Abstract
Hereditary breast cancer comprises 10% of all breast cancers. The most prevalent genes causing this pathology are BRCA1 and BRCA2 (breast cancer early onset 1 and 2), which also predispose to other cancers. Despite the outstanding relevance of genetic screening of BRCA deleterious variants in patients with a history of familial cancer, this practice is not common in Latin American public institutions. In this work we assessed mutations in the entire exonic and splice-site regions of BRCA in 39 patients with breast and ovarian cancer and with familial history of breast cancer or with clinical features suggestive for BRCA mutations by massive parallel pyrosequencing. First we evaluated the method with controls and found 41–485 reads per sequence in BRCA pathogenic mutations. Negative controls did not show deleterious variants, confirming the suitability of the approach. In patients diagnosed with cancer we found 4 novel deleterious mutations (c.2805_2808delAGAT and c.3124_3133delAGCAATATTA in BRCA1; c.2639_2640delTG and c.5114_5117delTAAA in BRCA2). The prevalence of BRCA mutations in these patients was 10.2%. Moreover, we discovered 16 variants with unknown clinical significance (11 in exons and 5 in introns); 4 were predicted as possibly pathogenic by in silico analyses, and 3 have not been described previously. This study illustrates how massive pyrosequencing technology can be applied to screen for BRCA mutations in the whole exonic and splice regions in patients with suspected BRCA-related cancers. This is the first effort to analyse the mutational status of BRCA genes on a Mexican-mestizo population by means of pyrosequencing.
Introduction
About 10% of all breast cancers are of monogenic origin [1]. The most prevalent entity is Hereditary Breast and Ovarian Cancer (HBOC), an autosomal dominant disease with incomplete penetrance. The two high-penetrance genes most commonly mutated in HBOC are the tumor suppressor genes BRCA1 and BRCA2 (breast cancer, early onset 1 and 2). The BRCA1 gene, localized at 17q21, and BRCA2, at 13q12, have long coding sequences (5589 and 10254 nt for BRCA1 and BRCA2, respectively) and are essential components of the double-strand break repair by homologous recombination system [2]. Almost 3500 deleterious mutations in these genes have been found in all the coding sequence [3]. Furthermore BRCA1 and BRCA2 mutation carriers are also at increased risk of fallopian tubes, pancreatic, prostate and endometrial cancer [4]–[6].
The molecular diagnosis of mutations in BRCA genes implies high degree of clinical suspicion based principally in history of familial BRCA-related cancers in first- or second-degree relatives, age of presentation and tumor characteristics (morphological, immunohistochemical and molecular features) [7]. For patients with a BRCA mutation, current clinical alternatives include breast and ovarian screening, prophylactic surgery, and chemoprevention [8]. The approach extends to their family in order to identify other members at risk to allow the genetic advice, screening and/or predictive testing [9].
Unfortunately, genetic testing for mutations in BRCA1 and BRCA2 is not always available in public institutions in developing countries due to its high cost and limitations in infrastructure. As BRCA genes have long coding sequences and lack mutation hot spots, the current strategies for BRCA genotyping typically include a first step to detect occurring mutations by protein truncation test (PTT), denaturing high-performance liquid chromatography (dHPLC), denaturing gradient gel electrophoresis (DGGE) or high-resolution melting curve analysis (HRMCA); and a final step to determine the mutation by Sanger sequencing [10]. These approaches are laborious, expensive and time consuming, and could be substituted by high throughput, cost efficient testing methods such as massively parallel sequencing [11], [12].
In this work we used massive parallel pyrosequencing to screen for mutations in the complete coding regions and splice sites of BRCA genes in Mexican women. We studied 39 patients with breast and/or ovary cancer and with history of familial cancer and with early-onset breast cancer, suggestive for BRCA mutations. We found 4 pathogenic mutations, of which 3 have not been described. We also identified 16 missense mutations with unknown deleterious effects. In addition, by a directed sequencing strategy, we evaluated the presence of the deleterious mutations in the family members of the patients. Also, we identified family members with the mutations and with no clinical manifestations of cancer. These patients began clinical management (that includes follow-up and prophylactic measures). This work illustrates how new sequencing technology for screening of mutations in BRCA genes impacts the familial health scenario and can be conducted as part of the genetic approach for patients with familial cancer in public health care institutions.
Methods
Patients
A total of 39 patients were screened. Thirty-five female patients with breast and/or ovarian cancer and with two or more first- or second-degree relatives with tumors associated with BRCA mutations were studied. Two male patients with breast cancer were included. All patients were clinically approached and a three-generation genealogy of each family was made. Two patients without familial cancer history, one with early-onset (age of diagnosis: 28) breast cancer and one with breast and ovarian cancer, suggestive for BRCA mutations, were also included. Patients were fully informed about the study and gave their written consent. The protocol was approved by the Institutional Review Boards of the National Cancer Institute of Mexico (http://www.incan.edu.mx/) and carried out in accordance with the Declaration of Helsinki, good clinical practices, and local ethical and legal requirements.
DNA isolation
Genomic DNA was isolated of peripheral blood with the Magna Pure System (Roche) following manufacturer instructions. The integrity of the material was verified by agarose electrophoresis. Sample quantification was done with the Quant-it Picogreen kit (Invitrogen) in a QuantiFluor Fluorometer (Promega).
Pyrosequencing
A Sequencing Master library of amplicons covering all the coding exons and splice sites of BRCA1 and BRCA2 was produced for each patient using the BRCAMASTR kit (Multiplicom) following manufacturer instructions. Briefly, 50 ng of gDNA were used as template in each of 12 multiplex PCR reactions for each patient. These reactions amplified the complete exonic and splice sites of BRCA1 and BRCA2. A 1∶1000 dilution of the purified PCR products were re-amplified using molecular identification (MID) adaptors for each patient. A BRCA amplicon library of each patient was generated and equivalent concentrations of the libraries were pooled to generate a Sequencing Master library. Pyrosequencing of the Master libraries were done in the sense and anti-sense strands with the 454 GS Junior (Roche) technology. Data analysis was done with the GS Amplicon Variant Analyzer software (Roche) comparing against genomic references NG_005905 and NG_012772 for BRCA1 and BRCA2, respectively. The cDNA references utilized were NM_007294 and NM_000059 for BRCA1 and BRCA2, respectively. The nomenclature used is based on the cDNA sequence and is according to Human Genome Variation Society (http://www.hgvs.org/). All the deleterious mutations found were verified by Sanger sequencing of original patient blood DNA and by restriction analysis when possible. The putative functional effects of missense variants were analyzed in silico with PolyPhen-2 (http://genetics.bwh.harvard.edu/pph2/).
