Abstract
African American (AA) adolescent girls are at heightened risk for HIV and sexually transmitted infections (STIs), and thus knowledge of factors related to risky sexual behavior in this population is crucial. Using Social Learning Theory (Bandura, 1977), this paper examines pathways from female caregivers’ risky sexual behavior and substance use to adolescent girls’ risky sexual behavior and substance use in a sample of 214 low-income, urban AA female caregivers and daughters recruited from outpatient mental health clinics in Chicago. Structural equation modeling (SEM) revealed that sexual risk reported by female caregivers was associated with adolescent sexual risk, and illicit drug use reported by female caregivers was related to adolescent-reported substance use, which was in turn associated with adolescent-reported sexual risk behavior. These findings suggest that female caregivers’ sexual behavior and substance use both relate to girls’ sexual risk. Thus, results emphasize the role of female caregivers in transmitting risk.
Keywords: substance use, risky sexual behavior, female caregivers, adolescent girls
Introduction
Dating and sexual relationships typically begin in adolescence and serve important developmental functions related to establishing intimacy, forming identity, and asserting independence from families (Wolfe, Jaffe, & Crooks, 2006). However, unsafe sexual behavior can have significant negative health consequences including HIV, other sexually transmitted infections (STIs), and pregnancy. Despite an overall decrease in adolescent sexual activity between 1991 and 2007 (Centers for Disease Control and Prevention, 2008b), rates of STIs and unintended pregnancies among United States (US) teens remain high (Gavin et al., 2009).
Racial and gender disparities characterize patterns of risky sexual behavior and STI rates in the United States, with African American (AA) females disproportionately at risk. AA adolescent girls have higher rates of unintended pregnancies and diagnoses of HIV and STIs (i.e., gonorrhea and Chlamydia) than Whites (Finer, 2006; Latka, 2001; Halpern, 2004). Compared to same-aged AA boys, AA girls in some studies report earlier age of sexual debut, higher rates of risky sexual behavior, and lower perceived HIV/AIDS risk (DiClemente et al., 1996; Newman & Zimmerman, 2000), and AA girls consistently report older partners and less condom use than their AA male peers (Centers for Disease Control, 2010). Girls seeking mental health services are at even greater risk because teens with mental health symptoms engage in higher rates of risky sexual behavior than their peers (Brown, 1997; Donenberg & Pao, 2005; Donenberg, Emerson, Bryant, Wilson, & Weber-Shifrin, 2001). Psychological distress is also linked to STIs among AA female adolescents and young adult women in the US (Seth, 2009; Miller-Johnson, 1999; Brown, 2006; Khan, 2009).
Early sexual debut and substance use are associated with riskier sexual behavior in teens. Early sexual debut is an important predictor of sexual risk because it is linked to inconsistent condom use, more sexual partners, and sex while using alcohol or drugs (Kuortti, 2009), as well as increased risk for teen pregnancy and STIs (Coker et al., 1994). Adolescent substance use is linked directly and indirectly to sexual risk behaviors including unprotected sex and sex with multiple partners (Cavazos-Rehg et al., 2010). In the United States marijuana is the most prevalent type of illicit drug used by adolescents (Walker, et al., 2011) and has been linked to increased likelihood of teenage pregnancy (Cavazos-Rehg et al., 2011). Adolescents with behaviorally acquired HIV were more likely to report first use of alcohol or marijuana before the age of 14 (Conner et al, 2011). In this paper, substance use refers to the consumption of legal or illegal drugs (such as alcohol and marijuana) for recreational purposes. Understanding factors that predict adolescents’ sexual risk-taking, early sexual debut, and substance use are critical for developing interventions to reduce teen pregnancy and STIs.
This study was guided by Social Learning Theory (SLT), which posits that people learn from one another in a social context via imitation, observation, and modeling (Bandura, 1977). Thus, children will model their parents’ healthy or risky behaviors (Bandura, 2004). We examined the role of female caregiver behavior (i.e., substance use and sexual risk behavior) in predicting early and risky sexual behavior and substance use among low-income, urban African American (AA) adolescent girls seeking mental health treatment. According to SLT, observation of maternal sexual behaviors and substance use may be associated with early and risky sexual behavior and substance use in adolescent offspring.
Female caregivers’ behavior may be a particularly powerful influence for urban AA girls since they are likely to be raised by single female caregivers and often describe these relationships as foundational (Stevens, 2002). Moreover, strong family relationships are central to AA culture and are related to improved mental health outcomes and less risk behavior (Brody et al., 2006; Brody et al., 2005). Offspring of teenage mothers are more likely to become teenage parents themselves (Shaw, 2006). However, one study with AA daughters of teenage mothers found that the majority did not become adolescent parents, although they did have disparaging educational and financial prospects, similar to their mothers (Furstenburg, 1990). Other evidence suggests that early sexual activity is associated with having a female caregiver who was sexually active or became pregnant at a young age (Udry, 1988; Mott et al., 1996; Bonell et al., 2006; Cavazos-Rehg et al., 2010). In addition to the biological correspondence between biological mothers and daughters’ age at puberty, these female caregivers may convey through their behavior or verbal messages that early sexual activity is acceptable (Mott et al., 1996). Likewise, caregiver substance use, including use of alcohol or drugs, may be modeled by adolescent girls (Denton & Kampfe, 1994) and is associated with girls’ early and risky sexual behavior. Parenting characteristics affected by even casual substance use, such as support and supervision, can lead to poor quality parental-child relationships, which are consistently associated with early and risky sexual activity (Roche et al., 2005; Li, Feigelman, & Stanton, 2000; Meschke, Bartholomae, & Zentall, 2002).
