Abstract
Objectives
The broad aim of this study was to assess the homogeneity of patients included in trials of non-specific low back pain (NSLBP). To do this, we investigated the consistency and clarity of criteria used to identify and exclude participants with serious pathologies and nerve root compromise in randomized controlled trials, investigating interventions for NSLBP.
Methods
We searched Medline database for randomized controlled trials of low back pain (LBP). published between 2000 and 2009. We then randomly selected and screened trials for inclusion until we had 50 eligible trials. Data were extracted on the criteria used to identify cases of serious conditions (e.g. cancer, fracture) and nerve root involvement.
Results
The majority of papers (35/50) explicitly excluded patients with serious pathology. However, the terminology used and examples given were highly variable. Nerve root involvement was an exclusion criterion in the majority but not all studies. The criteria used for excluding patients with nerve root involvement varied greatly between studies. The most common criteria were ‘motor, sensory or reflex changes’ (nine studies), followed by ‘pain radiating below the knee’ (five studies) and ‘reduced straight leg raise which reproduces leg pain’ (five studies). In half of the included studies, the criteria used, while alluding to nerve root involvement, were not explained adequately for us to determine the types of patients included or excluded.
Discussion
The inconsistent and unclear criteria used to identify cases of serious pathology and nerve root compromise means that published trials of LBP likely include heterogeneous patient populations. This trait limits our ability to make comparisons across trials or pool studies. Standardization and consensus is important for future research.
Keywords: Low back pain, Sciatica, Nerve root compromise, Red flags
Introduction
Low back pain (LBP) guidelines recommend the application of a diagnostic triage in (LBP) management, to differentiate patients with non-specific low back pain (NSLBP) from those with serious pathologies such as fracture and cancer or nerve root involvement.1,2 However, many guidelines do not provide clear or consistent criteria for identifying the patients with serious pathologies or nerve root involvement. The terms used to describe patients with nerve root involvement vary and include radicular syndrome,3 sciatica,4 nerve root compression,5 nerve root <1?show=[to]?>compromise,6 and radiculopathy.7 These terms are generally poorly defined with inconsistent diagnostic criteria between authors. A recent study8 of (LBP) guidelines identified that different guidelines reported different criteria for identifying patients with nerve root involvement.
Clear consistent criteria for identifying those with serious pathology or nerve root involvement are important for future research and interpretation of previous research studies. The types of patients included in trials of (NSLBP) will be determined largely by the criteria used to exclude patients with serious pathology and nerve root involvement. Estimates of the proportion of patients with nerve root involvement vary, but can be as high as 25%.9 Therefore, the criteria for excluding these patients are particularly important, as they are likely to significantly impact on the types of patients included in trials of NSLBP. If studies of NSLBP include different types of patients, then it may limit the ability to pool findings from randomized trials or prognostic studies. For example, patients with nerve root involvement are likely to have different prognoses, and responses to treatment, to those with NSLBP, so it is particularly important to standardize exclusion criteria used to identify those with nerve root involvement.
At present, it is not clear whether studies have used a consistent approach to identify and exclude participants with serious pathologies or nerve root involvement in clinical studies of NSLBP. Therefore, this study investigated the consistency and clarity of criteria used to exclude patients with serious pathologies and nerve root involvement in a random sample of randomized controlled trials (RCTs), investigating interventions for NSLBP. A secondary aim was to describe the range of criteria used to characterize nerve root compromise in trials of NSLBP.
Materials and Methods
Search strategy
We identified a random sample of 50 RCTs published between 2000 and 2009 that evaluated treatment for NSLBP via a search of Medline. The search strategy used keywords describing LBP (low back pain OR low back ache OR sciatica OR lumbago) AND randomized controlled trials (randomized controlled trial OR controlled clinical trial OR Randomized Controlled Trials OR Random Allocation OR Double-Blind Method OR Single-Blind Method OR Animal/not human OR clinical trial OR clinic$ adj25 trial$ OR ((single$ or double$ or treble$ or triple$) adj (mask$ or blind$)) OR random$ OR Cross-Over Studies NOT animal NOT review NOT guidelines). All identified trials were transferred to a reference managing program and allocated a random number generated in Excel. Potential studies were then screened for inclusion starting with the study allocated random number 1. We then continued screening studies in the order of their random number allocation until 50 trials were identified that met the inclusion criteria. Screening was performed by title and abstract and then by full text. All stages of screening were performed by two authors with discrepancies resolved by discussion. These 50 trials formed the data for this study (Fig. 1).
