Abstract
In recent years, health inequalities have become an important public health concern and the subject of both research and policy attention in Korea. Government reports, as well as many epidemiological studies, have provided evidence that a wide range of health outcomes and health-related behaviors are socioeconomically patterned, and that the magnitude of health inequalities is even increasing. However, except for the revised Health Plan 2010 targets for health equity, few government policies have explicitly addressed health inequalities. Although a number of economic and social policies may have had an impact on health inequalities, such impact has scarcely been evaluated. In this review, we describe the current status of research and policy on health inequalities in Korea. We also suggest future challenges of approaches and policies to reduce health inequalities and highlight the active and intensive engagement of many policy sectors and good evidence for interventions that will make meaningful reduction of health inequalities possible.
Keywords: Economic Recession, Educational Status, Epidemiologic Studies, Health Policy, Income, Korea, Occupations, Poverty, Social Policy, Socioeconomic Factors
INTRODUCTION
In recent years, health inequalities have become an important public health concern internationally and the subject of both research and policy attention in South Korea (1). Government reports and epidemiological studies have reported on the socioeconomic patterns of a wide range of health outcomes, and, in fact, socioeconomic gaps in several health outcomes are increasing (2, 3). However, government policies explicitly addressing health inequalities are scant, although a number of economic and social policies may have inadvertently had a socioeconomically differentiated impact. The purpose of this review was to briefly describe the current status and future challenges in research and policy on health inequalities in Korea.
SOCIOECONOMIC CONTEXTS IN KOREA
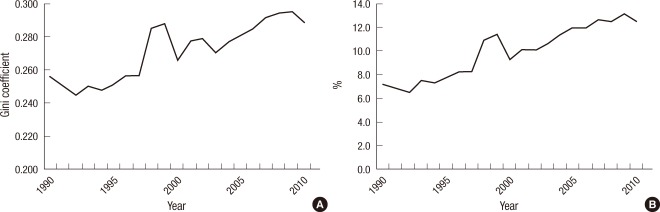
Remarkable economic growth has occurred in Korea over the past several decades. During the Korean War between 1950 and 1953, its economy could not even provide the basic needs of food and housing. At that time, Korea's per capita gross national income was less than the equivalent of US$100, but by 2010 it had surpassed US$20,000 (4). Korea joined the Organization for Economic Co-operation and Development in 1996. The World Bank called it the "miracle economy" (5). However, despite its uninterrupted economic growth for decades, the Korean economy was not immune to the economic crisis of the late 1990s, which struck many Asian countries (6). This economic crisis changed Korean society in many ways. The structural re-adjustment and the resulting economic policies heavily influenced by neo-liberalism expanded 'flexible' labor markets, which resulted in a rapid rise in the number of workers in precarious employment (6-8). While precarious workers have been experiencing job insecurity, disadvantages in wages and benefits, and social discrimination, the Korean government has provided a very limited social safety net for them (6-8). In addition, as seen in Fig. 1, the disposable income Gini coefficient, a measure of income inequality, soared during the economic crisis period and has persistently increased up to the present. Accordingly, the prevalence of relative poverty (less than 50% of median disposable income) nearly doubled between 1990 and 2010. With these sobering statistics, social polarization, social division, and social inequality became major items on the policy agenda after the late 1990s in Korea. This social divide has compelled many Korean researchers to study socioeconomic health inequalities and social determinants of health.
Fig. 1.
Trends in (A) Gini coefficient for disposable income and (B) prevalence of relative poverty (less than 50% of median disposable income) in Korea, 1990-2010. Source: Statistics Korea, Korean Statistical Information Service.
THE EXTENT OF SOCIOECONOMIC INEQUALITIES IN HEALTH IN THE PAST AND PRESENT
Despite controversy over the sampling of income data, it has often been argued that income distribution before the economic crisis was relatively equitable in Korea compared to other developed Western countries and had maintained an equitable trend since the 1970s (9, 10). Suggested contributors to this equitable trend were the history of Japanese colonial occupation and the Korean War ironically resulting in relatively equitable distribution of human and physical assets (and land reforms in 1947 and 1949), as well as export-oriented economic development since the 1960s, which provided a steadily expanding pool of job opportunities to the unemployed and the underemployed (9, 10). In a similar vein, there exists an assumption that socioeconomic inequalities in health may be a recent phenomenon related to new economic instability or the recent influx of minority ethnic groups, which, unlike in Western countries, have been a negligible proportion of the population until the past few years.
