Abstract
Background
The rising costs, limited supply, and clinical risks associated with allogeneic blood transfusion have prompted investigation into autologous blood management strategies, such as post-operative red cell salvage. This study provides a cost comparison of transfusing washed post-operatively salvaged red cells using the OrthoPat device versus unwashed shed blood and banked allogeneic blood.
Study Design and Methods
Cell salvage data was retrospectively reviewed for a sample of 392 patients who underwent primary hip or knee arthroplasty. Average unit costs were calculated for washed salvaged red cells, equivalent units of unwashed shed blood, and therapeutically equivalent volumes of allogeneic packed red cells.
Results
No initial capital investment was required for the establishment of the post-operative cell salvage program. For patients undergoing total knee arthroplasty (TKA), the average unit cost for washed post-operatively salvaged cells, unwashed shed blood, and allogeneic banked blood was $758.80, $474.95, and $765.49, respectively. In patients undergoing total hip arthroplasty (THA), the average unit cost for washed post-operatively salvaged cells, unwashed shed blood, and allogeneic banked blood was $1827.41, $1167.41, and $2609.44, respectively.
Conclusion
This analysis suggests that transfusing washed post-operatively salvaged cells using the OrthoPat device is more costly than using unwashed shed blood in both THA and TKA. When compared to allogeneic transfusion, washed post-operatively salvaged cells carry a comparable cost in TKA, but potentially represent a significant savings in patients undergoing THA. Sensitivity analysis suggests that in the case of TKA, however, cost comparability exists within a narrow range of units collected and infused.
Keywords: blood salvage, autologous transfusion, allogeneic transfusion, cost study analysis
INTRODUCTION
Blood transfusion is an essential component of the peri-operative management of patients undergoing elective hip and knee arthroplasty procedures, which are frequently associated with significant blood loss. While estimates vary, review of the existing literature reveals transfusion rates ranging from 22–97%,1–4 suggesting that blood management strategies have a significant economic impact in these procedures as well, especially when one considers recent cost estimates of $522–$1183 per unit of allogeneic packed red blood cells.5 The healthcare industry's increasing focus on cost containment coupled with provider and patient concerns about the limited supply of, and potential complications associated with, allogeneic blood transfusion have prompted investigation into alternative methods of peri-operative blood conservation.
Autologous transfusion in the post-operative period, specifically the techniques of post-operative salvage, has sparked growing interest. One method of post-operative salvage is the collection and reinfusion of unwashed shed blood from wound drainage. While early studies warned of significant complications associated with this technique,6 more recent studies suggest that the reinfusion of unwashed shed blood may represent a safe strategy to reduce exposure to allogeneic transfusion.7–12 Alternatively, blood may be collected, washed, filtered, and reinfused using a specialized device such as the OrthoPat, an automated bread-box sized device that can be mounted on an intravenous pole near the patient.
Previous studies have highlighted the potential clinical advantages of cell salvage in decreasing the need for and risks associated with allogeneic transfusion.12 However, there is some debate as to the overall cost-effectiveness of utilizing cell salvage when compared to allogeneic transfusion, specifically with elective total hip and knee arthroplasty procedures.11,13
Given the use of processed post-operative cell salvage in elective orthopedic hip and knee arthroplasty in our health system, we initiated a retrospective study to evaluate the cost-effectiveness of this technique when compared with the costs of transfusing unwashed post-operatively salvaged shed blood as well as standard allogeneic blood transfusion. We hypothesized that our currently employed blood conservation technique would be less cost-effective than both the transfusion of unwashed cells and banked allogeneic blood.
MATERIALS AND METHODS
A post-operative cell salvage program was established at the University of Pittsburgh Medical Center St. Margaret's Hospital (UPMC-SMH) in conjunction with BioTronics, Inc., a subsidiary company of the health system. BioTronics, Inc. created and maintains a database to collect the necessary information to perform ongoing cost analyses. The use of de-identified information from the database for the purpose of research was approved by the University of Pittsburgh Medical Center's Institutional Review Board.
Retrospective cell salvage information from a twelve-month period from January through December 2009 was obtained from the database. Three hundred ninety-two primary hip and knee arthroplasty procedures were performed during this time. Hip and knee arthroplasties were further differentiated given the varying degree of post-operative blood loss between the procedures.14,15
Red cell mass was calculated by multiplying the volume of blood collected by the hematocrit of that particular unit. Given that previous studies have defined one unit of allogeneic packed cells as having a red cell mass of 200 mL, the number of allogeneic equivalent units was calculated using this definition.16,17 Supplemental allogeneic transfusion was not considered in this study. Process maps were formulated to capture the associated costs of obtaining and transfusing one unit of allogeneic blood and one unit of post-operatively salvaged blood. A cost comparison study, with corresponding sensitivity analysis, was then performed to determine the most economical peri-operative blood management strategy.
Initial Capital Investment
This aspect of cost includes expenditures related to the establishment of a post-operative cell salvage program exclusive of daily operating costs. The costs assessed included the purchase of the required equipment, supplies, and training of personnel necessary for daily operations. Administrative costs were difficult to obtain and therefore excluded from our analysis.
The equipment utilized was the OrthoPat Cell Salvage system developed by Haemonetics, Inc. At the time of the establishment of this autotransfusion program, the OrthoPat device was selected given that it was fully automated and therefore more suitable for use on a nursing floor. UPMC-SMH did not purchase the OrthoPat devices; rather, these devices were provided on an as-needed basis from BioTronics, Inc. The costs associated with the purchase of the OrthoPat devices and the training of the technicians were incorporated into the cost of the disposable equipment required for its use, which was purchased from BioTronics, Inc. As a result, this cost assessment did not require consideration of an initial capital outlay.
Operating Costs
Operating costs are those expenditures related to the daily functioning of the program and consist of both direct and indirect costs. Direct costs, namely those that are specifically linked to the cell salvage program, include labor and supplies. Indirect costs, which are not directly associated with the production process, include the costs for utilities and those associated with requisite administrative tasks, such as staff meetings.
