Abstract
Globus is a persistent or intermittent non-painful sensation of a lump or foreign body in the throat. It is a commonly encountered clinical condition that is usually long-lasting, difficult to treat, and has a tendency to recur. Furthermore, due to the uncertain etiology of globus, it remains difficult to establish standard investigation and treatment strategies for affected patients. As a first step for managing globus, careful history taking and nasolaryngoscopy are essential. Given the benign nature of the condition and the recent notion that gastroesophageal reflux disease is a major cause of globus, empirical therapy with a high dose of proton pump inhibitors is reasonable for patients with typical globus. If patients are nonresponsive to this therapy, definitive assessments such as endoscopy, multichannel intraluminal impedance/pH monitoring, and manometry should be considered. Speech and language therapy, anti-depressants, and cognitive-behavioral therapy can be helpful in patients whose symptoms persist despite negative investigations.
Keywords: Diagnosis, Gastroesophageal reflux disease, Globus, Proton pump inhibitor, Treatment
INTRODUCTION
Globus, a persistent or intermittent non-painful sensation of a lump or foreign body in the throat, is a well-defined clinical symptom that is usually long-lasting, difficult to treat, and has a tendency to recur. This symptom frequently improves with eating and is generally unaccompanied by dysphagia or odynophagia[1]. It is a common condition that accounts for approximately 4% of new referrals to ear, nose and throat (ENT) clinics, and it is reported by up to 46% of apparently healthy individuals, with a peak incidence in middle age[2,3]. This condition is equally prevalent in men and women, though the latter are more likely to seek health care for this symptom[4].
Hippocrates first noted globus pharyngeus approximately 2500 years ago[5]. In 1707, Purcell[6] was the first to accurately describe the condition; he believed that globus resulted from pressure on the thyroid cartilage due to contraction of the strap muscles of the neck. In the past, globus was described as “globus hystericus” because of its frequent association with menopause or psychogenic factors. However, Malcomson[7] coined the more accurate term “globus pharyngeus” in 1968 after discovering that most patients experiencing globus did not have a hysterical personality. The etiology of globus is still unknown but appears to be multifactorial (Table 1). Although data are limited, recent studies have focused on gastroesophageal reflux disease (GERD), abnormalities of the upper esophageal sphincter (UES), psychological and psychiatric disorders, and stress as major factors contributing to the globus sensation. The variety of potential etiologies has made it difficult to establish standard investigation and treatment strategies for affected patients.
Table 1.
Potential cause of globus
| Gastroesophageal reflux disease |
| Abnormal upper esophageal sphincter function |
| Esophageal motor disorders |
| Pharyngeal inflammatory causes including: pharyngitis, tonsillitis and chronic sinusitis |
| Upper aerodigestive malignancy |
| Hypertrophy of the base of the tongue |
| Retroverted epiglottis |
| Thyroid diseases |
| Cervical heterotopic gastric mucosa |
| Rare laryngopharyngeal tumors |
| Psychological factors and stress |
The aim of this review is to present the current literature on globus and to discuss its natural history and potential causes, current trends in its diagnosis, and methods for its treatment.
NATURAL HISTORY
Since few long-term follow-up studies have been conducted on patients with globus, the natural history of this condition has not been fully elucidated. In one study that followed 74 globus patients for an average of 7 years and 7 mo, 45% of the patients had persistent symptoms during the follow-up period[8]. An in-depth analysis of the features at clinical presentation failed to reveal any reliable prognostic indicators. In another long-term follow-up study, 60% of the patients had improved or resolved symptoms over a 5-year period, and the male patients with a history of globus less than 3 mo and who did not complain of any associated throat symptoms were reported to have the greatest chance of becoming asymptomatic or symptomatically improved[9].
POTENTIAL CAUSES OF GLOBUS
Gastroesophageal reflux disease
Although there is still considerable debate about the causative role of GERD in patients with globus, gastroesophageal reflux (GER) has been suggested to be a major etiology of this symptom, potentially accounting for 23%-68% of globus patients[10-18].
Malcomson[7] was the first to link GERD to the globus sensation through the use of barium swallow to uncover the presence of reflux in over 60% of patients with globus. Moreover, Koufman[16] found that 58% of patients with globus had abnormal pH results, and Cherry et al[19] demonstrated that 10 out of 12 subjects complained of globus when acid was infused into the distal esophagus. In a study that performed 24-h double-probe pH monitoring on 25 patients with globus and hoarseness, 72% of the patients exhibited pathologic reflux[20], and the globus symptom score was significantly higher in patients with GERD than in those without[21]. Additionally, globus sensation improved after 8 wk of proton pump inhibitor (PPI) therapy[22]. Several population-based surveys have supported such a potential link between GERD and the globus symptom by demonstrating an increased risk of globus among patients with GERD symptoms[23-25]. In a study by Dore et al[26], 38.7% of patients with GERD had the globus symptom, and the globus sensation was more prevalent in the non-erosive reflux disease group. Discordant data have also been reported[4,27-31]. However, it is clear that many patients with globus have concomitant GERD and that there is a true association between GERD and globus.
Two basic mechanisms have been proposed to explain the association between GERD and the globus sensation[14,32,33]: (1) Direct irritation and inflammation of the laryngopharynx by retrograde flow of gastric contents, also known as laryngopharyngeal reflux (LPR)[15,16,34]; (2) Vagovagal reflex hypertonicity of the UES triggered by acidification or distention of the distal esophagus[18].
Abnormal upper esophageal sphincter function
Abnormal UES function has also been suggested to be a cause of globus sensation[20,35-38]. Elevated UES pressure has been found to be much more frequent in patients with globus sensation than in controls (28% vs 3%), suggesting that hypertensive UES is a background factor for globus[30]. Additionally, injection of botulinum toxin into the cricopharyngeal muscle in a patient with both globus and extremely high UES pressure led to a resolution of the globus symptom and a decrease in UES pressure[35]. In a study of high-resolution manometry in patients with globus sensation, normal controls, and GERD patients without globus, hyperdynamic respiratory UES pressure changes were most prevalent in patients reporting globus[38]. However, other studies have reported contrary results[39-41].
Esophageal motor disorders
The prevalence of esophageal motor disorders has been reported to be 6%-90% in patients with globus, suggesting that esophageal motor disorders are a possible cause of, or a contributing factor in the development of globus[27,28,31,42]. Esophageal manometry has revealed abnormalities in as many as 67% of globus patients, with nonspecific esophageal motility disorder being the most frequent finding[31]. Moser et al[43] noted that esophageal motor disorders might, before giving rise to dysphagia, be sensed more vaguely and induce the globus sensation. However, to infer an etiological significance of this disorder in globus, it must be shown that the sensation resolves after treatment for the motor disorder.
Pharyngeal inflammatory causes
Many conditions that cause irritation and inflammation of the pharynx, such as pharyngitis, tonsillitis, and chronic sinusitis with postnasal drip, can be the cause of globus sensation by producing increased local sensitivity[28,44].
Upper aerodigestive tract malignancy
The presence of pharyngolaryngeal or upper esophageal malignancy must be excluded in patients with globus sensation, particularly in cases with “high risk” symptoms, such as weight loss, dysphagia, throat pain, and lateralization of pathology[5,45].
Hypertrophy of the tongue base
Globus can be induced by severe hypertrophy of the tongue base, probably due to the follicles touching the posterior wall of the pharynx. Mamede et al[46] demonstrated that hypertrophied follicles were frequent in patients with signs and symptoms of GER and that the symptoms of hypertrophy of the tongue base could be confused with those of GER.
Retroverted epiglottis
Through contact with the tongue base or the posterior pharyngeal wall, retroverted epiglottis may cause globus sensation. Symptom relief has been observed after partial epiglottectomy[47,48].
