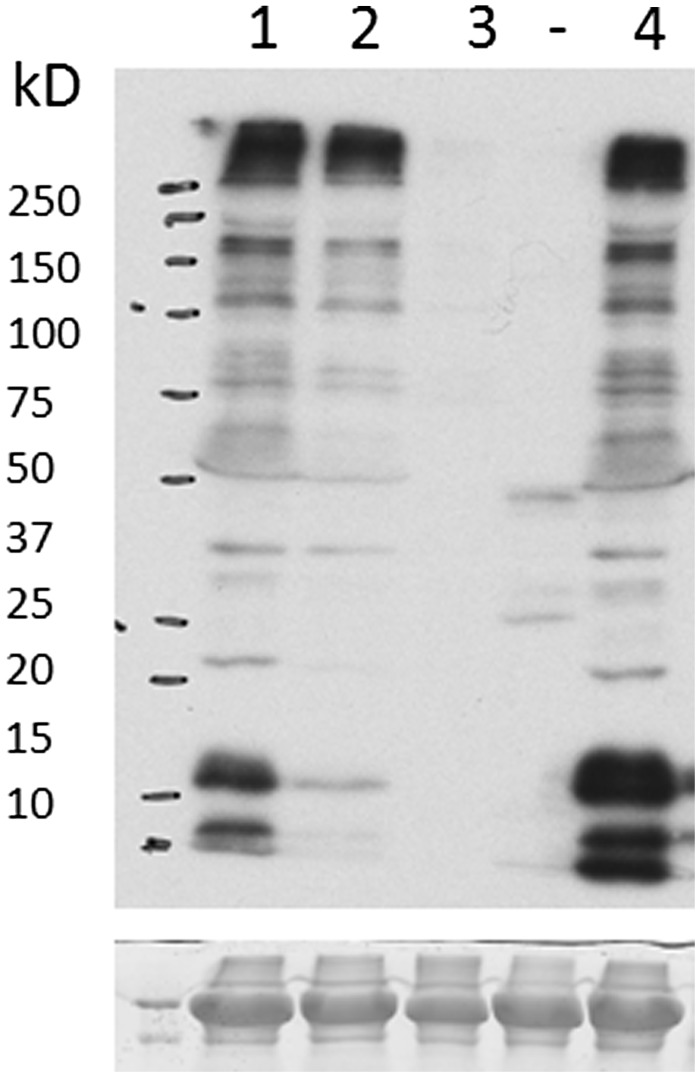
Western blot analysis of titin
Western blot analysis using an antibody directed against the M10 domain of titin showed a normal expression and banding pattern in Patient A-III:6, in contrast to patients with tibial muscular dystrophy and LGMD2J, where the C-terminal fragments were reduced or absent (Fig. 6).
Figure 6.
Western blot of the titin protein (post-blotting gel stained with Coomassie). Lane 1, healthy control muscle; Lane 2, tibial muscular dystrophy muscle; Lane 3, LGMD2J muscle; Lane (-), unrelated sample; Lane 4, quadriceps muscle from Patient A-III:6. The observed banding pattern for our patient from Family A is similar to that seen in control muscle.
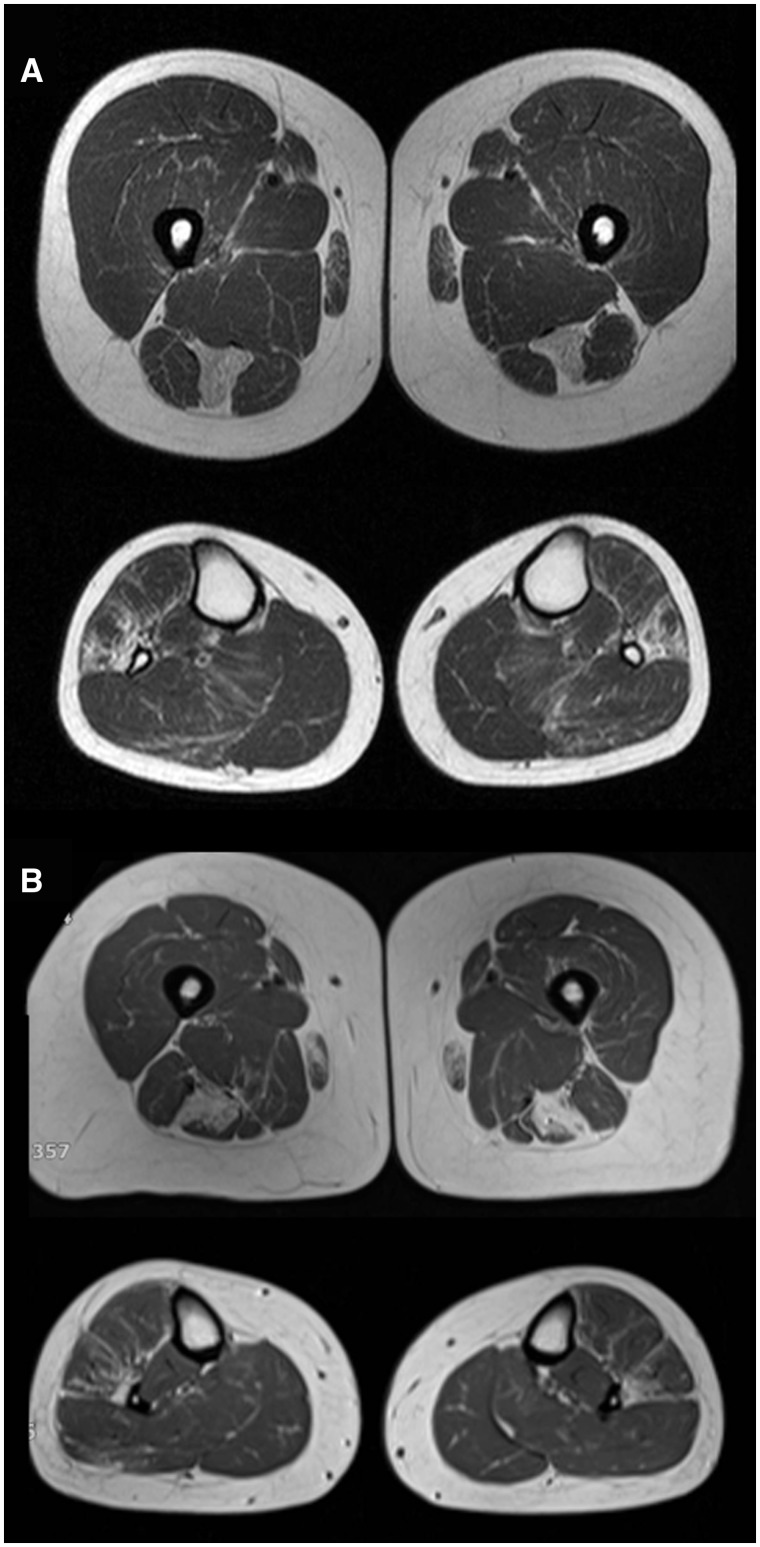
Muscle magnetic resonance imaging findings
Muscle MRI findings are summarized in Table 3, and were consistent with the findings in our previous study (Birchall et al., 2005). Novel findings include three patients who had imaging when presymptomatic, which demonstrated similar (albeit milder) abnormalities to patients who were already clinically affected. Based on these patients, semitendinosus and peroneus longus are the first muscles to show fatty infiltration on MRI (Fig. 7). Two of these patients (Patients A-IV:9 and A-V:3) had imaging seven and six years ago, respectively (both at 30 years of age), and still have not developed the condition. The third patient (Patient B-III:10) already had mildly abnormal pulmonary function tests at the time of initial assessment and developed symptoms of muscle weakness shortly after the time of her scan.
