Abstract
Rationale: Positive airway pressure therapy is frequently used to treat obstructive sleep apnea in children. However, it is not known whether positive airway pressure therapy results in improvements in the neurobehavioral abnormalities associated with childhood sleep apnea.
Objectives: We hypothesized that positive airway pressure therapy would be associated with improvements in attention, sleepiness, behavior, and quality of life, and that changes would be associated with therapy adherence.
Methods: Neurobehavioral assessments were performed at baseline and after 3 months of positive airway pressure therapy in a heterogeneous group of 52 children and adolescents.
Measurements and Main Results: Adherence varied widely (mean use, 170 ± 145 [SD] minutes per night). Positive airway pressure therapy was associated with significant improvements in attention deficits (P < 0.001); sleepiness on the Epworth Sleepiness Scale (P < 0.001); behavior (P < 0.001); and caregiver- (P = 0.005) and child- (P < 0.001) reported quality of life. There was a significant correlation between the decrease in Epworth Sleepiness Scale at 3 months and adherence (r = 0.411; P = 0.006), but not between other behavioral outcomes and adherence. Behavioral factors also improved in the subset of children with developmental delays.
Conclusions: These results indicate that, despite suboptimal adherence use, there was significant improvement in neurobehavioral function in children after 3 months of positive airway pressure therapy, even in developmentally delayed children. The implications for improved family, social, and school function are substantial.
Clinical trial registered with www.clinicaltrials.gov (NCT 00458406).
Keywords: continuous positive airway pressure, obstructive sleep apnea, sleepiness
At a Glance Commentary
Scientific Knowledge on the Subject
The childhood obstructive sleep apnea syndrome is common, and some of these children require positive airway pressure therapy. Although neurobehavioral disturbances are important comorbidities of childhood sleep apnea, the efficacy of positive airway pressure therapy in treating these neurobehavioral deficits is unknown.
What This Study Adds to the Field
Our data confirm that neurobehavioral deficits, such as daytime sleepiness, deficits in attention, behavioral problems, and decreased quality of life, are common in children with obstructive sleep apnea. We found that children treated with positive airway pressure therapy exhibited significant improvements in multiple neurobehavioral domains.
The obstructive sleep apnea syndrome (OSAS) affects up to 4% of children (1). In most children, OSAS is associated with adenotonsillar hypertrophy, and improves after adenotonsillectomy (2). However, a significant proportion of children have residual OSAS postoperatively (3). Furthermore, many children with OSAS have other underlying conditions, such as obesity or Down syndrome. In these children, continuous positive airway pressure (CPAP) is usually used as the second line of treatment (2). Although CPAP is now being used commonly in children, only a handful of studies have evaluated its efficacy.
If left untreated, OSAS may lead to substantial comorbidities. In particular, childhood OSAS has been shown to be associated with behavioral disturbances and learning deficits (4). The effect of PAP therapy in treating these neurobehavioral deficits in children is unknown. We therefore prospectively evaluated changes in neurobehavioral parameters, including symptoms of attention-deficit/hyperactivity disorder (ADHD), sleepiness, behavior, and quality of life, at baseline and after 3 months of PAP in children with OSAS. We hypothesized that children treated effectively with PAP, including children with developmental delays, would show improvements in neurobehavioral outcomes.
Some of the results of these studies have been previously reported in the form of an abstract (5).
Methods
See the online supplement for additional details.
This study was conducted prospectively as part of a clinical trial comparing two modes of PAP delivery: CPAP versus bilevel pressure release. No difference in adherence or efficacy was found between the modes (6). Children with OSAS aged 2 to 16 years, who were naive to PAP and clinically required PAP, were eligible. The study was approved by the Institutional Review Board of The Children's Hospital of Philadelphia, Philadelphia, Pennsylvania. Written informed consent was obtained from the parent or legal guardian, and assent from children 7 years of age or older when able.
All subjects underwent baseline clinical polysomnography before study entry. Subjects then had a 2-week habituation period at home, followed by a PAP titration study. At the end of 3 months, polysomnography was repeated on PAP, and objective adherence data were downloaded (EncorePro2; Philips Respironics, Murrysville, PA).
