Abstract
Recent research on the post-1980 widening of US socioeconomic mortality inequalities has emphasized the contribution of smoking and high-tech medicine, with some studies treating the growing inequalities as effectively inevitable. No studies, however, have analyzed long-term trends in US mortality rates and inequities unrelated to smoking or due to lack of basic medical care, even as a handful have shown that US socioeconomic inequalities in overall mortality shrank between the mid-1960s and 1980. We accordingly analyzed US mortality data for 1960–2006, stratified by county income quintile and race/ethnicity, for mortality unrelated to smoking and preventable by 1960s standards of medical care. Key findings were that relative and absolute socioeconomic inequalities in US mortality unrelated to smoking and preventable by 1960s medical care standards shrank between the 1960s and 1980 and then increased and stagnated, with absolute rates on par with several leading causes of death, and with the burden worst for US populations of color. None of these findings can be attributed to trends in smoking-related deaths and access to high-tech medicine, and they also demonstrate that socioeconomic inequities in mortality can shrink and need not inevitably rise.
Recent research has emphasized the contribution of smoking and high-tech medicine to the post-1980 widening of socioeconomic inequalities in mortality in the US and other affluent nations, a pattern posited to reflect how more affluent persons most quickly adopt healthy behaviours (especially stop, or never start, smoking) and obtain access to medical innovation.1–3 These rising inequalities have been argued to be acceptable as long as rates of adverse outcomes are falling for everyone, even if more quickly for those with more versus less economic resources.2
However, both extant data – and gaps in evidence – call into question inferences about the inevitability of rising health inequalities as well as the centrality of smoking and high-tech medicine to these trends. In the US, for example, the handful of studies examining trends in socioeconomic inequalities in mortality over longer time periods have shown that between the mid-1960s and 1980, also a period of declining US mortality rates, the magnitude of socioeconomic inequalities declined for premature mortality and infant death rates,4 life expectancy,1 and all-cause mortality among US white women ages 25–64 years old.5 These results, along with the lack of US or other data on long-term trends in socioeconomic inequalities for causes of death unrelated to smoking or due to lack of basic medical care,1–4 imply more critical scrutiny is needed regarding long-term trends in socioeconomic inequalities in mortality and their causes.
Accordingly, informed by the ecosocial theory of disease distribution and its approach to analyzing how we literally embody, biologically, our societal and ecological context, thereby creating population patterns of health and health inequities,6 we newly examine the past half-century’s trends in US mortality rates to test the a priori hypotheses that: (1) between the mid-1960s and 1980, socioeconomic inequalities for mortality (a) unrelated to smoking and (b) preventable by medical care standards of the 1960s (i.e., basic, not high-tech, medicine) would shrink, and then rise or stagnate thereafter, and (2) their current absolute burden of inequitable mortality, far from being small, would equal or exceed mortality rates due to several leading causes of death.
METHODS
Mortality data
Following a previously established protocol,4 we obtained US county-level mortality data for 1960–1967 from the US National Center for Health Statistics (NCHS),7 for which we then manually located and identified the correct county codes for each of the 3,073 counties. We also extracted the available 1968–2006 data from the NCHS US Compressed Mortality files.8 The study was approved as exempt by the Harvard School of Public Health Human Subjects Committee (HSC Protocol #P15744-101).
Codes for the underlying cause of death, as defined by the International Classification of Diseases (ICD),9 corresponded to the year in which the deaths occurred: ICD-7 (1960–1967), ICD-8 (1968–1978), ICD-9 (1979–1998), and ICD-10 (1999–2006); see Supplemental Table 1. Deaths unrelated to smoking (Table 1; ICD codes: Supplemental Table 1) included any cause of death not listed in the 2008 US Centers for Disease Control and Prevention update on smoking-related causes of death.10 Deaths preventable by medical care standards of the 1960s comprised 14 causes of death (Table 1; ICD codes: Supplemental Table 1) for which medical procedures available since the 1960s should have prevented death, given the occurrence of the illness or injury (i.e., secondary or tertiary, not primary, prevention).11–13 Causes of death more recently deemed medically preventable (e.g., breast cancer) were not included.14
Table 1.
Number of deaths (N) and person-years (PY) at risk by cause of death for the total population, white population, and populations of color, United States, 1960–2006.
| Cause of death |
Total population | White population | Populations of color | |||
|---|---|---|---|---|---|---|
| PY | N | PY | N | PY | N | |
| All-cause | 11,077,768,226 | 97,573,286 | 9,384,715,232 | 84,802,395 | 1,693,052,994 | 12,770,891 |
| Medically preventable* | 14,056,313 | 12,039,994 | 2,016,319 | |||
| Not smoking related** | 41,156,141 | 34,687,362 | 6,468,779 | |||
Medically preventable mortality = deaths due to causes preventable by medical intervention available since at least 1960 (tuberculosis, cervical cancer, Hodgkin’s disease, chronic rheumatic heart disease, hypertensive heart disease, cerebrovascular disease, acute upper respiratory disease, bronchitis, pneumonia, influenza, asthma, appendicitis, inguinal (abdominal) hernia, and cholecystitis)11–13
Not smoking related = all causes of death excluding the causes of death listed as at least partially attributable to smoking in the 2004 US Surgeon’s General Report Health Consequences of Smoking and in the updated list published by the CDC in 2008,10 consisting of: Malignant neoplasm (lip, oral cavity, pharynx; esophagus; stomach; pancreas; trachea/lung/bronchus; cervix uteri; kidney and renal pelvis; urinary bladder; acute myeloid leukemia); Cardiovascular disease (ischemic heart disease; other heart disease; cerebrovascular disease; arteriosclerosis; aortic aneurysm; other circulatory disease); Respiratory disease (pneumonia, influenza; bronchitis, emphysema; chronic airways obstruction); Perinatal conditions (short gestation/low birth weight; respiratory distress syndrome; other respiratory (newborn); Sudden Infant Death Syndrome); Residential Fire; Secondhand smoke (lung cancer; ischemic heart disease.
Denominator data
We obtained the county-level denominator data from the 1960–2000 US decennial counts, US Census Bureau intercensal population estimates, and NCHS interpolated estimates for 1968 and 1969 and extrapolated estimates for 2001–2006.8 We estimated the 1961–1967 denominators using linear interpolation, based on the 1960 and 1968 population data, and followed NCHS guidelines for merging and unmerging the small number of counties over time which were eliminated, established, or had boundaries redrawn.8 Because Alaska used non-identical county boundaries in their pre-1989 population and mortality data, Alaska analyses before 1989 were for the entire state only (equaling 0.01%–0.02% of the US population).
County income quintiles and racial/ethnic classification
We supplemented the annual county mortality data with US decennial county data on: (a) median family income15–17 (adjusted for inflation and regional cost of living18), and also, to ensure diversity of socioeconomic measures,6,19 (b) the proportion of adults age 25 and older with less than a high school education15,16; given similar results, we report only the county income analyses. To generate annual data on the socioeconomic measures, we used linear interpolation for intercensal years and extrapolated for 2001–2006 based on the slope for 1990–2000. We then assigned counties to quintiles, weighted by county population size, given its enormous variation; cut-points for the decennial county income quintiles are provided in Supplemental Table 2, with Quintile 1 (Q1) and Quintile 5 (Q5) respectively set as the lowest and highest county income quintiles. Missingness due to counties lacking income data was minimal (<1%) for both denominators and numerators.