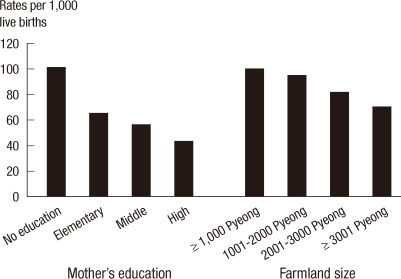
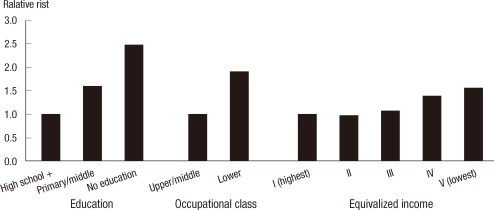
However, Fig. 2 indicates that health inequalities existed in the 1950s after the Korean War (11). This study on infant mortality employed representative random samples of Korean rural areas and found that infant mortality rates in 1954-1959 were inversely associated with maternal education and farmland size. This study is also important in that the proportion of the rural population in 1955 was 75.6% in Korea (12) and the contribution of infant mortality to life expectancy in the 1950s would be definitively greater than now. The 1970s and 1980s, when income Gini coefficients reportedly decreased (9, 10), were no exception. Using census and mortality data, Kwon (13) and Kim (14) showed educational and occupational differentials in childhood and adulthood mortality rates in the 1970s and 1980s, although these studies have limitations of numerator-denominator bias (due to the use of unlinked data) and the use of mortality data with less than optimal death certification. As shown in Fig. 3, recent data also reveal increased mortality risks among disadvantaged Korean people in terms of education, occupational class, and equivalized household income (15). After adjusting for confounders (survey year, gender, and age), the mortality risk was 2.47 times (95% confidence interval, CI: 1.61-3.77) greater for those with no education than those with a high school education or greater. Lower occupational class had a 1.92 times (95% CI: 1.21-3.04) greater risk of dying than upper and middle classes. In addition, those with the lowest income quintile had a mortality risk 1.56 times (95% CI: 1.05-2.31) greater than those with the highest income quintile and a linear relationship between income and mortality was found (P value for linear trend = 0.003). This study is of importance regarding research design because it used nationally representative mortality follow-up data and thus is free from the numerator-denominator bias of prior unlinked mortality studies.
Fig. 2.
Differences in infant mortality rates by mother's education and farmland size (1 Pyeong = 3.3 square meter) in 1955-1959 (14,325 live births and 1,187 infant deaths). Source: Adapted from reference 11.
Fig. 3.
Mortality differentials (measured by adjusted relative risks) according to education, occupational class, and equivalized household income: Mortality follow-up of 1998 and 2001 Korea National Health and Nutrition Examination Survey data. Source: Adapted from reference 15.
Here, we are not suggesting that income inequality is unimportant for health inequality. Income inequality is of crucial importance in creating health gaps between social classes. However, evidence shows that temporal and cross-national relationships between income inequality and health inequality are complex (16, 17). Redistributing income may not be enough to achieve equity in health (18-20). By presenting historical evidence of socioeconomic differentials in mortality, we indicate here that health inequalities have been persistent societal phenomena in Korea.
International comparison studies on the magnitude of health inequalities as well as studies on time trends in health inequalities would be helpful for policy agenda setting on health inequalities (21). Some Korean researchers have suggested that, based on the magnitude of mortality differentials by education and occupation found in Korean studies and Western studies, the magnitude of mortality inequalities are expected to be greater in Korea than the West (22, 23). However, a direct comparison has been rare until now. Meanwhile, there has been a surge in studies on time trends in health inequalities in Korea. Several research attempts using several rounds of nationally representative data have been made to trace the magnitude of health inequalities over recent years (2, 3, 24-28). Meanwhile, there has been a lack of studies examining longer-term trends covering the early 1980s and before.
RESEARCH: CURRENT STATUS AND FUTURE CHALLENGES
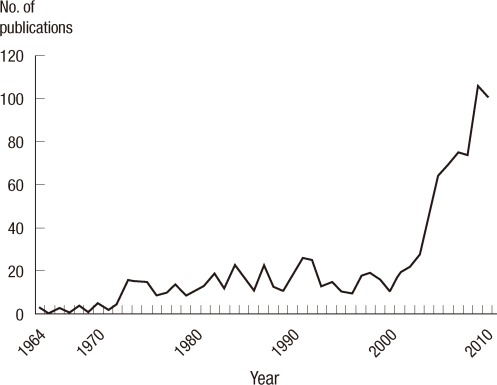
Research interests in socioeconomic inequalities in health have grown significantly over a relatively short period in Korea. As shown in Fig. 4, there has been a remarkable increase in the number of articles on health inequalities since the early 2000s, when issues on social inequalities emerged in Korea (21). This figure also suggests that research interests measured by the number of publications have lagged behind Western countries by about 10-15 yr (29). With this increasing interest in health inequalities, the Korean Society for Equity in Health (http://www.healthequity.or.kr/) was established in 2003 and has sponsored regular academic meetings and provided educational programs on monitoring health inequalities. The society published a book on the measurement of health inequalities (30). Government-funded research activities were performed (25-28, 31). Health inequality research was also conducted by governmental and non-governmental research institutes (32, 33). Monitoring health inequalities has become a key element of official government reports. For example, a recent national health report from the Korea Centers for Disease Control and Prevention included age-standardized prevalences (for dichotomous outcomes) or means (for continuous outcomes) by income quartiles and urbanity levels in a wide range of health behaviors, healthcare utilization, and chronic diseases, using four rounds of the Korean National Health and Nutrition Examination Survey (KNHANES) between 1998 and 2009 (2).
