Abstract
Owing to striking features of numerous multinucleated cells and bone destruction, giant cell tumor (GCT) of bone, often called as osteoclastoma, has drawn major attractions from orthopaedic surgeons, pathologists, and radiologists. The name GCT or osteoclastoma gives a false impression of a tumor comprising of proliferating osteoclasts or osteoclast precursors. The underlying mechanisms for excessive osteoclastogenesis are intriguing and GCT has served as an exciting disease model representing a paradigm of osteoclastogenesis for bone biologists. The modern interpretation of GCT is predominantly osteoclastogenic stromal cell tumors of mesenchymal origin. A diverse array of inflammatory cytokines and chemokines disrupts osteoblastic differentiation and promotes the formation of excessive multi-nucleated osteoclastic cells. Pro-osteoclastogenic cytokines such as receptor activator of nuclear factor kappa-B ligand (RANKL), interleukin (IL)-6, and tumor necrosis factor (TNF) as well as monocyte-recruiting chemokines such as stromal cell-derived factor-1 (SDF-1) and monocyte chemoattractant protein (MCP)-1 participate in unfavorable osteoclastogenesis and bone destruction. This model represents a self-sufficient osteoclastogenic paracrine loop in a localized area. Consistent with this paradigm, a recombinant RANK-Fc protein and bisphosphonates are currently being tried for GCT treatment in addition to surgical excision and conventional topical adjuvant therapies.
Keywords: Bone tumor, Giant cell tumor, Osteoclast
Giant cell tumor (GCT) of bone has occupied a central stage in musculoskeletal tumor practice because of its relatively common incidence, striking features of giant cell formation, severe destruction of bone (osteolysis), diverse but controversial topical adjuvant therapeutic options, and preponderance for local recurrences. GCT has oft en been referred to as osteoclastoma due to its unusually high population of multi-nucleated giant cells.1,2) The terms GCT and osteoclastoma have given the impression of giant cells as being the major neoplastic component of the lesion. Many new pathophysiologic concepts have emerged since the discovery of a new paradigm of osteoclastogenesis in 1997; it is time to revisit the pathophysiology of GCT to develop new mechanism-based treatments. This article highlights a molecular pathophysiologic aspect of GCT that is characterized by proliferation of mesenchymal stromal osteoprogenitor cells that effectively initiate and maintain predominant osteoclastogenesis instead of differentiating into osteoblasts and osteocytes. Based on the modern interpretation of pathophysiology, GCT is a predominantly osteoclastogenic stromal tumor (POST) of bone.
HISTORICAL PERSPECTIVE
The neoplasm known as the GCT has had multiple classifications as researchers and clinicians refine the understanding of its presentation and pathophysiology.
In 1983, McCarthy3) wrote an elegant review article tracing the history of GCT starting from Boyer's classification in 1805 of osteosarcoma and "spina ventosa", hemorrhagic cystic dilation of the bone, as the two main forms of bone tumor. From 1818 to the early 1950's, most of the literature on GCT illuminated clinical, radiological, and morphological aspects as well as its histopathology. In what would come to be known as a giant-cell tumor, Astley Cooper described an expansive lesion of the fibular head through the first gross pathological drawings of GCT. He named the lesion "fungus medullary exostosis" and until the advent of the clinical use of microscopes in 1845, this categorization of bone tumors prevailed.
Par H. Lebert described the first microscopic observations of multinucleated giant cells and fusiform cells as 'tumeur fiblastique' in 1845. About a decade later, Sir James Paget provided the first description of the tumor in English literature in 1854. He described myeloid tumors of bone containing giant cells and showed illustrations of spindle cells and multi-nucleated giant cells based on gross and microscopic examination. As X-ray came into widespread use around the early 1900's, it provided a valuable aid to managing and diagnosing the tumor. Bloodgood,4) a surgeon at Johns Hopkins University, was credited with coining the term "giant-cell tumor" in his publication on radiographic features, conservative treatment, and use of bone grafts. While Bloodgood focused on mainly radiographic features to examine GCTs, Jaffe and Lichtenstein5) described the clinical-radiographic-histologic identity of GCT in 1940. Prior to Jaffe's radiographic description of GCT, the term osteoclast sarcoma was proposed in the 1920s to denote the most differentiated member of the GCT cellular composition. As studies were shown to support the assertion that the lesion is benign,6) the term sarcoma was dropped to yield the name osteoclastoma.