Table 3.
MRI findings in 21 affected patients ordered according to severity of clinical picture at time of imaging
| Patient ID | Clinical status | Distal legs |
Proximal legs |
Axial |
Upper extremities |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PL | GS | TA | TP | EHL | EDL | ST | OE | IP | Sa | Gr | BF | Gl | SM | QF | ABD | ES | SSp | SSc | IS | D | SAn | ||
| A-IV:9 | Presymptomatic | ++ | – | – | – | – | – | ++ | – | – | – | – | – | – | – | – | |||||||
| A-V:3 | Presymptomatic | + | – | – | – | – | – | ++ | + | – | ++ | – | – | – | – | – | |||||||
| B-III:10 | Presymptomatic | ++ | – | – | – | – | – | ++ | – | – | – | – | – | – | – | – | |||||||
| A-V:4 | Respiratory symptoms | + | – | – | – | – | – | ++ | + | – | + | + | – | – | – | – | |||||||
| A-IV:4 | Minor wk | – | – | – | – | – | – | + | – | – | – | – | + | – | – | – | |||||||
| 4 year follow-up | – | – | – | – | – | – | + | – | – | – | – | + | + | + | – | ||||||||
| A-IV:10 | Minor wk | + | + | – | – | – | + | ++ | ++ | – | ++ | ++ | – | – | – | + | |||||||
| A-IV:20 | Minor wk | – | – | – | – | + | – | + | – | – | – | – | – | + | – | – | |||||||
| A-V:1 | Minor wk | – | – | – | – | – | – | – | – | – | + | – | – | – | – | – | |||||||
| A-V:2 | Minor wk | ++ | – | ++ | – | – | – | +++ | ++ | – | – | ++ | – | – | – | – | |||||||
| B-II:2 | Minor wk | + | – | +++ | – | ++ | ++ | +++ | ++ | +++ | – | – | – | + | – | – | – | + | ++ | ++ | ++ | – | + |
| B-II:11 | Minor wk | ++ | – | ++ | – | – | ++ | ++ | – | – | – | – | – | ++ | ++ | ++ | |||||||
| B-III:9 | Minor wk | – | – | ++ | – | – | ++ | ++ | ++ | – | – | – | – | – | – | – | |||||||
| A-V:14 | Moderate wk | +++ | – | +++ | – | – | +++ | +++ | ++ | – | ++ | +++ | ++ | ++ | ++ | ++ | |||||||
| B-II:1 | Moderate wk | +++ | + | +++ | – | +++ | +++ | +++ | ++ | +++ | – | – | – | + | – | ++ | ++ | – | ++ | ++ | ++ | ++ | + |
| B-II-6 | Moderate wk | ++ | ++ | ++ | – | – | ++ | ++ | ++ | – | – | ++ | – | – | – | – | – | ++ | |||||
| A-III:6 | Severe wk | +++ | ++ | +++ | ++ | +++ | +++ | +++ | +++ | +++ | +++ | +++ | – | + | – | +++ | +++ | – | ++ | – | + | – | + |
| A-III:7 | Severe wk | – | – | – | ++ | – | – | +++ | +++ | ++ | – | ++ | – | – | – | + | ++ | ++ | |||||
| A-IV:6 | Severe wk | + | – | + | – | + | – | +++ | ++ | ++ | ++ | ++ | – | – | – | + | – | – | ++ | – | + | ++ | ++ |
| A-IV:12 | Severe wk | ++ | – | ++ | ++ | ++ | – | +++ | ++ | ++ | – | – | – | – | – | – | ++ | – | |||||
| B-II:3 | Severe wk | +++ | ++ | +++ | ++ | – | +++ | +++ | ++ | – | – | – | – | – | ++ | +++ | – | ++ | |||||
| B-II:9 | Severe wk | +++ | ++ | +++ | +++ | + | +++ | +++ | +++ | +++ | + | +++ | + | ++ | ++ | +++ | +++ | +++ | +++ | ++ | +++ | ++ | +++ |
ABD = rectus femoris and/or transversus abdominis; BF = biceps femoris; D = deltoid; EDL = extensor digitorum longus; EHL = extensor hallucis longus; ES = erector spinae; Gl = gluteals; Gr = gracilis; GS = gastrosoleus; IP = iliopsoas; IS = infraspinatus; OE = obturator externus; PL = peroneus longus; Sa = sartorius; SAn = serratus anterior; SM = semimembranosus; SSc = subscapularis; SSp = supraspinatus; ST = semitendinosus; TA = tibialis anterior; TP = tibialis posterior; wk = weakness.
Figure 7.
Muscle MRI in unaffected mutation carriers. (A) Patient A-IV:9 and (B) Patient B-III:10 in Fig. 1 remain clinically unaffected but show characteristic MRI abnormalities with symmetrical fatty replacement of semitendinosus in the proximal lower extremity, and milder involvement of peroneus longus in the distal lower extremity.
We also report results of serial imaging in one patient (Patient A-IV:4) with a mild phenotype. She had two MRI studies in a 4-year interval showing minimal progression, in keeping with her stable clinical course over this period.
The most commonly affected muscle was semitendinosus (20 of 21 subjects), followed by peroneus longus (16/21) and obturator externus (15/21). Some of the patients with mild phenotype had mild abnormalities on imaging, although moderate and severe phenotypes were always associated with pronounced imaging abnormalities. Axial muscles were also involved, including rectus abdominis, transversus abdominis or erector spinae (total of eight patients, in advanced disease), in keeping with our observation that axial muscle weakness is common in this disorder.
Genome-wide linkage analysis
Genome-wide microsatellite analysis performed on Family A identified a 30-cM region on chromosome 2q24.1-2q32.2 with a maximum multipoint log of odds (LOD) score of 3.8 at microsatellite marker D2S335 (Fig. 8). Observed heterozygosity at this marker was 97%. No other chromosomal regions achieved multi-point LOD score of >2.0. This marker also achieved the maximum single point LOD score of 3.4. No other markers produced a single point LOD score of >2.3. Following the addition of nine further microsatellite markers surrounding D2S335, the maximum single point LOD score remained at microsatellite marker D2S335 with a LOD score of 3.8, but the maximum multipoint LOD score shifted to give a maximum LOD at marker D2S2188 located at 180.79 cM on chromosome 2. Linkage analysis and additional manual haplotype analysis within the pedigree indicated the disease locus lay between microsatellite markers D2S2188 and D2S2310, with all affected family members sharing a common haplotype flanked by these two markers. Several unaffected family members also shared the common haplotype between D2S2188 and D2S2173, indicating the disease locus was likely to be situated between markers D2S2173 and D2S2310. This represents a 3.61-cM region including titin (TTN).
Figure 8.
Multi-point linkage analysis of chromosome 2 from Families 1 and 2, using 1000 microsatellite markers, and autosomal dominant model. The linkage region of 2q24-31 includes the TTN gene and the haplotype, which is shared between all three families.
Array comparative genomic hybridization
No abnormalities were detected with array comparative genomic hybridization.
