Abstract
Objectives
Upper limb neurodynamic testing (ULNT) can be used clinically to assist in identifying neural tissue involvement in patients with upper quarter pain and dysfunction. Consideration for scapular positioning is a crucial component of ULNT standardization, as variations in positioning may dramatically impact sensory and motor responses. This study aimed to determine if there was a meaningful difference in test outcomes when the ULNT was performed in alternative scapular positions.
Methods
This cross-sectional study included 40 asymptomatic individuals. Repeated ULNT testing was performed on the dominant limb with the scapula blocked in neutral (ULNTb) and in scapular depression (ULNTd). Sensory responses, muscle activity, and range of motion outcomes were compared between the two test variations.
Results
Pre-positioning in scapular depression (ULNTd) led to reduced elbow extension range of motion, provoked greater upper trapezius muscle activity and an earlier onset and broader area of sensory responses compared to ULNTb.
Discussion
During ULNTb, the limbs were taken further into range and elicited reduced muscle activation and more localized sensory response providing a less vigorous version of the test. This study demonstrates that scapular positioning has a meaningful impact on ULNT test outcomes in healthy, asymptomatic individuals. The ULNTd can be considered a more vigorous version that may be appropriate when the cervical motions commonly utilized for structural differentiation are limited or contraindicated.
Keywords: Mechanosensitivity, Neurodynamics, Range of motion
Introduction
The brachial plexus tension test was first introduced by Elvey,1 and was later referred to as the upper limb nerve tension test by Kenneally et al.2 Shacklock3 and Butler4,5 further refined the testing procedures and expanded our understanding of the construct being examined, beyond merely tensioning the nervous system; introducing the term upper limb neurodynamic test (ULNT). The ULNT aids in determining whether the nervous system is responsible for symptoms and mobility impairments seen in patients with upper extremity dysfunctions.5,6 The test involves gradually applying increasing amounts of elongation to the neural pathway by sequential additions of limb movements. The sequence of limb movements in one of the most commonly utilized ULNT versions includes manually stabilizing the scapula, followed by passive shoulder abduction, wrist and finger extension, forearm supination, shoulder external rotation, and lastly elbow extension.4–6
Variations have existed among ULNT methods since its inception, including scapular positioning and stabilization. However, consistency in the position and stabilization of the scapula is paramount for determining accurate test outcomes. Biomechanically, it has been suggested that scapular depression increases tension on the C5 and C6 spinal nerves and the lateral cord of the brachial plexus,7,8 as well as the median nerve in the forearm.9 It logically follows that variations in scapular position would apply differing degrees of tension to the neural pathway and would likely alter the test outcomes.
The original definitions of scapular positioning for the ULNT include the clinician controlling scapular elevation by blocking in a ‘neutral’ scapular position.1,2,4–6 It was suggested that the examiner achieve this goal by leaning a fist into the plinth while applying a caudal force with the forearm to the point of onset of tissue resistance to movement.5 Unfortunately, current descriptions in many research studies and textbooks remain vague or inadequately defined. The term, ‘scapular depression’ is often used but the interpretation of the position is left up to the reader or requires examining the original references.10–13 Others use the description, ‘slight scapular depression’, but again the position is not clearly explained.14,15 Collectively, the exact depression methodology and position of the scapula is frequently insufficiently described, preventing clinicians from having a standardized version to utilize with their patients and researchers from accurately replicating the testing protocols.
Research studies investigating outcomes from the ULNT have used multiple scapular positioning and fixation methodologies. Pressure sensor protocols applied with inferiorly directed pressure to the scapula have utilized an increase from 20 to 40 mmHg,13,15–17 referencing the original protocol by Edgar et al.18 This protocol was derived from attempts to consistently replicate positioning the scapula inferiorly to the first onset of resistance to movement and demonstrated good consistency between examiners.18 Alternatively, examiners have measured the force using a load cell, where 30 N initial caudal pressure was applied to create a ‘gentle depression’ in an effort to ‘neutralize the elevation of the shoulder girdle caused by abduction of the arm’.19–21 In comparison, shoulder positioning has been determined based on a change in distance of 1.5 inches (3.81 cm) of depression.9 Lastly, many studies have utilized manual stabilization of the scapula to either prevent scapular elevation,22 position in ‘slight’ or ‘gentle’ scapular depression,14,23,24 position in ‘scapular depression’,10,25 or utilized the ULNT without any specific description of scapular positioning.26–29 It is clear that significant variations still exist in the description and achievement of scapular positioning.