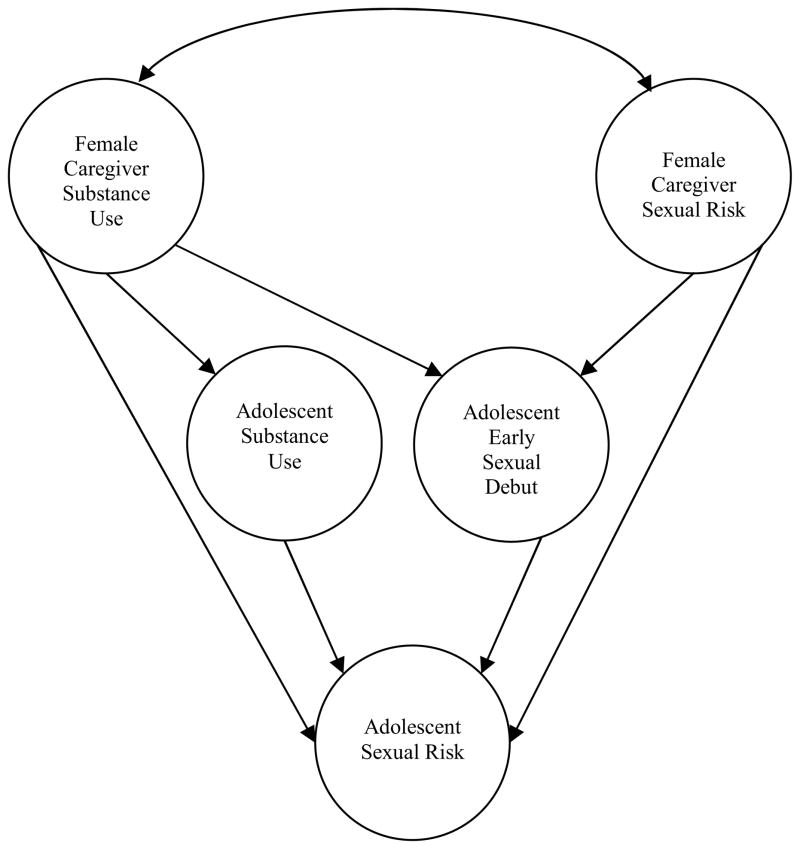
Identifying distinct patterns of risk and understanding family processes that underlie these patterns are important steps in developing prevention and intervention efforts, especially for high risk youth. This study examines links among female caregiver sexual behavior and substance use, and adolescent substance use, early sexual debut, and risky sexual behavior in low-income, urban AA girls with histories of mental health treatment. Consistent with SLT (Bandura, 1977), we predicted that more illicit drug and alcohol use and more risky sexual behavior reported by female caregivers would be associated with similar patterns of behavior (more illicit drug and alcohol use, earlier age of sexual debut, and riskier sexual behavior) reported by daughters. We also expected girls’ substance use to mediate the relationship between maternal substance use and adolesent risky sexual behavior, and early sexual debut to mediate the relationship between maternal risky sexual behavior and adolescent risky sexual behavior. Figure 1 depicts hypothesized pathways.
Figure 1.
Hypothesized model linking female caregiver substance use to adolescent substance use, early sexual debut, and sexual risk behaviors.
Methods
Participants
Participants were part of a larger longitudinal study of HIV-risk among low-income AA adolescent girls seeking mental health services. AA girls (12–16 years-old; M=14.3) and their primary female caretakers were recruited from several outpatient mental health clinics in Chicago. Clinic staff invited eligible families to participate. A total of 281 mother-daughter dyads were consented and 268 completed the baseline interview. Female caregivers and girls completed a series of paper-and-pencil and computerized questionnaires every 6 months between baseline and 24-months (5 waves of data collection in total). At baseline girls completed the Diagnostic Interview Schedule for children (DISC 4.0), and 5% met DSM-IV criteria for PTSD in the past year, 4% for major depressive disorder, and 11% for conduct disorder.
The present study includes data from Waves 1 and 2 (N=214). All interviews took place at the Institute for Juvenile Research at the University of Illinois at Chicago (UIC). Informed consent and assent were obtained from female caregivers and daughters separately, and each received $40 for their participation. Retention at 6-months was strong (81%). There were no significant differences in girls’ age (t(265) = −.19, p > .10), caretaker age (t(265) = −.21, p > .10), relationship type of the female caretaker (biological mother, adopted mother, grandmother, aunt, etc; χ2(5), N=267 = 1.77, p > .10), or family socioeconomic status (SES; χ2(4), N=267 = 7.3, p > .12) (Hollingshead, 1975) between families who completed Wave 2 and those who did not. There were also no significant differences between female caregivers who did or did not complete Wave 2 in regard to any of the caregiver variables included in the present analyses. As shown in Table 1, nearly three fourths (73.5%) of the female caregivers were biological mothers with grandmothers the second most common (14.9 %). Additionally 73.2% considered themselves single parents. Non-biological female caregivers were included in the sample since they self-identified as the primary female caregiver and represent the person whom the adolescent would have observed most often.
Table 1.
Descriptive Statistics
| Range | Adolescents (N=268) | Female Caregivers (N=268) | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| N | % | M(SD) | N | % | M(SD) | ||
| Female Caregiver Type | |||||||
| Biological mom | 197 | 73.5 | |||||
| Adoptive mom | 12 | 4.5 | |||||
| Foster mom | 2 | 0.7 | |||||
| Aunt | 10 | 3.7 | |||||
| Grandmother | 40 | 14.9 | |||||
| Other | 7 | 2.6 | |||||
| Single Parent | 194 | 73.2 | |||||
| Age at baseline | 14.45(1.2) | 42.93(11.1) | |||||
| Substance Use | |||||||
| Freq. of Alcohol Use^ | 0–20 | .80(1.6) | 4.45(6.3) | ||||
| Lifetime Illicit Drug Use | 0–1 | 50 | 23.4 | ||||
| Lifetime Illicit Drug Use | 0–5 | .93(1.2) | |||||
| Early Sexual Debut^ | |||||||
| Not sexually active | 0–1 | 181 | 67.8 | ||||
| Age 15 or older | 0–1 | 12 | 4.5 | 176 | 65.9 | ||
| Age 13 to 14 | 0–1 | 57 | 21.3 | 62 | 23.2 | ||
| Age 13 or younger | 0–1 | 17 | 6.4 | 29 | 10.9 | ||
| Sexual Risk Behaviors^ | |||||||
| Teen pregnancy* | 0–1 | 22 | 8.2 | 135 | 51.3 | ||
| Condom Use | .74(1.4) | ||||||
| No sex in past 6 mo | 0–1 | 151 | 70.9 | ||||
| Always | 0–1 | 27 | 12.7 | ||||
| More than half | 0–1 | 10 | 4.7 | ||||
| Half of the time | 0–1 | 7 | 3.3 | ||||
| Some of the time | 0–1 | 5 | 2.3 | ||||
| Never | 0–1 | 13 | 6.1 | ||||
| Sex while using substances | 0–1 | 15 | 7.0 | ||||
| High Risk partner | 0–1 | 50 | 23.4 | 49 | 18.5 | ||
| Lifetime number of partners | 0–100 | 9.6(11.2) | |||||
| Number of partners^ | 0–12 | .57(1.1) | .90(1.0) | ||||
Note: Frequencies (%) are reported for dichotomous variables and means and standard deviations for continuous variables.