Neurobehavioral surveys were administered at baseline and after 3 months of PAP use. Based on known data regarding the domains affected by childhood OSAS, the following were evaluated. (1) Sleepiness, using the Epworth Sleepiness Scale modified for children (7–9). A score greater than 12 was considered abnormal because it was greater than the 95th percentile for normal children (7). (2) Behavioral problems, using the Child Behavior Checklist (CBCL) (10, 11). This is a survey of behavior competencies that yields standardized, age-adjusted scores on internalizing, externalizing, and total behavior difficulties. Scores between 60 and 63 are borderline; scores greater than 63 are abnormal. (3) ADHD, using the Conners Abbreviated Symptom Questionnaire and the Attention Problems subscale of the CBCL. The Conners scale evaluates inattention, distractibility, and overactivity. Scores range from 0 to 30; greater than or equal to 15 is considered clinically relevant (12). (4) Quality of life was measured using two instruments. The Pediatric Quality of Life Inventory (PedsQL) (13) is a well-validated measure of global quality of life. The score ranges from 0 to 100; the cutoff for moderate to severe impairment in quality of life is greater than 73 for children less than 8 years, and greater than or equal to 65 for children greater than or equal to 8 years (14). The OSAS-18 (15) is a composite of OSAS-related symptoms and disease-specific quality of life. Scores range from 18 to 126. Scores less than 60 suggest a small impact, 60 to 80 suggest a moderate impact, and greater than 80 suggest a large impact of OSAS on quality of life.
Surveys were completed by the same caregiver at each time point. In addition, developmentally able youths aged 11 to 18 completed the CBCL Youth Self Report, and those greater than or equal to 5 years completed the PedsQL.
Statistical Analysis
Unless otherwise specified, data are shown as mean ± SD. Differences between subjects at baseline versus 3 months were analyzed using paired Student t tests, Wilcoxon signed rank tests, or McNemar tests of equality of paired proportions. Differences between those who dropped out and those who completed the study were evaluated using unpaired Student t tests, Mann-Whitney rank sum tests, or Fisher exact test. Pearson or Spearman correlations were used to determine the relationship between adherence and behavioral outcomes. Analysis of covariance models were used to evaluate the effects of demographic variables on neurobehavioral outcomes. P less than 0.05 was considered significant.
Results
Study Group
Details of enrollment have been published elsewhere (6). Sixty subjects were initially enrolled; four were excluded because of medical interventions preventing PAP use, institutionalization, or having moved. Four subjects were lost to follow-up. One subject followed-up with neurocognitive testing but declined repeat polysomnography; this subject was included for analyses other than polysomnography. Thus, 52 subjects completed the study. There were no differences in baseline parameters between those lost to follow-up and those who completed the study.
Details of the study group are shown in Table 1. As is typical for childhood OSAS, where CPAP is usually reserved for children who fail surgical therapy, the study group was heterogeneous, with many children having underlying medical conditions, such as obesity or genetic syndromes (2, 16–22). Of note, 19% of subjects had developmental delays (Table 1). Overall, subjects had severe OSAS by pediatric standards (Table 2).
TABLE 1.
STUDY GROUP CHARACTERISTICS
| N | 52 |
| Age, yr | 12 ± 4 |
| Males | 36 (69) |
| Race | |
| African American | 32 (62) |
| White | 18 (35) |
| More than one race | 2 (4) |
| Hispanic ethnicity | 3 (6) |
| BMI z-score | 2 ± 0.9 |
| Other diagnoses* | |
| Obesity† | 36 (69) |
| Genetic syndrome | 9 (17) |
| Central nervous system abnormality | 6 (11) |
| Craniofacial syndrome | 3 (5) |
| Pulmonary disease | 3 (5) |
| Growth hormone deficiency | 1 (2) |
| Neurodevelopmental disability‡ | 10 (19) |
| Maternal education | |
| Did not complete high school | 2 (4) |
| Completed high school, no college | 14 (27) |
| Some college | 20 (39) |
| Completed college | 9 (17) |
| Completed postgraduate degree | 7 (14) |
| PAP adherence | |
| Nights used over 3 mo | 60 ± 25 |
| Average use per night, min | 170 ± 145 |
Definition of abbreviations: BMI = body mass index; PAP = positive airway pressure.