While current literature has utilized some degree of scapular depression or scapular blocking in neutral, there are no studies to date in which both positions have been tested in the same individuals. Therefore, the primary purpose of this study was to determine the differences in ULNT outcomes in asymptomatic individuals between scapular depression and scapular blocking. We expected to find that pre-positioning in scapular depression would provoke earlier sensory responses in a broader area of the limb during the ULNT sequence. Additionally, we anticipated that scapular depression will trigger a greater increase in local muscle activity and subsequently reduce the available elbow extension range of motion compared to blocking the scapula in neutral.
Methods
Participants
This cross-sectional study included a convenience sample of 40 participants. Participants were recruited through postings online and at local academic and medical center campuses. The inclusion criteria required the participant be at least 18 years old and have full pain free range of motion of bilateral shoulders, elbows, wrists, hands, and cervical spine. Exclusion criteria included presence of current or recent (more than 3 consecutive days in the last 6 months) neck or upper extremity pain, diagnoses of peripheral neuropathy, diabetes mellitus, carpal tunnel syndrome, complex regional pain syndrome, upper extremity or cervical spine surgeries, drug or alcohol abuse, and chemotherapy within the last year. The Samuel Merritt University institutional review board approved this study and assured the ethical treatment of participants. Participants submitted written informed consent prior to testing. Prior to physical examination procedures each participant completed the modified Baecke questionnaire: a self-report measure of activity level with work, sports and leisure activities.30
Equipment set-up
A Myosystem 1400A unit was used in conjunction with MR-XP 1.07 Master Edition software for data collection (Noraxon USA Inc., Scottsdale, AZ, USA). The sampling frequency was 1000 Hz with a high pass bandwidth filter of 500 Hz. Surface electrodes (1 cm circular bipolar Ag/AgCl with a 2 cm inter-electrode distance; Noraxon USA Inc.) were placed on the upper trapezius, biceps brachii, and forearm wrist and finger flexor group to capture electromyographic (EMG) data consistent with surface electromyography for the non-invasive assessment of muscles guidelines.31 Specifically, the electrode placement was half-way between the acromion and C7 spinous process for the upper trapezius, the distal third of the line between the acromion and cubital fossa for the biceps brachii, and the proximal third of the line between the medial epicondyle and wrist crease for the forearm flexor muscle group. The reference electrode was placed over the C7 spinous process. A twin-axis electrogoniometer (Noraxon USA Inc.) was used to record elbow range of motion and was placed medially across the elbow joint with the proximal end in line with the humerus and the distal end in line with the ulnar styloid process. Full elbow extension to neutral was defined as 180°. A hand-held trigger was used to identify the first onset of any sensory response during the last phase of the ULNT (elbow extension). A hand brace was used to keep the fingers in neutral and the carpometacarpal joint of the thumb fully extended throughout testing while allowing full wrist extension from a neutral position.
Testing protocol
The participant was positioned in supine in a neutral, anatomical position. A standard 2.5 cm thick foam pillow was used to support the participant’s head during testing. Testing was performed on the participant’s dominant limb as determined by the hand used for writing. The testing sequence began with one of two passive scapular positions based on a previously determined random order. This included either scapular blocking in neutral (ULNTb), which involved placing the scapula in a neutral position by applying a caudal force with the tester’s forearm until the first onset of resistance to movement was felt (R1), or scapular depression (ULNTd), designated by the end range position (R2) determined by the tester. Randomization of order was utilized to help control for the effect of repeated testing and allow comparisons between the two test variations. This was then followed, in order, by passive shoulder abduction, wrist extension, forearm supination, shoulder external rotation, and finally elbow extension. Each motion was either taken to the end range of motion (R2) or to the onset of any sensory response, if any was provoked, including but not limited to stretch, pulling, tension, pain, tingling, or numbness. One practice trial was performed for each ULNT version prior to repeating for testing purposes. Two-minute breaks were given between each trial.
Data processing
EMG data were rectified using a root mean squared conversion with a 50-millisecond interval and then normalized to resting muscle activity levels recorded in supine with limbs supported prior to ULNT procedure. EMG data are reported as percent increases above resting values. The authors believe this comparison is more appropriate for passive testing procedures where comparisons to resting muscle tone are more relevant, instead of comparing to maximal voluntary isometric contractions which would be more appropriate for actively performed movements. Muscle activation was determined using a threshold of three standard deviations (SDs) above the mean resting values as has been previously utilized for EMG analysis.15,32 Elbow extension range of motion was calculated from a 100-millisecond window centered at the moment the participant indicated a sensory response with this movement. This measure was utilized to indicate the relative flexibility during the ULNT as this was the final limb motion for each test variation. Reliability analysis was performed on a subset of participants (n = 6) using elbow extension measured during the practice trial and measurement trial for both ULNTb and ULNTd. Intraclass correlation coefficients (2,1) were calculated to examine measurement consistency. For analysis purposes, sensory responses were coded as occurring in the arm (spanning the acromion process to the crease in antecubital fossa), forearm (spanning the crease in antecubital fossa to the distal wrist crease), and hand (spanning the distal wrist crease into the hand).