defined as less than age 18 for mothers
reflects behavior during past 6 months
Measures
Adolescent sexual behavior and substance use
Adolescent sexual behavior was assessed with the AIDS-Risk Behavior Assessment - Adolescent Version (ARBA). The ARBA is a computer-assisted structured interview designed specifically for use with teens to assess sexual behavior, drug use, and needle use (Donenberg et al., 2001). The ARBA was derived from five well-established measures used in large-scale studies to examine drug use, sexual behavior, and HIV-risk behaviors in youth (IBS, 1991; Needle, Fisher, Weatherby et al., 1995; NIDA, 1995; Teplin, Mericle, McClelland, & Abram, 2003; Watters, 1994). The ARBA uses a skip structure so that questions initially answered in the negative are not followed by more detailed questions. The ARBA assesses type, frequency, and method of substance use and sexual behavior directly related to HIV transmission. An early sexual debut scale was created from the adolescent’s report of the age of her earliest vaginal, oral, or anal sexual experience (0=never; 1 = age 15 or later; 2 = age 13 or 14; 3 = before age 13) based on evidence that these age ranges are reasonable indicators of relative risk (Coker et al., 1994). The early sexual debut variable refers only to the reported age of first sexual experience, not whether these experiences were coerced or consensual, as any sexual contact may contribute to later risk. Legally, of course, many of these sexual experiences could be considered abuse, even if they were consensual. Furthermore, a small number (n=5) reported sexual experiences at very young ages (before age 11) and therefore, some of these experiences most likely reflect sexual abuse. Adolescent sexual risk behaviors included in the present analyses were (1) teen pregnancy; (2) number of partners in the past 6 months (male or female partners with whom they had anal or vaginal sex; both male and female partners are included as any sexual partner is associated with risk); (3) having had a high risk partner (defined as someone with unknown sexual history or two or more years older); (4) inconsistent condom use during vaginal sex, a scaled variable ranging from 0 (did not have sex) to 5 (never used condoms); (5) sex while under the influence of alcohol or drugs (a binary variable coded as “1” if they reported this experience or “0” if they did not). Substance use variables were (1) frequency of alcohol use in the past 6 months (number of occasions on which alcohol was consumed) and (2) lifetime use of any illicit drugs used (a binary variable reflecting any use of marijuana, crack, cocaine, amphetamines, ice, heroin, heroin/cocaine mixed, heroin/speed mixed, non-prescription methadone, opiates/narcotics, barbiturates, tranquilizers, psychedelics, or any other recreational drug).
The Wave 1 ARBA assessed lifetime behavior and behavior over the past 6 months; the Wave 2 ARBA assessed behavior over the past 6 months. When possible, Wave 2 data were used for adolescent behavior so that female caregiver behavior was assessed at a previous time point, and longitudinal data is recommended for testing mediation models (MacKinnon, 2008). However, for accurate data on the full sample, Wave 1 and 2 data were combined for age of sexual debut and pregnancy and also for lifetime report of drug use since drug use was relatively low in the sample over the past 6 months. Wave 1 was used in the few cases of inconsistencies between Wave 1 and Wave 2. All other variables used in the analysis were assessed at Wave 2.
Maternal sexual behavior and substance use
Female caregivers reported their sexual behavior and use of alcohol and illicit drugs on a parallel version of the ARBA. Sexual risk behaviors assessed for female caregivers included early sexual debut (the same scaled variable used for adolescents created from reported age of first vaginal or anal sexual intercourse), teen pregnancy (before age 18), number of sexual partners in the past 6 months (including both males and females), lifetime number of partners (including both males and females), and having had a high risk sexual partner (defined as someone with an unknown sexual history, an intravenous drug user, or a prostitute). Substance use variables for female caregivers included frequency of alcohol use in the past 6 months and lifetime number of illicit drugs used (including marijuana, crack, cocaine, amphetamines, ice, heroin, heroin/cocaine mixed, heroin/speed mixed, non-prescription methadone, opiates/narcotics, barbiturates, tranquilizers, psychedelics, or any other recreational drug; see table 1). Lifetime number of illicit drugs was used to reflect overall substance use history rather than current drug abuse or dependence, which might suggest a more acute problem. This variable is not meant to identify or distinguish between substance abuse or substance dependence and may include both casual and chronic, problematic use. Lifetime substance use also reflects general female caregiver patterns of behavior that were potentially observed and modeled throughout the girls’ lifetimes. Wave 1 data were used to assess maternal behavior.
Analyses
Statistical outliers (those more than 2 standard deviations higher than the mean) were transformed to reflect the upper quartile. Zero count data were included in the analyses in order to retain the largest sample size. Hypotheses were tested with bivariate correlations and latent variable structural equation modeling (SEM) using Mplus 5.1. SEM tested the measurement and structural models according to overall goodness of fit and examination of specific parameter estimates (i.e., regression coefficients). Goodness of fit was evaluated with multiple indices: the Chi-Square Test of Model Fit (χ2), the Comparative Fit Model (CFI), the Tucker-Lewis index (TLI), the Root Mean Square Error of Approximation (RMSEA), and the Weighted Root Mean Square Residual (WRMR). Individual factor loadings (measurement model) and path estimates (structural model) were reported in the form of standardized linear regression coefficients for continuous factor indicators or dependent variables. Statistical significance was assessed with z-scores, and R2 provided a measure of effect size. To address missing data, we used full information maximum likelihood estimation, which minimizes bias and loss of power (Allison, 2003; Curran & Hussong, 2003). Weighted least square parameter estimates were calculated using a diagonal weight matrix with standard errors and mean- and variance-adjusted χ2 test statistics that use a full weight matrix (WLSMV). WLSMV is appropriate for models with binary variables and missing data (Muthen and Muthen, 1998–2007).
Results
Descriptives
Descriptive statistics are shown in Table 1; 40% (86) of the girls reported being sexually active by Wave 2. Among the sexually active girls 12.6% (n=27) reported more than one partner in the past 6 months, 23% (n=50) reported a high risk partner, 12.7 (n=27) % reported always using a condom in the past 6 months, and 7% (n=15) reported having sex while using substances in the past 6 months. A fourth of the adolescents reported using alcohol at least once in past 6 months, and 23% (n=50) reported illicit drug use in their lifetimes (22% one type of drug; 1% 2 or more types). Among female caregivers, mean frequency of alcohol use was 4.45 times over the past 6 months. Just over half (54.1%, n=147) of the female caregivers reported illicit drug use in their lifetime with 35.1% reporting one type of drug (n=95) and 19% (n=52) of the sample reporting 2 or more drug types. More than a third of female caregivers (34.1%, n=91) reported becoming sexually active before age 15, and slightly more than half (51.3%, n=135) reported teen pregnancy.
As shown in Table 2, there were some bivariate associations between female caregivers’ and girls’ sexual behavior. Earlier female caregiver sexual debut was associated with girls reporting more sexual partners, and more sexual partners reported by female caregivers in the past 6 months was associated with girls’ early sexual debut, number of partners, and sex while using substances. Interestingly, female caregiver teen pregnancy was negatively correlated with teen pregnancy for girls. Female caregiver illicit drug use was associated with girls’ number of partners, illicit drug use, and frequency of alcohol use.
Table 2.