Thyroid diseases
Impalpable, ultrasound-detectable abnormalities in the thyroid are known to be more common in patients with globus sensation than in controls[32]. Burns et al[49] noted that as many as one-third of patients with a thyroid mass complained of globus-like symptoms. Post-thyroidectomy patients may also complain of globus pattern symptoms, but these frequently diminish with time. Although the exact mechanism of the association between globus and thyroid diseases is poorly understood, some reports have concluded that a thyroidectomy could improve the globus symptom[49-51].
Cervical heterotopic gastric mucosa
Globus sensation has also been linked to the presence of cervical heterotopic gastric mucosa (CHGM)[52-54], and acid secretion from CHGM appears to cause symptoms similar to those of GERD, including globus sensation. Patients with CHGM who complained of globus sensation and/or sore throat experienced a significant decrease in their symptoms after argon plasma ablation of CHGM[55,56]. Recently, it has been suggested that the globus symptom may be related to Helicobacter pylori infection of the CHGM[57].
Rare tumors
Smooth muscle tumors of the pharynx and post cricoid lymphangioma, as well as oropharyngeal metastasis of Merkel cell carcinoma, have been reported in patients complaining of globus[58-60]. These cases illustrate that patients with persistent globus should be further investigated to exclude rare lesions[32].
Psychological factors and stress
Psychogenic problems have often been thought to cause or trigger the globus sensation. Personality studies have found higher levels of alexithymia, neuroticism, and psychological distress (including anxiety, low mood, and somatic concerns) and lower levels of extraversion in patients presenting with globus[61,62]. In addition, several studies have reported increased numbers of stressful life events preceding symptom onset, suggesting that life stress might be a cofactor in symptom genesis and in exacerbation. Indeed, up to 96% of patients with globus report symptom exacerbation during periods of high emotional intensity[63,64]. However, some reports have found no differences in the psychological states of patients with globus compared to normal controls[4,10,65]. In actuality, psychiatric diagnoses are prevalent in subjects seeking health care for globus, but an explanation distinct from ascertainment bias has not been established, causing the etiological significance of these psychological characteristics to remain uncertain[1,65]. Two recent studies reported that psychological status might be different between LPR-positive and LPR-negative patients with globus[15,66]. Globus patients with LPR exhibited weaker psychological symptoms than non-LPR globus patients[15], and globus patients who did not respond to PPI had significantly higher anxiety scores[66].
Others
There have been numerous isolated case reports that have suggested an association of globus with cervical osteophytes[67], temporomandibular joint disorders[68], hyperviscosity of the nasopharyngeal mucosa[69], Eagle’s syndrome[70], excessive laryngeal and pharyngeal tension[61], and salivary hypofunction[33].
DIAGNOSIS
There has been no consensus regarding how best to diagnose and manage globus. A study of United Kingdom-based ENT specialists found that 14% performed no tests on globus patients but rather simply prescribed antacid medication if clinically indicated[71]. The remaining 86% investigated globus symptoms in a variety of ways, including rigid endoscopy (61%), barium swallow (56%), or a combination of these methods (17.5%).
Since globus is essentially a benign disorder, investigation is primarily aimed at identifying those few cases with upper aerodigestive malignancy. Thus, the first step of an investigation of globus symptoms should be to take a detailed patient history, paying particular attention to the presence of “high risk” symptoms, associated reflux symptoms, and psychological problems. Additionally, physicians should perform a physical examination of the neck followed by nasolaryngoscopic examination of the laryngopharynx, although the routine use of nasolaryngoscopy in patients with typical globus symptoms remains controversial[1]. Patients with typical globus symptoms usually require no further investigation beyond an outpatient nasolaryngoscopy[5]. However, patients with “alarm signs”, such as dysphagia, odynophagia, throat pain, weight loss, hoarseness, and lateralization of pathology, should undergo more extensive evaluation[1].
Reflux symptom index and reflux finding score
The symptoms and physical findings of LPR are nonspecific and can be confused with other laryngeal conditions caused by smoking, allergies, infections, vocal abuse, postnasal discharge, or neurogenic mechanisms as well as non-pathological variations[72]. Belafsky et al[73,74] proposed a useful self-administered tool, the reflux symptom index (RSI), for assessing the degree of LPR symptoms and developed the reflux finding score (RFS) based on 8 endolaryngeal signs for documenting the physical findings and severity of LPR. However, Park et al[15] demonstrated that RFS and RSI have low specificity in globus patients, suggesting that these may not be valid diagnostic tools for LPR in patients with globus.
Barium swallow
Barium swallow studies have been reported to identify benign lesions in up to one-third of patients with globus, and the most common findings include hiatal hernia and/or reflux (8%-18%), cervical osteophytes (0.4%-23%), and cricopharyngeal spasm (2.2%)[27,29,75,76]. However, given the prevalence of these findings in the general population, it is difficult to link these disorders to globus[45]. Two studies demonstrated that barium swallow did not identify any malignancy in typical globus patients[5,29]. Additionally, no pharyngeal or esophageal malignancy was found in a study that reviewed 1145 barium swallows in patients presenting with globus, prompting the authors to conclude that barium swallow should not be systematically requested for the exclusion of malignancies in patients with globus[77]. Thus, this test seems to have limited diagnostic value in the investigation of patients with globus.
Videofluoroscopy
Of 23 globus patients who received videofluoroscopy, 8 patients showed abnormal results; 5 had laryngeal aspiration, 2 had barium stasis in the vallecula and pyriform sinuses, and 4 had poor pharyngeal elevation[78]. Although it is unlikely that this indicates a causal relationship, videofluoroscopy may help to identify pharyngeal dysfunction in a substantial proportion of globus patients.
24-h dual-probe ambulatory pH monitoring
Whereas dual-probe ambulatory pH monitoring has been widely used in the clinical assessment of supra-esophageal GERD, this technology is not yet standardized, and its usefulness in the definition of a clinically relevant association with GERD is under debate. This technique has been used to show abnormal esophageal acid exposure in some globus patients[4,11]. However, reflux symptoms such as acid regurgitation and/or heartburn were also noted in these study populations. In a study of globus patients without reflux-like symptoms, all 24 focal individuals had normal dual-probe pH results[78]. Therefore, ambulatory pH monitoring seems to be less helpful for the evaluation of globus without reflux-like symptoms.
24-h multichannel intraluminal impedance monitoring
The results from several trials indicate that the best way to detect GER in patients with extraesophageal manifestations of GERD is to conduct multichannel intraluminal impedance (MII)/pH monitoring. In patients experiencing persistent globus during PPI therapy, MII/pH monitoring increased the diagnostic yield of standard pH testing in the identification of positive symptom indices through the detection of nonacid reflux; furthermore, proximal reflux was a significant predictor of the globus symptom[79]. In studies investigating the utility of MII/pH monitoring in patients displaying atypical symptoms while “off PPI”, MII/pH monitoring increased the diagnostic yield for objective detection of atypical manifestations of GERD[80-82]. Thus, this technique appears to be a more promising method of obtaining reliable data for the detection of LPR than 24-h dual probe monitoring, as it can monitor acid as well as nonacid reflux events and can distinguish between liquid and gaseous events. Therefore, MII/pH monitoring appears to be useful for ruling out GERD and for redirecting management of patients with suspected extraesophageal manifestations of GERD.