As with the US census,16,20 the only racial/ethnic categories consistently available in the US mortality data from 1960 to 2006 were for what the NCHS termed “white” and “non-white” populations.7,8 This distinction – and the data limitations that underlie it – reflect the persistence of what W.E.B. Du Bois in 1904 famously termed the US “colorline,”21 which divides the politically dominant US white population from all other racial/ethnic groups. Consistent with US Census and contemporary scholarship,16,20 in our analyses, we accordingly conceptualize race/ethnicity as a social and political, and not intrinsically biological, category.6 New Jersey death certificates did not identify race/ ethnicity in 1962 and 1963, precluding use of these two years’ data (< 3% of the US population).
Statistical analysis
For each calendar year we aggregated the county mortality and population data in each county income quintile and calculated each quintile’s age-standardized mortality rates, standardized to the Year 2000 standard million.22 We conducted these analyses for all-cause mortality, selected leading causes of death (Supplemental Table 3), and the two main study outcomes: mortality unrelated to smoking and mortality due to causes of death preventable by 1960s standards of medical care. We used SAS 9.1 to conduct all of our analyses,23 except where indicated otherwise.
For both the two study outcomes and also all-cause mortality (data not shown; available upon request), we calculated each year’s age-standardized incidence rate ratio (IRR), a measure of relative disparity,19 and also the incidence rate difference (IRD), a measure of absolute difference,19 setting as referent group the highest county income quintile. We also calculated the population attributable fraction (PAF)19,24 as a metric for quantifying the gap between the empirically observed and the then achievable death rates across county income quintiles.4,19 For these analyses, we calculated the total and proportion of deaths that would not have occurred each year if residents of the four lowest county income quintiles experienced the same yearly age-specific death rates as persons in the highest county income quintile; a related set of calculations for the white population and populations of color set as referent group the mortality rate of white persons in the highest county income quintile.
