Abstract
Background
Little existing data describe which medical professionals and which medical studies are used to assess sport-related concussions in high school athletes.
Purpose
To describe the medical providers and medical studies used when assessing sport-related concussions. To determine the effects of medical provider type on timing of return to play, frequency of imaging, and frequency of neuropsychological testing.
Study Design
Descriptive epidemiology study.
Methods
All concussions recorded by the High School Reporting Information Online (HS RIO) injury surveillance system during the 2009 to 2010 academic year were included. χ2 analyses were conducted for categorical variables. Fisher exact test was used for nonparametric data. Logistic regression analyses were used when adjusting for potential confounders. Statistical significance was considered for P < .05.
Results
The HS RIO recorded 1056 sport-related concussions, representing 14.6% of all injuries. Most (94.4%) concussions were assessed by athletic trainers (ATs), 58.8% by a primary care physician. Few concussions were managed by specialists. The assessment of 21.2% included computed tomography. Computerized neuropsychological testing was used for 41.2%. For 50.1%, a physician decided when to return the athlete to play; for 46.2%, the decision was made by an AT. After adjusting for potential confounders, no associations between timing of return to play and the type of provider (physician vs AT) deciding to return the athlete to play were found.
Conclusion
Concussions account for nearly 15% of all sport-related injuries in high school athletes. The timing of return to play after a sport-related concussion is similar regardless of whether the decision to return the athlete to play is made by a physician or an AT. When a medical doctor is involved, most concussions are assessed by primary care physicians as opposed to subspecialists. Computed tomography is obtained during the assessment of 1 of every 5 concussions occurring in high school athletes.
Keywords: athletic injuries, athletic trainer, medical personnel, computed tomography, neuropsychological testing
There has been a recent flurry of interest in the incidence, assessment, and management of sport-related concussions. This is a likely result of several key medical and scientific findings. First, cognitive function is temporarily diminished after sport-related concussions and can remain diminished even after athletes report resolution of their symptoms.4,10,35 Second, athletes who return to play before full resolution of their symptoms are at risk for catastrophic outcomes such as second-impact syndrome.6,30 Third, athletes who sustain multiple concussive injuries or perhaps multiple subconcussive blows to the head during their athletic careers may be at risk for long-term dementia and other potential problems such as chronic traumatic encephalopathy.7,20
As a result of this recent interest, several major international conferences on concussion in sports have been held, generating consensus statements and updated guidelines to assist clinicians in the assessment and management of sport-related concussions.1,18,19 While these updated guidelines have been distributed throughout the sports medicine literature, they have not been as widely published in journals more commonly read by internists, pediatricians, and primary care practitioners.
There have been very little data published describing how and by whom sport-related concussions are diagnosed and managed. Given their presence at professional and collegiate athletic events, team physicians, certified athletic trainers (ATs), or perhaps emergency medical technicians (EMTs) might be expected to assess and manage most of these injuries, at least acutely. However, at the high school level, the majority of schools in the United States (US) do not employ ATs.36 While in some areas, EMTs may be routinely on site for high school football competitions, we believe team physicians are a rarity. It is likely that physicians and EMTs are even less frequently present at non-football sporting events. Thus, it is possible that primary care physicians are frequently diagnosing and managing concussions sustained by adolescent athletes. However, the extent of physician involvement in caring for athletes after a sport-related concussion is largely unknown. Results of a survey of ATs published in 2001 suggested that team physicians were most commonly responsible for making return-to-play decisions, followed by ATs.12 However, this has not been confirmed by prospective data collection. Additionally, we are aware of no published data describing how frequently medical providers are on site when a sport-related concussion occurs in the high school setting, which medical providers are assessing these sport-related concussions, which methods are being utilized to assess sport-related concussions, and which medical providers make the decision to return athletes to play. Similarly, there are scant data describing how frequently neuropsychological testing is used when assessing sport-related concussions when making return-to-play decisions.21 Recently, new legislation specifying which types of medical personnel should assess and manage sport-related concussions is being passed.13 Knowledge of the current practices could advise medical groups and law makers when developing these regulations.
Using a large national sample of US high school athletes, we conducted a prospective cohort study to describe the type of medical personnel and the type of medical assessments being used to manage sport-related concussions, including imaging and computerized neuropsychological testing.