Flexible esophagogastroscopy
Endoscopy has been shown to be superior to barium swallow as a principal means of diagnosing upper aerodigestive tract malignancy[83]. Excellent views of the pyriform fossa and the postcricoid area can be achieved by insufflating air via flexible esophagogastroscopy[75]. Moreover, this procedure enables full esophageal evaluation and diagnosis of reflux esophagitis and/or upper esophageal malignancy as a cause of globus. However, in general, endoscopy is known to have low sensitivity and to be of limited value for the diagnosis of extraesophageal GERD. A study of 58 patients with pH-documented LPR found that only 19% had esophagitis or Barrett’s metaplasia[84]. In another study of patients with suspected LPR symptoms, esophagitis was generally prevalent[85] but occurred least in patients with globus and throat symptoms. Due to the association between globus and CGHM, it is necessary to carefully evaluate the cervical esophagus[54].
Manometry
If abnormal UES function and esophageal motor disorder are suspected to be the potential cause of globus, manometry is a useful tool for assessing UES and lower esophageal sphincter pressure, esophageal body contraction amplitude, and peristaltic sequence. However, the etiological significance of such a disorder is difficult to define.
TREATMENT
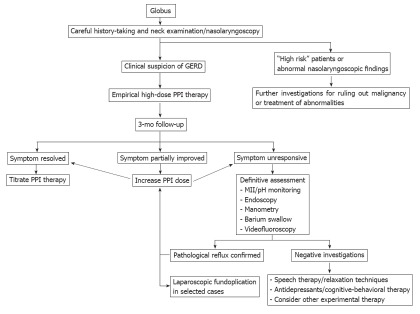
A suggested algorithm for the management of globus patients based on available evidence is shown in Figure 1. Since there is a paucity of controlled studies on the treatment of globus, evidence-based treatment concepts are currently not available, and a review of the literature reveals that there is no single effective treatment. Given the benign nature of the condition, the likelihood of long-term symptom persistence, and the absence of highly effective pharmacotherapy, the mainstays of treatment are explanation and reassurance[1]. Other established treatment options include anti-reflux therapy, speech and language therapy, anti-depressants, and cognitive-behavioral therapy[86].
Figure 1.
Algorithm for management of globus. GERD: Gastroesophageal reflux disease; PPI: Proton pump inhibitor; MII: Multichannel intraluminal impedance.
Anti-reflux treatment
Since GER has been suggested to be a major cause of globus[10-18], it seems practical that anti-reflux treatment should be the first attempted method for managing patients with globus. As diagnostic tests for GERD are somewhat invasive and costly and because a negative study result does not definitively rule out GER, it seems reasonable to use empirical PPI therapy as a combined method of diagnosis and treatment[87-92]. Although there are no controlled trials looking at the role of PPIs specifically for the treatment of globus, there is a variety of literature addressing the role of PPIs in LPR management[34,91,93-95]. Current evidence shows that the clinical response to PPIs in LPRD is variable[96,97] and that LPR symptoms improve more slowly than esophageal symptoms following acid-suppression therapy[98]. It is now widely accepted that extraesophageal GERD requires more aggressive and more prolonged therapy than typical GERD[32]. Empirical twice-daily therapy with PPIs for at least 3 mo is recommended; this can be extended for a maximum period of 6 mo[87-92,99-102]. A PPI should be taken 30-60 min before meals so that it has reached its highest concentration by the time food intake stimulates the proton pumps. After 3-6 mo, responders can be weaned, whereas non-responders should undergo a definitive assessment, such as endoscopy, pH monitoring, or MII/pH monitoring. If available, MII/pH monitoring is preferable to simple pH monitoring because it facilitates the detection of nonacid reflux. Nocturnal acid breakthrough (NAB) may cause incomplete treatment response[103,104]. The addition of h.s. histamine-2 receptor antagonists to twice-daily PPI therapy has been suggested to control NAB[103], but it is currently unclear whether this method offers any additional benefit to the long-term control of LPRD[105,106]. Prokinetics are utilized when it is necessary to speed up esophageal and gastric emptying; they can be useful when the clinical response to PPIs is unsatisfactory[16]. Diet and behavioral modification can also decrease the amount of reflux. Recommended dietary modifications include a reduction in the intake of chocolate, fats, citrus fruits, carbonated beverages, spicy tomato-based products, red wines, caffeine, and late-night meals. Additionally, patients should make more general behavioral modifications, including exercising regularly, avoiding smoking and alcohol, elevating the head of the bed (10-15 cm), avoiding tight clothes around the waist, and losing weight. Sleeping on one’s left-hand side also helps to decrease reflux. Steward et al[107] demonstrated that lifestyle modification was an independently significant variable in determining the response to pharmacological therapy. An alternative therapeutic strategy is anti-reflux surgery, with some authors having reported good improvement rates of LPR symptoms after laparoscopic nissen fundoplication[108-114]. To achieve a better patient outcome, a surgical approach must be taken into consideration in a carefully selected patient population, especially for patients who respond to treatment but are unable to tolerate PPIs due to side effects, those with confirmed pathological GER who do not respond to maximal medical treatment, and those in whom nonacid reflux has been demonstrated by a MII study[115]. However, if symptoms do not improve in the 4 mo following aggressive acid suppression, laparoscopic fundoplication may be unlikely to yield additional benefits[116]. Previous clinical responses to pharmacological acid suppression and abnormal pharyngeal pH results are preoperative predictors of relief from atypical symptoms[117].
Speech and language therapy/relaxation techniques
Speech therapy/relaxation techniques, including neck and shoulder exercises, general relaxation techniques, voice exercises, and voice hygiene to relieve vocal tract discomfort and tension, have successfully been used to treat patients with persistent globus symptoms[61]. In one uncontrolled study using these techniques on 25 globus patients, 92% experienced improvement following treatment. Khalil et al[118] randomly allocated 36 globus patients to either a speech therapy group or a reassurance group. Those in the speech therapy group used a number of exercises to relieve pharyngolaryngeal tension, including yawning, adopting a “giggle posture” (which helps retract the false vocal cords), and a “wet swallow” (as opposed to a “dry” or “check swallow,” which patients often perform habitually and which tends to aggravate the globus symptom). Patients also attempted to eliminate throat clearing and promote adequate hydration by avoiding smoking, excess tea, and coffee. At the end of 3 mo, patients in the speech therapy group demonstrated significantly better globus symptom scores compared with those recorded prior to the intervention. Individuals in the speech therapy group also experienced significant improvements in globus symptoms when compared with controls. However, further research is needed to distinguish whether speech therapy has a specific effect or whether patients simply benefit from general attention and reassurance[119].
Cognitive-behavioral therapy/antidepressants
Globus is the fourth most common symptom of somatization disorder after vomiting, aphonia, and pain in the extremities[120]. Cognitive-behavioral therapy has emerged as the best treatment for a variety of somatoform disorders and medically unexplained symptoms[121]. Although there has not yet been a substantial trial of cognitive-behavioral therapy in globus patients, it is likely to be a promising treatment for repeat attenders whose symptoms remain refractory[76].
A small series of anti-depressants have been found to be beneficial for some globus patients with concomitant psychiatric disorders, such as panic, somatization, major depression, and agoraphobia[122,123].
Other treatment strategies
Thyroidectomy in patients with thyroid disorder[49-51] or partial epiglottectomy in selected cases whose retroverted epiglottis made contact with the tongue base[47,48], were both reported to significantly relieve the globus symptom. In addition, ablation of CHGM by argon plasma coagulation has shown some promise in improving chronic globus symptoms[55,56]. Although additional research of these techniques is needed, these approaches would provide some benefit to patients with unexplained chronic globus who are refractory to any medical treatments.