To explore changes in the slope of the decline in mortality rates, the IRR, and the IRD, we used joinpoint regression techniques.25 In these models, also called segmented line regression models, line segments are joined at points called “joinpoints,” which denote statistically significant changes (p < 0.05) in the time trend; the slope of these line segments, when fit on the log scale, is interpretable as the log annual percent change (APC) in the rate.25
The study funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
RESULTS
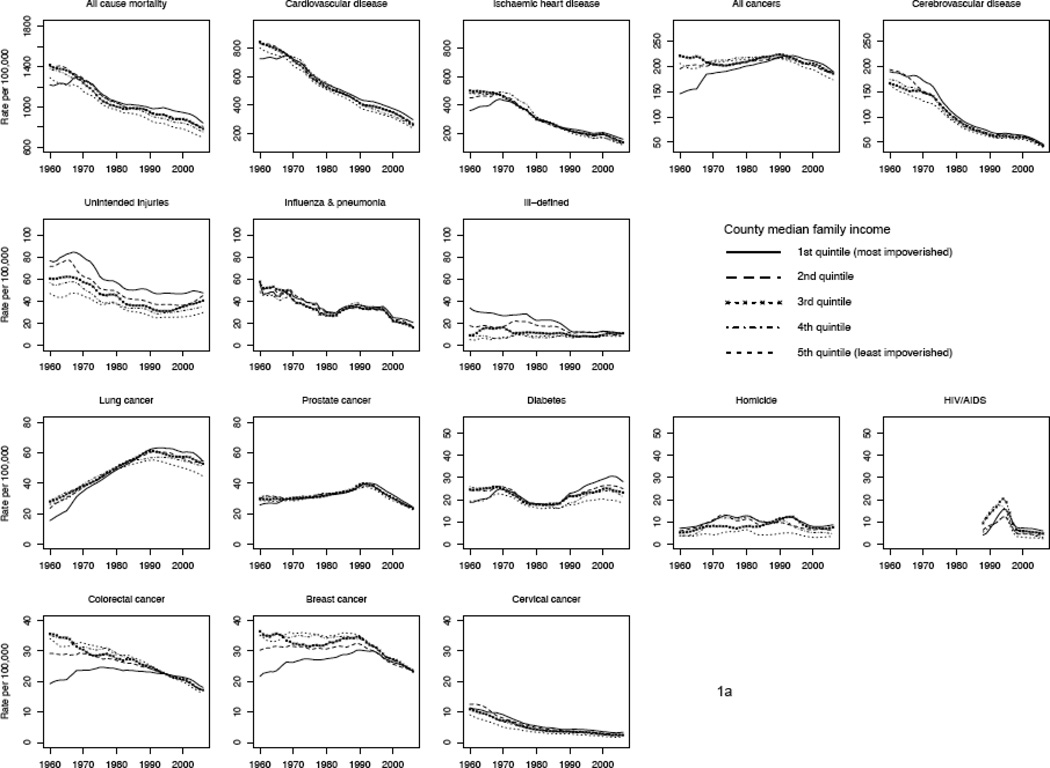
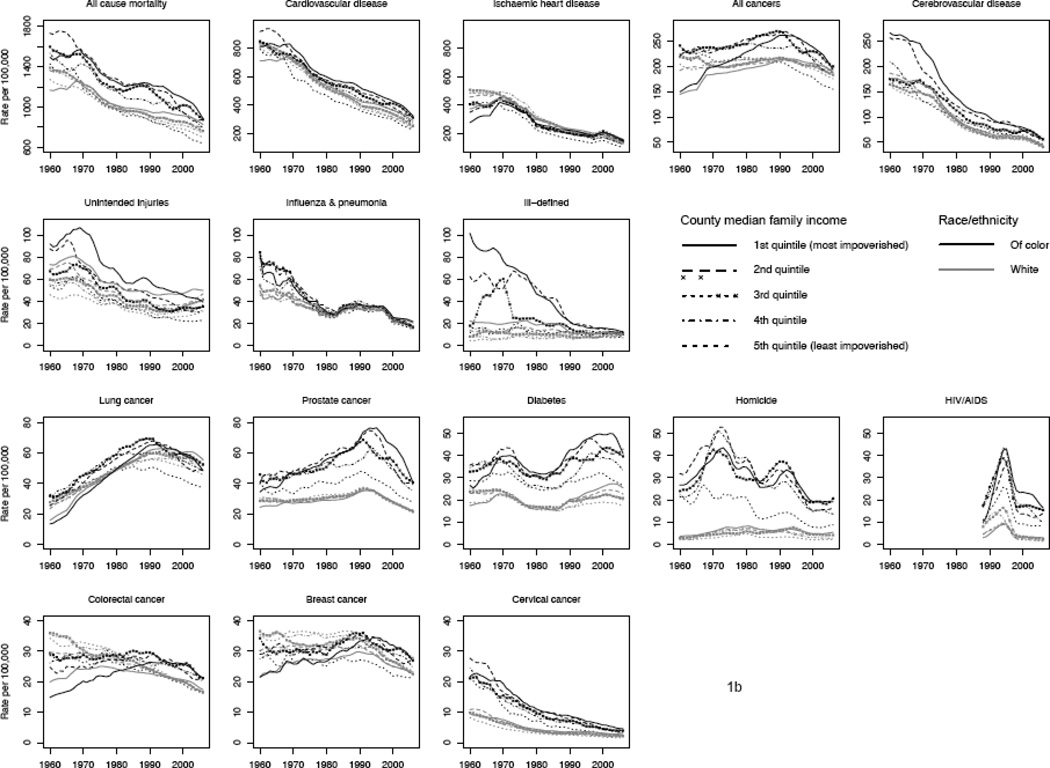
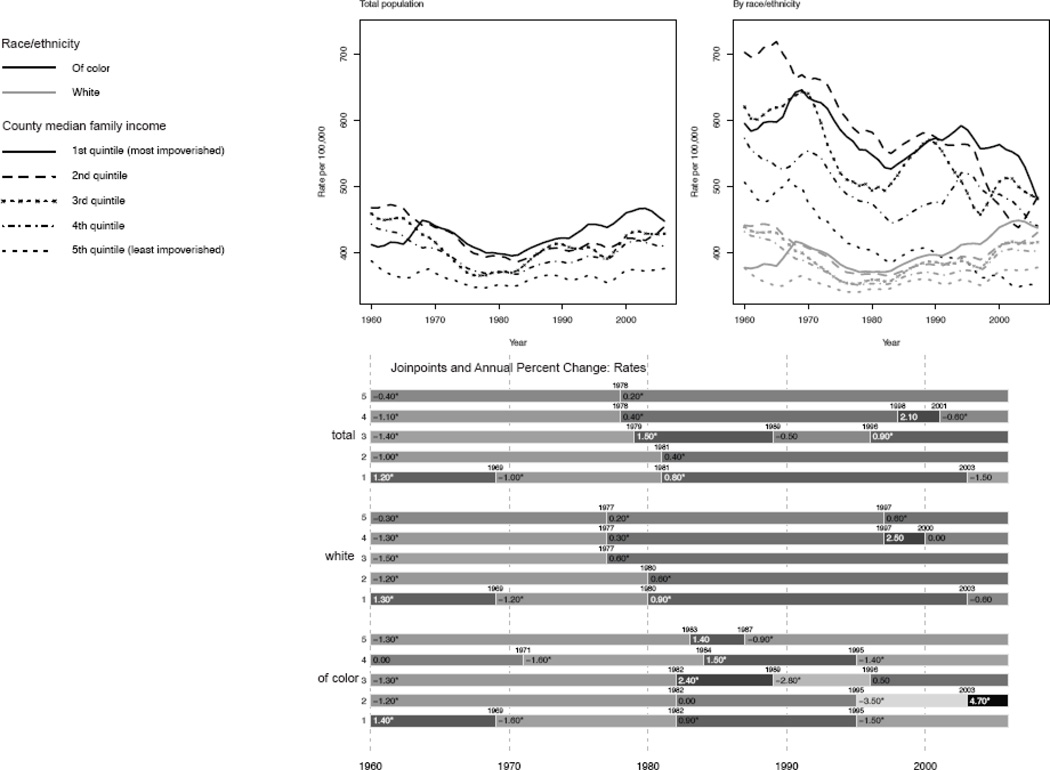
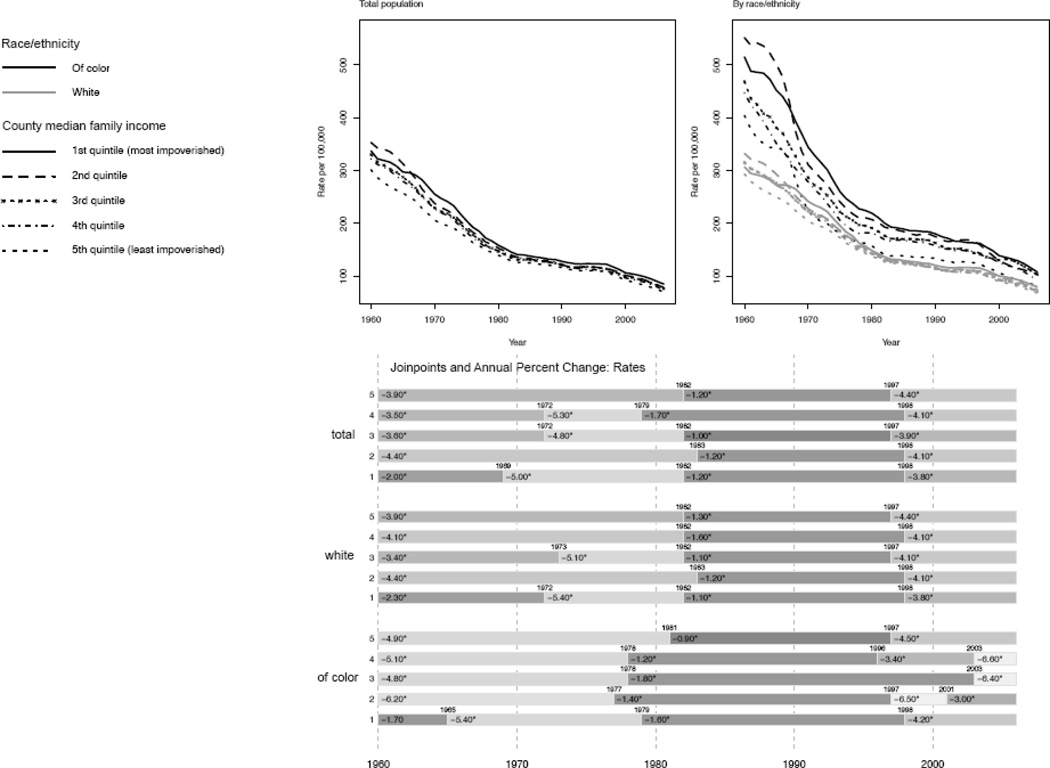
Table 1 provides data on the study population pertaining to number of person-years and number of deaths observed. To provide context, Figure 1 shows trends for 1960–2006, stratified by county income quintile, for 3-year moving averages for the age-standardized rates for all-cause mortality and for selected leading causes of death, Figure 2a and 2b, show: (1) analogous graphs for, respectively, mortality unrelated to smoking and mortality due to deaths preventable by 1960s medical care standards, and (2) results of the joinpoint analyses, which show the years in which a statistically significant inflection points (p <0.05) in the slope of the mortality rate occurred along with the average annual percent change (APC) in mortality rates between these time points. Figure 3 in turn supplies data on the changing proportion of deaths unrelated to smoking, rising from ~40% in 1960 to over 60% in 2000.
Figure 1.
All-cause, cause-specific, and grouped-cause mortality rates (age-standardized to the Year 2000 standard million) by county income quintile, for (a) the total population, and (b) the white population and populations of color: United States, 1960–2006.
Figure 2.
Mortality rate for: (a) deaths unrelated to smoking (age-standardized to the Year 2000 standard million), and (b) deaths preventable by 1960s standards of medical care (age-standardized to the Year 2000 standard million), by county income quintile, joinpoints, and annual percent change (APC) (95% CI) between joinpoints for total population, white population, and populations of color: United States, 1960–2006.
Figure 3.
Proportion of deaths unrelated to smoking (age-standardized to the Year 2000 standard million), by county income quintile by year, for total population, white population, and populations of color: United States, 1960–2006.