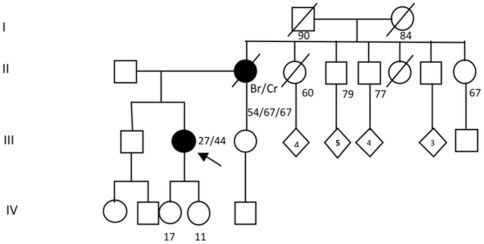
Restriction analysis
The presence of the mutation c.3124_3133delAGCAATATTA found in patient 11 was verified by restriction analysis of the PCR product (554 pb) amplified with the primers BRCA1-11.1F: TCAGAGGCAACGAAACTGGACTCA and BRCA1-11.1R: CAGCCTATGGGAAGTAGTCATGCA. The mutated allele lacks the restriction site for SspI (AATATT) and is not cleaved by this enzyme, while the wild-type allele is cleaved in two fragments (257 and 297 pb). 500 ng of PCR products were digested with 1 U of SspI (Fermentas) at 37°C for 4 h in 20 uL. Ten uL of the reactions were visualized in 1.5% agarose gels.
Results
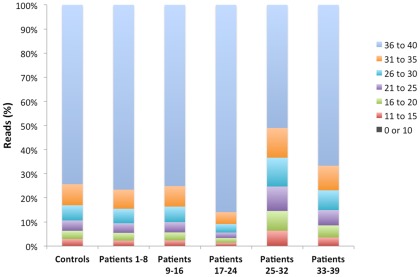
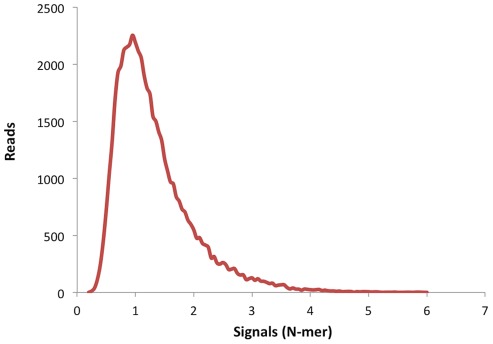
To analyze the performance of the amplicon strategy for the sequencing of BRCA genes we carried out an evaluation run with 6 patients' samples, of which 4 had previously identified mutations and 2 were negative controls [13]. We used three inclusion criteria to accept valid mutated sequences: 1) mutation found in forward and reverse sequences, 2) at least 30% of sequences with the mutations and 3) at least 20X of sequence coverage of the amplicons with the mutation. Also we defined three exclusion criteria: 1) mutations detected in an homopolymeric tract of ≥6, 2) mutations found in the last nucleotide of the sequence and with frequencies of less than 30% and 3) quality score lower than 20 in forward and reverse reads. Similar criteria have been described elsewhere [12]. As seen in table 1, we detected all the deleterious mutations in the positive controls and no pathogenic variants were found in the negative controls. In the mutations observed the minimal and maximal coverage was 41 and 485 reads per nucleotide, respectively. Also in this control experiment more than 70% of all the reads across the whole exon and splice sites had a quality score (Q) ranging from 36 to 40 (highest score), and low quality reads with Q>20 were less than 10% (Fig. 1). As expected, we observed that the majority of these low quality reads were in homopolymeric tracts, especially of >6 bases. Although present, these homopolymeric sequences are a negligible number of the total reads (Fig. 2). With this analysis we concluded that the strategy used was robust and suitable for its application in the screening of BRCA mutations in patients' samples.
Table 1. Evaluation of the methodological strategy for the detection of BRCA mutations.
| Sample | Gene | Deleterious Mutation | Type of mutationa | Position (aa) | Stop codón position (aa) | Coverage1 | Clinical relevance | BIC reported | Reference |
| Control (+)1 | BRCA1 | c.4065_4068delTCAA | F | 1355 | 1364 | 41 | Yes | Yes | [13], [47]–[49] |
| Control (+)2 | BRCA2 | c.2808_2811delACAA | F | 936 | 958 | 459 | Yes | Yes | [50] |
| Control (+)3 | BRCA2 | c.9382C>T | S | 3128 | 3128 | 485 | Yes | Yes | [51], [52] |
| Control (−)1 | - | None detected | - | - | - | - | - | - | - |
| Control (−)2 | - | None detected | - | - | - | - | - | - | - |
Number of reads per nucleotide.
Types of mutations: F: frameshift; S: stop.
Figure 1. Quality of the sequencing runs.
The percentages of the reads with their associated quality numbers of all runs are plotted.
Figure 2. Distribution of homopolymeric tracts across the reads.
The base number signals are plotted against the sequence reads of the control run.
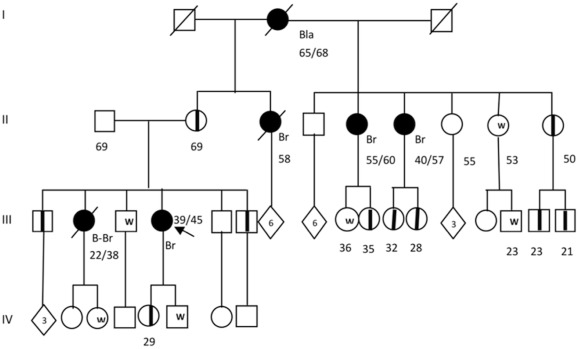
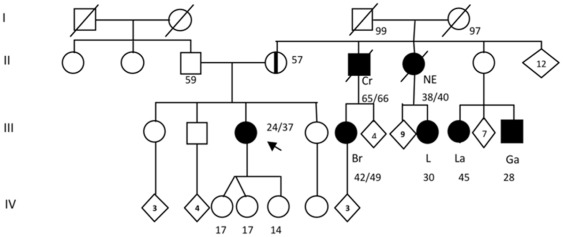
We screened for mutations in the whole coding sequence of BRCA genes in 39 patients with early-onset breast and ovarian tumors and/or with familial history of cancer, suggestive for BRCA mutations, as determined by our Clinic of Genetics. The main clinical characteristics of the patients are listed in table 2 and 3. After the pyrosequencing analysis and careful examination of the reads with our criteria of inclusion and exclusion, we found 4 mutations in the BRCA genes (c.2805_2808delAGAT and c.3124_3133delAGCAATATTA in BRCA1; c.2639_2640delTG and c.5114_5117delTAAA in BRCA2). All mutations were predicted to be deleterious because each generated a stop codon in the open reading frame (Table 4). These pathogenic mutations were confirmed by Sanger sequencing and the c.3124_3133delAGCAATATTA mutation in BRCA1 was also confirmed by restriction analysis (Fig 3). In the family of patient 1 (mutation c.5114_5117delTAAA) we found 10 clinically asymptomatic carriers (Fig. 4). The family with the c.2639_2640delTG mutation in BRCA2 (patient 15) had a strong history of cancer, including laryngeal, gastric, lung and colon cancer in second- and third-degree relatives in the maternal branch (Fig. 5). In the family with the c.2805delAGAT mutation in BRCA1 (patient 39), one first-degree relative had breast and colon cancer (Fig. 6). Interestingly, 3 of the 4 deleterious mutations have not been described previously. Likewise, we detected 16 genetic variants with unknown clinical significance (VUS), which included missense mutations and changes in intronic sequences (Table 5). Four VUS were predicted to be potentially deleterious by in silico analyzes (Table 5). Intronic variants that have been evaluated functionally through in vitro experiments by others were not present [14]. No Ashkenazi founder mutations were found.