Bivariate correlations
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Female caregiver early sexual debut | - | ||||||||||||||
| 2. Female caregiver teen pregnancy | .33** | - | |||||||||||||
| 3. Female caregiver high risk partners | .16** | −.10 | - | ||||||||||||
| 4. Female caregiver number of partners1 | .36** | .65** | .33** | - | |||||||||||
| 5. Female caregiver number of lifetime partners | .32** | .13* | .47** | .36** | - | ||||||||||
| 6. Female caregiver illicit drug use | .09 | .01 | .26** | .17 | .40** | - | |||||||||
| 7. Female caregiver frequency of alcohol use1 | .08 | −.07 | .10 | .07 | .16** | .19** | - | ||||||||
| 8. Adolescent early sexual debut | .02 | −.10 | .01 | .18** | .07 | .03 | −.07 | - | |||||||
| 9. Adolescent pregnancy | −.10 | −.12* | −.08 | −.06 | . 07 | .02 | −.01 | .37** | - | ||||||
| 10. Adolescent number of sexual partners1 | .14* | −.01 | .02 | .15* | . 06 | .20** | −.05 | .36** | .03 | - | |||||
| 11. Adolescent high risk partners1 | .02 | −.10 | .02 | .10 | .06 | .07 | −.01 | .52** | .22** | .44** | - | ||||
| 12. Adolescent condom use1 | .05 | −.10 | .02 | .10 | −.02 | .06 | .03 | .39** | .28** | .61** | .59** | - | |||
| 13. Adolescent sex while using substances1 | .06 | −.09 | .01 | .33** | .09 | .09 | .02 | .36 | .06 | .35** | .45** | .42** | - | ||
| 14. Adolescent illicit drug use1 | −.02 | −.06 | .03 | .12 | .27** | .17* | .03 | .51** | .23** | .30** | .57** | .27** | .42** | - | |
| 15. Adolescent frequency of alcohol use1 | −.06 | −.04 | .09 | .10 | .16* | .15* | .02 | .29** | .14* | .28** | .39** | .29** | .48** | .56** | - |
denotes frequency from past 6 months
Confirmatory factor analyses (CFA)
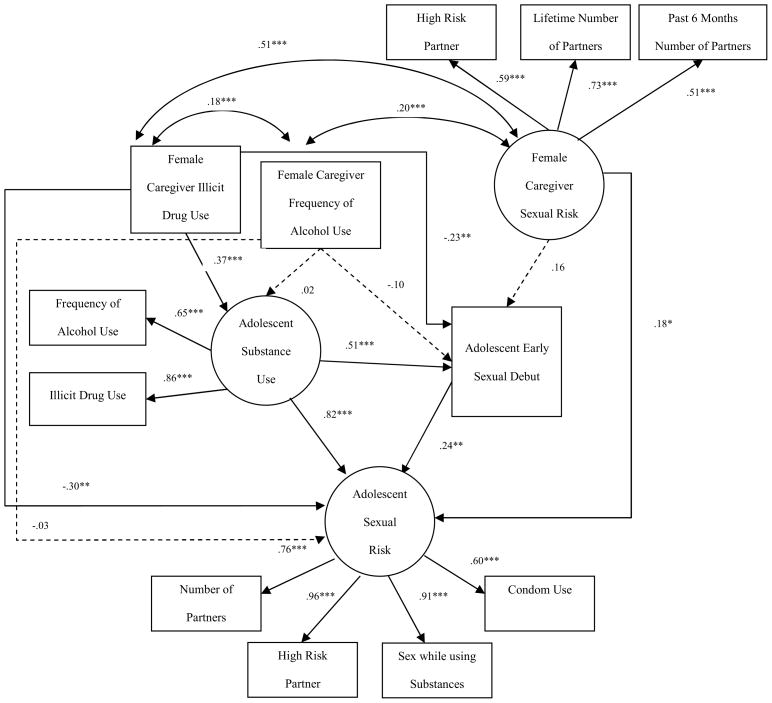
The original measurement model included five observed indicators of female caregiver sexual risk (early sexual debut, teen pregnancy, past 6 month number of partners, lifetime number of partners, and sex with a high risk partner), but early sexual debut (β = .31) and teen pregnancy (β = .38) did not load strongly onto the latent factor and so were dropped from the model. In addition, female caregiver frequency of alcohol use did not load strongly on the latent factor with illicit drug use (β = .28), and therefore female caregiver alcohol use and illicit drug use were split into separate observed variables. The final measurement model included single observed indicators of female caregiver frequency of alcohol use, female caregiver illicit drug use, and adolescent early sexual debut and latent variables for female caregiver sexual risk (number of partners in past 6 months, lifetime number of partners, and sex with a high risk partner), adolescent substance use (frequency of alcohol use and any illicit drug use), and adolescent sexual risk (number of partners, high risk partners, sex while using substances, and inconsistent condom use). The measurement model also included bivariate correlations among the primary model variables (see Table 3). Fit indexes for the CFA model were satisfactory: χ2 = 39.31, df = 16, p < .01; CFI = .94; TLI = .94; RMSEA = .07; WRMR = .75. The significant chi-square is common even in good-fitting models with sample sizes over 200, and the more important indicator of model fit is that the chi-square to degrees of freedom ratio is under 3 (Kline, 1998). Factor loadings of the observed variables on the latent constructs were all above .50 and statistically significant (p ≤ .001; see Figure 2). As shown in Table 3, correlations among the primary model variables were significant, except for those between female caregiver illicit drug use and adolescent early sexual debut, female caregiver illicit drug use and adolescent sexual risk, female caregiver frequency of alcohol use and adolescent substance use, and female caregiver sexual risk and adolescent early sexual debut.
Table 3.
Bivariate correlations between primary model variables
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Female caregiver frequency of alcohol use | - | ||||
| 2. Female caregiver illicit drug use | .19*** | - | |||
| 3. Female caregiver sexual risk | .20*** | .47*** | - | ||
| 4. Adolescent substance use | .06 | .27*** | .33*** | - | |
| 5. Adolescent early sexual debut | −.07 | .02 | .12 | .45*** | - |
| 6. Adolescent sexual risk | .00 | .09 | .21** | .85*** | .63*** |
p ≤ .05;
p ≤ .01;
p ≤ .001
Figure 2.
Structural equation model linking female caregiver substance use to adolescent early sexual debut and adolescent sexual risk behaviors through adolescent substance use. Numbers above the paths are standardized linear regression coefficients for continuous dependent variables. Circles represent latent constructs, and rectangles represent observed variables. ***p<.001 (two tailed).
Latent variable path analysis
A mediated path model specified female caregiver frequency of alcohol use and illicit drug use as predictors of girls’ substance use, girls’ early sexual debut, and girls’ sexual risk. Female caregiver sexual risk also predicted girls’ early sexual debut and sexual risk. In turn, girls’ substance use predicted both early sexual debut and adolescent sexual risk behavior, and early sexual debut predicted sexual risk (see Figure 1). Mediation was assessed according to the criteria described by Baron & Kenny (1986) and tests of indirect effects (MacKinnon, 2008).