Statistical analysis
All statistical analyses were performed using SPSS software, version 18.0 (IBM Corporation, Somers, NY, USA). The means and SDs are reported for continuous variables and frequencies are reported for dichotomous and categorical data. Paired t-tests were used for between-test comparisons, and repeated measures analysis was utilized for within test comparisons. Repeated measures general linear regression analysis was utilized to determine the specific impact of test variation and testing order on elbow extension range of motion. Non-parametric analysis was utilized for sensory response variables due to non-normal distributions of data. Alpha was set at 0.05. Power analysis revealed that with a sample of 40, alpha of 0.05, and power of 80%, we would have the ability to detect a 4.5° difference in elbow extension between ULNTb and ULNTd with an SD of 10°.
Results
Demographics
The participant’s demographic characteristics are presented in Table 1. There were no significant differences between the male (n = 9) and female (n = 31) participants with the following exceptions. The males were on average slightly taller (0.08 m, P<0.01) and weighed more (12.29 kg, P = 0.04) than the female participants. However, since there was no difference in body mass index between these subgroups, male and female participants were grouped together for further analysis. The modified Baecke questionnaire scores indicate that these participants were moderately active in all three subscales (work, sports, and leisure), based on the average total score of 8.58 on a scale of 3 as the lowest and 15 as the highest activity rating.30,33
Table 1. Demographics.
| Demographics | Total group (n = 40) |
| Hand dominance (writing) | 85% right/15% left |
| Age (years) | 33.98 (11.14) |
| Height (m) | 1.67 (0.08) |
| Weight (kg) | 69.85 (15.75) |
| BMI (kg/m2) | 24.94 (5.21) |
| Modified Baecke questionnaire | |
| Work subscale | 2.47 (0.61) |
| Sports subscale | 3.28 (0.83) |
| Leisure subscale | 2.82 (0.53) |
| Total score | 8.58 (1.50) |
Note: BMI, body mass index.
ULNT testing
Elbow extension range of motion
ICC2,1 values for elbow extension measurements were 0.93 (95% CI: 0.60–0.99) during ULNTb and 0.92 (95% CI: 0.56–0.99) during ULNTd demonstrating excellent reliability of repeated measurements for both ULNT versions. The range of elbow extension at the end of the test sequence is presented in Fig. 1 for ULNTb compared to ULNTd. Average elbow extension was 144.7° (19.1° SD) during ULNTb and 139.5° (20.6° SD) during ULNTd. Of note, all of the participants in the lower quartile for elbow extension range (n = 10) were females (130° or less). There was greater elbow extension during ULNTb compared to ULNTd by an average of 5.3° (10.9° SD, P<0.01). Further comparison shows that 72.5% (29/40) of participants had more elbow extension during ULNTb (above y = x line) while 27.5% (11/40) had more elbow extension during ULNTd (below y = x line) (Fig. 1). Interestingly, the testing order influenced the difference in elbow extension between ULNTb and ULNTd (P = 0.03). Repeated measures general linear analysis revealed that the test variation (ULNTb or ULNTd) explained 29% of the variance (eta2) in elbow extension range of motion (P<0.01), while testing order only explained 12% of the variance (eta2) (P = 0.03).
Figure 1.
