Abstract
Rationale: The incidence of intensive care unit (ICU) readmissions across the United States is unknown.
Objectives: To determine incidence of ICU readmissions in United States hospitals, and describe the distribution of time between ICU discharges and readmissions.
Methods: This retrospective cohort study used 196,202 patients in 156 medical and surgical ICUs in 106 community and academic hospitals participating in Project IMPACT from April 1, 2001, to December 31, 2007. We used mixed-effects logistic regression, adjusting for patient and hospital characteristics, to describe how ICU readmission rates differed across patient types, ICU models, and hospital types.
Measurements and Main Results: Measurements consisted of 48- and 120-hour ICU readmission rates and time to readmission. A total of 3,905 patients (2%) were readmitted to the ICU within 48 hours, and 7,171 (3.7%) within 120 hours. In adjusted analysis, there was no difference in ICU readmissions across patient types or ICU models. Among medical patients, those in academic hospitals had higher odds of 48- and 120-hour readmission than patients in community hospitals without residents (1.51 [95% confidence interval, 1.12–2.02] and 1.63 [95% confidence interval, 1.24–2.16]). Median time to ICU readmission was 3.07 days (interquartile range, 1.27–6.58). Closed ICUs had the longest times to readmission (3.55 d [interquartile range, 1.42–7.50]).
Conclusions: Approximately 2% and 4% of ICU patients discharged to the ward are readmitted within 48 and 120 hours, within a median time of 3 days. Medical patients in academic hospitals are more likely to be readmitted than patients in community hospitals without residents. ICU readmission rates could be useful for policy makers and investigations into their causes and consequences.
Keywords: ICU readmissions, quality indicators, hospital trends
At a Glance Commentary
Scientific Knowledge on the Subject
There is interest in using intensive care unit (ICU) readmissions as an ICU quality indicator, yet little is known about the incidence, timing, and risk factors for readmission.
What This Study Adds to the Field
This study provides risk-adjusted rates of ICU readmissions across different patient, ICU, and hospital types in the United States. It also describes the timing of ICU readmissions, and patient, ICU, and hospital risk factors associated with readmission.
Intensive care unit (ICU) readmissions are associated with mortality, cost, and length of stay (1–9). They may also capture a component of hospital efficiency through optimal patient flow management (2, 5, 10), and have been proposed as an appropriate measure of the quality of ICU care (11). However, little is known regarding the epidemiology of ICU readmissions in the United States: how commonly they occur, when, and where they occur, or whether rates have changed over time. Past studies in small numbers of ICUs (2, 5, 8, 10, 12–21) using heterogeneous definitions of ICU readmission have estimated rates from 4.6–13.4%, and a recent larger study in Australia examined patient risk factors for ICU readmission (22). Thus, although ICU readmission rate is a promising measure for assessing patient triage decisions and ICU performance, its use as a quality metric depends on a better understanding of their incidence and the hospital-level factors associated with their occurrence.
In the present study we used a large and diverse sample of United States ICUs to assess differences in ICU readmission incidence rates among different ICU and hospital types; the distribution of time between ICU discharges and readmissions; and patient, ICU, and hospital variables associated with readmission. We hypothesized that after adjusting for patient, ICU, and hospital characteristics, patients hospitalized in ICUs located in academic hospitals and in closed ICUs would have comparable predicted rates of ICU readmission compared with those hospitalized in community hospitals and open ICUs not requiring intensivist consultation. Some of these results have been previously reported in the form of an abstract (23).
Methods
Data Source
We performed a retrospective cohort study using the Project IMPACT database (Cerner Corporation, Kansas City, MO). Project IMPACT is a nationally representative, voluntary, fee-based ICU clinical information system used for benchmarking and research (24–34). Each ICU uses a trained data collector and a standardized web-based instrument to collect data regarding individual patients, care processes, and ICU structural characteristics (27).
Patients and Variables
Eligible patients were admitted to ICUs from April 1, 2001, to December 31, 2007. We compared patients discharged alive to a hospital ward from the ICU later readmitted at least once with those never readmitted, adjusting for patient characteristics at the time of first ICU admission. Patients dying during the initial ICU stay were excluded. Our primary definition of ICU readmission excluded patients discharged from one ICU and subsequently readmitted to a different ICU because readmissions to other ICUs are more likely to be elective rather than related to care in the initial ICU. To enhance comparability of our results to several prior studies (2, 5, 8, 10, 12–22) we included readmissions to other ICUs in secondary analyses.
To preserve independence between observations, we examined only first ICU readmissions. We excluded patients who were (1) ineligible to receive an Mortality Prediction Model III (MPM0-III) severity of illness score (30), (2) less than 18 years of age, (3) admitted to ICUs with less than 10 patients in a given year or that provided data for less than 12 consecutive months, (4) discharged from the ICU with documented limitations on life support beyond simple do-not-resuscitate orders, (5) discharged in a “moribund” condition, or (6) died after ICU discharge before they could be readmitted to an ICU within either 48 or 120 hours of ICU discharge. We also excluded patients admitted to government hospitals because of limited sample sizes.
Statistical Analyses
We evaluated ICU readmission within 48 and 120 hours (3). We chose 48 hours because proximate readmissions may be most likely attributable to ICU care or triage decisions (11, 35). By contrast, readmissions after 120 hours may be more likely elective or caused by events occurring on the floor after discharge. Patient and ICU characteristics were described using means or percentages, and compared across outcome groups using mixed-effects logistic regression models with ICU-specific random intercepts. Covariates were included in final models based on prespecified scientific plausibility (8, 10, 12–14, 36–39), or associations with the outcomes with an odds ratio (OR) of more than 1.2 or less than 0.8 accompanied by a P value of less than 0.0001 chosen because of large sample size. Backward elimination techniques were used to create a parsimonious final model. Patient variables included age (<65, 65–74, 75–84, ≥85); race (black, white, other); discharge time (6 am–12 pm, 12 pm–6 pm, 6 pm–6 am); ICU occupancy within 2 hours of ICU discharge (less than or equal to one open bed versus more than one open bed); and length of ICU stay. We used a piecewise linear polynomial to model associations with patient severity of illness, using the MPM0-III (30).
Four sets of analyses were conducted. First, diagnoses were examined among readmitted patients on index ICU admission and first readmission to estimate the proportion of patients who were readmitted for new versus unresolved problems. For this purpose, approximately 50 primary diagnoses were grouped into nine categories (see Table E1 in the online supplement). Second, to test whether ICU readmission rates differed across patient, hospital, and ICU types, we examined the relationship between 48- and 120-hour ICU readmission rates and these variables. Patient type (elective surgical, emergency surgical, or medical) was the primary exposure. ICU model was closed, mandatory intensivist consult, optional intensivist consult, or no consult available. The last two categories were combined because of small sample size in the latter category (40, 41). Hospital types included academic, community with residents during the day, or community without residents.
To examine the independent effects of ICU model, hospital type, and patient type on ICU readmission rates, we examined the distribution of the rates of 48- and 120-hour readmission across different types of patients, hospitals, and ICU models, while adjusting for patient, ICU, and hospital characteristics. Multivariable mixed-effects logistic regression models with ICU-specific random-intercepts were used (42) for all models. Hospital type and ICU model were modeled as interaction terms with patient type. We used postestimation to obtain expected probabilities of ICU readmission for each patient type within each ICU model or hospital type (43); Wald tests to compare ICU readmission odds across patient, ICU, and hospital types; and a Holm correction to adjust for multiple comparisons.