Data are shown as mean ± SD or N (%).
Note that some children had multiple diagnoses.
Obesity defined as BMI greater than or equal to 95th percentile for age and sex (38).
Includes six children with Down syndrome, one with Prader-Willi syndrome, one with cerebral palsy, one with autism, and one with a complex chromosomal disorder.
TABLE 2.
POLYSOMNOGRAPHIC DATA (N = 51)
| Baseline | On PAP | P Value | |
| Sleep efficiency, % total sleep time | 82 ± 11 | 83 ± 18 | 0.81 |
| Arousal index, N/hr | 23 ± 15 | 16 ± 18 | 0.019 |
| Stage N1, % TST | 8.8 ± 5.9 | 6.1 ± 6.7 | <0.001 |
| Stage N2, % TST | 49.1 ± 9.9 | 46.7 ± 11.2 | 0.16 |
| Stage N3, % TST | 22.3 ± 8.8 | 24.6 ± 13.5 | 0.18 |
| Rapid eye movement sleep, % TST | 19.7 ± 6.9 | 22.5 ± 7.5 | 0.036 |
| Apnea hypopnea index, N/hr | 18.1 ± 14.7 | 2 ± 2.3 | <0.001 |
| SpO2 nadir, % | 80 + 13 | 90 ± 4 | <0.001 |
| Time with SpO2 <90%, % TST | 4.9 ± 9.1 | 0.1 ± 0.5 | 0.001 |
| Peak end-tidal CO2, mm Hg | 57 ± 5 | 55 ± 5 | 0.027 |
| Time with end-tidal Pco2 >50 mm Hg, % TST | 16.7 ± 22.4 | 12 ± 19.6 | 0.42 |
Definition of abbreviations: PAP = positive airway pressure; SpO2 = oxygen saturation as measured by pulse oximetry; TST = total sleep time.
Data are shown as mean ± SD. Significant P values shown in bold.
Efficacy and Adherence
All subjects had adequate control of their OSAS by PAP on the titration night, with highly significant improvements in respiratory and sleep parameters compared with baseline (Table 2). There was a large variability in adherence, although most subjects attempted to use PAP on most nights (Table 1).
Neurobehavioral Changes
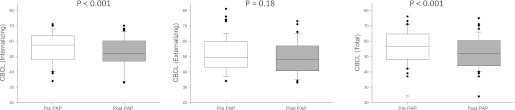
A large number of subjects had neurobehavioral scores in the clinically abnormal range (Table 3). After 3 months of PAP use, there were highly significant improvements in almost all domains (Figures 1–3). There were significant improvements in symptoms of ADHD (P < 0.001 for the Conner scale and P = 0.005 for the Attention Problems subscale of the CBCL) and daytime sleepiness on the Epworth Sleepiness Scale (P < 0.001). By parental report, internalizing behavior symptoms and total behavior, as measured by the CBCL, improved (both P < 0.001), although externalizing behavior symptoms did not improve (P = 0.181). Twenty-three subjects who were old enough and developmentally able completed the CBCL youth self-report; all three domains improved significantly (P = 0.023 for internalizing symptoms, P < 0.001 for externalizing symptoms, and P = 0.001 for total symptoms). There was an improvement in OSAS-specific (P < 0.001) and general health-related quality of life, as reported by caregivers (P = 0.005) and the children themselves (P < 0.001).
TABLE 3.
FREQUENCY OF CHILDREN FALLING IN THE CLINICALLY ABNORMAL RANGE ON NEUROBEHAVIORAL MEASURES AT BASELINE AND AFTER PAP THERAPY
| Measure | Baseline | On PAP | P Value |
| Conners Abbreviated Symptom Questionnaire* | 10 (19.2) | 6 (11.5) | 0.289 |
| Modified Epworth Sleepiness Scale | 14 (26.9) | 5 (9.6) | 0.004 |
| Child Behavior Checklist | |||
| Attention problems | 13 (25) | 8 (15.4) | 0.18 |
| Internalizing | 13 (25) | 9 (17.3) | 0.34 |
| Externalizing | 8 (15.4) | 6 (11.5) | 0.73 |
| Total | 17 (32.7) | 12 (23.1) | 0.063 |
| OSAS-18 | |||
| Moderate impairment | 28 (53.8) | 5 (9.6) | <0.001 |
| Large impairment | 9 (17.3) | 2 (3.8) | 0.039 |
| PedsQL | |||
| Impairment (caregiver report) | 27 (51.9) | 16 (30.8) | 0.013 |
| Impairment (child report)† | 26 (61.9) | 13 (31) | 0.002 |
Definition of abbreviations: OSAS = obstructive sleep apnea syndrome; PAP = positive airway pressure.
