Abstract
Purpose
High-dose radiotherapy can cause contracture of the anophthalmic socket, but the incidence of this complication in patients with enucleation for uveal melanoma has not previously been reported. We reviewed the surgical management and outcomes in terms of successful prosthesis wear in patients with severe contracture of the anophthalmic socket treated with high-dose radiotherapy for high-risk uveal melanoma and estimated the relative risk of this complication.
Methods
The medical records of all consecutive patients enrolled in a prospective uveal-melanoma tissue-banking protocol at our institution who underwent enucleation between January 2003 and December 2010 were reviewed. Patients who underwent adjuvant radiotherapy of the enucleated socket were further studied.
Results
Of the 68 patients enrolled in the prospective tissue banking protocol, 12 had high-risk histologic features (e.g., extrascleral spread or vortex vein invasion) and were treated with 60 Gy of external-beam radiotherapy after enucleation. Five of these patients (41.7%) experienced severe socket contracture precluding prosthesis wear. The median time to onset of contracture following completion of radiotherapy was 20 months. Three patients underwent surgery, which entailed scar tissue release, oral mucous membrane grafting, and socket reconstruction; 2 patients declined surgery. All 3 patients who had surgery experienced significant improvement of socket contracture that enabled patients to wear a prosthesis again.
Conclusion
High-dose radiotherapy after enucleation in patients with uveal melanoma caused severe socket contracture and inability to wear a prosthesis in approximately 40% of patients. Surgical repair of the contracted socket using oral mucous membrane grafting can allow resumption of prosthesis wear.
INTRODUCTION
The indications for irradiation of the anophthalmic socket after enucleation in patients with uveal melanoma with high-risk histologic features are controversial. Some authorities advocate observation while others advocate post-operative radiation therapy to decrease the risk of local-regional recurrence. Most authorities agree that irradiation of the anophthalmic socket does not affect the risk of distant metastasis from uveal melanoma. High-dose irradiation of the anophthalmic socket after enucleation can lead to severe socket contracture and render patients unable to wear a prosthesis.1–5
Reports have been published on the surgical management of acquired contracted sockets in patients with retinoblastoma.6,7 However, we were unable to find a report on the incidence of anophthalmic socket contracture secondary to radiation therapy after enucleation for uveal melanoma or the surgical outcomes after reconstructive surgery for a contracted socket in this situation.
We herein report 5 patients with uveal melanoma with high-risk histologic features noted on the enucleation specimen who had severe socket contracture and inability to retain an ocular prosthesis after radiation therapy. The surgical management and outcomes in terms of successful prosthesis wear were retrospectively reviewed in each case. We further report on the relative risk of severe socket contracture as a result of post-operative radiation therapy.
METHODS
The medical records of all consecutive patients enrolled in a prospective tissue banking protocol for uveal melanoma who underwent enucleation between January 2003 and February 2011 were reviewed. Patients who underwent radiation therapy after enucleation because of high-risk histologic features were identified and further studied. In the patients who underwent radiation therapy, the following main outcome measures were examined: type of high-risk histologic feature (e.g.extrascleral spread or tumor invasion of the vortex vein), the total dose and fractionation of radiation, occurrence of socket contracture, timing of socket contracture in relation to radiation therapy, severity of socket contracture, surgical treatment for socket contracture, and ability to retain an ocular prosthesis after reconstructive surgery for contracted socket. For each patient who underwent radiation therapy, the status at last contact with respect to local recurrence, distant metastasis, time to recurrence, and death due to disease was also recorded. This retrospective chart review was approved by the Institutional Review Board (IRB) at M. D. Anderson and the IRB waived the requirement for informed consent.