Fig. 4.
Trends in the number of publications on health inequalities in Korea: Search results in Pubmed with MESH terms being "socioeconomic factors" and "Korea".
Increased research activities on health inequalities in Korea in the past decade may be partly attributed to improved research infrastructure for the measurement of health inequality. Several national cross-sectional data sets (most importantly KNHANES) have been constructed and became publicly available. KNHANES contains socioeconomic variables such as education, occupation, employment, and household income, as well as data on a variety of health outcomes. The Korean census and mortality data contain information about education and occupation, which made unlinked mortality studies possible. In Korea, all citizens have their own unique personal identification numbers, which allows for efficient longitudinal follow-ups with nationwide secondary data such as mortality data, healthcare utilization data, and national cancer registry data (32, 34-39). In addition, many government-funded research institutes have started to establish panel data (e.g., Korea Labor and Income Panel Study, Korean Longitudinal Study of Aging, Korean Welfare Panel Study) since the late 1990s, which are now used for health inequality research (8, 40, 41).
Despite the growth in health inequality research, most of the research in this field has been devoted to describing and monitoring socioeconomic differentials in health in Korea, mostly using secondary public data. There has been a paucity of studies exploring the mechanisms of health inequalities and evaluating the interventions or policies on the magnitude of health inequalities. Primary data specifically focused on a health inequality issue (e.g., Whitehall study in the UK) have rarely been established in Korea. Although life-course approaches using information during an individual's early life and multilevel approaches including neighborhood characteristics may have the potential to reveal the structural mechanisms in creating health inequalities, such research designs have been uncommon, partly due to a lack of data on neighborhood characteristics and early life factors in the secondary data.
POLICIES: CURRENT STATUS
Many policies are likely to have had an impact on the magnitude of health inequalities. For example, Korea's national family planning campaign, which started in the 1960s with successive governmental economic development plans, might have widened social gradients in the quantity and quality of schooling, and subsequently health inequalities, because more educated and economically advantaged families participated more in the campaign and thus could provide higher per child expenditures for education (42). Historically, the marked reduction of communicable diseases associated with improvements in clean water supply and hygiene may have reduced the disease burden of the disadvantaged and contributed to the decrease in absolute inequalities in associated mortality (43). The introduction of national health insurance achieved by 1989 and subsequent insurance coverage expansion may have reduced the unmet needs of the economically disadvantaged and ultimately affected the health status of the poor, although there has understandably been a scarcity of studies examining the potential policy effects on inequalities in health outcomes rather than healthcare utilization (44). The economic crisis and associated economic and social policies may have had an impact on health inequalities (6) and recent studies have shown increasing inequalities in self-rated health (2, 27, 45), suicide (46-48), low birth weight (49), and infant mortality (28).
In the past decade, the occasional airing of health inequalities in the media based on a single study has drawn public attention. This public attention peaked when a major newspaper (Hankyoreh) of Korea, academically supported by the Korean Society for Equity in Health, published an eight part 'health inequality series' (http://www.hani.co.kr/arti/SERIES/7/) in January and February of 2006, dealing with a wide range of health inequality issues (50). A similar effort was also made recently (between December 2010 and February 2011) by a weekly magazine (Hankyoreh 21) (http://h21.hani.co.kr/arti/SERIES/62/). Although there have been several government-funded research activities on health inequalities, research findings have sometimes been ignored and are rarely publicized by the government or associated funding agencies. A national report on disparities in healthcare utilization and quality such as the US National Healthcare Disparity Report has not been made.