Data are shown as N (%). P values are based on McNemar tests of equality of paired proportions. Significant P values shown in bold.
N = 51.
N = 42.
Figure 1.
The box plots show improvements in symptoms of attention-deficit/hyperactivity disorder as measured by the Conners scale (left panel) and Child Behavior Checklist (CBCL) attention scale (center panel), and changes in daytime sleepiness as measured by the Epworth Sleepiness Scale (right panel), before and after 3 months of positive airway pressure (PAP). There was a significant improvement in symptoms of attention-deficit/hyperactivity disorder and sleepiness. The box represents the interquartile ranges, which contains 50% of all values. The line across the box indicates the median. The whiskers extend from the box to the 90th and 10th percentiles, excluding outliers. Outliers (open circles) are defined as cases outside the 90th and 10th percentiles.
Figure 3.
The box plots show improvements in obstructive sleep apnea (OSA)–specific (left panel, as measured by the OSA-18 scale) and general health-related quality of life (center and right panels, as measured by the caregiver and child PedsQL) before and after 3 months of positive airway pressure (PAP). The box represents the interquartile ranges, which contains 50% of all values. The line across the box indicates the median. The whiskers extend from the box to the 90th and 10th percentiles, excluding outliers. Outliers (open circles) are defined as cases outside the 90th and 10th percentiles.
Figure 2.
The box plots show changes in internalizing, externalizing, and total scores on the Child Behavior Checklist (CBCL) before and after 3 months of positive airway pressure (PAP). There were significant improvements in internalizing and total behavior symptom scores, but not in externalizing symptoms. The box represents the interquartile ranges, which contains 50% of all values. The line across the box indicates the median. The whiskers extend from the box to the 90th and 10th percentiles, excluding outliers. Outliers (open circles) are defined as cases outside the 90th and 10th percentiles.
The percentage of children with scores in the clinically abnormal range decreased on PAP for all domains, with significant reductions seen in the percentage of children with pathologic sleepiness on the Epworth Sleepiness Scale, and with low quality of life (Table 3).
The effect of age, sex, race, body mass index z-score, maternal education, and baseline scores on neurobehavioral outcomes was assessed. Baseline scores had a significant effect for all outcomes (P = 0.002 for OSA-18; P < 0.0005 for all other outcomes). Other than baseline scores, the only other significant effect was for sex on the change in score of the internalizing symptoms of the CBCL, with girls showing a greater improvement than boys (−6.9 ± 6.9 vs. −2.3 ± 7.9, respectively; P = 0.049).
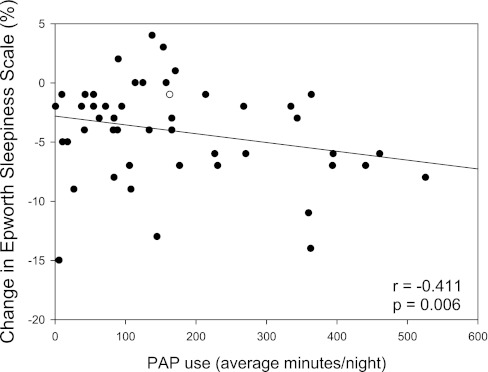
To assess the relationship between the degree of adherence and behavioral outcomes, the correlation between adherence parameters and behavioral outcomes was measured. There was a significant correlation between the change in the Epworth Sleepiness Scale score at 3 months and PAP adherence (mean minutes used per night, r = −0.411, P = 0.006; nights used, r = −0.348, P = 0.028) (Figure 4), but no significant correlation between other behavioral outcomes and PAP use.
Figure 4.