Whole exome sequencing and bioinformatics
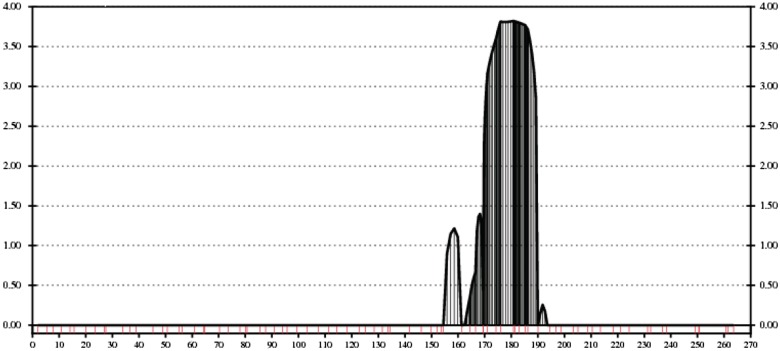
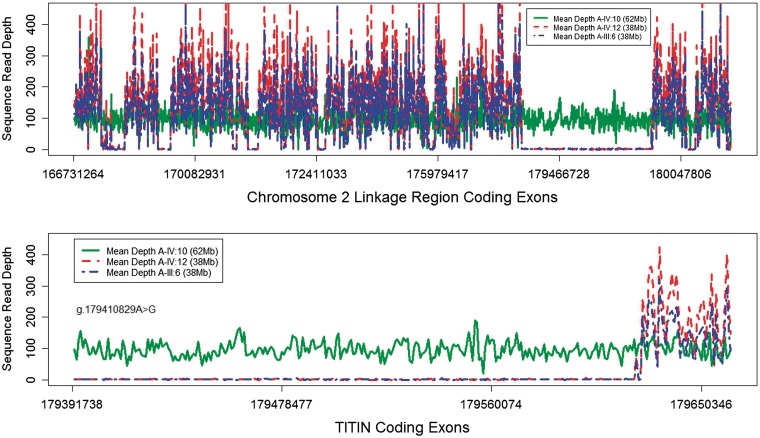
Whole exome sequencing using the Agilent SureSelect Human All Exon (38 Mb) capture system generated more than 152 million 75-bp paired-end reads (11.4 Gb) in Patient A-III:6 and >127 million 75-bp single-end reads (9.6 Gb) in Patient A-IV:12. The exome was captured at a mean per target base sequence depth of 111- and 116-fold for Patients A-III:6 and A-IV:12, respectively, with 88 and 91% of target bases covered at a minimum depth of 10-fold. Within the linkage region on chromosome 2, only 54 and 55% of coding exon bases (CCDS May 2009) were covered at a minimum depth of 10-fold; the coverage of TTN was particularly poor, with only 10% of coding bases covered at a minimum depth of 10-fold in both patients. Due to the poor coverage of TTN, an additional Patient A-IV:10 was sequenced using the Illumina TruSeq® Exome Enrichment (62 Mb) capture system, which generated more than 137 million 101-bp reads (13.9 Gb). Using these targets, there was a mean per target base coverage of 99-fold and 94% of target bases were covered at a minimum depth of 10-fold. Within the linkage region, 98% of coding bases were covered (minimum 10-fold) at a mean depth of 105-fold and 99.8% of the coding region of TTN was covered (minimum 10-fold) with a mean depth of 105-fold. Figure 9 shows the difference in coverage between the three patients using the different exome capture systems.
Figure 9.
Whole exome sequence coverage of the linkage region in three patients. By design, the 38-Mb capture kit did not sequence the majority of the TTN gene (blue/red lines), although coverage was adequate for the 62-Mb capture kit (green line), thus identifying the causative mutation.
Table 4 shows the number of variant predictions from the exome sequence. The initial sequencing of Patients A-III:6 and A-IV:12 yielded four novel heterozygous variants in the linkage region (Table 5: note that insertion/deletions are only available for Patient A-III:6 because a technical problem resulted in the generation of non-paired-end reads for Patient A-IV:12). One of these variants caused an amino acid substitution, although this variant did not segregate with the disease within the families. One of the variants was in the TTN gene and segregation analysis was performed because of high suspicion for mutations in this gene. After exome sequencing was performed on Patient A-IV:10 by using a different probe set, 30 novel variants were identified. Three of these were in TTN and two further were predicted to be pathogenic (a deletion in the 5′-untranslated region of RAPGEF4 and a single base variant in the 5′-untranslated region of CERKL) (Table 6). These five variants were selected for segregation analysis. The remaining 25 variants either were non-coding changes that were not predicted to alter splice sites or had been eliminated in the first round of sequencing (Supplementary Table 2).
Table 4.
Summary of genetic variants detected from the first and second whole exome sequencing runs
| Patient | Variant type | Total predicteda | On targetb | dbSNP132c | Noveld | Shared novele | Linkage regionf |
|---|---|---|---|---|---|---|---|
| A-IV:12 | SBV | 163 998 | 39 756 | 39 510 | 741 | 64 | 2 |
| A-III:6 | 402 858 | 44 531 | 44 143 | 1 022 | |||
| A-IV:10 | 1 373 612 | 81 795 | 80 201 | 2 738 | – | 20 | |
| A-IV:12 | Indel | – | – | – | – | – | – |
| A-III:6 | 104 495 | 2736 | 1571 | 1102 | – | 2 | |
| A-IV:10 | 56 677 | 9740 | 6683 | 2566 | – | 10 |
a SBV = Varscan parameters minimum total coverage ≥ 5-fold; minimum variant coverage ≥ 3-fold, min. Quality > 10; Indel = Dindel output filter minimum variant coverage ≥ 4.
b Variants located within Agilent 38-Mb targets ± 500 bp (FG/AD) or Illumina 62-Mb targets ± 500 bp (RG), seen on both (forward and reverse) strands and (SBVs only) variant allele frequency > 24%.
c Variants that match dbSNP132 - hg19; there are some duplicate positions with different rs numbers included in the totals.
d Variants not found in dbSNP132.
e Novel SBVs shared between Patient A-III:6 and Patient A-IV:12.
f chr2:166 697 613–183 034 559 (reference sequence: GRCh37).
Table 5.
Candidate mutations considered for segregation analysis after the first whole exome sequencing run
| Gene | Chromosome | Position | Mutation type | Reference | Varianta | Coding change | Prediction | Segregation analysis |
|---|---|---|---|---|---|---|---|---|
| WIPF1 | chr2 | 175 437 060 | SBVb | C | T | R158K | Disease causing | Non-segregating |
| TTN | chr2 | 179 659 327 | SBVb | G | C | Intronic | Polymorphism | Non-segregating |
| GORASP2 | chr2 | 171 808 025 | Deletion | T | –G | Intronic | Polymorphism | N/A |
| CDCA7 | chr2 | 174 232 452 | Insertion | A | +T | 3′-UTR | Polymorphism | N/A |
Novel heterozygous variants shared between both patients (Patients A-III:6 and A-IV:12), within the linkage region.
a All variants are reported in the forward (5′ to 3′) direction; therefore, for reverse coding genes (such as TTN) intragenic locations are in reverse complement to those above.
b SBV = Varscan parameters minimum total coverage ≥ 5-fold; minimum variant coverage ≥ 3-fold, min.
Table 6.