The third analysis compared the distribution of time between ICU discharge and readmission using a histogram among different patient, hospital, and ICU types using Wilcoxon rank sum tests, adjusting for multiple comparisons using the Holm test.
The fourth analysis examined hospital, ICU, and patient characteristics associated with readmission, and changes in ICU readmission rates April 1, 2001, to December 31, 2007, compared with the reference year of 2007, and presents P values following Holm adjustments for multiple comparisons. This model included ICU and hospital variables not included in other analyses because of failure to meet selection criteria described previously. We tested model discrimination using the C statistic, or area under the receiver operating characteristic curve (44).
All analyses were performed using STATA 11.2 (StataCorp, College Station, TX).
Results
Description of Participating ICUs and Patients
The dataset initially contained 365,968 admissions in 192 ICUs. The exclusions are shown in Figure E1. Because MPM0-III has not been validated in coronary (n = 16,388), cardiac surgery (n = 22,920), and burn patients (n = 385), they were excluded from the analysis, as were patients missing variables needed to compute an MPM0-III score (n = 1,625). A total of 196,250 eligible patients were discharged from study ICUs. The final analytic datasets included 195,202 patients eligible for readmission within 48 hours, and 194,028 patients eligible for readmission within 120 hours. These patients derived from 156 ICUs in 106 hospitals.
Overall Readmission Rates
Among 196,250 eligible patients, 3,905 (2%) were readmitted within 48 hours; 7,171 (3.7%) within 120 hours; and 10,608 (5.4%) within 21 days of discharge. A total of 389 patients readmitted within 48 hours (10%) were readmitted more than once. The median 48- and 120-hour readmission rates were 1.8% (interquartile range [IQR], 1.1–2.4%, max 5.4%) and 3.2% (IQR, 2.2–4.4%, max 9.8%), respectively. Among patients admitted to an ICU, 8.6% died during their initial ICU stay; 5% died in the hospital subsequent to initial ICU discharge; and 86.4% survived hospitalization. Comparing never-readmitted patients with those readmitted within 48 hours, 3.7% versus 20.7% died in the hospital after ICU discharge, 64.4% versus 36.6% were discharged home, and median hospital length of stay was 8 versus 15 days, respectively (all P values < 0.001).
During the index ICU admission, patients who were readmitted within 48 hours had higher index admission MPM scores (13.1 vs. 10.9; P < 0.001) (Table 1). Patients requiring mechanical ventilation were more likely to be readmitted than those not requiring it (1.8% vs. 2.5%; P < 0.001), as were patients with comorbidities, such as chronic cardiovascular disease (2% vs. 2.2%; P < 0.001), chronic respiratory disease (1.9% vs. 2.8%; P < 0.001), and baseline serum creatinine greater than 2 mg/dl (1.9% vs. 2.7%; P < 0.001). Patients hospitalized in academic hospitals (Table 2) (academic, 2.4% vs. community without residents, 1.6%; P = 0.008) were more likely to be readmitted, as were patients discharged during the afternoon or night (morning, 1.6% vs. afternoon, 2% [P = 0.003], vs. night, 2.2% [P < 0.001]). Readmitted patients had longer ICU lengths of stay (4.3 vs. 3.4 d) during their first ICU admission than patients never readmitted.
TABLE 1.
ADJUSTED PATIENT CHARACTERISTICS ASSOCIATED WITH ICU READMISSION
| Patient Characteristics at the Time of First ICU Admission | Bivariable Models, 48-h Readmissions |
Multivariable Models |
|||||
| % Not Readmitted | % Readmitted | 48-h Readmissions |
120-h Readmissions |
||||
| Number of patients, n | 191,308 | 3,894 | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value |
| Age | |||||||
| <65 | 98.2 | 1.8 | — | Reference | Reference | ||
| 65–74 | 97.8 | 2.3 | <0.001 | 1.07 (0.96–1.20) | 0.438 | 1.07 (0.99–1.16) | 0.332 |
| 75–84 | 97.6 | 2.4 | <0.001 | 1.14 (1.01–1.29) | 0.088 | 1.07 (0.98–1.17) | 0.258 |
| ≥85 | 98.0 | 2.0 | 0.004 | 1.02 (0.86–1.21) | 0.791 | 0.95 (0.84–1.08) | 0.459 |
| Race/ethnicity, % | |||||||
| Black | 98.2 | 1.8 | — | Reference | Reference | ||
| White | 97.9 | 2.1 | 0.003 | 1.13 (1.02–1.27) | 0.052 | 1.18 (1.08–1.28) | <0.001 |
| Other or missing | 98.3 | 1.7 | 0.155 | 0.96 (0.81–1.13) | 0.584 | 0.95 (0.84–1.07) | 0.411 |
| Sex | |||||||
| Females | 98.1 | 1.9 | — | Not included in multivariable models | |||
| Males | 97.9 | 2.1 | 0.036 | ||||
| Functional status | |||||||
| Independent | 98.1 | 1.9 | — | Reference | Reference | ||
| Partially dependent | 97.6 | 2.4 | <0.001 | 1.14 (1.04–1.25) | 0.006 | 1.22 (1.14–1.31) | <0.001 |
| Fully dependent | 97.3 | 2.7 | <0.001 | 1.32 (1.14–1.52) | <0.001 | 1.48 (1.34–1.65) | <0.001 |
| Insurance | |||||||
| Private | 98.3 | 1.8 | — | Reference | Reference | ||
| Medicare | 97.8 | 2.3 | <0.001 | 1.06 (0.96–1.18) | 0.534 | 1.06 (0.98–1.14) | 0.349 |
| Medicaid | 98.0 | 2.1 | 0.034 | 1.16 (1.01–1.33) | 0.120 | 1.14 (1.03–1.26) | 0.036 |