The most important government action on health inequality in the past decade would be that national targets for health equity have been included for the first time in the revised Health Plan 2010 by the Ministry of Health and Welfare (51). Increasing health expectancy and achieving health equity have been set as the two major goals in the revised Health Plan 2010 (51). These two major goals remained in the recent National Health Plan 2020 (52). A fundamental reason why targets for health equity have became a component in the revised Health Plan 2010 and the National Health Plan 2020 may lie in Korean society, which has experienced widening gaps in education, occupation (especially precarious employment), and income and subsequently increasing health inequalities. The US Healthy People 2010, where eradication of health disparities was included as one of the two overarching goals, has provided a good example since the revised Health Plan 2010 was partly based on the framework of the US Healthy People 2010. However, limitations should be noted (53). During the establishment process of the revised Health Plan 2010, the 'health equity' issue was exclusively dealt with in the 'health equity' section, one of 12 sections for the revised Health Plan 2010. Subsequently, specific health equity targets were only set for mortality and two health behaviors (smoking and physical exercise). In addition, explicit governmental action plans to achieve health equity were not made even in major health promotion areas (smoking, alcohol consumption, physical exercise, and nutrition) of the revised Health Plan 2010. Despite these limitations, the health equity target in the revised Health Plan 2010 had a symbolic value in raising awareness and inspiring and motivating related research and policies.
To characterize one nation's stage of diffusion of ideas on health inequalities, Margaret Whitehead (54) proposed an action spectrum on inequalities in health, which was used to evaluate policy developments in European countries (55). The spectrum covers the stages of 'measurement', 'recognition', 'awareness raising', 'concern', 'denial/indifference', 'will to take action', 'isolated initiatives', 'more structured developments', and 'comprehensive coordinated policy'. Based on policy changes that have occurred in Korea during the past decade, we can suggest that Korea is beyond the 'measurement' stage but not into the 'will to take action' stage. The Korean government has sometimes shown concern about health inequalities but has often ignored these problems. This swing in the stages of governmental position in terms of actions on health inequalities has been affected by the characteristics of the administration and its political will (the centrist administration of 2003-2008 and the conservative administration of 2008-2013), as has also been seen in European experiences in the UK and Spain (in Barcelona) (56).
FUTURE CHALLENGES FOR POLICIES TO REDUCE HEALTH INEQUALITIES
Recently, health inequalities have gained worldwide attention (1). Policy efforts are exercised at national and international levels (57, 58). However, in Korea, the most crucial policy issue regarding health inequalities today lies in how to put health inequalities policy on the government agenda. Although the presence of political will is crucial and is a function of political administration characteristics, it should be noted that initiation of the process toward governmental action on health inequalities can be facilitated by the availability of convincing data. Dutch experience provides an example that a broad consensus across political parties regarding health inequality issues could be achieved by deliberate efforts by those promoting the issue (56). Continuous monitoring of the magnitude of health inequalities and exploration of newly emerging problems (e.g., health of the minority ethnic population, the working poor, single mothers, etc.) are important. Moreover, communication on research findings among key players in agenda setting and subsequent policy processes (across media, researchers, non-governmental organizations, political parties, and government) should be further strengthened.
Policies for health equity require the development of new programs. For example, the Strategic Review of Health Inequalities in England post-2010, also known as the Marmot Review, highlighted the importance of early childhood development in reducing health inequalities (57). Early childhood development has also been supported by high profile economists, who suggested that intervention in early childhood is a rare social program free from efficiency/equity trade-off (59, 60). Some Western countries have started to recognize the importance of early childhood development in government policies (61-63). However, the Korean government has no experience in developing intensive intervention programs for early childhood (e.g., the Nurse Family Partnership program). A minimum income for healthy living (MIHL) can be a useful tool to improve the standard of living for the poor and has been suggested as a measure for health equity in the Marmot review (57). In Korea, a research effort was made to calculate the MIHL (64). However, consensus building processes for the MIHL among key players in deciding the minimum income standard as well as improved calculation and regular revision of the MIHL will be required. Precarious employment and associated health problems are emerging as an important policy agenda item (7, 8). Alternative labor market policies to provide better access and quality of jobs and intervention programs to improve the work environment need to be developed. Health impact assessment, if given an equity focus, may have an important potential to raise awareness of health inequalities among policy-makers in other policy areas. However, the institutionalization of this approach in government policy processes will be a daunting task.