Individual changes in Epworth Sleepiness Scale at 3 months, as a percentage of baseline, is shown on the y-axis, and positive airway pressure (PAP) adherence, reflected as mean minutes used per night, is shown on the x-axis. There was a significant correlation between PAP use and change in sleepiness.
Subjects with developmental delays.
Ten subjects had significant developmental delays. Exploratory analyses were performed for this small subset of children. There were similar findings to the total study group, with significant improvements in the Epworth Sleepiness Scale (P = 0.003), internalizing (P = 0.024), and total behavior scores (P = 0.049), and OSAS-specific (P = 0.001) and general (P = 0.037) quality of life.
Subjects younger than 7 years of age.
Because PAP is not approved by the Food and Drug Administration for children less than 7 years of age or weighing less than 40 lb (18 kg), this subgroup was evaluated separately in exploratory analyses. In this small subset (n = 7; age 4.5 ± 1.7 yr; range, 2–6 yr), significant improvements were found in sleepiness on the Epworth Sleepiness Scale (P = 0.012) and OSAS-specific quality of life (P = 0.021).
Discussion
PAP use is known to be highly effective at treating OSAS as demonstrated on polysomnograpy (18). However, the clinical benefits of using PAP in children have not been well-studied. It is very difficult to get young children to wear the PAP apparatus (18, 21–23). Furthermore, many children requiring PAP therapy have underlying chronic illnesses or developmental delays (2, 16–22), further complicating efforts to improve adherence. It is therefore imperative to show that PAP use actually improves clinical outcomes in addition to improving polysomnographic abnormalities, before widespread pediatric PAP programs can be advocated. This study showed that PAP use was associated with significant changes in neurobehavioral parameters after only 3 months of use, even in a heterogeneous group of children with OSAS, including very young children and children with developmental delays. In addition to statistically significant improvements in neurobehavioral parameters, there was a reduction in the number of children falling into the clinically abnormal range (Table 3).
In adults, OSAS is associated with a wide range of neurocognitive deficits. These include deficits in daytime sleepiness, mood, cognitive processing, sustained attention, executive functioning, short-term working memory, and quality of life, all of which lead to diminished ability to execute various activities of daily living, such as occupational performance, driving safety, and psychosocial functioning (24, 25). However, in adults PAP use has not been clearly shown to improve many of these deficits (25, 26). A possible explanation for the improvement in function seen in children in the current study compared with the studies of adults may be that the children had a shorter duration of OSAS and therefore increased reversibility. Another explanation may be the increased plasticity of the child's central nervous system. The improvements may have been caused by improvements in gas exchange during sleep and improvements in sleep fragmentation.
Although neurobehavioral consequences of OSAS have been investigated extensively in adults, the consequences in children have not been fully evaluated. There is emerging evidence that children with OSAS show deficits in neurocognitive performance, behavioral impairments, and reduced school performance (4, 27–32), similar to those noted in the current study. Several studies have shown that these neurocognitive and behavioral abnormalities are at least partially reversible with surgical treatment in otherwise healthy children (27, 30, 33–35), although these studies were limited by small sample sizes or lack of full polysomnography. Only a handful of studies have examined the impact of PAP therapy on daytime functioning in children with OSAS. A study of 13 obese adolescents with OSAS found improvements in school performance, vigilance, and school-related quality of life in those who were adherent to PAP (36). Another study only evaluated subjective measures, and found improvements in sleepiness but no change in subjective assessments of attention or behavior (18).
In this study, changes in behavioral function were seen after only 3 months of PAP use. The time required for maximal improvements in behavioral function is unknown but may well be longer than 3 months, and further studies with long-term follow-up are needed.
The use of PAP therapy with children can be challenging despite close follow-up and support. In the current study, there was considerable variability in PAP adherence among subjects, with low overall adherence, consistent with findings from previous studies (18, 21, 22, 36). Despite this, improvements were found in all neurobehavioral domains. Conceivably, better adherence would result in even further improvements. Surprisingly, however, a significant correlation between improvements and adherence was found only in regards to daytime sleepiness, as measured on the Epworth Sleepiness Scale. Similarly, in adults, sleepiness improves in response to increased CPAP use (37). One reason for the lack of correlation between PAP use and other neurobehavioral outcomes in the current study may be the difference in physiologic sleep requirements over the age spectrum studied, and the differing degree of baseline neurobehavioral function in the subjects. Thus, the effects of wearing CPAP for 4 hours a night may be less beneficial in a 2 year old sleeping for 12 hours a night than in a 16 year old sleeping 8 hours a night.