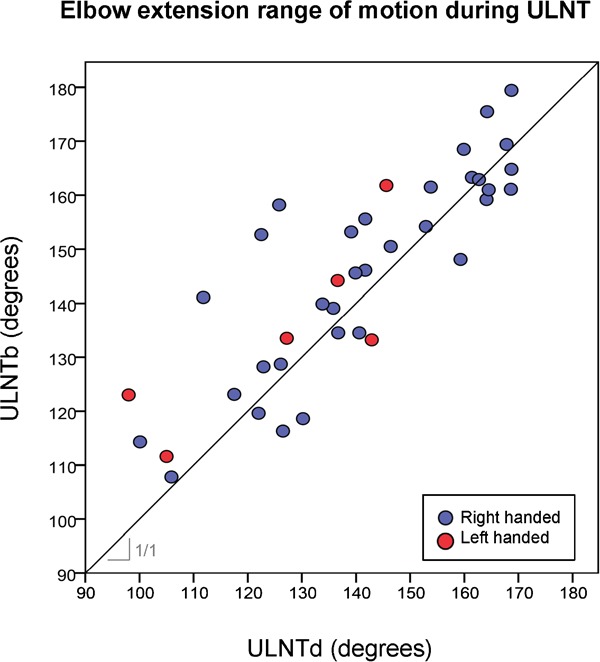
Elbow extension range of motion at the end of the ULNT test sequence for ULNTb (y-axis) and ULNTd (x-axis). Line represents the absolute y = x condition indicated by the slope 1/1. Data points above the line are indicative of more elbow extension range during ULNTb compared to ULNTd. Data points below the y = x line are indicative of less elbow extension range during ULNTb compared to ULNTd. Right handed individuals are represented with blue circles and left handed individuals are represented with red circles. Full elbow extension is defined as 180°.
Muscle activity
Data for EMG were not able to be calculated for two participants due to equipment malfunction which resulted in the following EMG analysis being performed in 38 participants. There was no difference in muscle activity when lying at rest in supine with the limbs supported or with scapular positioning for the upper trapezius (P = 0.19), biceps brachii (P = 0.99), and flexor muscles (P = 0.81) between the ULNTb and ULNTd. Figure 2 demonstrates the muscle activity at the end of the testing sequences (i.e. elbow extension) including the average threshold for muscle activation (three SD above resting levels).
Figure 2.
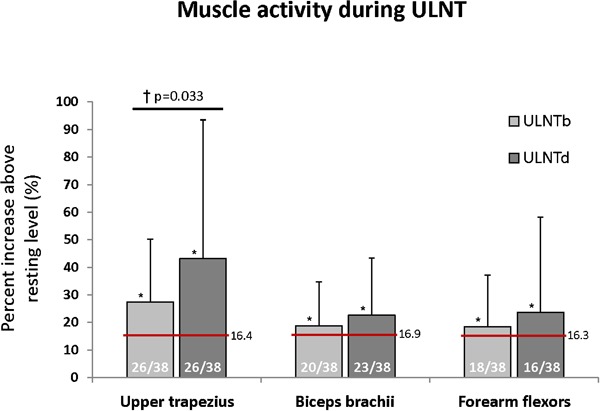
Muscle activity during ULNT is represented as percent increase above resting levels with error bars representing the SD. The numbers within each bar graph represent the frequency of muscle activity above the threshold (three SDs above resting muscle activity level). The horizontal red line indicates the average threshold for muscle activation. Asterisk (*) indicates significant increase muscle activity above resting levels and cross (†) indicates significant differences between ULNTb and ULNTd (P<0.05).
During ULNTb, the activity of the upper trapezius muscle increased by 27.4% (22.8% SD) above resting levels (P<0.01). In comparison, during ULNTd, the upper trapezius increased to 43.2% (50.3% SD) of resting levels (P <0.01). The difference between activation during ULNTb and ULNTd was 15.9% (44.2% SD, P = 0.03). However, not all participants had an increase in upper trapezius muscle activity. When using the conservative threshold for muscle activation (three SDs above resting levels), only 68.4% of participants (26/38) had upper trapezius muscle activation at the end of the ULNTb and ULNTd sequence (Fig. 2). This means that 12 individuals (31.6%) did not have an upper trapezius muscle response in each of the testing variations. It should be noted that the ULNTd did not produce more participants with an upper trapezius response compared to ULNTb, but instead created a larger magnitude of upper trapezius activation above resting levels in the same percentage of participants. Both the biceps brachii and forearm flexor muscles had significantly increased muscle activity above resting levels at the end of the testing sequences (P<0.01), but there was no difference between ULNTb and ULNTd (biceps brachii, P = 0.40; forearm flexors, P = 0.25) (Fig. 2). Biceps brachii muscle activation was only present in 52.6% of participants (20/38) at the end of the ULNTb and 60.5% (23/38) for ULNTd. In comparison, even fewer participants had forearm flexor muscle activation at the end of the ULNTb (47.4%, 18/38) and ULNTd (42.1%, 16/38) (Fig. 2).