In an effort to reduce the risk of recurrence, many local adjuvant therapies such as liquid nitrogen or phenol were proposed between the 1950's and 1970's.7,8) Between the early 1980's and late 1990's, advances in understanding pathologic cellular biology provided additional insights into GCT pathophysiology. Since the discovery of key signaling molecules governing the osteoclast formation in 1997, recent studies have highlighted the interactions between osteoprogenitor cells and monocytes/macrophages. The name 'giant cell tumor' gives an unintended impression that the giant cells are the major neoplastic components of the tumor. Based on current cellular and molecular evidence, GCT stromal cells are the major neoplastic or disease components. Resorptive giant cells are the byproducts of interactions between GCT stromal cells and recruited monocytes which subsequently fuse to form tumor osteoclasts.9)
PATHOLOGY AND PATHOPHYSIOLOGY
GCTs have been well studied in radiologic and histologic arenas; but the pathogenicity remains elusive. According to Dahlin's bone tumors, GCT is a distinctive neoplasm of undifferentiated cells. The multinucleated giant cells apparently result from fusion of the proliferating mononuclear cells, and although they are a constant and prominent part of these tumors, "The giant cells are probably of less significance than the mononuclear cells. The basic proliferating cell has a round-to-oval or even spindle-shaped nucleus in the field that is a diagnostic of true GCT."10) More recent descriptions further distinguish mononuclear cells into monocytes and mesenchymal stromal cells.9,11) Cellular markers for monocytes such as CD14 are positive in mononuclear cells around the blood vessels.9,12,13) Multinucleated giant cells are positively stained with CD45, which indicates monocyte/macrophage origin. There are also numerous cells which are stained for receptor activator of nuclear factor kappa-B ligand (RANKL) and stromal cell-derived factor (SDF)-1.9)
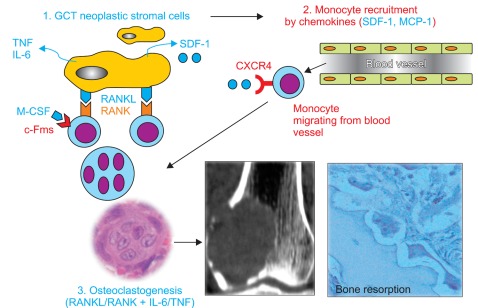
The GCT stromal cells are now widely understood to be the major neoplastic and proliferative component of GCTs.2,14) This supposition is supported by the observation that only stromal cells remain and flourish in GCT tissue subcultures. Furthermore, GCT stromal cells oft en make osteoids, suggesting their potential to differentiate into osteoblastic cells. GCT stromal cells also exhibit many chemotactic factors which are invaluable in recruiting monocytic cells and the resulting fusion into resorptive giant-cells. Stromal cells in GCT secrete various chemokines including monocyte chemoattractant protein (MCP)-1 and SDF-1, which attract blood monocytes and stimulate their migration into tumor tissues (Table 1). These monocytes ultimately fuse to form osteoclast-like, multinucleated giant cells (Fig. 1). The monocytes express receptor activator of nuclear factor kappa (RANK) receptor and GCT stromal cells express RANKL which are essential for mature osteoclast differentiation and activation with a cofactor macrophage colony-stimulating factor (M-CSF). Osteoclasts-like multinucleated giant cells are able to resorb the bone, leading to osteolysis.
Table 1.
Pathophysiology: Cytokines and Chemokines Associated with Giant-Cell Tumor
IL: interleukin, MMP: matrix metalloproteinase, TNF: tumor necrosis factor, GCT: giant cell tumor, M-CSF: macrophage colony-stimulating factor, ODF: osteoclast differentiation factor, RANKL: receptor activator of nuclear factor kappa-B ligand, TRANCE: tumor necrosis factor-related activation-induced cytokine, RANK: receptor activator of nuclear factor kappa, MCP: monocyte chemoattractant protein, TGF-β: transforming growth factor-beta, SDF: stromal cell-derived factor.
Fig. 1.
Osteoclastogenesis by giant-cell tumor is constituted of stromal cells (GCTSCs). A diagram representing pathophysiology of osteoclast-rich giant-cell tumor (GCT). A neoplastic component of GCT is mainly dysfunctional stromal cells. Mesenchymal stromal cell markers such as STRO-1 and SDF-1α are positive. Stromal cells produce sufficient chemokines and cytokines which recruit CXCR4 (+) osteoclast precursors from blood vessels and promote osteoclastogenesis. SDF: stromal cell-derived factor, MCP: monocyte chemoattractant protein, TNF: tumor necrosis factor, IL: interleukin, RANKL: receptor activator of nuclear factor kappa-B ligand, RANK: receptor activator of nuclear factor kappa, M-CSF: macrophage colony-stimulating factor.
Recent advances in understanding key osteoclastogenic factors have shed light on the resorptive aspects of GCT.15,16) Analysis of gene expression in GCT samples along with cytokine and chemokine studies are beginning to clarify some of the origins and actions of GCT components. As extensively identified by histological analysis, the major cellular components of the GCT is constituted of stromal cells (GCTSC), mononuclear monocyte cells (MNMC), and multinucleated giant-cells (MNGC).17) The stromal cells are the main neoplastic component of GCTs and while they are not directly responsible for resorptive activity, they have been shown to express and secrete a variety of chemotactic factors to enlist pathologic components.2) MNMCs are considered to be either reactive macrophages or osteoclast precursors. The main reactive components of GCTs are the multinucleated giant-cells which mimic osteoclasts. This is supported by the comparison between the cellular factors associated with osteoclasts to GCT samples.
Osteoclasts develop from hematopoietic cells of the monocyte/macrophage lineage, whereas multinucleated giant cells are thought to be formed from blood monocytes through tumor-induced cell fusion. The MNGC in GCT resemble many of the qualities of osteoclasts including the expression of monocyte/macrophage markers like CD68, titrate-resistant acid phosphatase (TRAP), cathepsin K, matrix metalloproteinase (MMP)-9, and vitronectin receptors.5)
CYTOKINES AND CHEMOKINES
The cellular environment of GCT is rich with cytokines and chemokines, i.e., cytokines with chemoattractive properties (Fig. 1). Due to recent studies of GCT-associated chemokines, the role that GCTSC initiate monocyte recruitment and giant-cell fusion is becoming clearer. mRNA analysis of GCTSCs illustrated the encoding of numerous osteoclastogenic cytokines and chemokines such as interleukin (IL)-6, IL-11, IL-17 as well as parathyroid hormone-related protein (PTHrP) and transforming growth factor-beta (TGF-β).15) TGF-β1 is commonly produced by the bone and is known as a potent chemotactic agent for monocytes and macrophages. Furthermore, TGF-β type II receptor has been shown to be expressed in osteoclast-like GCT cells, thereby highlighting the role that stromal cells have in the fusion of multinucleated giant-cells.18) TGF-β may also play a role in the expression of other cytokines found in GCT samples such as tumor necrosis factor (TNF)-α, interferon (IFN)-γ, and IL-1 since TGF-β has been shown to upregulate these cytokines in other cells.
