Abstract
Background
On 30 September 2009, a 7.6 magnitude earthquake severely hit the coast of Padang city in West Sumatra, Indonesia leaving about 1,117 people dead and injuring another 3,515. Health consequences such as physical injury, co-morbidity, disability and quality of life over time are seldom reported among survivors after earthquakes.
Objectives
To investigate the associations between injury, disability and quality of life amongst adult survivors in Padang city after the 2009 earthquake.
Design/Methods
A prospective cohort study was conducted to compare adult injured (184) and adult non-injured (93) subjects over a 6-month period. Data on physical injury, co-morbidities, disability and quality of life were collected through interviews and measured quantitatively in three phases, i.e. at baseline, end of 3 and 6 months.
Results
Disability scores were consistently and significantly higher among injured subjects compared to non-injured, even when adjusted for co-morbidities (i.e. acute symptoms and chronic diseases). The highest disability score amongst injured subjects was attributed to ‘feeling discomfort/pain’. Quality of life attribute (QLA) scores, were significantly lower amongst injured people as compared to those non-injured even when adjusted for co-morbidities. The lowest QLA item score amongst the injured was ‘pain, depression and anxiety’. Significant and consistent negative correlations were found between disability and QLA scores in both the injured and non-injured groups.
Conclusion
Physical injury is significantly correlated with both higher disability and lower quality of life, while disability has significant negative correlation with quality of life. The findings suggest that, through disability, injury may contribute to decreased quality of life. It is therefore recommended to promptly and adequately treat injuries after disasters to prevent any potential for disability and hence restore quality of life.
Keywords: injury, disability, quality of life, quality of life attribute (QLA), earthquake, Padang, Indonesia
One of the strongest earthquakes in Indonesia in the recent times (magnitude of 7.6 on the Richter scale) struck on 30 September 2009 on the coast of West Sumatra at 17:16 hrs local time. Eleven of the 19 cities/districts were affected by the earthquake. Padang city, the capital of West Sumatra province, was amongst the worst hit (1). As of 28 October 2009, almost a month after the disastrous earthquake, authorities reported that as many as 135,299 buildings were severely damaged. Furthermore, an estimated 1,117 people were reported dead, 788 people experienced major injuries and 2727 minor injuries. The total affected population of the West Sumatra earthquake was estimated at about 1.2 million. It was also reported that 217 health facilities were damaged with various degrees of destruction (2).
Serious injuries like crush syndromes, sustained during earthquakes, by their nature may lead to long term health consequences such as disability or chronic physical and mental stressors. Further physical disabilities may also result from negligence, inadequate management or mismanagement of serious injuries (3).
Although disability as a patient outcome is a significant concern; it has not been sufficiently addressed in existing literature (4).
Following the Padang city earthquake long term health consequences of physical injuries in the presence of co-morbidities resulting in disability and/or decrease in quality of life among the survivors were neither completely documented over time nor studied. This was partly due to limitations in recording and reporting of relevant medical data during the emergency phases. Understanding the epidemiology of health consequences after an earthquake and the associations between physical injury, disability and the resulting quality of life, would be beneficial in preventing and limiting future disaster impacts. This study aims to investigate these associations amongst the injured adults after the Padang city earthquake and further the discussion on preparedness planning after earthquakes.
Methodology
Study area and population
Padang is the capital city of West Sumatra Province in Indonesia with total population of 856,000 and a population density of 1,233 people/km2 (5). Geographically, Padang has broad range of altitude from 0–1833 m above sea level and its western part lies in the Indian Ocean.
Concerning the potential hazards of earthquakes, it is important to note that the city is located on the Eurasian plate and quite near to the inter-plate boundary between the Eurasian Plates and Indo-Australian Plates. This inter-plate boundary is reported to be the most seismically active in the region (6).
Study design
A prospective cohort study was conducted from February to August 2010. Two cohorts of injured and non-injured adult survivors were compared longitudinally. Both the cohorts were followed-up for a total period of 6.5 months.
Data were collected at baseline and at two endpoints – months 3 and 6.
Definitions used
Injury was defined as: ‘damage to a person's body in a physical sense such as a graze, bruise, sprain, strain, broken bone, etc.’ (7), while disability was defined as: ‘a physical or mental impairment that substantially limits one or more major life activities.’ (8). Quality of life was defined as: ‘Reflection on how an individual spends his daily life in good way’ (9). Quality of life was measured by Quality of Life Attribute (QLA) scoring system.
Inclusion and exclusion criteria
The inclusion criteria of the cohort of injured survivors were as follows:
Adult (i.e. aged 18 years old or older, and/or had already been married) survivor, suffered from injury during the earthquake.
Has been a permanent resident of Padang city at the beginning of the study.
Can still make effective verbal communication and were willing to participate cooperatively during 6-month follow-up of period.
The inclusion criteria for the cohort of non-injured survivors were the same as the injured cohort except that they did not suffer any injury from the earthquake and were living as close neighbors (i.e. next to the houses) of the injured cohort participants.
During the 6-month follow-up period, the cohort participants could also be excluded with following criteria:
Worsening health condition or undergoing major treatment (e.g. major surgery) within the injured cohort.
No longer willing to continue participation in the middle of follow-up.
Moving out from Padang city in the middle of follow-up.
Data sources and collection
The injured subjects were identified and listed from several available sources of injury cases, i.e. the data compilation of the injured victims obtained from Health Office, Handicap International (NGO), five main general hospitals in Padang City (i.e. one provincial general hospital, one city general hospital, and three private general hospitals) and also a specific list of injured victims obtained from five villages/sub-district Offices in Padang City. Each of eligible injured case was then traced back to his/her respective home and mapped for the purposes of verification, invitation and agreement to participate in the study. The eligible non-injured subjects were identified from the neighboring households of selected injured subjects.
The whole data collection activities from phase 1 (at baseline) until phase 3 (6-month follow-up) were done from third week of January 2010 (almost 4 months after the earthquake) until the first week of August 2010.