Sensory response
There were no reports of sensory responses when lying at rest in supine with the limbs supported prior to testing or with scapular positioning in either block or depression. During the ULNTd version, there were significantly more participants who experienced sensory responses during shoulder abduction (P = 0.02) and during wrist extension (P = 0.02) compared to during ULNTb (Fig. 3). The first onset of sensory response occurred most frequently (mode) with shoulder abduction during ULNTd compared to with wrist extension during ULNTb. The average onset was significantly earlier for ULNTd compared to ULNTb (P<0.01); however, the median onset of sensory response was during wrist extension for both test variations. These group differences are small, and individual participant analysis revealed that only 10 participants (25.0%) had an earlier onset of sensory response during ULNTd compared to ULNTb. No participants had earlier onset of sensory responses with ULNTb compared to ULNTd.
Figure 3.
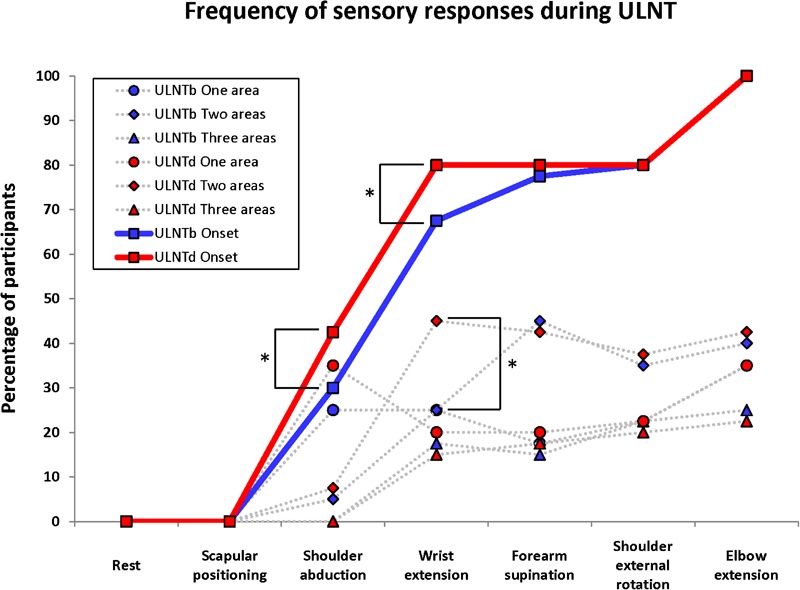
Sensory responses during ULNT are presented. Blue data points represent the ULNTb and red data points represent the ULNTd. The onsets of sensory responses are indicated by boxes with a solid line showing the cumulative percentages throughout the testing sequences. The number of areas within the limb that were reported to have sensory responses is presented as circles (one area reported), diamonds (two areas reported) and triangles (all three areas reported) with the dashed line. Asterisks (*) indicate significant differences between ULNTb and ULNTd.
When considering the location of sensory responses in the limb, the frequency of sensory responses felt in the arm, forearm, and hand did not differ between the two test versions at any stage of testing. Sensory responses in the arm were most frequently provoked during shoulder abduction and then were often increased with wrist extension. Sensory responses in the forearm were most often provoked during wrist extension and frequently increased during forearm supination and elbow extension. In the hand, sensory responses were most frequently provoked during wrist extension and often increased during forearm supination and elbow extension. When analyzing sensory responses reported in multiple areas, there was an increase in participants that reported sensory responses in two simultaneous locations (most often the forearm and hand) with wrist extension during ULNTd (45.0%) compared to ULNTb (25.0%) (P = 0.01). This difference was only apparent at this stage of the ULNT procedures and was not evident later in the test sequence (Fig. 3). There was no statistical difference in the frequency of the sensory responses with a quality descriptor associated with neurogenic sources,34,35 such as numbness, tingling or pins and needles (35.0% during ULNTb and 40.0% during ULNTd, P = 0.41), or those associated with non-neurogenic sources such as stretch, tightness, tension or pulling (87.5% during both versions, P = 1.00).
Discussion
Scapular depression to the end of range (R2) created meaningful alterations in range of motion and sensory and motor responses during the ULNT compared to blocking the scapula in a neutral position. Specifically, the ULNTd reduced elbow extension range of motion by an average of 5° (reduced in ∼75% of participants) and increased the response of upper trapezius muscle activation by >50% at the end of the test sequence compared to ULNTb. Additionally, the ULNTd increased the frequency of earlier sensory responses and broadened the sensory response being provoked at an earlier time in the test sequence compared to the ULNTb. These findings suggest the impacts of scapular positioning are not negligible and thus should be an important part of test standardization.