The recruitment of monocytes and osteoclast precursors by GCTSC is strengthened by the migration of CD14-monocytes, CD68+ macrophages, and CD34+ hematopoietic stem cells to GCT-conditioned media, which contains chemotactic concentrations of SDF-1.9) This illustrates a strong involvement of GCTSC in the recruitment of osteoclast precursor cells for pathologic osteoclastogenesis.19,20)
The discovery and subsequent exploration into the osteoclast differentiation factor (ODF)/RANKL/tumor necrosis factor-related activation-induced cytokine (TRANCE) osteoclastogenic cytokine in GCT samples has led to considerable gains in the knowledge of fusion of monocytes. RANKL and M-CSF are widely known to be unequivocally required cytokines in normal osteoclastogenesis.21,22) RANKL is a member of the TNF family, and is expressed by many cell types - including stromal cells.23) Many studies confirmed RANKL to be highly expressed in GCTSC.19,24-26) The monocytes recruited in GCTs express the RANK receptor and thus can take advantage of this neoplastic osteoclastogenic pathway. Studies performed by Atkins et al. revealed that neoplastic stromal cells of GCTs share phenotypic traits such as cytokine and gene expression to osteoblasts.15,19,26) This suggests a neoplastic paradigm of the physiological osteoblast-osteoclast structure involving GCT stromal cells and monocytes.
The expression of IL-1 by the osteoclastic cells of GCTs account for the increased activity of MMP-9, which is an osteoclast bone matrix resorptive enzyme. Furthermore, IL-1 is linked to the metastatic activity of GCT since it has been correlated with increased vascular and lung invasion.2) The locally aggressive osteolytic activity that giant-cells exhibit is further explained by the expression of other matrix metalloproteinases such as type IV collagenase (MMP-2).27-29)
IL-6 overexpression in GCT samples is yet another factor that is implicated in multi-nucleated giant cell formation.30) Due to this overexpression, c-Jun is activated in GCTSCs which leads to the inhibition of osteoblastic differentiation of these stromal cells and enhanced oncogenesis of GCT by acting as a proto-oncogene.31) IL-6 is involved in the regulation of bone resorptive activity by giant-cells in GCTs and other giant-cell lesions. IL-6 neutralizing antibodies have also been able to reduce resorption in a dose dependent manner.30) Cell-cycle regulators such as IL-6 and similar proteins provide a channel to understanding pathogenic processes such as GCT with strong implications on therapeutic development.
Cytogenetic Findings
Along with cytokine and chemokine analysis, differential gene expression in GCT samples can yield relevant insights into the pathophysiology of this neoplasm, which can be used in the exploration of treatment options. Babeto et al.32) used rapid subtractive hybridization (RaSH) to identify genes like kinectin, Rho-associated coil containing protein kinase 1, and sterile alpha motif and leucine zipper containing kinase (KTN1, ROCK1, and ZAK) which were differentially expressed in GCT when compared to normal bone samples. KTN1, which encodes kinectin, a membrane receptor involved in the transport of vesicles along microtubules, is highly expressed in GCT cells. ROCK1 is upregulated in GCT cells and encodes proteins associated with Rho kinase which are involved in cellular functions such as regulation of cell migration, gene expression and apoptosis as well as reorganization of the actin cytoskeleton. Thus ROCK1 upregulation could play a role in the metastatic potential of GCTs.32) Alternatively, ZAK stops the cell cycle in the G2 phase. The low expression of this gene leads to a halt in proliferation and support for a larger growth of giant-cell lesions in GCTs.
Metastatic Potential
Although GCTs are classified as benign, with aggressively destructive local activity, they exhibit possible metastatic potential upon recurrence.33-36) In up to 3% of the cases,35) GCTs have been reported to metastasize to pulmonary tissue.33,35,37,38) Other possible yet exceedingly rare metastatic locations for GCT to arise is in the breast tissue.39) These metastasized tumors present a challenge in treatment as they can arise in surgically unsuitable locations and have higher rates of recurrence. Based on a longitudinal review of cases, local recurrence in metastasized GCTs was found to be near 63%.40) This suggests that the metastasized forms of the tumor might be more aggressive.
Modern experimentations such as proteomic screening can help us identify the metastatic potential and elucidate the mechanism of GCT pathology. Comparative proteomics analysis had led to the identification of biomarkers possibly involved in recurrence and metastasis. Certain factors in primary tumors such as glutathione peroxidase 1 are strongly related to metastasis.41) The use of cutting edge scientific methods to uncover the pathophysiological scheme of GCT will be essential in the discovery of new and more effective treatment options.
TREATMENTS
Surgical Treatment
Prior to the advancement of new technology and development of novel surgical techniques, GCT of the bone were treated by amputations of the body extremities.3) This technique commonly left the patient with emotional and physical distress due to functional limitations. After Volkman developed curettage, a technique of scooping out tissues, Mikulicz successfully used this technique to treat patients with GCTs without the need of amputations.3) Furthermore, the development of newer technologies led to creation of surgical drills such as high speed burr, which facilitated the removal of tumors with higher efficiency.42) In 1969, Marcove and Miller43) introduced a new adjuvant technique of tumor removal known as cryosurgery where liquid nitrogen is utilized to freeze the tumor cells, which is subsequently thawed. This process is repeated multiple times to cause the necrosis of pathogenic cells. Although cryosurgery has been shown to be a method of efficient tumor removal, the possibility of other complications has been noted, including the possibility of bone fracture and skin necrosis.44) In some cases, the tumor may be too large to be removed by curettage. In these situations, wide resection, a more aggressive surgical treatment, may be necessary to remove the tumor completely.45)
In order to reconstruct bone defects after the removal of the tumor, bone grafting has been used.3) Synthetic grafts such as polymethylmethacrylate (PMMA) have improved patient recovery and tumor removal due to the graft's exothermic reaction that causes thermal necrosis of cells and innate inflammatory reaction.45,46) Currently, all of these surgical techniques and graft s are commonly used to treat GCTs,47) yet the possibility of recurrence of the tumor still remains an issue in not only within the bone, but also in the surrounding soft tissues.48) To further reduce the rate of recurrence, many surgeons are combining surgical treatment with other adjuvant therapies.