Sample size
In this study, from the aforementioned sources, we recruited in the beginning of the study 184 adult injured survivors (regardless of the degree of severity) who met the study inclusion criteria, as identified. As comparison, a non-injured cohort group consisting of 93 adult non-injured survivors was randomly selected from the neighboring households living closest to the households of the selected injured cohort participants. The above sample size gave sufficient statistical powerful to test the main hypothesis ‘that injury is associated with disability and with quality of life’. However, due to loss to follow-up, size of injured cohort reduced from 184 at baseline to 150 at the end of study, while the size of non-injured cohort reduced from 93 at baseline to 80 at the end of study.
Study instruments
Quantitative structured interviews were conducted in three phases of data collection, i.e. first phase at baseline period, second phase at third month follow-up period, and the third phase at sixth month follow-up period.
To assess the score of disability, a questionnaire was developed by modifying the disability questionnaire of Basic Health Research (Riskesdas) from the Health Research and Development Institute, Ministry of Health (Badan Litbangkes, Kemenkes) which was then pilot tested in the field. The questionnaire consisted of 20 basic components assessing the ability to conduct Activities of Daily Living (ADL) during the past 1 month (i.e. mobility, self maintenance ability, pain and uncomfortable feeling, memory ability, interpersonal relationship, rest and sleep, feeling, hearing and seeing ability). For each question five response categories that corresponded with five scales of score, ranging from 1.0 for ‘very easy’ (no disability/limitation) to 5.0 for ‘very difficult (severe/total disability/limitation) were offered. Thus, the possible disability scores ranged from score of ‘20’ (if all 20 disability questions were answered ‘very easy’) to a score of ‘100’ (if all 20 disability questions were answered ‘very difficult’). Total score were summarized as total average disability scores with equal weighting for each question.
For assessing score of quality of life attributes, the Indonesia Health Related Quality of Life Questionnaire, which was originally developed, validated and patented by one of the authors, Rivany (9), was adapted and modified for the disaster setting in Padang city. The adjusted questionnaire consisted of 10 quality of life attributes (QLA) including aspects of mobility, private activities, common and social activities, vision, hearing, food tasting, oral communication, communication, pain, depression and anxiety. The score scale for each question ranged from 0.0 (zero) referring to lowest ability to perform quality of life attribute to 3.0 or 4.0 in seven questions referring to highest ability to perform quality of life attribute. Thereby, the possible QLA scores ranged from score of ‘0’ (if all 10 questions were given lowest answer option of ‘0’) to the score of ‘37’ (if all 10 questions were given the highest answer option of ‘3’ or ‘4’). Total score were summarized as total average QLA scores with equal weighting for each question.
This paper reports the results of analysis of the main variables, i.e. injury, co-morbidity, disability and quality of life after the earthquake and their relevant determinants (e.g. socio-demographic factors), at baseline and statistical testing of main associations between injury and the degree of disability and quality of life amongst the injured and non-injured.
Ethical clearance and data analysis
Ethical clearance was obtained from the Ethical Research Committee of Faculty of Public Health (FPH), Universitas Indonesia (UI) and legal study permits were obtained from relevant authorities in Padang city.
Data was entered, cleaned and analyzed using EpiData® version 2.0 and SPSS® version16.
Results
Socio-demographic characteristics
Our study found that, there were higher proportions of males (although majority of both injured and non-injured subjects were females); young adults (aged 18–29); older people (aged 50 and above); single/widowed individuals; moderate size household; less educated (junior high school or lower); and housewife/student/unemployed individuals in the injured group as compared to the non-injured group (Table 1). The study also indicated that occupation of the individual also determined the impact from the earthquake. The majority of the injured lived in permanent houses (64.6%), while the majority of the houses in both groups showed partial to total destruction of the house wall.
Table 1.
Socio-demographic characteristics at baseline
| Injured (n=184)* | Non-injured (n=93)** | ||
|---|---|---|---|
| Socio-demographic characteristics | Frequency (%) | Frequency (%) | p-Value*** |
| Gender | |||
| Male | 53 (28.8) | 22 (23.7) | 0.36 |
| Female | 131 (71.2) | 71 (76.3) | |
| Age group | |||
| 18–29 | 52 (28.3) | 15 (16.1) | 0.68 |
| 30–39 | 27 (14.7) | 26 (28.0) | |
| 40–49 | 28 (15.2) | 24 (25.8) | |
| 50–59 | 45 (24.5) | 18 (19.4) | |
| 60–85 | 32 (17.4) | 10 (10.8) | |
| Marital status | |||
| Married | 124 (67.2) | 76 (81.7) | 0.01 |
| Never/ever been married (single/widowed) | 60 (32.7) | 17 (18.3) | |
| Influence of earthquake on occupation/daily activities | |||
| No influence at all | 59 (32.0) | 41 (44.1) | 0.02 |
| Slightly influenced | 72 (39.1) | 36 (38.7) | |
| Much influenced (job were disturbed/lost) | 53 (28.8) | 16 (17.2) | |
| Type of your house at the time of earthquake | |||
| Not or semi permanent | 63 (35.4) | 36 (39.1) | 0.55 |
| Permanent | 115 (64.6) | 56 (60.9) | |
| Level of house damage | |||
| Severe/total damaged | 51 (28.5) | 28 (30.4) | 0.83 |
| Moderate damaged | 73 (40.8) | 32 (34.8) | |
| Slight damaged | 55 (30.7) | 32 (34.8) | |
*Size (number of subject) of injured cohort group at baseline of study.
**Size of non-injured cohort at baseline of study.
Injury and co-morbidity
As shown in Table 2, after bruises (41%), bone fracture and/or dislocation (39%) were the most predominant type of injury. The extremities (both upper and lower) were the most affected part of the injured body (81%). Among the injured, almost half (about 45%) sustained various types and degrees of physical impairment including non-union or mal-union (deformed) of bone fractures (14%) and amputated or paralyzed extremities (9%). It is important to note that the injury occurred at the time of earthquake, while the impairment may have occurred during the time period between the earthquake and baseline interview (which was almost 4 months after the earthquake).