Table 2. Clinical features of the patients with BRCA mutations.
| Sample | Age (years) | Cancer Type | Age diagnosis (years) | Familial cancer history | Tumor Histological Features | Other Tumor Features a |
| Patient 1 | 31 | Breast cancer | 31 | Yes | Canalicular carcinoma | ER positive, PR positive, Her2/neu positive |
| Patient 3 | 42 | Ovarian cancer | 33 | No | Ovarian serous adenocarcinoma | Not reported |
| Unilateral Breast cancer | 38 | Canalicular carcinoma | Triple negative | |||
| Patient 15 | 37 | Ovarian cancer | 24 | Yes | Ovarian serous adenocarcinoma | Not reported |
| Unilateral breast cancer (right) | 37 | Canalicular carcinoma, brisk lymphocytic infiltrate | ER positive, PR positive and Her2/neu negative Ki-67: 5% | |||
| Patient 39 | 44 | Bilateral breast cancer | 27 | Yes | Canalicular carcinoma | Triple negative |
ER = estrogen receptor; PR = progesterone receptor; HER2/neu = human epidermal growth factor receptor 2; Ki-67 = antigen KI 67.
Table 3. Clinical and familial features of the patients included in the study.
| Sample | Age (years) | Gender | Cancer Type | Tumor Histological Features | Other Tumor Features | Age diagnosis (years) | Familial cancer history | Family members with cancer | |||
| Number | Tumor type | Degree | Youngest age at diagnosis (years) | ||||||||
| Patient 1 | 31 | Female | Breast cancer | Canalicular carcinoma | ER (+), PR (+) and Her2/neu (+) | 31 | Yes | 5 | Bilateral BC, Unilateral BC Bladder cancer | 1st, 2nd and 3rd | 22 |
| Patient 2 | 35 | Female | Unilateral Breast cancer | Canalicular carcinoma | ER (+), PR (+) and Her2/neu (−) | 30 | Yes | 5 | Breast cancer. Colorectal cancer | 1st and 2nd | 36 |
| Patient 3 | 42 | Female | Ovarian cancer | Ovarian serous adenocarcinoma | Not reported | 33 | No | ||||
| Unilateral Breast cancer | Canalicular carcinoma | Triple negative | 38 | ||||||||
| Patient 4 | 40 | Female | Unilateral breast cancer | In situ, canalicular carcinoma | ER (+), PR (+) and Her2/neu (−) | 38 | Yes | 3 | Breast cancer | 1st and 2nd | 42 |
| Patient 5 | 64 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (+), PR (+) | 63 | Yes | 2 | Breast cancer | 1st | 51 |
| Patient 6 | 66 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (+), PR (+) | 53 | Yes | 10 | Breast cancer. Ovarian cancer. Lymphoma. Intestinal cancer. | 1st, 2nd and 3rd. | 40 |
| Patient 7 | 29 | Female | Unilateral breast cancer | Canalicular carcinoma | Triple negative | 28 | Yes | 5 | Breast, pancreatic, colorectal and bladder cancer | 2nd | 47 |
| Patient 8 | 48 | Female | Breast cancer | Canalicular carcinoma | NA | 47 | Yes | 2 | Breast cancer. Ovarian cancer. | 1st | 41 |
| Patient 9 | 42 | Female | Breast cancer | Canalicular carcinoma | NA | 41 | Yes | 2 | Breast cancer. Ovarian cancer | 1st | 45 |
| Patient 10 | 68 | Female | Breast cancer | Canalicular carcinoma | ER (+), PR (+) | 60 | Yes | 13 | Breast, pancreatic, lung, liver and colorectal cancer | 2nd and 3rd | 44 |
| Patient 11 | 53 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (+), PR (+) and Her2/neu (−) | 49 | Yes | 13 | Breast, pancreatic, lung, liver and colorectal cancer | 2nd and 3rd | 44 |
| Patient 12 | 68 | Male | Unilateral breast cancer and colorectal cancer | Breast: Canalicular carcinoma. | NA | Colorectal cancer: 52 Breast cancer: 56 | Yes | 1 | Breast cancer | 1st | 39 |
| Patient 13 | 62 | Female | Bilateral breast cancer | Multifocal, canalicular carcinoma | ER (+), PR (+) and Her2/neu (−) | 1st: 48, 2nd: 60 | Yes | 5 | Breast, ovarian and skin cancer | 1st and 2nd | 36 |
| Patient 14 | 37 | Female | Unilateral breast cancer | Canalicular carcinoma | Triple negative | 35 | Yes | 6 | Breast, prostatic and renal cancer | 1st and 2nd | 28 |
| Patient 15 | 37 | Female | Ovarian cancer | Ovarian serous adenocarcinoma | Not reported | 24 | Yes | 6 | Breast, laryngeal, lung, gastric and colorectal. | 2nd and 3rd | 28 |
| Unilateral breast cancer (right) | Canalicular carcinoma, brisk lymphocytic infiltrate | ER (+), PR (+) and Her2/neu (−) | 37 | ||||||||
| Patient 16 | 30 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (+), PR (+) and Her2/neu (−) | 28 | Yes | 1 | Abdominal cancer (NA) | 1st | 31 |
| Patient 17 | 33 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (+), PR (+) and Her2/neu (−) | 30 | Yes | 1 | Breast and ovarian cancer | 1st | 55 |
| Patient 18 | 42 | Female | Bilateral breast cancer | Canalicular carcinoma | Triple negative (both tumors) | 1st: 34, 2nd: 39 | Yes | 1 | Breast cancer | 1st | 41 |
| Patient 19 | 39 | Female | Unilateral breast cancer | Canalicular carcinoma | Triple negative | 36 | Yes | 7 | Breast cancer | 1st, 2nd and 3rd | <40 (NA) |
| Patient 20 | 65 | Male | Unilateral breast cancer | Lobulillar carcinoma | Triple negative, androgen negative | 63 | Yes | 1 | Ovarian cancer | 1st | 44 |
| Patient 21 | 28 | Female | Unilateral breast cancer | Canalicular carcinoma | Triple negative | 27 | Yes | 2 | Laringeal cancer and abdominal caáncer (NA) | 2nd | 50 |