CONCLUSION
Although globus is a common clinical condition, its etiology remains uncertain, and there is no standard protocol for its diagnosis and management. The results of recent studies have strongly suggested that GERD is a major cause of globus, though this remains under considerable debate. Numerous other disorders, such as abnormal UES function, esophageal motility disorders, structural head and neck diseases, and psychological factors, have been suggested as potential causes of globus. However, it has been rather difficult to establish a causal relationship between globus and these disorders because most of the reported studies were uncontrolled, had a small sample size, or were case reports. Currently, careful history taking and nasolaryngoscopy are essential as a first step in managing globus. Given the benign nature of the condition, patients with typical globus do not appear to need further investigation; rather, a 3-mo treatment with high-dose PPIs seems to be a reliable treatment option. If patients are nonresponsive to PPI therapy, they should undergo a definitive assessment, such as endoscopy, pH monitoring, or MII/pH monitoring; MII/pH monitoring in particular may increase the diagnostic yield of GER in globus patients. In cases with negative clinical investigations and consistent globus symptom, other treatment strategies, including speech therapy, anti-depressants, and cognitive-behavioral therapy, should be considered. In the future, well-designed, randomized controlled studies are needed to definitively determine the effect of PPI treatment on globus. In addition, it is necessary to ascertain the etiology of globus via large-scale studies.
Footnotes
Supported by A Pusan National University Hospital Clinical Research Grant (2011); a grant from the National R and D Program for Cancer Control, Ministry for Health, Welfare and Family Affairs, Republic of Korea, No. 0920050
Peer reviewers: Justin Che Yuen Wu, Professor, Department of Medicine and Therapeutics, The Chinese University of Hong Kong, 9/F Clinical Science Building, Prince of Wales Hospital, Shatin, Hong Kong, China; Diego Garcia-Compean, Faculty of Medicine, Autonomous University of Nuevo Leon, Monterrey 64700, Mexico; Tomohiko Shimatani, Professor, Lab of Adult Nursing and Internal Medicine, Hiroshima International University, 5-1-1 Hirokoshingai, Kure 7370112, Japan
S- Editor Gou SX L- Editor Rutherford A E- Editor Li JY
References
- 1.Galmiche JP, Clouse RE, Bálint A, Cook IJ, Kahrilas PJ, Paterson WG, Smout AJ. Functional esophageal disorders. Gastroenterology. 2006;130:1459–1465. doi: 10.1053/j.gastro.2005.08.060. [DOI] [PubMed] [Google Scholar]
- 2.Moloy PJ, Charter R. The globus symptom. Incidence, therapeutic response, and age and sex relationships. Arch Otolaryngol. 1982;108:740–744. doi: 10.1001/archotol.1982.00790590062017. [DOI] [PubMed] [Google Scholar]
- 3.Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, Whitehead WE, Janssens J, Funch-Jensen P, Corazziari E. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569–1580. doi: 10.1007/BF01303162. [DOI] [PubMed] [Google Scholar]
- 4.Batch AJ. Globus pharyngeus (Part I) J Laryngol Otol. 1988;102:152–158. doi: 10.1017/s0022215100104384. [DOI] [PubMed] [Google Scholar]
- 5.Harar RP, Kumar S, Saeed MA, Gatland DJ. Management of globus pharyngeus: review of 699 cases. J Laryngol Otol. 2004;118:522–527. doi: 10.1258/0022215041615092. [DOI] [PubMed] [Google Scholar]
- 6.Purcell J. A treatise of vapours or hysteric fits. 2nd ed. London: Edward Place; 1707. pp. 72–74. [Google Scholar]
- 7.Malcomson KG. Globus hystericus vel pharyngis (a recommaissance of proximal vagal modalities) J Laryngol Otol. 1968;82:219–230. doi: 10.1017/s0022215100068687. [DOI] [PubMed] [Google Scholar]
- 8.Rowley H, O’Dwyer TP, Jones AS, Timon CI. The natural history of globus pharyngeus. Laryngoscope. 1995;105:1118–1121. doi: 10.1288/00005537-199510000-00019. [DOI] [PubMed] [Google Scholar]
- 9.Timon C, O’Dwyer T, Cagney D, Walsh M. Globus pharyngeus: long-term follow-up and prognostic factors. Ann Otol Rhinol Laryngol. 1991;100:351–354. doi: 10.1177/000348949110000501. [DOI] [PubMed] [Google Scholar]
- 10.Hill J, Stuart RC, Fung HK, Ng EK, Cheung FM, Chung CS, van Hasselt CA. Gastroesophageal reflux, motility disorders, and psychological profiles in the etiology of globus pharyngis. Laryngoscope. 1997;107:1373–1377. doi: 10.1097/00005537-199710000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Chevalier JM, Brossard E, Monnier P. Globus sensation and gastroesophageal reflux. Eur Arch Otorhinolaryngol. 2003;260:273–276. doi: 10.1007/s00405-002-0544-0. [DOI] [PubMed] [Google Scholar]
- 12.Wilson JA, Pryde A, Piris J, Allan PL, Macintyre CC, Maran AG, Heading RC. Pharyngoesophageal dysmotility in globus sensation. Arch Otolaryngol Head Neck Surg. 1989;115:1086–1090. doi: 10.1001/archotol.1989.01860330076021. [DOI] [PubMed] [Google Scholar]
- 13.Koufman JA, Amin MR, Panetti M. Prevalence of reflux in 113 consecutive patients with laryngeal and voice disorders. Otolaryngol Head Neck Surg. 2000;123:385–388. doi: 10.1067/mhn.2000.109935. [DOI] [PubMed] [Google Scholar]
- 14.Oridate N, Nishizawa N, Fukuda S. The diagnosis and management of globus: a perspective from Japan. Curr Opin Otolaryngol Head Neck Surg. 2008;16:498–502. doi: 10.1097/MOO.0b013e328313bb69. [DOI] [PubMed] [Google Scholar]
- 15.Park KH, Choi SM, Kwon SU, Yoon SW, Kim SU. Diagnosis of laryngopharyngeal reflux among globus patients. Otolaryngol Head Neck Surg. 2006;134:81–85. doi: 10.1016/j.otohns.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 16.Koufman JA. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991;101:1–78. doi: 10.1002/lary.1991.101.s53.1. [DOI] [PubMed] [Google Scholar]
- 17.Koufman J, Sataloff RT, Toohill R. Laryngopharyngeal reflux: consensus conference report. J Voice. 1996;10:215–216. doi: 10.1016/s0892-1997(96)80001-4. [DOI] [PubMed] [Google Scholar]
- 18.Tokashiki R, Funato N, Suzuki M. Globus sensation and increased upper esophageal sphincter pressure with distal esophageal acid perfusion. Eur Arch Otorhinolaryngol. 2010;267:737–741. doi: 10.1007/s00405-009-1134-1. [DOI] [PubMed] [Google Scholar]