Causes of death unrelated to smoking
For causes of death unrelated to smoking (Figure 2a), both mortality rates and their socioeconomic IRR and IRD significantly declined from 1960 to about 1980 (APC across income quintiles ranging between 0.4 to 1.4% per year; p < 0.05), except in the lowest quintile, for which rates significantly rose between 1960 and 1969, and then declined. After 1980, mortality rates for deaths unrelated to smoking significantly increased (p <0.05) in all income quintiles, with the increases greatest in the lower income quintiles (APC of 0.2% in the highest income quintile vs. 0.8% in the lowest income quintile), yielding rising IRRs and IRDs. The post-1980 rise was sufficiently great that in 2006, mortality rates unrelated to smoking (rates approximately 380/100,000 in the highest income quintile to about 460/100,000 in the lowest income quintile) exceeded those for cardiovascular disease in each income quintile (approximately 250 to 350/100,000, respectively; Figure 1a). In 2006, the absolute gap comparing rates in the most versus least affluent counties (71.5/100,000; Table 2a) equalled that for total US mortality for lung cancer and diabetes combined (51.5 and 23.3 per 100,000 respectively).
Table 2.
Mortality (a) unrelated to smoking, and (b) preventable by 1960s standards of medical care: incidence rate ratio (IRR) and incidence rate difference (IRD) by county income quintile, and population attributable fraction (PAF), for total, white, and of color populations: United States, 1960, 1970, 1980, 1990, 2000, and 2006.
| (a) Mortality unrelated to smoking | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| County income |
Year | ||||||||||||
| Population | quintile | 1960 | 1970 | 1980 | 1990 | 2000 | 2006 | ||||||
| IRR | (95% CI) | IRR | (95% CI) | IRR | (95% CI) | IRR | (95% CI) | IRR | (95% CI) | IRR | (95% CI) | ||
| Total | 5 (highest) | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . |
| 4 | 1.14 | (1.13, 1.15) | 1.10 | (1.09, 1.11) | 1.06 | (1.05, 1.07) | 1.06 | (1.06, 1.07) | 1.11 | (1.10, 1.12) | 1.09 | (1.08, 1.10) | |
| 3 | 1.18 | (1.17, 1.19) | 1.12 | (1.11, 1.13) | 1.06 | (1.05, 1.07) | 1.14 | (1.13, 1.15) | 1.13 | (1.13, 1.14) | 1.14 | (1.13, 1.15) | |
| 2 | 1.21 | (1.20, 1.22) | 1.19 | (1.18, 1.20) | 1.13 | (1.12, 1.14) | 1.12 | (1.11, 1.13) | 1.13 | (1.12, 1.14) | 1.17 | (1.16, 1.17) | |
| 1 (lowest) | 1.06 | (1.05, 1.07) | 1.19 | (1.18, 1.20) | 1.14 | (1.13, 1.15) | 1.16 | (1.15, 1.17) | 1.23 | (1.22, 1.24) | 1.19 | (1.18, 1.20) | |
| White | 5 (highest) | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . |
| 4 | 1.14 | (1.13, 1.16) | 1.07 | (1.06, 1.08) | 1.03 | (1.02, 1.04) | 1.03 | (1.03, 1.04) | 1.08 | (1.07, 1.09) | 1.07 | (1.06, 1.07) | |
| 3 | 1.16 | (1.15, 1.17) | 1.09 | (1.08, 1.10) | 1.04 | (1.03, 1.05) | 1.09 | (1.08, 1.10) | 1.10 | (1.09, 1.10) | 1.10 | (1.09, 1.11) | |
| 2 | 1.17 | (1.16, 1.18) | 1.13 | (1.12, 1.14) | 1.07 | (1.06, 1.07) | 1.07 | (1.06, 1.08) | 1.11 | (1.10, 1.12) | 1.14 | (1.13, 1.15) | |
| 1 (lowest) | 1.00 | (0.99, 1.01) | 1.13 | (1.12, 1.14) | 1.08 | (1.07, 1.08) | 1.11 | (1.10, 1.12) | 1.18 | (1.17, 1.19) | 1.16 | (1.15, 1.16) | |
| Of color | 5 (highest) | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . |
| 4 | 1.13 | (1.09, 1.17) | 1.12 | (1.09, 1.15) | 1.17 | (1.14, 1.20) | 1.18 | (1.16, 1.21) | 1.34 | (1.31, 1.36) | 1.27 | (1.25, 1.29) | |
| 3 | 1.22 | (1.19, 1.26) | 1.31 | (1.27, 1.35) | 1.26 | (1.23, 1.29) | 1.42 | (1.39, 1.45) | 1.36 | (1.34, 1.38) | 1.39 | (1.36, 1.41) | |
| 2 | 1.39 | (1.35, 1.43) | 1.36 | (1.33, 1.40) | 1.48 | (1.45, 1.52) | 1.43 | (1.40, 1.46) | 1.30 | (1.28, 1.32) | 1.39 | (1.37, 1.42) | |
| 1 (lowest) | 1.18 | (1.14, 1.21) | 1.29 | (1.26, 1.33) | 1.38 | (1.35, 1.41) | 1.43 | (1.40, 1.46) | 1.53 | (1.50, 1.55) | 1.38 | (1.36, 1.40) | |
| IRD | (95% CI) | IRD | (95% CI) | IRD | (95% CI) | IRD | (95% CI) | IRD | (95% CI) | IRD | (95% CI) | ||
| Total | 5 (highest) | . | . . | . | . . | . | . . | . | . . | . | . . | . | . . |
| 4 | 55.4 | (51.6, 59.1) | 36.0 | (32.7, 39.3) | 20.3 | (17.5, 23.2) | 22.7 | (20.1, 25.3) | 41.9 | (39.4, 44.3) | 34.3 | (32.0, 36.6) | |
| 3 | 71.3 | (67.6, 75.0) | 44.8 | (41.5, 48.1) | 20.8 | (18.0, 23.6) | 51.8 | (49.1, 54.4) | 50.3 | (47.9, 52.7) | 52.5 | (50.2, 54.8) | |
| 2 | 80.3 | (76.6, 84.0) | 69.8 | (66.4, 73.1) | 46.1 | (43.2, 48.9) | 42.8 | (40.2, 45.4) | 48.8 | (46.4, 51.1) | 63.4 | (61.1, 65.7) | |
| 1 (lowest) | 24.7 | (21.1, 28.3) | 69.8 | (66.5, 73.1) | 48.7 | (45.9, 51.5) | 58.5 | (55.9, 61.1) | 87.0 | (84.6, 89.4) | 71.5 | (69.2, 73.8) | |
| White | 5 (highest) | . | . . | . | . . | . | . . | . | . . | . | . . | . | . . |
| 4 | 54.5 | (50.6, 58.3) | 23.8 | (20.4, 27.2) | 9.3 | (6.4, 12.3) | 12.4 | (9.6, 15.1) | 29.5 | (26.9, 32.0) | 25.2 | (22.8, 27.7) | |
| 3 | 61.9 | (58.1, 65.7) | 31.2 | (27.8, 34.6) | 14.5 | (11.6, 17.4) | 31.2 | (28.4, 33.9) | 36.0 | (33.5, 38.6) | 37.9 | (35.5, 40.4) | |
| 2 | 64.2 | (60.4, 68.0) | 47.2 | (43.8, 50.6) | 22.8 | (19.8, 25.7) | 25.0 | (22.4, 27.7) | 40.5 | (38.0, 43.0) | 52.5 | (50.1, 55.0) | |
| 1 (lowest) | 0.3 | (−3.4, 3.9) | 47.7 | (44.3, 51.1) | 26.3 | (23.4, 29.2) | 40.1 | (37.5, 42.8) | 67.1 | (64.6, 69.7) | 59.4 | (56.9, 61.9) | |