| Patient 22 | 35 | Female | Unilateral breast cancer | Canalicular carcinoma | Triple negative | 32 | Yes | 2 | Prostatic cancer | 2nd | 58 |
| Patient 23 | 33 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (+), PR (+) and Her2/neu (+) | 32 | NA (no contact with family) | NA | NA | NA | - |
| Patient¶24 | 58 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (−), PR (−) and Her2/neu (+) | 56 | Yes | 2 | Breast and colorectal cancer | 1st | 33 |
| Patient 25 | 48 | Female | Unilateral breast cancer | Canalicular carcinoma | NA | 37 | Yes | 2 | Breast and gastric cancer | 2nd | 40 |
| Patient 26 | 31 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (+), PR (+) and Her2/neu (+) | 29 | Yes | 4 | Skin, laringeal and intestinal cancer | 2nd and 3rd | 35 |
| Patient 27 | 35 | Female | Unilateral breast cancer | Canalicular carcinoma | Triple negative | 33 | Yes | 1 | Abdominal cancer (NA) | 2nd | 30 |
| Patient 28 | 30 | Female | Unilateral breast cancer | Canalicular carcinoma | Triple negative | 25 | Yes | 4 | Brest, gastric and thyroid cancer | 2nd | 30 |
| Patient 29 | 53 | Female | Bilateral breast cancer | Canalicular carcinoma | Triple negative | 52 | Yes | 5 | Bilateral and unilateral breast cancer. Liver cancer | 1st, 2nd and 3rd | 40 |
| Patient 30 | 25 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (+), PR (+) and Her2/neu (+) | 24 | Yes | 10 | Breast cancer. Prostatic cancer | 1st and 2nd | 41 |
| Patient 31 | 41 | Female | Unilateral breast cancer | Multifocal, canalicular carcinoma | ER (+), PR (+) and Her2/neu (−) | 39 | Yes | 5 | Breast and gastric cancer | 1st and 2nd | 38 |
| Patient 32 | 46 | Female | Ovarian cancer | Endometrioid carcinoma | Not reported | 42 | Yes | 4 | Breast cancer. Ovarian cancer | 1st and 2nd | 30 |
| Patient 33 | 61 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (+), PR (+) and Her2/neu (−) | 56 | Yes | 3 | Breast cancer (Father with breast cancer) | 1st and 2nd | 31 |
| Patient 34 | 28 | Female | Unilateral breast cancer | Canalicular carcinoma | ER (+), PR (+) and Her2/neu (−) | 27 | NA (no contact with family) | NA | NA | NA | - |
| Patient 35 | 52 | Female | Unilateral breast cancer + NF-1 | Canalicular carcinoma | ER positive, PR (+)and Her2/neu (−) | 46 | Yes | 2 | Breast cancer. Liver cancer | 1st | 49 |
| Patient 36 | 60 | Female | Unilateral breast cancer + NF-1 | Canalicular carcinoma | Triple negative | 49 | Yes | 2 | Breast cancer. Liver cancer | 1st | 46 |
| Patient 37 | 40 | Female | Unilateral breast cancer | Canalicular carcinoma | Triple negative | 36 | No | - | - | - | - |
| Patient 38 | 39 | Female | Unilateral breast cancer | Canalicular carcinoma | Triple negative | 35 | No | - | - | - | - |
| Patient 39 | 44 | Female | Bilateral breast cancer | Canalicular carcinoma | Triple negative | 1st: 27, 2nd: 33 | Yes | 1 | Breast and colorectal cancer | 1st | 54 |
ER = estrogen receptor; PR = progesterone receptor; HER2/neu = human epidermal growth factor receptor 2.
NA: Information not available.
NF-1: Neurofibromatosis type 1
Table 4. Detection of BRCA deleterious mutations in patients.
| Sample | Gene | Mutation | Type of mutation | Position (aa) | Stop position (aa) | Coverage1 | Clinical relevance | BIC reported | References |
| Patient 3 | BRCA1 | c.3124_3133delAGCAATATTA | F | 1042 | 1047 | 77 | Yes | No | Not reported |
| Patient 39 | BRCA1 | c.2805_2808del AGAT | F | 935 | 998 | 21 | Yes | No | Not reported |
| Patient 1 | BRCA2 | c.5114_5117delTAAA | F | 1705 | 1710 | 70 | Yes | Yes | [53] |
| Patient 15 | BRCA2 | c.2639_2640delTG | F | 880 | 888 | 29 | Yes | No | Not reported |
Number of reads per nucleotide.
Types of mutations: F: frameshift; S: stop.
Figure 3. Restriction analysis of the mutation c.3124_3133delAGCAATATTA found in patient 3.
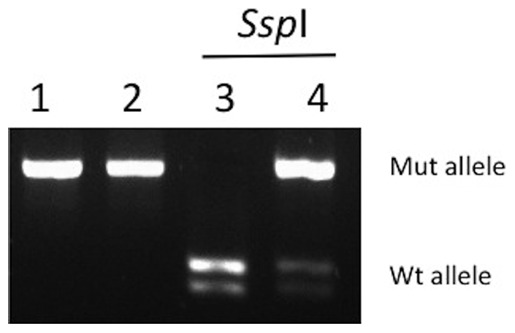
PCR products encompassing the mutation were digested with SspI (see methods). The mutated allele has lost the SspI site and is not cleaved by the enzyme, while the wild-type allele is cut in two fragments. Lanes: 1) wild-type control PCR product not digested, 2) patient 11 PCR product not digested, 3) wild-type control PCR product digested, 4) patient 11 PCR product digested. Mut: mutated; Wt: wild-type.
Figure 4. Genealogy of the family 1 carrier of the deleterious mutation c.5114_5117delTAAA in BRCA2.
Index patient is denoted with an arrow. Individuals with cancer are represented with in dark circles or with dark squares; the type of cancer is indicated as follows: Bla: Bladder cancer; Br: Unilateral Breast Cancer; B-Br: Bilateral breast cancer. Current age or known ages of cancer diagnosis and decease are showed. Numbers inside the rhombi indicate quantity of relatives. Asymptomatic carriers are represented with a midline. Unaffected family members confirmed by the predictive molecular testing are shown with a W (wild type).
Figure 5. Genealogy of the family 15 carrier of the deleterious mutation c.2639_2640delTG in BRCA2.