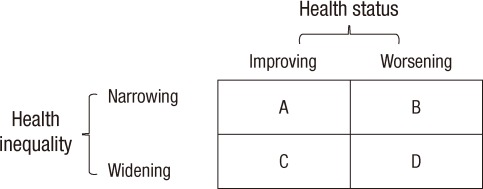
Health behavior- and health problem-oriented approaches, on which the Korean government's Health Plan has largely been based, should also be developed. Fig. 5 shows the relationship of changes in health status (mean) with changes in health inequalities (distribution) and provides information on policy priority areas (25). If the mean and inequality levels are improved and narrowed, respectively, the policy priority would be low (A in the Fig. 5). On the other hand, the policy priority will increase when those mean and inequality measures simultaneously deteriorate (D in the Fig. 5). This latter case can be found for suicide in Korea (46-48). If the mean value for a health indicator is being improved but the level of inequality widens (C in the Fig. 5, e.g., men's smoking), more specific policy measures should be directed toward disadvantaged groups of the Korean population. To be informed of the policy priority areas, it is warranted to monitor the current status and time trends of socioeconomic differentials in all indicators included in the Health Plan of Korea. Regarding equity-sensitive interventions related to health behaviors and health problems, the importance of programs for reducing socioeconomic inequalities in cigarette smoking and suicide need to be highlighted. Cigarette smoking is the most important factor among established cardiovascular risk factors in explaining relative and absolute inequalities in all-cause mortality, especially among men in Korea (65). Governmental policy efforts to reduce smoking during the past 15 yr have not succeeded in reducing socioeconomic differentials in smoking in men and women (66-69). With skyrocketing increases in average mortality rates, especially among the elderly population (48), suicide showed widening socioeconomic inequalities in Korea (46-48). Thus, interventions to decrease social gaps in suicidal deaths would also contribute to the reduction of average suicide mortality rates.
Fig. 5.
A framework for prioritizing health problems, taking into account changes in health status and health inequalities.
Reducing health inequalities is not an easy task, as recently seen in the UK, where the target for health inequalities, the 10% reduction of the gaps in life expectancy and infant mortality, was not achieved despite long-term governmental engagement with socioeconomic inequalities in health. Tackling health inequalities requires a broad response from all government departments, not just the health sector. In addition to 'upstream' policies, 'midstream' and 'downstream' policies and programs are also necessary. 'Good intention and received wisdom' is not necessarily a good guide toward health equity (70). Policies should be informed by evidence-based interventions.
CONCLUSIONS
Health inequalities are an important aspect of social injustice. Health inequalities are not only an ethical issue but also a public health problem. Reducing health inequalities should be a major objective of governmental health, social, and economic policies in Korea. The magnitude of health inequalities needs to be monitored to evaluate policies and guide the future directions of the policies. Upstream, midstream, and downstream mechanisms in the creation of health inequalities should be extensively explored to indicate entry points of policies. Intervention programs intensive enough to significantly improve the health status of the disadvantaged should be newly developed, tested, and applied. Considering the unabated trends in the social divide in Korea, active and intensive engagement of many policy sectors equipped with good evidence are needed to realize a meaningful reduction of health inequalities in the future.
References
- 1.CSDH (Commission on Social Determinants of Health) Final report of the commission on social determinants of health. Geneva: WHO; 2008. Closing the gap in a generation: health equity through action on the social determinants of health. [Google Scholar]
- 2.Ministry of Health and Welfare and Korea Centers for Disease Control and Prevention. 2009 Nation's Health Statistics: findings of Korea national health and nutrition examination survey IV-3 (2009) Seoul: Ministry of Health and Welfare and Korea Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 3.Kim YM, Kim MH. Health inequalities in Korea: current conditions and implications. J Prev Med Public Health. 2007;40:431–438. doi: 10.3961/jpmph.2007.40.6.431. [DOI] [PubMed] [Google Scholar]
- 4.Statistics Korea. Korean Statistical Information Service. [accessed on 2 May 2011]. Available at http://kosis.kr/
- 5.World Bank. The East Asian Miracle: economic growth and public policy. New York: Oxford University Press; 1993. [Google Scholar]
- 6.Khang YH, Lynch J. Asian economic crises and health: population health impacts and policy responses. J Epidemiol Community Health. 2010;64:282–283. doi: 10.1136/jech.2009.090761. [DOI] [PubMed] [Google Scholar]
- 7.Kim IH, Muntaner C, Khang YH, Paek DM, Cho SI. The relationship between nonstandard working and mental health in a representative sample of the South Korean population. Soc Sci Med. 2006;63:566–574. doi: 10.1016/j.socscimed.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Kim MH, Kim CY, Park JK, Kawachi I. Is precarious employment damaging to self-rated health? Results of propensity score matching methods, using longitudinal data in South Korea. Soc Sci Med. 2008;67:1982–1994. doi: 10.1016/j.socscimed.2008.09.051. [DOI] [PubMed] [Google Scholar]
- 9.Choo H. Economic growth and income distribution in Korea. Seoul: Korea Development Institute; 1978. [Google Scholar]
- 10.Suh SM. Economic growth and change in income distribution: the Korean case. Seoul: Korea Development Institute; 1985. [Google Scholar]
- 11.Park HJ. A study on infant deaths in Korean rural area. Seoul J Med. 1962;3:41–51. [Google Scholar]
- 12.Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat. World population prospects: the 2006 revision and world urbanization prospects: the 2007 revision. [accessed on 4 May 2011]. Available at http://esa.un.org/unup.