| Of color | 5 (highest) | . | . . | . | . . | . | . . | . | . . | . | . . | . | . . |
| 4 | 66.4 | (48.6, 84.1) | 59.7 | (45.3, 74.1) | 69.4 | (58.8, 80.0) | 73.4 | (64.4, 82.4) | 123.7 | (115.9, 131.6) | 93.1 | (86.5, 99.8) | |
| 3 | 113.9 | (97.7, 130.1) | 151.7 | (136.3, 167.2) | 106.5 | (94.7, 118.4) | 167.3 | (158.0, 176.5) | 132.6 | (125.3, 140.0) | 134.5 | (128.1, 141.0) | |
| 2 | 196.0 | (179.7, 212.3) | 178.1 | (163.3, 192.8) | 196.9 | (186.0, 207.8) | 172.8 | (163.3, 182.2) | 110.2 | (102.6, 117.8) | 136.9 | (130.2, 143.6) | |
| 1 (lowest) | 88.7 | (74.3, 103.1) | 143.0 | (129.1, 157.0) | 156.4 | (146.2, 166.6) | 172.8 | (163.8, 181.8) | 194.4 | (187.2, 201.7) | 132.9 | (126.8, 138.9) | |
| referent | PAF | PAF | PAF | PAF | PAF | PAF | |||||||
| total | total, Q5 | 12.6% | (12.1%, 13.0%) | 12.7% | (12.2%, 13.2%) | 8.6% | (8.1%, 9.0%) | 10.4% | (10.0%, 10.8%) | 11.8% | (11.4%, 12.2%) | 11.6% | (11.3, 12.0%) |
| white | white, Q5 | 10.4% | (9.9%, 10.9%) | 9.5% | (9.0%, 10.1%) | 5.3% | (4.8%, 5.8%) | 7.0% | (6.5%, 7.4%) | 9.1% | (8.7%, 9.5%) | 9.2% | (8.8, 9.6%) |
| of color | white, Q5 | 45.4% | (44.9%, 45.9%) | 45.9% | (45.4%, 46.3%) | 36.7% | (36.2%, 37.2%) | 36.3% | (35.8%, 36.8%) | 27.1% | (26.6%, 27.6%) | 19.5% | (19.0, 20.1%) |
| (b) Mortality preventable by 1960s standards of medical care | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| County income |
Year | ||||||||||||
| Population | quintile | 1960 | 1970 | 1980 | 1990 | 2000 | 2006 | ||||||
| IRR | (95% CI) | IRR | (95% CI) | IRR | (95% CI) | IRR | (95% CI) | IRR | (95% CI) | IRR | (95% CI) | ||
| Total | 5 (highest) | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . |
| 4 | 1.07 | (1.06, 1.08) | 1.10 | (1.09, 1.11) | 1.06 | (1.04, 1.07) | 1.04 | (1.03, 1.06) | 1.04 | (1.03, 1.05) | 1.06 | (1.04, 1.07) | |
| 3 | 1.10 | (1.08, 1.11) | 1.11 | (1.10, 1.13) | 1.04 | (1.02, 1.05) | 1.04 | (1.03, 1.06) | 1.07 | (1.06, 1.08) | 1.08 | (1.07, 1.10) | |
| 2 | 1.17 | (1.16, 1.19) | 1.16 | (1.14, 1.17) | 1.09 | (1.08, 1.11) | 1.05 | (1.03, 1.06) | 1.10 | (1.09, 1.12) | 1.12 | (1.10, 1.13) | |
| 1 (lowest) | 1.12 | (1.11, 1.13) | 1.25 | (1.23, 1.26) | 1.12 | (1.11, 1.14) | 1.11 | (1.09, 1.12) | 1.14 | (1.13, 1.16) | 1.21 | (1.19, 1.23) | |
| White | 5 (highest) | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . |
| 4 | 1.07 | (1.05, 1.08) | 1.07 | (1.06, 1.09) | 1.03 | (1.02, 1.05) | 1.02 | (1.00, 1.03) | 1.02 | (1.01, 1.03) | 1.04 | (1.02, 1.05) | |
| 3 | 1.08 | (1.06, 1.09) | 1.09 | (1.08, 1.11) | 1.02 | (1.01, 1.04) | 1.00 | (0.99, 1.02) | 1.04 | (1.02, 1.05) | 1.04 | (1.03, 1.06) | |
| 2 | 1.13 | (1.12, 1.15) | 1.11 | (1.10, 1.13) | 1.05 | (1.04, 1.07) | 1.01 | (0.99, 1.02) | 1.09 | (1.07, 1.10) | 1.09 | (1.08, 1.11) | |
| 1 (lowest) | 1.05 | (1.03, 1.06) | 1.19 | (1.17, 1.20) | 1.07 | (1.05, 1.08) | 1.06 | (1.05, 1.08) | 1.11 | (1.09, 1.12) | 1.16 | (1.15, 1.18) | |
| Of color | 5 (highest) | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . | 1.00 | . . |
| 4 | 1.11 | (1.06, 1.15) | 1.26 | (1.20, 1.32) | 1.16 | (1.11, 1.21) | 1.18 | (1.14, 1.23) | 1.14 | (1.10, 1.19) | 1.15 | (1.11, 1.20) | |
| 3 | 1.16 | (1.12, 1.20) | 1.27 | (1.21, 1.33) | 1.24 | (1.18, 1.29) | 1.25 | (1.20, 1.30) | 1.19 | (1.15, 1.23) | 1.28 | (1.23, 1.32) | |
| 2 | 1.36 | (1.32, 1.42) | 1.40 | (1.34, 1.47) | 1.33 | (1.28, 1.39) | 1.34 | (1.29, 1.39) | 1.20 | (1.15, 1.24) | 1.28 | (1.23, 1.33) | |
| 1 (lowest) | 1.27 | (1.23, 1.32) | 1.57 | (1.50, 1.64) | 1.39 | (1.33, 1.44) | 1.37 | (1.32, 1.43) | 1.28 | (1.23, 1.32) | 1.33 | (1.29, 1.38) | |
| IRD | (95% CI) | IRD | (95% CI) | IRD | (95% CI) | IRD | (95% CI) | IRD | (95% CI) | IRD | (95% CI) | ||
| Total | 5 (highest) | 0 | . . | 0 | . . | 0 | . . | 0 | . . | 0 | . . | . | . . |
| 4 | 20.6 | (16.9, 24.4) | 20.6 | (17.9, 23.4) | 8.2 | (6.3, 10.1) | 5.2 | (3.7, 6.8) | 3.9 | (2.6, 5.1) | 3.9 | (2.9, 4.9) | |
| 3 | 29.1 | (25.4, 32.7) | 23.1 | (20.4, 25.9) | 5.2 | (3.3, 7.2) | 5.0 | (3.5, 6.6) | 6.4 | (5.2, 7.6) | 5.9 | (4.9, 6.9) | |
| 2 | 51.7 | (48.0, 55.4) | 31.8 | (29.0, 34.6) | 13.4 | (11.5, 15.4) | 5.6 | (4.1, 7.1) | 9.7 | (8.5, 10.9) | 8.2 | (7.2, 9.1) | |
| 1 (lowest) | 35.8 | (32.2, 39.4) | 50.8 | (48.1, 53.5) | 18.0 | (16.1, 19.8) | 12.5 | (11.0, 13.9) | 13.5 | (12.3, 14.7) | 14.7 | (13.7, 15.7) | |
| White | 5 (highest) | 0 | . . | 0 | . . | 0 | . . | 0 | . . | 0 | . . | . | . . |
| 4 | 19.6 | (15.8, 23.4) | 14.7 | (11.8, 17.5) | 4.8 | (2.9, 6.8) | 1.8 | (0.2, 3.4) | 1.8 | (0.5, 3.1) | 2.5 | (1.5, 3.6) | |
| 3 | 22.1 | (18.4, 25.9) | 19.0 | (16.2, 21.9) | 3.0 | (1.1, 5.0) | 0.4 | −(1.2, 1.9) | 3.4 | (2.2, 4.6) | 2.9 | (1.9, 3.9) | |
| 2 | 38.8 | (35.0, 42.6) | 23.0 | (20.2, 25.9) | 7.3 | (5.3, 9.3) | 0.9 | −(0.6, 2.4) | 8.1 | (6.8, 9.3) | 6.3 | (5.3, 7.3) | |
| 1 (lowest) | 13.3 | (9.6, 17.0) | 37.9 | (35.1, 40.7) | 9.7 | (7.8, 11.7) | 7.2 | (5.7, 8.8) | 9.8 | (8.5, 11.0) | 11.3 | (10.2, 12.3) | |
| Of color | 5 (highest) | 0 | . . | 0 | . . | 0 | . . | 0 | . . | 0 | . . | . | . . |
| 4 | 42.7 | (24.5, 61.0) | 57.7 | (46.2, 69.3) | 25.5 | (18.0, 33.1) | 24.0 | (18.2, 29.7) | 15.9 | (11.5, 20.3) | 12.3 | (9.0, 15.5) | |