RESULTS
Sixty-eight patients were enrolled in the prospective tissue banking protocol during the study period. Of these, 12 patients received external beam radiation therapy following standard enucleation. No patients had received prior plaque therapy. The indications for radiation therapy were recurrence in 1 patient (8%) (a patient who underwent enucleation for a localized uveal melanoma and developed orbital melanoma 6 months later); microscopic extrascleral spread in 6 patients (50%); tumor invasion of the vortex vein in 2 patients (17%); both extrascleral spread and tumor invasion of the vortex vein in 2 patients (17%); and spread to the trabecular meshwork in 1 patient (8%). In all 12 patients, external beam radiation therapy was standard fractionation to a total dose of 60 Gy in 30 fractions of 2 Gy per fraction delivered daily over 6 weeks.
Using the grading system for acquired socket contracture proposed by Krishna3 in 1980 (Table 1), 5 of the 12 patients (42%) had severe contracture (grade 4), with loss of all fornices and reduction of the palpebral aperture in the horizontal and vertical dimensions (Figure 1). One patient was lost to followed up elsewhere and died 10 months following completion of radiation therapy with no information available regarding the status of his socket. 3 other patients died soon after radiation therapy and had no information about socket contracture in their medical records. In each of the 5 patients with severe socket contracture, the contracture occurred gradually over a few months, during which time a smaller prosthesis had to be made by an ocularist (Figure 2), and the patient was eventually unable to retain even the smallest possible prosthesis. Inability to wear a prosthesis occurred at a median time of 20 months (range, 10–34 months) after completion of radiation therapy. All 5 patients were offered reconstructive surgery to repair the contracted socket. Two patients declined surgery, while the remaining 3 patients underwent reconstructive surgery performed by the same surgeon (BE) as outlined in the next section.
TABLE 1.
Krishna’s five grades of socket contracture3
| Grade | Socket description |
|---|---|
| 0 | Socket lined by healthy epithelia and has deep and well-formed fornices |
| I | Shallowing of the lower fornix |
| II | Loss of upper and lower fornices |
| III | Loss of upper, lower, medial, and lateral fornices |
| IV | Loss of all fornices with reduction of palpebral aperture in horizontal and vertical dimensions |
| V | Recurrence of socket contracture after repeated trial of reconstruction |
Figure 1.

Patient with severe contracture of the socket with loss of palpebral aperture due to significant scarring on the left side.
Figure 2.
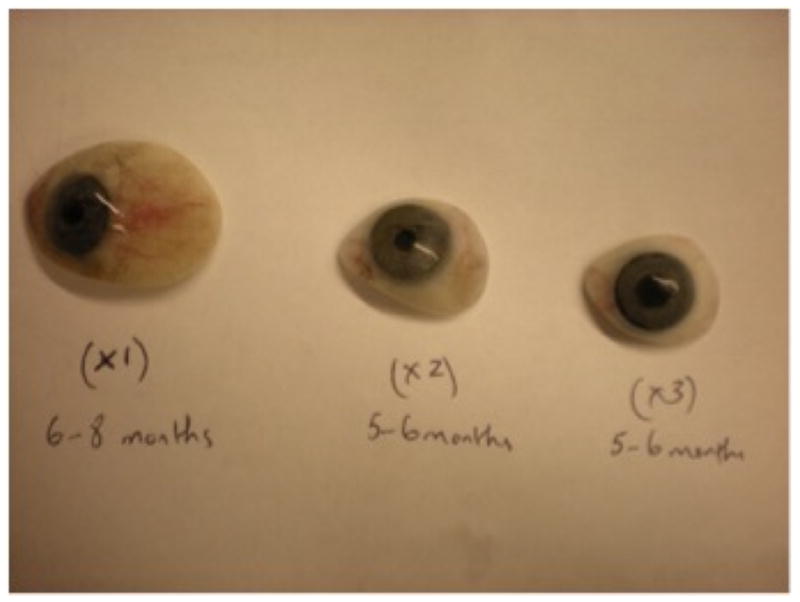
Progressively smaller prostheses required in a patient with socket contracture. The contracture occurred over a span of 16–20 months, at the end of which the patient was unable to retain the prosthesis. The prosthesis at left was worn for the first 6 to 8 months after radiation therapy, the prosthesis in the middle was worn for the next 5–6 months, and the prosthesis at right was worn for the next 5–6 months, after which the patient was no longer able to retain even a small prosthesis.