MATERIALS AND METHODS
During the 2009 to 2010 academic year, 192 US high schools reported data for athletes participating in 20 sports (boys: baseball, basketball, football, ice hockey, lacrosse, soccer, swimming and diving, track and field, volleyball, and wrestling; and girls: basketball, field hockey, gymnastics, lacrosse, soccer, softball, swimming and diving, track and field, volleyball, and cheerleading) using the High School Reporting Information Online (HS RIO) injury surveillance system. The HS RIO has been described elsewhere in detail.28,32,33 In brief, high schools with at least one AT affiliated with the National Athletic Trainer’s Association who had a valid e-mail address were invited to participate. Athletic trainers from participating high schools received a small financial incentive to log onto the HS RIO Web site weekly throughout the academic year to report injury incidence and athletic exposure (AE) data. For each injury, ATs completed a detailed injury report form providing information on the injured athlete (eg, age, position played), the injury itself (eg, body site injured, diagnosis), and the injury event (eg, mechanism, activity at the time of injury). The number of schools reporting for each sport varied from 158 schools reporting girls’ basketball data to 27 schools reporting boys’ volleyball data. However, only boys’ volleyball and girls’ gymnastics had fewer than 50 schools reporting data; 12 of the 20 sports had over 100 schools reporting data. Injuries are defined as those resulting from participation in an organized high school athletic practice or competition and requiring medical attention from an AT. The surveillance system is designed to capture all time-loss injuries as well as any fracture, any concussion, and any dental injury, regardless of whether it resulted in restriction of the student athlete’s participation. This article focuses on concussions.
All concussions that (1) occurred during an organized high school athletic practice or competition, (2) resulted in the athlete receiving care from a medical provider, and (3) were brought to the attention of the AT were recorded. An AE was defined as one athlete participating in one organized high school athletic practice or competition, regardless of the amount of time played. All statistical analyses were performed using SPSS software (SPSS version 16.0, SPSS Inc, Chicago, Illinois). χ2 analyses were performed for all categorical variables. Fisher exact test was used for comparisons among specialties, registered nurses, and physician assistants, given the relatively low numbers of their involvement. Logistic regression analyses were used to assess for associations between the dependent variable, the timing of return to play, and 2 independent variables: the type of provider returning the athlete to play and the duration of symptoms. The timing of return to play was collected as a categorical variable: 1 to 2 days, 3 to 6 days, 7 to 9 days, 10 to 21 days, and 22 days or more. Statistical significance was considered for P < .05.
RESULTS
Description of Concussions
Over the course of the 2009 to 2010 academic year, HS RIO recorded 7257 sport-related injuries, of which 1056 (14.6%) were concussions. Concussion accounted for 90.0% of the 1173 injuries recorded to the head and face, followed distantly by lacerations (3.8%) and contusions (2.8%). Male athletes sustained 75.7% of all recorded concussions. Most concussions (88.6%) were new injuries, while 11.4% were recurrent. Of recurrent concussions, 37.0% recurred within the 2009 to 2010 academic year, while for 61.3%, the index concussion occurred before the 2009 to 2010 academic year. Data regarding the timing of prior concussions were unavailable for 1.7% of recurrent injuries.