Overall model fit was satisfactory: χ2 = 42.62, p < .01, df = 16; CFI = .93; TLI = .93; RMSEA = .08; WRMR = .80. Statistically significant pathways are depicted in Figure 2 as solid lines, and non-significant paths are indicated by dotted lines. This model explained 86% of the variance in girls’ risky sexual behavior. Female caregiver illicit drug use predicted girls’ substance use (β = .37, p < .001), which in turn was associated with both girls’ early sexual debut (β = .82, p < .001) and sexual risk (β = .51, p < .001). Although traditional criteria for mediation (Baron & Kenny, 1986) were not supported since the bivariate relationship between female caregiver illicit drug use and adolescent risky sex was non-significant, a significant indirect pathway from female caregiver illicit drug use to girls’ sexual risk, via girls’ substance use was indicated (β = .30, p < .001). Girls’ early sexual debut was also associated with riskier sexual behavior (β = .24, p < .001), and an additional indirect pathway from female caregiver illicit drug use through both girls’ substance use and early sexual debut was supported (β = .05, p < .05). As predicted, female caregiver sexual risk was also associated with girls’ sexual risk, although the relationship was very small in magnitude (β = .18, p < .05). In addition, a direct relationship was revealed in this multivariate model, whereby female caregiver illicit drug use was negatively associated with girls’ early sexual debut (β = −.30, p < .01) and sexual risk behavior (β = −.23, p < .01).
Discussion
Findings from this study shed new light on how female caregiver behavior can influence sexual risk taking and substance use among low-income, treatment seeking, urban African American girls. Previous research shows that female caregivers exert substantial influence on their daughters’ risk-related behaviors (Hutchinson & Montgomery, 2007). Our findings provide modest support for a social learning effect in this sample of girls, but they also suggest that mechanisms linking female caregivers’ and daughters’ risk behaviors may be more complex than direct behavioral modeling.
As predicted, girls’ risk behavior reflected their female caregivers’ behavior – both substance use and risky sexual behavior. These findings emphasize the influence of maternal behavior on AA girls’ behavior and the importance of addressing female caregivers’ behaviors in efforts to reduce sexual risk in urban AA girls with histories of mental health treatment. Our findings particularly highlight the role of substance use – both of girls and their female caregivers -- in treatment-seeking AA girls’ sexual risk behavior. In our multivariate analysis, the strongest relationships found linked girls’ substance use to early onset of sexual intercourse and to riskier sexual behavior. In addition, female caregivers’ illicit drug use was indirectly linked to girls’ early sexual debut and sexual risk.
These findings indicate that substance use, including casual use, of both female caregivers and girls should be addressed in clinical interventions to reduce sexual risk in mental health treatment-seeking AA girls. Family based HIV prevention or sexual risk interventions often target general health care, educational needs, or children’s mental health concerns (Richter, Manegold, & Pather, 2004). Maternal sexual risk behaviors or illicit drug use are typically not included in such interventions where the focus is on addressing negative sexual risk outcomes in the adolescent. Family based therapies aim to intervene with youth during early adolescence, prior to the initiation of sexual and drug risk-taking behavior (Bhana, McKay, Mellins, Petersen, & Bell, 2010), but may not address either of these same risk behaviors in female caregivers. Our findings are based on a sample of AA girls with mental health problems, who may engage in higher rates of risky sexual behavior and overall substance use than their peers (Brown, 1997; Donenberg & Pao, 2005; Donenberg, Emerson, Bryant, Wilson, & Weber-Shifrin, 2001; Lamps, Sood, & Sood, 2008).
The National Household Survey on Drug Abuse (NHSDA) estimates that 10% of children (more than seven million) in the US have at least one parent who is dependent on drugs or alcohol, and 6% have at least one parent who needs alcohol or substance abuse treatment (Conners, 2004). Children of substance users are at high risk for a variety of developmental, biological, and behavioral problems, including becoming a drug or alcohol addict themselves (Conners, 2004). However, the majority of studies assessing the impact of alcohol and substance use on older children have focused on intact family units with an alcoholic father (Johnson, 1991). Few studies have examined the role of female caregivers’ illicit drug use or have considered the effects of casual substance use on adolescent risk behavior. This study provides much needed insight into the potential role of general maternal substance use for the development of AA girls who seek mental health treatment and highlights risk associated with female caregivers’ drug use versus alcohol use in this particular population.
Adolescent outcomes result from complex mediated pathways through which caregivers’ behavior histories both directly and indirectly predict child outcomes (Serbin & Karp, 2004). Our findings support a direct transfer of risk from female caregivers’ drug use history to girls’ current level of substance use. Girls’ substance use was, in turn, associated with early and risky sexual behavior. These findings suggest that a cascade of risk may be initiated from female caregivers’ substance use, whether or not it is severe enough to be labeled as abuse or dependence, leading to girls’ substance use, followed by early adolescent sexual debut and risky sexual behaviors.
A number of other factors may contribute to this pattern of intergenerational transmission of HIV-risk, such as parent-child communication (Hutchinson, 2002), parenting style (Bonell et al., 2006), parental monitoring (DiClemente et al., 2001), and maternal connectedness (Aronowitz & Morrison-Beedy, 2004). Previously indentified parental influences on adolescent substance use include low warmth (Nash et al, 2005), non-engagement/involvement (Simons-Morton & Chen, 2005), inconsistency (Windle, 1996), and poor monitoring (Dishion & Loeber, 1985). Family influence on adolescent drug use may also be mediated by social environment factors (Stice & Barrera, 1995; Taylor & Repetti, 1997), whereby teens whose parents abuse substances are more vulnerable to stress (Barrera et al, 1995) and tend to affiliate with substance-using peers (Wills et al, 1994). Lack of support, rejection, and detachment from caregivers, common characteristics of homes with frequent parental substance use, have also been associated with adolescent substance use (Barrera et al, 1993). Similar patterns exist for adolescent sexual risk taking (Metzler et al, 1994).
Findings also support literature linking adolescent substance use and risky sexual behavior (Cavazos-Rehg, 2010). Alcohol and illicit drug use may lead to risky sexual behavior due to impaired judgment, poor decision-making, and associations with peers who use illicit substances. Substance use debut and risky sexual behavior often emerge during adolescence (Taylor & Repetti, 1997) and can have direct and indirect health consequences (e.g., HIV/STIs, sleep disturbance, poor diet) (Donovan et al, 1991). Adolescent sexual decision-making in an urban setting is complex and reflects a combination of social and psychological factors (Paikoff, Parfenoff, Williams, & McCormick, 1997), especially in a mental health population. The strong link between substance use and sexual risk may relate to a “race-ethnic crossover effect” whereby AA youths are found to be at less risk of drug and alcohol use relative to Caucasian or Hispanic teens, although they are at heightened risk after age 35 (Watt & Rogers, 2007; Watt, 2008). Thus, AA girls who are involved in substance use during adolescence may represent a particularly high risk population relative to their peers, especially those seeking mental health treatment.