- 19.Cherry J, Siegel CI, Margulies SI, Donner M. Pharyngeal localization of symptoms of gastroesophageal reflux. Ann Otol Rhinol Laryngol. 1970;79:912–914. doi: 10.1177/000348947007900506. [DOI] [PubMed] [Google Scholar]
- 20.Smit CF, van Leeuwen JA, Mathus-Vliegen LM, Devriese PP, Semin A, Tan J, Schouwenburg PF. Gastropharyngeal and gastroesophageal reflux in globus and hoarseness. Arch Otolaryngol Head Neck Surg. 2000;126:827–830. doi: 10.1001/archotol.126.7.827. [DOI] [PubMed] [Google Scholar]
- 21.Sinn DH, Kim JH, Kim S, Son HJ, Kim JJ, Rhee JC, Rhee PL. Response rate and predictors of response in a short-term empirical trial of high-dose rabeprazole in patients with globus. Aliment Pharmacol Ther. 2008;27:1275–1281. doi: 10.1111/j.1365-2036.2008.03659.x. [DOI] [PubMed] [Google Scholar]
- 22.Tokashiki R, Yamaguchi H, Nakamura K, Suzuki M. Globus sensation caused by gastroesophageal reflux disease. Auris Nasus Larynx. 2002;29:347–351. doi: 10.1016/s0385-8146(02)00022-6. [DOI] [PubMed] [Google Scholar]
- 23.Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–1456. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 24.Rey E, Elola-Olaso CM, Rodríguez-Artalejo F, Locke GR, Díaz-Rubio M. Prevalence of atypical symptoms and their association with typical symptoms of gastroesophageal reflux in Spain. Eur J Gastroenterol Hepatol. 2006;18:969–975. doi: 10.1097/01.meg.0000230081.53298.03. [DOI] [PubMed] [Google Scholar]
- 25.Cho YS, Choi MG, Jeong JJ, Chung WC, Lee IS, Kim SW, Han SW, Choi KY, Chung IS. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Asan-si, Korea. Am J Gastroenterol. 2005;100:747–753. doi: 10.1111/j.1572-0241.2005.41245.x. [DOI] [PubMed] [Google Scholar]
- 26.Dore MP, Pedroni A, Pes GM, Maragkoudakis E, Tadeu V, Pirina P, Realdi G, Delitala G, Malaty HM. Effect of antisecretory therapy on atypical symptoms in gastroesophageal reflux disease. Dig Dis Sci. 2007;52:463–468. doi: 10.1007/s10620-006-9573-7. [DOI] [PubMed] [Google Scholar]
- 27.Wilson JA, Heading RC, Maran AG, Pryde A, Piris J, Allan PL. Globus sensation is not due to gastro-oesophageal reflux. Clin Otolaryngol Allied Sci. 1987;12:271–275. doi: 10.1111/j.1365-2273.1987.tb00201.x. [DOI] [PubMed] [Google Scholar]
- 28.Batch AJ. Globus pharyngeus: (Part II), Discussion. J Laryngol Otol. 1988;102:227–230. doi: 10.1017/s0022215100104591. [DOI] [PubMed] [Google Scholar]
- 29.Back GW, Leong P, Kumar R, Corbridge R. Value of barium swallow in investigation of globus pharyngeus. J Laryngol Otol. 2000;114:951–954. doi: 10.1258/0022215001904437. [DOI] [PubMed] [Google Scholar]
- 30.Corso MJ, Pursnani KG, Mohiuddin MA, Gideon RM, Castell JA, Katzka DA, Katz PO, Castell DO. Globus sensation is associated with hypertensive upper esophageal sphincter but not with gastroesophageal reflux. Dig Dis Sci. 1998;43:1513–1517. doi: 10.1023/a:1018862814873. [DOI] [PubMed] [Google Scholar]
- 31.Färkkilä MA, Ertama L, Katila H, Kuusi K, Paavolainen M, Varis K. Globus pharyngis, commonly associated with esophageal motility disorders. Am J Gastroenterol. 1994;89:503–508. [PubMed] [Google Scholar]
- 32.Remacle M. The diagnosis and management of globus: a perspective from Belgium. Curr Opin Otolaryngol Head Neck Surg. 2008;16:511–515. doi: 10.1097/moo.0b013e328313bb94. [DOI] [PubMed] [Google Scholar]
- 33.Baek CH, Chung MK, Choi JY, So YK, Son YI, Jeong HS. Role of salivary function in patients with globus pharyngeus. Head Neck. 2010;32:244–252. doi: 10.1002/hed.21176. [DOI] [PubMed] [Google Scholar]
- 34.Ford CN. Evaluation and management of laryngopharyngeal reflux. JAMA. 2005;294:1534–1540. doi: 10.1001/jama.294.12.1534. [DOI] [PubMed] [Google Scholar]
- 35.Halum SL, Butler SG, Koufman JA, Postma GN. Treatment of globus by upper esophageal sphincter injection with botulinum A toxin. Ear Nose Throat J. 2005;84:74. [PubMed] [Google Scholar]
- 36.Watson WC, Sullivan SN. Hypertonicity of the cricopharyngeal sphincter: A cause of globus sensation. Lancet. 1974;2:1417–1419. doi: 10.1016/s0140-6736(74)90074-9. [DOI] [PubMed] [Google Scholar]
- 37.Hunt PS, Connell AM, Smiley TB. The cricopharyngeal sphincter in gastric reflux. Gut. 1970;11:303–306. doi: 10.1136/gut.11.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kwiatek MA, Mirza F, Kahrilas PJ, Pandolfino JE. Hyperdynamic upper esophageal sphincter pressure: a manometric observation in patients reporting globus sensation. Am J Gastroenterol. 2009;104:289–298. doi: 10.1038/ajg.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Caldarelli DD, Andrews AH, Derbyshire AJ. Esophageal motility studies in globus sensation. Ann Otol Rhinol Laryngol. 1970;79:1098–1100. doi: 10.1177/000348947007900612. [DOI] [PubMed] [Google Scholar]
- 40.Cook IJ, Dent J, Collins SM. Upper esophageal sphincter tone and reactivity to stress in patients with a history of globus sensation. Dig Dis Sci. 1989;34:672–676. doi: 10.1007/BF01540336. [DOI] [PubMed] [Google Scholar]
- 41.Sun J, Xu B, Yuan YZ, Xu JY. Study on the function of pharynx upper esophageal sphincter in globus hystericus. World J Gastroenterol. 2002;8:952–955. doi: 10.3748/wjg.v8.i5.952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Knight RE, Wells JR, Parrish RS. Esophageal dysmotility as an important co-factor in extraesophageal manifestations of gastroesophageal reflux. Laryngoscope. 2000;110:1462–1466. doi: 10.1097/00005537-200009000-00010. [DOI] [PubMed] [Google Scholar]
- 43.Moser G, Vacariu-Granser GV, Schneider C, Abatzi TA, Pokieser P, Stacher-Janotta G, Gaupmann G, Weber U, Wenzel T, Roden M. High incidence of esophageal motor disorders in consecutive patients with globus sensation. Gastroenterology. 1991;101:1512–1521. doi: 10.1016/0016-5085(91)90386-y. [DOI] [PubMed] [Google Scholar]
- 44.Lee JW, Song CW, Kang CD, Hur BW, Jeen YT, Jeon HJ, Lee HS, Lee SW, Um SH, Choi JH, et al. Pharyngoesophageal motility in patients with globus sensation. Korean J Gastroenterol. 2000;36:1–9. [Google Scholar]
- 45.Cathcart R, Wilson JA. Lump in the throat. Clin Otolaryngol. 2007;32:108–110. doi: 10.1111/j.1365-2273.2007.01408.x. [DOI] [PubMed] [Google Scholar]
- 46.Mamede RC, De Mello-Filho FV, Dantas RO. Severe hypertrophy of the base of the tongue in adults. Otolaryngol Head Neck Surg. 2004;131:378–382. doi: 10.1016/j.otohns.2004.02.040. [DOI] [PubMed] [Google Scholar]