Direct Costs
Direct costs were assessed in terms of fixed and variable costs. Fixed costs, specifically those expenses that remain constant regardless of the volume produced, included equipment costs and certain labor expenses. Given the institutional procurement arrangement with BioTronics Inc., as well as the essential lack of salaried employee expenses, it was unnecessary to consider those elements of fixed cost in our analysis. However, we did account for the cost of the disposable equipment and technician time required to utilize the OrthoPat device, phlebotomy and blood bank costs associated with performing a type and cross, as well as the costs of intravenous infusion tubing and saline. These items were considered to be components of fixed cost as they were required for each patient, regardless of the number of units produced. Of note, the cost of the disposable equipment in our institution's procurement arrangement included a bundled lease fee for the OrthoPat equipment.
In contrast to fixed costs, variable costs are those expenditures that are incurred per unit of cells produced and transfused. These metrics were associated with the quantity of post-operatively salvaged blood processed and reinfused. In our assessment, this included costs associated with nursing time and the number of times the processed blood collection bags had to be exchanged.
Indirect Costs
Indirect costs, which include electricity necessary for operation of the device, physical space for equipment storage, disposal costs, and administrative costs were difficult to quantify at our institution. Additionally, many aspects of indirect costs, namely those associated with personnel and facilities, are applicable to all three transfusion modalities and thus unlikely to contribute significantly to cost variability. As a result, our analysis did not specifically address indirect costs.
Average Unit Costs
Based upon our consideration of operating expenses, we first calculated the average cost of one unit of packed red blood cells derived from washed, post-operatively salvaged blood. This was achieved by calculating the overall cost for transfusing washed, post-operatively salvaged cells for the patients in the study sample and dividing this by the total number of units transfused. Using this method, the average unit cost would necessarily incorporate the costs incurred in instances where the OrthoPat was utilized without the transfusion of post-operatively salvaged blood. However, we felt that this was an important consideration in understanding overall costs associated with this program.
This calculated cost was then compared to the calculated average costs of transfusing one unit of unwashed shed blood as well as one unit of banked allogeneic packed red blood cells (PRBC) obtained from the Central Blood Bank. In comparing the economics of transfusing washed versus unwashed post-operatively salvaged cells, we assumed that the same number of PRBC equivalent units would be collected by both salvage methods.
Calculation of the total cost of transfusing unwashed post-operatively salvaged cells for the patients in the study sample required consideration of fixed and variable costs. Fixed costs included phlebotomy, type and cross match, the equipment required to collect wound drainage and transfuse salvaged cells, and the labor cost associated with connecting and monitoring the equipment. Variable costs included the labor costs associated with hanging and priming each unit of unwashed, salvaged cells, as well as the cost associated with changing the collection bag. The overall cost of transfusing unwashed post-operatively salvaged cells for the patients in the study sample was calculated and was divided by the total number of units transfused to determine the average unit cost.
In making a comparison to allogeneic transfusion, the PRBC equivalent units obtained for each patient via processed salvage were rounded down to the nearest unit and summed to obtain a total for the study population. Our rationale was based on the premise that a PRBC volume of less than 1 unit would amount to a subtherapeutic intervention.18 Furthermore, the transfusion of partial allogeneic units is not part of our practice. Fixed costs included those associated with phlebotomy, performance of a type and cross, and equipment required for transfusion. Variable costs included per unit procurement costs, blood bank labor costs associated with processing each allogeneic unit, as well as nursing labor costs associated with transfusion and monitoring of the patient. The average cost of each allogeneic unit was determined using the same methodology described for washed and unwashed salvaged units.
RESULTS
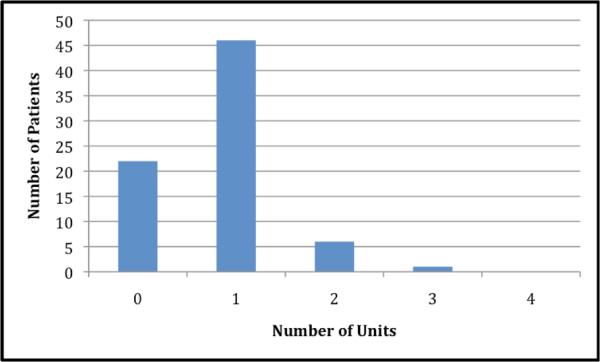
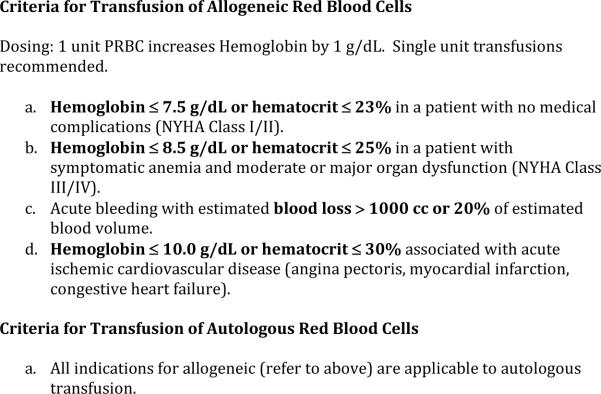
The OrthoPat device and full disposable setup were connected to all of the patients in this study. Of the 392 patients who underwent elective primary hip or knee arthroplasty during this time, 323 (82.4%) received post-operative transfusion of some quantity of salvaged blood. In examining the subset of 317 patients who underwent primary total knee arthroplasty (TKA), 270 (85.2%) received post-operatively salvaged blood (Figure 1). By comparison, 53 of the 75 (70.7%) patients who underwent primary total hip arthroplasty (THA) received salvaged blood (Figure 2).
Figure 1.
Frequency histogram showing the number of units of red cells produced by washed post-operative cell salvage per surgical procedure based on data from 317 total knee arthroplasty patients. One unit of packed red blood cells contains 200 mL of red cell mass. Cases with red cell mass <200 mL was considered to be 0 Units, 200–400 mL was 1 Unit, 400–600 mL was 2 Units, 600–800 mL was 3 units, and 800–1000 mL was 4 units.
Figure 2.
Frequency histogram showing the number of units of red cells produced by washed post-operative cell salvage per case of total hip arthroplasty on data from 75 patients. One unit of packed red blood cells contains 200 mL of red cell mass. Cases with red cell mass <200 mL was considered to be 0 Units, 200–400 mL was 1 Unit, 400–600 mL was 2 Units, 600–800 mL was 3 units, and 800–1000 mL was 4 units.
Given that one unit of PRBCs is equivalent to 200 mL of red cell mass, a total of 330.4 PRBC equivalent units were salvaged for the entire study sample, with 251 patients receiving the equivalent of 1 unit or less. In considering the sample overall, an average of 0.84 PRBCS equivalent units was salvaged per case. In the cases of TKA, an average of 0.95 PRBC equivalent units was salvaged per case compared to the average 0.39 PRBC equivalent units salvaged per case of THA (Table 1).