| 3 | 64.4 | (48.0, 80.8) | 59.5 | (47.6, 71.4) | 38.3 | (30.0, 46.6) | 32.3 | (26.7, 38.0) | 20.8 | (16.6, 25.0) | 22.4 | (19.2, 25.6) | |
| 2 | 147.4 | (131.0, 163.8) | 89.3 | (77.9, 100.7) | 53.7 | (46.2, 61.1) | 44.7 | (38.9, 50.6) | 21.8 | (17.5, 26.2) | 22.6 | (19.3, 25.9) | |
| 1 (lowest) | 110.9 | (96.2, 125.6) | 127.5 | (116.6, 138.5) | 62.7 | (55.6, 69.9) | 49.0 | (43.4, 54.5) | 30.5 | (26.5, 34.6) | 26.9 | (23.9, 29.9) | |
| referent | PAF | PAF | PAF | PAF | PAF | PAF | |||||||
| total | total, Q5 | 10.3% | (9.6%, 10.9%) | 13.4% | (12.7%, 14.2%) | 7.5% | (6.7%, 8.3%) | 6.1% | (5.3%, 6.9%) | 7.5% | (6.7%, 8.3%) | 9.5% | (8.7%, 10.3%) |
| white | white, Q5 | 7.2% | (6.5%, 7.9%) | 10.3% | (9.5%, 11.1%) | 4.6% | (3.7%, 5.5%) | 3.0% | (2.2%, 3.9%) | 5.5% | (4.6%, 6.3%) | 7.1% | (6.2%, 8.0%) |
| of color | white, Q5 | 54.1% | (53.6%, 54.6%) | 45.7% | (45.0%, 46.4%) | 38.7% | (37.9%, 39.6%) | 36.3% | (35.4%, 37.2%) | 33.5% | (32.6%, 34.4%) | 34.5% | (33.6%, 35.5%) |
Throughout, the magnitude of the socioeconomic gap for mortality unrelated to smoking was greater among the US populations of color compared to the US white population (Table 2a). Comparing the lowest to highest county income quintile, among the US populations of color, the IRR increased from 1.18 (95% 1.14, 1.21) in 1960 to 1.53 (95% CI 1.50, 1.55) in 2000, albeit dipping slightly to 1.38 (95% CI 1.36, 1.40) in 2006; for the white population, the corresponding IRR were 1.00 (95% 0.99, 1.01), 1.18 (95% CI 1.17, 1.19), and 1.16 (95% 1.15, 1.16). In 2006, the IRD among the four lower county income quintiles for the populations of color ranged from about 90 to 140 deaths per 100,000, differences far higher than the corresponding IRD for the white population (about 25 to 60 per 100,000) and nearly equal to the 2006 death rate for ischemic heart disease (134.9/100,000) for the total US population (Figure 1a).
Causes of death preventable by medical standards of the 1960s
Mortality rates for causes of death preventable by medical care standards of the 1960s fell sharply until about 1980, as did their socioeconomic IRR and IRD, after which rates continued to decline, albeit more slowly, and inequities stagnated (Figure 2b; Table 2b). Thus, until about 1980 APC declines on the order of 3.5 to 5% for this mortality rate were evident in each county income quintile, with the decline greatest in the poorer counties; starting in about 1980, however, the APC in each income quintile dropped to between 1 and 2%, and only in the mid-1990s again equalled the pre-1980 values. Similar temporal patterns were evident by race/ethnicity, even as the within-income quintile rates and the magnitude of the socioeconomic IRR and IRD were consistently higher for the US populations of color as compared to the white population. Consequently, in 2006 the IRD was 2 times higher among the US populations of color (26.9/100,000 (95% CI 23.9, 29.9) as compared to the white population (11.3/100,000 (95% CI 10.2, 12.3))(Table 2b). Moreover, despite declining rates and shrinking absolute socioeconomic gaps, in 2006 mortality rates for causes of death preventable by 1960s medical standards were 2 to 4 times higher, across income quintiles, than the corresponding mortality rates for the leading types of cancer (lung, breast, colorectal) and also mortality due to diabetes and to unintentional injuries (Figure 1a).
Population attributable fractions
Considering only the data for 2006 (Tables 2a and 2b), had all persons experienced the same age-specific mortality rates as persons in the most affluent county income quintile, 11.6% (95% CI 11.3, 12.0) of deaths unrelated to smoking (1-in-9) and 9.5% (95% CI 8.7, 10.3) of deaths preventable by 1960s standards of medical care (1-in-11) would not have occurred. The corresponding proportions, for analyses setting as referent the mortality of the white population in the most affluent counties, equalled: (a) for mortality unrelated to smoking: 9.2% (95% CI 8.8, 9.6), or 1-in-9, for the US white population and 19.5% (95% CI 19.0, 20.1), or 1-in-5, for the US populations of color; and (b) for mortality preventable by 1960s standards of medical care: 7.1% (95% CI 6.2, 8.0), or 1-in-14, and 34.5% (33.6, 35.5), or 1-in-3, respectively. Highlighting the disproportionate burden on the US populations of color, between 1960 and 2000, their PAFs never fell below 19% of deaths and reached to upwards of 50%.
DISCUSSION
Our results newly show that deaths due to causes unrelated to smoking and preventable by 1960s medical standards contribute substantially to US mortality rates and mortality inequities, with long-term trends indicating these inequities can shrink (as they did between 1960 and 1980) and need not inevitably rise (as they did after 1980). These findings not only counter current views that normalize growing social inequalities in health but also those which emphasize the centrality of smoking and high-tech medicine to temporal changes in health inequities.1–3 Our results instead clarify that not only is the patterning of these trends is historically contingent but also that in affluent countries, such as the US, social inequalities in mortality can both fall or rise even as overall mortality rates decline.
