Abstract
Background
Heat-related impacts may have greater public health implications as climate change continues. It is important to appropriately characterize the relationship between heatwave and health outcomes. However, it is unclear whether a case-crossover design can be effectively used to assess the event- or episode-related health effects. This study examined the association between exposure to heatwaves and mortality and emergency hospital admissions (EHAs) from non-external causes in Brisbane, Australia, using both case-crossover and time series analyses approaches.
Methods
Poisson generalised additive model (GAM) and time-stratified case-crossover analyses were used to assess the short-term impact of heatwaves on mortality and EHAs. Heatwaves exhibited a significant impact on mortality and EHAs after adjusting for air pollution, day of the week, and season.
Results
For time-stratified case-crossover analysis, odds ratios of mortality and EHAs during heatwaves were 1.62 (95% confidence interval (CI): 1.36–1.94) and 1.22 (95% CI: 1.14–1.30) at lag 1, respectively. Time series GAM models gave similar results. Relative risks of mortality and EHAs ranged from 1.72 (95% CI: 1.40–2.11) to 1.81 (95% CI: 1.56–2.10) and from 1.14 (95% CI: 1.06–1.23) to 1.28 (95% CI: 1.21–1.36) at lag 1, respectively. The risk estimates gradually attenuated after the lag of one day for both case-crossover and time series analyses.
Conclusions
The risk estimates from both case-crossover and time series models were consistent and comparable. This finding may have implications for future research on the assessment of event- or episode-related (e.g., heatwave) health effects.
Introduction
Heatwaves or excessive ambient heat exposures have significant impacts on mortality and morbidity [1]–[6]. For example, during the 1995 Chicago heatwave, there were over 700 excess deaths in a single day [7]. The well-known 2003 heatwaves led to 15,000 excess deaths in France alone [8], [9], and over 70,000 deaths across Europe [10], [11]. The 2006 California heatwave resulted in an increase in morbidity which included 16,166 excess emergency department visits and 1,182 excess hospitalizations state-wide [12]. Heat-related impacts may have greater public health implications as climate change continues. It is important to appropriately characterize the relationship between heatwaves and health outcomes.
Two common epidemiologic methods have been frequently used to assess the heat-related health effects. Time series analysis has been used to investigate the health impact of time varying environmental exposures (eg, air pollution and temperature) for many years [13], [14]. Recently, a case-crossover design (introduced by MaClure in 1991) has been increasingly used to examine an association between a transient exposure (eg, temperature or air pollution) and acute health outcomes [15], [16]. This design controls for time-invariant confounders by study design itself [17]. Therefore, it has some advantages compared with commonly-used time series analysis. However, some methodological issues in the use of case-crossover analysis have attracted much research attention. For example, unidirectional case-crossover design was initially applied and the referent period was designated by specific time period(s) before the case period [18]. Recently, ambidirectional and time-stratified case-crossover analyses have been assumed as ideal approaches because unidirectional design has often produced biased results [18]–[20]. The previous research mainly focused on the risk assessment of time-varying exposures (eg, air pollution and temperature) using relatively long time series datasets. However, little information is available on whether these findings are applicable to the assessment of event- or episode-related (eg, heatwave) health effects. Since time series and case-crossover methods are often viewed as two competing analytical approaches, this study examined whether these methods produced equivalent risk estimates in the assessment of the health effects of heatwaves in Brisbane, Australia.
Materials and Methods
Data collection
Brisbane, Australia's third largest city, is located in the south-east corner of the Queensland state (27°29′S, 153°8′E) and has a sub-tropical climate. The population increased from 896,649 on 30 June 2001 to 991 260 on 30 June 2006. 18% of the residents in Brisbane were aged 0–14, while 11% of them were aged 65+[21].
We obtained emergency hospital admissions (EHAs) data during 1st January 1996 to 31st December 2005, and mortality data during 1st January 1996 to 30th November 2004. Daily data on mortality and EHAs were provided by the Office of Economic and Statistical Research of the Queensland Treasury and the Health Information Centre of Queensland Health, respectively. Non-external causes (NEC) mortality and EHAs were categorised according to the International Classification of Diseases (revisions 9 and 10) (ICD 9, <800; and all ICD 10 codes excluding S00–U99 for external causes).
Daily data on maximum temperature and relative humidity data were obtained from the Australian Bureau of Meteorology during January 1996 to December 2005. The daily average values of climatic variables were calculated from five monitoring stations. We retrieved daily air pollution data from the Queensland Department of Environment and Resource Management (formerly Queensland Environmental Protection Agency), including ambient 24-hour average concentrations of particulate matter with diameter less than 10 µm (PM10), daily maximum 1-hour average nitrogen dioxide (NO2) and ozone (O3). Daily air pollution concentrations were averaged from seventeen monitoring stations in Brisbane. When data were missing for a particular monitoring station on a given day, the data recorded from other monitoring stations were used to calculate the daily average values.