Individuals with cancer are represented with dark circles or with dark squares; the type of cancer is indicated as follows: Br: unilateral breast cancer; Cr: colorectal cancer; NE: Not especified neoplasia; L: lung cancer; La: laryngeal cancer; Ga: gastric cancer. Index patient is denoted with an arrow. Current age or known ages of cancer diagnosis and decease are showed. Numbers inside the rhombi indicate quantity of first-degree relatives. Asymptomatic carriers are represented with a midline.
Figure 6. Genealogy of the family 39 carrier of the deleterious mutation c.2805_2808delAGAT in BRCA1.
Index patient is denoted with an arrow. Individuals with cancer are represented in dark; the type of cancer is indicated as follows: Br: unilateral breast cancer; Cr: colorectal cancer. Current age or known ages of cancer diagnosis and decease are showed. Numbers inside the rhombi indicate quantity of relatives.
Table 5. Variants of uncertain significance (VUS) detected in patients.
| Patient | Gene | Localization | Variant | Type of Mutation11 | Clinical Relevance | PolyPhen2 prediction2 | BIC Reported |
| 2, 26, 31, 33 | BRCA2 | Exon 27 | p.I3412V | M | VUS | B | Yes |
| 5, 26, 30 | BRCA1 | Exon 11 | p.Q356R | M | VUS | PD | Yes |
| 6 | BRCA2 | Exon 11 | p.H1561N | M | VUS | PD | Yes |
| 6 | BRCA2 | Exon 11 | p.V2138F | M | VUS | B | Yes |
| 7 | BRCA1 | Exon 11 | p.S1040N | M | VUS | B | Yes |
| 10, 13, 14, 18, 26, 27, 28, 30, 31, 39 | BRCA1 | Intron 1 | c.−19T>C | Ts | VUS | - | Yes |
| 10, 11, 17 | BRCA1 | Exon 11 | p.K1183R | M | Not reported | B | No |
| 10, 15, 16, 17 | BRCA2 | Intron 11 | c.6841+80del TTAA | D | VUS | - | Yes |
| 12, 17 | BRCA1 | Intron 7 | c.442−34C>T | Ts | VUS | - | Yes |
| 12 | BRCA1 | Exon 11 | p.D1344G | M | VUS | PD | Yes |
| 16 | BRCA2 | Exon 11 | p.T1915M | M | VUS | B | Yes |
| 17 | BRCA1 | Exon 12 | p.K1489E | M | Not reported | B | No |
| 18, 20, 39 | BRCA1 | Intron 12 | c.4097−141A>C | Tv | VUS | - | Yes |
| 18 | BRCA1 | Intron 14 | c.4485−64C>G | Tv | VUS | - | Yes |
| 19, 20, 21, 24, 27, 28, 31 | BRCA2 | Exon 15 | p.I2490T | M | VUS | B | Yes |
| 21 | BRCA1 | Exon 23 | p.V1810V | S | Not reported | B | No |
| 30 | BRCA1 | Exon 23 | p.V1804D | M | VUS | B | Yes |
| 30 | BRCA2 | Exon 11 | p.S1733S | S | VUS | B | Yes |
| 30 | BRCA2 | Exon 21 | K2950N | M | VUS | PD | Yes |
D: deletion; M: missense mutation; S: synonimous mutation; Ts: transition; Tv: transvertion.
B: benign; PD: probably damaging.
Discussion
Molecular genetic testing of germline mutations in BRCA genes is not common in public institutions in Latin America due to its high costs and limitations in infrastructure. Current protocols for BRCA mutation detection are time consuming and laborious, which makes difficult their implementation in developing countries. Also, the polymorphic nature of BRCA genes, their long size and lack of hot mutation spots highlight the necessity to implement new high throughput diagnostic methodologies. Almost 10% of breast cancer is associated to hereditary mutations [15]. Likewise, the lifetime risk of developing breast cancer is been reported as high as 80% and 50% for BRCA1 and BRCA2 mutation carriers, respectively; although it varies between different populations and ethnicities [16], [17]. In this light, BRCA genetic testing is of major diagnostic relevance not only because it provides a clinical preventive approach to family members before the development of cancer, but also can imply novel treatment strategies for affected patients, such as the use of poly-(ADP–ribose) polymerase inhibitors [18]–[20]. Additionally, BRCA genetic tests are central for the determination of founder mutations, which are frequent deleterious variants that can be screened in the population in first-line directed studies to reduce costs and accelerate diagnosis [21], [22]. In the Mexican population no founder mutations have been described.
In these work we analysed BRCA full exome and splice site mutations by massive parallel pyrosequencing. In the evaluation of the method, we found all the mutations present in previously characterized positive controls; negative controls showed no variants. The coverage of the sequences for the mutations varied from 41 to 485X, with quality scores of 20–40 in 95% of the reads throughout all the exonic and splice sites regions. These results led us to evaluate mutations in patients with hereditary breast and ovarian cancer syndrome and in patients with clinical features suggestive for BRCA deleterious mutations. In these analyses we found 4 (10.2%) BRCA mutations in the 39 patients, which is very similar to the prevalence reported by other studies of families with hereditary cancer in Latin America [13], [23], [24]. All the mutations found in these patients have not been previously described and are not reported in the Breast Cancer Information core (BIC) and NCBI variant databases, which is in concordance with the polymorphic nature of these genes [25]. Interestingly, one of these mutations was in a patient with no history of familial cancer, but with strong suggestive clinical manifestations of a BRCA mutation, such as early-onset breast cancer [26]. This result highlights the necessity to extend the screening for BRCA mutations also to candidate patients with no history of familial cancer, which is in concordance with reports that described that 30–50% of BRCA mutation carriers have not family history of breast and ovarian cancer [27], [28]. Remarkably, we found 10 clinically asymptomatic BRCA2 mutation (c.5114_5117delTAAA) carriers in family 1, which reflects the incomplete penetrance associated with different BRCA mutations and that there are other risk factors associated with the penetrance of BRCA mutations [29]–[32]. In this study we used massive parallel pyrosequencing because its capacity to screen the whole exonic and splice site regions of BRCA1 and BRCA2 in up to 8 samples per run and its high depth of sequence, which provides more sensitivity for mutation detection than conventional Sanger sequencing and makes this strategy cost-effective [33]. Also, these advantages offer great benefit to the diagnostic scenario, comparing to other methods. However, this technology has intrinsic limitations, namely the detection of whole exon deletions and the identification of mutations in homopolymeric tracts longer than 6 bases. Since the frequency of exon deletion and large genomic rearrangements is population-dependent and has been described as 1–30% in BRCA-associated cancers, it is determinant to further evaluate putative BRCA mutation-negative samples by complementary methods, such as Multiplex Ligation-dependent Probe Amplification analysis [34]–[36]. Also the evaluation of homopolymeric tract variants, which comprise 12 stretches longer than 6 nt in the BRCA1 and BRCA2 coding sequences, should be assessed with alternative methods such as high-resolution-melting-curve-analysis [37]. When negative, these analyzes would rule out the BRCA etiology of the tumor. Thus, in these patients with clear familial history of cancer, the evaluation of mutations in other genes, like PALB2, CHEK2 and RAD51C, should also be considered [38]–[41]. This could be the case of some of the families of this study, in which we screened 35 patients with a clear familial history of cancer, but we only found 3 patients with mutations in BRCA. Additionally, the presence of VUS could be related to pathogenic effects at the level of mRNA processing, stability, translation and protein function, as has been described in BRCA1 and other genes [42]–[46]. The effect of VUS is subject of great interest as their presence exceeds mutations in patients with familial cancer; however, their functional evaluation is far from being a common diagnostic practice. In this regard, the functional evaluation of some VUS in the BRCA genes has showed that single nucleotide variations in introns can influence mRNA processing, producing exon skipping and aberrant out of frame mRNA forms [14]. We found 16 not previously described VUS, especially in patients without deleterious BRCA variants and 4 were predicted to be pathogenic by computational analyses. Functional studies must be undertaken to evaluate their effects. In this concern, we foresee that new routine methods will soon be accessible to determine the molecular and pathological relevance of these variants.