Candidate mutations considered for segregation analysis after the second whole exome sequencing run
| Gene | Chromosome | Position | Mutation type | Reference | Varianta | Coding change | Prediction | Segregation analysis |
|---|---|---|---|---|---|---|---|---|
| TTN | chr2 | 179 410 829 | SBVc | A | G | C30071R | Polymorphism | Segregates with disease in all family members |
| TTNb | chr2 | 179 443 028 | SBVc | T | C | Intronic | Polymorphism | Non-segregating |
| TTN | chr2 | 179 455 928 | SBVc | G | A | P17607L | Disease causing | Non-segregating |
| RAPGEF4 | chr2 | 173 686 465 | Deletion | T | -AA | 5′-UTR | Disease causing | Non-segregating |
| CERKL | chr2 | 182 521 804 | SBVc | C | A | 5′-UTR | Disease causing | Non-segregating |
Novel heterozygous variants in Patient A-IV:10, within the linkage region, with amino acid exchanges or predicted to be disease causing.
a All variants are reported in the forward (5′>3′) direction, therefore for reverse coding genes (such as TTN) intragenic locations are in reverse complement to those above.
b This variant was not predictive to be deleterious and was non-coding, but given it was in our main candidate gene we felt it prudent to sequence this gene as well.
c SBV = Varscan parameters minimum total coverage ≥5-fold; minimum variant coverage ≥3-fold, min.
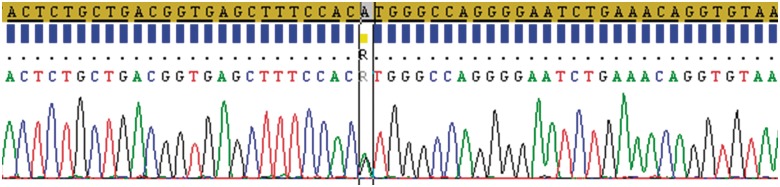
Segregation analysis
Sanger sequencing (Fig. 10) confirmed the presence of g.274375T>C in the TTN gene (Genebank#: AJ277892) in all affected individuals from Family A (n = 21), Family B (n = 9) and Family C (n = 1). The mutation was not detected in 182 ethnically-matched control subjects (364 chromosomes) or any of the unaffected family members (n = 9), who were sequenced using the same method. Other novel variants within the linkage region that caused amino acid substitutions and/or were predicted as pathogenic by MutationTaster were sequenced using the same method and did not segregate with the phenotype. To improve our confidence that the variant was the causative mutation, we identified exons within the TTN gene that were covered with<10-fold read-depth. This revealed 19 regions that were sequenced using 20 primer sets and the same method above. This analysis identified heterozygous polymorphism rs116792417 and novel heterozygous intronic single base variants g.21573C>T and g.162017A>T; neither of these were predicted to cause splice site changes. Furthermore, we selected 18 single base variants from the exome sequencing of Patient A-IV:10 that were in closest proximity to the putative mutation (Supplementary Table 3). These were sequenced in the other affected family members in order to further narrow the boundaries of the shared haplotype. Two variants upstream of the putative mutation demonstrated non-sharing of alleles with the mutation. The closest was at chromosomal position 179 236 831 (using GRCh37 as the reference sequence), in which sequencing in 13 affected individuals indicated that one was homozygous for the reference allele and 12 patients had rs6433724 (eight heterozygous and four homozygous), indicating that alleles were not shared with the mutation at this location. All of the variants downstream from the mutation (the furthest being rs6715406 at position 179 650 701) were sequenced in 30 affected individuals, but it was not possible to exclude allele sharing at those locations.
Figure 10.
Confirmatory Sanger sequencing demonstrating the heterozygous g.274375T>C substitution (p.Cys30071Arg) in exon 343 of TTN (indicated by ‘R’ in the box). This approach was used for the segregation analysis in three families.
These results narrowed the shared haplotype on chromosome 2 to positions 17 923 6831–182 166 459 (between rs2304340 and DS2310) for a maximum shared haplotype size of 2.93 Mb. The g.274375T>C mutation in TTN, which segregated with the disease in all family members, is at chromosomal position 179 410 829, which places it within this haplotype. This shared haplotype between the three families suggests a founder effect for this mutation.
Discussion
The heterozygous g.274375T>C substitution in TTN is highly likely to be the cause of hereditary myopathy with early respiratory failure in these families. It is a novel variant predicted to alter a highly conserved small/polar cysteine amino acid residue for a larger/basic arginine, which is likely to induce conformational change in A-band titin, and thus have functional consequences. The same variant segregates with the phenotype in three ostensibly unrelated families (a total of 31 affected and nine unaffected individuals) with the same rare disorder, and is not present in 364 control chromosomes. Other potentially pathogenic variants within the chromosomal region linked to the disease were excluded by direct sequencing. We also excluded the possibility of another mutation in TTN by sequencing the entire coding region of this gene. The exome sequencing had >10-fold coverage for all but 19 coding regions of TTN, and these remaining regions were excluded by Sanger sequencing. After further analysis of single nucleotide variants surrounding the putative mutation, the size of the shared haplotype in these three families was 2.93 Mbp, which contains only 10 protein-coding genes. The only sarcomeric protein in this region is TTN, and a muscle protein is the presumed cause of this disease due to the disturbed myofibrillar architecture on electron microscopy. As expected for a missense mutation, the size and abundance of the titin protein was normal in affected muscle, but the titin-binding partner calpain 3 was reduced, further implicating titin in the pathogenesis of the disorder. Finally, by carrying out a comprehensive study of the clinical phenotype in mutation carriers, we show that the clinical spectrum of disease in these families overlaps with that described in other families with mutations in the kinase domain of TTN (Lange, 2005), providing further evidence that TTN is the disease gene in the families described here.
Hereditary myopathy with early respiratory failure is a rare disease, but as we have demonstrated, there is enormous phenotypic variability within these families. The phenotype was mild or severe, with onset in early to late adulthood, and the predominant muscles affected were proximal, distal, axial, respiratory or, most frequently, a combination of these. Ultimately, nearly all patients eventually developed significant proximal and distal weakness, perhaps suggesting that the various initial presentations may converge into a common late-stage phenotype, as has been demonstrated in dysferlin myopathy (Paradas et al., 2010). Given these features of the condition and the difficulty in recognizing symptoms of respiratory failure due to muscle weakness (two of our patients were initially misdiagnosed as having obstructive sleep apnoea), it is quite possible that this disease is under-recognized, and the very small number of reported cases in the world literature (Table 7) may therefore under-represent the true prevalence of this disorder. This is compounded by the fact that muscle pathology can be non-specific (as was the case for 3/15 patients in our series), and even if detected, the presence of cytoplasmic bodies are a non-specific finding seen in other well-defined muscle diseases (Caron et al., 1999). Another common feature is Z-disc abnormality (Edstrom et al., 1990; Abe et al., 1993; Chinnery et al., 2001) and the accumulation of myofibrillar protein within inclusions, vacuoles and/or cytoplasmic bodies (Bertini et al., 1990; Baeta et al., 1996; Caron et al., 1999; Chinnery et al., 2001), which could result in cases of this disease being classified as myofibrillar myopathy [e.g. myopathy due to desmin, myotilin or filamin mutations may also present with early respiratory failure (Ferrer and Olive, 2008)]. Cytoplasmic bodies in hereditary myopathy with early respiratory failure have been found to contain desmin (Bertini et al., 1990; Baeta et al., 1996), dystrophin (Caron et al., 1999) and β-amyloid (Chinnery et al., 2001), which are also over-expressed in the muscle from patients with myofibrillar myopathy (Selcen, 2011). On account of these clinical and pathological similarities, as well as the similar genetic aetiology (since myofibrillar myopathies are caused by mutations in proteins associated with the Z-disc), it is reasonable to consider this disorder in the pathological differential diagnosis of myofibrillar myopathy, even though the hyaline and dark cytoplasmic abnormalities on trichrome stain are lacking in this disease.