Data analysis
According to the local heatwave definition (ie, daily maximum temperature higher than 37°C for two or more consecutive days) developed in the previous research [22], [23], three heatwaves occurred (20 and 21 January 2000; 24 to 26 December 2001; 21 and 22 February 2004) during the whole study period. We examined the short-term effects of heatwaves on mortality and EHAs within three different periods, 84 days (28 days as a strata length for time-stratified case-crossover analysis), summer season (from December to February) and whole study period (1996–2005). Spearman's correlation coefficients were used to evaluate the interrelations between air pollutants and climate variables in these three periods.
In this study, both time-series and case–crossover analyses were used to examine the heatwave effects on NEC mortality and EHAs. Poisson generalised additive model (GAM) was used to perform time series analyses on three different periods. We also used time-stratified case–crossover with a stratum length of 28 days, and matched case-control days using day of the week (one case day was matched with three control days). Because only three heatwaves were defined during the whole study period, three strata (84 days) were used for the case–crossover analysis. Heatwave days were categorised as 1, while non-heatwave days were categorised as 0. We adjusted for humidity and air pollutants (PM10, NO2 and O3) in these models. Additionally, lagged effects (ie, lag 0 to lag 5 and moving average of lags 0–5) were assessed using the same methods. When lagged effects of heatwaves on NEC mortality and EHAs were assessed, the same lagged effects of humidity and air pollution were controlled for. Relative risks (RRs) for time series analysis, odds ratios (ORs) for time-stratified case–crossover analysis, and 95% confidence intervals (CIs) were calculated in each model. R software (version 2.12.2) and the “mgcv” package were applied to fit the time series GAM and case–crossover analyses. The R codes are provided in Information S1 using an example dataset (Information S2), and results of estimation using different degree of freedom were presented in Figure S1.
Results
There were a total of 51,233 deaths and 488,005 EHAs recorded in Brisbane during the whole study period. Table 1 shows summary statistics of climatic variables, air pollutants, mortality and EHAs for three different periods, as well as the total number of different health outcomes used in each model. There was some variation in these variables during three periods. The mean concentrations of PM10, NO2 and O3 differed slightly across the different periods. The daily average deaths (17) and EHAs (142) during 84 days were higher than those during summer days (15 deaths and 128 EHAs) or whole study period (16 deaths and 134 EHAs).
Table 1. Summaries of daily weather, air pollutants and health outcomes in Brisbane, Australia.
| 84 days | Summer | 1996–2005 | |||||||
| Mean | SD | Range | Mean | SD | Range | Mean | SD | Range | |
| Tmaxa (°C) | 30.9 | 3.8 | 21.0 to 41.5 | 30.0 | 2.6 | 21.0 to 41.5 | 26.3 | 3.9 | 12.6 to 41.5 |
| Humidity (%) | 70.8 | 8.1 | 44.9 to 90.2 | 71.7 | 8.1 | 39.6 to 96.9 | 71.1 | 10.3 | 24.6 to 96.9 |
| PM10 (µg/m3) | 21.1 | 8.9 | 7.2 to 43.7 | 17.8 | 6.7 | 6.5 to 78.6 | 17.7 | 7.6 | 2.5 to 151.6 |
| NO2 (ppb) | 13.1 | 4.2 | 5.2 to 26.8 | 12.1 | 4.0 | 3.6 to 30.8 | 18.0 | 6.7 | 3.3 to 46.3 |
| O3 (ppb) | 35.4 | 12.3 | 13.9 to 67.8 | 31.7 | 12.1 | 7.7 to 88.2 | 31.8 | 9.8 | 7.1 to 88.2 |
| Deaths | 17 | 6 | 5 to 4 | 15 | 4 | 5 to 42 | 16 | 4 | 5 to 42 |
| (1,400)c | (11,432)c | (51,233)c | |||||||
| EHAsb | 142 | 21 | 101 to 202 | 128 | 21 | 71 to 202 | 134 | 22 | 71 to 212 |
| (11,962)c | (115,406)c | (488,005)c | |||||||
maximum temperature.
emergency hospital admissions.
the number of outcomes.
Table 2 shows that maximum temperatures positively correlated with most air pollutants in all periods except for NO2 during the whole study period. Moderate to high correlations were observed for temperature and PM10, NO2 and ozone. However, humidity inversely correlated with most air pollutants in different periods, although most of these correlations were week. There were significant associations between air pollutants.