Recurrence
The recurrence of GCTs remains a hot topic in the field of musculoskeletal tumors and the best treatment for these tumors remain controversial. Certain surgical procedures such as wide-excision and intralesional procedures along with the use of adjuvant therapies like PMMA, phenol, and local chemical application all affect the rate of recurrence. In a study of 384 procedures, the highest rate of recurrence was observed to be from 35 to 49% in intralesional procedures without the use of adjuvants.49,50) However, there was a dramatic decrease in recurrence with PMMA, PMMA with phenol, and phenol with other chemical adjuvants at 22%, 27% and 15%, respectively.49) Similar results were reported by Klenke et al.50) in their retrospective study of 46 patients. The use of PMMA with intralesional curettage lowers the recurrence rate from the average of 32% to 14%. The recurrence rates seen for wide resection are near 5-6%,50,51) but they entail considerable loss of function. In another series, Klenke et al.51) reported on the recurrence rates of GCT in 118 patients treated with wide resection and intralesional curettage and the rates are 5% and 25%, respectively. However, they suggested the use of curettage with PMMA, since this procedure lowers the recurrence rate and it provides equivalent tumor control compared to resection.50,51) In a multicentric retrospective Canadian sarcoma study, 186 patients with GCT were followed for an average of 5 years.52) The authors found the recurrence rates of GCT are 18% after intralesional curettage with the combination of adjuvants and 16% after resection. In contrast, Algawahmed et al.53) suggested that surgical adjuvants are not required since the data from 387 patients did not show significant difference in the recurrence rate compared to the control with the use of the toxic adjuvants in addition to high-speed burring.
Pathologic fracture through GCT is considered to be a risk factor of recurrence and poor functional outcome. The 5-year recurrence free survival rates is reported 82.6% with fracture and 77.9% without fracture. However, the functional outcome is similar in both groups and arthrofibrosis is more common in GCT group with fracture.54)
The tenacious nature of GCT recurrence has led to the rise of adjuvant therapies in surgical treatment. The use of bisphosphonates has been shown to yield lower recurrence rates in a dose dependent manner in vitro.11) Innovations in adjuvant therapy gained from a better understanding of the molecular mechanisms of pathologic bone-resorption and neoplastic activity can be utilized to halt the incidence of recurrence of GCT.
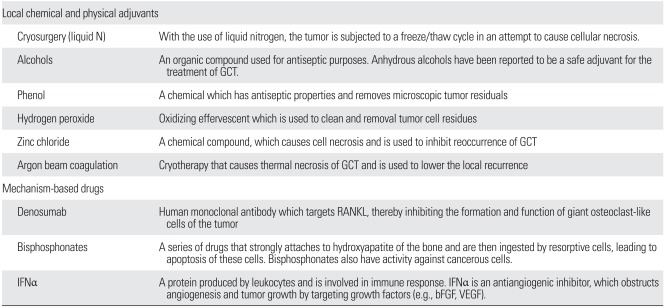
Adjuvant Therapy (Table 2)
Table 2.
Adjuvant Therapies for GCT
GCT: giant cell tumor, RANKL: receptor activator of nuclear factor kappa-B ligand, IFNα: interferon alpha, bFGF: basic fibroblast growth factor, VEGF: vascular endothelial growth factor.
Chemical adjuvant therapy
To decrease the incidence of recurrence in patients, multiple adjuvant therapies have been proposed and applied for the treatment of GCT. Application of chemical adjuvants such as alcohols, phenol, hydrogen peroxide, and zinc chloride to the affected area has been shown to dramatically reduce the rate of tumor recurrence in many cases.7) Alcohols have been used for decades in surgeries for antiseptic purposes, and it has been used as a safe adjuvant for the treatment of GCTs.7,46,55) Ever since 1980, phenol has been used commonly as a local adjuvant for the GCT.1,7) Although some studies have highlighted the efficacy of phenol as a local adjuvant for treating GCT,7,56) others have revealed no significant difference in the recurrence rate of phenol treated versus non-phenol treated patients. Therefore, it was concluded that the success of tumor removal by surgery is a greater factor for determining the possibility of recurrence rather than the use of phenol.57) Hydrogen peroxide has also been shown to affect GCT cells in vitro1,58) and in patient studies.59) Though hydrogen peroxide has been recommended for GCT treatment due to its short-life,7) this adjuvant has also been shown to increase the penetration of phenol though the tissues, causing some chemical burns.59) Thus, great care is needed when using these chemicals for GCT therapy. In addition to these chemicals, zinc chloride is another cytotoxic chemical which was supported for its use as an adjuvant for GCT treatment by Bloodgood4) and have been used for treating patients with GCT.44) In addition, Argon laser beam coagulation is an adjuvant treatment option for GCT which causes thermal necrosis and is associated with a low rate of local recurrence of GCT of bone.60)
Radiation therapy
Radiation therapy for GCT was initially performed by Pfahler and Parry in 1932.3) Although there are several reports of post-radial sarcoma development,3,61,62) several studies have suggested radiation for the treatment of GCT when surgical treatments are not feasible.63-66) Radiation seems to be less popular as a modern molecular therapy targeting osteoclastogenesis emerges.
Molecular adjuvant therapy
In addition to chemical adjuvants, drugs which have specific activity at the molecular level have been shown to have anti-GCT activities. These molecular drugs include Denosumab and bisphosphonates. Several studies have revealed intricate similarities of GCT cells to the osteoclasts of bones.24,47) For instance, RANKL, an essential molecule for osteoclast differentiation in bone metabolism, was found to be highly expressed in the cells of GCT.15,24,67) This observation hinted the possible involvement of RANKL in the pathogenesis of GCT and led to the idea of using RANKL-targeting drugs, such as Denosumab, to combat against this bone tumor.68) Currently, Denosumab is in clinical trials for the treatment of GCTs.68) Additionally, the similarities observed between the giant cells of the tumor and osteoclasts of bone led scientists to test the effect of bisphosphonates (anti-osteoclastic drugs) on GCTs. The results verified the anti-GCT activities of bisphosphonates, such as pamidronate and zoledronate, in vitro11,69,70) and in patient studies.8,69,71) These studies show the possibility of using these target-specific drugs for therapeutic purposes in treating GCTs near future.