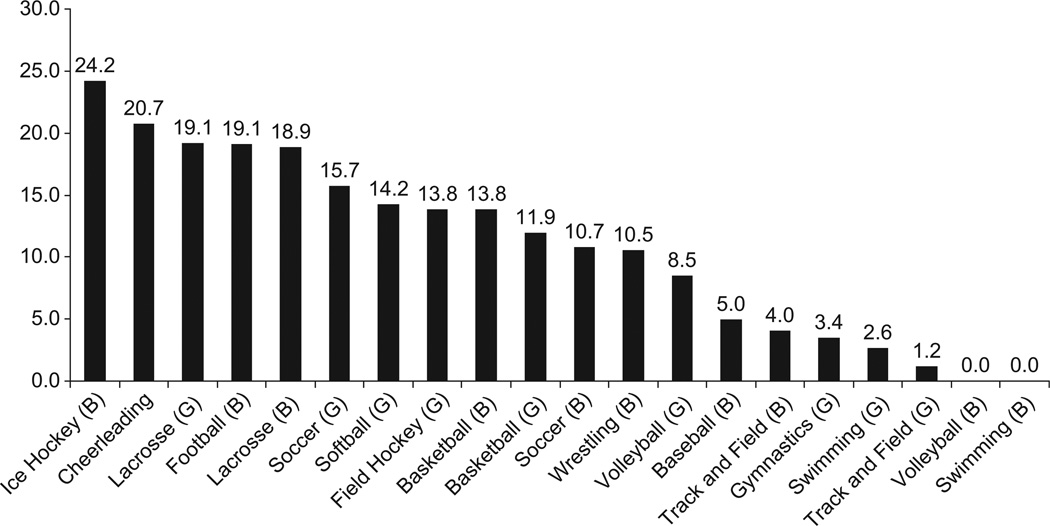
As expected, rates of concussion per AE were highest for collision sports, such as football, boys’ ice hockey, and boys’ lacrosse (Table 1). Most of the concussions recorded were sustained by football players (47.2%). Concussions accounted for a higher percentage of total injuries in boys’ ice hockey (24.2%) than in any other sport (Figure 1).
TABLE 1.
Number of Sport-Related Concussions per 100 000 Athletic Exposuresa
| Sport | Concussions per 100 000 Athletic Exposures, n (95% CI) |
|---|---|
| Boys’ football | 76.8 (74.1–79.5) |
| Boys’ ice hockey | 61.9 (59.4–64.4) |
| Boys’ lacrosse | 46.6 (44.5–48.7) |
| Girls’ soccer | 33.0 (31.2–34.8) |
| Girls’ lacrosse | 31.0 (29.3–32.7) |
| Girls’ field hockey | 24.9 (23.3–26.5) |
| Boys’ wrestling | 23.9 (22.4–25.4) |
| Boys’ basketball | 21.2 (19.8–22.6) |
| Boys’ soccer | 19.2 (17.8–20.6) |
| Girls’ basketball | 18.6 (17.2–20.0) |
| Girls’ softball | 16.3 (15.0–17.6) |
| Cheerleading | 11.5 (10.4–12.6) |
| Girls’ volleyball | 8.6 (7.7–9.5) |
| Girls’ gymnastics | 8.2 (7.3–9.1) |
| Boys’ baseball | 4.6 (3.9–5.3) |
| Boys’ track and field | 3.5 (2.9–4.1) |
| Girls’ track and field | 1.4 (1.2–1.6) |
| Girls’ swimming | 1.0 (0.8–1.2) |
| Boys’ volleyball | 0.0 (N/A) |
| Boys’ swimming | 0.0 (N/A) |
CI, confidence interval; N/A, not applicable.
Figure 1.
The percentage of total injuries represented by concussion. B, boys; G, girls.
Concussions were fairly evenly distributed among the grades, with 25.8% (95% confidence interval [CI], 23.1%–28.5%) sustained by freshmen, 25.1% (95% CI, 22.5%–27.7%) by sophomores, 26.4% (95% CI, 23.7%–29.1%) by juniors, and 22.7% (95% CI, 20.1%–25.3%) by seniors. Most (53.2%) concussions were sustained during varsity competitions, with 31.4% occurring in junior varsity competitions, 11.4% during freshmen competitions, and 3.9% during combined events.
The most commonly reported symptoms of concussion were headache (94.3%), dizziness/unsteadiness (75.5%), difficulty concentrating (53.9%), confusion/disorientation (44.0%), and visual disturbance/sensitivity to light (34.4%). Loss of consciousness was rare, associated with only 4.2% of all concussions. Amnesia was recorded with 21.6% of concussions.