Table 2. Spearman correlation between climatic variables and air pollutants in Brisbane, Australia.
| Humidity | PM10 | NO2 | O3 | |
| 84 days | ||||
| Tmaxa (°C) | −0.18 | 0.61** | 0.72** | 0.84** |
| Humidity (%) | −0.40** | −0.08 | −0.10 | |
| PM10 (µg/m3) | 0.40** | 0.62** | ||
| NO2 (ppb) | 0.68** | |||
| Summer | ||||
| Tmaxa (°C) | −0.06 | 0.35** | 0.24** | 0.65** |
| Humidity (%) | −0.31** | 0.01 | −0.09* | |
| PM10 (µg/m3) | 0.33** | 0.46** | ||
| NO2 (ppb) | 0.51** | |||
| 1996–2005 | ||||
| Tmaxa (°C) | −0.06** | 0.25** | −0.47** | 0.35** |
| Humidity (%) | −0.26** | −.0.06** | −0.20** | |
| PM10 (µg/m3) | 0.30** | 0.47** | ||
| NO2 (ppb) | 0.28** | |||
Tmax = maximum temperature.
P<0.05.
P<0.01.
In time-stratified case-crossover analysis we used 28 days as a stratum length. Since three heatwaves occurred during the study period, therefore 84 days (ie, three strata: 3×28 days) were used in data analysis. Table 3 shows the estimated odds ratios (ORs) and relative risks (RRs) for NEC mortality and EHAs during heatwave days compared with non-heatwave days during these 84 days. There was a broadly consistent and statistically significant increase in ORs or RRs for both mortality and EHAs during heatwaves.
Table 3. Odds ratios (ORs) and Relative risks (RRs) of mortality and EHAs during heatwaves in Brisbane (84 days).
| OR/RR (95% CI) | ||||
| HW effect | Model Ia | Model IIb | Model IIIc | Model IVd |
| Deaths | ||||
| Case-crossover | ||||
| Lag 0 | 1.53 (1.27, 1.85) | 1.47 (1.22, 1.78) | 1.52 (1.25, 1.83) | 1.51 (1.25, 1.83) |
| Lag 1 | 1.67 (1.40, 2.00) | 1.63 (1.36, 1.95) | 1.65 (1.38, 1.97) | 1.64 (1.38, 1.96) |
| Lag 2 | 1.39 (1.16, 1.67) | 1.37 (1.14, 1.65) | 1.39 (1.15, 1.67) | 1.38 (1.15, 1.66) |
| Lag 3 | 1.15 (0.94, 1.42) | 1.16 (0.94. 1.42) | 1.15 (0.94, 1.41) | 1.14 (0.93, 1.41) |
| Lag 4 | 1.18 (0.96, 1.46) | 1.17 (0.95, 1.45) | 1.17 (0.95, 1.45) | 1.18 (0.95, 1.45) |
| Lag 5 | 1.15 (0.92, 1.44) | 1.19 (0.95, 1.49) | 1.16 (0.93, 1.45) | 1.16 (0.93, 1.45) |
| 6-day average | 1.36 (1.12, 1.65) | 1.37 (1.12, 1.66) | 1.36 (1.11, 1.65) | 1.35 (1.11, 1.64) |
| Time-series | ||||
| Lag 0 | 1.44 (1.22, 1.70) | 1.26 (1.03, 1.54) | 1.48 (1.23, 1.79) | 1.25 (1.02, 1.55) |
| Lag 1 | 1.72 (1.48, 2.01) | 1.83 (1.51, 2.22) | 1.99 (1.67, 2.38) | 1.70 (1.39. 2.08) |
| Lag 2 | 1.47 (1.25, 1.73) | 1.50 (1.22, 1.83) | 1.66 (1.38, 2.00) | 1.45 (1.18, 1.79) |
| Lag 3 | 1.10 (0.92, 1.33) | 1.14 (0.92, 1.42) | 1.21 (0.98, 1.48) | 1.07 (0.85, 1.35) |
| Lag 4 | 1.04 (0.87, 1.26) | 1.05 (0.84, 1.31) | 1.12 (0.91, 1.39) | 1.09 (0.86, 1.37) |
| Lag 5 | 0.94 (0.77, 1.14) | 1.05 (0.83, 1.33) | 1.02 (0.82, 1.27) | 1.13 (0.89, 1.44) |