A surprising finding was revealed when multiple risk factors were taken into account in the multivariate model. Female caregivers’ illicit drug use was also directly associated with less sexual risk among girls. Although a clear pathway was revealed whereby female caregivers’ illicit drug use indirectly predicted sexual risk via girls’ own substance use, an alternate pathway suggested that for some girls, more extensive caregiver drug use may actually be associated with less risk if girls do not use substances themselves. Although this finding was unexpected, it may be related to other hypotheses used to explain the race-ethnic crossover effect. One theory suggests that familial characteristics are responsible for the protective effects seen in AA culture such as the role of religion and involvement of extended kinship networks (French, Finkbiner, & Duhamel, 2002), and these protective factors may extend to sexual risk even in some homes affected by caregiver drug use. It is also possible that illicit drug use in female caregivers results in some AA girls taking on a more independent or parental role within the family, thus, limiting opportunities for sexual risk. This unexpected finding was consistent with the negative correlation found between teen pregnancy in female caregivers and adolescent girls, and similar mechanisms may explain both. More longitudinal research is needed to determine whether this pattern is unique to this particular sample and what aspects of the family environment may explain it.
This study has a number of important strengths. In particular, we focus on low-income AA girls, who are at disproportionate risk for STIs and HIV but have been neglected in research on risk behavior and related family characteristics. Uniquely, we include a majority of families in which the female caregiver considers herself a single parent. We employed a longitudinal assessment and examined a multivariate path model including both direct and indirect relationships.
Nonetheless, study limitations warrant careful interpretation of findings. First, lack of power could account for some non-significant findings. Second, since the focus of this paper was on connections between female caretakers’ and daughters substance use and sexual risk, we did not examine the role of mental health symptoms. Although participant rates of diagnosable mental health disorders as assessed by the DISC were low, the presence of mental health symptoms likely play a role in the risk behaviors discussed here. Third, retrospective self-reports of substance use and sexual behavior may be biased in favor of social desirability. Moreover, retrospective recollections of age of sexual debut and lifetime substance use may not be accurate, particularly for female caregivers. Fourth, results may not generalize to non-African Americans, non-urban girls, or to girls who are not seeking mental health services. Fifth, important differences in these relationships may exist for biological and non-biological female caretakers. We did not examine differences because the majority of caretakers (74%) were biological female caregivers. Sixth, it is possible, and even likely, that reports of early sexual experience represent sexual abuse in at least some cases. With the existing data, however, we cannot tease apart which cases were perceived as voluntary or coerced, and this distinction is blurry regarding sexual experiences among minors. In either case, our findings suggest that early sexual contact, regardless of whether it is consensual or nonconsensual, appears to set the stage for later risky sexual behavior. Seventh, since the focus of this paper was on female caregivers, we did not examine the effects of peer influence on adolescent substance use, which likely influences sexual risk taking behavior. Finally, in this study pre-natal effects of substance use on adolescent behavior cannot be distinguished from effects of post-natal substance use.
Identification of maternal substance use as a risk factor may provide direction for family oriented clinical intervention and prevention efforts for AA girls seeking mental health services. These results support family based interventions focused on reduction of sexual risk taking and substance use in both female caregivers and girls. Treating only the adolescent while ignoring the influence of maternal behavior may not effectively reduce sexual risk taking. In fact, most positive outcomes are short-lived for youth (Snitzman et al., 2011) and by addressing maternal risk, benefits for youth may be sustained longer. Interventions are needed that target both caregiver and adolescent substance use and sexual risk taking and links between female caregivers’ and girls’ risk behaviors.
Acknowledgments
This research is supported by a grant from the National Institute of Mental Health (R01 MH65155).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Tiffany Brakefield, Email: tiffany.brakefield@gmail.com, Department of Psychology, Rosalind Franklin University of Medicine and Science, 3333 Green Bay Road, North Chicago, IL 60064, USA; ph: (001) 847-578-3311; fax: (001)847-578-8765.
Helen Wilson, Email: helen.wilson@gmail.com, Department of Psychology, Rosalind Franklin University of Medicine and Science, 3333 Green Bay Road, North Chicago, IL 60064, USA; ph: (001)847-578-3311; fax: (001) 847-578-8765.
Geri Donenberg, Email: gdonenberg@psych.uic.edu, University of Illinois at Chicago, Department of Psychiatry, Healthy Youths Program, 1747 W. Roosevelt Road (M/C 747), Chicago, IL 60608, USA; ph: (001) 312-996-8602; fax: (001) 312-413-2920.
References
- Allison P. Missing data techniques for structural equation models. Journal of Abnormal Psychology. 2003;112:545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- Aronowitz T, Morrison-Beedy D. Resilience to risk-taking behaviors in impoverished African American girls: the role of mother-daughter connectedness. Res Nurs Health. 2004;27(1):29–39. doi: 10.1002/nur.20004. [DOI] [PubMed] [Google Scholar]
- Bachman JG, OM, PM, Schulenberg JE, et al. The Decline of Substance Use in Young Adulthood: Changes in Social Activities, Roles, and Beliefs. Mahwah, NJ: Lawrence Erlbaum Associates; 2002. [Google Scholar]
- Bandura A. Social learning theory. Oxford, England: Prentice-Hall; 1977. [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrera M, Chassin L, Rogosch F. Effects of social support and conflict on adolescent children of alcoholic and nonalcoholic fathers. J Pers Soc Psycho. 1993;64:602–12. doi: 10.1037//0022-3514.64.4.602. [DOI] [PubMed] [Google Scholar]
- Barrera M, Li SA, Chassin L. Effects of parental alcoholism and life stress on Hispanic and non-Hispanic Caucasian adolescents: a prospective study. Am J Commmunity Psychol. 1995;23:479–507. doi: 10.1007/BF02506965. [DOI] [PubMed] [Google Scholar]