Table 2.
Injury characteristics among injured group at baseline
| Injury characteristics (n=184) | Frequency (%) |
|---|---|
| Type of injury | |
| Bone fracture | 51 (27.9) |
| Dislocation | 21 (11.5) |
| Sprain/wrench | 46 (25.1) |
| Laceration/torn/puncture wound | 49 (26.6) |
| Bruise | 75 (41.0) |
| Others (including burnt injury) | 12 (6.6) |
| Part of the body that was injured | |
| Face, head and neck | 47 (25.6) |
| Thorax and/or abdomen | 12 (6.6) |
| Spine/vertebrae | 34 (18.6) |
| Upper extremities | 42 (23.0) |
| Lower extremities | 106 (57.9) |
| Both upper and/or lower extremities | 133 (72.3) |
Concerning co-morbidity characteristics, the first phase of cohort study at baseline showed that the injured group reported significantly (p=0.02) higher proportions of acute (within the last 2 weeks) complaints as compared to the non-injured group (Table 3). Similarly, diagnosed chronic diseases were higher in the injured group as compared to the non-injured group, although not statistically significant.
Table 3.
Co-morbidity characteristics at baseline
| Percentage (%) | ||
|---|---|---|
| Co-morbidity | Injured (n=184) | Non-injured (n=93) |
| Ever diagnosed by a doctor as having at least one of the chronic diseases* | 27.3 | 21.7 |
| Cardiovascular | 7.7 | 7.5 |
| Hypertension | 11.5 | 11.8 |
| Stroke | 1.6 | 1.1 |
| Pulmonary TB and/or other chronic pulmonary diseases | 6.6 | 4.3 |
| Diabetes | 2.7 | 0 |
| Others (including hepatitis and renal disease) | 7.2 | 5.4 |
| Experiencing at least one complaints (symptoms and/or signs) within the last 2 weeks** | 79.2 | 66.7 |
| Fatigue | 24.0 | 23.7 |
| Headache, dizziness, migraine | 33.3 | 33.3 |
| Muscle and/or joint pain | 47.5 | 19.4 |
| Fever, high body temperature | 11.5 | 17.2 |
| Cough/running nose and/or difficulty in breathing | 12.6 | 19.4 |
| Chest pain/cardiac palpitation | 7.7 | 9.7 |
| Diarrhea, nausea, vomiting, gastric pain, stomach ache | 6.6 | 8.6 |
| Others (including dermatitis, skin wound and infection) | 11.1 | 6.5 |
*p-Value=0.31 (by chi-square test).
**p-Value=0.02 (by chi-square test).
In both the groups, history of hypertension and cardiovascular diseases were the most frequently reported diagnosed chronic illnesses, while muscle and/or joint pain, headache and fatigue were among the most prevalent acute complaints.
Disability status
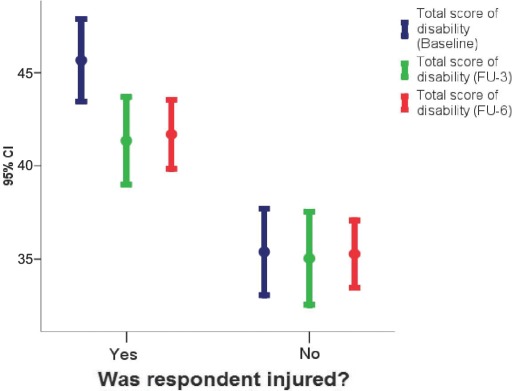
In all three phases of the cohort study (the mean and median of total disability scores were all consistently and significantly (p<0.0005) higher in the injured subjects as compared to the non-injured ones (Table 4). This trend could also be clearly seen in Fig. 1. Additionally all items of disability component, except having cough/sneezing, showed consistent higher average scores in the injured group in all three phases (Table 4). Amongst the injured subjects, during the entire study period, the highest average scores of disability were attributed by the respondents to feeling of discomfort/pain.
Table 4.
Scoring of disability components at baseline, follow-up at month 3 (FU-3) and at month 6 (FU-6)
| Mean score* of disability | ||||||
|---|---|---|---|---|---|---|
| Injured (n=150)** | Non-Injured (n=80)*** | |||||
| Disability components (DC) | Baseline | FU-3 | FU-6 | Baseline | FU-3 | FU-6 |
| DC1 to see and recognize other person across the street | 2.4 | 2.3 | 2.3 | 2.0 | 2.1 | 2.1 |
| DC2 to see and recognize an object located approximately 30 cm from you | 2.5 | 2.5 | 2.5 | 2.1 | 2.4 | 2.3 |
| DC3 to hear other person talking with a normal voice who is standing at the other side of the room you are in | 2.1 | 1.9 | 2.1 | 1.9 | 1.8 | 1.9 |
| DC4 to hear a person talking with other person in a quiet room | 2.1 | 1.7 | 1.9 | 1.9 | 1.6 | 1.7 |
| DC5 feel discomfort/pain | 3.1 | 3.0 | 2.7 | 2.1 | 2.3 | 2.2 |
| DC6 feel shortness of breath after finishing a mild exercise | 1.6 | 1.6 | 1.5 | 1.3 | 1.5 | 1.4 |
| DC7 cough or sneeze for 10 min duration or more | 1.4 | 1.5 | 1.4 | 1.4 | 1.5 | 1.4 |
| DC8 experience sleeping disorder | 2.4 | 2.6 | 2.4 | 1.8 | 2.2 | 1.9 |
| DC9 experience health problem that affects your emotion in shape of sadness and depressed | 2.4 | 2.3 | 2.0 | 2.0 | 1.9 | 1.7 |