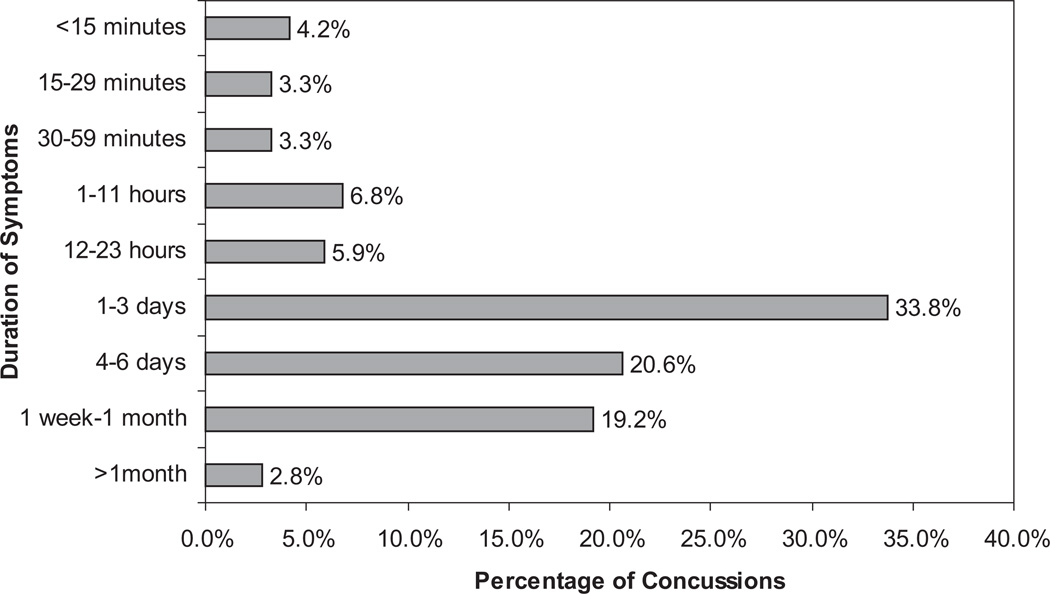
Nearly one fourth of concussed athletes (23.5%) had resolution of their symptoms within 24 hours of the injury. Of all athletes concussed, most (77.9%) had resolution of their symptoms within 7 days of injury, while 19.2% of concussed athletes had symptoms that lasted longer than 1 week but resolved within 1 month. Only 2.8% of concussed athletes had symptoms that lasted longer than 1 month (Figure 2). Female athletes appeared more likely to have symptoms lasting more than 7 days from the time of injury (26.4% vs 19.6%, P = .05).
Figure 2.
Duration of symptoms after sport-related concussions.
Assessment and Management of Concussions
A medical professional was on site at the time of injury for 92.7% of concussions. Athletic trainers were on site for at least 70.0% of concussions. Physicians were on site at the time of 7.7% of concussions. A medical professional was more likely to be on site if a concussion occurred during football as opposed to other sports (96.1% vs 89.6%, P < .001). Medical professionals were more often on site at the time of concussions that occurred during competition or performance as opposed to during practice or training sessions (94.7% vs 89.1%, P = .001). When sports played by both boys and girls were analyzed, there was no difference in the likelihood of a medical professional being on site at the time of injury between boys’ sports and girls’ sports. There were no significant associations between having a medical professional on site at the time of injury and duration of symptoms or timing of return to play.
Of all recorded concussions, 94.4% were assessed by ATs; 58.8% were assessed by a primary care physician. Table 2 shows the percentages of concussions assessed by various types of medical personnel. Most concussions (62.7%) were assessed by more than one medical professional. Of those concussed athletes seen by more than one medical provider, 87.4% were assessed by an AT and a primary care physician and 7.6% by an AT and an orthopaedic surgeon. Of those injuries assessed by only one type of medical professional, 88.7% were assessed by an AT; 9.7% were assessed by a primary care physician.
TABLE 2.
Percentage of Concussions Assessed by a Given Medical Professionala
| Medical Personnel Who Assessed Concussions |
Percentage of Concussions Assessed |
|---|---|
| Certified athletic trainer | 94.4 |
| General physician | 58.8 |
| Orthopaedic physician | 4.7 |
| Nurse practitioner | 2.4 |
| Neurologist | 2.1 |
| Sports medicine physician | 1.7 |
| Emergency medicine physician | 1.6 |
| Neuropsychologist | 1.1 |
| Physician assistant | 1.1 |
| Registered nurse | 0.7 |
| Neurosurgeon | 0.5 |
| Emergency medical technician | 0.4 |
Percentages do not equal 100, as athletes may have been seen by more than one type of provider. Although not included in the table, a dentist, a chiropractor, and a coach each assessed one (0.1%) concussion.