- 47.Agada FO, Coatesworth AP, Grace AR. Retroverted epiglottis presenting as a variant of globus pharyngeus. J Laryngol Otol. 2007;121:390–392. doi: 10.1017/S0022215106003422. [DOI] [PubMed] [Google Scholar]
- 48.Quesada JL, Lorente J, Quesada P. Partial epiglottectomy as a possible treatment for globus pharyngeus? Eur Arch Otorhinolaryngol. 2000;257:386–388. doi: 10.1007/s004059900226. [DOI] [PubMed] [Google Scholar]
- 49.Burns P, Timon C. Thyroid pathology and the globus symptom: are they related? A two year prospective trial. J Laryngol Otol. 2007;121:242–245. doi: 10.1017/S0022215106002465. [DOI] [PubMed] [Google Scholar]
- 50.Marshall JN, McGann G, Cook JA, Taub N. A prospective controlled study of high-resolution thyroid ultrasound in patients with globus pharyngeus. Clin Otolaryngol Allied Sci. 1996;21:228–231. doi: 10.1111/j.1365-2273.1996.tb01731.x. [DOI] [PubMed] [Google Scholar]
- 51.Maung KH, Hayworth D, Nix PA, Atkin SL, England RJ. Thyroidectomy does not cause globus pattern symptoms. J Laryngol Otol. 2005;119:973–975. doi: 10.1258/002221505775010760. [DOI] [PubMed] [Google Scholar]
- 52.von Rahden BH, Stein HJ, Becker K, Liebermann-Meffert D, Siewert JR. Heterotopic gastric mucosa of the esophagus: literature-review and proposal of a clinicopathologic classification. Am J Gastroenterol. 2004;99:543–551. doi: 10.1111/j.1572-0241.2004.04082.x. [DOI] [PubMed] [Google Scholar]
- 53.Lancaster JL, Gosh S, Sethi R, Tripathi S. Can heterotopic gastric mucosa present as globus pharyngeus? J Laryngol Otol. 2006;120:575–578. doi: 10.1017/S0022215106001307. [DOI] [PubMed] [Google Scholar]
- 54.Alaani A, Jassar P, Warfield AT, Gouldesbrough DR, Smith I. Heterotopic gastric mucosa in the cervical oesophagus (inlet patch) and globus pharyngeus--an under-recognised association. J Laryngol Otol. 2007;121:885–888. doi: 10.1017/S0022215106005524. [DOI] [PubMed] [Google Scholar]
- 55.Meining A, Bajbouj M, Preeg M, Reichenberger J, Kassem AM, Huber W, Brockmeyer SJ, Hannig C, Höfler H, Prinz C, et al. Argon plasma ablation of gastric inlet patches in the cervical esophagus may alleviate globus sensation: a pilot trial. Endoscopy. 2006;38:566–570. doi: 10.1055/s-2006-925362. [DOI] [PubMed] [Google Scholar]
- 56.Bajbouj M, Becker V, Eckel F, Miehlke S, Pech O, Prinz C, Schmid RM, Meining A. Argon plasma coagulation of cervical heterotopic gastric mucosa as an alternative treatment for globus sensations. Gastroenterology. 2009;137:440–444. doi: 10.1053/j.gastro.2009.04.053. [DOI] [PubMed] [Google Scholar]
- 57.Alagozlu H, Simsek Z, Unal S, Cindoruk M, Dumlu S, Dursun A. Is there an association between Helicobacter pylori in the inlet patch and globus sensation? World J Gastroenterol. 2010;16:42–47. doi: 10.3748/wjg.v16.i1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Husamaldin Z, Aung W, McFerran DJ. Smooth muscle tumour of the pharynx: a rare tumour presenting with globus pharyngeus symptoms. J Laryngol Otol. 2004;118:885–887. doi: 10.1258/0022215042703732. [DOI] [PubMed] [Google Scholar]
- 59.Smith NM, Stafford FW. Post cricoid lymphangioma. J Laryngol Otol. 1991;105:220–221. doi: 10.1017/s0022215100115427. [DOI] [PubMed] [Google Scholar]
- 60.Reichel OA, Mayr D, Issing WJ. Oropharyngeal metastasis of a Merkel cell carcinoma of the skin. Eur Arch Otorhinolaryngol. 2003;260:258–260. doi: 10.1007/s00405-002-0564-9. [DOI] [PubMed] [Google Scholar]
- 61.Wareing M, Elias A, Mitchell D. Management of globus sensation by the speech therapist. Logoped Phoniatr Vocol. 1997;22:39–42. [Google Scholar]
- 62.Deary IJ, Wilson JA, Kelly SW. Globus pharyngis, personality, and psychological distress in the general population. Psychosomatics. 1995;36:570–577. doi: 10.1016/S0033-3182(95)71614-0. [DOI] [PubMed] [Google Scholar]
- 63.Harris MB, Deary IJ, Wilson JA. Life events and difficulties in relation to the onset of globus pharyngis. J Psychosom Res. 1996;40:603–615. doi: 10.1016/0022-3999(96)00024-4. [DOI] [PubMed] [Google Scholar]
- 64.Thompson WG, Heaton KW. Heartburn and globus in apparently healthy people. Can Med Assoc J. 1982;126:46–48. [PMC free article] [PubMed] [Google Scholar]
- 65.Moser G, Wenzel-Abatzi TA, Stelzeneder M, Wenzel T, Weber U, Wiesnagrotzki S, Schneider C, Schima W, Stacher-Janotta G, Vacariu-Granser GV, et al. Globus sensation: pharyngoesophageal function, psychometric and psychiatric findings, and follow-up in 88 patients. Arch Intern Med. 1998;158:1365–1373. doi: 10.1001/archinte.158.12.1365. [DOI] [PubMed] [Google Scholar]
- 66.Siupsinskiene N, Adamonis K, Toohill RJ, Sereika R. Predictors of response to short-term proton pump inhibitor treatment in laryngopharyngeal reflux patients. J Laryngol Otol. 2008;122:1206–1212. doi: 10.1017/S0022215108001898. [DOI] [PubMed] [Google Scholar]
- 67.Maran A, Jacobson I. Cervical osteophytes presenting with pharyngeal symptoms. Laryngoscope. 1971;81:412–417. doi: 10.1288/00005537-197103000-00009. [DOI] [PubMed] [Google Scholar]
- 68.Kirveskari P, Puhakka H. Effect of occlusal adjustment on globus symptom. J Prosthet Dent. 1985;54:832–835. doi: 10.1016/0022-3913(85)90482-2. [DOI] [PubMed] [Google Scholar]
- 69.Shiomi Y, Shiomi Y, Oda N, Hosoda S. Hyperviscoelasticity of epipharyngeal mucus may induce globus pharyngis. Ann Otol Rhinol Laryngol. 2002;111:1116–1119. doi: 10.1177/000348940211101210. [DOI] [PubMed] [Google Scholar]
- 70.Beder E, Ozgursoy OB, Karatayli Ozgursoy S, Anadolu Y. Three-dimensional computed tomography and surgical treatment for Eagle’s syndrome. Ear Nose Throat J. 2006;85:443–445. [PubMed] [Google Scholar]
- 71.Webb CJ, Makura ZG, Fenton JE, Jackson SR, McCormick MS, Jones AS. Globus pharyngeus: a postal questionnaire survey of UK ENT consultants. Clin Otolaryngol Allied Sci. 2000;25:566–569. doi: 10.1046/j.1365-2273.2000.00386.x. [DOI] [PubMed] [Google Scholar]
- 72.Vaezi MF, Hicks DM, Abelson TI, Richter JE. Laryngeal signs and symptoms and gastroesophageal reflux disease (GERD): a critical assessment of cause and effect association. Clin Gastroenterol Hepatol. 2003;1:333–344. doi: 10.1053/s1542-3565(03)00177-0. [DOI] [PubMed] [Google Scholar]