Furthermore, studies of GCT revealed expressions of several angiogenic growth factors.72) This finding led to the proposal of using IFNα as an anti-angiogenic agent for the treatment of this debilitating disease. The application of IFNα for the treatment of GCT was initially conducted in 1995 by Kaban et al.,73) in which they successfully treated a 5-year-old girl who had the tumor in the jaw. After this successful treatment, several studies have also found IFNα to be an effective treatment option for GCT patients.74,75)
CONCLUSIONS
GCT or osteoclastoma has been a hot topic in the field of musculoskeletal tumors owing its predominant presence of osteoclast-like multinucleated giant cells. The name GCT or osteoclastoma gives a false impression of a tumor comprising of proliferating osteoclasts or osteoclast precursors. The cytokine environment coupled with tumorigenic gene expression causes neoplastic GCT stromal cells to fail to differentiate into osteoblasts. Subsequently, the stromal cells induce a chain of osteoclastogenesis by recruiting osteoclast precursors and supplying key proosteoclastogenic cytokines. Current biological knowledge of osteoclastogenesis and cytokine expression of GCT leads to the contention that this neoplasm is a POST. In regards to treatments, several adjuvant therapies have been used for the treatment of GCT. However, the use of adjuvant therapies alone in GCT treatment has been shown to be insufficient for tumor riddance. With this in mind, the current option for effective removal of the tumor and avoiding recurrence may be combinatory therapy, which includes vigorous tumor removal by surgery with other adjuvant therapies. Moreover, molecular drugs, which target cellular components involved in the pathology of GCT, may help decrease the rate of recurrence. Through a more modern approach focusing on pathophysiology, a wealth of mechanism-based treatments for GCT are sure to emerge.
ACKNOWLEDGEMENTS
Research support by Orthopaedic Science and Research Foundation (OSRF), National Institute of Health (NIAMS; NIBIB) and Department of Defense (FYL).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Eckardt JJ, Grogan TJ. Giant cell tumor of bone. Clin Orthop Relat Res. 1986;(204):45–58. [PubMed] [Google Scholar]
- 2.Wulling M, Engels C, Jesse N, Werner M, Delling G, Kaiser E. The nature of giant cell tumor of bone. J Cancer Res Clin Oncol. 2001;127(8):467–474. doi: 10.1007/s004320100234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCarthy EF. Giant-cell tumor of bone: an historical perspective. Clin Orthop Relat Res. 1980;(153):14–25. [PubMed] [Google Scholar]
- 4.Bloodgood JC. II. The conservative treatment of giant-cell sarcoma, with the study of bone transplantation. Ann Surg. 1912;56(2):210–239. doi: 10.1097/00000658-191208000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaffe HL, Lichtenstein L. Benign chondroblastoma of bone: a reinterpretation of the so-called calcifying or chondromatous giant cell tumor. Am J Pathol. 1942;18(6):969–991. [PMC free article] [PubMed] [Google Scholar]
- 6.Icihikawa K, Tanino R. Soft tissue giant cell tumor of low malignant potential. Tokai J Exp Clin Med. 2004;29(3):91–95. [PubMed] [Google Scholar]
- 7.Gortzak Y, Kandel R, Deheshi B, et al. The efficacy of chemical adjuvants on giant-cell tumour of bone: an in vitro study. J Bone Joint Surg Br. 2010;92(10):1475–1479. doi: 10.1302/0301-620x.92b10.23495. [DOI] [PubMed] [Google Scholar]
- 8.Balke M, Schremper L, Gebert C, et al. Giant cell tumor of bone: treatment and outcome of 214 cases. J Cancer Res Clin Oncol. 2008;134(9):969–978. doi: 10.1007/s00432-008-0370-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liao TS, Yurgelun MB, Chang SS, et al. Recruitment of osteoclast precursors by stromal cell derived factor-1 (SDF-1) in giant cell tumor of bone. J Orthop Res. 2005;23(1):203–209. doi: 10.1016/j.orthres.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 10.Unni KK, Dahlin DC. Dahlin's bone tumors: general aspects and data on 11,087 cases. Philadelphia: Lippincott-Raven; 1996. [Google Scholar]
- 11.Chang SS, Suratwala SJ, Jung KM, et al. Bisphosphonates may reduce recurrence in giant cell tumor by inducing apoptosis. Clin Orthop Relat Res. 2004;(426):103–109. doi: 10.1097/01.blo.0000141372.54456.80. [DOI] [PubMed] [Google Scholar]
- 12.Forsyth RG, De Boeck G, Baelde JJ, et al. CD33+ CD14-phenotype is characteristic of multinuclear osteoclast-like cells in giant cell tumor of bone. J Bone Miner Res. 2009;24(1):70–77. doi: 10.1359/jbmr.080905. [DOI] [PubMed] [Google Scholar]
- 13.Miyamoto N, Higuchi Y, Tajima M, et al. Spindle-shaped cells derived from giant-cell tumor of bone support differentiation of blood monocytes to osteoclast-like cells. J Orthop Res. 2000;18(4):647–654. doi: 10.1002/jor.1100180418. [DOI] [PubMed] [Google Scholar]
- 14.Wulling M, Delling G, Kaiser E. The origin of the neoplastic stromal cell in giant cell tumor of bone. Hum Pathol. 2003;34(10):983–993. doi: 10.1053/s0046-8177(03)00413-1. [DOI] [PubMed] [Google Scholar]