In summary, this work illustrates how hole exonic and splice site massive parallel pyrosequencing can be used as a diagnostic strategy to determine BRCA mutations. Its use circumvents the laborious and time-consuming efforts of the current methodologies. With this technology we found 4 mutations and 16 VUS in our series of patients with familial cancer, which highlights the relevance of this approach as a diagnostic tool and suggests it could be used as a routine practice in public health institutions.
Acknowledgments
We thank Omar Ruvalcaba and Gabriel Hernandez for technical assistance during the course of this work. This manuscript was submitted in partial fulfilment of the requirements for the M.Sc degree for RMAG at Posgrado en Ciencias Biológicas, Universidad Nacional Autónoma de México.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by federal funds SALUD-2010-01-141907 (http://www.conacyt.mx/) and by National Cancer Instite of Mexico funds (www.incan.edu.mx/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Meindl A, Ditsch N, Kast K, Rhiem K, Schmutzler R. Hereditary Breast and Ovarian Cancer: New Genes, New Treatments, New Concepts. Deutsches Ärzteblatt International. 2011;108:323. doi: 10.3238/arztebl.2011.0323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Narod SA, Foulkes WD. BRCA1 and BRCA2: 1994 and beyond. Nat Rev Cancer. 2004;4:665–676. doi: 10.1038/nrc1431. doi: 10.1038/nrc1431. [DOI] [PubMed] [Google Scholar]
- 3.Petrucelli N, Daly MB, Feldman GL. Hereditary breast and ovarian cancer due to mutations in BRCA1 and BRCA2. Genetics in Medicine. 2010;12:245–259. doi: 10.1097/GIM.0b013e3181d38f2f. doi: 10.1097/GIM.0b013e3181d38f2f. [DOI] [PubMed] [Google Scholar]
- 4.Medeiros F, Muto MG, Lee Y, Elvin JA, Callahan MJ, et al. The tubal fimbria is a preferred site for early adenocarcinoma in women with familial ovarian cancer syndrome. Am J Surg Pathol. 2006;30:230–236. doi: 10.1097/01.pas.0000180854.28831.77. [DOI] [PubMed] [Google Scholar]
- 5.Lynch HT, Deters CA, Snyder CL, Lynch JF, Villeneuve P, et al. BRCA1 and pancreatic cancer: pedigree findings and their causal relationships. Cancer Genet Cytogenet. 2005;158:119–125. doi: 10.1016/j.cancergencyto.2004.01.032. doi: 10.1016/j.cancergencyto.2004.01.032. [DOI] [PubMed] [Google Scholar]
- 6.Edwards SM, Kote-Jarai Z, Meitz J, Hamoudi R, Hope Q, et al. Two percent of men with early-onset prostate cancer harbor germline mutations in the BRCA2 gene. Am J Hum Genet. 2003;72:1–12. doi: 10.1086/345310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pruthi S, Gostout BS, Lindor NM. Identification and management of women with BRCA mutations or hereditary predisposition for breast and ovarian cancer. Mayo Clinic Proceedings. 2010;85:1111–1120. doi: 10.4065/mcp.2010.0414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paradiso A, Formenti S. Hereditary breast cancer: clinical features and risk reduction strategies. Annals of Oncology. 2011;22:i31–i36. doi: 10.1093/annonc/mdq663. doi: 10.1093/annonc/mdq663. [DOI] [PubMed] [Google Scholar]
- 9.Clark AS, Domchek SM. Clinical management of hereditary breast cancer syndromes. J Mammary Gland Biol Neoplasia. 2011;16:17–25. doi: 10.1007/s10911-011-9200-x. doi: 10.1007/s10911-011-9200-x. [DOI] [PubMed] [Google Scholar]
- 10.Gerhardus A, Schleberger H, Schlegelberger B, Gadzicki D. Diagnostic accuracy of methods for the detection of BRCA1 and BRCA2 mutations: a systematic review. Eur J Hum Genet. 2007;15:619–627. doi: 10.1038/sj.ejhg.5201806. doi: 10.1038/sj.ejhg.5201806. [DOI] [PubMed] [Google Scholar]
- 11.Wang G, Beattie MS, Ponce NA, Phillips KA. Eligibility criteria in private and public coverage policies for BRCA genetic testing and genetic counseling. Genetics in Medicine. 2011;13:1045–1050. doi: 10.1097/GIM.0b013e31822a8113. doi: 10.1097/GIM.0b013e31822a8113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Leeneer K, Hellemans J, De Schrijver J, Baetens M, Poppe B, et al. Massive parallel amplicon sequencing of the breast cancer genes BRCA1 and BRCA2: opportunities, challenges, and limitations. Hum Mutat. 2011;32(3):335–344. doi: 10.1002/humu.21428. [DOI] [PubMed] [Google Scholar]
- 13.Vidal-Millán S, Taja-Chayeb L, Gutiérrez-Hernández O, Ramírez U, Robles-Vidal C, et al. Mutational analysis of BRCA1 and BRCA2 genes in Mexican breast cancer patients. European journal of gynaecological oncology. 2009;30:527. [PubMed] [Google Scholar]
- 14.Théry J, Krieger S, Gaildrat P, Révillion F. Contribution of bioinformatics predictions and functional splicing assays to the interpretation of unclassified variants of the BRCA genes. Eur J Hum Genet. 2011;19(10):1052–1058. doi: 10.1038/ejhg.2011.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Szabo CI, King M-C. Hum Mol Genet 4 Spec No; 1995. Inherited breast and ovarian cancer. pp. 1811–1817. [DOI] [PubMed] [Google Scholar]
- 16.Easton DF, Ford D, Bishop DT. Breast and ovarian cancer incidence in BRCA1-mutation carriers. Breast Cancer Linkage Consortium. Am J Hum Genet. 1995;56:265–271. [PMC free article] [PubMed] [Google Scholar]