| Self-pay | 98.6 | 1.4 | 0.001 | 0.85 (0.73–1.00) | 0.140 | 0.83 (0.74–0.93) | 0.008 |
| Other | 97.9 | 2.1 | 0.522 | 1.05 (0.84–1.31) | 0.660 | 0.92 (0.77–1.10) | 0.349 |
| Avg. MPM0-III admission score | 10.9 (11.9) | 13.1 (12.7) | <0.001* | ||||
| Probability death >0.2 | 1.01 (0.98–1.04) | 0.551 | 1.00 (0.98–1.02) | 0.966 | |||
| Probability death 0.05–0.2 | 0.99 (0.97–1.00) | 0.051 | 0.99 (0.98–0.99) | 0.004 | |||
| Probability death <0.05 | 0.97 (0.95–0.98) | <0.001 | 0.97 (0.95–0.98) | <0.001 | |||
| Patient had critical care consult | 1.27 (1.15–1.40) | <0.001 | 1.27 (1.17–1.37) | <0.001 | |||
| No | 98.4 | 1.6 | |||||
| Yes | 97.7 | 2.3 | <0.001 | ||||
| Required pressor use | Not included in multivariable models | ||||||
| No | 98.2 | 1.9 | — | ||||
| Yes | 97.2 | 2.8 | <0.001 | ||||
| Required mechanical ventilation | 0.81 (0.69–0.95) | 0.010 | 0.85 (0.76–0.97) | 0.007 | |||
| No | 98.2 | 1.8 | — | ||||
| Yes | 97.5 | 2.5 | <0.001 | ||||
| Avg. duration days between extubation and ICU discharge | 2.1 (1.6) | 2.3 (2.2) | <0.001† | 1.17 (1.04–1.30) | 0.006 | 1.09 (1.00–1.18) | 0.038 |
| Avg. # days mechanical ventilation | 4.1 (6.3) | 4.9 (7.1) | <0.001† | 1.12 (1.02–1.23) | 0.013 | 1.05 (0.98–1.12) | 0.131 |
| Avg. # comorbidities | 0.41 (0.73) | 0.52 (0.82) | <0.001 | Not included in multivariable models | |||
| Chronic gastrointestinal disease | 97.7 | 2.3 | 0.027 | Not included in multivariable models | |||
| Chronic cardiovascular disease | 97.8 | 2.2 | <0.001 | ||||
| Chronic respiratory disease | 97.1 | 2.9 | <0.001 | 1.29 (1.14–1.47) | <0.001 | 1.31 (1.19–1.44) | <0.001 |
| Chronic hemo/peritoneal dialysis | 97.4 | 2.7 | <0.001 | 1.25 (1.07–1.45) | 0.005 | 1.24 (1.10–1.39) | <0.001 |
| Chronic immunosuppression | 96.8 | 3.2 | <0.001 | 1.50 (1.20–1.87) | <0.001 | 1.35 (1.14–1.61) | <0.001 |
| Chronic HIV | 97.4 | 2.6 | 0.125 | Not included in multivariable models | |||
| Cancer with proved metastasis | 97.8 | 2.2 | 0.325 | ||||
| Baseline serum creatinine >2 mg/dl | 97.3 | 2.7 | <0.001 | ||||
| Hematogenous cancer | 96.9 | 3.1 | 0.028 | ||||
| Lymphoma | 98.0 | 2.0 | 0.843 | ||||
| Solid organ tumor | 97.6 | 2.4 | 0.015 | 1.15 (1.02–1.30) | 0.028 | 1.17 (1.07–1.29) | <0.001 |
| Avg. length of ICU stay | 3.41 (4.84) | 4.28 (6.06) | <0.001† | 1.00 (0.91–1.09) | 0.993 | 1.17 (1.10–1.25) | <0.001 |
| Source of ICU admission | |||||||
| Emergency department | 98.2 | 1.8 | — | Reference | Reference | ||
| Direct admission | 97.7 | 2.3 | 0.001 | 1.15 (0.99–1.32) | 0.319 | 1.20 (1.07–1.33) | 0.006 |
| General care floor | 97.2 | 2.8 | <0.001 | 1.37 (1.23–1.52) | <0.001 | 1.42 (1.31–1.54) | <0.001 |
| Step-down unit | 97.6 | 2.4 | 0.008 | 1.09 (0.89–1.33) | 1.000 | 1.24 (1.07–1.43) | 0.018 |
| Procedure | 98.2 | 1.8 | 0.501 | 1.06 (0.92–1.23) | 1.000 | 1.10 (0.99–1.22) | 0.156 |
| SNF, rehab, LTAC | 97.5 | 2.5 | 0.050 | 1.16 (0.77–1.75) | 0.948 | 1.35 (1.01–1.80) | 0.121 |
| Other | 97.3 | 2.7 | <0.001 | 0.91 (0.68–1.22) | 0.526 | 0.95 (0.76–1.18) | 0.615 |
| ICU destination | |||||||
| Floor | 98.3 | 1.7 | — | Reference | Reference | ||
| Step-down unit | 97.5 | 2.5 | <0.001 | 1.42 (1.33–1.53) | <0.001 | 1.37 (1.29–1.44) | <0.001 |
| Patient type | |||||||
| Elective surgery | 98.3 | 1.7 | — | Reference | Reference | ||
| Emergency surgery | 97.7 | 2.3 | <0.001 | 1.07 (0.94–1.22) | 0.620 | 1.10 (1.00–1.21) | 0.096 |
| Medical | 97.9 | 2.1 | <0.001 | 1.02 (0.88–1.19) | 0.760 | 0.97 (0.87–1.09) | 0.636 |
| DNR status at ICU discharge | |||||||
| Full code | 98.5 | 1.5 | — | Reference | Reference | ||
| No cardiopulmonary resuscitation | 98.0 | 2.0 | <0.001 | 1.82 (1.53–2.17) | <0.001 | 1.99 (1.73–2.28) | <0.001 |
| Discharge time | |||||||
| Morning (6 a.m.–12 p.m.) | 98.4 | 1.6 | — | Reference | Reference | ||
| Afternoon (12 p.m.–6 p.m.) | 98.0 | 2.0 | 0.003 | 1.17 (1.03–1.32) | 0.015 | 1.12 (1.02–1.23) | 0.016 |
| Night (6 p.m.–6 a.m.) | 97.8 | 2.2 | <0.001 | 1.20 (1.05–1.37) | 0.012 | 1.13 (1.03–1.25) | 0.022 |
| ICU occupancy within 2 h of discharge | |||||||
| >1 bed available | 98.1 | 1.9 | — | Reference | Reference | ||
| ≤1 bed available | 97.9 | 2.1 | 0.920 | 0.98 (0.90–1.08) | 0.739 | 1.01 (0.95–1.09) | 0.648 |
Definition of abbreviations: CI = confidence interval; DNR = do-not-resuscitate; ICU = intensive care unit; LTAC = long-term acute care hospital; MPM0-III = Mortality Prediction Model III; OR = odds ratio; SNF = skilled nursing facility.
P values are from mixed-effects regression models with ICU-specific random intercepts.
Variables in bivariable analysis that were not also in multivariable analysis either did not meet criteria for inclusion in the multivariable model, or did alter model fit and were not important confounders.
All P values reflect Holm adjustment for multiple comparisons.
Month of initial ICU admission and hospital region are also included in the model.
Modeled as piecewise linear polynomial.
Natural log transformed.
TABLE 2.