- 73.Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI) J Voice. 2002;16:274–277. doi: 10.1016/s0892-1997(02)00097-8. [DOI] [PubMed] [Google Scholar]
- 74.Belafsky PC, Postma GN, Koufman JA. The validity and reliability of the reflux finding score (RFS) Laryngoscope. 2001;111:1313–1317. doi: 10.1097/00005537-200108000-00001. [DOI] [PubMed] [Google Scholar]
- 75.Takwoingi YM, Kale US, Morgan DW. Rigid endoscopy in globus pharyngeus: how valuable is it? J Laryngol Otol. 2006;120:42–46. doi: 10.1017/S0022215105006043. [DOI] [PubMed] [Google Scholar]
- 76.Burns P, O’Neill JP. The diagnosis and management of globus: a perspective from Ireland. Curr Opin Otolaryngol Head Neck Surg. 2008;16:503–506. doi: 10.1097/MOO.0b013e3283169258. [DOI] [PubMed] [Google Scholar]
- 77.Alaani A, Vengala S, Johnston MN. The role of barium swallow in the management of the globus pharyngeus. Eur Arch Otorhinolaryngol. 2007;264:1095–1097. doi: 10.1007/s00405-007-0315-z. [DOI] [PubMed] [Google Scholar]
- 78.Chen CL, Tsai CC, Chou AS, Chiou JH. Utility of ambulatory pH monitoring and videofluoroscopy for the evaluation of patients with globus pharyngeus. Dysphagia. 2007;22:16–19. doi: 10.1007/s00455-006-9033-8. [DOI] [PubMed] [Google Scholar]
- 79.Anandasabapathy S, Jaffin BW. Multichannel intraluminal impedance in the evaluation of patients with persistent globus on proton pump inhibitor therapy. Ann Otol Rhinol Laryngol. 2006;115:563–570. doi: 10.1177/000348940611500801. [DOI] [PubMed] [Google Scholar]
- 80.Bajbouj M, Becker V, Neuber M, Schmid RM, Meining A. Combined pH-metry/impedance monitoring increases the diagnostic yield in patients with atypical gastroesophageal reflux symptoms. Digestion. 2007;76:223–228. doi: 10.1159/000112728. [DOI] [PubMed] [Google Scholar]
- 81.Lee BE, Kim GH, Ryu DY, Kim DU, Cheong JH, Lee DG, Song GA. Combined Dual Channel Impedance/pH-metry in Patients With Suspected Laryngopharyngeal Reflux. J Neurogastroenterol Motil. 2010;16:157–165. doi: 10.5056/jnm.2010.16.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Malhotra A, Freston JW, Aziz K. Use of pH-impedance testing to evaluate patients with suspected extraesophageal manifestations of gastroesophageal reflux disease. J Clin Gastroenterol. 2008;42:271–278. doi: 10.1097/MCG.0b013e31802b64f3. [DOI] [PubMed] [Google Scholar]
- 83.Levine B, Nielsen EW. The justifications and controversies of panendoscopy--a review. Ear Nose Throat J. 1992;71:335–340, 343. [PubMed] [Google Scholar]
- 84.Koufman JA, Belafsky PC, Bach KK, Daniel E, Postma GN. Prevalence of esophagitis in patients with pH-documented laryngopharyngeal reflux. Laryngoscope. 2002;112:1606–1609. doi: 10.1097/00005537-200209000-00014. [DOI] [PubMed] [Google Scholar]
- 85.Poelmans J, Feenstra L, Demedts I, Rutgeerts P, Tack J. The yield of upper gastrointestinal endoscopy in patients with suspected reflux-related chronic ear, nose, and throat symptoms. Am J Gastroenterol. 2004;99:1419–1426. doi: 10.1111/j.1572-0241.2004.30066.x. [DOI] [PubMed] [Google Scholar]
- 86.Karkos PD, Wilson JA. The diagnosis and management of globus pharyngeus: our perspective from the United Kingdom. Curr Opin Otolaryngol Head Neck Surg. 2008;16:521–524. doi: 10.1097/MOO.0b013e328316933b. [DOI] [PubMed] [Google Scholar]
- 87.Divi V, Benninger MS. Diagnosis and management of laryngopharyngeal reflux disease. Curr Opin Otolaryngol Head Neck Surg. 2006;14:124–127. doi: 10.1097/01.moo.0000193200.78214.e9. [DOI] [PubMed] [Google Scholar]
- 88.Celik M, Ercan I. Diagnosis and management of laryngopharyngeal reflux disease. Curr Opin Otolaryngol Head Neck Surg. 2006;14:150–155. doi: 10.1097/01.moo.0000193177.62074.fd. [DOI] [PubMed] [Google Scholar]
- 89.Remacle M, Lawson G. Diagnosis and management of laryngopharyngeal reflux disease. Curr Opin Otolaryngol Head Neck Surg. 2006;14:143–149. doi: 10.1097/01.moo.0000193189.17225.91. [DOI] [PubMed] [Google Scholar]
- 90.Pontes P, Tiago R. Diagnosis and management of laryngopharyngeal reflux disease. Curr Opin Otolaryngol Head Neck Surg. 2006;14:138–142. doi: 10.1097/01.moo.0000193193.09602.51. [DOI] [PubMed] [Google Scholar]
- 91.Mahieu HF. Review article: The laryngological manifestations of reflux disease; why the scepticism? Aliment Pharmacol Ther. 2007;26 Suppl 2:17–24. doi: 10.1111/j.1365-2036.2007.03474.x. [DOI] [PubMed] [Google Scholar]
- 92.Bove MJ, Rosen C. Diagnosis and management of laryngopharyngeal reflux disease. Curr Opin Otolaryngol Head Neck Surg. 2006;14:116–123. doi: 10.1097/01.moo.0000193177.62074.fd. [DOI] [PubMed] [Google Scholar]
- 93.El-Serag HB, Lee P, Buchner A, Inadomi JM, Gavin M, McCarthy DM. Lansoprazole treatment of patients with chronic idiopathic laryngitis: a placebo-controlled trial. Am J Gastroenterol. 2001;96:979–983. doi: 10.1111/j.1572-0241.2001.03681.x. [DOI] [PubMed] [Google Scholar]
- 94.Noordzij JP, Khidr A, Evans BA, Desper E, Mittal RK, Reibel JF, Levine PA. Evaluation of omeprazole in the treatment of reflux laryngitis: a prospective, placebo-controlled, randomized, double-blind study. Laryngoscope. 2001;111:2147–2151. doi: 10.1097/00005537-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 95.Issing WJ, Karkos PD, Perreas K, Folwaczny C, Reichel O. Dual-probe 24-hour ambulatory pH monitoring for diagnosis of laryngopharyngeal reflux. J Laryngol Otol. 2004;118:845–848. doi: 10.1258/0022215042703660. [DOI] [PubMed] [Google Scholar]
- 96.Katz PO, Castell DO. Medical therapy of supraesophageal gastroesophageal reflux disease. Am J Med. 2000;108 Suppl 4a:170S–177S. doi: 10.1016/s0002-9343(99)00359-9. [DOI] [PubMed] [Google Scholar]
- 97.Vaezi MF. Extraesophageal manifestations of gastroesophageal reflux disease. Clin Cornerstone. 2003;5:32–38; discussion 39-40. doi: 10.1016/s1098-3597(03)90097-4. [DOI] [PubMed] [Google Scholar]
- 98.Oridate N, Takeda H, Asaka M, Nishizawa N, Mesuda Y, Mori M, Furuta Y, Fukuda S. Acid-suppression therapy offers varied laryngopharyngeal and esophageal symptom relief in laryngopharyngeal reflux patients. Dig Dis Sci. 2008;53:2033–2038. doi: 10.1007/s10620-007-0114-9. [DOI] [PubMed] [Google Scholar]