| DC10 difficulty to stand up in 30 min duration | 2.6 | 2.4 | 2.3 | 1.6 | 1.8 | 1.7 |
| DC11 difficulty to walk as far as 1 km | 2.6 | 2.6 | 2.5 | 1.7 | 1.8 | 1.6 |
| DC12 to focusing your thought to one activity or try to remember something as long as 10 min | 2.4 | 2.0 | 2.2 | 2.1 | 1.9 | 1.9 |
| DC13 to clean your whole body for example taking a bath | 2.2 | 1.8 | 1.8 | 1.5 | 1.4 | 1.6 |
| DC14 to get dressed | 2.2 | 1.7 | 1.8 | 1.5 | 1.3 | 1.5 |
| DC15 to do your daily activities/chores | 2.5 | 2.0 | 2.1 | 1.6 | 1.5 | 1.7 |
| DC16 to understand other people is saying | 2.0 | 1.8 | 1.9 | 1.6 | 1.6 | 1.7 |
| DC17 to interact/socialize with a stranger | 2.0 | 1.9 | 1.9 | 1.7 | 1.6 | 1.7 |
| DC18 to maintain your friendship | 2.1 | 1.8 | 2.0 | 1.7 | 1.6 | 1.7 |
| DC19 to do your duty as your responsibility as a member of a household | 2.5 | 2.1 | 2.2 | 1.8 | 1.7 | 1.8 |
| DC20 to participate in the social activities (neighborhood gathering, Qur'an recital, religious activity | 2.6 | 2.1 | 2.2 | 2.1 | 1.7 | 1.9 |
| DC21 in general, how extent those difficulties you are facing affect your life | 2.9 | 2.2 | 2.0 | 2.3 | 1.8 | 1.4 |
| Central tendency comparisons of disability score | ||||||
| Mean (Std Dev) | 45.3 (13.8) | 41.2 (14.6) | 41.8 (11.2) | 35.6 (10.7) | 35.3 (11.4) | 35.6 (8.7) |
| Median | 45.0 | 39.0 | 40.0 | 35.0 | 35.0 | 35.0 |
| Range | 2–76 | 20–89 | 23–79 | 20–59 | 20–64 | 20–64 |
| p-Values of mean comparisons**** | <0.0005 | <0.0005 | <0.0005 | |||
*Item range 1–5; total range 20–100.
**Size (number of subject) of injured group at the end (i.e. after 6 months) of study.
***Size of non-injured group at the end of study.
****Calculated based on independent t-test, comparing mean of disability scores in injured group with mean in non-injured group, at baseline, at FU-3 and at FU-6.
Fig. 1.
Comparison of disability scores between injured and non-injured groups.
After adjusting for co-morbidities, i.e. perceived acute symptom and history of chronic disease the total disability scores among injured cohort were all significantly higher than the scores amongst the non-injured cohort as indicated by the coefficients of multiple linear regression at baseline (8.7), at month 3 follow-up (5.8) and at month 6 follow-up (4.1) and the corresponding p-values (p<0.0005, p=0.001 and p=0.001. respectively) (Table 5).
Table 5.
Correlation between injury and disability score, using multiple linear regression, adjusted by chronic diseases and acute symptoms, at every phase of study
| Variables | At baseline | At follow-up month 3 | At follow-up month 6 | |||
|---|---|---|---|---|---|---|
| Unstandardized coefficients | Standardized coefficients | Unstandardized coefficients | Standardized coefficients | Unstandardized coefficients | Standardized coefficients | |
| Beta (Std. Error) | Beta | Beta (Std. Error) | Beta | Beta (Std. Error) | Beta | |
| (Constant) | −50.13 (2.87) | −39.03 (2.99) | −38.64 (2.01) | |||
| Chronic diseases | −12.14 (1.83) | −0.387 | −8.5 (1.76) | −0.289 | −7.7 (1.26) | −0.346 |
| Acute symptoms | −0.71 (1.84) | −0.023 | −6.63(2.0) | −0.197 | −5.94 (1.23) | −0.273 |
| Injury (reference: non-injured) | 8.72* (1.63) | 0.308 | 5.8** (1.78) | 0.193 | 4.08*** (1.23) | 0.185 |
*p-Value<0.0005.
**p-Value=0.001.
***p-Value=0.001.
Status of quality of life
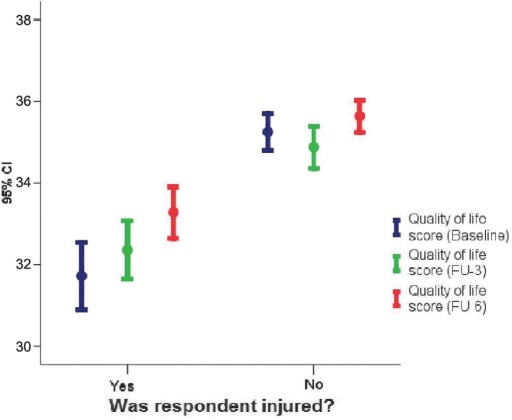
Concerning the quality of life, which was measured quantitatively by scores of quality of life attribute (QLA), the mean and median of total average of QLA scores in every phase of the cohort study (i.e. at baseline, at 3- and 6-month follow-up), were all consistently and significantly (p<0.0005) lower among the injured subjects as compared to the non-injured (Table 6). Fig. 2 shows this trend clearly and also shows that during the 6-month follow-up period the increasing trend of quality of life was more apparent in the injured group. In all phases of the study, particular items of QLA (except hearing and food tasting in month 6 follow-up) showed lower average scores in the injured group (Tables 5 and 6). Among the injured subjects the lowest average QLA score was attributed to pain, depression and anxiety during the entire study period.
Table 6.