Study Limitations
Several study limitations should be considered before interpreting the results. Potential problems include data completeness and accuracy and also reliance on cross-sectional county-level data.1,4 Of particular concern are well-known issues affecting census population counts, death registration, and the quality of death certificate data,26,27 compounded by changes in coding of causes of death across the different editions of IDC-7 through ICD-10.9
Counterbalancing these caveats, US death registration was 99% complete by 1960,26 and any greater tendency to underestimate cause-specific death counts among lower income populations and populations of color would result in underestimating, not overestimating, cause-specific mortality rates in the lower county income quintiles – thereby reducing, not inflating, the observed cause-specific inequities. Additionally, the census undercount, also disproportionately affecting lower income populations and populations of color, has declined substantially over time,27 further reducing, not inflating, the more recent estimates of mortality inequities. Moreover, despite known problems with misclassification of race/ethnicity in US death certificates (chiefly affecting groups other than “white” and “black”),27 the broad yet conceptually valid categories we used – “white” and “of color” – minimizes the impact of this potential problem. It is thus unlikely that our findings are an artifact of flawed data.
That said, reliance on repeat cross-sectional county-level data – the only nationally representative data available for estimating US socioeconomic inequities in mortality preceding 19681,4 – precludes testing directly the causal impact of county income level on county mortality rates. Suggesting, however, that our findings are unlikely to be unduly biased by ecologic fallacy, the direction and magnitude of the socioeconomic inequities we observed for all-cause mortality (Figure 1) are consistent with those of two extant studies based on data from individual-records, one extending back to 1967,28 and the other to 1980.2 Additionally, a related county-level study of trends in mortality disparities found that taking into account county migration data did not alter results.1
Implications
To interpret our data, we begin by emphasizing that our findings in no way counter the essential efforts needed to: (1) reduce mortality rates and inequities due to tobacco,10 and (2) support medical innovation.29 Indeed, the rising proportion of US deaths unrelated to smoking (Figure 3) stands as testimony to critical gains in reducing smoking-related deaths.10 That said, our results nevertheless point to the importance of tracking trends in mortality unrelated to smoking and due to lack of access to basic medical care. Additionally, the observed patterns of shrinking then rising socioeconomic inequities in both outcomes are broadly consistent with “U-turn” hypotheses pointing to the impacts of 1980s policy reversals, contrasting mid-1960s and 1970s policies that prioritized government-led initiatives promoting social, medical, occupational, and environmental justice and protection, versus post-1980 policies that that prioritized privatization and deregulation and undercut enforcement of civil rights and affirmative action.4,30–32 Testing of such hypotheses will require detailed long-term macro- and individual-level data.
More specific to the US, our findings also call attention to an under-recognized phenomenon: the larger absolute and relative socioeconomic inequities in the mortality among the US populations of color compared to the US white population. Reflecting the much greater racial/ethnic gaps in mortality among those in the most economically deprived as compared to most affluent county income quintiles, these results underscore that US efforts to reduce socioeconomic inequalities in health cannot afford to be “colorblind,” even as some new policy narratives assert the US has entered a “post-racial” period, ushered in by the mid-1960s enactment of civil rights and cemented by the 2008 election of President Obama.33,34
In summary, our results show that US socioeconomic inequities in death unrelated to smoking and preventable by basic medical care have shrunk and risen, with absolute rates on par with leading causes of death, and with the burden worst for US populations of color. None of these findings can be attributed to trends in smoking-related deaths and access to high-tech medicine.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Jacob Bor (doctoral student, Harvard School of Public Health) for his work, as a paid research assistant, in harmonizing the ICD codes used in these analyses (permission for this acknowledgement obtained in writing on October 5, 2010).
Funding: This work was supported by the National Institutes of Health/National Cancer Institute (NIH/NCI) grant R03CA137666. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Biographies
Nancy Krieger is Professor, Department of Society, Human Development and Health, Harvard School of Public Health (HSPH), Co-Director of the HSPH Interdisciplinary Concentration on Women, Gender, and Health, and co-founder and chair of the Spirit of 1848 Caucus of APHA. A social epidemiologist, she received her PhD in Epidemiology from University of California Berkeley in 1989; her background includes biochemistry, philosophy of science, and the history of public health, plus 25 years of engagement in issues involving social justice, science and health. A recipient of numerous NIH-funded grants (by NCI, NIA, NICHD, NHLBI, and OBSSR), her work focuses on etiology of, monitoring, and theories to explain population distributions of disease and inequities in health, including development of the ecosocial theory of disease distribution which she first proposed in 1994 and has elaborated since. Her most recent book is: Epidemiology and The People’s Health: Theory and Context (Oxford University Press, 2011); she has also edited: Embodying Inequality: Epidemiologic Perspectives (Baywood Publishing Co, 2004) and co-edited, with Elizabeth Fee, Women’s Health, Politics, and Power: Essays on Sex/Gender, Medicine, and Public Health (Baywood Publishing Co., 1994) and, with Glen Margo, AIDS: The Politics of Survival (Baywood Publishing Co., 1994).
Jarvis Chen, ScD, is a Research Scientist based in the Department of Society, Human Development and Health at the Harvard School of Public Health. A social epidemiologist by training, he received his ScD from the Harvard School of Public Health in 2001. Dr. Chen’s research focuses on racial/ethnic and socioeconomic disparities in health and the development of innovative methodologies for modeling health disparities in complex datasets. He is currently PI for the NIOSH funded study “Work, Neighborhoods, Commuting, and Occupational Health Disparities” (R03 OH009338-02) and for the NIH funded study “Socioeconomic Adjustment of Racial Disparities in Lung Cancer Relative Survival,” part of the Lung Cancer Disparities Center at HSPH (1 P50 CA148506-01).
Anna Kosheleva, MS, is a data manager in the Department of Society, Human Development and Health at the Harvard School of Public Health. She received her MS in math and statistics in 1993 from Ural State University in Yekaterinburg, Russia. Ms. Kosheleva has more than 10 years of experience in data management and data analysis in public health, with studies spaning from environmental to social epidemiology.
Pamela D. Waterman, MPH, is a Project Director at the Department of Society, Human Development and Health at the Harvard School of Public Health. She received her MPH in Epidemiology from Columbia University in 1997; her expertise is in project management, database construction and management, data analysis, and geocoding. Ms. Waterman is currently Project Director for 5 NIH-funded projects: “Racial Discrimination & Risk of Chronic Disease” (5R01AG027122-03; PI: Krieger); “Cancer and Changing Trends in US Mortality Inequities: 1960–2004” (1R03CA137666001A1; PI: Krieger); “Exploring Trends in US Health Inequities in Context: NHES to NHANES, 1959–2006” (1R21HD060828-01A2; PI: Krieger); “Work, Neighborhood, Commuting and Occupational Health Disparities” (1R03OH009338-02; PI: Chen); and “Socioeconomic Adjustment of Racial Disparities in Lung Cancer Relative Survival” (1P50CA148596-01; Ctr PI: Williams; Project PI: Chen).
Footnotes
Conflict of interest: None to declare.
AUTHOR CONTRIBUTIONS:
NK conceived the study, oversaw obtaining the data and conducting the analyses, interpreted the data, and wrote the first draft of the manuscript; JTC conducted the analyses, prepared the figures, and contributed to interpreting the data and writing the manuscript; AK assisted with the data analysis and contributed to interpreting the data and writing the manuscript; PDW assisted with obtaining the data and the data analyses and contributed to interpreting the data and writing the manuscript.