In adults, 4 hours of PAP use per night is traditionally considered to be adequate adherence. The current study suggests that, in children, the longer the PAP mask is worn, the better the outcomes (at least in regards to daytime sleepiness). However, some benefit can be obtained from even small amounts of PAP use. Thus, any degree of PAP use should be encouraged.
In the current study, even children with significant developmental delays showed an improvement in some parameters with PAP. Therefore, PAP is recommended for this patient population, to optimize each child's potential. Note that the study was underpowered for the developmentally delayed subjects subset and the subset of children younger than 7 years of age, and may thus have missed other changes in behavioral parameters. Further studies of these high-risk groups are warranted.
A limitation of this study is that a placebo group was not included, and reports from individuals other than the subjects (for some measures) and caregivers, such as teachers, were not obtained. Subjects and their caregivers were not masked as to PAP treatment, and this may have impacted the responses to the surveys used as outcome measures.
The inclusion of children with a variety of underlying medical conditions and across the age spectrum is a limitation and strength of this study. This is the first comprehensive study of the effects of PAP use in children, and thus the study was designed to include the typical pediatric patient populations requiring PAP therapy. The study results are directly applicable to clinical pediatric sleep medicine practice. Further studies evaluating more homogeneous study groups are warranted to more closely determine the relationship between PAP use and neurobehavioral outcomes.
In conclusion, the treatment of childhood OSAS with PAP therapy was associated with significant improvements in daytime sleepiness, symptoms of ADHD, internalizing behaviors, and quality of life in children with OSAS, including young children and children with developmental delays. These improvements occurred despite a mean use of only 3 hours per night, suggesting that clinicians should encourage any PAP use, and not be discouraged when adherence is suboptimal. These findings have important implications in managing children with OSAS, because reinforcing PAP use is beneficial in many domains of daily life.
Supplementary Material
Acknowledgments
The authors thank all the children and families who participated in this study, and the sleep technologists for their dedication and professionalism.
Footnotes
Supported by Philips Respironics. All data collection, statistical analyses, and manuscript writing were performed by the investigators independent of Philips Respironics. C.L.M. also received support from NIH HL58585, and L.J.M. from K23 MH077662.
Author Contributions: C.L.M. was the principal investigator and responsible for all aspects of study design, data collection, data analysis, and manuscript preparation. J.R. and L.J.M. helped with the selection and interpretation of the social and psychometric survey instruments and were involved in study design, data analysis, and manuscript preparation. S.K. assisted with data analyses and manuscript preparation. S.E.B. was the unblinded physician safety monitor. M.A.C. and L.R.K. were study coordinators and participated in subject recruitment, data collection, and data entry. J.T. managed the database and adherence data collection and analysis. N.D. was study nurse and provided subject evaluation and support, fitted equipment, evaluated and managed side effects in conjunction with study physicians, and provided behavioral counseling for continuous positive airway pressure use. P.R.G. was responsible for statistical analyses and was involved in study design and manuscript preparation.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.201112-2167OC on February 9, 2012
Author disclosures are available with the text of this article at www.atsjournals.org.