- Bhana A, McKay M, Mellins C, Petersen I, Bell C. Family-based HIV prevention and intervention services for youth living in poverty-affected contexts: the CHAMP model of collaborative, evidence-informed program development. J Int AIDS Soc. 2010;13(Suppl 2):S8. doi: 10.1186/1758-2652-13-S2-S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonell C, Allen E, Strange V, Oakley A, Copas A, Johnson A, Stephenson J. Influence of family type and parenting behaviors on teenage sexual behavior and conceptions. J Epidemiology Community Health. 2006;60(6):502–506. doi: 10.1136/jech.2005.042838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Murry VM, Gerrard M, Gibbons FX, McNair L, Brown AC, et al. The Strong African American Families Program: Prevention of youths’ high-risk behavior and a test of a model of change. Journal of Family Psychology. 2006;20:1–11. doi: 10.1037/0893-3200.20.1.1. [DOI] [PubMed] [Google Scholar]
- Brody GH, Murry VM, McNair L, Chen YF, Gibbons FX, Gerrard M, et al. Linking changes in parenting to parent-child relationship quality and youth self-control: The Strong African American Families Program. Journal of Research on Adolescence. 2005;15:47–69. [Google Scholar]
- Brown K, Tolou-Shams M, Lescano M, Lourie K. Depressive symptoms as a predictor of sexual risk among African American adolescents and young adults. Journal of Adolescent Health. 2006;39:444–448. doi: 10.1016/j.jadohealth.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Brown L. Adolescents with psychiatric disorders and the risk of HIV. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1609–1617. doi: 10.1016/S0890-8567(09)66573-4. [DOI] [PubMed] [Google Scholar]
- Cavazos-Rehg PA, Spitznagel EL, Bucholz KK, Nurnberger J, Jr, Edenberg HJ, Kramer JR, et al. Predictors of Sexual Debut at Age 16 or Younger. Arch Sex Behav. 2010;39(3):664–673. doi: 10.1007/s10508-008-9397-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavazos-Rehg P, Krauss M, Spitznagel E, Schootman M, Cottler L, Beirut L. Substance use and the risk for sexual intercourse with and without a history of teenage pregnancy among adolescent females. J Stud Alcohol Drugs. 2011;72(2):194–8. doi: 10.15288/jsad.2011.72.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance -- United States, 2009. Morbidity and Mortality Weekly Report. 2010;57(SS-4) [PubMed] [Google Scholar]
- Coker A, Richter D, Valois R, McKeown R, Garrison C, Vincent M. Correlates and consequences of early initiation of sexual intercourse. J Sch Health. 1994;64(9):372–7. doi: 10.1111/j.1746-1561.1994.tb06208.x. [DOI] [PubMed] [Google Scholar]
- Conners N, Bradley R, Mansell LW, Liu J, et al. Children of mothers with serious substance abuse problems: An accumulation of risks. The American Journal of Drug and Alcohol Abuse. 2004;30(1):85–100. doi: 10.1081/ada-120029867. [DOI] [PubMed] [Google Scholar]
- Conner L, Wiener J, Lewis J, Phill R, Peralta L, Chandwani S, Koenig L. Prevalence and Predictors of Drug Use Among Adolescents with HIV Infection Acquired Perinatally or Later in Life. AIDS Behav. 2011 Aug 14; doi: 10.1007/s10461-011-9950-x. [DOI] [PubMed] [Google Scholar]
- Curran P, Hussong A. The use of latent trajectory models in psychopathology research. Journal of Abnormal Psychology. 2003;112:526–544. doi: 10.1037/0021-843X.112.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denton R, Kampfe C. The relationship between family variables and adolescent substance abuse: a literature review. Adolescence. 1994;29:475–495. [PubMed] [Google Scholar]
- DiClemente RJ, Lodico M, Grinstead OA, Harper G, Rickman RL, Evans PE, et al. African-American adolescents residing in high-risk urban environments do use condoms: Correlates and predictors of condom use among adolescents in public housing developments. Pediatrics. 1996;98(2):269–278. [PubMed] [Google Scholar]
- DiClemente R, Wingood G, Crosby R, Sionean C, Brown L, Rothbaum B, Zimand E, Cobb B, Harrington K, Davies S. A prospective study of psychological distress and sexual risk behavior among black adolescent females. Pediatrics. 2001;108(5):E85. doi: 10.1542/peds.108.5.e85. [DOI] [PubMed] [Google Scholar]
- Dishion T, Loeber R. Adolescent marijuana and alcohol use: The role of parents and peers revisited. Am J of Drug Alc Abuse. 1985;11:11–25. doi: 10.3109/00952998509016846. [DOI] [PubMed] [Google Scholar]
- Donenberg G, Pao M. Youths and HIV/AIDS: Psychiatry’s role in a changing epidemic. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:728–747. doi: 10.1097/01.chi.0000166381.68392.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: Links to psychopathology and peer relationships. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:642–653. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan J, Jessor R, Costa F. Adolescent health behavior and conventionality-unconventionality: an extension of problem-behavior theory. Health Psychology. 1991;10:52–61. [PubMed] [Google Scholar]
- Finer L, Henshaw S. Disparities in rates of unintended pregnancy in the United States. Perspect Sex Reprod Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- French K, Finkbiner R, Duhamel L. Patterns of substance use among minority youth and adults in the United States: An overview and synthesis of national survey findings. Center for Substance AbuseTreatment (CSAT); 2002. [Google Scholar]
- Furstenburg F, Levine J, Brooks-Gunn J. The children of teenage mothers: Patterns of early childbearing in two generations. Family Planning Perspectives. 1990;22(2):54–61. [PubMed] [Google Scholar]
- Gavin L, MacKay A, Brown K, Harrier S, et al. Sexual and Reproductive Health of Persons Aged 10--24 Years --- United States, 2002--2007. CDC: Surveillance Summaries. 2009;58(SS06):1–58. [PubMed] [Google Scholar]
- Halpern C, Bauer D, Iritani B, Waller M, Cho H. Implications of racial and gender differences in patterns of adolescent risk behavior for HIV and other sexually transmitted diseases. Perspect Sex Reprod Health. 2004;36(6):239–247. doi: 10.1363/psrh.36.239.04. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Unpublished working paper. Department of Sociology, Yale University; New Haven, CT: 1975. A Four-Factor Index of Social Status. [Google Scholar]
- Hutchinson K, Montgomery A. Parent communication and sexual risk among African Americans. Western J Nurs Res. 2007;29:691–707. doi: 10.1177/0193945906297374. [DOI] [PubMed] [Google Scholar]
- Hutchinson M. Sexual risk communication with mothers and fathers: Influence on the sexual risk behaviors of adolescent daughters. Family Relations. 2002;51:238–247. [Google Scholar]
- IBS. Denver Youth Survey Youth Interview Schedule. University of Colorado; Boulder, CO: 1991. [Google Scholar]
- Johnson J. Forgotten no longer: am overview on children of chemically dependent parents. In: Rivinus T, editor. Children of Chemically Dependent Parents: Multiperspectives from the Cutting Edge. New York, NY: Brunner Macel; 1991. pp. 29–53. [Google Scholar]
- Khan M, Kaufman J, Pence B, Gaynes B, Adimora A, Weir S, Miller C. Depression, sexually transmitted infection, and sexual risk behavior among young adults in the United States. Arch Pediatr Adolesc Med. 2009;163(7):644–652. doi: 10.1001/archpediatrics.2009.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 1998. [Google Scholar]