ADJUSTED HOSPITAL AND ICU CHARACTERISTICS ASSOCIATED WITH ICU READMISSION
| Hospital and ICU Characteristics at the Time of First ICU Admission | % Not Readmitted | % Readmitted | 48-h Readmissions |
120-h Readmissions |
|||
| (n = 191,308) | (n = 3,894) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Year | |||||||
| 2001 | 98.5 | 1.6 | 0.068 | 0.96 (0.80–1.15) | 0.669 | 1.03 (0.90–1.19) | 1.000 |
| 2002 | 98.1 | 1.9 | 0.703 | 1.13 (0.97–1.31) | 0.493 | 1.13 (1.01–1.27) | 0.144 |
| 2003 | 98.0 | 2.0 | 0.435 | 1.16 (1.01–1.34) | 0.226 | 1.14 (1.02–1.27) | 0.094 |
| 2004 | 97.9 | 2.1 | 0.477 | 1.13 (0.99–1.30) | 0.331 | 1.14 (1.03–1.26) | 0.068 |
| 2005 | 97.9 | 2.1 | 0.319 | 1.10 (0.96–1.26) | 0.490 | 1.09 (0.99–1.21) | 0.268 |
| 2006 | 97.9 | 2.1 | 0.470 | 1.08 (0.95–1.24) | 0.486 | 1.02 (0.92–1.12) | 0.763 |
| 2007 | 98.0 | 2.0 | — | Reference | Reference | ||
| Fellowship programs | |||||||
| No program | 98.3 | 1.8 | — | Reference | Reference | ||
| Primary fellowship site | 97.5 | 2.5 | 0.002 | 1.36 (1.00–1.84) | 0.049 | 1.34 (1.01–1.78) | 0.044 |
| Residency programs | Not included in multivariable models | ||||||
| No residents | 98.3 | 1.7 | — | ||||
| Residents | 97.8 | 2.2 | 0.038 | ||||
| Hospital location | |||||||
| Urban | 98.0 | 2.0 | — | Reference | Reference | ||
| Suburban | 98.1 | 1.9 | 0.629 | 0.95 (0.78–1.15) | 0.594 | 0.98 (0.81–1.17) | 0.802 |
| Rural | 97.7 | 2.3 | 0.138 | 1.32 (1.02–1.70) | 0.071 | 1.20 (0.95–1.53) | 0.268 |
| ICU night coverage | |||||||
| Critical care attending | 98.1 | 1.9 | — | Reference | Reference | ||
| Other attending | 98.1 | 1.9 | 0.282 | 1.21 (1.00–1.46) | 0.198 | 1.17 (0.99–1.37) | 0.248 |
| Fellow | 97.1 | 2.9 | 0.032 | 1.34 (0.96–1.87) | 0.266 | 1.25 (0.92–1.69) | 0.300 |
| Resident | 98.0 | 2.0 | 0.154 | 1.22 (0.96–1.53) | 0.195 | 1.13 (0.92–1.39) | 0.237 |
| Other | 98.3 | 1.7 | 0.642 | 0.77 (0.54–1.08) | 0.132 | 0.77 (0.57–1.04) | 0.272 |
| # ICU beds | |||||||
| 4–12 | 98.4 | 1.6 | — | Reference | Reference | ||
| 13–15 | 98.0 | 2.0 | 0.393 | 1.20 (0.95–1.51) | 0.265 | 1.17 (0.95–1.44) | 0.395 |
| 16–18 | 97.8 | 2.3 | 0.015 | 1.18 (0.97–1.44) | 0.315 | 1.13 (0.94–1.35) | 0.386 |
| 19–24 | 97.9 | 2.1 | 0.001 | 1.27 (1.03–1.56) | 0.010 | 1.35 (1.12–1.62) | 0.006 |
| 25–66 | 97.8 | 2.2 | 0.606 | 1.03 (0.79–1.36) | 0.807 | 1.04 (0.81–1.34) | 0.761 |
| # hospital beds | |||||||
| 70–341 | 98.1 | 1.9 | — | Reference | Reference | ||
| 346–426 | 98.0 | 2.0 | 0.246 | 0.86 (0.67–1.11) | 0.261 | 0.82 (0.64–1.04) | 0.096 |
| 450–462 | 97.8 | 2.2 | 0.216 | 0.72 (0.53–0.97) | 0.059 | 0.61 (0.46–0.81) | 0.002 |
| 563–795 | 98.3 | 1.7 | 0.049 | 0.62 (0.47–0.82) | 0.003 | 0.57 (0.44–0.75) | <0.001 |
| 838–1,389 | 97.8 | 2.2 | 0.46 | 0.66 (0.48–0.93) | 0.051 | 0.64 (0.46–0.88) | 0.012 |
| ICU model | |||||||
| Optional consult or no consult | 98.2 | 1.8 | — | Reference | Reference | ||
| Mandatory intensivist consult | 97.7 | 2.4 | 0.032 | 0.93 (0.76–1.13) | 0.434 | 0.98 (0.83–1.15) | 0.7796 |
| Closed | 97.6 | 2.4 | 0.074 | 0.79 (0.54–1.15) | 0.448 | 0.85 (0.61–1.19) | 0.704 |
| Hospital organization | |||||||
| Community, no residents | 98.4 | 1.6 | — | Reference | Reference | ||
| Community, with residents | 98.0 | 2.0 | 0.148 | 1.21 (0.96–1.54) | 0.111 | 1.25 (1.00–1.57) | 0.048 |
| Academic | 97.6 | 2.4 | 0.008 | 1.31 (0.94–1.82) | 0.220 | 1.46 (1.07–2.00) | 0.035 |
Definition of abbreviations: CI = confidence interval; ICU = intensive care unit; OR = odds ratio.
P values are from mixed-effects regression models with ICU-specific random intercepts.
Variables in bivariable analysis that were not also in multivariable analysis either did not meet criteria for inclusion in the multivariable model, or did alter model fit and were not important confounders.
All P values reflect Holm adjustment for multiple comparisons.
Month of initial ICU admission and hospital region are also included in the model.
Patient Diagnoses: Index versus First Readmission
Never readmitted patients had similar index admission diagnoses as those eventually readmitted to the ICU. Readmission diagnoses in relation to index admission diagnoses are shown in Table 3. The most common readmission diagnoses were respiratory (42.3%), and cardiac arrest or failure (24.4%). Among readmitted patients, 42% and 41% were readmitted for a similar diagnosis as their index admission at 48 and 120 hours, respectively, suggesting a perpetuation or recurrence of the original problem, rather than a new problem. The proportion readmitted for an old problem was highest among patients originally admitted for respiratory (69.3%) or cardiac arrest or failure (56.6%).
TABLE 3.
INDEX ADMISSION AND READMISSION DIAGNOSES
| Never Readmitted |
48-h Readmissions |
120-h Readmissions |
|||||||
| Index Readmission Diagnosis | % | Index Readmission Diagnosis | % | Readmission Diagnosis | % | Index Readmission Diagnosis | % | Readmission Diagnosis | % |
| Respiratory arrest or failure | 20.5 | Respiratory arrest or failure | 23.5 | Respiratory arrest or failure | 69.3 | Respiratory arrest or failure | 23.1 | Respiratory arrest or failure | 65.2 |
| Cardiac arrest or failure | 15.7 | Cardiac arrest or failure | 16.1 | ||||||
| Sepsis | 5.9 | Sepsis | 7.1 | ||||||
| Surgical emergency | 0.5 | Surgical emergency | 1.4 | ||||||
| Postoperative observation | 0.4 | Postoperative observation | 1.1 | ||||||
| Hemorrhage | 3.1 | Hemorrhage | 3.9 | ||||||
| Neuro/neurosurgery | 3.6 | Neuro/neurosurgery | 3.6 | ||||||
| Metabolic | 1.0 | Metabolic | 1.2 | ||||||
| Other | 0.6 | Other | 0.5 | ||||||
| Cardiac arrest or failure | 16.1 | Cardiac arrest or failure | 15.2 | Respiratory arrest or failure | 25.5 | Cardiac arrest or failure | 14.9 | Respiratory arrest or failure | 25.1 |
| Cardiac arrest or failure | 56.6 | Cardiac arrest or failure | 52.4 | ||||||
| Sepsis | 5.1 | Sepsis | 6.7 | ||||||
| Surgical emergency | 0.8 | Surgical emergency | 1.2 | ||||||