Figure 1.
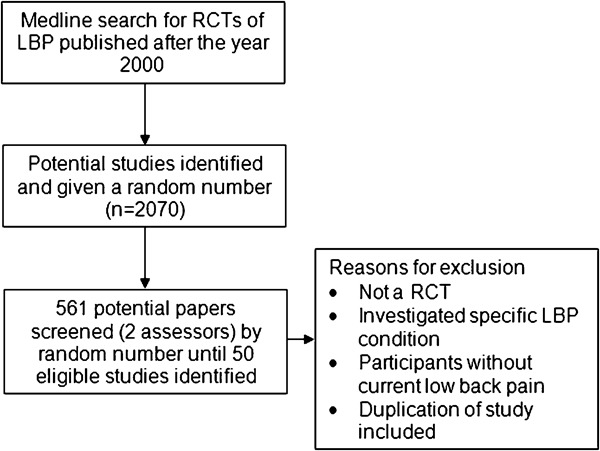
Flow chart: study selection.
Inclusion criteria
Studies were included if they met all of the following criteria:
a RCT;
study population of patients with NSLBP;
investigated an intervention for NSLBP;
published in English or Portuguese.
Data extraction
Data were extracted on the exclusion criteria reported by each trial. These data indirectly described the patients included with NSLBP. Authors reviewed the exclusion criteria of each trial, to ascertain if participants were excluded based on the presence of serious pathologies and/or nerve root involvement and the criteria used. Each trial was assessed against a number of pre-planned criteria for excluding patients with nerve root involvement. The criteria were motor/sensory/reflex changes, unilateral leg pain more intense than back pain, pain radiates below the knee and reduced straight leg raise. Authors determined if criteria used to exclude patients with serious pathologies and nerve root involvement were: (1) clearly stated as exclusion criteria, (2) not stated as exclusion criteria, or (3) if it was ambiguous or unclear.
To further summarize the types of patients included in each of the trials we rated each trial from 1 to 5 based on criteria used for inclusion/exclusion of patients with nerve root involvement. The definitions of each category are described in Table 1.
Table 1. Description of included patients (nerve root involvement).
| Description of included patients | Studies |
| 1. LBP above buttock crease only (explicitly excludes any referred pain below buttocks or neurological signs or symptoms) | Itoh et al.10 |
| Dreiser et al.22 | |
| 2. LBP±somatic type leg pain (excludes pain due to nerve root irritation, i.e. radicular pain, positive straight leg raise, with or without exclusion of those with motor, sensory or reflex changes) | Toda et al.23 |
| Ahlqwist et al.24 | |
| Childs et al.26 | |
| Katz et al.27 | |
| Brinkhaus et al.25 | |
| 3. LBP and any leg pain but excluded those with motor, sensory or reflex changes | Hurwitz et al.28 |
| Eisenburg et al.29 | |
| Hurley et al.30 | |
| Haas et al.31 | |
| Teyhen et al.32 | |
| Brennan et al.33 | |
| 4. LBP and any leg pain or motor, sensory or reflex changes | Hay et al.11 |
| Roberts et al.13 | |
| Penttinen et al.18 | |
| Heymans et al.34 | |
| Kendrick et al.35 | |
| Yip et al.36 | |
| Frerick et al.37 | |
| Lee et al.38 | |
| Grunnesjo et al.39 | |
| Marshall et al.40 | |
| Gabis et al.41 | |
| Chiradejnant et al.42 | |
| 5. Unable to classify due to inadequate information | Tuzun et al.12 |
| Kaapa et al.14 | |
| Hernandez et al.15 | |
| Yakhno et al.16 | |
| Helmhout et al.17 | |
| Helmhout et al.19 | |
| Smeets et al.20 | |
| Inoue et al.21 | |
| Yelland et al.49 | |
| Yip et al.50 | |
| Chrubasik et al.51 | |
| Steenstra et al.52 | |
| Rasmussen et al.53 | |
| Preyde et al.54 | |
| Seferlis et al.55 | |
| Storheim et al.56 | |
| Lierz et al.57 | |
| Bergoldt et al.58 | |
| Hawk et al.59 | |
| Molde Hagen et al.60 | |
| Chrubasik et al.61 | |
| Goldby et al.62 | |
| Snook et al.63 | |
| Prady et al.64 | |
| Leibing et al.65 |
Results
The search identified a total of 2070 potential papers. We screened 561 papers to find 50 that met the inclusion criteria. Papers were excluded on the basis of their design (not RCTs), their target population (not NSLBP) and/or because they failed to investigate a treatment for NSLBP. Included trials investigated a range of interventions including acupuncture, physiotherapy, exercise, manual therapy, massage, and advice.