Table 7.
Previously reported cases of cytoplasmic body myopathy with early respiratory failure
| Author, year | N | Onset age (years) | Myopathy characteristics | Other clinical features | Neurophysiology | Pathologic features | Outcome | Inheritance, linkage region |
|---|---|---|---|---|---|---|---|---|
| Kinoshita, 1975 | 1 | 16 |
|
Micrognathia, cleft palate | EMG: myopathic changes | Inclusions in muscle fibre periphery. Thickened Z-discs and disorganized myofibrillar material | Death at 23 years from RF | Sporadic, N/A |
| Jerusalem, 1979 | 1 | Childhood | Respiratory, axial and shoulder muscle weakness | EMG: active neurogenic changes | Numerous cytoplasmic bodies in type I fibres. Endoplasmic reticulum dilations in axons | Death at 31 years from RF | Sporadic, N/A | |
| Patel, 1983 | 3 | Childhood |
|
Scoliosis, dysmorphic features, cardiac hypertrophy and conduction defects, constipation | EMG: myopathic changes | Cytoplasmic bodies predominant in type I fibres |
|
Autosomal dominant or recessive, N/A |
| Winter, 1986 | 1 | 25 | Respiratory and proximal muscle weakness | Polydactyly, neck stiffness |
|
Eosinophilic cytoplasmic bodies, mainly in type I fibres and internal nuclei | Requiring intermittent positive pressure ventilation at night | Sporadic, N/A |
| Chapon, 1989 | 3 | 18, 40, 44 | Respiratory, axial and proximal weakness | Mild cardiac hypokinesis in one patient | EMG: myopathic changes. | Cytoplasmic bodies in type I fibres | Autosomal dominant, N/A | |
| Edstrom, 1990 | 16 (3 families) | 14–50 | Respiratory, proximal and sternomastoid weakness | EMG: myopathic changes | Myofibrillar lesions in Z-disks and distributed filamentous masses. Cytoplasmic bodies | Autosomal dominant, 2q24-31, R279W TTN mutation (Lange, 2005) | ||
| Bertini, 1990 | 1 | 1 | Respiratory failure, bulbar/neck flexor weakness | Hyporeflexia | EMG: myopathic changes | Inclusions with positive immunostaining for desmin and actin | Death at 14 months from RF | Sporadic |
| Abe, 1993 | 5 | 35–48 | Respiratory and distal muscle weakness, worst in tibialis anterior | Weight loss, finger contractures | EMG: myopathic changes, slight neurogenic changes | Eosinophilic inclusions. Cytoplasmic bodies predominantly in type I fibres | Early death from RF in some family members | Autosomal dominant, N/A |
| Baeta, 1996 | 1 | 67 | Respiratory failure (limited clinical information) | Cardiomyopathy | Cytoplasmic bodies predominantly in type I fibres | Autosomal dominant, N/A | ||
| Evangelista, 2009 | 1 | 74 | Hip flexor weakness, respiratory fatigue | Symptoms provoked by HMG-CoA reductase inhibitor therapy and improved with cessation |
|
Eosinophilic inclusions (termed as cytoplasmic bodies but no EM analysis) | Resolution with cessation of HMG CoA reductase inhibitor | Sporadic, N/A |
| Tasca, 2010 | 1 | 32 | Respiratory failure, neck flexor, hip flexor, hip flexor, tibialis anterior, peroneal weakness. Scapular winging and nasal voice | Eosinophilic inclusions. Diffuse IHC staining for sarcoplasmic proteins. Cytoplasmic bodies on EM. Z-line abnormalities | Sporadic, N/A (R279W TTN mutation was excluded) | |||
| Chinnery, 2001; Birchall, 2005; current study | 31 (3 families) | 22–71 | Respiratory failure, proximal and/or distal muscle weakness, some patients with neck flexor weakness | EMG: myopathic and active neurogenic changes | Eosinophilic inclusions, some rimmed vacuoles, no fibre-type predominance. No cytoplasmic bodies on EM | Slowly progressive course. Early death from RF in one patient. Night-time CPAP and walking aids for several family members | Autosomal dominant, 2q24-31, p.Cys30071Arg TTN mutation |
CPAP = continuous positive airway pressure; EM = electron microscopy; EMG = electromyography; IHC = immunohistochemistry; NCS = nerve conduction studies; RF = respiratory failure; M = male; F = female; HMG-CoA = 3-hydroxy-3-methyl-glutaryl-coenzyme A.
By studying the largest series of patients described to date, our observations cast light on the optimal means to diagnose and manage patients with this disorder, providing a guide to the natural history. Selective fat infiltration of semitendinosus on muscle MRI was present in all but one of the patients in this series, and was also present in all presymptomatic mutation carriers before symptom onset. MRI abnormalities of semitendinosus and peroneus longus (the two most frequently affected muscles in our series) are also observed in myofibrillar myopathies, particularly desminopathy, αB-crystallinopathy and myotilinopathy (refer to diagnostic algorithm in Fig. 5 of Wattjes et al., 2010). These shared patterns on MRI are not likely to be coincidental: it has already been demonstrated that phenotypes resembling ‘titinopathy’ can be caused by mutations in αB-crystallin and that the mechanism appears to be due to altered interaction of αB-crystallin with titin protein (Inagaki et al., 2006; Zhu et al., 2009). Our series has provided MRI data on 21 patients and firmly defines the MRI features of hereditary myopathy with early respiratory failure, showing for the first time that thigh MRI is a sensitive predictor of mutation status. Future MRI algorithms should include hereditary myopathy with early respiratory failure in the category of diseases that have predominant semitendinosus and peroneal muscle involvement. This would improve recognition and appropriate genetic testing for this condition. After diagnosis, the early recognition of asymptomatic respiratory failure and its treatment with nocturnal ventilation is likely to have improved the quality and length of life, with several individuals remaining semi-independent at home up to 31 years after the initial diagnosis.
The reported cases of this disorder in the world literature are summarized in Table 7, with the majority not defined genetically. For those cases with onset in adulthood, it seems plausible that these might also be due to TTN mutations, given the overlap of clinical and pathological findings. One of the reported adult-onset cases had cardiomyopathy, which was not demonstrated in any of our patients. Nonetheless, titin is also expressed in cardiac muscle and it is possible a different mutation in this gene could be responsible. The massive size of titin has rendered complete screening of this gene near-impossible in the past, but exome sequencing is a cost-effective way forward. However, our findings show that this should not be considered an ‘off the shelf’ routine clinical test at present. Our initial exome sequencing failed to identify the causative mutation in Family A because only a small proportion of titin was sequenced following 38-Mb capture. Only by further re-sequencing using a 62-Mb capture system did we obtain adequate coverage to detect the causal variant in this family.