The assessment of 21.2% of concussions included computed tomography (CT), and 3.0% included magnetic resonance imaging (MRI). Two athletes underwent electroencephalography as part of their assessment. Computerized neuropsychological testing was used in the management of 41.2% of all recorded concussions.
When the decision to return an athlete to play was made by a physician as opposed to an AT, the athlete was more likely to undergo computerized neuropsychological testing (52.6% vs 35.7%, P < .001), CT (30.0% vs 10.9%, P < .001), and MRI (5.5% vs 0.6%, P < .001). Concussed athletes were more likely to undergo CT if assessed by emergency medicine physicians (75.0% vs 20.2%, P < .001) and neurologists (72.7% vs 19.9%, P < .001) than when assessed without these specialists. There were no significant differences in the frequency of CT when athletes were assessed by sports medicine physicians as opposed to those athletes not assessed by sports medicine physicians. There were no differences in MRI rates regardless of which specialists were involved in the assessment.
Decisions to return athletes to play were most commonly made by a physician (50.1%) or an AT (46.2%). However, at least 2.5% of athletes were returned to play by nonmedical personnel, such as coaches. Athletes who had symptoms lasting longer than a week were more likely to have a physician decide when to return them to play than those athletes with symptoms of shorter duration (67.0% vs 48.0%, P < .001).
Logistic regression analyses were performed to assess whether the type of provider who returned the athlete to play (AT vs physician) affected the timing of return to play. After adjusting for age of athlete, sport played by athlete, gender of athlete, and duration of concussion symptoms, no associations between timing of return to play and the type of provider deciding to return the athlete to play were found. Most athletes (54.2%) were returned to play within 10 days of their injury. The timing of return to play is shown in Table 3.
TABLE 3.
Percentage of Athletes Who Returned to Play at Given Time Points
| Timing of Return to Play | Percentage of All Concussed Athletes |
Percentage of Athletes Returned to Play by Athletic Trainer |
Percentage of Athletes Returned to Play by Physician |
|---|---|---|---|
| 1–2 d | 4.7 | 6.4 | 2.5 |
| 3–6 d | 20.7 | 25.5 | 14.9 |
| 7–9 d | 30.0 | 31.9 | 28.7 |
| 10–21 d | 34.5 | 31.1 | 39.3 |
| >22 d | 4.5 | 2.5 | 6.7 |
| Medical disqualification for season | 5.4 | 2.7 | 7.1 |
| Medical disqualification for career | 0.3 | 0.0 | 0.7 |
There were no significant associations between the timing of return to play after a sport-related concussion and level of competition (varsity, junior varsity, or freshmen). Gender was not significantly associated with (1) the timing of return to play, (2) whether the athlete was returned to play by a medical professional, or (3) which medical professional (AT or physician) decided to return the athlete to play.
DISCUSSION
We found that concussion accounts for nearly 15% of all sport-related injuries in US high schools. Our data suggest that when a high school athlete attending a school that employs an AT sustains a concussion, there is usually a medical professional on site at the time of injury. This is most often an AT. Interestingly, once we adjusted for potential confounders, there was no significant association between the type of medical provider who cleared the athlete to return to play and the timing of return to play. This suggests that ATs and physicians use similar return-to-play intervals when managing athletes who have sustained sport-related concussions.
Approximately 60% of concussions in our study were assessed by primary care physicians as opposed to sports medicine subspecialists. This is significant, as many primary care physicians may not have adequate resources or understanding of current concussion management practices. A survey by Pleacher and Dexter24 revealed that many primary care providers are either unaware of current management guidelines or find the guidelines too confusing to put into practice. That same study revealed that only 16% had reliable access to neuropsychological testing within 1 week of an injury.24 As our data suggest that many primary care physicians are called upon to care for concussive brain injuries, efforts to support them in this regard could have a major influence on management. Any changes in the recommendations on managing concussed athletes should be communicated directly to pediatricians, internists, and family practitioners. This could be accomplished by publishing sport-related concussion guidelines in medical journals that target these specialties and by increasing the number of sport-related concussion presentations at national conferences that target these specialties. Furthermore, our results show that orthopaedic surgeons and midlevel providers, such as nurse practitioners and physician assistants, are caring for an additional 8.2% of concussions. Targeting these clinicians, in addition to primary care physicians, when communicating concussion management recommendations may also result in significant improvements in care.