| Postoperative observation | 2.3 | Postoperative observation | 4.2 | ||||||
| Hemorrhage | 3.8 | Hemorrhage | 3.7 | ||||||
| Neuro/neurosurgery | 4.1 | Neuro/neurosurgery | 4.5 | ||||||
| Metabolic | 1.3 | Metabolic | 1.7 | ||||||
| Other | 0.7 | Other | 0.6 | ||||||
| Sepsis | 6.7 | Sepsis | 9.6 | Respiratory arrest or failure | 37.5 | Sepsis | 9.6 | Respiratory arrest or failure | 34.8 |
| Cardiac arrest or failure | 21.6 | Cardiac arrest or failure | 19.4 | ||||||
| Sepsis | 26.7 | Sepsis | 30.6 | ||||||
| Surgical emergency | 1.8 | Surgical emergency | 2.1 | ||||||
| Postoperative observation | 1.0 | Postoperative observation | 1.3 | ||||||
| Hemorrhage | 5.9 | Hemorrhage | 6.3 | ||||||
| Neuro/neurosurgery | 2.3 | Neuro/neurosurgery | 3.4 | ||||||
| Metabolic | 1.5 | Metabolic | 1.3 | ||||||
| Other | 1.5 | Other | 0.8 | ||||||
| Surgical emergency | 6.4 | Surgical emergency | 7.2 | Respiratory arrest or failure | 45.2 | Surgical emergency | 7.9 | Respiratory arrest or failure | 41.0 |
| Cardiac arrest or failure | 23.5 | Cardiac arrest or failure | 19.3 | ||||||
| Sepsis | 7.6 | Sepsis | 12.0 | ||||||
| Surgical emergency | 7.9 | Surgical emergency | 11.3 | ||||||
| Postoperative observation | 1.0 | Postoperative observation | 1.5 | ||||||
| Hemorrhage | 3.8 | Hemorrhage | 4.1 | ||||||
| Neuro/neurosurgery | 3.8 | Neuro/neurosurgery | 3.6 | ||||||
| Metabolic | 2.4 | Metabolic | 2.6 | ||||||
| Other | 4.8 | Other | 4.6 | ||||||
| Postoperative observation | 10.7 | Postoperative observation | 10.0 | Respiratory arrest or failure | 46.4 | Postoperative observation | 9.9 | Respiratory arrest or failure | 43.7 |
| Cardiac arrest or failure | 30.8 | Cardiac arrest or failure | 26.0 | ||||||
| Sepsis | 4.1 | Sepsis | 7.2 | ||||||
| Surgical emergency | 0.2 | Surgical emergency | 1.7 | ||||||
| Postoperative observation | 4.8 | Postoperative observation | 7.2 | ||||||
| Hemorrhage | 2.4 | Hemorrhage | 4.3 | ||||||
| Neuro/neurosurgery | 6.3 | Neuro/neurosurgery | 5.4 | ||||||
| Metabolic | 3.1 | Metabolic | 2.3 | ||||||
| Other | 1.9 | Other | 2.3 | ||||||
| Hemorrhage | 7.4 | Hemorrhage | 8.7 | Respiratory arrest or failure | 16.8 | Hemorrhage | 8 | Respiratory arrest or failure | 17.9 |
| Cardiac arrest or failure | 12.8 | Cardiac arrest or failure | 13.5 | ||||||
| Sepsis | 4.0 | Sepsis | 7.3 | ||||||
| Surgical emergency | 3.7 | Surgical emergency | 4.7 | ||||||
| Postoperative observation | 2.3 | Postoperative observation | 3.7 | ||||||
| Hemorrhage | 50.4 | Hemorrhage | 43.4 | ||||||
| Neuro/neurosurgery | 6.6 | Neuro/neurosurgery | 5.1 | ||||||
| Metabolic | 1.4 | Metabolic | 1.2 | ||||||
| Other | 2 | Other | 3.2 | ||||||
| Neuro/neurosurgery | 18.3 | Neuro/neurosurgery | 14.2 | Respiratory arrest or failure | 28.1 | Neuro/neurosurgery | 15.7 | Respiratory arrest or failure | 27.2 |
| Cardiac arrest or failure | 15.5 | Cardiac arrest or failure | 12.9 | ||||||
| Sepsis | 2.6 | Sepsis | 2.8 | ||||||
| Surgical emergency | 0.9 | Surgical emergency | 1.0 | ||||||
| Postoperative observation | 0.5 | Postoperative observation | 1.0 | ||||||
| Hemorrhage | 0.9 | Hemorrhage | 1.6 | ||||||
| Neuro/neurosurgery | 50.4 | Neuro/neurosurgery | 52.2 | ||||||
| Metabolic | 0.7 | Metabolic | 1.0 | ||||||
| Other | 0.4 | Other | 0.5 | ||||||
| Metabolic | 7.6 | Metabolic | 3.8 | Respiratory arrest or failure | 38.2 | Metabolic | 3.5 | Respiratory arrest or failure | 34.5 |
| Cardiac arrest or failure | 19.1 | Cardiac arrest or failure | 18.0 | ||||||
| Sepsis | 6.6 | Sepsis | 9.4 | ||||||
| Surgical emergency | 2.6 | Surgical emergency | 3.1 | ||||||
| Postoperative observation | 1.3 | Postoperative observation | 2.0 | ||||||
| Hemorrhage | 5.3 | Hemorrhage | 5.5 | ||||||
| Neuro/neurosurgery | 5.9 | Neuro/neurosurgery | 7.5 | ||||||
| Metabolic | 20.4 | Metabolic | 19.2 | ||||||
| Other | 0.7 | Other | 0.8 | ||||||
| Other | 6.3 | Other | 7.6 | Respiratory arrest or failure | 48.1 | Other | 7.4 | Respiratory arrest or failure | 45.6 |
| Cardiac arrest or failure | 15.9 | Cardiac arrest or failure | 14.8 | ||||||
| Sepsis | 5.2 | Sepsis | 4.6 | ||||||
| Surgical emergency | 9.1 | Surgical emergency | 11.1 | ||||||
| Postoperative observation | 0.3 | Postoperative observation | 0.6 | ||||||
| Hemorrhage | 2.0 | Hemorrhage | 3.3 | ||||||
| Neuro/neurosurgery | 6.2 | Neuro/neurosurgery | 7.5 | ||||||
| Metabolic | 0.7 | Metabolic | 1.5 | ||||||
| Other | 12.7 | Other | 11.1 | ||||||
ICU Readmission Rates Across Patient Types, ICU Models, and Hospital Types
In adjusted models with no interaction terms, there was no difference in 48-hour ICU readmission rates between elective surgery (1.5% [1.3–1.7%]); emergency surgery (2% [1.7–2.2%]); and medical patients (1.9% [1.7–2%]). ICU readmission rates within 120 hours were 2.8% (2.5–3%) for elective surgery; 3.9% (3.5–4.3%) for emergency surgery; and 3.3% (3.1–3.6%) for medical patients.
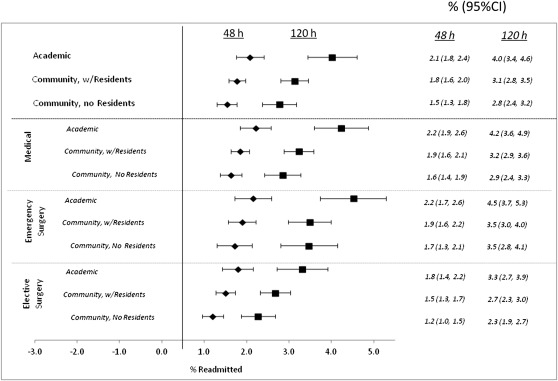
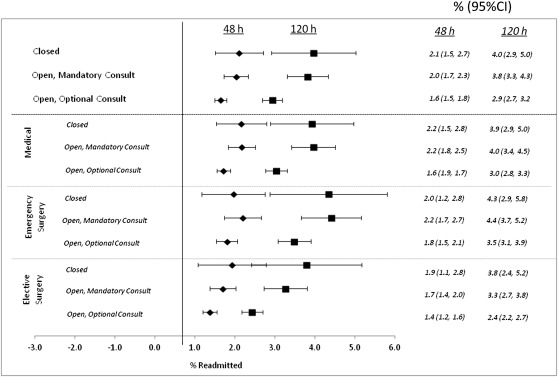
In adjusted models with interaction terms between patient-type and hospital-type ICU model, rates of 48-hour readmission did not differ across hospital type or ICU model (Figures 1 and 2). Among medical patients, academic hospitals had nonsignificantly higher 48-hour ICU readmission rates than community hospitals with residents (OR, 1.23 [0.97–1.55]; pHolm = 0.092), and significantly higher readmission rates than community hospitals without residents (OR, 1.51 [1.12–2.02]; pHolm = 0.018). The odds of 120-hour readmission for medical patients in academic hospitals were higher than in community hospitals with residents (OR, 1.31 [1.05–1.64]; pHolm = 0.031) and without residents (OR, 1.63 [1.24–2.16]; pHolm = 0.001). The odds of 120-hour readmission in community hospitals with residents were nonsignificantly higher than in community hospitals without residents (OR, 1.25 [1.00–1.55]; pHolm = 0.051). There were no differences in adjusted 48- or 120-hour readmission rates between ICU models.