| 6-day average | 1.28 (1.08, 1.52) | 1.29 (1.07, 1.56) | 1.29 (1.078, 1.564 | 1.29 (1.07, 1.55) |
| EHAs | ||||
| Case-crossover | ||||
| Lag 0 | 1.17 (1.10, 1.26) | 1.16 (1.08, 1.24) | 1.16 (1.09, 1.25) | 1.17 (1.10, 1.26) |
| Lag 1 | 1.23 (1.15, 1.31) | 1.22 (1.14, 1.30) | 1.23 (1.15, 1.32) | 1.23 (1.15, 1.32) |
| Lag 2 | 1.17 (1.10, 1.26) | 1.17 (1.09, 1.25) | 1.18 (1.10, 1.26) | 1.18 (1.10, 1.26) |
| Lag 3 | 1.13 (1.05, 1.21) | 1.13 (1.05, 1.21) | 1.13 (1.05, 1.21) | 1.13 (1.05, 1.21) |
| Lag 4 | 1.11 (1.03, 1.19) | 1.10 (1.03, 1.18) | 1.11 (1.03, 1.19) | 1.11 (1.03, 1.19) |
| Lag 5 | 1.04 (0.97, 1.12) | 1.04 (0.97, 1.11) | 1.04 (0.97, 1.12) | 1.04 (0.97, 1.11) |
| 6-day average | 1.14 (1.07, 1.23) | 1.15 (1.07, 1.23) | 1.14 (1.07, 1.23) | 1.14 (1.07, 1.23) |
| Time-series | ||||
| Lag 0 | 1.14 (1.07, 1.21) | 1.08 (1.01, 1.17) | 1.12 (1.04, 1.20) | 1.09 (1.01, 1.17) |
| Lag 1 | 1.20 (1.13, 1.28) | 1.15 (1.07, 1.24) | 1.19 (1.11, 1.27) | 1.13 (1.05, 1.22) |
| Lag 2 | 1.16 (1.10, 1.24) | 1.13 (1.05, 1.21) | 1.18 (1.10, 1.26) | 1.11 (1.03, 1.20) |
| Lag 3 | 1.09 (1.03, 1.16) | 1.06 (0.98, 1.14) | 1.11 (1.03, 1.19) | 1.03 (0.96, 1.12) |
| Lag 4 | 1.07 (1.01, 1.14) | 1.03 (0.96, 1.11) | 1.08 (1.01, 1.16) | 1.01 (0.94, 1.10) |
| Lag 5 | 1.03 (0.97, 1.10) | 1.01 (0.94, 1.09) | 1.04 (0.97, 1.12) | 0.99 (0.92, 1.07) |
| 6-day average | 1.12 (1.05, 1.19) | 1.04 (0.97, 1.11) | 1.08 (1.01, 1.15) | 1.05 (0.99, 1.12) |
unadjusted.
adjusted for humidity and O3.
adjusted for humidity and PM10.
adjusted for humidity and NO2.
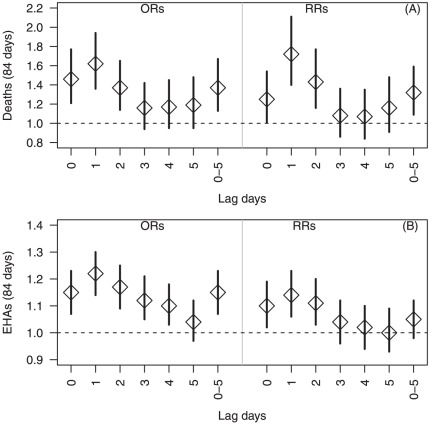
Figure 1 shows the similar results as Table 3 when both methods was used to adjust for humidity, PM10, NO2 and O3. ORs of mortality and morbidity during heatwaves were 1.62 (95% CI: 1.36–1.94) (Figure 1A) and 1.22 (95% CI: 1.14–1.30) (Figure 1B) at lag 1, respectively. RRs of mortality and morbidity during heatwaves were 1.72 (95% CI: 1.40–2.11) (Figure 1A) and 1.14 (95% CI: 1.06–1.23) (Figure 1B) at lag 1, respectively. The risk estimates also generally alleviated after lag 1 for both mortality and EHAs.
Figure 1. Odds ratios and Relative risks of daily mortality (1A) and emergency hospital admissions (1B) during heatwaves (84 days), using both case crossover and time series analyses.
Table 4 shows the delayed effects of heatwaves on NEC mortality and EHAs for summer season and whole study period using time series models to adjust for different sets of confounders. There were also broadly consistent increased risks for both mortality and EHAs during heatwaves across different periods. The highest risk estimates were observed at lag 1 for both mortality and EHAs after adjusting for confounders.