The majority of papers (35/50, 70%) explicitly excluded patients with serious pathologies. However, the terminology used and examples given were highly variable. For example, terms used included, ‘major trauma or systemic disease’,10 ‘potentially serious pathology’,11 ‘non-mechanical origin’,12 and ‘red flags’.13 Ambiguous phrases which may or may not have been referring to serious pathologies were used in a further nine (18%) papers (see Table 2). Several of the studies we rated as ambiguous, referred to ‘specific’14–19 or exact diagnoses of LBP (Table 2). Six studies (12%) did not report any exclusion criteria for identifying patients with potential serious pathology.
Table 2. Unclear criteria for exclusion of serious pathologies.
| ‘Unclear’ serious pathology exclusion criteria | Study |
| All patients were examined by an orthopaedic surgeon prior to enrolment, and any whose symptoms or findings on imaging indicated the need for medication or surgery or suggested an underlying disease were excluded | Inoue et al.21 |
| Specific back disorder | Kaapa et al.14 |
| Back pain due to fractured vertebrae, herniated or degenerated disks | Hernandez-Reif et al.15 |
| Other serious illness, which could influence on their sleep | Bergholdt et al.58 |
| Specific spinal pathology or symptoms related to other pathologies | Yakhno et al.16 |
| Specific LBP, defined as herniated disc, ankylosing spondylitis, spondylolisthesis or other relevant | Helmhout et al.17 |
| (Back pain non-specific), those with exact diagnoses being excluded | Penttinen et al.18 |
| Presence of severe postural abnormality or neuromuscular disorder, previous diagnosis of pathology (confirmed by magnetic resonance imaging or radiograph) which would contraindicate exercise or manipulation | Marshall et al.40 |
| Specific LBP, defined as herniated disk, ankylosing spondylitis, spondylolisthesis, or other relevant neurologic diseases | Helmhout et al.19 |
While most studies (38/50, 76%) alluded to excluding people with nerve root involvement, the criteria used varied greatly between studies and no single criterion was used by more than nine studies (Fig. 2). The most common criterion was ‘motor, sensory or reflex changes’ (nine studies), followed by ‘pain radiating below the knee’ (five studies) and ‘reduced straight leg raise which reproduces leg pain’ (five studies) (Fig. 2). In half of the included studies, the criteria used, while alluding to nerve root involvement, were not explained adequately for us to determine the types of patients included or excluded (Table 1, category 5). Examples of terms used that we considered ambiguous were sciatic nerve involvement,15 current nerve root pathology,20 other relevant neurologic diseases,19 and leg symptoms.21 Table 1 presents the types of patients included in each study, based on the reported exclusion criteria for nerve root involvement. The studies we could confidently classify included patients with quite different presentations of nerve root involvement. Some studies used very strict criteria where only patients with LBP and no pain extending past the knee were included.10,22 Other studies included patients with leg pain but excluded them, if they had signs of nerve root irritation (i.e. radicular pain, positive straight leg raise, with or without exclusion of those with motor, sensory or reflex changes).23–27 Some studies only excluded patients when motor, reflex or sensory deficits were present.28–33 Other studies did not appear to exclude even those patients with motor, reflex or sensory deficits.11,13,18,34–42
Figure 2.
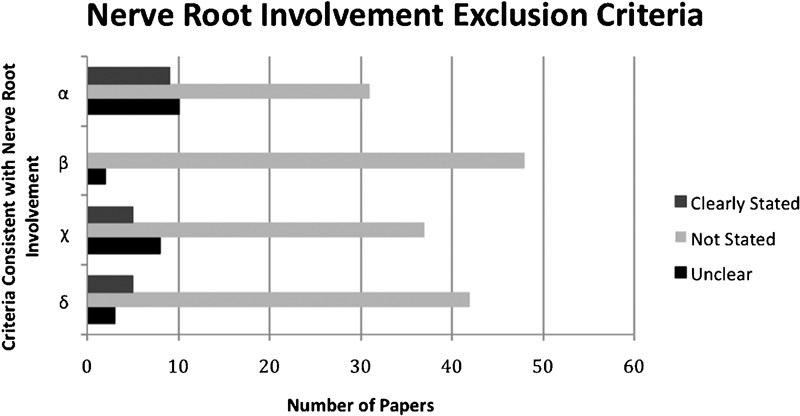
Criteria for exclusion of nerve root involvement (n = 50). α, motor, sensory, reflex changes; β, leg pain greater than back pain; χ, pain radiates below the knee; δ, reduced straight leg raise which reproduces pain.