- Kuortti M, Kosunen E. Risk-taking behavior is more frequent in teenage girls with multiple sexual partners. Scandinavian Journal of Primary Health Care. 2009;27:47–52. doi: 10.1080/02813430802691933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latka M, Ahern J, Garfein R, et al. Prevalence, incidence, and correlates of chlamydia and gonorrhea among young adult injection drug users. Journal of Substance Abuse. 2001;13:73–88. doi: 10.1016/s0899-3289(01)00071-2. [DOI] [PubMed] [Google Scholar]
- Lamps C, Sood A, Sood R. Youth with substance abuse and comorbid mental health disorders. Curr Psychiatry Rep. 2008;10(3):265–271. doi: 10.1007/s11920-008-0043-0. [DOI] [PubMed] [Google Scholar]
- Li X, Feigelman S, Stanton B. Perceived parental monitoring and health risk behaviors among urban low-income African-American children and adolescents. Journal of Adolescent Health. 2000;27:43–48. doi: 10.1016/s1054-139x(99)00077-4. [DOI] [PubMed] [Google Scholar]
- Lillie-Blanton M, Anthony JC, Schuster CR. Probing the meaning of racial/ethnic group comparisons in crack cocaine smoking. Journal of the American Medical Association. 1993;269(8):993–997. [PubMed] [Google Scholar]
- Meschke L, Bartholomae S, Zentall S. Adolescent sexuality and parent-adolescent processes: Promoting healthy teen choices. Journal of Adolescent Health. 2002;31(6S):264–279. doi: 10.1016/s1054-139x(02)00499-8. [DOI] [PubMed] [Google Scholar]
- Metzler C, Noell J, Biglan A, Ary D, Smolkowski K. The social context for risky sexual behavior among adolescents. J Behav Med. 1994;17:419–38. doi: 10.1007/BF01858012. [DOI] [PubMed] [Google Scholar]
- Miller-Johnson S, Winn D, Coie J, Maurmary G, et al. Motherhood during the teenage years: A developmental perspective on risk factors for child-bearing. Development and Psychopathology. 1999;11:85–100. doi: 10.1017/s0954579499001960. [DOI] [PubMed] [Google Scholar]
- Mott F, Fondell M, Hu P, Kowaleski-Jones L, Menaghan E. The determinants of first sex by age 14 in a high-risk adolescent population. Family Planning Perspectives. 1996;28(1):13–18. [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. 5. Los Angeles, CA: Muthen & Muthen; 1998–2007. [Google Scholar]
- Naimi T, Brewer R, Mokdad A, Denny C, Serdula M, Marks J. Binge drinking among US adults. JAMA. 2003;289:70–75. doi: 10.1001/jama.289.1.70. [DOI] [PubMed] [Google Scholar]
- Nash S, McQueen A, Bray J. Pathways to adolescent alcohol use: Family environment, peer influence, and parental expectations. Journal of Adolescent Health. 2005;37:717–731. doi: 10.1016/j.jadohealth.2004.06.004. [DOI] [PubMed] [Google Scholar]
- Needle R, Fisher DG, Weatherby N, Chitwood D, Brown B, Cesari H, et al. Reliability of self-reported HIV risk behaviors of drug users. Psychology of Addictive Behaviors. 1995;9:242–250. [Google Scholar]
- Newman PA, Zimmerman MA. Gender differences in HIV-related risk behavior among urban African American youth: A multivariate approach. AIDS Education and Prevention. 2000;12(4):308–325. [PubMed] [Google Scholar]
- NIDA. Prevalence of Drug Use in the DC Metropolitan Area Adult and Juvenile Offender Populations: 1991. Rockville, MD: USDHHS; 1995. [Google Scholar]
- Paikoff R, Parfenoff S, Williams S, McCormick A. Parenting, parent-child relationships, and sexual possibility situations among urban African American preadolescents: preliminary findings and implications for HIV prevention. J Fam Psychol. 1997;11(1):11–22. [Google Scholar]
- Richter L, Manegold J, Pather R. Family and community interventions for children affected by AIDS. Cape Town: HSRC Press; 2004. [Google Scholar]
- Roche K, Mekos D, Alexander C, Astone N. Parenting influences on early sexual initiation among adolescents: How neighborhood matters. Journal of Family Issues. 2005;26:32–54. [Google Scholar]
- Serbin L, Karp J. The intergenerational transfer of psychosocial risk: Mediators of vulnerability and resilience. Annu Rev Psychol. 2004;55:333–363. doi: 10.1146/annurev.psych.54.101601.145228. [DOI] [PubMed] [Google Scholar]
- Seth P, Raiji P, DiClemente R, Wingood G, Rose E. Psychological distress as a correlate of a biologically confirmed STI, risky sexual practices, self-efficacy and communication with male sex partners in African-American female adolescents. Psychology, Health & Medicine. 2009;14(3):291–300. doi: 10.1080/13548500902730119. [DOI] [PubMed] [Google Scholar]
- Shaw M, Lawlor D, Najman J. Teenage children of teenage mothers: Psychological, behavioural and health outcomes from an Australian prospective longitudinal study. Social Science & Medicine. 2006;62:2526–2539. doi: 10.1016/j.socscimed.2005.10.007. [DOI] [PubMed] [Google Scholar]
- Sznitman S, Stanton BF, Vanable P, Carey MP, Valois RF, Brown L, Diclemente R, Hennessy M, Salazar LF, Romer D. Long term effects of community-based STI screening and mass media HIV prevention messages on sexual risk behaviors of African American adolescents. AIDS Behav. 2011 doi: 10.1007/s10461-011-9946–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens JW. Smart and Sassy: The Strengths of Inner-City Black Girls. New York: Oxford University Press; 2002. [Google Scholar]
- Stice E, Barrera M. A longitudinal examination of the reciprocal relations between parenting and adolescents’ substance use and externalizing behaviors. Developmental Psychology. 1995;31:322–334. [Google Scholar]
- Taylor S, Repetti R. Health psychology: What is an unhealthy environment and how does it get under the skin? Annual Review of Psychology. 1997;48:411–447. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- Teplin LA, Mericle AA, McClelland GM, Abram KM. HIV and AIDS risk behaviors in juvenile detainees: Implications for public health policy. American Journal of Public Health. 2003;93(6):906–912. doi: 10.2105/ajph.93.6.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udry J. Biological predispositions and social control in adolescent sexual behavior. American Sociological Review. 1988;53:709–722. [Google Scholar]
- Walker D, Neighbors C, Rodriquez L, Stephans R, Roffman R. Social norms and self-efficacy among heavy using adolescent marijuana smokers. Psych Addict Behav. 2011 Aug 15; doi: 10.1037/a0024958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt T, Rogers J. Factors contributing to differences in substance use among Black and White adolescents. Youth & Society. 2007;39:54–74. [Google Scholar]
- Watt T. The race/ethnic age crossover effect in drug use and heavy drinking. J of Ethnicity in Substance Abuse. 2008;7:94–114. doi: 10.1080/15332640802083303. [DOI] [PubMed] [Google Scholar]
- Watters JK. Street Youth at Risk for AIDS. Rockville, MD: National Institute on Drug Abuse; 1994. [Google Scholar]
- Wills T, Schreibman D, Benson G, Vaccaro D. Impact of parental substance use on adolescents: a test of a mediation model. J Pediatr Psychol. 1994;19:537–56. doi: 10.1093/jpepsy/19.5.537. [DOI] [PubMed] [Google Scholar]
- Windle M. Effect of parental drinking on adolescents. Alcohol Health and Research World. 1996;20:181–184. [PMC free article] [PubMed] [Google Scholar]
- Wolfe DA, Jaffe PG, Crooks CV. Adolescent Risk Behaviors: Why Teens Experiment and Strategies to Keep Them Safe. New Haven, CT: Yale University Press; 2006. [Google Scholar]