Table 4. Relative risks (RRs) of daily mortality and EHAs during heatwaves in Brisbane (summer season and whole study period), using time series analysis.
| OR/RR (95% CI) | ||||
| HW effect | Model Ia | Model IIb | Model IIIc | Model IVd |
| Deaths | ||||
| Summer | ||||
| Lag 0 | 1.59 (1.36, 1.86) | 1.49 (1.27, 1.75) | 1.53 (1.31, 1.80) | 1.54 (1.32, 1.81) |
| Lag 1 | 1.87 (1.62, 2.16) | 1.80 (1.55, 2.08) | 1.85 (1.60, 2.14) | 1.86 (1.60, 2.15) |
| Lag 2 | 1.64 (1.41,1.91) | 1.60 (1.36, 1.87) | 1.63 (1.39, 1.90) | 1.63 (1.39, 1.91) |
| Lag 3 | 1.24 (1.04, 1.48) | 1.22 (1.02, 1.46) | 1.23 (1.03, 1.47) | 1.24 (1.04, 1.48) |
| Lag 4 | 1.17 (0.98, 1.40) | 1.15 (0.96, 1.38) | 1.17 (0.98, 1.41) | 1.18 (0.98, 1.42) |
| Lag 5 | 1.05 (0.87, 1.27) | 1.07 (0.88, 1.30) | 1.06 (0.88, 1.29) | 1.09 (0.90, 1.32) |
| 6-day average | 1.42 (1.21, 1.67) | 1.39 (1.18, 1.65) | 1.40 (1.19, 1.65) | 1.42 (1.21, 1.68) |
| 1996-2005 | ||||
| Lag 0 | 1.47 (1.26, 1.72) | 1.44 (1.23, 1.68) | 1.45 (1.25, 1.70) | 1.49 (1.27, 1.73) |
| Lag 1 | 1.73 (1.50, 1.99) | 1.71 (1.48, 1.98) | 1.71 (1.48, 1.97) | 1.73 (1.50, 2.00) |
| Lag 2 | 1.52 (1.30, 1.77) | 1.53 (1.31, 1.78) | 1.51 (1.30, 1.76) | 1.52 (1.31, 1.77) |
| Lag 3 | 1.15 (0.97, 1.37) | 1.17 (0.98, 1.39) | 1.15 (0.96, 1.37) | 1.16 (0.97, 1.38) |
| Lag 4 | 1.09 (0.91, 1.30) | 1.10 (0.92, 1.32) | 1.08 (0.91, 1.30) | 1.09 (0.91, 1.30) |
| Lag 5 | 0.98 (0.81, 1.18) | 1.02 (0.84, 1.23) | 0.99 (0.82, 1.19) | 0.99 (0.82, 1.19) |
| 6-day average | 1.32 1.12, 1.55) | 1.37 (1.16, 1.61) | 1.33 (1.13, 1.56) | 1.39 (1.18, 1.64) |
| EHAS | ||||
| Summer | ||||
| Lag 0 | 1.26 (1.19, 1.34) | 1.21 (1.14, 1.29) | 1.20 (1.13, 1.27) | 1.23 (1.15, 1.30) |
| Lag 1 | 1.32 (1.25, 1.40) | 1.28 (1.21, 1.36) | 1.27 (1.19, 1.34) | 1.30 (1.22, 1.38) |
| Lag 2 | 1.29 (1.22, 1.37) | 1.26 (1.18, 1.33) | 1.24 (1.17, 1.31) | 1.27 (1.19, 1.34) |
| Lag 3 | 1.21 (1.14, 1.29) | 1.19 (1.12, 1.26) | 1.17 (1.10, 1.24) | 1.20 (1.13, 1.28) |
| Lag 4 | 1.18 (1.11, 1.26) | 1.15 (1.09, 1.23) | 1.14 (1.07, 1.21) | 1.18 (1.11, 1.25) |
| Lag 5 | 1.14 (1.07, 1.21) | 1.12 (1.05, 1.19) | 1.10 (1.03, 1.17) | 1.13 (1.07, 1.21) |
| 6-day average | 1.23 (1.16, 1.31) | 1.22 (1.15, 1.29) | 1.19 (1.12, 1.26) | 1.23 (1.16, 1.30) |
| 1996–2005 | ||||
| Lag 0 | 1.20 (1.13, 1.27) | 1.20 (1.13, 1.27) | 1.18 (1.11, 1.25) | 1.20 (1.13, 1.27) |
| Lag 1 | 1.26 (1.19, 1.34) | 1.27 (1.20, 1.34) | 1.25 (1.18, 1.32) | 1.26 (1.19, 1.34) |
| Lag 2 | 1.23 (1.17, 1.31) | 1.24 (1.17, 1.32) | 1.22 (1.15, 1.29) | 1.23 (1.16, 1.30) |
| Lag 3 | 1.16 (1.09, 1.23) | 1.17 (1.10, 1.25) | 1.15 (1.08, 1.22) | 1.15 (1.09, 1.22) |
| Lag 4 | 1.13 (1.07, 1.20) | 1.15 (1.08, 1.22) | 1.12 (1.06, 1.19) | 1.13 (1.06, 1.20) |
| Lag 5 | 1.09 (1.02, 1.16) | 1.10 (1.04, 1.17) | 1.08 (1.01, 1.15) | 1.08 (1.02, 1.15) |
| 6-day average | 1.18 (1.11, 1.25) | 1.22 (1.15, 1.29) | 1.17 (1.11, 1.25) | 1.20 (1.13, 1.27) |
unadjusted.