Discussion
Our review of the literature indicated that the criteria used to identify patients with serious disease and nerve root involvement were not consistent across RCTs. Many of the papers adopted ambiguous or vague exclusion criteria and therefore, failed to clearly outline to the reader what type of patient was included in the trial. Interestingly, there was no consistency between trials regarding the degree of nerve root involvement that warrants exclusion from a trial of NSLBP. This is an important finding as it strongly suggests that trials reported to include patients with NSLBP likely include heterogeneous patients.
In a recent review of 11 different national clinical guidelines for NSLBP, Koes and colleagues1 found that although all of the guidelines recommended the use of a diagnostic triage, a number of them only distinguished NSLBP from LBP caused by a serious pathology. The authors commented that patients with nerve root involvement were variously included in the serious pathology or NSLBP group for management. The findings of Koes et al.1 align with the results of our review, as we found that although the majority of trials excluded those with serious pathologies, they differed markedly in terms of the degree of neurological impairment that would constitute evidence of nerve root involvement.
Although 70% of the trials in this review explicitly excluded LBP caused by serious pathologies, there was little consistency in the terminology or examples used to do so. With such variability, it is unclear if different trials are excluding the same types of patients. One area of confusion identified is the common reference to terms such as ‘specific back disorder’ or an ‘exact diagnosis’. In many cases, it is unclear if authors used these terms to exclude patients with a specific but non-serious spinal pathology (e.g. disc protrusion, disc degeneration, spondylolisthesis) or were they excluding patients with a specific and serious spinal pathology (e.g. metastatic cancer of the spine or a vertebral fracture). Currently, it is unclear where specific spinal pathologies like canal stenosis, spondylolisthesis or disc herniation fit in the diagnostic triage. Until future expert consensus on this issue is reached, we suggest authors avoid terms like specific disorders and clearly explain the condition excluded from a trial.
Haswell et al.8 found that LBP clinical guidelines differed considerably in the criteria they used to diagnose ‘nerve root syndrome’. A number of these guidelines outlined clinical assessment findings like nerve conduction block signs,43–47 a reduced straight leg raise that reproduces pain,44,45,47 unilateral leg pain worse than back pain,44,45,47 as consistent with nerve root syndrome. Our review found the lack of consistency in defining nerve root involvement in guidelines was also present in published trials of NSLBP.
While most studies in our review alluded to excluding patients with nerve root involvement the criteria used varied greatly between studies (Table 1). The result of this is that the patients included in these trials of NSLBP range from those with no pain extending past the buttock to those with neurological signs of motor sensory or reflex changes. Therefore, these papers have potentially included patients with quite different prognoses and responses to the intervention applied. Previous studies show that compared to people with only back pain people with ‘sciatica’ have more persistent and severe pain, greater disability and consume more healthcare resources.9,48 This has important implications for the external validity of different trials and also for systematic reviews which typically pool the results from these studies.
Our results highlight an important issue in NSLBP research, how do we ensure homogeneous study populations between trials? When we consider NSLBP research, the study population of interest is achieved by excluding other causes of LBP, i.e. serious pathologies and/or neurological involvement. Therefore, in order to achieve homogeneous study populations between trials, there is a need for homogenous exclusion criteria for the other causes of low back pain. Consensus expert definition of nerve root involvement and what constitutes serious pathology would be very important in the field.
Limitations
A limitation of this study is that we did not include all trials of NSLBP and instead included a random sample of trials. However, we believe we have gained a representative sample that highlights the inconsistent and unclear nature of the exclusion criteria used in trials of NSLBP. It is possible that some publication bias was introduced as we only conducted a literature search in Medline, and a language bias may have been introduced as we only looked at papers published in English and Portuguese. However, we believe inclusion of studies published in different databases or in different languages would be unlikely to change the key findings. Our study focused on potential differences in patients included in trials of NSLBP due to the exclusion criteria for serious pathologies and nerve root involvement. There are many other important reasons why patients in trials of NSLBP may be heterogeneous between studies. Examples include chronicity of patients, the setting (e.g. primary of secondary care) and the age of participants. While these are clearly important, they were not the focus of the current study.