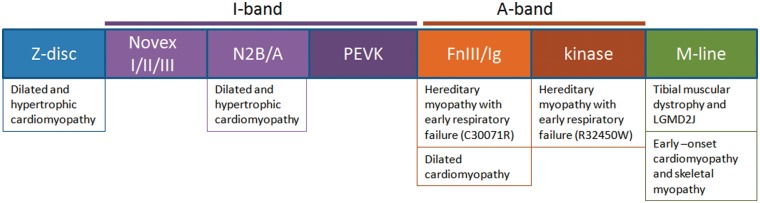
The spectrum of disease due to TTN mutations is already broad, and a schematic of the regional distribution of mutations causing the various phenotypes is summarized in Fig. 11. Mutations of the M-band region (at the C-terminal limit of the protein) cause tibial muscular dystrophy in heterozygous state (Hackman et al., 2002), which bears some similarity to hereditary myopathy with early respiratory failure due to its onset in adulthood, and preferential involvement of ankle dorsiflexion. Mutations that cause premature stop codons have been suggested to cause a more severe phenotype of this disorder in some reported families (Hackman et al., 2008). M-band mutations in homozygous state cause a severe, early onset skeletal myopathy, LGMD type 2J (Udd et al., 2005). Homozygous deletions in the M-band are causative of early onset cardiomyopathy and skeletal myopathy (Carmignac et al., 2007). A missense mutation in the kinase region of TTN (proximal to the M-band) has been demonstrated to be causative of hereditary myopathy with early respiratory failure in three families (Lange, 2005). Interestingly, the mutation described in the current report is a missense mutation proximal to the kinase region, in the A-band of titin. This suggests that the mechanism is not directly related to altered kinase activity of titin, and further study will be required to determine the cause of early respiratory muscle involvement, which appears to be mutation-specific at present. Given the myofibrillar pathology and inclusion bodies, the mutation may cause hyperaggregation of titin and/or its binding partners in the A-band or interference with the calpain 3 proteolytic system.
Figure 11.
Schematic diagram of the various domains of TTN (not drawn to scale), represented from N-terminus to C-terminus, and described based on their location within the sarcomere. There is some domain specificity for the observed phenotypes. Cardiomyopathy occurs from a broad range of mutations, although those in the N2B and A-band domains are most common (Herman et al., 2012). Mutations causing late-onset autosomal dominant myopathies are within the A-band, kinase region and M-line: tibial muscular dystrophy is caused by mutations in the M-line, and hereditary myopathy with early respiratory failure is now demonstrated to be caused by A-band or kinase mutations. The novex and N2B regions contain isoform-specific sequences (mainly for cardiac muscle). PEVK is the region characterized by repeats of amino acids PEVK. The A-band contains repetitive fibronectin III (FnIII) and immunoglobulin-like (Ig) elements (Gregorio et al., 1999; Bang et al., 2001; Freiburg et al., 2000; Krüger et al., 2009).
Protein studies from muscle in our patients did not reveal abnormalities in the most C-terminal part of titin with the antibodies tested. However, detailed pathological studies of eight muscle biopsies and three separate skeletal muscle tissues from a single patient (post-mortem material) demonstrated decreased calpain 3 expression. Calpain 3 is a muscle-specific calcium-dependent protease responsible for LGMD2A. Secondary reduction of calpain 3 on muscle biopsies has been reported in LGMD2B (Anderson et al., 2000) and LGMD2I (Yamamoto et al., 2008), without any apparent correlation between the levels of calpain 3 and the stage of muscle pathology (Charlton et al., 2009). However, in the post-mortem tissue studied here, the greatly reduced levels of calpain 3 in the diaphragm correlated with the severity of the myopathy. To our knowledge, this is the first report of comparative calpain 3 analysis in multiple muscle groups from the same patient and is consistent with the role of titin as a regulatory factor controlling calpain 3 autolysis (Ono et al., 2006). Although preliminary, these observations suggest that secondary loss of calpain 3 may exacerbate the disease.
In conclusion, we present a detailed clinical description of the largest reported series to date of patients with hereditary myopathy with early respiratory failure. This condition has variable clinical presentation, progressive respiratory muscle weakness, occasionally highly non-specific muscle pathology and as such is likely under-recognized. We show that patients with this condition may be identified when they are presymptomatic with muscle MRI, revealing semitendinosus and peroneus longus as the first affected muscles. In more advanced cases, semitendinosus, peroneus longus and obturator externus are the most commonly affected muscles on MRI. Using microsatellite linkage analysis and whole exome sequencing, we have identified the g.274375T>C mutation in TTN, which lies within a 2.93-Mb haplotype shared between these three families, and excluded the possibility of another TTN gene mutation by sequencing all coding regions of the gene. Hereditary myopathy with early respiratory failure can be due to mutations in the A-band (as in this report) and the kinase domain, and further study will be required to discover the full repertoire of TTN lesions capable of causing this disease.
Funding
This work was supported by the Association Francaise Contre les Myopathies. P.F.C. is a Wellcome Trust Senior Fellow in Clinical Science and an NIHR Senior Investigator who also receives funding from the Medical Research Council (UK) through the MRC Translational Neuromuscular Centre, the Wellcome Trust Centre for Mitochondrial Research, the UK NIHR Biomedical Research Centre for Ageing and Age-related disease and Biomedical Research Unit award to the Newcastle upon Tyne Foundation Hospitals NHS Trust. R.H. is supported by the MRC (UK). G.P. receives funding from the Clinician Investigator Program (University of British Columbia) and a Bisby Fellowship from the Canadian Institutes of Health Research.
Supplementary material
Supplementary material is available at Brain online.
Acknowledgements
We are grateful to Sharon Keers for technical assistance with the linkage analysis. We thank Dr Steve Laval and Dr Hanns Lochmuller for advice relating to this research.