Figure 1.
Adjusted rates of readmission by hospital organization. Percent readmitted after 48 and 120 hours. Rates represent predicted probabilities of intensive care unit readmission after adjusting for patient, intensive care unit, and hospital characteristics. CI = confidence interval.
Figure 2.
Adjusted rates of readmission by intensive care unit (ICU) model. Percent readmitted after 48 and 120 hours. Rates represent predicted probabilities of ICU readmission after adjusting for patient, ICU, and hospital characteristics. CI = confidence interval.
Time to Readmission
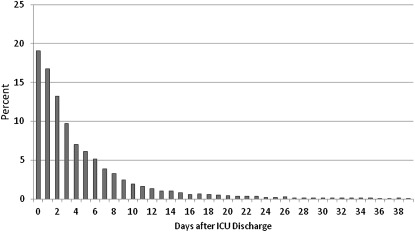
Figure 3 illustrates the distribution of time between ICU discharge and first readmission. Ninety-nine percent occurred within 30 days of discharge. The median time to ICU readmission was 3.07 days (IQR, 1.27–6.58). Roughly 20% of readmissions occurred within 24 hours of ICU discharge; 90% occurred within 12 days.
Figure 3.
Days to first intensive care unit (ICU) readmission. Unadjusted time to readmission across all ICU, hospital, and patient types, calculated from the time of discharge to the time of ICU readmission. Does not include readmissions to ICUs other than that from which the patient was initially discharged.
In closed ICUs, the median time to ICU readmission (3.55 d; IQR, 1.42–7.50) was longer than in ICUs requiring an intensivist consult (3.15 d; IQR, 1.31–6.65; pHolm = 0.006) or in ICUs with optional consults (2.95 d; IQR, 1.21–6.29; pHolm = 0.0001). Mandatory-consult ICUs displayed longer times to readmission than optional (pHolm = 0.008). ICUs in academic centers had longer times to readmission (3.24 d; IQR, 1.39–6.73) than community hospitals with residents (2.95 d; IQR, 1.20–6.41; pHolm = 0.0002), but not community hospitals without residents (3.06 d; IQR, 1.28–6.70; pHolm = 0.455). Elective (3.26 d; IQR, 1.36–6.72) and emergency surgical patients (3.37 d; IQR, 1.49–6.83) had longer times to ICU readmission than medical patients (2.94 d; IQR, 1.20–6.44) (emergency, pHolm = 0.0001; elective, pHolm = 0.0007).
Adjusted Hospital and Temporal Variables Associated with ICU Readmission
Several patient variables remained associated with increased odds ICU readmission in multivariable analysis (Tables 1 and 2) including severity of illness, functional status, admission from a general care floor, duration of mechanical ventilation, chronic respiratory or renal disease, chronic immunosuppression, and solid organ tumor. Length of ICU stay was no longer associated with 48-hour readmission, but was with 120-hour readmission. Patients admitted to ICUs with critical care fellows had higher readmission odds; hospitals with more beds had lower readmission odds. Compared with patients discharged from the ICU in the morning, those discharged in the afternoon or at night were more commonly readmitted. There was no association between ICU occupancy at discharge and readmission odds. ICU readmission odds did not change 2001–2007.
Model Fit
The C statistics for the models estimating 48- and 120-hour ICU readmission rates over time were 0.64 (95% confidence interval, 0.63–0.65) and 0.65 (95% confidence interval, 0.64–0.66), respectively, indicating moderate discrimination, but with important unexplained variability remaining. Models including interaction terms and nested models for 48-hour readmissions with hospital and ICU level random intercepts had comparable discrimination.
Secondary Analysis
Including patients readmitted to other ICUs as readmissions increased the 48- and 120-hour readmission rates from 2–2.3% and 3.7–4%, respectively. Including these readmissions, there were still no differences in readmission rates among ICUs using different staffing models. Because hospitals naturally vary in the numbers and types of ICUs they have, and the possibility of being readmitted to a different ICU depends on the availability of another ICU within the same hospital, differences among hospital types were not assessed using this secondary definition of ICU readmission.
Discussion
This national study across a diverse sample of ICUs shows that roughly 2% of critically ill patients are readmitted to the same ICU within 48 hours of ICU discharge; 4% are readmitted within 120 hours. Neither 48- nor 120-hour readmission rates varied across patient or ICU type. ICU readmission rates did not change 2001–2007. Among medical patients, those in academic hospitals were more likely to be readmitted after 48 hours than those in community hospitals without residents, and more likely to be readmitted after 120 hours than patients in community hospitals with or without residents. We did not evaluate readmissions after 120 hours because they are more likely to be determined by disease trajectories and care on the floor than ICU decisions. Further, the data suggest that fewer than 35% of readmissions occur beyond 120 hours, and modest C statistics suggest that even during these short windows, unmeasured risk factors may lead to ICU readmission. Future research should explore how patients’ severity of illness at ICU discharge (rather than at ICU admission), and how floor-based rather than ICU-based organizational structures, contribute to ICU readmission risk. Future research should also explore whether decision making by residents influences ICU readmission rates.
Approximately 60% of readmitted patients were readmitted for different diagnoses than their original diagnosis, whereas the other 40% may have had perpetuation or recrudescence of their initial problem. Evidence-based discharge criteria for vulnerable patient groups, such as sepsis or mechanically ventilated patients, which could prevent adverse events after ICU discharge deserve further exploration. However, the challenge is to develop effective criteria across diverse institutions that limit unintended negative consequences.
Fifty percent of readmitted patients returned to the ICU within 3 days. Closed ICUs and academic hospitals had the longest median times to readmission, possibly because of differences in case-mix or discharge practices, or because increased bed scarcity in closed ICUs creates delays in or higher thresholds for readmission. Alternatively, if ICU readmissions after longer time periods on the floor imply that adverse events post-ICU discharge rather than ICU practices precipitate readmissions, these findings could be attributable to different post-ICU discharge practices or events.
Afternoon and evening discharge were important risk factors for ICU readmission in multivariable analyses. This finding is consistent with a prior study (22) and may be because such patients may be more likely discharged to create room for other patients, suggesting that they are less “ready” for initial ICU discharge. Alternatively, differences in ICU night staffing, discharge protocols, or handoff quality may account for these findings. Although no association was found between ICU occupancy at patient discharge and ICU readmission in this analysis, the idea that “early” discharge because of ICU capacity strain could lead to adverse patient outcomes deserves further exploration (45).