Scoring of quality of life attributes at baseline, follow-up at month 3 (FU-3) and at month 6 (FU-6)
| Quality of life attributes (QLA) | Mean score* of quality of life attributes (QLA) | |||||
|---|---|---|---|---|---|---|
| Injured (n=150)** | Non-injured (n=80)*** | |||||
| Baseline | FU-3 | FU-6 | Baseline | FU-3 | FU-6 | |
| QLA-1 mobility | 3.2 | 3.3 | 3.4 | 3.9 | 3.9 | 3.9 |
| QLA-2 private activities | 3.3 | 3.5 | 3.7 | 4.0 | 3.9 | 4.0 |
| QLA-3 common and social activities | 3.2 | 3.5 | 3.6 | 4.0 | 3.9 | 3.9 |
| QLA-4 vision | 3.4 | 3.5 | 3.5 | 3.7 | 3.6 | 3.8 |
| QLA-5 hearing | 3.7 | 3.9 | 4.0 | 3.9 | 4.0 | 4.0 |
| QLA-6 food tasting | 4.0 | 3.9 | 4.0 | 4.0 | 4.0 | 4.0 |
| QLA-7 oral communication | 3.9 | 3.9 | 3.9 | 4.0 | 4.0 | 4.0 |
| QLA-8 communication | 3.9 | 3.8 | 3.9 | 4.0 | 4.0 | 4.0 |
| QLA-9 pain | 2.9 | 2.7 | 2.9 | 3.5 | 3.4 | 3.5 |
| QLA-10 depression and anxiety | 2.9 | 2.9 | 3.1 | 3.0 | 3.1 | 3.6 |
| Central tendency comparisons of QLA scores | ||||||
| Mean (Std Dev) | 31.8 (5.1) | 32.4 (4.4) | 33.3 (3.9) | 35.1 (2.6) | 34.7 (2.6) | 35.5 (2.1) |
| Median | 34.0 | 34.0 | 34.0 | 36.0 | 36.0 | 36.0 |
| Range | 11–37 | 15–37 | 20–37 | 20–37 | 24–37 | 26–37 |
| p-Values of mean comparisons**** | <0.0005 | <0.0005 | <0.0005 | |||
*Item range 0–4; total range 0–37.
**Size (number of subject) of injured group at the end (i.e. after 6 months) of study.
***Size of non-injured group at the end of study.
****Calculated based on independent t-test, comparing mean of QLA scores in injured group with mean in non-injured group, at baseline, at FU-3 and at FU-6.
Fig. 2.
Comparison of QLA (quality of life attributes) scores between injured and non-injured groups.
After adjusting for co-morbidities (i.e. the perceived acute symptom and history of chronic disease), the total scores of quality of life attributes (QLA) amongst the injured cohort were all significantly lower than the scores amongst the non-injured cohort as indicated by the coefficients of the regression at baseline (−3.0), at month 3 follow-up (−2.4) and at month 6 follow-up (−1.6), and the corresponding p-values (all<0.0005) (Table 7).
Table 7.
Correlation between injury and quality of life attributes (QLA) score, using multiple linear regression, adjusted by chronic diseases and acute symptoms, at every phase of study
| Variables | At baseline | At follow-up month 3 | At follow-up month 6 | |||
|---|---|---|---|---|---|---|
| Unstandardized coefficients | Standardized coefficients | Unstandardized coefficients | Standardized coefficients | Unstandardized coefficients | Standardized coefficients | |
| Beta (Std. Error) | Beta | Beta (Std. Error) | Beta | Beta (Std. Error) | Beta | |
| (Constant) | −29.59 (1.0) | −31.96 (0.94) | −33.15 (0.69) | |||
| Chronic diseases | 3.8 (0.64) | 0.36 | 2.24 (0.55) | 0.25 | 2.39 (0.43) | 0.33 |
| Acute symptoms | −0.25 (0.64) | −0.02 | 1.63 (0.63) | 0.16 | 0.66 (0.42) | 0.09 |
| Injury (reference: non-injured) | −3.03* (0.57) | −0.31 | −2.35** (0.56) | −0.25 | −1.61*** (0.42) | −0.22 |
*p-Value<0.0005.
**p-Value<0.0005.
***p-Value<0.0005.
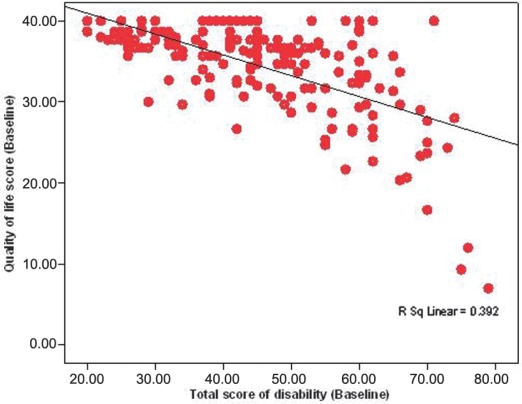
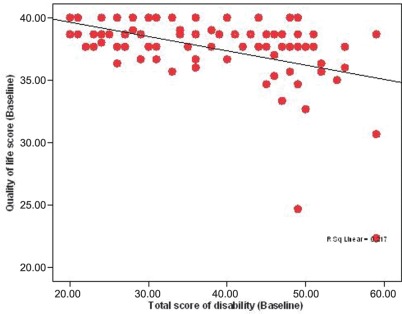
Disability scores were negatively correlated to QLA scores at baseline observation, i.e. in the injured group; r=−0.26 for unstandardized coefficients (or −0.63 standardized coefficients), while in non-injured group; r=−0.12 for unstandardized coefficients (or −0.47 for standardized coefficients) (Figs. 3 and 4). This means that every unit increase of total average disability score is significantly followed in linear pattern by decrease of every unit of total average QLA score. The negative correlations in both injured and non-injured groups were consistent and equally significant (p-values<0.0005). However, the slopes of these negative correlations were found larger in injured subjects than those in the non-injured subjects.
Fig. 3.
Correlation between disability and QLA (quality of life attributes) scores among injured subjects.
Fig. 4.
Correlation between disability and QLA (quality of life attributes) scores among non-injured subjects.
Discussion
Few studies indicate that women were relatively more affected by earthquake injuries than men (10–14). After the tsunami disaster in Aceh, odds of injury of the females were 50% significantly lower than that of the males (15). Our study did not suggest any significant relationship between gender and injury.