Table 1.
| Supply Cost | ||
| OrthoPat Full Setup | $375 | |
| OrthoPat Collection Line | $11.10 | |
| Unwashed Shed Blood Setup | $105 | |
| Saline (1 liter) | $0.99 | |
| Intravenous tubing | $4.49 | |
| Blood (per unit) | $156 | |
| Alcohol Swab | $0.03 | |
| Tourniquet | $0.33 | |
| Butterfly angiocath | $0.36 | |
| Gauze | $0.02 | |
| Vacutainer Collection Tube | $0.09 | |
| Tape | $0.02 | |
|
| ||
| Labor Cost | ||
| OrthoPat technician (per hour) | $19.50 | |
| Phlebotomist (per blood draw) | $20 | |
| Staff Nurse (per hour) | $42 | |
| Orthopedic surgeon (per hour) | $212.71 | |
| Laboratory Technician (per hour) | $18.54 | |
| Blood Bank Technician (per hour) | $19 | |
| Blood Bank Aide (per hour) | $9.50 | |
|
| ||
| Laboratory Cost | ||
| Complete Blood Count (CBC) | $15 | |
| Type and Crossmatch | $205 | |
Capital Outlay
No initial capital outlay was required to establish a post-operative cell salvage program at UPMC-SMH, as described in Methods. The equipment was purchased and maintained by our subsidiary, BioTronics, Inc., and was provided on an as-needed basis to the health system. The costs of the equipment, technician training, and transportation were incorporated into the cost of the disposable equipment, which was purchased from BioTronics, Inc.
Operating Costs
All operating costs are summarized in Table 1.
Fixed Costs
Each patient in the study sample required a type and crossmatch, which was performed by a phlebotomist at a cost of $20 per blood draw using the necessary phlebotomy supplies at a cost of $0.93. Each type and cross carried a cost of $205 and required 50 minutes of processing and analysis by technicians in our institution's blood bank. Sixty percent of the processing was performed by a skilled blood bank technician with an average hourly wage of $19 per hour including benefits. The remaining 40 percent of the processing was performed by a blood bank aide with an average hourly wage of $9.50. The cost of the disposable equipment required for post-operative cell salvage was $386.10 and consisted of a disposable setup and a connection line placed intraoperatively. Each use of the OrthoPat, regardless of the amount of blood collected, required one hour of setup time by a trained technician with an hourly wage of $19.50 including benefits. Each patient received intravenous tubing and a saline carrier, which carried costs of $4.49 and $0.99, respectively. Thus, the fixed cost per patient was $649.68.
Variable Costs
When an adequate volume of the patient's blood is collected, a staff nurse exchanges the filled collection bag and replaces it with an empty collection bag. Patient identifiers are inspected, blood administration tubing is primed, collected cells are transfused, and the patient's vitals are monitored closely, a process which requires approximately 1 hour. While this segment of the process may be performed multiple times during a patient's post-operative hospital stay, there are numerous variables involved in determining the frequency with which this occurs. Thus, for the purposes of this study, we estimated two changes per patient based upon the consideration that the median volume contained in each collection bag is approximately 275 cc. The hourly compensation for the nursing staff at this institution was $42 per hour. As previously mentioned, 323 of the 392 patients received some volume of salvaged blood, even if the reinfusion volume amounted to less than 1 PRBC equivalent unit. Therefore, the nursing cost was applied to the 251 patients who received 1 unit or less of salvaged packed red cells.
Average Unit Costs
In calculating average unit costs, we calculated the overall cost associated with transfusing processed salvaged blood using the OrthoPat in our study sample and divided that cost by the total number of units of PRBCs transfused. The average cost of transfusing 1 unit of processed salvaged red cells in the study sample overall was $852.92. In considering the procedures independently, the average unit cost in primary TKA was $758.80 compared with $1827.41 in primary THA (Table 2). The significant cost difference between the two procedures is largely attributable to the burden of fixed cost. Given that fewer units were salvaged in the THA group, the overall fixed cost for the patient sample was distributed over fewer units when compared to the TKA group in which there was a larger volume of cells salvaged.
Table 2.
| TKA | THA | ||
|---|---|---|---|
|
| |||
| Salvaged Autologous Transfusion | |||
| OrthoPat | # of Units Salvaged (Total) | 301.3 | 29.1 |
| Average # of Units Salvaged per case | 0.95 | 0.39 | |
| Median # of Units Salvaged per Case | 0.84 | 0.375 | |
| Average Unit Cost | $758.80 | $1827.41 | |
| Fixed Cost per Unit | $683.53 (90.1%) | $1674.42 (91.6%) | |
| Variable Cost per Unit | $75.27 (9.9%) | $152.99 (8.4%) | |
| Unwashed Shed Blood | # of Units Salvaged (Total) | 301.3 | 29.1 |
| Average # of Units Salvaged per case | 0.95 | 0.39 | |
| Median # of Units Salvaged per case | 0.84 | 0.375 | |
| Average Unit Cost | $474.95 | $1167.41 | |
| Fixed Cost per Unit | $389.36 (82%) | $953.80 (81.7%) | |
| Variable Cost per Unit | $85.59 (18%) | $213.61 (18.3%) | |
| Allogcncic Transfusion | |||
| # of Therapeutic Equivalents (Total) | 195 | 10 | |
| Average # of Units per case | 0.62 | 0.13 | |
| Median # of Units per case | 0 | 0 | |
| Average Unit Cost | $765.49 | $2609.44 | |
| Fixed Cost per Unit | $510.29 (66.7%) | $2354.24 (90.2%) | |
| Variable Cost per Unit | $255.20 (33.3%) | $255.20 (9.8%) | |
Next, we calculated the cost associated with transfusing unwashed cells from wound drainage. Similar to the patients receiving washed salvaged blood, patients receiving unwashed salvaged blood also require phlebotomy for a type and crossmatch. The cost of the disposable equipment required to collect wound drainage was approximately $105. Connection of the equipment and monitoring require approximately 0.5 hours of time by a skilled staff nurse. Intravenous tubing and a saline carrier are also used in these patients. The process of priming the tubing, transfusing the shed blood, and monitoring the patient requires 1 hour of time by a skilled staff nurse. This process of reinfusing unwashed cells from wound drainage occurs over a 6-hour period, after which it expires as per transfusion standards at our institution. We again estimated an average of 2 collection bag changes per patient. The average cost of transfusing 1 unit of unwashed salvaged cells in the study sample was $535.94. In differentiating between the procedures, the average unit cost was $474.95 in TKA procedures and $1167.41 in THA procedures.