Glossary
Abbreviations
- LGMD
limb girdle muscular dystrophy
Appendix A
| Current study | Birchall, 2005 | Chinnery, 2001 |
|---|---|---|
| Family A | ||
| Patient A-III:2 | Patient III:3 | |
| Patient A-III:3 | ||
| Patient A-III:6 | Patient A1 | Patient III:15 |
| Patient A-III:7 | Patient A2 | Patient III:11 |
| Patient A-III:8 | ||
| Patient A-III:16 | Patient III:10 | |
| Patient A-IV:1 | Patient IV:1 | |
| Patient A-IV:4 | ||
| Patient A-IV:6 | Patient A3 | |
| Patient A-IV:9 | ||
| Patient A-IV:10 | ||
| Patient A-IV:12 | Patient A4 | Patient IV:3 |
| Patient A-V:14 | ||
| Patient A-IV:16 | Patient IV:15 | |
| Patient A-IV:17 | Patient IV:12 | |
| Patient A-IV:19 | Patient IV:7 | |
| Patient A-IV:20 | Patient A5 | Patient IV:11 |
| Patient A-V:1 | ||
| Patient A-V:2 | ||
| Patient A-V:3 | ||
| Patient A-V:4 | ||
| Family B | ||
| Patient B-II:1 | Patient B3 | |
| Patient B-II:2 | Patient B2 | |
| Patient B-II:3 | ||
| Patient B-II-6 | ||
| Patient B-II:9 | Patient B1 | |
| Patient B-II:10 | ||
| Patient B-II:11 | ||
| Patient B-III:9 | ||
| Patient B-III:10 | ||
| Family C | ||
| Patient C-II:1 |
References
- Abe K, Kobayashi K, Chida K, Kimura N, Kogure K. Dominantly inherited cytoplasmic body myopathy in a Japanese kindred. Tohoku J Exp Med. 1993;170:261–72. doi: 10.1620/tjem.170.261. [DOI] [PubMed] [Google Scholar]
- Albers CA, Lunter G, MacArthur DG, McVean G, Ouwehand WH, Durbin R. Dindel: accurate indel calls from short-read data. Genome Res. 2011;21:961–73. doi: 10.1101/gr.112326.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson LV, Davison K. Multiplex Western blotting system for the analysis of muscular dystrophy proteins. Am J Pathol. 1999;154:1017–22. doi: 10.1016/S0002-9440(10)65354-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson LV, Harrison RM, Pogue R, Vafiadaki E, Pollitt C, Davison K, et al. Secondary reduction in calpain 3 expression in patients with limb girdle muscular dystrophy type 2B and Miyoshi myopathy (primary dysferlinopathies) Neuromuscul Disord. 2000;10:553–9. doi: 10.1016/s0960-8966(00)00143-7. [DOI] [PubMed] [Google Scholar]
- Baeta AM, Figarella-Branger D, Bille-Turc F, Lepidi H, Pellissier JF. Familial desmin myopathies and cytoplasmic body myopathies. Acta Neuropathol. 1996;92:499–510. doi: 10.1007/s004010050552. [DOI] [PubMed] [Google Scholar]
- Bang ML, Centner T, Fornoff F, Geach AJ, Gotthardt M, McNabb M, et al. The complete gene sequence of Titin, expression of an unusual ≈700-kDa Titin isoform, and its interaction with obscurin identify a novel Z-line to I-band linking system. Circ Res. 2001;89:1065–72. doi: 10.1161/hh2301.100981. [DOI] [PubMed] [Google Scholar]
- Bertini E, Ricci E, Boldrini R, Servidei S, Fusilli S, Dionisi-Vici C, et al. Involvement of respiratory muscles in cytoplasmic body myopathy–a pathology study. Brain Dev. 1990;12:798–806. doi: 10.1016/s0387-7604(12)80010-6. [DOI] [PubMed] [Google Scholar]
- Birchall D, von der Hagen M, Bates D, Bushby KM, Chinnery PF. Subclinical semitendinosus and obturator externus involvement defines an autosomal dominant myopathy with early respiratory failure. Neuromuscul Disord. 2005;15:595–600. doi: 10.1016/j.nmd.2005.05.002. [DOI] [PubMed] [Google Scholar]
- Carmignac V, Salih MA, Quijano-Roy S, Marchand S, Al Rayess MM, Mukhtar MM, et al. C-terminal titin deletions cause a novel early-onset myopathy with fatal cardiomyopathy. Ann Neurol. 2007;61:340–51. doi: 10.1002/ana.21089. [DOI] [PubMed] [Google Scholar]
- Caron A, Gohel C, Mollaret K, Morello R, Chapon F. Study of some components of the cytoskeleton in muscular disorders with nonspecific cytoplasmic bodies. Acta Neuropathol. 1999;97:267–74. doi: 10.1007/s004010050984. [DOI] [PubMed] [Google Scholar]
- Chapon F, Viader F, Fardeau M, Tome F, Daluzeau N, Berthelin C, et al. Familial myopathy with ‘cytoplasmic body’ (or ‘spheroid’) type inclusions, disclosed by respiratory insufficiency. Rev Neurol (Paris) 1989;145:460–5. [PubMed] [Google Scholar]
- Charlton R, Henderson M, Richards J, Hudson J, Straub V, Bushby K, et al. Immunohistochemical analysis of calpain 3: advantages and limitations in diagnosing LGMD2A. Neuromuscul Disord. 2009;19:449–57. doi: 10.1016/j.nmd.2009.05.005. [DOI] [PubMed] [Google Scholar]
- Chinnery PF, Johnson MA, Walls TJ, Gibson GJ, Fawcett PR, Jamieson S, et al. A novel autosomal dominant distal myopathy with early respiratory failure: clinico-pathologic characteristics and exclusion of linkage to candidate genetic loci. Ann Neurol. 2001;49:443–52. [PubMed] [Google Scholar]
- Edstrom L, Thornell LE, Albo J, Landin S, Samuelsson M. Myopathy with respiratory failure and typical myofibrillar lesions. J Neurol Sci. 1990;96:211–28. doi: 10.1016/0022-510x(90)90134-9. [DOI] [PubMed] [Google Scholar]
- Evangelista T, Ferro J, Pereira P, de Carvalho M. A case of asymptomatic cytoplasmic body myopathy revealed by sinvastatin. Neuromuscul Disord. 2009;19:66–68. doi: 10.1016/j.nmd.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Ferrer I, Olive M. Molecular pathology of myofibrillar myopathies. Expert Rev Mol Med. 2008;10:e25. doi: 10.1017/S1462399408000793. [DOI] [PubMed] [Google Scholar]
- Freiburg A, Trombitas K, Hell W, Cazorla O, Fougerousse F, Centner T, et al. Series of exon-skipping events in the elastic spring region of titin as the structural basis for myofibrillar elastic diversity. Circ Res. 2000;86:1114–21. doi: 10.1161/01.res.86.11.1114. [DOI] [PubMed] [Google Scholar]
- Gautier G, Verschueren A, Monnier A, Attarian S, Salort-Campana E, Pouget J. ALS with respiratory onset: clinical features and effects of non-invasive ventilation on the prognosis. Amyotroph Lateral Scler. 2010;11:379–82. doi: 10.3109/17482960903426543. [DOI] [PubMed] [Google Scholar]
- Gregorio CC, Granzier H, Sorimachi H, Labeit S. Muscle assembly: a titanic achievement? Curr Opin Cell Biol. 1999;11:18–25. doi: 10.1016/s0955-0674(99)80003-9. [DOI] [PubMed] [Google Scholar]
- Gudbjartsson DF, Jonasson K, Frigge ML, Kong A. Allegro, a new computer program for multipoint linkage analysis. Nat Genet. 2000;25:12–13. doi: 10.1038/75514. [DOI] [PubMed] [Google Scholar]
- Hackman P, Vihola A, Haravuori H, Marchand S, Sarparanta J, De Seze J, et al. Tibial muscular dystrophy is a titinopathy caused by mutations in TTN, the gene encoding the giant skeletal-muscle protein titin. Am J Hum Genet. 2002;71:492–500. doi: 10.1086/342380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hackman P, Marchand S, Sarparanta J, Vihola A, Penisson-Besnier I, Eymard B, et al. Truncating mutations in C-terminal titin may cause more severe tibial muscular dystrophy (TMD) Neuromuscul Disord. 2008;18:922–8. doi: 10.1016/j.nmd.2008.07.010. [DOI] [PubMed] [Google Scholar]