Nearly 1 in 5 concussed athletes received CT as part of their evaluation. Given the recent concern over radiation exposure in younger patients,2,3,17,22 and the relatively low rates of structural intracranial injury resulting from high school sports,14,25 this may represent an area for future improvement. Three percent of concussions were evaluated with MRI. As there is no radiation associated with this imaging modality, and MRI is superior in detecting traumatic lesions,23 this might be a more favorable type of imaging, when indicated, for assessing traumatic sport-related brain injuries, especially after the acute period.26 Athletes assessed by physicians were more likely to undergo neuroimaging and computerized neuropsychological testing than those athletes not assessed by a physician. This likely reflects, in part, confounding by indication: more severe injuries were more likely to be referred to a physician and more likely to warrant further testing. This is consistent with our findings, as athletes in our study with symptoms lasting longer than 7 days were more likely to have a physician decide when to return them to play.
Decisions to return the athlete to play were most often made by physicians and ATs. However, at least 2.5% of these decisions were made by nonmedical personnel. This number is likely higher for schools that do not employ ATs. The National Athletic Trainer’s Association reports that only 42% of high schools in the United States use the services of an AT.36 As returning to play before symptom resolution can be associated with poor outcomes, such as second-impact syndrome,6,30 efforts should be made to decrease the number of athletes being returned to play by nonmedical professionals. To that end, recent legislation in many states now requires that athletes suspected of sustaining a concussion be removed from play and held out until cleared by a medical professional.13 Some states require that coaches and other school personnel who work with athletes undergo specific concussion training.13 At the time of this writing, 28 states currently have specific concussion laws.29
We have previously reported the percentage of concussions associated with various symptoms, the duration of concussion symptoms, the timing of return to play, and the frequency of computerized neuropsychological testing in the management of sport-related concussions.21 The distribution of reported symptoms, distribution by year in school, and timing of return to play were similar to our previous report,21 attesting to the reliability of the HS RIO surveillance system. Computerized neuropsychological testing was used in the evaluation of 41.2% of all concussions recorded, representing an increase of 15.5% from the 2008 to 2009 academic year.21 Given its rapid rise in usage in the high school setting, future research should focus on the use of computerized neuropsychological testing for the management of concussions in sports.
Interestingly, female athletes were more likely than male athletes to have symptoms that persisted longer than 7 days. This adds to previous literature that suggests more significant symptoms and poorer neuropsychological assessments in female athletes after sustaining sport-related concussions.5,8,9,11
Several prior studies have suggested that men’s ice hockey carries the highest risk of sport-related concussion.15,16,34 In a 16-year study of college athletes, Hootman et al15 reported that men’s ice hockey players sustained more concussions per 1000 AEs than football players. Similar conclusions were reached by other investigators.16,34 Our analyses, however, demonstrate that although concussions represent a higher proportion of all injuries sustained by boys’ ice hockey players than other sports, American football had the highest rate of sport-related concussions per 100 000 AEs. This discrepancy may result from the increased attention focused on concussions in football.31 Such attention may have resulted in an increase in the diagnosis of concussion, as has recently been reported in the National Football League.27
All schools included in the HS RIO have an AT who cares for their athletes. Therefore, we would not recommend generalizing our findings to high schools that do not employ ATs. In addition, concussion can be a difficult injury to diagnose, as there is no visible structural damage. Therefore, there may have been athletes who sustained a sport-related concussion but did not report it to the AT. While all concussions, dental injuries, and fractures brought to the attention of the AT were recorded, other injuries such as contusions, strains, and sprains were only recorded if they resulted in time lost from play. Thus, the percentage of all sport-related injuries accounted for by concussion would be smaller if minor injuries that did not result in time lost from play were included. Despite these limitations, this study reports findings from the largest national sample of athletes sustaining concussions in the US high school setting.