Surgical Technique for Reconstruction of Contracted Irradiated Sockets
Reconstruction of the contracted socket in each patient was done under general endotracheal anesthesia.
Traction sutures (4-0 silk) were placed through the upper and lower eyelid margin, and cicatricial tissue in the fornix and the upper and lower eyelids was released. Care was taken not to expose the hydroxyapatite orbital implant during release of scar tissue. An oral mucous membrane graft was then harvested from inside the lower lip and sutured to the surrounding tissue in the orbital socket (Figure 3). A symblepharon ring was placed with an overlying conformer, which was sutured (with 4-0 silk) to the fornix and passed transcutaneously through the eyelid. The symblepharon ring and conformer were left in place for up to 4 weeks. A temporary suture tarsorraphy (with 4-0 silk) was done through the upper and lower eyelid margins to help keep the conformer and symblepharon ring in place. The donor site was dressed with Gelfoam. Postoperatively, patients were discharged with prescriptions for oral and topical antibiotics.
Figure 3.
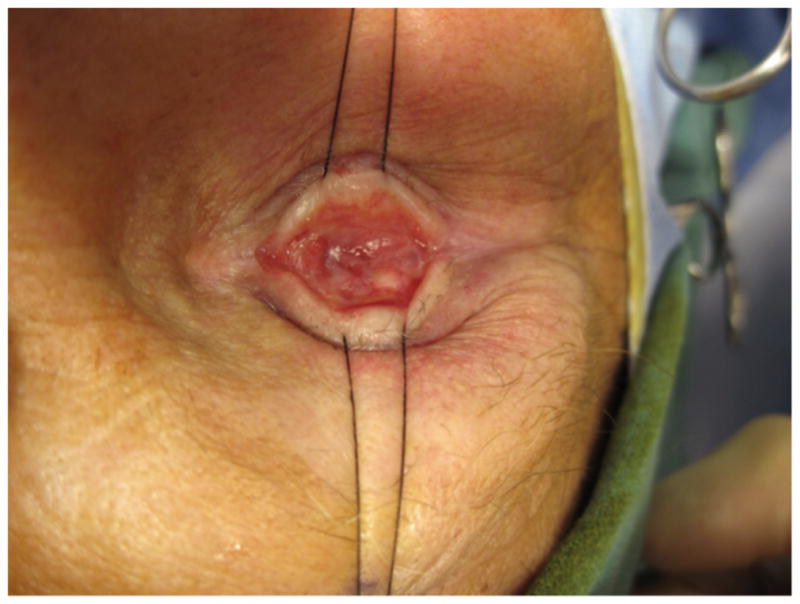

A) Intraoperative photograph of severely contracted socket. B) Oral mucous membrane graft has been added centrally in the socket after release of severe cicatrix with significant increase in volume and space in the socket.
Surgical Outcomes after Socket Reconstruction
The median follow-up time from surgical reconstruction of the socket to last contact was 10 months (range, 1–11 months). All 3 patients who underwent reconstruction were able to retain a prosthesis after surgical repair of the contracted socket (Figure 4). In 1 patient, severe orbital pain and pressure that had been present preoperatively resolved after reconstruction of the socket. The only postoperative complication encountered in our series was mild periorbital cellulitis in 1 patient, which resolved following a 7-day course of oral antibiotics.
Figure 4.