- 15.Atkins GJ, Haynes DR, Graves SE, et al. Expression of osteoclast differentiation signals by stromal elements of giant cell tumors. J Bone Miner Res. 2000;15(4):640–649. doi: 10.1359/jbmr.2000.15.4.640. [DOI] [PubMed] [Google Scholar]
- 16.Huang L, Xu J, Wood DJ, Zheng MH. Gene expression of osteoprotegerin ligand, osteoprotegerin, and receptor activator of NF-kappaB in giant cell tumor of bone: possible involvement in tumor cell-induced osteoclast-like cell formation. Am J Pathol. 2000;156(3):761–767. doi: 10.1016/s0002-9440(10)64942-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Werner M. Giant cell tumour of bone: morphological, biological and histogenetical aspects. Int Orthop. 2006;30(6):484–489. doi: 10.1007/s00264-006-0215-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zheng MH, Fan Y, Wysocki SJ, et al. Gene expression of transforming growth factor-beta 1 and its type II receptor in giant cell tumors of bone: possible involvement in osteoclast-like cell migration. Am J Pathol. 1994;145(5):1095–1104. [PMC free article] [PubMed] [Google Scholar]
- 19.Nishimura M, Yuasa K, Mori K, et al. Cytological properties of stromal cells derived from giant cell tumor of bone (GCTSC) which can induce osteoclast formation of human blood monocytes without cell to cell contact. J Orthop Res. 2005;23(5):979–987. doi: 10.1016/j.orthres.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 20.Salerno M, Avnet S, Alberghini M, Giunti A, Baldini N. Histogenetic characterization of giant cell tumor of bone. Clin Orthop Relat Res. 2008;466(9):2081–2091. doi: 10.1007/s11999-008-0327-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yasuda H, Shima N, Nakagawa N, et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci U S A. 1998;95(7):3597–3602. doi: 10.1073/pnas.95.7.3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Itoh K, Udagawa N, Matsuzaki K, et al. Importance of membrane-or matrix-associated forms of M-CSF and RANKL/ODF in osteoclastogenesis supported by SaOS-4/3 cells expressing recombinant PTH/PTHrP receptors. J Bone Miner Res. 2000;15(9):1766–1775. doi: 10.1359/jbmr.2000.15.9.1766. [DOI] [PubMed] [Google Scholar]
- 23.Thomas DM, Skubitz KM. Giant cell tumour of bone. Curr Opin Oncol. 2009;21(4):338–344. doi: 10.1097/CCO.0b013e32832c951d. [DOI] [PubMed] [Google Scholar]
- 24.Morgan T, Atkins GJ, Trivett MK, et al. Molecular profiling of giant cell tumor of bone and the osteoclastic localization of ligand for receptor activator of nuclear factor kappaB. Am J Pathol. 2005;167(1):117–128. doi: 10.1016/s0002-9440(10)62959-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ng PK, Tsui SK, Lau CP, et al. CCAAT/enhancer binding protein beta is up-regulated in giant cell tumor of bone and regulates RANKL expression. J Cell Biochem. 2010;110(2):438–446. doi: 10.1002/jcb.22556. [DOI] [PubMed] [Google Scholar]
- 26.Baud'huin M, Renault R, Charrier C, et al. Interleukin-34 is expressed by giant cell tumours of bone and plays a key role in RANKL-induced osteoclastogenesis. J Pathol. 2010;221(1):77–86. doi: 10.1002/path.2684. [DOI] [PubMed] [Google Scholar]
- 27.Masui F, Ushigome S, Fujii K. Giant cell tumor of bone: an immunohistochemical comparative study. Pathol Int. 1998;48(5):355–361. doi: 10.1111/j.1440-1827.1998.tb03918.x. [DOI] [PubMed] [Google Scholar]
- 28.Rao VH, Singh RK, Bridge JA, et al. Regulation of MMP-9 (92 kDa type IV collagenase/gelatinase B) expression in stromal cells of human giant cell tumor of bone. Clin Exp Metastasis. 1997;15(4):400–409. doi: 10.1023/a:1018450204980. [DOI] [PubMed] [Google Scholar]
- 29.Rao VH, Singh RK, Delimont DC, et al. Transcriptional regulation of MMP-9 expression in stromal cells of human giant cell tumor of bone by tumor necrosis factor-alpha. Int J Oncol. 1999;14(2):291–300. doi: 10.3892/ijo.14.2.291. [DOI] [PubMed] [Google Scholar]
- 30.Ohsaki Y, Takahashi S, Scarcez T, et al. Evidence for an autocrine/paracrine role for interleukin-6 in bone resorption by giant cells from giant cell tumors of bone. Endocrinology. 1992;131(5):2229–2234. doi: 10.1210/endo.131.5.1425421. [DOI] [PubMed] [Google Scholar]
- 31.Wuelling M, Delling G, Kaiser E. Differential gene expression in stromal cells of human giant cell tumor of bone. Virchows Arch. 2004;445(6):621–630. doi: 10.1007/s00428-004-1113-2. [DOI] [PubMed] [Google Scholar]
- 32.Babeto E, Conceicao AL, Valsechi MC, et al. Differentially expressed genes in giant cell tumor of bone. Virchows Arch. 2011;458(4):467–476. doi: 10.1007/s00428-011-1047-4. [DOI] [PubMed] [Google Scholar]
- 33.Takanami I, Takeuchi K, Naruke M, Kodaira S. Aggressive surgery for treating a pulmonary metastasis of a benign giant cell tumor of the bone: results in four cases. J Thorac Cardiovasc Surg. 1998;116(4):649–651. doi: 10.1016/S0022-5223(98)70174-6. [DOI] [PubMed] [Google Scholar]
- 34.Gresen AA, Dahlin DC, Peterson LF, Payne WS. "Benign" giant cell tumor of bone metastasizing to lung. Ann Thorac Surg. 1973;16(5):531–535. doi: 10.1016/s0003-4975(10)65030-8. [DOI] [PubMed] [Google Scholar]