The fact that proportions of young adults (aged 18–29 years) and older people (aged 50 and above) were higher than the other age categories (i.e. 30–39 and 40–49) in the same injured group and that the young adults and elder categories in injured group were higher than the same categories in non-injured group, may indicate a bimodal-like pattern. A similar pattern was reported in another study in Pakistan (10). Assuming the pattern is correct, it is understandable that elderly people would be a more vulnerable segment of adult population, due to limitations in their movement making it difficult for them to escape from danger. However, it is unclear as to why younger adults aged 18–29 years were more frequently injured than the older complement age group, i.e. 30–49 years. Nevertheless, our findings did not indicate any significant association between age and injury, suggesting that the bimodal-like pattern needs further investigation. There are some other studies that reported either consistent findings with our study, such as earthquake studies from Kocaeli, Turkey (12) and Armenia (14) or inconsistent findings, such as from the Northridge earthquake, California that indicated a significant relationship between age and injury (16).
Like the study from Luzon earthquake in The Philippines (17), our study also showed that most of the injured subjects were either single or widowed by marital status. The proportion of the injured subjects having single/widowed marital status (about 33%) were significantly (p-value=0.01) higher than the proportion of the non-injured subjects having the corresponding status (18%). This finding may indicate that being single/widowed somehow contributed to higher risk of injury as compared to being married. The reasons are difficult to explain and in-depth exploration of associated socio-economic and/or psychological factors is required.
As for the type of injury, our findings suggest that minor injuries like bruises, lacerations, and wounds were the dominant type of injury. This was supported by the Microdis literature review report which stated that majority of injuries after an earthquake were simple contusions, lacerations, cuts and minor soft tissue injuries. Bone fracture and/or dislocation the most common orthopedic injury (18) were the second most predominant type of injury (17). Similarly with a study report from Marmara earthquake in Turkey (11), we found that extremity fractures (both upper and lower) were reported in a majority (72%) of the injured survivors.
With respect to the body part injured, the thorax and abdomen injuries were less (only about 7%). However, since the proportion of injured body part in our study was only counted among the living survivors, it is quite likely that this small proportion was underestimated due to the possibility that more serious cases of thorax and abdomen injuries might not have survived. A study from Northridge earthquake, California (16) observed that head, thoracic, abdominal and lower extremity injuries, in consecutive order, were the most frequent injuries seen in dead victims. Another study of Hanshin-Awaji earthquake reported that the mortality rate from head, abdominal and thoracic injuries was the highest (19).
In this study, the occurrence of perceived acute complaints and chronic diseases were also investigated as important co-morbidities of the injury. Our study showed that within 2 weeks before interview, injured subjects significantly reported higher proportion of acute complaints, as compared to the non-injured group (79 vs. 67%). The high proportion (79%) of any acute complaints, especially muscle and/or joint pain, headache and fatigue (with proportion ranging from 24 to 48%) among injured subjects may be suspected as continuing symptomatic health problems since the occurrence of injury in the last 4 months. Learned from another study (20) among patients of social anxiety disorder in Philadelphia and New York, the persistent symptomatic health problems may reduce life satisfaction and hence affect significantly further quality of life.
Concerning the chronic disease co-morbidity, we found that our estimate of prevalence rates of diagnosed cardiovascular disease in both the injured (7.7%) and the non-injured (7.5%) group were higher than the official estimate of the corresponding rate in population of West Sumatra province in 2007, i.e. 1.3% (21). Similarly, our estimate of prevalence rate of hypertension in both the injured group (11.5%) and the non-injured group (11.8%) was higher than the official estimate of the corresponding rate in population of West Sumatra province in 2007, i.e. 7.6% (21). The reported increases of acute presentation of chronic disease prevalence were also reported in another study in Aceh, after the tsunami (15).
It is not difficult to understand that serious injuries due to disaster may cause disability. Our findings showing an evidence that injury is associated with the increase the disability score, were in line with findings from another study about disaster-related illness and injury from hurricane Ike striking Galveston, Texas in September, 2008. This hurricane study demonstrated that those with personal injuries and household illnesses have an increased risk of disability (22).
As injury leads to disability and disability affects quality of life, we may expect, as actually proven in our study, that injury decreases the quality of life. Our study results demonstrated that during the whole 6 months follow-up period, most items of quality of life attributes, especially items of pain, depression and anxiety, were perceived worse, among the injured subjects as compared to the non-injured ones. This fact is supported by some other studies too. A study of SCI (spinal cord injury) among earthquake survivors in Mianzhu County, Sichuan Province, China showed that the injured survivors tended to assess their overall quality of life as rather low (23). Study of adult patients admitted to Emergency Department (ED) in New York city reported that those with exposure to two disasters (World Trade Center disaster and American Airlines Flight 587 crash) had worse Health Related Quality of Life (HRQOL) score than those with only one disaster and those experiencing one disaster had worse score than general population (24).
The perceived acute complaints and chronic diseases which occurred more frequently in injured cohort than non-injured might possibly be related, to some extent, to the disability and quality of life of the survivors. This relation may confound the valid associations between injury and disability or between injury and quality of life. Using a multiple linear regression, we control the effect of these co-morbidities (i.e. acute complaints and chronic diseases) and found that after adjustment the injury is very significantly correlated to both the increase of disability status and the decrease of quality of life, during the whole phases of study, i.e. at baseline, at months 3 and 6 of follow-up periods.
Although from this finding, we can prove our hypothesis that the injury increases the disability status and decrease the quality of life of the survivors up to the end of follow-up period, (i.e. 10 months after disaster, given the fact that the data collection began about 4 months after the earthquake) after controlling the confounding effect of those co-morbidities, we unfortunately cannot assure that the associations are not confounded by post traumatic psychological impairment or psychosocial problem, since we did not measure this psychological or psychosocial factor (as potential determinant of disability and quality of life of the survivors).