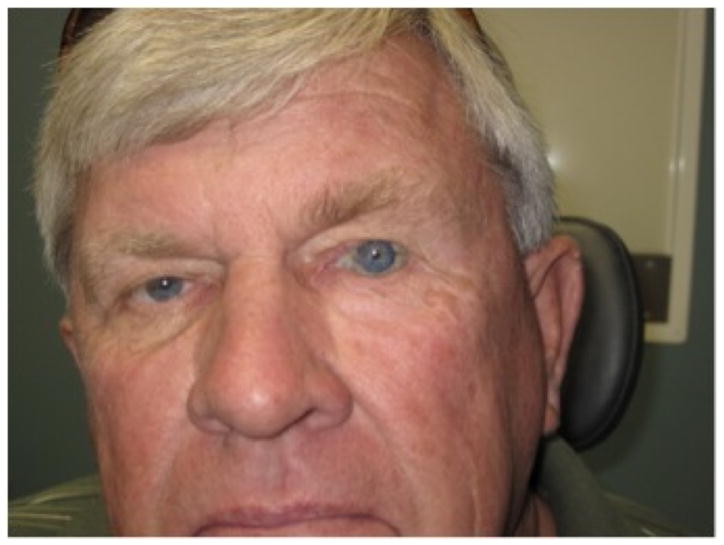
Patient with prosthesis in his left eye 6 months after surgical repair of a severely contracted socket.
Survival Data
The median follow-up time from completion of radiation therapy to last contact or death, whichever occurred first, was 34 months (range, 7–72 months).
At last follow-up, of the 12 patients who received radiation therapy after enucleation, 7 patients (58%) were free of disease (no local recurrence or distant metastasis), 1 patient (8%) was alive but had recently been diagnosed with metastasis (65 months following completion of radiation therapy), and 4 patients (33%) had died of their disease. Of the 4 patients who had died, 1 had socket contracture but opted not to have surgery and died 37 months after completion of radiation therapy. The remaining 3 patients died of metastatic uveal melanoma at 10, 13, and 19 months after completion of radiation therapy, and no information could be found in the medical records regarding ocular prosthesis wear.
DISCUSSION
Our report suggests about a 40% crude rate of severe socket contracture after high-dose adjuvant orbital radiation therapy in patients with uveal melanoma and enucleated sockets. This rate may be an underestimate given that 4 of the 12 patients who received high-dose radiation therapy died soon after completion of radiation therapy.
The high rate of severe socket contracture seen in this series is most likely related to the high dose of radiation (60 Gy). This dose is much higher than and almost double that used in patients with retinoblastoma; however, it is a standard dose of postoperative radiation in the head and neck for a variety of histologies, including melanoma and squamous carcinoma. Many articles in the literature discuss the role of external beam radiation therapy in retinoblastoma,8–14 and the radiation doses described in these articles range from 30 to 55 Gy. Nahum et al. reported a case series of 21 pediatric patients with retinoblastoma, 13 of whom had bilateral retinoblastoma and received external beam radiation therapy to a median dose of 32.3 Gy.13 At a median follow-up period of 12 years, only 1 patient (7.6%) had developed severe socket contracture. In a larger case series of 36 pediatric patients with bilateral retinoblastoma, Anteby et al. reported a 3% rate of severe socket contracture at a median follow-up time of 36 months.14 The significantly lower rates of severe socket contracture in patients with retinoblastoma than in patients with uveal melanoma could be explained by the lower dose of radiation used. It could also be explained by the fact that most retinoblastoma patients who undergo radiation therapy may not have had significant surgery; surgical intervention may have an additive effect to contracture of the socket. Finally, the presence of the globe which provides some volume for the socket while the patient is receiving radiation therapy may have a protective effect. Fewer articles discuss the role of external beam radiation therapy in patients with uveal melanoma.15–19 In a phase I/II study, Zehetmayer et al. used 45–70 Gy of gamma knife stereotactic external beam radiation to treat 62 patients with uveal melanoma who were deemed unsuitable for brachytherapy or local resection.15 In their report on this series of patients, there was no mention of socket contracture as a side effect at a median follow-up period of 28.3 months. However, eight eyes (13%) required enucleation. This underscores the possible protective effect of the presence of the globe during radiation therapy in terms of preventing severe socket contracture due to higher dose of radiation therapy. However, caution must be used in comparing these different techniques, total dose and fractionation schemes, and targets.