Conclusion
The current study highlights that the criteria used to exclude patients with serious pathologies and neurological conditions are often not reported or ambiguous. Even when reported the criteria especially for nerve root involvement varies greatly across published trials. There is a clear need for consensus on what constitutes serious pathology and nerve root involvement in patients with LBP.
References
- 1.Koes BW, van Tulder M, Lin CW, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J. 2010;19:2075–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bekkering G, Hendriks H, Koes B, Oostendorp R, Ostelo R, Thomassen J, et al. Dutch physiotherapy guidelines for low back pain. Physiotherapy. 2003;89:82–96 [Google Scholar]
- 3.Luijsterburg PA, Verhagen AP, Ostelo RW, van Os TA, Peul WC, Koes BW. Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Eur Spine J. 2007;16:881–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dahm KT, Brurberg KG, Jamtvedt G, Hagen KB. Advice to rest in bed versus advice to stay active for acute low-back pain and sciatica. Cochrane Database Syst Rev. 2010;15:CD007612. [DOI] [PubMed] [Google Scholar]
- 5.Bokov A, Skorodumov A, Isrelov A, Stupak Y, Kukarin A. Differential treatment of nerve root compression pain caused by lumbar disc herniation applying nucleoplasty. Pain Phys. 2010;13:469–80 [PubMed] [Google Scholar]
- 6.Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 2004;230:583–8 [DOI] [PubMed] [Google Scholar]
- 7.Jensen OK, Nielsen CV, Stengaard-Pedersen K. One-year prognosis in sick-listed low back pain patients with and without radiculopathy. Prognostic factors influencing pain and disability. Spine J. 2010;10:659–75 [DOI] [PubMed] [Google Scholar]
- 8.Haswell K, Gilmour J, Moore B. Clinical decision rules for identification of low back pain patients with neurologic involvement in primary care. Spine (Phila Pa 1976). 2008;33:68–73 [DOI] [PubMed] [Google Scholar]
- 9.Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine (Phila Pa 1976). 2008;33:2464–72 [DOI] [PubMed] [Google Scholar]
- 10.Itoh K, Katsumi Y, Kitakoji H. Trigger point acupuncture treatment of chronic low back pain in elderly patients — a blinded RCT. Acupunc Med. 2004;22:170–7 [DOI] [PubMed] [Google Scholar]
- 11.Hay EM, Dunn KM, Hill JC, Lewis M, Mason EE, Konstantinou K, et al. A randomised clinical trial of subgrouping and targeted treatment for low back pain compared with best current care. The STarT Back Trial Study Protocol. BMC Musculoskelet Disord. 2008;9:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tuzun F, Unalan H, Oner N, Ozguzel H, Kirazli Y, Icagasioglu A, et al. Multicenter, randomized, double-blinded, placebo-controlled trial of thiocolchicoside in acute low back pain. Joint Bone Spine. 2003;70:356–61 [DOI] [PubMed] [Google Scholar]
- 13.Roberts L, Little P, Chapman J, Cantrell T, Pickering R, Langridge J. The back home trial: general practitioner-supported leaflets may change back pain behavior. Spine (Phila Pa 1976). 2002;27:1821–8 [DOI] [PubMed] [Google Scholar]
- 14.Kaapa EH, Frantsi K, Sarna S, Malmivaara A. Multidisciplinary group rehabilitation versus individual physiotherapy for chronic nonspecific low back pain: a randomized trial. Spine (Phila Pa 1976). 2006;31:371–6 [DOI] [PubMed] [Google Scholar]
- 15.Hernandez-Reif M, Field T, Krasnegor J, Theakston H. Lower back pain is reduced and range of motion increased after massage therapy. Int J Neurosci. 2001;106:131–45 [DOI] [PubMed] [Google Scholar]
- 16.Yakhno N, Guekht A, Skoromets A, Spirin N, Strachunskaya E, Ternavsky A, et al. Analgesic efficacy and safety of lornoxicam quick-release formulation compared with diclofenac potassium: randomised, double-blind trial in acute low back pain. Clin Drug Investig. 2006;26:267–77 [DOI] [PubMed] [Google Scholar]