- 13.Kwon TH. The trends and patterns of mortality and health in the Republic of Korea. Asian population studies series. No. 76. Bankok: Economic and Social Commission for Asia and the Pacific; 1986. [Google Scholar]
- 14.Kim TH. Mortality transition in Korea: 1960-1980. Seoul: Seoul National University, The Population and Development Studies Center; 1990. [Google Scholar]
- 15.Khang YH, Lynch JW, Harper S, Yang S, Yun SC, Jung-Choi K, Kim HR. The contribution of material, psychosocial, and behavioral factors to explain educational and occupational mortality inequalities in a nationally representative sample of South Koreans: relative and absolute perspectives. Soc Sci Med. 2009;68:858–866. doi: 10.1016/j.socscimed.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 16.Mackenbach JP, Stirbu I, Roskam AJ, Schaap MM, Menvielle G, Leinsalu M, Kunst AE European Union Working Group on Socioeconomic Inequalities in Health. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358:2468–2481. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 17.Regidor E, Ronda E, Pascual C, Martínez D, Calle ME, Domínguez V. Decreasing socioeconomic inequalities and increasing health inequalities in Spain: a case study. Am J Public Health. 2006;96:102–108. doi: 10.2105/AJPH.2004.053983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blakely T, Wilson N. Shifting dollars, saving lives: What might happen to mortality rates, and socio-economic inequalities in mortality rates, if income was redistributed. Soc Sci Med. 2006;62:2024–2034. doi: 10.1016/j.socscimed.2005.08.059. [DOI] [PubMed] [Google Scholar]
- 19.Deaton A. Policy implications of the gradient of health and wealth. Health Aff (Millwood) 2002;21:13–30. doi: 10.1377/hlthaff.21.2.13. [DOI] [PubMed] [Google Scholar]
- 20.Starfield B, Birn AE. Income redistribution is not enough: income inequality, social welfare programs, and achieving equity in health. J Epidemiol Community Health. 2007;61:1038–1041. doi: 10.1136/jech.2006.054627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khang YH. Historical advances in health inequality research. J Prev Med Public Health. 2007;40:422–430. doi: 10.3961/jpmph.2007.40.6.422. [DOI] [PubMed] [Google Scholar]
- 22.Khang YH. Lifecourse approaches to socioeconomic health inequalities. J Prev Med Public Health. 2005;38:267–275. [PubMed] [Google Scholar]
- 23.Son M. Commentary: why the educational effect is so strong in differentials of mortality in Korea? Int J Epidemiol. 2004;33:308–310. doi: 10.1093/ije/dyh017. [DOI] [PubMed] [Google Scholar]
- 24.Jung-Choi KH. Contribution of causes of death to socioeconomic mortality inequalities: current status and time trends in Korea [dissertation] Seoul: University of Ulsan; 2008. [Google Scholar]
- 25.Khang YH, Kang MA, Kim MH, Kim YM, Shin YJ, Yoo WS, Yoon TH, Jang SN, Jeong BG, Jungchoi KH, Cho SI, Cho HJ, Choi YE, Choi YJ, Heo SI. Developing indicators of equity in health and monitoring magnitude of socioeconomic inequalities in health. Seoul: University of Ulsan & Management Center for Health Promotion; 2006. [Google Scholar]
- 26.Kwon SM, Son M, Lee EJ, Cho SI, Cho YT, Ku MJ, Kim YH, Oh J, Chung HJ. Developing performance indicators of equity in health. Seoul: Seoul National University & Management Center for Health Promotion; 2006. [Google Scholar]
- 27.Shin YJ, Kim MH, Yoon TH. Health promotion strategies and programmes development for health inequalities alleviation. Seoul: Hanyang University & Management Center for Health Promotion; 2009. [Google Scholar]
- 28.Son M, Kim SJ, Lee JH, Kim JO, Bae SH, Oh JH, Hwang SS, Kim YJ, Jung SM, Lee WJ, Lee SY, Park JH, Park JH, Lim DO, Park IS, Yoon CK. Reducing inequalities in cancer incidence and mortality: developing epidemiologic health inequality index and health policy in Korea. Seoul: Kangwon National University & Ministry of Health and Welfare; 2008. [Google Scholar]
- 29.Kaplan GA, Lynch JW. Whither studies on the socioeconomic foundations of population health? Am J Public Health. 1997;87:1409–1411. doi: 10.2105/ajph.87.9.1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The Korean Society for Equity in Health. Methods in health inequalities measurement. Seoul: Hanul Publishing Group; 2007. [Google Scholar]