The authors recommend utilizing the ULNTb as the ‘base’ test instead of the ULNTd version because the former is a less provocative version that allows the healthy limb to be taken further into the testing sequence before sensory responses are provoked and induces more localized sensations with less upper limb muscular activation. Since sensory responses were provoked in all healthy individuals with the less vigorous version (ULNTb), the addition of more stress to the nervous system through scapular depression is not a necessary addition to the base ULNT. The findings of the present study support the use of early descriptions of scapular positioning in neutral to block scapular elevation provided by the originators and developers of the ULNT.1–5
Since pre-positioning in scapular depression is thought to increase loading on the nervous system, one potential use of the ULNTd could be as a ‘sensitized’ version to compare to the base test (ULNTb). Previous literature has found that pre-positioning the cervical spine in contralateral side bending as a ‘sensitized’ ULNT test, decreases the elbow extension range of motion19,36 and increases upper trapezius muscle activation16 compared to a ULNT with the cervical spine positioned in neutral. When cervical motions are contraindicated or limited due to local pain or hypomobility, scapular depression could be considered an alternative. The normal magnitude and variations in test outcomes between ULNTb and ULNTd in healthy individuals have now been established for future comparisons to patients with upper quarter and neck symptoms.
It is important to note that the testing order did impact the range of motion outcome. This implicates that repeated testing does have an effect on range of motion with ULNT. While this finding is statistically significant, it is not likely very clinically relevant as it only explains 12% of the variability in range of motion during these ULNT procedures, while in comparison, the specific test variation (ULNTb or ULNTd) explained ∼2.5 times as much variance (29%). Furthermore, the frequency of participants experiencing more range of motion with ULNTd compared to ULNTb (below the x = y line in Fig. 1) was essentially equal between the two testing orders (five received ULNTb first and six received ULNTd first). Previous literature has noted a small trend of increasing range of motion with repeated ULNT trials, but this trend was not statistically significant in this smaller sample (n = 25).19 With this potential confounding variable, the utilization of randomized testing order in the present study was critical to counter balance this order effect as has been done previously with ULNT research.19,36
The increased activation in local musculature seen during ULNT has been described as a protective response of the nervous system to limit tensile forces acting on the neural tissue.15,16,37 A previous study found sequential limb positioning increased muscle activity in the upper trapezius above baseline when taken to the onset of pain in 20 asymptomatic males during a version similar to ULNTb in the present study.16 An additional study examining a similar ULNTb variant in 20 asymptomatic males and females, found an increase in muscle activation in 55–90% of participants within the upper trapezius, 30–50% within the biceps brachii, and 45–55% within the triceps brachii.15 Lastly, a recent study found increased upper and middle trapezius, pectoralis major, biceps brachii, brachialis, triceps brachii, and flexor carpi radialis muscle activity when the test was taken to the onset of pain during a similar version of the ULNTb.37 We found similar muscle activation during ULNTb in the upper trapezius (68%), biceps brachii (53%) and forearm flexors (47%).
It has been previously hypothesized that the mechanism driving this muscular protective response is due to nociceptive input triggering either a spinal reflex response15 or specifically a flexor withdrawal reflex16,37 or due to stretch receptor mediated reflexes.16 The fact that there is activation of the triceps brachii,15,37 suggests that the mechanism is not simply triggering a flexor withdrawal reflex. In fact, a similar response of cocontraction of the biceps and triceps brachii seen in the upper limb15 has been found in the quadriceps and hamstring muscles, as well as the gastroc-soleus and anterior tibialis muscles, with straight leg raise neurodynamic testing in the lower limb.38 Since anterior and posterior limb muscles are activated during ULNT and are innervated by multiple peripheral nerves, including the median, radial, musculocutaneous, spinal accessory, C3 and C4 spinal nerves, this suggests that the response is triggered by a complex mechanism within the central nervous system. It is possible that the response to loading the neural structures with the ULNT may be to limit further movement by creating a cocontraction of the limb muscles instead of moving into an antalgic posture via a flexor withdrawal.
The main limitation to this study is the use of only healthy, asymptomatic individuals; however, the aim of the study was to establish a baseline normative evaluation of the two test versions as a means for comparisons with multiple patient populations. Another limitation is the small number of males in this convenience sample. It is not expected that there would be a different response in males compared to females so equal distribution of sex was not sought in this study. Lastly, the elbow extension measurement tool (digital goniometer) and use of the hand brace for fixation of the finger position during testing are not commonly used clinical so the outcomes cannot be assumed to be equivalent to manual stabilization of the fingers and visual estimation or standard manual goniometry for range of motion measures.