- 17.Helmhout PH, Harts CC, Staal JB, de Bie RA. Rationale and design of a multicenter randomized controlled trial on a ‘minimal intervention’ in Dutch army personnel with nonspecific low back pain [ISRCTN19334317]. BMC Musculoskelet Disord. 2004;5:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Penttinen J, Nevala-Puranen N, Airaksinen O, Jaaskelainen M, Sintonen H, Takala J. Randomized controlled trial of back school with and without peer support. J Occup Rehabil. 2002;12:21–9 [DOI] [PubMed] [Google Scholar]
- 19.Helmhout PH, Harts CC, Viechtbauer W, Staal JB, de Bie RA. Isolated lumbar extensor strengthening versus regular physical therapy in an army working population with nonacute low back pain: a randomized controlled trial. Arch Phys Med Rehabil. 2008;89:1675–85 [DOI] [PubMed] [Google Scholar]
- 20.Smeets RJ, Vlaeyen JW, Kester AD, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J Pain. 2006;7:261–71 [DOI] [PubMed] [Google Scholar]
- 21.Inoue M, Kitakoji H, Ishizaki N, Tawa M, Yano T, Katsumi Y, et al. Relief of low back pain immediately after acupuncture treatment — a randomised, placebo controlled trial. Acupunct Med. 2006;24:103–8 [DOI] [PubMed] [Google Scholar]
- 22.Dreiser RL, Marty M, Ionescu E, Gold M, Liu JH. Relief of acute low back pain with diclofenac-K 12.5 mg tablets: a flexible dose, ibuprofen 200 mg and placebo-controlled clinical trial. Int J Clin Pharmacol Ther. 2003;41:375–85 [DOI] [PubMed] [Google Scholar]
- 23.Toda Y. Impact of waist/hip ratio on the therapeutic efficacy of lumbosacral corsets for chronic muscular low back pain. J Orthop Sci. 2002;7:644–9 [DOI] [PubMed] [Google Scholar]
- 24.Ahlqwist A, Hagman M, Kjellby-Wendt G, Beckung E. Physical therapy treatment of back complaints on children and adolescents. Spine (Phila Pa 1976). 2008;33:E721–7 [DOI] [PubMed] [Google Scholar]
- 25.Brinkhaus B, Witt CM, Jena S, Linde K, Streng A, Wagenpfeil S, et al. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med. 2006;166:450–7 [DOI] [PubMed] [Google Scholar]
- 26.Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004;141:920–8 [DOI] [PubMed] [Google Scholar]
- 27.Katz N, Rodgers DB, Krupa D, Reicin A. Onset of pain relief with rofecoxib in chronic low back pain: results of two four-week, randomized, placebo-controlled trials. Curr Med Res Opin. 2004;20:651–8 [DOI] [PubMed] [Google Scholar]
- 28.Hurwitz EL, Morgenstern H, Yu F. Satisfaction as a predictor of clinical outcomes among chiropractic and medical patients enrolled in the UCLA low back pain study. Spine (Phila Pa 1976). 2005;30:2121–8 [DOI] [PubMed] [Google Scholar]
- 29.Eisenberg DM, Post DE, Davis RB, Connelly MT, Legedza AT, Hrbek AL, et al. Addition of choice of complementary therapies to usual care for acute low back pain: a randomized controlled trial. Spine (Phila Pa 1976). 2007;32:151–8 [DOI] [PubMed] [Google Scholar]
- 30.Hurley DA, McDonough SM, Dempster M, Moore AP, Baxter GD. A randomized clinical trial of manipulative therapy and interferential therapy for acute low back pain. Spine (Phila Pa 1976). 2004;29:2207–16 [DOI] [PubMed] [Google Scholar]
- 31.Haas M, Groupp E, Kraemer DF. Dose-response for chiropractic care of chronic low back pain. Spine J. 2004;4:574–83 [DOI] [PubMed] [Google Scholar]
- 32.Teyhen DS, Miltenberger CE, Deiters HM, Del Toro YM, Pulliam JN, Childs JD, et al. The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J Orthop Sports Phys Ther. 2005;35:346–55 [DOI] [PubMed] [Google Scholar]
- 33.Brennan GP, Fritz JM, Hunter SJ, Thackeray A, Delitto A, Erhard RE. Identifying subgroups of patients with acute/subacute ‘nonspecific’ low back pain: results of a randomized clinical trial. Spine (Phila Pa 1976). 2006;31:623–31 [DOI] [PubMed] [Google Scholar]