- 31.Lee SY, Kim SY, Kim CW, Park HK, Yoon TH, Kim JH. Inequality on medical service utilization among stroke patients across income groups. Seoul: Cheju National University & Management Center for Health Promotion; 2007. [Google Scholar]
- 32.Kim HR, Khang YH, Yoon KJ, Kim CS. Socioeconomic health inequalities and counter policies in Korea. Seoul: Korea Institute for Health and Social Affairs; 2004. [Google Scholar]
- 33.Kim MH, Seo JH, Son JI, Cho HJ, Choi YJ. Anti-smoking policies and health inequalities in Korea. Seoul: People's Health Institute; 2004. PHI health equity report 2010. [Google Scholar]
- 34.Cho HJ. Mortality differentials of government officers and private school teachers by social stratification in Korea [dissertation] Seoul: Seoul National University; 1997. [Google Scholar]
- 35.Kim CW, Lee SY, Moon OR. Inequalities in cancer incidence and mortality across income groups and policy implications in South Korea. Public Health. 2008;122:229–236. doi: 10.1016/j.puhe.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 36.Kim HR, Khang YH, Park EJ, Choi JS, Lee YH, Kim YS. Socioeconomic, behavioral, nutritional, and biological determinants of morbidity, mortality, and medical utilization in South Korea. Seoul: Korea Institute for Health and Welfare; 2006. [Google Scholar]
- 37.Song YM, Ferrer RL, Cho SI, Sung J, Ebrahim S, Davey Smith G. Socioeconomic status and cardiovascular disease among men: the Korean national health service prospective cohort study. Am J Public Health. 2006;96:152–159. doi: 10.2105/AJPH.2005.061853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yim J, Hwang SS, Yoo KY, Kim CY. Contribution of income-related inequality and healthcare utilisation to survival in cancers of the lung, liver, stomach and colon. J Epidemiol Community Health. 2012;66:37–40. doi: 10.1136/jech.2009.104554. [DOI] [PubMed] [Google Scholar]
- 39.Yoon TH, Lee SY, Kim CW, Kim SY, Jeong BG, Park HK. Inequalities in medical care utilization by South Korean cancer patients according to income: a retrospective cohort study. Int J Health Serv. 2011;41:51–66. doi: 10.2190/HS.41.1.d. [DOI] [PubMed] [Google Scholar]
- 40.Jang SN, Cho SI, Chang J, Boo K, Shin HG, Lee H, Berkman LF. Employment status and depressive symptoms in Koreans: results from a baseline survey of the Korean Longitudinal Study of Aging. J Gerontol B Psychol Sci Soc Sci. 2009;64:677–683. doi: 10.1093/geronb/gbp014. [DOI] [PubMed] [Google Scholar]
- 41.Seo JH, Kim H, Shin YJ. Analysis for the impact of adulthood and childhood socioeconomic positions and intergenerational social mobility on adulthood health. J Prev Med Public Health. 2010;43:138–150. doi: 10.3961/jpmph.2010.43.2.138. [DOI] [PubMed] [Google Scholar]
- 42.Khang YH, Lynch JW, Kaplan GA. Health inequalities in Korea: age- and sex-specific educational differences in the 10 leading causes of death. Int J Epidemiol. 2004;33:299–308. doi: 10.1093/ije/dyg244. [DOI] [PubMed] [Google Scholar]
- 43.Yang S, Khang YH, Harper S, Davey Smith G, Leon D, Lynch J. Understanding rapid increase in life expectancy in Korea. Am J Public Health. 2010;100:896–903. doi: 10.2105/AJPH.2009.160341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bae JY. Impacts of health insurance coverage expansion on healthcare utilization and health status [dissertation] Seoul: Seoul National University; 2009. [Google Scholar]
- 45.Khang YH, Lynch JW, Yun S, Lee SI. Trends in socioeconomic health inequalities in Korea: use of mortality and morbidity measures. J Epidemiol Community Health. 2004;58:308–314. doi: 10.1136/jech.2003.012989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee WY, Khang YH, Noh M, Ryu JI, Son M, Hong YP. Trends in educational differentials in suicide mortality beforebetween 1993-2006 in Korea. Yonsei Med J. 2009;50:482–492. doi: 10.3349/ymj.2009.50.4.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Khang YH, Hwang IA, Yun SC, Jo MW, Lee MJ, Lee MS, Lee SI. Changes in mortality inequality in relation to the South Korea economic crisis: use of area-based socioeconomic position. J Prev Med Public Health. 2005;38:359–365. [PubMed] [Google Scholar]
- 48.Kim MH, Jung-Choi K, Jun HJ, Kawachi I. Socioeconomic inequalities in suicidal ideation, parasuicides, and completed suicides in South Korea. Soc Sci Med. 2010;70:1254–1261. doi: 10.1016/j.socscimed.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 49.Son M. The effects of the parents' social class on the low birthweight among the births, 1995-2001. Korean J Health Policy Adm. 2004;14:148–168. [Google Scholar]