We were unable to find studies specifically on the impact of high-dose radiation therapy on the enucleated socket in patients with uveal melanoma. We were also unable to find any published reports on the specific timing of socket contracture following radiation therapy. In our series, the median interval from completion of high-dose radiation to onset of severe socket contracture was 20 months.
Surgical reconstruction of a severely contracted socket after radiation therapy can be difficult because of the compromised vascularity of the anophthalmic socket and severe and generalized scarring of the conjunctiva. Our report suggests that reconstruction of the severely contracted socket using an oral mucous membrane graft can permit successful prosthesis wear. All 3 patients who underwent surgery were able to retain an ocular prosthesis. In 1 patient, severe refractory orbital pain and pressure sensation resolved after reconstructive surgery. Several authors have reported success using vascularized flaps in severely contracted sockets, both to augment orbital volume and to improve anterior socket vascularization.20–25 In a retrospective observation case series of 22 patients, Li et al.7 reported successful functional and clinical outcomes after treatment of severely contracted eye sockets using microvascular radial forearm free flaps. Fourteen of the 22 patients had undergone enucleation followed by adjuvant radiation therapy for retinoblastoma. The report does not specify the radiation dosage but mentions that these patients developed unilateral orbitofacial growth retardation and severe socket contracture resulting in an inability to wear an ocular prosthesis. Postoperatively, all 14 patients had adequate socket size and were able to wear their ocular prosthesis with a mean follow-up period of 23 months (range, 6–72 months). Reconstruction with an oral mucous membrane graft, as performed in our study, is a much less invasive procedure than reconstruction with a vascularized free flap and is associated with a shorter surgical time. Another reported surgical technique for correction of socket contracture is the use of hard palate grafts, as reported by Holck et al. in 10 patients.26 These investigators achieved an 80% success rate with repair of severely contracted sockets using hard-palate mucosal grafts with a mean follow-up period of 19 months (range, 6–28 months). It should be noted, however, that none of the patients in their study had previously been treated with radiation therapy; 9 of the 10 patients had a contracted socket due to trauma, and in the remaining patient, who had retinoblastoma, there was no history of radiation exposure.
The other important observation in our series is that a significant number of the patients who received radiation therapy because of high-risk histologic features (5 of 12 patients; 42%) developed metastatic disease or died of their disease during follow-up after radiation therapy, which ranged from 7 to 72 months. In their multicenter study of 289 patients treated for choroidal or ciliary body melanoma, Kujala et al.27 reported that tumors with a basal tumor diameter greater than 13 mm or height greater than 7 mm, tumors located in the ciliary body, and tumors with histological evidence of extrascleral spread were associated with a higher risk of development of metastasis. According to their report, about 50% of patients with uveal melanoma develop metastatic disease, which is invariably fatal despite the successful eradication of the intraocular tumor, and 5- and 15-year survival rates are 68% and 50%, respectively. The report does not mention the specific survival rate for patients with uveal melanoma with high-risk histologic features; thus, comparison with the survival data in our series is difficult.
In summary, our study suggests that severe socket contraction is a fairly frequent occurrence after high-dose irradiation of the anophthalmic socket in patients with uveal melanoma. Surgical correction of severe socket contracture using oral mucous membrane grafting can be successful and can permit resumption of prosthesis wear. A significant number of patients with uveal melanoma with high-risk histologic features go on to develop metastatic disease despite delivery of high-dose radiation therapy to the socket. Advances in systemic therapies are needed to improve overall outcomes for this disease. We acknowledge that our sample size is small and future studies of perhaps multicenter nature and of larger numbers of patients would be needed to ascertain the utility of radiation therapy for high-risk uveal melanoma after enucleation.