- 17.Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. Journal of Clinical Oncology. 2007;25:1329–1333. doi: 10.1200/JCO.2006.09.1066. doi: 10.1200/JCO.2006.09.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kwon JS, Daniels MS, Sun CC, Lu KH. Preventing future cancers by testing women with ovarian cancer for BRCA mutations. Journal of Clinical Oncology. 2010;28:675–682. doi: 10.1200/JCO.2008.21.4684. doi: 10.1200/JCO.2008.21.4684. [DOI] [PubMed] [Google Scholar]
- 19.Trainer AH, Lewis CR, Tucker K, Meiser B, Friedlander M, et al. The role of BRCA mutation testing in determining breast cancer therapy. Nature Publishing Group. 2010;7:708–717. doi: 10.1038/nrclinonc.2010.175. doi: 10.1038/nrclinonc.2010.175. [DOI] [PubMed] [Google Scholar]
- 20.Tutt A, Robson M, Garber JE, Domchek SM, Audeh MW, et al. Oral poly (ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept trial. Lancet. 2010;376:235–244. doi: 10.1016/S0140-6736(10)60892-6. [DOI] [PubMed] [Google Scholar]
- 21.Ferla R, Calò V, Cascio S, Rinaldi G, Badalamenti G, et al. Founder mutations in BRCA1 and BRCA2 genes. Ann Oncol. 2007;18(Suppl 6):vi93–8. doi: 10.1093/annonc/mdm234. doi: 10.1093/annonc/mdm234. [DOI] [PubMed] [Google Scholar]
- 22.Zhang L, Kirchhoff T, Yee CJ, Offit K. A rapid and reliable test for BRCA1 and BRCA2 founder mutation analysis in paraffin tissue using pyrosequencing. J Mol Diagn. 2009;11:176–181. doi: 10.2353/jmoldx.2009.080137. doi: 10.2353/jmoldx.2009.080137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ruiz-Flores P, Sinilnikova OM, Badzioch M, Calderon-Garcidueñas AL, Chopin S, et al. BRCA1 and BRCA2 mutation analysis of early-onset and familial breast cancer cases in Mexico. Hum Mutat. 2002;20:474–475. doi: 10.1002/humu.9084. doi: 10.1002/humu.9084. [DOI] [PubMed] [Google Scholar]
- 24.Gutiérrez Espeleta G, Llacuachaqui M, García-Jiménez L, Aguilar Herrera M, Loáiciga Vega K, et al. Clinical Genetics; 2011. BRCA1 and BRCA2 mutations among familial breast cancer patients from Costa Rica. doi: 10.1111/j.1399-0004.2011.01774.x. [DOI] [PubMed] [Google Scholar]
- 25.Lips EH, Laddach N, Savola SP, Vollebergh MA, Oonk AM, et al. Quantitative copy number analysis by Multiplex Ligation-dependent Probe Amplification (MLPA) of BRCA1-associated breast cancer regions identifies BRCAness. Breast Cancer Res. 2011;13:R107. doi: 10.1186/bcr3049. doi: 10.1186/bcr3049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Musolino A, Bella MA, Bortesi B, Michiara M, Naldi N, et al. BRCA mutations, molecular markers, and clinical variables in early-onset breast cancer: a population-based study. Breast. 2007;16:280–292. doi: 10.1016/j.breast.2006.12.003. doi: 10.1016/j.breast.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 27.de Sanjosé S, Léoné M, Bérez V, Izquierdo A, Font R, et al. Prevalence of BRCA1 and BRCA2 germline mutations in young breast cancer patients: a population-based study. Int J Cancer. 2003;106:588–593. doi: 10.1002/ijc.11271. doi: 10.1002/ijc.11271. [DOI] [PubMed] [Google Scholar]
- 28.Møller P, Hagen AI, Apold J, Maehle L, Clark N, et al. Genetic epidemiology of BRCA mutations-family history detects less than 50% of the mutation carriers. Eur J Cancer. 2007;43:1713–1717. doi: 10.1016/j.ejca.2007.04.023. [DOI] [PubMed] [Google Scholar]
- 29.Thompson D, Easton D, Breast Cancer Linkage Consortium. Variation in cancer risks, by mutation position, in BRCA2 mutation carriers. Am J Hum Genet. 2001;68:410–419. doi: 10.1086/318181. doi: 10.1086/318181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lecarpentier J, Noguès C, Mouret-Fourme E, Stoppa-Lyonnet D, Lasset C, et al. Variation in breast cancer risk with mutation position, smoking, alcohol, and chest X-ray history, in the French National BRCA1/2 carrier cohort (GENEPSO). Breast Cancer Res Treat. 2011;130:927–938. doi: 10.1007/s10549-011-1655-3. doi: 10.1007/s10549-011-1655-3. [DOI] [PubMed] [Google Scholar]
- 31.Milne RL, Osorio A, Ramón y Cajal T, Baiget M, Lasa A, et al. Parity and the risk of breast and ovarian cancer in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res Treat. 2010;119:221–232. doi: 10.1007/s10549-009-0394-1. doi: 10.1007/s10549-009-0394-1. [DOI] [PubMed] [Google Scholar]
- 32.Nkondjock A, Robidoux A, Paredes Y, Narod SA, Ghadirian P. Diet, lifestyle and BRCA-related breast cancer risk among French-Canadians. Breast Cancer Res Treat. 2006;98:285–294. doi: 10.1007/s10549-006-9161-8. doi: 10.1007/s10549-006-9161-8. [DOI] [PubMed] [Google Scholar]
- 33.Gilles A, Meglécz E, Pech N, Ferreira S, Malausa T, et al. Accuracy and quality assessment of 454 GS-FLX Titanium pyrosequencing. BMC Genomics. 2011;12:245. doi: 10.1186/1471-2164-12-245. doi: 10.1186/1471-2164-12-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hofmann W, Görgens H, John A, Horn D, Hüttner C, et al. Screening for large rearrangements of the BRCA1 gene in German breast or ovarian cancer families using semi-quantitative multiplex PCR method. Hum Mutat. 2003;22:103–104. doi: 10.1002/humu.9154. [DOI] [PubMed] [Google Scholar]
- 35.Montagna M, Dalla Palma M, Menin C, Agata S, De Nicolo A, et al. Genomic rearrangements account for more than one-third of the BRCA1 mutations in northern Italian breast/ovarian cancer families. Hum Mol Genet. 2003;12:1055–1061. doi: 10.1093/hmg/ddg120. [DOI] [PubMed] [Google Scholar]