- 50.Lee CG. Reports for agenda setting. Seoul: Mim Books; 2007. Tracking health inequalities in Korea. [Google Scholar]
- 51.Ministry of Health and Welfare and Korea Institute for Health and Social Affairs. Establish of new health plan 2010. Seoul: Ministry of Health and Welfare and Korea Institute for Health and Social Affairs; 2005. pp. 42–46.pp. 883 [Google Scholar]
- 52.Ministry of Health and Welfare. The national health plan 2020. Seoul: Ministry of Health and Welfare; 2011. [Google Scholar]
- 53.Yoon TH. The proposal of policies aimed at tackling health inequalities in Korea. J Prev Med Public Health. 2007;40:447–453. doi: 10.3961/jpmph.2007.40.6.447. [DOI] [PubMed] [Google Scholar]
- 54.Whitehead M. Diffusion of ideas on social inequalities in health: a European perspective. Milbank Q. 1998;76:469–492. 306. doi: 10.1111/1468-0009.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mackenbach JP, Bakker MJ European Network on Interventions and Policies to Reduce Inequalities in Health. Tackling socioeconomic inequalities in health: analysis of European experiences. Lancet. 2003;362:1409–1414. doi: 10.1016/S0140-6736(03)14639-9. [DOI] [PubMed] [Google Scholar]
- 56.Mackenbach JP, Bakker M, editors. Reducing inequalities in health. A European perspective. London: Routledge; 2002. [Google Scholar]
- 57.The Marmot Review. Fair society, healthy lives. London: UK Department of Health; 2010. [Google Scholar]
- 58.European Review on the Social Determinants of Health and the Health Divide. [accessed on 11 May 2011]. Available at http://www.marmotreview.org/european-review-of-hi/description.aspx.
- 59.Heckman JJ. Skill formation and the economics of investing in disadvantaged children. Science. 2006;312:1900–1902. doi: 10.1126/science.1128898. [DOI] [PubMed] [Google Scholar]
- 60.Cunha F, Heckman JJ. The economics and psychology of inequality and human development. J Eur Econ Assoc. 2009;7:320–364. doi: 10.1162/jeea.2009.7.2-3.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.UK Department of Education. Every child matters. London: UK Department of Education; 2003. [Google Scholar]
- 62.UK Department of Children, Schools, and Families and UK Department of Health. Healthy lives, brighter futures. London: UK Department of Children, Schools, and Families and UK Department of Health; 2009. [Google Scholar]
- 63.Australian Government. Investing in the early years: a national early childhood development strategy. An initiative of the council of Australian governments. ACT, Australia: Australian Government; 2009. [Google Scholar]
- 64.Kim MH, Kim IA, Park YJ, Park JW, Son JI, Lee SI, Jung MS. A report on the calculation of the minimum income for hHealthy living in Korea. [accessed on 11 May 2011]. Available at http://www.healthequity.or.kr/
- 65.Khang YH, Lynch JW, Jung-Choi KH, Cho HJ. Explaining age specific inequalities in mortality from all causes, cardiovascular disease and ischaemic heart disease among South Korean male public servants: relative and absolute perspectives. Heart. 2008;94:75–82. doi: 10.1136/hrt.2007.117747. [DOI] [PubMed] [Google Scholar]
- 66.Cho HJ, Song YM, Smith GD, Ebrahim S. Trends in socio-economic differentials in cigarette smoking behaviour between 1990 and 1998: a large prospective study in Korean men. Public Health. 2004;118:553–558. doi: 10.1016/j.puhe.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 67.Khang YH, Cho HJ. Socioeconomic inequality in cigarette smoking: trends by gender, age, and socioeconomic position in South Korea, 1989-2003. Prev Med. 2006;42:415–422. doi: 10.1016/j.ypmed.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 68.Khang YH, Yun SC, Jung-Choi K, Cho HJ. The impact of governmental anti-smoking policy on socioeconomic disparities in cigarette smoking in South Korea. Nicotine Tob Res. 2009;11:262–269. doi: 10.1093/ntr/ntn036. [DOI] [PubMed] [Google Scholar]
- 69.Kim HR. Socioeconomic inequality and its trends in cigarette smoking in South Korea, 1998-2005. Health Soc Welf Rev. 2007;27:25–43. [Google Scholar]
- 70.Macintyre S. Good intentions and received wisdom are not good enough: the need for controlled trials in public health. J Epidemiol Community Health. 2010;65:564–567. doi: 10.1136/jech.2010.124198. [DOI] [PubMed] [Google Scholar]