CONCLUSION
Concussions account for nearly 15% of all sport-related injuries in high school athletes. In US high schools that employ an AT, a medical professional is usually on site when a sport-related concussion occurs. The timing of return to play after a sport-related concussion is similar regardless of whether the decision to return the athlete to play is made by a physician or an AT. When a medical doctor is involved, most concussions are assessed by primary care physicians as opposed to subspecialists. Computed tomography is obtained during the assessment of 1 of every 5 concussions occurring in high school athletes.
Acknowledgments
One or more of the authors has declared the following potential conflict of interest or source of funding: The content of this work was funded in part by the Centers for Disease Control and Prevention (CDC) grants #R49/CE000674-01 and #R49/CE001172-01. The content of this work is solely the responsibility of the authors and does not necessarily represent the official views of the CDC. The authors also acknowledge the generous research funding contributions of the National Federation of State High School Associations (NFHS), the National Operating Committee on Standards for Athletic Equipment (NOCSAE), EyeBlack, and Don-Joy Orthotics. This study was supported by the National Institutes of Health (NIH) T32 Award to Dr Meehan (T32 HD040128-06A1).
REFERENCES
- 1.Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001: recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002;36(1):6–10. doi: 10.1136/bjsm.36.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 3.Brody AS, Frush DP, Huda W, Brent RL. Radiation risk to children from computed tomography. Pediatrics. 2007;120(3):677–682. doi: 10.1542/peds.2007-1910. [DOI] [PubMed] [Google Scholar]
- 4.Broglio SP, Macciocchi SN, Ferrara MS. Neurocognitive performance of concussed athletes when symptom free. J Athl Train. 2007;42(4):504–508. [PMC free article] [PubMed] [Google Scholar]
- 5.Broshek DK, Kaushik T, Freeman JR, Erlanger D, Webbe F, Barth JT. Sex differences in outcome following sports-related concussion. J Neurosurg. 2005;102(5):856–863. doi: 10.3171/jns.2005.102.5.0856. [DOI] [PubMed] [Google Scholar]
- 6.Cantu R. Second impact syndrome: a risk in any contact sport. Physician and Sportsmedicine. 1995;23(6):27. doi: 10.1080/00913847.1995.11947799. [DOI] [PubMed] [Google Scholar]
- 7.Cantu RC. Chronic traumatic encephalopathy in the National Football League. Neurosurgery. 2007;61(2):223–225. doi: 10.1227/01.NEU.0000255514.73967.90. [DOI] [PubMed] [Google Scholar]
- 8.Covassin T, Schatz P, Swanik CB. Sex differences in neuropsychological function and post-concussion symptoms of concussed collegiate athletes. Neurosurgery. 2007;61(2):345–350. doi: 10.1227/01.NEU.0000279972.95060.CB. discussion 350–351. [DOI] [PubMed] [Google Scholar]
- 9.Covassin T, Swanik CB, Sachs ML. Sex differences and the incidence of concussions among collegiate athletes. J Athl Train. 2003;38(3):238–244. [PMC free article] [PubMed] [Google Scholar]
- 10.Erlanger D, Saliba E, Barth J, Almquist J, Webright W, Freeman J. Monitoring resolution of postconcussion symptoms in athletes: preliminary results of a web-based neuropsychological test protocol. J Athl Train. 2001;36(3):280–287. [PMC free article] [PubMed] [Google Scholar]
- 11.Farace E, Alves WM. Do women fare worse? A metaanalysis of gender differences in outcome after traumatic brain injury. Neurosurg Focus. 2000;8(1):e6. doi: 10.3171/foc.2000.8.1.152. [DOI] [PubMed] [Google Scholar]
- 12.Ferrara MS, McCrea M, Peterson CL, Guskiewicz KM. A survey of practice patterns in concussion assessment and management. J Athl Train. 2001;36(2):145–149. [PMC free article] [PubMed] [Google Scholar]
- 13.Foreman M. Sidelined for safety: new laws keep student athletes with concussions benched. State Legis. 2010;36(6):28–30. [PubMed] [Google Scholar]