This is the first study to demonstrate how alterations in scapular positioning influence the symptomatic and muscular responses and subsequently range of motion during the ULNT. Establishing the response to scapular positioning in asymptomatic populations allows clinicians to perform one of the most fundamental comparison for their patients; comparing to known norms. Understanding the range of normal responses in healthy individuals provides a baseline comparison for all clinical populations for which the ULNT is appropriate.
Acknowledgments
The authors would like to thank the following people for their contributions with data collection and manuscript editing: Emily Hellmuth, Alissa Lamb, Leanna Stracco, and Philip Villa. This study was funded in part by a Faculty Research Grant through Samuel Merritt University.
The authors declare that they have no conflicts of interest.
References
- 1.Elvey R. Brachial plexus tension tests and the pathoanatomical origin of arm pain. Idczak R, ed, editor. Aspects of manipulative therapy. Melbourne: Manipulative Physiotherapists Association of Australia; 1979 [Google Scholar]
- 2.Kenneally M, Rubenach H, Elvey R. The upper limb tension test: the SLR of the arm. Grant R, ed, editor. Physical therapy of the cervical and thoracic spine New York: Churchill Livingstone; 1988 [Google Scholar]
- 3.Shacklock M. Neurodynamics. Physiother. 1995;81:9–16 [Google Scholar]
- 4.Butler DS. Mobilisation of the nervous system. Edinburgh: Churchill Livingstone; 1991 [Google Scholar]
- 5.Butler DS. The sensitive nervous system. Adelaide: Noigroup Publications; 2000 [Google Scholar]
- 6.Shacklock M. Clinical neurodynamics: a new system of musculoskeletal treatment. Edinburgh: Elsevier; 2005 [Google Scholar]
- 7.Yaxley G, Jull G. A modified upper limb tension test: an investigation of responses in normal subjects. Aust J Physiother. 1991;37:143–52 [DOI] [PubMed] [Google Scholar]
- 8.Sunderland S. Nerves and nerve injuries. 2nd ed Edinburgh: Churchill Livingstone; 1978 [Google Scholar]
- 9.Byl C, Puttlitz C, Byl N, Lotz J, Topp K. Strain in the median and ulnar nerves during upper-extremity positioning. J Hand Surg Am. 2002;27:1032–40 [DOI] [PubMed] [Google Scholar]
- 10.Selvaratnam PJ, Matyas TA, Glasgow EF. Noninvasive discrimination of brachial plexus involvement in upper limb pain. Spine. 1994;19:26–33 [DOI] [PubMed] [Google Scholar]
- 11.Petty N. Neuromusculoskeletal examination and assessment: a handbook for therapists. 3rd ed Edinburgh: Elsevier/Churchill Livingstone; 2006 [Google Scholar]
- 12.Magee D. Orthopedic physical assessment. 4th ed Philadelphia, PA: Saunders; 2002 [Google Scholar]
- 13.Lewis J, Ramot R, Green A. Changes in mechanical tension in the median nerve: possible implications for the upper limb tension test. Physiotherapy. 1998;84:254–61 [Google Scholar]
- 14.Davis DS, Anderson IB, Carson MG, Elkins CL, Stuckey LB. Upper limb neural tension and seated slump tests: the false positive rate among healthy young adults without cervical or lumbar symptoms. J Man Manip Ther. 2008;16:136–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heide van derB, Allison GT, Zusman M. Pain and muscular responses to a neural tissue provocation test in the upper limb. Man Ther. 2001;6:154–62 [DOI] [PubMed] [Google Scholar]
- 16.Balster SM, Jull GA. Upper trapezius muscle activity during the brachial plexus tension test in asymptomatic subjects. Man Ther. 1997;2:144–9 [DOI] [PubMed] [Google Scholar]
- 17.Byng J. Overuse syndromes of the upper limb and the upper limb tension test: a comparison between patients, asymptomatic keyboard workers and asymptomatic non-keyboard workers. Man Ther. 1997;2:157–64 [DOI] [PubMed] [Google Scholar]
- 18.Edgar D, Jull G, Sutton S. The relationship between upper trapezius muscle length and upper quadrant neural tissue extensibility. Aust J Physiother. 1994;40:99–110 [DOI] [PubMed] [Google Scholar]