adjusted for humidity and O3.
adjusted for humidity and PM10.
adjusted for humidity and NO2.
Figure 2 reveals the similar results as Table 4 when time series GAM models were used with different periods to adjust for humidity, PM10, NO2 and O3. The results show that RRs of mortality and EHAs ranged from 1.77 (95% CI: 1.53–2.04) to 1.81 (95% CI: 1.56–2.10) in Figure 2A and 1.28 (95% CI: 1.21–1.36) (Figure 2B) at lag 1, respectively. The risk estimates generally attenuated after the lag of one day for both mortality and EHAs.
Figure 2. Relative risks of daily mortality (2A) and emergency hospital admissions (2B) during heatwaves (summer season and whole study period), using time series analyses.
Discussion
An increase in the frequency, duration and intensity of heatwaves is one of the most certain impacts of global climate change [24], and therefore, it is important to characterise the heat-related health risks. In this study, we found consistent and significant risks of NEC deaths and EHAs during heatwaves using both time series and case-crossover methods. For time series analyses, a similar pattern of heatwave-related risks was observed even though different periods of data were used. In general, the effect estimates using time series analyses were quite comparable to those estimated by the case-crossover method. We also found that heatwaves had acute effects on mortality and EHAs, and the highest impact usually occurred at lag 1 in Brisbane – a subtropical city in Australia.
In a recent study of the relationship between temperature and mortality among the elderly, the results from a case-crossover study design using three different approaches for the selection of referent periods were compared with those from the time-series analysis [19]. Consistent results were found by using either the time-series or time-stratified case-crossover analysis. Our findings support and extend the previous study, demonstrating that time-stratified case-crossover design can also be used to estimate the event or episode-related (e.g., heatwave) health effects, and both time series and time-stratified case-crossover methods produced robust and comparable results.
Previous studies reported that increases in mortality and morbidity usually occurred within a short time frame after a heatwave [5], [25]–[28]. For example, in the 2003 French heatwave, relative risk for mortality increased rapidly in most cities during a 4-day period from 10 to 13 August [9]. Similarly, in the Chicago heatwave, there was the highest dose–response relationship for lags of 1 and 2 days of high minimum or maximum temperatures before all-cause mortality occurred, with an RR of 1.20 (95% CI: 1.15–1.27) for high temperature on lag day 1 and an indication of a cumulative effect (RR = 1.40; 95% CI:1.30–1.51) when temperatures stayed high both on lag days 1 and 2 [15]. In our study, we also found that exposure to heatwaves at the same day, lag 1 and lags 0–5 was strongly associated with risks of mortality and EHAs. The strongest heatwave effects appeared at lag 1 and lagged effects were gradually decreased after lag 1 for both EHAs and mortality (Figures 1 and 2).
Previous studies including our own research show an immediate impact of high temperature on the patients with cardiovascular diseases [29], suggesting that cardiovascular deaths tend to happen quickly during hot days because their ability to cope with heat is already compromised. Several pathophysiological mechanisms may explain this. Firstly, heat stress can reduce cerebral blood velocity and markedly impair orthostatic tolerance in humans [23], [30]. Secondly, water loss and reduced plasma volume during hot days may facilitate the release of platelets into circulation and increase red and white cell counts, blood viscosity, and plasma cholesterol levels, which may be connected to the increased mortality from arterial thrombosis in hot weather [31]. Finally, results from a mice study indicate that heat stress will stimulate cells of living organisms to generate heat shock proteins which may cause systematic damages in the body [32].
This study has three main strengths: (1) it is the first study to compare time series and case crossover analyses in the examination of heatwave effects on mortality and EHAs. Time-stratified case-crossover design is comparable to time series analysis in estimating event or episode-related health risks; (2) sophisticated statistical methods were used to assess lagged and cumulative average effects of heatwaves on both mortality and EHAs after adjustment for confounding factors; and (3) the datasets used is this study are quite comprehensive, with no missing values.