- 35.Miller IJ, Blank A, Yin SM, McNickle A, Gray R, Gitelis S. A case of recurrent giant cell tumor of bone with malignant transformation and benign pulmonary metastases. Diagn Pathol. 2010;5:62. doi: 10.1186/1746-1596-5-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Viswanathan S, Jambhekar NA. Metastatic giant cell tumor of bone: are there associated factors and best treatment modalities? Clin Orthop Relat Res. 2010;468(3):827–833. doi: 10.1007/s11999-009-0966-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Okamoto Y, Mathew S, Daw NC, et al. Giant cell tumor of bone with pulmonary metastases. Med Pediatr Oncol. 2003;41(5):454–459. doi: 10.1002/mpo.10258. [DOI] [PubMed] [Google Scholar]
- 38.Guo H, Garcia RA, Perle MA, Amodio J, Greco MA. Giant cell tumor of soft tissue with pulmonary metastases: pathologic and cytogenetic study. Pediatr Dev Pathol. 2005;8(6):718–724. doi: 10.1007/s10024-005-0014-y. [DOI] [PubMed] [Google Scholar]
- 39.Alacacioglu A, Bengi G, Oztop I, et al. Metastasis of giant cell tumor to the breast: case report and review of the literature. Tumori. 2006;92(4):351–353. doi: 10.1177/030089160609200416. [DOI] [PubMed] [Google Scholar]
- 40.Maloney WJ, Vaughan LM, Jones HH, Ross J, Nagel DA. Benign metastasizing giant-cell tumor of bone: report of three cases and review of the literature. Clin Orthop Relat Res. 1989;(243):208–215. [PubMed] [Google Scholar]
- 41.Conti A, Rodriguez GC, Chiechi A, et al. Identification of potential biomarkers for giant cell tumor of bone using comparative proteomics analysis. Am J Pathol. 2011;178(1):88–88. doi: 10.1016/j.ajpath.2010.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O'Donnell RJ, Springfield DS, Motwani HK, Ready JE, Gebhardt MC, Mankin HJ. Recurrence of giant-cell tumors of the long bones after curettage and packing with cement. J Bone Joint Surg Am. 1994;76(12):1827–1833. doi: 10.2106/00004623-199412000-00009. [DOI] [PubMed] [Google Scholar]
- 43.Marcove RC, Miller TR. The treatment of primary and metastatic localized bone tumors by cryosurgery. Surg Clin North Am. 1969;49(2):421–430. doi: 10.1016/s0039-6109(16)38799-0. [DOI] [PubMed] [Google Scholar]
- 44.Lu YP, Fan QY, Wang QL. Treatment of giant cell tumor of bone. Iowa Orthop J. 1988;8:39–42. [Google Scholar]
- 45.Futani H, Okumura Y, Fukuda Y, Fukunaga S, Hasegawa S, Yoshiya S. Giant cell tumor of the sternum: a case report and review of the literature. Anticancer Res. 2008;28(6B):4117–4120. [PubMed] [Google Scholar]
- 46.Oh JH, Yoon PW, Lee SH, Cho HS, Kim WS, Kim HS. Surgical treatment of giant cell tumour of long bone with anhydrous alcohol adjuvant. Int Orthop. 2006;30(6):490–494. doi: 10.1007/s00264-006-0154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goldring SR, Schiller AL, Mankin HJ, Dayer JM, Krane SM. Characterization of cells from human giant cell tumors of bone. Clin Orthop Relat Res. 1986;(204):59–75. [PubMed] [Google Scholar]
- 48.Lee FY, Montgomery M, Hazan EJ, Keel SB, Mankin HJ, Kattapuram S. Recurrent giant-cell tumor presenting as a soft-tissue mass: a report of four cases. J Bone Joint Surg Am. 1999;81(5):703–707. [PubMed] [Google Scholar]
- 49.Arbeitsgemeinschaft Knochentumoren. Becker WT, Dohle J, et al. Local recurrence of giant cell tumor of bone after intralesional treatment with and without adjuvant therapy. J Bone Joint Surg Am. 2008;90(5):1060–1067. doi: 10.2106/JBJS.D.02771. [DOI] [PubMed] [Google Scholar]
- 50.Klenke FM, Wenger DE, Inwards CY, Rose PS, Sim FH. Recurrent giant cell tumor of long bones: analysis of surgical management. Clin Orthop Relat Res. 2011;469(4):1181–1187. doi: 10.1007/s11999-010-1560-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klenke FM, Wenger DE, Inwards CY, Rose PS, Sim FH. Giant cell tumor of bone: risk factors for recurrence. Clin Orthop Relat Res. 2011;469(2):591–599. doi: 10.1007/s11999-010-1501-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Turcotte RE, Wunder JS, Isler MH, et al. Giant cell tumor of long bone: a Canadian Sarcoma Group study. Clin Orthop Relat Res. 2002;(397):248–258. doi: 10.1097/00003086-200204000-00029. [DOI] [PubMed] [Google Scholar]
- 53.Algawahmed H, Turcotte R, Farrokhyar F, Ghert M. High-speed burring with and without the use of surgical adjuvants in the intralesional management of giant cell tumor of bone: a systematic review and meta-analysis. Sarcoma. 2010;2010:586090. doi: 10.1155/2010/586090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Deheshi BM, Jaffer SN, Griffin AM, Ferguson PC, Bell RS, Wunder JS. Joint salvage for pathologic fracture of giant cell tumor of the lower extremity. Clin Orthop Relat Res. 2007;459:96–104. doi: 10.1097/BLO.0b013e31805d85e4. [DOI] [PubMed] [Google Scholar]
- 55.Jones KB, DeYoung BR, Morcuende JA, Buckwalter JA. Ethanol as a local adjuvant for giant cell tumor of bone. Iowa Orthop J. 2006;26:69–76. [PMC free article] [PubMed] [Google Scholar]