Although we did not specifically measure the psychological or psychosocial factor, the fact from our study that perception or experience of pain, depression and anxiety were items with the lowest average scores of quality of life attributes, suggests that psychological problems were the most important factors contributing to the overall quality of life. A study in Vietnam among male veterans clearly demonstrated that PTSD (post traumatic stress disorder) was associated with functional impairment and a decreased quality of life (25). Another longitudinal study of earthquake-related PTSD in a randomly selected community sample in North China, showed that mean total score of quality of life among subjects with PTSD was significantly lower than the corresponding mean among subjects without PTSD (26). Similarly one study in Taiwan demonstrated that the quality of life of survivors of Chi-chi earthquake, with psychological problems, especially PTSD or major depression, was inferior as compared to the mentally healthy survivors (27).
Concerning conceptualization of disability and quality of life we consider that the concepts of disability and quality of life after injury are two different constructs, although they may be interrelated to each other. With regard to this relation, our finding showing negative correlation between disability and quality of life (i.e. the decrease in degree of quality of life is directly related to an increase in degree of disability), especially among the injured subjects, is consistent with the finding from Hambrick et al. (20). Borrowing the view from Hambrick et al. (20), based on their study among patients of social anxiety disorder in anxiety clinics in Philadelphia and New York, disability may bridge the gap between expression of symptoms and self-perceived quality of life.
Limitations of the study
One of the limitations of this study was that many injury cases and their important clinical profiles had not been documented in medical records, because some hospitals where the cases might have been referred to, either did not make complete standard medical records in the emergency phase of disaster or had lost their records due to the damage to some unit of the hospitals (like the severe damage to the medical record unit of the main general hospital in Padang city). Factually, until several months after the earthquake, we could only trace or find medical records of only about half (i.e. 89) injured subjects, out of total 184 injured subjects. We found from our observation on available medical records, that relevant patient information concerning demographic identity, injury history and description, case diagnosis, clinical examination and profile, medical or surgical treatment were mostly incomplete (i.e. each piece of information was missing in more than 50% medical records) and inaccurate. Specifically, for information of ‘type of injury’, among 89 available medical records of injured subjects, about 90% were missing Some information about the injury status were found based on both the records of an international humanitarian organization and interview and observation of the subjects by the research staff in the field.
Our study also faced a problem of a loss of follow-up (about 18% of the injured cohort and 14% of the non-injured cohort) which is actually quite common in prospective cohort study. Thereby a certain degree of loss to follow-up bias may have occurred. Another limitation was that interviewing subjects that were affected physically and psychologically by the earthquake with many questions about disability and quality of life were perhaps not so easy, despite our restriction (in inclusion criteria) to only include those subjects who can still communicate effectively.
Conclusions
Based on the findings, we may conclude the following points. Along with injury (which mostly affected the extremities causing bone fracture and/or dislocation), existence of co-morbidity conditions were also observed, like perceived acute symptoms (especially muscle and/or joint pain, headache and fatigue) and chronic diseases (mainly hypertension and cardiovascular diseases). Injury was found to be very significantly correlated with both increase of disability and decrease of self perceived quality of life, even after controlling the confounding effect of co-morbidities occurrence, while disability showed very significant negative correlations with quality of life in both injured and non-injured groups.
Therefore we recommend prompt and adequate treatment of all injuries in order to prevent disability and to restore the quality of life to those people injured. Further studies are certainly needed to investigate how more specific and predominant aspects of injury and impairment and other relevant determinants like mental/psychosocial problems and individual coping mechanisms may affect both the disability and future quality of life of the injured after earthquakes.
Acknowledgements
Funding for this report was made available by the European Commission under the 6th Framework Programme – Contract n° GOCE-CT-2007-036877.
We would like to thank all colleagues from the following participating institutions; Local Government of Padang city, Padang city Health Office, West Sumatra Provincial Health Office, M. Djamil General Hospital, Padang Local General Hospital, Siti Rahmah General Hospital, Yos Sudarso General Hospital and Ibnu Sina General Hospital.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Emergency and Humanitarian Action (EHA), WHO Indonesia. Earthquake in Padang, West Sumatra Province, Republic of Indonesia. Emergency Situation Report (ESR-1) Jakarta, Indonesia: WHO Indonesia; 2009. p. 4. [Google Scholar]
- 2.Emergency and Humanitarian Action (EHA), WHO Indonesia. Earthquake in Padang, West Sumatra Province, Republic of Indonesia. Emergency Situation Report (ESR-15) Jakarta, Indonesia: WHO Indonesia; 2009. pp. 1–2. [Google Scholar]