Several limitations of this study must also be acknowledged. We only focused on one city, so the results might not be generalisable to other areas. However, the approaches applied in this study can be used in further research in other areas. We only compared time series and case crossover analyses using the data on NEC mortality and EHAs. We did not use cause-specific mortality and morbidity because the number for each category was much smaller. Additionally, there might be exposure misclassification, as we used exposure data from fixed monitors rather than individual exposure data.
In conclusion, the results of this study demonstrate that both time-stratified case-crossover and time series analyses produced a similar pattern of the relationship between heatwave and health outcomes. This finding may have implications for future studies of event or episode-related health effects.
Supporting Information
The coefficients of temperature effects on mortality using different degrees of freedom for day of the year.
(TIFF)
Supplemental Material.
(DOCX)
Example dataset.
(CSV)
Acknowledgments
We thank the Queensland Health, Department of Environment and Resource Management, Office of Economic and Statistical Research of the Queensland Treasury, and Australia Bureau of Meteorology for providing the relevant data.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was funded by the Australian Research Council (DP0559655). ST was supported by a National Health and Medical Research Council (NHMRC) research fellowship (#553043). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Anderson GB, Bell ML. Heat Waves in the United States: Mortality Risk during Heat Waves and Effect Modification by Heat Wave Characteristics in 43 U.S. Communities. Environ Health Perspect. 2011;119:210–218. doi: 10.1289/ehp.1002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gasparrini A, Armstrong B. The impact of heat waves on mortality. Epidemiology. 2011;22:68–73. doi: 10.1097/EDE.0b013e3181fdcd99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fouillet A, Rey G, Wagner V, Laaidi K, Empereur-Bissonnet P, et al. Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int J Epidemiol. 2008;37:309–317. doi: 10.1093/ije/dym253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kovats RS, Hajat S, Wilkinson P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occupational and Environmental Medicine. 2004;61:893–898. doi: 10.1136/oem.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Michelozzi P, Accetta G, De Sario M, D'Ippoliti D, Marino C, et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am J Respir Crit Care Med. 2009;179:383–389. doi: 10.1164/rccm.200802-217OC. [DOI] [PubMed] [Google Scholar]
- 6.Argaud L, Ferry T, Le QH, Marfisi A, Ciorba D, et al. Short- and long-term outcomes of heatstroke following the 2003 heat wave in Lyon, France. Arch Intern Med. 2007;167:2177–2183. doi: 10.1001/archinte.167.20.ioi70147. [DOI] [PubMed] [Google Scholar]
- 7.Semenza JC, Rubin CH, Falter KH, Selanikio JD, Flanders WD, et al. Heat-related deaths during the July 1995 heat wave in Chicago. The New England Journal Of Medicine. 1996;335:84–90. doi: 10.1056/NEJM199607113350203. [DOI] [PubMed] [Google Scholar]
- 8.Fouillet A, Rey G, Jougla E, Frayssinet P, Bessemoulin P, et al. A predictive model relating daily fluctuations in summer temperatures and mortality rates. BMC Public Health. 2007;7:114. doi: 10.1186/1471-2458-7-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Le Tertre A, Lefranc A, Eilstein D, Declercq C, Medina S, et al. Impact of the 2003 heatwave on all-cause mortality in 9 French cities. Epidemiology. 2006;17:75–79. doi: 10.1097/01.ede.0000187650.36636.1f. [DOI] [PubMed] [Google Scholar]
- 10.Conti S, Meli P, Minelli G, Solimini R, Toccaceli V, et al. Epidemiologic study of mortality during the Summer 2003 heat wave in Italy. Environ Res. 2005;98:390–399. doi: 10.1016/j.envres.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 11.Johnson H, Kovats RS, McGregor G, Stedman J, Gibbs M, et al. The impact of the 2003 heat wave on mortality and hospital admissions in England. Health Stat Q. 2005:6–11. [PubMed] [Google Scholar]
- 12.Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117:61–67. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20:205–213. doi: 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hajat S, Armstrong B, Baccini M, Biggeri A, Bisanti L, et al. Impact of high temperatures on mortality: is there an added heat wave effect? Epidemiology. 2006;17:632–638. doi: 10.1097/01.ede.0000239688.70829.63. [DOI] [PubMed] [Google Scholar]
- 15.Kaiser R, Le Tertre A, Schwartz J, Gotway CA, Daley WR, et al. The effect of the 1995 heat wave in Chicago on all-cause and cause-specific mortality. Am J Public Health. 2007;97(Suppl 1):S158–162. doi: 10.2105/AJPH.2006.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stafoggia M, Forastiere F, Agostini D, Biggeri A, Bisanti L, et al. Vulnerability to Heat-Related Mortality: A Multicity, Population-Based, Case-Crossover Analysis. Epidemiology. 2006;17:315–323. doi: 10.1097/01.ede.0000208477.36665.34. [DOI] [PubMed] [Google Scholar]
- 17.Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events. Am J Epidemiol. 1991;133:144–153. doi: 10.1093/oxfordjournals.aje.a115853. [DOI] [PubMed] [Google Scholar]
- 18.Lumley T, Levy D. Bias in the case – crossover design: implications for studies of air pollution. Environmetrics. 2000;11:689–704. [Google Scholar]
- 19.Basu R, Dominici F, Samet JM. Temperature and mortality among the elderly in the United States - A comparison of epidemiologic methods. Epidemiology. 2005;16:58–66. doi: 10.1097/01.ede.0000147117.88386.fe. [DOI] [PubMed] [Google Scholar]
- 20.Levy D, Lumley T, Sheppard L, Kaufman J, Checkoway H. Referent selection in case-crossover analyses of acute health effects of air pollution. Epidemiology. 2001;12:186–192. doi: 10.1097/00001648-200103000-00010. [DOI] [PubMed] [Google Scholar]
- 21.QLD Queensland Government Population and Housing Fact sheet - Brisbane City Council. 2009. Available: http://www.oesr.qld.gov.au/queensland-by-theme/demography/population-characteristics/profiles/pop-housing-fact-sheets-lga/pop-housing-fact-sheets-brisbane-200908.pdf. Accessed 2009 Nov 26.