- 14.Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495–503. [PMC free article] [PubMed] [Google Scholar]
- 15.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 16.Koh JO, Cassidy JD, Watkinson EJ. Incidence of concussion in contact sports: a systematic review of the evidence. Brain Inj. 2003;17(10):901–917. doi: 10.1080/0269905031000088869. [DOI] [PubMed] [Google Scholar]
- 17.Mannix R, Bourgeois FT, Schutzman SA, Bernstein A, Lee LK. Neuroimaging for pediatric head trauma: do patient and hospital characteristics influence who gets imaged? Acad Emerg Med. 2010;17(7):694–700. doi: 10.1111/j.1553-2712.2010.00797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Br J Sports Med. 2005;39(4):196–204. doi: 10.1136/bjsm.2005.018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. J Sci Med Sport. 2009;12(3):340–351. doi: 10.1016/j.jsams.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 20.McKee AC, Cantu RC, Nowinski CJ, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68(7):709–735. doi: 10.1097/NEN.0b013e3181a9d503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meehan WP, 3rd, d’Hemecourt P, Comstock RD. High school concussions in the 2008–2009 academic year: mechanism, symptoms, and management. Am J Sports Med. 2010;38(12):2405–2409. doi: 10.1177/0363546510376737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meehan WP, 3rd, Mannix R. Pediatric concussions in United States emergency departments in the years 2002 to 2006. J Pediatr. 2010;157(6):889–893. doi: 10.1016/j.jpeds.2010.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mendez CV, Hurley RA, Lassonde M, Zhang L, Taber KH. Mild traumatic brain injury: neuroimaging of sports-related concussion. J Neuropsychiatry Clin Neurosci. 2005;17(3):297–303. doi: 10.1176/jnp.17.3.297. [DOI] [PubMed] [Google Scholar]
- 24.Pleacher MD, Dexter WW. Concussion management by primary care providers. Br J Sports Med. 2006;40(1):e2. doi: 10.1136/bjsm.2005.019067. discussion e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA. 1999;282(10):958–963. doi: 10.1001/jama.282.10.958. [DOI] [PubMed] [Google Scholar]
- 26.Prabhu SP. The role of neuroimaging in sport-related concussion. Clin Sports Med. 2011;30(1):103–114. doi: 10.1016/j.csm.2010.09.003. ix. [DOI] [PubMed] [Google Scholar]
- 27.Press A. Concussions reported in NFL up 21 percent from last season. NFL.com News. 2010 Dec 13; [Google Scholar]
- 28.Rechel JA, Yard EE, Comstock RD. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197–204. doi: 10.4085/1062-6050-43.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rickerson J. Concussion laws: 2010. [Accessed July 22, 2011]; Available at: http://sportsconcussions.org/laws.html. [Google Scholar]
- 30.Saunders RL, Harbaugh RE. The second impact in catastrophic contact-sports head trauma. JAMA. 1984;252(4):538–539. [PubMed] [Google Scholar]
- 31.Schwarz A. N.F.L. acknowledges long-term concussion effects. New York Times. 2009 Dec 20; [Google Scholar]
- 32.Shankar PR, Fields SK, Collins CL, Dick RW, Comstock RD. Epidemiology of high school and collegiate football injuries in the United States, 2005–2006. Am J Sports Med. 2007;35(8):1295–1303. doi: 10.1177/0363546507299745. [DOI] [PubMed] [Google Scholar]
- 33.Sports-related injuries among high school athletes: United States 2005–06 school year. MMWR Morb Mortal Wkly Rep. 2006;55(38):1037–1040. [PubMed] [Google Scholar]
- 34.Tommasone BA, Valovich McLeod TC. Contact sport concussion incidence. J Athl Train. 2006;41(4):470–472. [PMC free article] [PubMed] [Google Scholar]
- 35.Van Kampen DA, Lovell MR, Pardini JE, Collins MW, Fu FH. The “value added” of neurocognitive testing after sports-related concussion. Am J Sports Med. 2006;34(10):1630–1635. doi: 10.1177/0363546506288677. [DOI] [PubMed] [Google Scholar]
- 36.Waxenberg R, Satloff E. Athletic trainers fill a necessary niche in secondary schools. National Athletic Trainer’s Association: 2009. [Accessed July 22, 2011]; Available at: http://www.nata.org/NR031209. [Google Scholar]