Reference
- 1.Lumeng JC, Chervin RD. Epidemiology of pediatric obstructive sleep apnea. Proc Am Thorac Soc 2008;5:242–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2002;109:704–712 [DOI] [PubMed] [Google Scholar]
- 3.Bhattacharjee R, Kheirandish-Gozal L, Spruyt K, Mitchell RB, Promchiarak J, Simakajornboon N, Kaditis AG, Splaingard D, Splaingard M, Brooks LJ, et al. Adenotonsillectomy outcomes in treatment of obstructive sleep apnea in children: a multicenter retrospective study. Am J Respir Crit Care Med 2010;182:676–683 [DOI] [PubMed] [Google Scholar]
- 4.Beebe DW. Neurobehavioral morbidity associated with disordered breathing during sleep in children: a comprehensive review. Sleep 2006;29:1115–1134 [DOI] [PubMed] [Google Scholar]
- 5.Difeo N, Meltzer LJ, Karamessinis L, Beck SE, Davis K, Schultz B, Samuel J, Traylor J, Marcus CL, et al. Effects of positive airway pressure (PAP) on neurobehavioral function in children. Sleep 2009;32:A87 [Google Scholar]
- 6.Marcus CL, Beck SE, Traylor J, Cornaglia MA, Meltzer LJ, Difeo N, Karamessinis LR, Samuel J, Falvo J, DiMaria M, et al. Randomized, double-blind clinical trial of two different modes of positive airway pressure therapy on adherence and efficacy in children. J Clin Sleep Med 2012;8:37–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melendres MC, Lutz JM, Rubin ED, Marcus CL. Daytime sleepiness and hyperactivity in children with suspected sleep-disordered breathing. Pediatrics 2004;114:768–775 [DOI] [PubMed] [Google Scholar]
- 8.Elkhayat HA, Hassanein SM, Tomoum HY, Abd-Elhamid IA, Asaad T, Elwakkad AS. Melatonin and sleep-related problems in children with intractable epilepsy. Pediatr Neurol 2010;42:249–254 [DOI] [PubMed] [Google Scholar]
- 9.Chan EY, Ng DK, Chan CH, Kwok KL, Chow PY, Cheung JM, Leung SY. Modified Epworth Sleepiness Scale in Chinese children with obstructive sleep apnea: a retrospective study. Sleep Breath 2009;13:59–63 [DOI] [PubMed] [Google Scholar]
- 10.Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth & Families; 2001.
- 11.Achenbach TM, Rescorla LA. Manual for the ASEBA preschool forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth & Families; 2000.
- 12.Casat CD, Norton HJ, Boyle-Whitesel M. Identification of elementary school children at risk for disruptive behavioral disturbance: validation of a combined screening method. J Am Acad Child Adolesc Psychiatry 1999;38:1246–1253 [DOI] [PubMed] [Google Scholar]
- 13.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800–812 [DOI] [PubMed] [Google Scholar]
- 14.Huang IC, Thompson LA, Chi YY, Knapp CA, Revicki DA, Seid M, Shenkman EA. The linkage between pediatric quality of life and health conditions: establishing clinically meaningful cutoff scores for the PedsQL. Value Health 2009;12:773–781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Franco RA, Jr, Rosenfeld RM, Rao M. First place–resident clinical science award 1999. Quality of life for children with obstructive sleep apnea. Otolaryngol Head Neck Surg 2000;123:9–16 [DOI] [PubMed] [Google Scholar]
- 16.Waters KA, Everett FM, Bruderer JW, Sullivan CE. Obstructive sleep apnea: the use of nasal CPAP in 80 children. Am J Respir Crit Care Med 1995;152:780–785 [DOI] [PubMed] [Google Scholar]
- 17.Marcus CL, Ward SL, Mallory GB, Rosen CL, Beckerman RC, Weese-Mayer DE, Brouillette RT, Trang HT, Brooks LJ. Use of nasal continuous positive airway pressure as treatment of childhood obstructive sleep apnea. J Pediatr 1995;127:88–94 [DOI] [PubMed] [Google Scholar]
- 18.Marcus CL, Rosen G, Ward SL, Halbower AC, Sterni L, Lutz J, Stading PJ, Bolduc D, Gordon N. Adherence to and effectiveness of positive airway pressure therapy in children with obstructive sleep apnea. Pediatrics 2006;117:e442–e451 [DOI] [PubMed] [Google Scholar]
- 19.Guilleminault C, Pelayo R, Clerk A, Leger D, Bocian RC. Home nasal continuous positive airway pressure in infants with sleep- disordered breathing. J Pediatr 1995;127:905–912 [DOI] [PubMed] [Google Scholar]