- 99.Park W, Hicks DM, Khandwala F, Richter JE, Abelson TI, Milstein C, Vaezi MF. Laryngopharyngeal reflux: prospective cohort study evaluating optimal dose of proton-pump inhibitor therapy and pretherapy predictors of response. Laryngoscope. 2005;115:1230–1238. doi: 10.1097/01.MLG.0000163746.81766.45. [DOI] [PubMed] [Google Scholar]
- 100.Williams RB, Szczesniak MM, Maclean JC, Brake HM, Cole IE, Cook IJ. Predictors of outcome in an open label, therapeutic trial of high-dose omeprazole in laryngitis. Am J Gastroenterol. 2004;99:777–785. doi: 10.1111/j.1572-0241.2004.04151.x. [DOI] [PubMed] [Google Scholar]
- 101.Amin MR, Postma GN, Johnson P, Digges N, Koufman JA. Proton pump inhibitor resistance in the treatment of laryngopharyngeal reflux. Otolaryngol Head Neck Surg. 2001;125:374–378. doi: 10.1067/mhn.2001.118691. [DOI] [PubMed] [Google Scholar]
- 102.Belafsky PC, Postma GN, Koufman JA. Laryngopharyngeal reflux symptoms improve before changes in physical findings. Laryngoscope. 2001;111:979–981. doi: 10.1097/00005537-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 103.Peghini PL, Katz PO, Bracy NA, Castell DO. Nocturnal recovery of gastric acid secretion with twice-daily dosing of proton pump inhibitors. Am J Gastroenterol. 1998;93:763–767. doi: 10.1111/j.1572-0241.1998.221_a.x. [DOI] [PubMed] [Google Scholar]
- 104.Peghini PL, Katz PO, Castell DO. Ranitidine controls nocturnal gastric acid breakthrough on omeprazole: a controlled study in normal subjects. Gastroenterology. 1998;115:1335–1339. doi: 10.1016/s0016-5085(98)70010-1. [DOI] [PubMed] [Google Scholar]
- 105.Fackler WK, Ours TM, Vaezi MF, Richter JE. Long-term effect of H2RA therapy on nocturnal gastric acid breakthrough. Gastroenterology. 2002;122:625–632. doi: 10.1053/gast.2002.31876. [DOI] [PubMed] [Google Scholar]
- 106.Ours TM, Fackler WK, Richter JE, Vaezi MF. Nocturnal acid breakthrough: clinical significance and correlation with esophageal acid exposure. Am J Gastroenterol. 2003;98:545–550. doi: 10.1111/j.1572-0241.2003.07304.x. [DOI] [PubMed] [Google Scholar]
- 107.Steward DL, Wilson KM, Kelly DH, Patil MS, Schwartzbauer HR, Long JD, Welge JA. Proton pump inhibitor therapy for chronic laryngo-pharyngitis: a randomized placebo-control trial. Otolaryngol Head Neck Surg. 2004;131:342–350. doi: 10.1016/j.otohns.2004.03.037. [DOI] [PubMed] [Google Scholar]
- 108.Lindstrom DR, Wallace J, Loehrl TA, Merati AL, Toohill RJ. Nissen fundoplication surgery for extraesophageal manifestations of gastroesophageal reflux (EER) Laryngoscope. 2002;112:1762–1765. doi: 10.1097/00005537-200210000-00010. [DOI] [PubMed] [Google Scholar]
- 109.Oelschlager BK, Eubanks TR, Oleynikov D, Pope C, Pellegrini CA. Symptomatic and physiologic outcomes after operative treatment for extraesophageal reflux. Surg Endosc. 2002;16:1032–1036. doi: 10.1007/s00464-001-8252-1. [DOI] [PubMed] [Google Scholar]
- 110.Fernando HC, El-Sherif A, Landreneau RJ, Gilbert S, Christie NA, Buenaventura PO, Close JM, Luketich JD. Efficacy of laparoscopic fundoplication in controlling pulmonary symptoms associated with gastroesophageal reflux disease. Surgery. 2005;138:612–616; discussion 612-616. doi: 10.1016/j.surg.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 111.Westcott CJ, Hopkins MB, Bach K, Postma GN, Belafsky PC, Koufman JA. Fundoplication for laryngopharyngeal reflux disease. J Am Coll Surg. 2004;199:23–30. doi: 10.1016/j.jamcollsurg.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 112.Catania RA, Kavic SM, Roth JS, Lee TH, Meyer T, Fantry GT, Castellanos PF, Park A. Laparoscopic Nissen fundoplication effectively relieves symptoms in patients with laryngopharyngeal reflux. J Gastrointest Surg. 2007;11:1579–1587; discussion 1579-1587. doi: 10.1007/s11605-007-0318-5. [DOI] [PubMed] [Google Scholar]
- 113.Sala E, Salminen P, Simberg S, Koskenvuo J, Ovaska J. Laryngopharyngeal reflux disease treated with laparoscopic fundoplication. Dig Dis Sci. 2008;53:2397–2404. doi: 10.1007/s10620-007-0169-7. [DOI] [PubMed] [Google Scholar]
- 114.Antoniou SA, Delivorias P, Antoniou GA, Natsiopoulos I, Kalambakas A, Dalenbäck J, Makridis C. Symptom-focused results after laparoscopic fundoplication for refractory gastroesophageal reflux disease--a prospective study. Langenbecks Arch Surg. 2008;393:979–984. doi: 10.1007/s00423-008-0294-6. [DOI] [PubMed] [Google Scholar]
- 115.Hassall E. Decisions in diagnosing and managing chronic gastroesophageal reflux disease in children. J Pediatr. 2005;146:S3–12. doi: 10.1016/j.jpeds.2004.11.034. [DOI] [PubMed] [Google Scholar]
- 116.Qadeer MA, Swoger J, Milstein C, Hicks DM, Ponsky J, Richter JE, Abelson TI, Vaezi MF. Correlation between symptoms and laryngeal signs in laryngopharyngeal reflux. Laryngoscope. 2005;115:1947–1952. doi: 10.1097/01.mlg.0000176547.90094.ac. [DOI] [PubMed] [Google Scholar]
- 117.So JB, Zeitels SM, Rattner DW. Outcomes of atypical symptoms attributed to gastroesophageal reflux treated by laparoscopic fundoplication. Surgery. 1998;124:28–32. [PubMed] [Google Scholar]
- 118.Khalil HS, Bridger MW, Hilton-Pierce M, Vincent J. The use of speech therapy in the treatment of globus pharyngeus patients. A randomised controlled trial. Rev Laryngol Otol Rhinol (Bord) 2003;124:187–190. [PubMed] [Google Scholar]
- 119.Millichap F, Lee M, Pring T. A lump in the throat: Should speech and language therapists treat globus pharyngeus? Disabil Rehabil. 2005;27:124–130. doi: 10.1080/09638280400007448. [DOI] [PubMed] [Google Scholar]
- 120.Othmer E, DeSouza C. A screening test for somatization disorder (hysteria) Am J Psychiatry. 1985;142:1146–1149. doi: 10.1176/ajp.142.10.1146. [DOI] [PubMed] [Google Scholar]
- 121.Kroenke K. Efficacy of treatment for somatoform disorders: a review of randomized controlled trials. Psychosom Med. 2007;69:881–888. doi: 10.1097/PSY.0b013e31815b00c4. [DOI] [PubMed] [Google Scholar]
- 122.Cybulska EM. Globus hystericus--a somatic symptom of depression? The role of electroconvulsive therapy and antidepressants. Psychosom Med. 1997;59:67–69. doi: 10.1097/00006842-199701000-00009. [DOI] [PubMed] [Google Scholar]
- 123.Brown SR, Schwartz JM, Summergrad P, Jenike MA. Globus hystericus syndrome responsive to antidepressants. Am J Psychiatry. 1986;143:917–918. doi: 10.1176/ajp.143.7.917. [DOI] [PubMed] [Google Scholar]