- 22.Tong S, Wang XY, Barnett AG. Assessment of heat-related health impacts in Brisbane, Australia: comparison of different heatwave definitions. PLoS One. 2010;5:e12155. doi: 10.1371/journal.pone.0012155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang XY, Barnett AG, Yu W, FitzGerald G, Tippett V, et al. The impact of heatwaves on mortality and emergency hospital admissions from non-external causes in Brisbane, Australia. Occup Environ Med. 2012;69:163–169. doi: 10.1136/oem.2010.062141. [DOI] [PubMed] [Google Scholar]
- 24.IPCC. Intergovernmental Panel on Climate Change. Climate Change 2007: Synthesis Report. Geneva, Switzerland. 2007. Available: http://www.ipcc.ch/pdf/assessment-report/ar4/syr/ar4_syr.pdf. Accessed 2009 Nov 26.
- 25.Basu R, Ostro BD. A multicounty analysis identifying the populations vulnerable to mortality associated with high ambient temperature in California. Am J Epidemiol. 2008;168:632–637. doi: 10.1093/aje/kwn170. [DOI] [PubMed] [Google Scholar]
- 26.Bell ML, O'Neill MS, Ranjit N, Borja-Aburto VH, Cifuentes LA, et al. Vulnerability to heat-related mortality in Latin America: a case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol. 2008;37:796–804. doi: 10.1093/ije/dyn094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ishigami A, Hajat S, Kovats RS, Bisanti L, Rognoni M, et al. An ecological time-series study of heat-related mortality in three European cities. Environmental Health. 2008;7:5. doi: 10.1186/1476-069X-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baccini M, Biggeri A, Accetta G, Kosatsky T, Katsouyanni K, et al. Heat effects on mortality in 15 European cities. Epidemiology. 2008;19:711–719. doi: 10.1097/EDE.0b013e318176bfcd. [DOI] [PubMed] [Google Scholar]
- 29.Huynen MM, Martens P, Schram D, Weijenberg MP, Kunst AE. The impact of heat waves and cold spells on mortality rates in the Dutch population. Environ Health Perspect. 2001;109:463–470. doi: 10.1289/ehp.01109463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson TE, Cui J, Zhang R, Crandall CG. Heat stress reduces cerebral blood velocity and markedly impairs orthostatic tolerance in humans. Am J Physiol Regul Integr Comp Physiol. 2006;291:R1443–1448. doi: 10.1152/ajpregu.00712.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Keatinge WR, Coleshaw SR, Easton JC, Cotter F, Mattock MB, et al. Increased platelet and red cell counts, blood viscosity, and plasma cholesterol levels during heat stress, and mortality from coronary and cerebral thrombosis. American Journal of Medicine. 1986;81:795–800. doi: 10.1016/0002-9343(86)90348-7. [DOI] [PubMed] [Google Scholar]
- 32.Li SQ, Li RF, Xi SM, Hu S, Jia ZQ, et al. Systematical analysis of impacts of heat stress on the proliferation, apoptosis and metabolism of mouse hepatocyte. J Physiol Sci. 2012;62:29–43. doi: 10.1007/s12576-011-0183-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The coefficients of temperature effects on mortality using different degrees of freedom for day of the year.
(TIFF)
Supplemental Material.
(DOCX)
Example dataset.
(CSV)