High-dose radiotherapy in uveal melanoma patients causes severe anophthalmic socket contracture and inability to wear a prosthesis in approximately 40% of patients. Surgical repair using oral mucous membrane grafting can allow resumption of prosthesis wear.
Acknowledgments
Financial support: This research was supported in part by the National Institutes of Health through MD Anderson’s Cancer Center Support Grant, CA016672.
Footnotes
Proprietary interest statement: The authors have no commercial associations or financial interests that might pose a conflict of interest with information presented in this article.
References
- 1.Lederman M. Radiotherapy in treatment of orbital tumours. Br J Ophthalmol. 1956;40:592–610. doi: 10.1136/bjo.40.10.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foster JA, Castro E, Papay FA. Reconstruction of the irradiated contracted socket with an expanded superficial temporalis fascial flap. Am J Ophthalmol. 1999;127:621–2. doi: 10.1016/s0002-9394(98)00429-2. [DOI] [PubMed] [Google Scholar]
- 3.Krishna G. Contracted sockets--I (aetiology and types) Indian J Ophthalmol. 1980;28:117–20. [PubMed] [Google Scholar]
- 4.Shildkrot Y, Kirzhner M, Haik BG, Qaddoumi I, Rodriguez-Galindo C, Wilson MW. The Effect of Cancer Therapies on Pediatric Anophthalmic Sockets. Ophthalmology. 2011 Dec;118(12):2480–6. doi: 10.1016/j.ophtha.2011.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tawfik HA, Raslan AO, Talib N. Surgical management of acquired socket contracture. Curr Opin Ophthalmol. 2009;20:406–11. doi: 10.1097/ICU.0b013e32832ed85b. [DOI] [PubMed] [Google Scholar]
- 6.Mu X, Dong J, Chang T. Correction of the contracted eye socket and orbitozygomatic hypoplasia using postauricular skin flap and temporal fascial flap. J Craniofac Surg. 1999 Jan;10(1):11–7. doi: 10.1097/00001665-199901000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Li D, Jie Y, Liu H, et al. Reconstruction of anophthalmic orbits and contracted eye sockets with microvascular radial forearm free flaps. Ophthal Plast Reconstr Surg. 2008;24:94–7. doi: 10.1097/IOP.0b013e318166dad1. [DOI] [PubMed] [Google Scholar]
- 8.Schipper J. An accurate and simple method for megavoltage radiation therapy of retinoblastoma. Radiother Oncol. 1983;1:31–41. doi: 10.1016/s0167-8140(83)80005-x. [DOI] [PubMed] [Google Scholar]
- 9.Hernandez JC, Brady LW, Shields JA, et al. External beam radiation for retinoblastoma: results, patterns of failure, and a proposal for treatment guidelines. Int J Radiat Oncol Biol Phys. 1996;35:125–32. doi: 10.1016/s0360-3016(96)85020-6. [DOI] [PubMed] [Google Scholar]
- 10.Phillips C, Sexton M, Wheeler G, McKenzie J. Retinoblastoma: review of 30 years' experience with external beam radiotherapy. Australas Radiol. 2003;47:226–30. doi: 10.1046/j.1440-1673.2003.01167.x. [DOI] [PubMed] [Google Scholar]
- 11.Blach LE, McCormick B, Abramson DH. External beam radiation therapy and retinoblastoma: long-term results in the comparison of two techniques. Int J Radiat Oncol Biol Phys. 1996;35:45–51. doi: 10.1016/s0360-3016(96)85010-3. [DOI] [PubMed] [Google Scholar]