Using the methodology described above, the number of therapeutic equivalent units of allogeneic blood was calculated. Given that our institution does not transfuse partial allogeneic units, the number of units salvaged for each patient was rounded down to the nearest whole unit to obtain the number of allogeneic therapeutic equivalent units. In our study sample, a total of 205 therapeutic equivalent units of allogeneic cells were transfused. As in the case of both salvage modalities, patients receiving allogeneic transfusions must undergo phlebotomy to obtain a blood sample as well as a type and crossmatch. These costs are quantified earlier in this section. Post-operatively, each patient undergoes a complete blood count (CBC) in order to assess hematocrit and determine the need for allogeneic transfusion. This process again requires the skills of a phlebotomist and the requisite disposable equipment. The process of receiving, processing, and reporting the results of the CBC requires 1 hour of the skills of a laboratory technician with hourly compensation of $18.54. The results are then reviewed by the patient's physician, and a computerized order may be placed for blood transfusion. This process requires approximately 5 minutes, and the average hourly wage of an orthopedic surgeon is approximately $212.71. The time required for the institution's blood bank to receive the order, prepare the blood, package the unit, and transport it to the appropriate floor is approximately 1 hour. The labor costs associated with blood bank personnel are quantified earlier in this section. With regard to procurement of allogeneic packed red blood cells, our institution obtains each unit of allogeneic packed red blood cells from the Central Blood Bank at a cost of $156. Intravenous tubing and a saline carrier are required to transfuse blood products. The process of obtaining an allogeneic unit, verifying patient identifiers and blood compatibility, priming the blood administration set, transfusing, and monitoring the patient for adverse reactions requires approximately 2 hours and the skills of a staff nurse, which appears to be in agreement with nursing times in previously published cost analyses for allogeneic transfusion.19
The average cost of transfusing each unit of allogeneic cells in the overall study sample is $855.43. The calculated average cost of transfusing each unit of allogeneic packed red cells is approximately $765.49 in cases of TKA and $2609.44 in cases of THA.
A sensitivity analysis was then performed by varying the number of units salvaged by the OrthoPat system, which translated into varying the number of therapeutic equivalent units of allogeneic PRBCs (Table 3). In TKA patients, as the number of units salvaged decreased, the average unit cost approached and then exceeded that of allogeneic blood when salvaged volume was decreased by approximately 2.7 percent. Conversely, as the volume collected using OrthoPat is increased, the average unit cost of post-operatively salvaged cells decreased disproportionately faster than the decrease in the average unit cost of allogeneic cells. In THA, when the number of units salvaged by Orthopat is increased or decreased by 5%, the average unit cost of allogeneic blood exceeded that of washed post-operatively salvaged blood. In both TKA and THA patients, the reinfusion of unwashed cell salvage remained the least costly option.
Table 3.
| Number of Units Salvaged | Total Knee Arthroplasty | Total Hip Arthroplasty | ||||
|---|---|---|---|---|---|---|
| Allogenei c | OrthoPat | Unwashed Shed Blood | Allogeneic | OrthoPat | Unwashed Shed Blood | |
| Decrease by 5% | $792.34 | $798.74 | $499.95 | $2733.34 | $1923.59 | $1228.86 |
| Decrease by 4% | $786.75 | $790.42 | $494.74 | $2707.53 | $1903.56 | $1215.06 |
| Decrease by 3% | $781.27 | $782.27 | $489.64 | $2682.25 | $1883.93 | $1203.52 |
| Decrease by 2% | $775.90 | $774.29 | $484.64 | $2657.48 | $1864.71 | $1191.24 |
| Decrease by 1% | $770.64 | $766.47 | $479.75 | $2633.22 | $1845.87 | $1179.21 |
| Current number of units salvaged by OrthoPat | $765.49 | $758.80 | $474.95 | $2609.44 | $1827.41 | $1167.41 |
| Increase by 1% | $760.43 | $751.29 | $470.25 | $2586.13 | $1809.32 | $1155.86 |
| Increase by 2% | $755.48 | $743.93 | $465.64 | $2563.28 | $1791.58 | $1144.52 |
| Increase by 3% | $750.62 | $736.70 | $461.12 | $2540.87 | $1774.19 | $1133.41 |
| Increase by 4% | $745.86 | $729.62 | $456.68 | $2518.89 | $1757.13 | $1122.51 |
| Increase by 5% | $741.19 | $722.67 | $452.33 | $2497.33 | $1740.39 | $1111.82 |
DISCUSSION
Although previous studies have suggested that cell salvage may represent a cost-effective alternative to allogeneic blood transfusion, we had anticipated that the current utilization of the OrthoPat represented the most costly post-operative blood management strategy. However, our cost comparison suggests that while it is more costly than transfusing unwashed shed blood, it is substantially less costly than allogeneic transfusion in the subset of patients undergoing THA. In the subset of patients undergoing TKA, OrthoPat usage carries a cost that is comparable to the cost of allogeneic blood transfusion within a narrow range of units salvaged and reinfused.
OrthoPat utilization creates a cost savings of approximately $6.69 per unit when compared with allogeneic transfusion in TKA at current salvage and reinfusion rates. With regard to THA, the cost savings are much more substantial at $782.03 per unit. Autologous transfusion of unwashed shed blood from wound drainage represented the most cost-effective method of peri-operative blood management. When compared to allogeneic transfusion, the reinfusion of unwashed shed blood represented a cost savings of $290.54 per unit in TKA and $1442.03 per unit in THA. When compared to using the OrthoPat system, transfusion of unwashed shed blood created a cost savings of $283.85 per unit in TKA and $660 per unit in THA. The latter savings figures essentially amount to the cost associated with washing salvaged cells (Table 2).
At first glance, these savings figures suggest that the institution should adjust its blood management strategy from utilizing the OrthoPat to a device that collects, filters, and reinfuses unwashed shed blood. However, cost containment must be considered within the context of patient care and outcomes as well as the frequency and potential costs of complications associated with both allogeneic and salvaged products (Tables 4–6).