- Haravuori H, Vihola A, Straub V, Auranen M, Richard I, Marchand S, et al. Secondary calpain3 deficiency in 2q-linked muscular dystrophy: titin is the candidate gene. Neurology. 2001;56:869–77. doi: 10.1212/wnl.56.7.869. [DOI] [PubMed] [Google Scholar]
- Herman DS, Lam L, Taylor MR, Wang L, Teekakirikul P, Christodoulou D, et al. Truncations of titin causing dilated cardiomyopathy. N Engl J Med. 2012;366:619–28. doi: 10.1056/NEJMoa1110186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchinson D, Whyte K. Neuromuscular disease and respiratory failure. Pract Neurol. 2008;8:229–37. doi: 10.1136/pn.2008.152611. [DOI] [PubMed] [Google Scholar]
- Inagaki N, Hayashi T, Arimura T, Koga Y, Takahashi M, Shibata H, et al. Alpha B-crystallin mutation in dilated cardiomyopathy. Biochem Biophys Res Commun. 2006;342:379–86. doi: 10.1016/j.bbrc.2006.01.154. [DOI] [PubMed] [Google Scholar]
- Jerusalem F, Ludin H, Bischoff A, Hartmann G. Cytoplasmic body neuromyopathy presenting as respiratory failure and weight loss. J Neurol Sci. 1979;41:1–9. doi: 10.1016/0022-510x(79)90134-5. [DOI] [PubMed] [Google Scholar]
- Kinoshita M, Satoyoshi E, Suzuki Y. Atypical myopathy with myofibrillar aggregates. Arch Neurol. 1975;32:417–20. doi: 10.1001/archneur.1975.00490480083010. [DOI] [PubMed] [Google Scholar]
- Koboldt DC, Chen K, Wylie T, Larson DE, McLellan MD, Mardis ER, et al. VarScan: variant detection in massively parallel sequencing of individual and pooled samples. Bioinformatics. 2009;25:2283–5. doi: 10.1093/bioinformatics/btp373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krüger M, Linke WA. Titin-based mechanical signalling in normal and failing myocardium. J Mol Cell Cardiol. 2009;46:490–8. doi: 10.1016/j.yjmcc.2009.01.004. [DOI] [PubMed] [Google Scholar]
- Lange S, Xiang F, Yakovenko A, Vihola A, Hackman P, Rostkova E, et al. The kinase domain of titin controls muscle gene expression and protein turnover. Science. 2005;308:1599–1603. doi: 10.1126/science.1110463. [DOI] [PubMed] [Google Scholar]
- Li H, Durbin R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics. 2010;26:589–95. doi: 10.1093/bioinformatics/btp698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H, Handsaker B, Wysoker A, Fennell T, Ruan J, Homer N, et al. The sequence alignment/map format and SAMtools. Bioinformatics. 2009;25:2078–9. doi: 10.1093/bioinformatics/btp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindner TH, Hoffmann K. easyLINKAGE: a PERL script for easy and automated two-/multi-point linkage analyses. Bioinformatics. 2005;21:405–7. doi: 10.1093/bioinformatics/bti009. [DOI] [PubMed] [Google Scholar]
- Mellies U, Lofaso F. Pompe disease: a neuromuscular disease with respiratory muscle involvement. Respir Med. 2009;103:477–84. doi: 10.1016/j.rmed.2008.12.009. [DOI] [PubMed] [Google Scholar]
- Nicolao P, Xiang F, Gunnarsson LG, Giometto B, Edstrom L, Anvret M, et al. Autosomal dominant myopathy with proximal weakness and early respiratory muscle involvement maps to chromosome 2q. Am J Hum Genet. 1999;64:788–92. doi: 10.1086/302281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nogalska A, Terracciano C, D'Agostino C, King Engel W, Askanas V. p62/SQSTM1 is overexpressed and prominently accumulated in inclusions of sporadic inclusion-body myositis muscle fibers, and can help differentiating it from polymyositis and dermatomyositis. Acta Neuropathol. 2009;118:407–13. doi: 10.1007/s00401-009-0564-6. [DOI] [PubMed] [Google Scholar]
- Ono Y, Torii F, Ojima K, Doi N, Yoshioka K, Kawabata Y, et al. Suppressed disassembly of autolyzing p94/CAPN3 by N2A connectin/titin in a genetic reporter system. J Biol Chem. 2006;281:18519–31. doi: 10.1074/jbc.M601029200. [DOI] [PubMed] [Google Scholar]
- Paradas C, Llauger J, Diaz-Manera J, Rojas-Garcia R, De Luna N, Iturriaga C, et al. Redefining dysferlinopathy phenotypes based on clinical findings and muscle imaging studies. Neurology. 2010;75:316–23. doi: 10.1212/WNL.0b013e3181ea1564. [DOI] [PubMed] [Google Scholar]
- Patel H, Berry K, MacLeod P, Dunn HG. Cytoplasmic body myopathy. Report on a family and review of the literature. J Neurol Sci. 1983;60:281–92. doi: 10.1016/0022-510x(83)90069-2. [DOI] [PubMed] [Google Scholar]
- Qureshi AI, Choundry MA, Mohammad Y, Chua HC, Yahia AM, Ulatowski JA, et al. Respiratory failure as a first presentation of myasthenia gravis. Med Sci Monit. 2004;10:CR684–9. [PubMed] [Google Scholar]
- Schwarz JM, Rodelsperger C, Schuelke M, Seelow D. MutationTaster evaluates disease-causing potential of sequence alterations. Nat Methods. 2010;7:575–6. doi: 10.1038/nmeth0810-575. [DOI] [PubMed] [Google Scholar]
- Selcen D. Myofibrillar myopathies. Neuromuscul Disord. 2011;21:161–71. doi: 10.1016/j.nmd.2010.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorimachi H, Kinbara K, Kimura S, Takahashi M, Ishiura S, Sasagawa N, et al. Muscle-specific calpain, p94, responsible for limb girdle muscular dystrophy type 2A, associates with connectin through IS2, a p94-specific sequence. J Biol Chem. 1995;270:31158–62. doi: 10.1074/jbc.270.52.31158. [DOI] [PubMed] [Google Scholar]
- Tasca G, Mirabella M, Broccolini A, Monforte M, Sabatelli M, Biscione GL, et al. An Italian case of hereditary myopathy with early respiratory failure (HMERF) not associated with the titin kinase domain R279W mutation. Neuromuscul Disord. 2010;20:730–4. doi: 10.1016/j.nmd.2010.07.269. [DOI] [PubMed] [Google Scholar]
- Udd B, Vihola A, Sarparanta J, Richard I, Hackman P. Titinopathies and extension of the M-line mutation phenotype beyond distal myopathy and LGMD2J. Neurology. 2005;64:636–42. doi: 10.1212/01.WNL.0000151853.50144.82. [DOI] [PubMed] [Google Scholar]
- Winter JH, Neilly JB, Henderson AF, Stevenson RD, Doyle D, Wiles CM, et al. Life-threatening respiratory failure due to a previously undescribed myopathy. Q J Med. 1986;61:1171–8. [PubMed] [Google Scholar]
- Wattjes MP, Kley RA, Fischer D. Neuromuscular imaging in inherited muscle diseases. Eur Radiol. 2010;20:2447–60. doi: 10.1007/s00330-010-1799-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto LU, Velloso FJ, Lima BL, Fogaca LL, de Paula F, Vieira NM, et al. Muscle protein alterations in LGMD2I patients with different mutations in the Fukutin-related protein gene. J Histochem Cytochem. 2008;56:995–1001. doi: 10.1369/jhc.2008.951772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y, Bogomolovas J, Labeit S, Granzier H. Single molecule force spectroscopy of the cardiac titin N2B element: effects of the molecular chaperone alphaB-crystallin with disease-causing mutations. J Biol Chem. 2009;284:13914–23. doi: 10.1074/jbc.M809743200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.