- 12.Choi SY, Kim MS, Yoo S, et al. Long term follow-up results of external beam radiotherapy as primary treatment for retinoblastoma. J Korean Med Sci. 2010;25:546–51. doi: 10.3346/jkms.2010.25.4.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nahum MP, Gdal-On M, Kuten A, et al. Long-term follow-up of children with retinoblastoma. Pediatr Hematol Oncol. 2001;18:173–9. doi: 10.1080/08880010151114769. [DOI] [PubMed] [Google Scholar]
- 14.Anteby I, Ramu N, Gradstein L, et al. Ocular and orbital complications following the treatment of retinoblastoma. Eur J Ophthalmol. 1998;8:106–11. doi: 10.1177/112067219800800210. [DOI] [PubMed] [Google Scholar]
- 15.Zehetmayer M, Kitz K, Menapace R, et al. Local tumor control and morbidity after one to three fractions of stereotactic external beam irradiation for uveal melanoma. Radiother Oncol. 2000;55:135–44. doi: 10.1016/s0167-8140(00)00164-x. [DOI] [PubMed] [Google Scholar]
- 16.Rennie I, Forster D, Kemeny A, et al. The use of single fraction Leksell stereotactic radiosurgery in the treatment of uveal melanoma. Acta Ophthalmol Scand. 1996;74:558–62. doi: 10.1111/j.1600-0420.1996.tb00734.x. [DOI] [PubMed] [Google Scholar]
- 17.Tokuuye K, Akine Y, Sumi M, et al. Fractionated stereotactic radiotherapy for choroidal melanoma. Radiother Oncol. 1997;43:87–91. doi: 10.1016/s0167-8140(97)01910-5. [DOI] [PubMed] [Google Scholar]
- 18.Marchini G, Gerosa M, Piovan E, et al. Gamma Knife stereotactic radiosurgery for uveal melanoma: clinical results after 2 years. Stereotact Funct Neurosurg. 1996;66 (Suppl 1):208–13. doi: 10.1159/000099812. [DOI] [PubMed] [Google Scholar]
- 19.Marchini G, Babighian S, Tomazzoli L, et al. Stereotactic radiosurgery of uveal melanomas: preliminary results with Gamma Knife treatment. Stereotact Funct Neurosurg. 1995;64 (Suppl 1):72–9. doi: 10.1159/000098766. [DOI] [PubMed] [Google Scholar]
- 20.Bosniak SL. Reconstruction of the anophthalmic socket: state of the art. Adv Ophthalmic Plast Reconstr Surg. 1987;7:313–48. [PubMed] [Google Scholar]
- 21.Guyuron B. The role of flaps in the management of contracted eye sockets. Adv Ophthalmic Plast Reconstr Surg. 1992;9:143–57. [PubMed] [Google Scholar]
- 22.Bonavolonta G. Temporalis muscle transfer in the treatment of severely contracted socket. Adv Ophthalmic Plast Reconstr Surg. 1992;9:121–9. [PubMed] [Google Scholar]
- 23.Guyuron B, Labandter HP, Berlin AJ. Fasciocutaneous flap, secondary axial pattern flap, and microvascular free flap in socket reconstruction. Ophthalmology. 1984;91:94–101. doi: 10.1016/s0161-6420(84)34325-1. [DOI] [PubMed] [Google Scholar]
- 24.Björnsonn A, Einarsson O. Repair of the contracted eye socket using a flap from the upper eyelid. Plast Reconstr Surg. 1984;74:287–9. doi: 10.1097/00006534-198408000-00021. [DOI] [PubMed] [Google Scholar]
- 25.Asato H, Harii K, Yamada A, Ueda K. Eye socket reconstruction with free-flap transfer. Plast Reconstr Surg. 1993;92:1061–7. doi: 10.1097/00006534-199311000-00010. [DOI] [PubMed] [Google Scholar]
- 26.Holck DE, Foster JA, Dutton JJ, Dillon HD. Hard palate mucosal grafts in the treatment of the contracted socket. Ophthal Plast Reconstr Surg. 1999;15:202–9. doi: 10.1097/00002341-199905000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Kujala E, Mäkitie T, Kivelä T. Very long-term prognosis of patients with malignant uveal melanoma. Invest Ophthalmol Vis Sci. 2003;44:4651–9. doi: 10.1167/iovs.03-0538. [DOI] [PubMed] [Google Scholar]