Table 4.
| Complication | Incidence | Estimated Cost |
|---|---|---|
| Post-operative bacterial infection | 4.6% – 15.3% 23 | Up to $12,980+ depending upon severity 33 |
| Transfusion associated circulatory overload (TACO) | 1–8% 1 | Variable depending upon severity |
| Deep vein thrombosis (DVT) | 2% 1 | $17,114 34 – $17,512 35 |
| Allergic Transfusion Reaction | 1–3% 36 | Variable depending upon severity |
| Increased Length of Hospital Stay 1 | 1.3% per unit of RBCs transfused 23 | $1,000 – $1,500 per unit transfused 37 |
| Transfusion-related Acute Lung Injury (TRALI) | 0.02% 24–1.3% 25 | Variable depending upon severity |
| Febrile Non-Hemolytic Transfusion Reactions | 0.02% 26 | $8602 but variable depending upon severity26 |
| Mistransfusion/Acute Hemolytic Transfusion Reaction | 0.007% 38 | $5125 39 but variable depending upon severity |
| HIV/Hepatitis Transmission | 0.0001% 40 | $117,000 – $119,000 lifetime cost 41 |
Table 6.
| Complication | Incidence | Estimated Cost |
|---|---|---|
| Febrile reactions | Rare, but incidence not consistently reported in the literature9 | Up to $5,125+ 39,44 |
| Infection | 2%49 | $2,836 46 – $35,000 depending upon severity and sequelae 39,44,47 |
| Contamination by fat droplets/bacteria | Significant reduction in contamination as compared to unwashed cell salvage50,51 | Variable depending upon degree of severity and sequelae |
| Air embolism | 0.003%38 | Variable, depending upon degree of severity and sequelae |
| Coagulopathy/'salvaged cell syndrome' | Described in case reports 52,53 | Variable depending upon severity, treatment, and sequelae |
Allogeneic transfusion carries the advantage of delivering a consistent hematocrit. However, variability in supply, concerns with regard to disease transmission, and well-described complications - including incompatibility reactions, increased risk of post-operative infections, and concerns for acute lung injury and volume overload - have tempered clinician and patient enthusiasm for allogeneic transfusion (Table 4).1,10,20–26 Many of these considerations have made autologous transfusion a more attractive alternative.
Reinfusion of unwashed cells is the least expensive of the modalities discussed and is widely utilized; over 2,500 salvaged but unprocessed procedures are performed annually in our health system alone. This modality decreases allogeneic exposure12 and mitigates concerns regarding overcollection, storage, and incompatibility reactions.10 However, disadvantages include concerns of dilution of the salvaged product,27 restrictions on quantity and duration of transfusion, febrile reactions,28,29 and contamination by microbes or fat droplets.10 As with allogeneic transfusions, complications associated with the use of unwashed drainage have the potential to wield significant complications (Table 5).
Table 5.
| Complication | Incidence | Estimated Cost |
|---|---|---|
| Febrile reactions | 2–22% depending upon timing of collection in relation to surgery 28,42,43 | Up to $5,125+ 44,39 |
| Infection | 2–4% 45 | $2,836 46 – $35,000 depending upon severity and sequelae 39, 44,47 |
| Contamination by fat droplets | May be as high as 100% 8,27 | Variable depending upon degree of severity and sequelae |
| Immunomodulation | May be as high as 100% 48 | Variable depending upon degree of severity and sequelae |
| Air embolism | Fatal: 0.003% 38
Subclinical: variable |
Variable, depending upon degree of severity and sequelae |
| Hypotension | 12.5% 28 | Up to $12,302 47 depending upon severity and etiology |
| Coagulopathy | 0–3.84% 27
Dependent upon volume transfused – no consistently reported coagulopathy with infusion of 10–15% of blood volume 42 |
Variable depending upon severity, treatment, and sequelae |
Reinfusion of washed post-operatively salvaged blood using the OrthoPat device has many of the same advantages as unwashed shed blood, including a similar decrease in the rate of allogeneic transfusion, specifically in orthopedic procedures.12 Additionally, the washing process appears to decrease many contaminants found in unwashed salvaged cells and provides a more consistent hematocrit. Previous studies have also demonstrated higher erythrocyte viability in washed cell salvage as compared to allogeneic blood.30,31 Concerns associated with the use of this modality include logistics associated with implementation, training of personnel, and cost,17 as well as rare complications such as air embolism, hemolysis, bacterial contamination, and coagulopathy (Table 6). 9,31
Interpreting the results of our cost comparison study requires several other considerations. First, we focused our analysis on identifiable direct costs associated with each modality. There are a multitude of indirect costs associated with allogeneic transfusion, as outlined by the Cost-of-Blood Consensus Working Group (COBCON),32 that were difficult to assign and quantify at our institution. Many of these indirect costs relate to autologous transfusion techniques as well. These costs include administrative (administrative meetings, nursing meetings, equipment inservice costs), electricity, and equipment storage costs.
Second, with regard to THA, the majority of blood loss generally occurs in the intra-operative period, in direct contrast to TKA.14,15 It is possible that patients undergoing THA receive allogeneic transfusion intra- operatively, mitigating the need for post-operative transfusion. Further, the majority of THA patients in our study sample who received post-operatively salvaged blood received 1 unit or less, thus calling into question the medical necessity of the transfusion. Therefore, there may actually be an overall cost benefit to discontinuing the use of OrthoPat in patients undergoing total hip arthroplasty.
Further, with regard to the medical necessity of post-operative transfusion, specifically in cases where patients received 1 unit or less of post-operatively salvaged cells, transfusion triggers must be considered. UPMC-SMH has adopted a system-wide transfusion protocol based upon hemoglobin thresholds and patient co-morbidities. Frequently, however, transfusion is dependent upon clinician preferences and the rigidity with which thresholds were followed is not always clear. Patients may have received both allogeneic and autologous transfusions based upon clinician judgment and not based upon the transfusion protocol.
Additionally, our study considered each of these blood management strategies in relative isolation in the post-operative period. Our analysis did not specifically incorporate the financial impact of supplementation of OrthoPat usage with breakthrough allogeneic transfusion. Given the structure of our comparison, supplemental transfusion would have resulted in largely constant costs for each of the three blood management strategies evaluated. While not specifically captured in our de-identified dataset, internal review of blood utilization in orthopedic procedures at our institution reveals that annually, approximately 36.7% of patients undergoing THA receive allogeneic transfusion with an average of 1.4 units transfused per case. In TKA procedures, 19.2% of patients receive allogeneic transfusion, with an average of 1.6 units transfused per case.