Contributor Information
Nancy Krieger, Department of Society, Human Development and Health (SHDH), Harvard School of Public Health (HSPH), Boston, MA, USA.
Jarvis T. Chen, SHDH, HSPH, Boston, MA, USA.
Anna Kosheleva, SHDH, HSPH, Boston, MA, USA.
Pamela D. Waterman, SHDH, HSPH, Boston, MA, USA.
REFERENCES
- 1.Ezzati M, et al. The reversal of fortunes: trends in county mortality and cross-county mortality disparities in the United States. PLoS Med. 2008;5:e66. doi: 10.1371/journal.pmed.0050066. Erratum. PLoS Med 5(5), 2008, doi: 10.1371/journal.pmed.0050119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meara ER, Richards S, Cutler DM. The gap gets bigger: changes in mortality and life expectancy, by education, 1981–2000. Health Affairs. 2008;27:350–360. doi: 10.1377/hlthaff.27.2.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crimmins EM, Preston SH, Cohen B, editors. Panel on Understanding Divergent Trends in Longevity in High-Income Countries, National Research Council. Washington, DC: National Academies Press; 2011. Explaining Divergent Levels of Longevity in High-Income Countries. [PubMed] [Google Scholar]
- 4.Krieger N, et al. The fall and rise of US inequities in premature mortality: 1960–2002. PLoS Med. 2008;5(2):e 46. doi: 10.1371/journal.pmed.0050046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Preston S, Elo IT. Are educational differences in adult mortality increasing in the United States? J Aging Health. 1995;7:476–496. doi: 10.1177/089826439500700402. [DOI] [PubMed] [Google Scholar]
- 6.Krieger N. Epidemiology and the People’s Health: Theory and Context. New York: Oxford University Press; 2011. [Google Scholar]
- 7.Documentation of the Detail Mortality Tape File (1959–1961, 1962–1967) Washington, DC: US Department of Health, Education, and Welfare; 1969. National Office of Vital Statistics, Public Health Service, US Department of Health, Education and Welfare. [Google Scholar]
- 8.National Center for Health Statistics (NCHS) [July 11, 2011];Compressed Mortality Files. http://www.cdc.gov/nchs/data_access/cmf.htm.
- 9.World Health Organization (WHO) International Classification of Diseases (ICD) [July 11, 2011]; http://www.who.int/classifications/icd/en/
- 10.US Centers for Disease Control and Prevention. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. MMWR. 2008;57:1226–1228. [PubMed] [Google Scholar]
- 11.Charlton JRH, et al. Geographical variation in mortality from conditions amenable to medical intervention in England and Wales. Lancet. 1983;i:691–696. doi: 10.1016/s0140-6736(83)91981-5. [DOI] [PubMed] [Google Scholar]
- 12.Charlton JRH, Velez R. Some international comparisons of mortality amenable to medical intervention. Br Med J. 1986;292:295–301. doi: 10.1136/bmj.292.6516.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwartz E, et al. Black/white comparisons of deaths preventable by medical intervention: United States and the District of Columbia 1980–1986. Int J Epidemiol. 1990;19:591–598. doi: 10.1093/ije/19.3.591. [DOI] [PubMed] [Google Scholar]
- 14.Simonato L, et al. Avoidable mortality in Europe 1955–1994: a plea for prevention. J Epidemiol Community Health. 1998;52:624–630. doi: 10.1136/jech.52.10.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.GeoLytics Census Reference Package. Nation 1 (2002) CRP Census CD 1970 (ver 2.0), CensusCD 1980 (ver 2.5), CensusCD 1990 + Maps (ver 4.1), 2000 Long Form DVD Upgrade (ver 2.2) New Brunswick, NJ: GeoLytics; 2011. [July 11, 2011]. http://www.geolytics.com/USCensus,Census-Research-Package,Products.asp. [Google Scholar]
- 16.US Census Bureau. [July 11, 2011];US decennial census data: 1980, 1990, 2000. http://www.census.gov/
- 17.US Census Bureau. [July 11, 2011];Historical income tables for counties. http://www.census.gov/hhes/www/income/data/historical/county/county1.html.
- 18.US Department of Labor, Bureau of Labor Statistics. [July 11, 2011];Consumer Price Indexes. http://www.bls.gov/cpi/home.htm.
- 19.Shaw M, et al. The Handbook of Inequality and Socioeconomic Position: Concepts and Measures. Bristol: Policy Press; 2007. [Google Scholar]
- 20.Mays VM, et al. Classification of race and ethnicity: implications for public health. Annu Rev Public Health. 2003;24:83–110. doi: 10.1146/annurev.publhealth.24.100901.140927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Du Bois WEB. With a foreword by Charles Lemert; an introduction by Manning Marable; and an afterword by Cheryl Townsend Gilkes. 100th Anniversary ed. Boulder, Colorado: Paradigm; LIII; 1904/2004. The Souls of Black Folk. [Google Scholar]
- 22.Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Report. 1998;37(3) [PubMed] [Google Scholar]
- 23.SAS Institute. SAS 9/1/3: Language Reference Dictionary. Fifth Edition. Cary, NC: SAS Institute; 2002–2006. [Google Scholar]
- 24.Greenland S, Drescher K. Maximum likelihood estimation of the attributable fraction from logistic models. Biometrics. 1993;49:865–872. Stable URL: http://www.jstor.org/stable/2532206. [PubMed] [Google Scholar]
- 25.Kim HJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–351. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 26.Hetzel AM. History and Organization of the Vital Statistics System. Bethesda, MD: National Center for Health Statistics; 1997. [Google Scholar]
- 27.Rosenberg HM, et al. Quality of death rates by race and Hispanic origin: a summary of current research, 1999. Vital Health Stat. 1999;128(2):1–13. [PubMed] [Google Scholar]
- 28.Schalick LM, et al. The widening gap in death rates among income groups in the United States from 1967 to 1986. Int J Health Services. 2000;30:13–26. doi: 10.2190/8QMH-4FAB-XAWP-VU95. [DOI] [PubMed] [Google Scholar]
- 29.Medical Innovation in the Changing Healthcare Marketplace: Conference Summary. Washington, DC: National Academy Press; 2002. Institute of Medicine, Board on Science, Technology, and Economic Policy. [PubMed] [Google Scholar]
- 30.Beckfield J, Krieger N. Epi + demos + cracy: linking political systems and priorities to the magnitude of health inequities – evidence, gaps, and a research agenda. Epidemiol Review. 2009;31:152–177. doi: 10.1093/epirev/mxp002. [DOI] [PubMed] [Google Scholar]
- 31.Navarro V, editor. Neoliberalism, Globalization, and Inequalities: Consequences for Health and Quality of Life. Amityville, NY: Baywood Pub. Co.; 2007. [Google Scholar]
- 32.Navarro V, Muntaner C, editors. Political and Economic Determinants of Population Health and Well-Being: Controversies and Developments. Amityville, NY: Baywood Pub. Co.; 2004. [Google Scholar]
- 33.Fritz C, Stone J. A post-racial America: myth or reality? Ethnic Racial Studies. 2009;32:1083–1088. [Google Scholar]
- 34.Wise T. Colorblind: The Rise of Post-Racial Politics and the Retreat from Racial Equality. San Francisco: City Light Books; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.