- 20.Uong EC, Epperson M, Bathon SA, Jeffe DB. Adherence to nasal positive airway pressure therapy among school-aged children and adolescents with obstructive sleep apnea syndrome. Pediatrics 2007;120:e1203–e1211 [DOI] [PubMed] [Google Scholar]
- 21.O'Donnell AR, Bjornson CL, Bohn SG, Kirk VG. Compliance rates in children using noninvasive continuous positive airway pressure. Sleep 2006;29:651–658 [PubMed] [Google Scholar]
- 22.Massa F, Gonsalez S, Laverty A, Wallis C, Lane R. The use of nasal continuous positive airway pressure to treat obstructive sleep apnoea. Arch Dis Child 2002;87:438–443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koontz KL, Slifer KJ, Cataldo MD, Marcus CL. Improving pediatric compliance with positive airway pressure therapy: the impact of behavioral intervention. Sleep 2003;26:1010–1015 [DOI] [PubMed] [Google Scholar]
- 24.Beebe DW, Groesz L, Wells C, Nichols A, McGee K. The neuropsychological effects of obstructive sleep apnea: a meta-analysis of norm-referenced and case-controlled data. Sleep 2003;26:298–307 [DOI] [PubMed] [Google Scholar]
- 25.Sanchez AI, Martinez P, Miro E, Bardwell WA, Buela-Casal G. CPAP and behavioral therapies in patients with obstructive sleep apnea: effects on daytime sleepiness, mood, and cognitive function. Sleep Med Rev 2009;13:223–233 [DOI] [PubMed] [Google Scholar]
- 26.Gay P, Weaver T, Loube D, Iber C. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep 2006;29:381–401 [DOI] [PubMed] [Google Scholar]
- 27.Gozal D. Sleep-disordered breathing and school performance in children. Pediatrics 1998;102:616–620 [DOI] [PubMed] [Google Scholar]
- 28.Beebe DW, Wells CT, Jeffries J, Chini B, Kalra M, Amin R. Neuropsychological effects of pediatric obstructive sleep apnea. J Int Neuropsychol Soc 2004;10:962–975 [DOI] [PubMed] [Google Scholar]
- 29.Lewin DS, Rosen RC, England SJ, Dahl RE. Preliminary evidence of behavioral and cognitive sequelae of obstructive sleep apnea in children. Sleep Med 2002;3:5–13 [DOI] [PubMed] [Google Scholar]
- 30.Ali NJ, Pitson D, Stradling JR. Sleep disordered breathing: effects of adenotonsillectomy on behaviour and psychological functioning. Eur J Pediatr 1996;155:56–62 [DOI] [PubMed] [Google Scholar]
- 31.Chervin RD, Ruzicka DL, Giordani BJ, Weatherly RA, Dillon JE, Hodges EK, Marcus CL, Guire KE. Sleep-disordered breathing, behavior, and cognition in children before and after adenotonsillectomy. Pediatrics 2006;117:e769–e778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chervin RD, Weatherly RA, Ruzicka DL, Burns JW, Giordani BJ, Dillon JE, Marcus CL, Garetz SL, Hoban TF, Guire KE. Subjective sleepiness and polysomnographic correlates in children scheduled for adenotonsillectomy vs other surgical care. Sleep 2006;29:495–503 [PMC free article] [PubMed] [Google Scholar]
- 33.Montgomery-Downs HE, Crabtree VM, Gozal D. Cognition, sleep and respiration in at-risk children treated for obstructive sleep apnoea. Eur Respir J 2005;25:336–342 [DOI] [PubMed] [Google Scholar]
- 34.Mitchell RB, Kelly J. Adenotonsillectomy for obstructive sleep apnea in obese children. Otolaryngol Head Neck Surg 2004;131:104–108 [DOI] [PubMed] [Google Scholar]
- 35.Li HY, Huang YS, Chen NH, Fang TJ, Lee LA. Impact of adenotonsillectomy on behavior in children with sleep-disordered breathing. Laryngoscope 2006;116:1142–1147 [DOI] [PubMed] [Google Scholar]
- 36.Beebe DW, Byars KC. Adolescents with obstructive sleep apnea adhere poorly to positive airway pressure (PAP), but PAP users show improved attention and school performance. PLoS ONE 2011;6:e16924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, Greenberg H, Kader G, Mahowald M, Younger J, Pack AI. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep 2007;30:711–719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rosner B, Prineas R, Loggie J, Daniels SR. Percentiles for body mass index in US children 5 to 17 years of age. J Pediatr 1998;132:211–222 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.