Previous studies have considered the possible costs associated with the potential complications of both allogeneic and autologous transfusion.33. However, these costs were not included in our analysis due to discrepancies in the nature and actual incidence of those complications. Additionally, the suggested incidence of the described complications was sufficiently low as to render it negligible in the sample size under consideration.
Incorporation of certain practice modifications will also likely affect relative costs between the modalities. First, more focused use in patients expected to sustain significant post-operative blood loss, specifically in TKA, may improve the cost effectiveness of OrthoPat utilization. Second, post-operative vigilance by the nursing staff in collecting drainage output could potentially improve red cell recovery. As our sensitivity analysis suggests, by increasing the number of red cell units recovered, the average unit costs of salvaged blood would decrease further (Table 3). Integration of an available equipment modification - specifically the use of a standby system that could be converted to a full setup once a minimum volume of 400 cc is collected - may also help to reduce costs. This standby system, priced at approximately $100 for our institution, was not part of our practice at the time of our study. While yielding savings in terms of equipment cost, the modification would likely require additional labor costs for monitoring and conversion. Finally, utilization of other autologous modalities and blood conservation strategies, such as the incorporation of antifibrinolytic medications, may also aid in cost containment. More detailed cost-benefit and risk analyses will be required prior to incorporating these modifications into our practice.
While this cost study has clear implications for peri-operative blood management at UPMC-SMH, it may have variable applicability to other institutions, primarily due to differences in pricing and procurement arrangements and options to outsource this service. As previously stated, market procurement costs for the OrthoPat devices themselves amount to approximately $18,500 per device, a cost that our institution sustains as part of the bundled cost of the disposable equipment. While our pricing arrangement with BioTronics, Inc. allows for procurement of disposable equipment at a price of $386.10, the price charged by Haemonetics is highly variable across the country and dependent upon the specifics of the institution's procurement arrangement. Another source of cost variability between institutions involves the brand of equipment as well. Our institution chose the OrthoPat device based upon its operational suitability in the setting of the nursing floor. Alternative devices may be more suitable for other institutions. Furthermore, cost-effectiveness will also be affected by an institution's overall case volume and provider competence with regard to the efficiency of red cell recovery.
In conclusion, the current post-operative cell salvage practice at UPMC-SMH may represent a less costly alternative to allogeneic transfusion in TKA procedures within certain volume parameters. With regard to THA, further investigation is required to determine the medical necessity for a post-operative cell salvage device in a procedure where the majority of blood loss occurs intra-operatively. Despite the apparent cost advantages to using unwashed salvaged blood, clinician preference at our institution remains strongly in favor of the washed salvage option. Prospective cost and outcomes analyses will be required to determine the optimal post-operative blood management modality from both a clinical and economic standpoint.
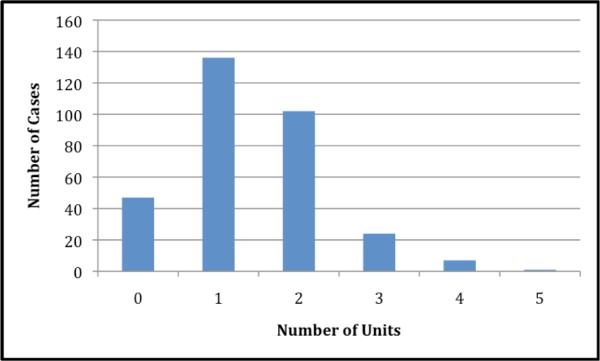
Figure 3.
Criteria for transfusing allogeneic and autologous red blood cells at UPMC-SMH.
ACKNOWLEDGEMENTS
This publication was made possible by Grant Number UL1 RR024153 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Source of Funding No external funding source was utilized in this study.
Footnotes
Conflicts of Interest:
- Robert Dyga is an employee of BioTronics, Inc.
- The remaining authors declare that they do not have conflicts of interest relevant to the manuscript submitted to TRANSFUSION.
REFERENCES
- 1.Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81:2–10. doi: 10.2106/00004623-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Rosencher N, Kerkkamp HE, Macheras G, Munuera LM, Menichella G, Barton DM, Cremers S, Abraham IL. Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion. 2003;43:459–69. doi: 10.1046/j.1537-2995.2003.00348.x. [DOI] [PubMed] [Google Scholar]
- 3.Sturdee SW, Beard DJ, Nandhara G, Sonanis SV. Decreasing the blood transfusion rate in elective hip replacement surgery using an autologous drainage system. Ann R Coll Surg Engl. 2007;89:136–9. doi: 10.1308/003588407X155518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sinclair KC, Clarke HD, Noble BN. Blood management in total knee arthroplasty: a comparison of techniques. Orthopedics. 2009;32:19. doi: 10.3928/01477447-20090101-21. [DOI] [PubMed] [Google Scholar]
- 5.Shander A, Hofmann A, Ozawa S, Theusinger OM, Gombotz H, Spahn DR. Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion. 2010;50:753–65. doi: 10.1111/j.1537-2995.2009.02518.x. [DOI] [PubMed] [Google Scholar]
- 6.Rakower SR, Worth MH, Jr., Lackner H. Massive intraoperative autotransfusion of blood. Surg Gynecol Obstet. 1973;137:633–6. [PubMed] [Google Scholar]