ICU readmissions are considered a promising candidate for assessing ICU performance (12). This study addresses the epidemiology of ICU readmissions, and may guide sample selection for future studies that more directly assess the relevance of readmissions. This study does not settle the important questions of whether readmissions are preventable or causally related to poor outcomes. Too many readmissions could suggest the occurrence of preventable adverse events, but some readmissions may be inevitable, and others may even benefit patients. Similarly, too few readmissions could imply that hospitals retain patients in ICUs longer than necessary, exposing patients to unnecessary risks, causing denial of critical care to other patients, and increasing healthcare costs. Low ICU readmission rates could also be attributable to higher than expected mortality, or hasty hospital discharge. Therefore, any use of ICU readmissions as a quality metric must be accompanied by mortality and length-of-stay metrics. Further research should explore the circumstances surrounding readmissions, and the attributable mortality caused by them.
Other studies have reported higher ICU readmission rates than found in this study. However, many of these studies have been small, and may have been undertaken by participating institutions out of concern that ICU readmissions were too frequent. Further, many included readmissions after longer time periods, to other ICUs, or were performed in academic centers (5, 10, 12–14, 16–18, 20), which have higher rates of unadjusted ICU readmission than community ICUs.
Our results could be biased toward finding lower readmission rates. ICUs pay to participate in Project IMPACT, and participating hospitals may be particularly invested in quality improvement, although previous studies have shown that ICUs in Project IMPACT are representative of ICUs in the United States (27). The results of this study may still be appropriate to use for benchmarking purposes, because benchmarks should be established from a sample of ICUs concerned about quality (8, 10, 12, 16–20, 46).
Additionally, our definition of ICU readmission was more restrictive than that used by other studies. Our definition was designed to describe unintended, potentially preventable ICU readmissions, rather than elective readmissions. Therefore, the sample was limited to first readmissions and excluded readmissions to different ICUs. We established, a priori, temporal cut-points expected to provide clinically useful information, and also examined the full distribution of readmissions to a full picture of the relationships between patient, hospital, and ICU type and readmission rates. In secondary analyses, we found that including ICU readmissions to other ICUs increased rates by 0.3% in absolute terms.
This study has additional limitations. Severity of illness at the time of ICU discharge and adverse events occurring post-ICU discharge were not available for analysis. However, we used other variables as proxies for severity of illness at ICU discharge, such as duration of mechanical ventilation, time between extubation and ICU discharge, ICU length of stay, and the use of a step-down unit. Because no prior study has used similar adjustments, our severity adjusted readmission rate, while imperfect, represents the best estimate currently available.
Burn, cardiac, or coronary patients were not included in the analysis because they lacked an MPM0-III score, preventing a valid severity of illness adjustment. These estimates should be applied with caution to ICUs that serve primarily these patients.
Finally, because the study focuses on ICUs in the United States, results may not be generalizable to ICUs in other countries where healthcare systems, ICU management including criteria for readmission, and patient characteristics may differ substantively.
In summary, no differences were found between ICU models and hospital types in the rates of 48-hour ICU readmission in the largest and most representative sample of ICUs in the United States studied to date. The observed differences in 120-hour readmission rates across hospital types likely were attributable to residual confounding by unmeasured phenomena occurring on the floors. Using a shorter timeframe to define ICU readmission may avoid mixing readmissions attributable to ICU decisions with those attributable to post-ICU discharge events. Future research describing the clinical course of a prototypical ICU readmission, and the attributable mortality caused by readmissions, will provide further guidance for whether or how to use ICU readmissions as a quality benchmark.
Supplementary Material
Acknowledgments
The authors are grateful to Maximilian Herlim for invaluable help preparing the data for analysis, to Nicole Gabler for her help with data interpretation and presentation, and to Cerner Corporation for permitting access to the Project IMPACT database. Neither funding sources nor Cerner Corporation had a role in the design of this study or in the decision to submit it for publication.
Footnotes
Supported by F30 HL107020 from the National Heart, Lung, and Blood Institute (S.E.S.B.) and K08 HS018406 from the Agency for Healthcare Research and Quality (S.D.H.). These sponsors had no roles in the preparation, review, or approval of the poster.
Author Contributions: Conceived of idea, performed analyses, and wrote manuscript (all drafts) (S.E.S.B.); biostatistical expertise, analytic suggestions, data interpretation, and manuscript revisions (S.J.R.); content expertise and manuscript revisions (J.M.K.); and assisted with conception of idea, analytic plan, data interpretation, and manuscript revisions (S.D.H.). All coauthors had access to the study data, take responsibility for the analysis, and had authority over manuscript preparation and the decision to submit for publication.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201109-1720OC on January 26, 2012
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.de Vos M, Graafmans W, Keesman E, Westert G, van der Voort PH. Quality measurement at intensive care units: which indicators should we use? J Crit Care 2007;22:267–274 [DOI] [PubMed] [Google Scholar]
- 2.Cooper GS, Sirio CA, Rotondi AJ, Shepardson LB, Rosenthal GE. Are readmissions to the intensive care unit a useful measure of hospital performance? Med Care 1999;37:399–408 [DOI] [PubMed] [Google Scholar]
- 3.Woodhouse D, Berg M, van der Putten J, Houtepen J. Will benchmarking ICUs improve outcome? Curr Opin Crit Care 2009;15:450–455 [DOI] [PubMed] [Google Scholar]
- 4.McMillan TR, Hyzy RC. Bringing quality improvement into the intensive care unit. Crit Care Med 2007;35:S59–S65 [DOI] [PubMed] [Google Scholar]
- 5.Afessa B, Keegan MT, Hubmayr RD, Naessens JM, Gajic O, Long KH, Peters SG. Evaluating the performance of an institution using an intensive care unit benchmark. Mayo Clin Proc 2005;80:174–180 [DOI] [PubMed] [Google Scholar]
- 6.Berenholtz SM, Dorman T, Ngo K, Pronovost PJ. Qualitative review of intensive care unit quality indicators. J Crit Care 2002;17:1–12 [DOI] [PubMed] [Google Scholar]
- 7.Zimmerman JE, Alzola C, Von Rueden KT. The use of benchmarking to identify top performing critical care units: a preliminary assessment of their policies and practices. J Crit Care 2003;18:76–86 [DOI] [PubMed] [Google Scholar]
- 8.Chen LM, Martin CM, Keenan SP, Sibbald WJ. Patients readmitted to the intensive care unit during the same hospitalization: clinical features and outcomes. Crit Care Med 1998;26:1834–1841 [DOI] [PubMed] [Google Scholar]
- 9.Renton J, Pilcher DV, Santamaria JD, Stow P, Bailey M, Hart G, Duke G. Factors associated with increased risk of readmission to intensive care in Australia. Intensive Care Med 2011;37:1800–1808 [DOI] [PubMed] [Google Scholar]
- 10.Baker DR, Pronovost PJ, Morlock LL, Geocadin RG, Holzmueller CG. Patient flow variability and unplanned readmissions to an intensive care unit. Crit Care Med 2009;37:2882–2887 [DOI] [PubMed] [Google Scholar]
- 11. Society of Critical Care Medicine Quality Indicators Committee. Candidate critical care quality indicators. Anaheim, CA: Society of Critical Care Medicine; 1995.