- 34.Heymans MW, de Vet HCW, Bongers PM, Knol DL, Koes BW, van Mechelen W. The effectiveness of high-intensity versus low-intensity back schools in an occupational setting: a pragmatic randomized controlled trial. Spine (Phila Pa 1976). 2006;31:1075–82 [DOI] [PubMed] [Google Scholar]
- 35.Kendrick D, Fielding K, Bentley E, Miller P, Kerslake R, Pringle M. The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial. Health Technol Assess. 2001;5:1–69 [DOI] [PubMed] [Google Scholar]
- 36.Yip YB, Tse HM, Wu KK. An experimental study comparing the effects of combined transcutaneous acupoint electrical stimulation and electromagnetic millimeter waves for spinal pain in Hong Kong. Complement Ther Clin Pract. 2007;13:4–14 [DOI] [PubMed] [Google Scholar]
- 37.Frerick H, Keitel W, Kuhn U, Schmidt S, Bredehorst A, Kuhlmann M. Topical treatment of chronic low back pain with a capsicum plaster. Pain. 2003;106:59–64 [DOI] [PubMed] [Google Scholar]
- 38.Lee PB, Kim YC, Lim YJ, Lee CJ, Choi SS, Park SH, et al. Efficacy of pulsed electromagnetic therapy for chronic lower back pain: a randomized, double-blind, placebo-controlled study. J Int Med Res. 2006;34:160–7 [DOI] [PubMed] [Google Scholar]
- 39.Grunnesjo MI, Bogefeldt JP, Svardsudd KF, Blomberg SI. A randomized controlled clinical trial of stay-active care versus manual therapy in addition to stay-active care: functional variables and pain. J Manipulative Physiol Ther. 2004;27:431–41 [DOI] [PubMed] [Google Scholar]
- 40.Marshall P, Murphy B. Self-report measures best explain changes in disability compared with physical measures after exercise rehabilitation for chronic low back pain. Spine (Phila Pa 1976). 2008;33:326–38 [DOI] [PubMed] [Google Scholar]
- 41.Gabis L, Shklar B, Geva D. Immediate influence of transcranial electrostimulation on pain and beta-endorphin blood levels: an active placebo-controlled study. Am J Phys Med Rehabil. 2003;82:81–5 [DOI] [PubMed] [Google Scholar]
- 42.Chiradejnant A, Maher CG, Latimer J, Stepkovitch N. Efficacy of ‘therapist-selected’ versus ‘randomly selected’ mobilisation techniques for the treatment of low back pain: a randomised controlled trial. Australian J Physiother. 2003;49:233–41 [DOI] [PubMed] [Google Scholar]
- 43.Spitzer WO, LeBlanc FE, Dupuis M. Scientific approach to the assess- ment and management of activity-related spinal disorders. Spine (Phila Pa 1976). 1987;12(7 Suppl):S1–59 [PubMed] [Google Scholar]
- 44.Bigos S, Bowyer O, Braen G. Acute low back problems in adults: clinical practice guideline no. 14. AHCPR publication no. 95-0642. Services USDoHaH, editor. Rockville (MD): Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services; 1994 [Google Scholar]
- 45.Waddell G, Feder G, McIntosh A. Clinical guidelines for the management of acute low back pain. London: Royal College of General Practitioners; 1996 [Google Scholar]
- 46.Danish Institute for Health Technology Assessment Low back pain: frequency, management and prevention from HTA perspective. Copenhagen: DIHTA; 1999 [Google Scholar]
- 47.Nachemson A, Jonsson E. Neck and back pain: the scientific evidence of causes, diagnosis and treatment. Philadelphia, PA: Lippincott Williams & Wilkins; 2000 [Google Scholar]
- 48.Selim AJ, Ren XS, Fincke G, Deyo RA, Rogers W, Miller D, et al. The importance of radiating leg pain in assessing health outcomes among patients with low back pain. Results from the Veterans Health Study. Spine (Phila Pa 1976). 1998;23:470–4 [DOI] [PubMed] [Google Scholar]
- 49.Yelland MJ, Glasziou PP, Bogduk N, Schluter PJ, McKernon M. Prolotherapy injections, saline injections, and exercises for chronic low-back pain: a randomized trial. Spine (Phila Pa 1976). 2004;29:9–16 [DOI] [PubMed] [Google Scholar]