- 7.Munoz M, Slappendel R, Thomas D. Laboratory characteristics and clinical utility of post-operative cell salvage: washed or unwashed blood transfusion? Blood Transfus. 2011;9:248–61. doi: 10.2450/2010.0063-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Healy WL, Pfeifer BA, Kurtz SR, Johnson C, Johnson W, Johnston R, Sanders D, Karpman R, Hallack GN, Valeri CR. Evaluation of autologous shed blood for autotransfusion after orthopaedic surgery. Clin Orthop Relat Res. 1994:53–9. [PubMed] [Google Scholar]
- 9.Huet C, Salmi LR, Fergusson D, Koopman-van Gemert AW, Rubens F, Laupacis A. A meta-analysis of the effectiveness of cell salvage to minimize perioperative allogeneic blood transfusion in cardiac and orthopedic surgery. International Study of Perioperative Transfusion (ISPOT) Investigators. Anesth Analg. 1999;89:861–9. doi: 10.1097/00000539-199910000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Munoz M, Garcia-Vallejo JJ, Ruiz MD, Romero R, Olalla E, Sebastian C. Transfusion of post-operative shed blood: laboratory characteristics and clinical utility. Eur Spine J. 2004;13(Suppl 1):S107–13. doi: 10.1007/s00586-004-0718-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas D, Wareham K, Cohen D, Hutchings H. Autologous blood transfusion in total knee replacement surgery. Br J Anaesth. 2001;86:669–73. doi: 10.1093/bja/86.5.669. [DOI] [PubMed] [Google Scholar]
- 12.Carless PA, Henry DA, Moxey AJ, O'Connell D, Brown T, Fergusson DA. Cell salvage for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev. 2010:CD001888. doi: 10.1002/14651858.CD001888.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Davies L, Brown TJ, Haynes S, Payne K, Elliott RA, McCollum C. Cost-effectiveness of cell salvage and alternative methods of minimising perioperative allogeneic blood transfusion: a systematic review and economic model. Health Technol Assess. 2006;10:iii–iv. ix–x, 1–210. doi: 10.3310/hta10440. [DOI] [PubMed] [Google Scholar]
- 14.Majkowski RS, Currie IC, Newman JH. Postoperative collection and reinfusion of autologous blood in total knee arthroplasty. Ann R Coll Surg Engl. 1991;73:381–4. [PMC free article] [PubMed] [Google Scholar]
- 15.Moonen AF, Knoors NT, van Os JJ, Verburg AD, Pilot P. Retransfusion of filtered shed blood in primary total hip and knee arthroplasty: a prospective randomized clinical trial. Transfusion. 2007;47:379–84. doi: 10.1111/j.1537-2995.2007.01127.x. [DOI] [PubMed] [Google Scholar]
- 16.Brecher ME, Monk T, Goodnough LT. A standardized method for calculating blood loss. Transfusion. 1997;37:1070–4. doi: 10.1046/j.1537-2995.1997.371098016448.x. [DOI] [PubMed] [Google Scholar]
- 17.Waters JR, Meier HH, Waters JH. An economic analysis of costs associated with development of a cell salvage program. Anesth Analg. 2007;104:869–75. doi: 10.1213/01.ane.0000258039.79028.7c. [DOI] [PubMed] [Google Scholar]
- 18.Strauss RG. The value of postoperative red cell transfusions is unclear. Transfusion. 1993;33:622–3. doi: 10.1046/j.1537-2995.1993.33793325063.x. [DOI] [PubMed] [Google Scholar]
- 19.Cantor SB, Hudson DV, Jr., Lichtiger B, Rubenstein EB. Costs of blood transfusion: a process-flow analysis. J Clin Oncol. 1998;16:2364–70. doi: 10.1200/JCO.1998.16.7.2364. [DOI] [PubMed] [Google Scholar]
- 20.Hill GE, Frawley WH, Griffith KE, Forestner JE, Minei JP. Allogeneic blood transfusion increases the risk of postoperative bacterial infection: a meta-analysis. J Trauma. 2003;54:908–14. doi: 10.1097/01.TA.0000022460.21283.53. [DOI] [PubMed] [Google Scholar]
- 21.Shander A. Financial and clinical outcomes associated with surgical bleeding complications. Surgery. 2007;142:S20–5. doi: 10.1016/j.surg.2007.06.025. [DOI] [PubMed] [Google Scholar]
- 22.Vanderlinde ES, Heal JM, Blumberg N. Autologous transfusion. Bmj. 2002;324:772–5. doi: 10.1136/bmj.324.7340.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vamvakas EC, Carven JH. Allogeneic blood transfusion, hospital charges, and length of hospitalization: a study of 487 consecutive patients undergoing colorectal cancer resection. Arch Pathol Lab Med. 1998;122:145–51. [PubMed] [Google Scholar]
- 24.Toy P, Popovsky MA, Abraham E, Ambruso DR, Holness LG, Kopko PM, McFarland JG, Nathens AB, Silliman CC, Stroncek D. Transfusion-related acute lung injury: definition and review. Crit Care Med. 2005;33:721–6. doi: 10.1097/01.ccm.0000159849.94750.51. [DOI] [PubMed] [Google Scholar]
- 25.Triulzi DJ, Vanek K, Ryan DH, Blumberg N. A clinical and immunologic study of blood transfusion and postoperative bacterial infection in spinal surgery. Transfusion. 1992;32:517–24. doi: 10.1046/j.1537-2995.1992.32692367194.x. [DOI] [PubMed] [Google Scholar]
- 26.Ezidiegwu CN, Lauenstein KJ, Rosales LG, Kelly KC, Henry JB. Febrile nonhemolytic transfusion reactions. Management by premedication and cost implications in adult patients. Arch Pathol Lab Med. 2004;128:991–5. doi: 10.5858/2004-128-991-FNTR. [DOI] [PubMed] [Google Scholar]
- 27.Blevins FT, Shaw B, Valeri CR, Kasser J, Hall J. Reinfusion of shed blood after orthopaedic procedures in children and adolescents. J Bone Joint Surg Am. 1993;75:363–71. doi: 10.2106/00004623-199303000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Clements DH, Sculco TP, Burke SW, Mayer K, Levine DB. Salvage and reinfusion of postoperative sanguineous wound drainage. A preliminary report. J Bone Joint Surg Am. 1992;74:646–51. [PubMed] [Google Scholar]
- 29.Wixson RL, Kwaan HC, Spies SM, Zimmer AM. Reinfusion of postoperative wound drainage in total joint arthroplasty. Red blood cell survival and coagulopathy risk. J Arthroplasty. 1994;9:351–8. doi: 10.1016/0883-5403(94)90044-2. [DOI] [PubMed] [Google Scholar]