- 56.Durr HR, Maier M, Jansson V, Baur A, Refior HJ. Phenol as an adjuvant for local control in the treatment of giant cell tumour of the bone. Eur J Surg Oncol. 1999;25(6):610–618. doi: 10.1053/ejso.1999.0716. [DOI] [PubMed] [Google Scholar]
- 57.Trieb K, Bitzan P, Lang S, Dominkus M, Kotz R. Recurrence of curetted and bone-grafted giant-cell tumours with and without adjuvant phenol therapy. Eur J Surg Oncol. 2001;27(2):200–202. doi: 10.1053/ejso.2000.1086. [DOI] [PubMed] [Google Scholar]
- 58.Nicholson NC, Ramp WK, Kneisl JS, Kaysinger KK. Hydrogen peroxide inhibits giant cell tumor and osteoblast metabolism in vitro. Clin Orthop Relat Res. 1998;(347):250–260. [PubMed] [Google Scholar]
- 59.Ward WG, Sr, Li G., 3rd Customized treatment algorithm for giant cell tumor of bone: report of a series. Clin Orthop Relat Res. 2002;(397):259–270. doi: 10.1097/00003086-200204000-00030. [DOI] [PubMed] [Google Scholar]
- 60.Lewis VO, Wei A, Mendoza T, Primus F, Peabody T, Simon MA. Argon beam coagulation as an adjuvant for local control of giant cell tumor. Clin Orthop Relat Res. 2007;454:192–197. doi: 10.1097/01.blo.0000238784.98606.d4. [DOI] [PubMed] [Google Scholar]
- 61.Goldenberg RR, Campbell CJ, Bonfiglio M. Giant-cell tumor of bone: an analysis of two hundred and eighteen cases. J Bone Joint Surg Am. 1970;52(4):619–664. [PubMed] [Google Scholar]
- 62.Brien EW, Mirra JM, Kessler S, Suen M, Ho JK, Yang WT. Benign giant cell tumor of bone with osteosarcomatous transformation ("dedifferentiated" primary malignant GCT): report of two cases. Skeletal Radiol. 1997;26(4):246–255. doi: 10.1007/s002560050230. [DOI] [PubMed] [Google Scholar]
- 63.Malone S, O'Sullivan B, Catton C, Bell R, Fornasier V, Davis A. Long-term follow-up of efficacy and safety of megavoltage radiotherapy in high-risk giant cell tumors of bone. Int J Radiat Oncol Biol Phys. 1995;33(3):689–694. doi: 10.1016/0360-3016(95)00159-V. [DOI] [PubMed] [Google Scholar]
- 64.Caudell JJ, Ballo MT, Zagars GK, et al. Radiotherapy in the management of giant cell tumor of bone. Int J Radiat Oncol Biol Phys. 2003;57(1):158–165. doi: 10.1016/s0360-3016(03)00416-4. [DOI] [PubMed] [Google Scholar]
- 65.Micke O, Bruns F, Eich HT, et al. Radiation therapy for giant cell tumors of bone: long-term results of a multicenter study in Germany. Int J Radiat Oncol Biol Phys. 2005;63(Suppl 1):S108. [Google Scholar]
- 66.Ruka W, Rutkowski P, Morysinski T, et al. The megavoltage radiation therapy in treatment of patients with advanced or difficult giant cell tumors of bone. Int J Radiat Oncol Biol Phys. 2010;78(2):494–498. doi: 10.1016/j.ijrobp.2009.07.1704. [DOI] [PubMed] [Google Scholar]
- 67.Roux S, Amazit L, Meduri G, Guiochon-Mantel A, Milgrom E, Mariette X. RANK (receptor activator of nuclear factor kappa B) and RANK ligand are expressed in giant cell tumors of bone. Am J Clin Pathol. 2002;117(2):210–216. doi: 10.1309/BPET-F2PE-P2BD-J3P3. [DOI] [PubMed] [Google Scholar]
- 68.Thomas D, Henshaw R, Skubitz K, et al. Denosumab in patients with giant-cell tumour of bone: an open-label, phase 2 study. Lancet Oncol. 2010;11(3):275–280. doi: 10.1016/S1470-2045(10)70010-3. [DOI] [PubMed] [Google Scholar]
- 69.Cheng YY, Huang L, Lee KM, Xu JK, Zheng MH, Kumta SM. Bisphosphonates induce apoptosis of stromal tumor cells in giant cell tumor of bone. Calcif Tissue Int. 2004;75(1):71–77. doi: 10.1007/s00223-004-0120-2. [DOI] [PubMed] [Google Scholar]
- 70.Yu J, Chang SS, Suratwala S, et al. Zoledronate induces apoptosis in cells from fibro-cellular membrane of unicameral bone cyst (UBC) J Orthop Res. 2005;23(5):1004–1012. doi: 10.1016/j.orthres.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 71.Tse LF, Wong KC, Kumta SM, Huang L, Chow TC, Griffith JF. Bisphosphonates reduce local recurrence in extremity giant cell tumor of bone: a case-control study. Bone. 2008;42(1):68–73. doi: 10.1016/j.bone.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 72.Knowles HJ, Athanasou NA. Hypoxia-inducible factor is expressed in giant cell tumour of bone and mediates paracrine effects of hypoxia on monocyte-osteoclast differentiation via induction of VEGF. J Pathol. 2008;215(1):56–66. doi: 10.1002/path.2319. [DOI] [PubMed] [Google Scholar]
- 73.Kaban LB, Mulliken JB, Ezekowitz RA, Ebb D, Smith PS, Folkman J. Antiangiogenic therapy of a recurrent giant cell tumor of the mandible with interferon alfa-2a. Pediatrics. 1999;103(6 Pt 1):1145–1149. doi: 10.1542/peds.103.6.1145. [DOI] [PubMed] [Google Scholar]
- 74.Kaban LB, Troulis MJ, Ebb D, August M, Hornicek FJ, Dodson TB. Antiangiogenic therapy with interferon alpha for giant cell lesions of the jaws. J Oral Maxillofac Surg. 2002;60(10):1103–1111. doi: 10.1053/joms.2002.34975. [DOI] [PubMed] [Google Scholar]
- 75.Wei F, Liu X, Liu Z, et al. Interferon alfa-2b for recurrent and metastatic giant cell tumor of the spine: report of two cases. Spine (Phila Pa 1976) 2010;35(24):E1418–E1422. doi: 10.1097/BRS.0b013e3181e7bf5a. [DOI] [PubMed] [Google Scholar]