- 50.Yip YB, Tse SH. The effectiveness of relaxation acupoint stimulation and acupressure with aromatic lavender essential oil for non-specific low back pain in Hong Kong: a randomised controlled trial. Complement Ther Med. 2004;12:28–37 [DOI] [PubMed] [Google Scholar]
- 51.Chrubasik S, Kunzel O, Black A, Conradt C, Kerschbaumer F. Potential economic impact of using a proprietary willow bark extract in outpatient treatment of low back pain: an open non-randomized study. Phytomedicine. 2001;8:241–51 [DOI] [PubMed] [Google Scholar]
- 52.Steenstra IA, Anema JR, Bongers PM, de Vet HCW, van Mechelen W. Cost effectiveness of a multi-stage return to work program for workers on sick leave due to low back pain, design of a population based controlled trial [ISRCTN60233560]. BMC Musculoskelet Disord. 2003;4:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rasmussen J, Laetgaard J, Lindecrona AL, Qvistgaard E, Bliddal H. Manipulation does not add to the effect of extension exercises in chronic low-back pain (LBP). A randomized, controlled, double blind study. Joint Bone Spine. 2008;75:708–13 [DOI] [PubMed] [Google Scholar]
- 54.Preyde M. Effectiveness of massage therapy for subacute low-back pain: a randomized controlled trial. CMAJ. 2000;162:1815–20 [PMC free article] [PubMed] [Google Scholar]
- 55.Seferlis T, Lindholm L, Nemeth G. Cost-minimisation analysis of three conservative treatment programmes in 180 patients sick-listed for acute low-back pain. Scand J Prim Health Care. 2000;18:53–7 [DOI] [PubMed] [Google Scholar]
- 56.Storheim K, Brox JI, Holm I, Koller AK, Bo K. Intensive group training versus cognitive intervention in sub-acute low back pain: short-term results of a single-blind randomized controlled trial. J Rehabil Med. 2003;35:132–40 [DOI] [PubMed] [Google Scholar]
- 57.Lierz P, Gustorff B, Markow G, Felleiter P. Comparison between bupivacaine 0.125% and ropivacaine 0.2% for epidural administration to outpatients with chronic low back pain. Eur J Anaesthesiol. 2004;21:32–7 [DOI] [PubMed] [Google Scholar]
- 58.Bergholdt K, Fabricius RN, Bendix T. Better backs by better beds? Spine (Phila Pa 1976). 2008;33:703–8 [DOI] [PubMed] [Google Scholar]
- 59.Hawk C, Long CR, Rowell RM, Gudavalli MR, Jedlicka J. A randomized trial investigating a chiropractic manual placebo: a novel design using standardized forces in the delivery of active and control treatments. J Altern Complement Med. 2005;11:109–17 [DOI] [PubMed] [Google Scholar]
- 60.Hagen MoldeE, Grasdal A, Eriksen HR. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain: a 3-year follow-up study. Spine (Phila Pa 1976). 2003;28:2309–15 [DOI] [PubMed] [Google Scholar]
- 61.Chrubasik S, Kunzel O, Model A, Conradt C, Black A. Treatment of low back pain with a herbal or synthetic anti-rheumatic: a randomized controlled study. Willow bark extract for low back pain. Rheumatology (Oxford). 2001;40:1388–93 [DOI] [PubMed] [Google Scholar]
- 62.Goldby LJ, Moore AP, Doust J, Trew ME. A randomized controlled trial investigating the efficiency of musculoskeletal physiotherapy on chronic low back disorder. Spine (Phila Pa 1976). 2006;31:1083–93 [DOI] [PubMed] [Google Scholar]
- 63.Snook SH, Webster BS, McGorry RW. The reduction of chronic, nonspecific low back pain through the control of early morning lumbar flexion: 3-year follow-up. J Occup Rehabil. 2002;12:13–9 [DOI] [PubMed] [Google Scholar]
- 64.Prady SL, Thomas K, Esmonde L, Crouch S, MacPherson H. The natural history of back pain after a randomised controlled trial of acupuncture vs usual care — long term outcomes. Acupunct Med. 2007;25:121–9 [DOI] [PubMed] [Google Scholar]
- 65.Leibing E, Leonhardt U, Koster G, Goerlitz A, Rosenfeldt JA, Hilgers R, et al. Acupuncture treatment of chronic low-back pain — a randomized, blinded, placebo-controlled trial with 9-month follow-up. Pain. 2002;96:189–96 [DOI] [PubMed] [Google Scholar]