- 30.Ashworth A, Klein AA. Cell salvage as part of a blood conservation strategy in anaesthesia. Br J Anaesth. 2010;105:401–16. doi: 10.1093/bja/aeq244. [DOI] [PubMed] [Google Scholar]
- 31.Bridgens JP, Evans CR, Dobson PM, Hamer AJ. Intraoperative red blood-cell salvage in revision hip surgery. A case-matched study. J Bone Joint Surg Am. 2007;89:270–5. doi: 10.2106/JBJS.F.00492. [DOI] [PubMed] [Google Scholar]
- 32.The cost of blood: multidisciplinary consensus conference for a standard methodology. Transfus Med Rev. 2005;19:66–78. doi: 10.1016/j.tmrv.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 33.Sonnenberg FA, Gregory P, Yomtovian R, Russell LB, Tierney W, Kosmin M, Carson JL. The cost-effectiveness of autologous transfusion revisited: implications of an increased risk of bacterial infection with allogeneic transfusion. Transfusion. 1999;39:808–17. doi: 10.1046/j.1537-2995.1999.39080808.x. [DOI] [PubMed] [Google Scholar]
- 34.Ollendorf DA, Vera-Llonch M, Oster G. Cost of venous thromboembolism following major orthopedic surgery in hospitalized patients. Am J Health Syst Pharm. 2002;59:1750–4. doi: 10.1093/ajhp/59.18.1750. [DOI] [PubMed] [Google Scholar]
- 35.MacDougall DA, Feliu AL, Boccuzzi SJ, Lin J. Economic burden of deep-vein thrombosis, pulmonary embolism, and post-thrombotic syndrome. Am. J Health Syst Pharm. 2006;63:S5–15. doi: 10.2146/ajhp060388. [DOI] [PubMed] [Google Scholar]
- 36.Tobian AA, Savage WJ, Tisch DJ, Thoman S, King KE, Ness PM. Prevention of allergic transfusion reactions to platelets and red blood cells through plasma reduction. Transfusion. 2011 doi: 10.1111/j.1537-2995.2010.03008.x. [DOI] [PubMed] [Google Scholar]
- 37.Blumberg N, Kirkley SA, Heal JM. A cost analysis of autologous and allogeneic transfusions in hip-replacement surgery. Am J Surg. 1996;171:324–30. doi: 10.1016/S0002-9610(97)89635-3. [DOI] [PubMed] [Google Scholar]
- 38.Linden JV, Wagner K, Voytovich AE, Sheehan J. Transfusion errors in New York State: an analysis of 10 years' experience. Transfusion. 2000;40:1207–13. doi: 10.1046/j.1537-2995.2000.40101207.x. [DOI] [PubMed] [Google Scholar]
- 39.Lubarsky DA, Hahn C, Bennett DH, Smith LR, Bredehoeft SJ, Klein HG, Reves JG. The hospital cost (fiscal year 1991/1992) of a simple perioperative allogeneic red blood cell transfusion during elective surgery at Duke University. Anesth Analg. 1994;79:629–37. doi: 10.1213/00000539-199410000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Goodnough LT. Risks of blood transfusion. Crit Care Med. 2003;31:S678–86. doi: 10.1097/01.CCM.0000100124.50579.D9. [DOI] [PubMed] [Google Scholar]
- 41.Hellinger FJ. The lifetime cost of treating a person with HIV. JAMA. 1993;270:474–8. [PubMed] [Google Scholar]
- 42.Faris PM, Ritter MA, Keating EM, Valeri CR. Unwashed filtered shed blood collected after knee and hip arthroplasties. A source of autologous red blood cells. J Bone Joint Surg Am. 1991;73:1169–78. [PubMed] [Google Scholar]
- 43.Waters JH, Dyga RM, Waters JF, Yazer MH. The volume of returned red blood cells in a large blood salvage program: where does it all go? (CME) Transfusion. 2011;51:2126–32. doi: 10.1111/j.1537-2995.2011.03111.x. [DOI] [PubMed] [Google Scholar]
- 44.Fuller RL, McCullough EC, Bao MZ, Averill RF. Estimating the costs of potentially preventable hospital acquired complications. Health Care Financ Rev. 2009;30:17–32. [PMC free article] [PubMed] [Google Scholar]
- 45.Munoz M, Kuhlmorgen B, Ariza D, Haro E, Marroqui A, Ramirez G. Which patients are more likely to benefit from postoperative shed blood salvage after unilateral total knee replacement? An analysis of 581 consecutive procedures. Vox Sang. 2007;92:136–41. doi: 10.1111/j.1423-0410.2006.00868.x. [DOI] [PubMed] [Google Scholar]
- 46.Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control. 2000;28:68–75. doi: 10.1016/s0196-6553(00)90015-4. [DOI] [PubMed] [Google Scholar]
- 47.Brown PP, Kugelmass AD, Cohen DJ, Reynolds MR, Culler SD, Dee AD, Simon AW. The frequency and cost of complications associated with coronary artery bypass grafting surgery: results from the United States Medicare program. Ann Thorac Surg. 2008;85:1980–6. doi: 10.1016/j.athoracsur.2008.01.053. [DOI] [PubMed] [Google Scholar]
- 48.Munoz M, Cobos A, Campos A, Ariza D, Munoz E, Gomez A. Post-operative unwashed shed blood transfusion does not modify the cellular immune response to surgery for total knee replacement. Acta Anaesthesiol Scand. 2006;50:443–50. doi: 10.1111/j.1399-6576.2006.00977.x. [DOI] [PubMed] [Google Scholar]
- 49.del Trujillo MM, Carrero A, Munoz M. The utility of the perioperative autologous transfusion system OrthoPAT in total hip replacement surgery: a prospective study. Arch Orthop Trauma Surg. 2008;128:1031–8. doi: 10.1007/s00402-007-0440-6. [DOI] [PubMed] [Google Scholar]
- 50.Waters JH, Tuohy MJ, Hobson DF, Procop G. Bacterial reduction by cell salvage washing and leukocyte depletion filtration. Anesthesiology. 2003;99:652–5. doi: 10.1097/00000542-200309000-00021. [DOI] [PubMed] [Google Scholar]
- 51.Sullivan I, Faulds J, Ralph C. Contamination of salvaged maternal blood by amniotic fluid and fetal red cells during elective Caesarean section. Br J Anaesth. 2008;101:225–9. doi: 10.1093/bja/aen135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bull BS, Bull MH. The salvaged blood syndrome: a sequel to mechanochemical activation of platelets and leukocytes? Blood Cells. 1990;16:5–20. discussion -3. [PubMed] [Google Scholar]
- 53.McKie JS, Herzenberg JE. Coagulopathy complicating intraoperative blood salvage in a patient who had idiopathic scoliosis. A case report. J Bone Joint Surg Am. 1997;79:1391–4. doi: 10.2106/00004623-199709000-00014. [DOI] [PubMed] [Google Scholar]