- 3.Phalkey R, Reinhardt JD, Marx M. Injury epidemiology after the 2001 Gujarat earthquake in India: a retrospective analysis of injuries treated at a rural hospital in the Kutch district immediately after the disaster. Glob Health Action. 2011;4:7196. doi: 10.3402/gha.v4i0.7196. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3144753/pdf/GHA-4-7196.pdf [cited 20 Oct 2011] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Osaki Y, Minowa M. Factors associated with earthquake deaths in the Great Hanshin-Awaji Earthquake, 1995. Am J Epidemiol. 2001;53:153–6. doi: 10.1093/aje/153.2.153. [DOI] [PubMed] [Google Scholar]
- 5.BPS West Sumatera Province. Luas Daerah, Jumlah Penduduk dan Kepadatan Penduduk Menurut Kabupaten/Kota. Available from: http://sumbar.bps.go.id/?page=artikel&fd=artikel&act=lihat&idtopik=203&idartikel=102 [cited 22 Mar 2012]
- 6.Delfebriyadi. Seismic hazard assessment of Padang City using probabilistic method. Asian Trans Eng. 2011;1:56–62. [Google Scholar]
- 7.Queensland Government. Australia. Definition. What is injury? [updated 4 April 2007] 2007 Available from: http://www.health.qld.gov.au/chipp/what_is/definitions.asp [cited 20 October 2011]
- 8.Americans with Disabilities Act of 1990, as Amended. Definition of disability. Chapter 126 – Equal opportunity for individuals with disabilities sec; 2009. 12102. [Google Scholar]
- 9.Rivany R. Depok: Faculty of Public Health, Universitas Indonesia; 2004. Development of Indonesia Health Related Quality of Life model at Cost Utility Analysis. Case study of infectious disease (TBC) and non infectious disease (hypertension) treatment (Pengembangan Model Indonesia Health Related Quality of Life pada Cost Utility Analysis. Studi Kasus Pengobatan Penyakit Infeksi (TBC) dan Non-infeksi (Hipertensi)) ; p. 255. PhD thesis dissertation. [Google Scholar]
- 10.Sami F, Ali F, Zaidi SHH, Rehman H, Ahmad T, Siddiqui MI. The October 2005 earthquake in Northern Pakistan: pattern of injuries in victims brought to the emergency relief hospital, Doraha, Mansehra. Prehosp Disaster Med. 2009;24:535–9. doi: 10.1017/s1049023x00007470. [DOI] [PubMed] [Google Scholar]
- 11.Bulut M, Fedakar R, Akkose S, Akgoz S, Ozguc H, Tokyay R. Medical experience of a university hospital in Turkey after the 1999 Marmara earthquake. Emerg Med J. 2005;22:494–8. doi: 10.1136/emj.2004.016295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petal MA. Urban disaster mitigation and preparedness: the 1999 Kocaeli earthquake. 2004. ProQuest dissertations and theses [serial online]. Available from: http://gradworks.umi.com/31/42/3142562.html [cited 19 October 2011]
- 13.Peek-Asa C, Ramirez M, Seligson H, Shoaf K. Seismic, structural, and individual factors associated with earthquake related injury. Inj Prev. 2003;9:62–6. doi: 10.1136/ip.9.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Armenian HK, Noji EK, Oganesian AP. A case-control study of injuries arising from the earthquake in Armenia, 1988. Bull World Health Organ. 1992;70:251–7. [PMC free article] [PubMed] [Google Scholar]
- 15.Guha-Sapir D, van Panhuis WG, Lagoutt J. Short communication: patterns of chronic and acute diseases after natural disasters – a study from the International Committee of the Red Cross field hospital in Banda Aceh after the 2004 Indian Ocean tsunami. Trop Med Int Health. 2007;12:1338–41. doi: 10.1111/j.1365-3156.2007.01932.x. [DOI] [PubMed] [Google Scholar]
- 16.Peek-Asa C, Kraus JF, Bourque LB, Vimalachandra D, Yu J, Abrams J. Fatal and hospitalized injuries resulting from the 1994 Northridge Earthquake. Int J Epidemiol. 1998;27:459–65. doi: 10.1093/ije/27.3.459. [DOI] [PubMed] [Google Scholar]
- 17.Roces MC, White ME, Dayrit MM, Durkin ME. Risk factors for injuries due to the 1990 earthquake in Luzon, Phillipines. Bull World Health Organ. 1992;70:509–14. [PMC free article] [PubMed] [Google Scholar]
- 18.Louis VL, Phalkey R, le Polain de Waroux O, Wind T, Komproe I, Luotomo M, et al. 2008. Sep, The health and health care system impacts of earthquakes, windstorms and floods. A report of literature review from Health Working Group, Microdis Research Project. [Google Scholar]
- 19.Tanaka H, Oda J, Iwai A, Kuwagata Y, Matsuoka T, Takaoka M, et al. Short communication: morbidity and mortality of hospitalized patients after the 1995 Hanshin-Awaji earthquake. Am J Emerg Med. 1999;17:186–91. doi: 10.1016/s0735-6757(99)90059-1. [DOI] [PubMed] [Google Scholar]
- 20.Hambrick JP, Turk CL, Heimberg RG, Schneier FR, Liebowitz MR. The experience of disability and quality of life in social anxiety disorder. Depress Anxiety. 2003;18:46–50. doi: 10.1002/da.10110. [DOI] [PubMed] [Google Scholar]
- 21.Health Research and Development Institute, Ministry of Health of Republic of Indonesia. Jakarta, Indonesia: Health Research and Development Institute, Ministry of Health of Republic of Indonesia; 2008. Laporan Riset Kesehatan Dasar (Riskesdas 2007) (Report of Baseline Health Research 2007) p. 291. xliv. [Google Scholar]
- 22.Norris FH, Galea S, Sherrieb K. Prevalence and consequences of disaster-related illness and injury from hurricane Ike. Rehabil Psychol. 2010;55:221–30. doi: 10.1037/a0020195. [DOI] [PubMed] [Google Scholar]
- 23.Tasiemski T, Nielsen S, Wilski M. Quality of life in people with spinal cord injury – earthquake survivors from Sichuan Province in China. Asia Pac Disabil Rehabil J. 2010;21:28–36. [Google Scholar]
- 24.Fernandez WG, Galea S, Miller J, Ahern J, Chiang W, Kennedy EL, et al. Health status among emergency department patients approximately one year after consecutive disasters in New York City. Acad Emerg Med. 2005;12:958–64. doi: 10.1197/j.aem.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 25.Zatzick DF, Marmar CR, Weiss DS, Browner WS, Metzler TJ, Golding JM, et al. Posttraumatic stress disorder and functioning and quality of life outcomes in a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1997;154:1690–5. doi: 10.1176/ajp.154.12.1690. [DOI] [PubMed] [Google Scholar]
- 26.Wang X, Gao L, Shinfuku N, Zhang H, Zhao C, Shen Y. Longitudinal study of earthquake-related PTSD in a randomly selected community sample in North China. Am J Psychiatry. 2000;157:1260–6. doi: 10.1176/appi.ajp.157.8.1260. [DOI] [PubMed] [Google Scholar]
- 27.Wu HC, Chou P, Chou FHC, Su CY, Tsai KY, Yang WCO, et al. Survey of quality of life and related risk factors for a Taiwanese village population 3 years post-earthquake. Aust N Z J Psychiatry. 2006;40:355–61. doi: 10.1080/j.1440-1614.2006.01802.x. [DOI] [PubMed] [Google Scholar]