- 19.Coppieters M, Stappaerts K, Janssens K, Jull G. Reliability of detecting ‘onset of pain’ and ‘submaximal pain’ during neural provocation testing of the upper quadrant. Physiother Res Int. 2002;7:146–56 [DOI] [PubMed] [Google Scholar]
- 20.Coppieters MW, Stappaerts KH, Staes FF, Everaert DG. Shoulder girdle elevation during neurodynamic testing: an assessable sign? Man Ther. 2001;6:88–96 [DOI] [PubMed] [Google Scholar]
- 21.Coppieters MW, Stappaerts KH, Everaert DG, Staes FF. A qualitative assessment of shoulder girdle elevation during the upper limb tension test 1. Man Ther. 1999;4:33–8 [DOI] [PubMed] [Google Scholar]
- 22.Lohkamp M, Small K. Normal response to Upper Limb Neurodynamic Test 1 and 2A. Man Ther. 2011;16:125–30 [DOI] [PubMed] [Google Scholar]
- 23.Quintner JL. A study of upper limb pain and paraesthesiae following neck injury in motor vehicle accidents: assessment of the brachial plexus tension test of Elvey. Br J Rheumatol. 1989;28:528–33 [DOI] [PubMed] [Google Scholar]
- 24.Sterling M, Treleaven J, Jull G. Responses to a clinical test of mechanical provocation of nerve tissue in whiplash associated disorder. Man Ther. 2002;7:89–94 [DOI] [PubMed] [Google Scholar]
- 25.Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28:52–62 [DOI] [PubMed] [Google Scholar]
- 26.Greening J, Dilley A, Lynn B. In vivo study of nerve movement and mechanosensitivity of the median nerve in whiplash and non-specific arm pain patients. Pain. 2005;115:248–53 [DOI] [PubMed] [Google Scholar]
- 27.Kleinrensink G, Stoeckart R, Vleeming A, Snijders C, Mulder P, Wingerden J. Peripheral nerve tension due to joint motion. A comparison between embalmed and unembalmed human bodies. Clin Biomech. 1995;10:235–9 [DOI] [PubMed] [Google Scholar]
- 28.Kleinrensink G, Stoeckart R, Vleeming A, Snijders C, Mulder P. Mechanical tension in the median nerve. The effects of joint position. Clin Biomech. 1995;10:240–4 [DOI] [PubMed] [Google Scholar]
- 29.Kleinrensink G, Stoeckart R, Mulder P, Hoek G, Broek T, Vleeming A, et al. Upper limb tension tests as tools in the diagnosis of nerve and plexus lesions: anatomical and biomechanical aspects. Clin Biomech. 2000;15:9–14 [DOI] [PubMed] [Google Scholar]
- 30.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36:936–42 [DOI] [PubMed] [Google Scholar]
- 31.Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10:361–74 [DOI] [PubMed] [Google Scholar]
- 32.Di Fabio RP. Reliability of computerized surface electromyography for determining the onset of muscle activity. Phys Ther. 1987;67:43–8 [DOI] [PubMed] [Google Scholar]
- 33.Pols MA, Peeters PH, Bueno-De-Mesquita HB, Ocke MC, Wentink CA, Kemper HC, et al. Validity and repeatability of a modified Baecke questionnaire on physical activity. Int J Epidemiol. 1995;24:381–8 [DOI] [PubMed] [Google Scholar]
- 34.Epstein JB, Wilkie DJ, Fischer DJ, Kim YO, Villines D. Neuropathic and nociceptive pain in head and neck cancer patients receiving radiation therapy. Head Neck Oncol. 2009;1:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wilkie DJ, Molokie R, Boyd-Seal D, Suarez ML, Kim YO, Zong S, et al. Patient-reported outcomes: descriptors of nociceptive and neuropathic pain and barriers to effective pain management in adult outpatients with sickle cell disease. J Natl Med Assoc. 2010;102:18–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Coppieters MW, van de Velde M, Stappaerts KH. Positioning in anesthesiology: toward a better understanding of stretch-induced perioperative neuropathies. Anesthesiology. 2002;97:75–81 [DOI] [PubMed] [Google Scholar]
- 37.Jaberzadeh S, Scutter S, Nazeran H. Mechanosensitivity of the median nerve and mechanically produced motor responses during Upper Limb Neurodynamic Test 1. Physiother. 2005;91:94–100 [Google Scholar]
- 38.Boyd BS, Wanek L, Gray AT, Topp KS. Mechanosensitivity of the lower extremity nervous system during straight leg raise neurodynamic testing in healthy individuals. J Ortho Sports Phys Ther. 2009;39:780–90 [DOI] [PubMed] [Google Scholar]