- 12.Durbin CG, Jr, Kopel RF. A case-control study of patients readmitted to the intensive care unit. Crit Care Med 1993;21:1547–1553 [DOI] [PubMed] [Google Scholar]
- 13.Rosenberg AL, Watts C. Patients readmitted to ICUs*: a systematic review of risk factors and outcomes. Chest 2000;118:492–502 [DOI] [PubMed] [Google Scholar]
- 14.Snow N, Bergin KT, Horrigan TP. Readmission of patients to the surgical intensive care unit: patient profiles and possibilities for prevention. Crit Care Med 1985;13:961–964 [DOI] [PubMed] [Google Scholar]
- 15.Fernandez R, Serrano JM, Umaran I, Abizanda R, Carrillo A, Lopez-Pueyo MJ, Rascado P, Balerdi B, Suberviola B, Hernandez G. Ward mortality after ICU discharge: a multicenter validation of the Sabadell score. Intensive Care Med 2010;36:1196–1201 [DOI] [PubMed] [Google Scholar]
- 16.Kaben A, Correa F, Reinhart K, Settmacher U, Gummert J, Kalff R, Sakr Y. Readmission to a surgical intensive care unit: incidence, outcome and risk factors. Crit Care 2008;12:R123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Franklin C, Jackson D. Discharge decision-making in a medical ICU: characteristics of unexpected readmissions. Crit Care Med 1983;11:61–66 [DOI] [PubMed] [Google Scholar]
- 18.Baigelman W, Katz R, Geary G. Patient readmission to critical care units during the same hospitalization at a community teaching hospital. Intensive Care Med 1983;9:253–256 [DOI] [PubMed] [Google Scholar]
- 19.Lee JY, Park SK, Kim HJ, Hong SB, Lim CM, Koh Y. Outcome of early intensive care unit patients readmitted in the same hospitalization. J Crit Care 2009;24:267–272 [DOI] [PubMed] [Google Scholar]
- 20.Utzolino S, Kaffarnik M, Keck T, Berlet M, Hopt UT. Unplanned discharges from a surgical intensive care unit: readmissions and mortality. J Crit Care 2010;25:375–381 [DOI] [PubMed] [Google Scholar]
- 21.Chan KS, Tan CK, Fang CS, Tsai CL, Hou CC, Cheng KC, Lee MC. Readmission to the intensive care unit: an indicator that reflects the potential risks of morbidity and mortality of surgical patients in the intensive care unit. Surg Today 2009;39:295–299 [DOI] [PubMed] [Google Scholar]
- 22.Renton J, Pilcher DV, Santamaria JD, Stow P, Bailey M, Hart G, Duke G. Factors associated with increased risk of readmission to intensive care in Australia. Intensive Care Med 2011;37:1800–1808 [DOI] [PubMed] [Google Scholar]
- 23.Brown SES, Ratcliffe SJ, Kahn JM, Halpern SD. ICU readmissions in the United States: incidence and trends [abstract]. Am J Respir Crit Care Med 2011;183:A2374 [Google Scholar]
- 24.Description of Project IMPACT. Accessed 2011 September 9. Available from: http://investing.businessweek.com/research/stocks/private/snapshot.asp?privcapId=24623915
- 25.Levy MM, Rapoport J, Lemeshow S, Chalfin DB, Phillips G, Danis M. Association between critical care physician management and patient mortality in the intensive care unit. Ann Intern Med 2008;148:801–809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Glance LG, Li Y, Osler TM, Dick A, Mukamel DB. Impact of patient volume on the mortality rate of adult intensive care unit patients. Crit Care Med 2006;34:1925–1934 [DOI] [PubMed] [Google Scholar]
- 27.Cook SF, Visscher WA, Hobbs CL, Williams RL. Project IMPACT: results from a pilot validity study of a new observational database. Crit Care Med 2002;30:2765–2770 [DOI] [PubMed] [Google Scholar]
- 28.Chalfin DB, Trzeciak S, Likourezos A, Baumann BM, Dellinger RP. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med 2007;35:1477–1483 [DOI] [PubMed] [Google Scholar]
- 29.Fong JJ, Kanji S, Dasta JF, Garpestad E, Devlin JW. Propofol associated with a shorter duration of mechanical ventilation than scheduled intermittent lorazepam: a database analysis using Project IMPACT. Ann Pharmacother 2007;41:1986–1991 [DOI] [PubMed] [Google Scholar]
- 30.Higgins TL, Teres D, Copes WS, Nathanson BH, Stark M, Kramer AA. Assessing contemporary intensive care unit outcome: an updated mortality probability admission model (MPM0-III). Crit Care Med 2007;35:827–835 [DOI] [PubMed] [Google Scholar]
- 31.Nasraway SA, Jr, Albert M, Donnelly AM, Ruthazer R, Shikora SA, Saltzman E. Morbid obesity is an independent determinant of death among surgical critically ill patients. Crit Care Med 2006;34:964–970, quiz 971 [DOI] [PubMed] [Google Scholar]
- 32.Nathanson BH, Higgins TL, Teres D, Copes WS, Kramer A, Stark M. A revised method to assess intensive care unit clinical performance and resource utilization. Crit Care Med 2007;35:1853–1862 [DOI] [PubMed] [Google Scholar]
- 33.Taylor RW, O'Brien J, Trottier SJ, Manganaro L, Cytron M, Lesko MF, Arnzen K, Cappadoro C, Fu M, Plisco MS, et al. Red blood cell transfusions and nosocomial infections in critically ill patients. Crit Care Med 2006;34:2302–2308, quiz 2309 [DOI] [PubMed] [Google Scholar]
- 34.Teres D, Rapoport J, Lemeshow S, Kim S, Akhras K. Effects of severity of illness on resource use by survivors and nonsurvivors of severe sepsis at intensive care unit admission. Crit Care Med 2002;30:2413–2419 [DOI] [PubMed] [Google Scholar]
- 35. Available from: http://www.cwru.edu/med/epidbio/mphp439/Hospital_Acquired_Infections.htm. Accessed 2011 August 19.
- 36.Gajic O, Malinchoc M, Comfere TB, Harris MR, Achouiti A, Yilmaz M, Schultz MJ, Hubmayr RD, Afessa B, Farmer JC. The stability and workload index for transfer score predicts unplanned intensive care unit patient readmission: initial development and validation. Crit Care Med 2008;36:676–682 [DOI] [PubMed] [Google Scholar]
- 37.Ho KM, Dobb GJ, Lee KY, Finn J, Knuiman M, Webb SA. The effect of comorbidities on risk of intensive care readmission during the same hospitalization: a linked data cohort study. J Crit Care 2009;24:101–107 [DOI] [PubMed] [Google Scholar]
- 38.Brook RH, McGlynn EA, Cleary PD. Quality of health care. Part 2: measuring quality of care. N Engl J Med 1996;335:966–970 [DOI] [PubMed] [Google Scholar]
- 39.Chung DA, Sharples LD, Nashef SA. A case-control analysis of readmissions to the cardiac surgical intensive care unit. Eur J Cardiothorac Surg 2002;22:282–286 [DOI] [PubMed] [Google Scholar]
- 40.Kim MM, Barnato AE, Angus DC, Fleisher LA, Kahn JM. The effect of multidisciplinary care teams on intensive care unit mortality. Arch Intern Med 2010;170:369–376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA 2002;288:2151–2162 [DOI] [PubMed] [Google Scholar]
- 42.Localio AR, Berlin JA, Ten Have TR, Kimmel SE. Adjustments for center in multicenter studies: an overview. Ann Intern Med 2001;135:112–123 [DOI] [PubMed] [Google Scholar]
- 43.Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. Hoboken, NJ: John Wiley & Sons; 2004.
- 44.Hosmer DW, Lemeshow S. Applied logistic regression, 2nd ed. Hoboken, NJ: John Wiley & Sons; 2000.
- 45.Halpern SD. ICU capacity strain and the quality and allocation of critical care. Curr Opin Crit Care 2011;17:648–657 [DOI] [PubMed] [Google Scholar]
- 46.Rosenberg AL, Hofer TP, Hayward RA, Strachan C, Watts CM. Who bounces back? Physiologic and other predictors of intensive care unit readmission. Crit Care Med 2001;29:511–518 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.