- 36.Ewald IP, Ribeiro PLI, Palmero EI, Cossio SL, Giugliani R, et al. Genomic rearrangements in BRCA1 and BRCA2: A literature review. Genet Mol Biol. 2009;32:437–446. doi: 10.1590/S1415-47572009005000049. doi: 10.1590/S1415-47572009005000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.De Leeneer K, Coene I, Poppe B, De Paepe A, Claes K. Genotyping of frequent BRCA1/2 SNPs with unlabeled probes: a supplement to HRMCA mutation scanning, allowing the strong reduction of sequencing burden. J Mol Diagn. 2009;11:415–419. doi: 10.2353/jmoldx.2009.090032. doi: 10.2353/jmoldx.2009.090032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blanco A, la Hoya de M, Balmaña J, Ramón y Cajal T, Teulé A, et al. Breast Cancer Res Treat; 2011. Detection of a large rearrangement in PALB2 in Spanish breast cancer families with male breast cancer. doi: 10.1007/s10549-011-1842-2. [DOI] [PubMed] [Google Scholar]
- 39.Manoukian S, Peissel B, Frigerio S, Lecis D, Bartkova J, et al. Two new CHEK2 germ-line variants detected in breast cancer/sarcoma families negative for BRCA1, BRCA2, and TP53 gene mutations. Breast Cancer Res Treat. 2011;130:207–215. doi: 10.1007/s10549-011-1548-5. doi: 10.1007/s10549-011-1548-5. [DOI] [PubMed] [Google Scholar]
- 40.Meindl A, Hellebrand H, Wiek C, Erven V, Wappenschmidt B, et al. Germline mutations in breast and ovarian cancer pedigrees establish RAD51C as a human cancer susceptibility gene. Nat Genet. 2010;42:410–414. doi: 10.1038/ng.569. doi: 10.1038/ng.569. [DOI] [PubMed] [Google Scholar]
- 41.Vuorela M, Pylkäs K, Hartikainen JM, Sundfeldt K, Lindblom A, et al. Further evidence for the contribution of the RAD51C gene in hereditary breast and ovarian cancer susceptibility. Breast Cancer Res Treat. 2011;130:1003–1010. doi: 10.1007/s10549-011-1677-x. doi: 10.1007/s10549-011-1677-x. [DOI] [PubMed] [Google Scholar]
- 42.Liu HX, Cartegni L, Zhang MQ, Krainer AR. A mechanism for exon skipping caused by nonsense or missense mutations in BRCA1 and other genes. Nat Genet. 2001;27:55–58. doi: 10.1038/83762. doi: 10.1038/83762. [DOI] [PubMed] [Google Scholar]
- 43.Carvalho MA, Marsillac SM, Karchin R, Manoukian S, Grist S, et al. Determination of cancer risk associated with germ line BRCA1 missense variants by functional analysis. Cancer Res. 2007;67:1494–1501. doi: 10.1158/0008-5472.CAN-06-3297. doi: 10.1158/0008-5472.CAN-06-3297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tischkowitz M, Hamel N, Carvalho MA, Birrane G, Soni A, et al. Pathogenicity of the BRCA1 missense variant M1775K is determined by the disruption of the BRCT phosphopeptide-binding pocket: a multi-modal approach. Eur J Hum Genet. 2008;16:820–832. doi: 10.1038/ejhg.2008.13. doi: 10.1038/ejhg.2008.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nackley AG, Shabalina SA, Tchivileva IE, Satterfield K, Korchynskyi O, et al. Human Catechol-O-Methyltransferase Haplotypes Modulate Protein Expression by Altering mRNA Secondary Structure. Science. 2006;314:1930–1933. doi: 10.1126/science.1131262. doi: 10.1126/science.1131262. [DOI] [PubMed] [Google Scholar]
- 46.Duan J. Synonymous mutations in the human dopamine receptor D2 (DRD2) affect mRNA stability and synthesis of the receptor. Hum Mol Genet. 2003;12:205–216. doi: 10.1093/hmg/ddg055. doi: 10.1093/hmg/ddg055. [DOI] [PubMed] [Google Scholar]
- 47.Liede A, Malik IA, Aziz Z, Rios Pd P de L, Kwan E, et al. Contribution of BRCA1 and BRCA2 mutations to breast and ovarian cancer in Pakistan. Am J Hum Genet. 2002;71:595–606. doi: 10.1086/342506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Evans DGR, Neuhausen SL, Bulman M, Young K, Gokhale D, et al. Haplotype and cancer risk analysis of two common mutations, BRCA1 4184del4 and BRCA2 2157delG, in high risk northwest England breast/ovarian families. Journal of Medical Genetics. 2004;41:e21. doi: 10.1136/jmg.2003.012104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saxena S, Chakraborty A, Kaushal M, Kotwal S, Bhatanager D, et al. Contribution of germline BRCA1 and BRCA2 sequence alterations to breast cancer in Northern India. BMC Med Genet. 2006;7:75. doi: 10.1186/1471-2350-7-75. doi: 10.1186/1471-2350-7-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Salazar R, Cruz-Hernandez JJ, Sanchez-Valdivieso E, Rodriguez CA, Gomez-Bernal A, et al. BRCA1-2 mutations in breast cancer: identification of nine new variants of BRCA1-2 genes in a population from central Western Spain. Cancer Letters. 2006;233:172–177. doi: 10.1016/j.canlet.2005.03.006. doi: 10.1016/j.canlet.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 51.Simard J, Dumont M, Moisan A-M, Gaborieau V, Malouin H, et al. Evaluation of BRCA1 and BRCA2 mutation prevalence, risk prediction models and a multistep testing approach in French-Canadian families with high risk of breast and ovarian cancer. Journal of Medical Genetics. 2007;44:107–121. doi: 10.1136/jmg.2006.044388. doi: 10.1136/jmg.2006.044388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Borg A, Haile RW, Malone KE, Capanu M, Diep A, et al. Characterization of BRCA1 and BRCA2 deleterious mutations and variants of unknown clinical significance in unilateral and bilateral breast cancer: the WECARE study. Hum Mutat. 2010;31:E1200–40. doi: 10.1002/humu.21202. doi: 10.1002/humu.21202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Díez Gilbert O, Machuca Cordano I, Angel Navarro M. [Characterization of the BRCA1 gene and its significance in hereditary breast cancer]. Med Clin (Barc) 1996;107:623–627. [PubMed] [Google Scholar]