Abstract
The engineering of insulin analogs represents a triumph of structure-based protein design. A framework has been provided by structures of insulin hexamers. Containing a zinc-coordinated trimer of dimers, such structures represent a storage form of the active insulin monomer. Initial studies focused on destabilization of subunit interfaces. Because disassembly facilitates capillary absorption, such targeted destabilization enabled development of rapid-acting insulin analogs. Converse efforts were undertaken to stabilize the insulin hexamer and promote higher-order self-assembly within the subcutaneous depot toward the goal of enhanced basal glycemic control with reduced risk of hypoglycemia. Current products either operate through isoelectric precipitation (insulin glargine, the active component of Lantus®; Sanofi-Aventis) or employ an albumin-binding acyl tether (insulin detemir, the active component of Levemir®; Novo-Nordisk). To further improve pharmacokinetic properties, modified approaches are presently under investigation. Novel strategies have recently been proposed based on subcutaneous supramolecular assembly coupled to (a) large-scale allosteric reorganization of the insulin hexamer (the TR transition), (b) pH-dependent binding of zinc ions to engineered His-X3-His sites at hexamer surfaces, or (c) the long-range vision of glucose-responsive polymers for regulated hormone release. Such designs share with wild-type insulin and current insulin products a susceptibility to degradation above room temperature, and so their delivery, storage, and use require the infrastructure of an affluent society. Given the global dimensions of the therapeutic supply chain, we envisage that concurrent engineering of ultra-stable protein analog formulations would benefit underprivileged patients in the developing world.
Keywords: protein design, bottom-up, nanotechnology, zinc finger, hormone
Insulin and analogs
The crystal structure of the zinc insulin hexamer was a landmark in the history of structural biology (Fig. 1).1,2 Elucidated by Hodgkin and colleagues in 1969, this structure provided the first depiction of a protein homo-oligomer and continues to this day to provide a framework for analysis of multiple biological issues, including the biosynthesis and storage of insulin in pancreatic β-cells. Indeed, despite the small size of the insulin monomer (51 amino acids), the zinc hexamer exhibits key features of globular proteins in general: well-defined elements of secondary structure, their tertiary organization about a hydrophobic core, formation of specific interfaces for self-assembly, and intrinsic capacity for long-range conformational change.3 The crystal structure of insulin has also motivated efforts to optimize its molecular properties for use in the treatment of diabetes mellitus.4,5 Modification of the insulin molecule to modulate its pharmacokinetic and pharmacodynamic properties thus represents a pioneering triumph of rational protein design.6,7 Products in current clinical use are summarized in Table 1; these fall into two classes, rapid-acting analog formulations intended for bolus injection before meals (1A) and basal analog formulations intended for once-a-day injection (Table 1B). Because their pharmacokinetic properties remain suboptimal, however, as highlighted by the 2011 strategic planning document of the National Institute of Diabetes Digestive and Kidney Diseases8 and the 2011 Meeting Report of the American Diabetes Association9, modified approaches are presently under investigation.
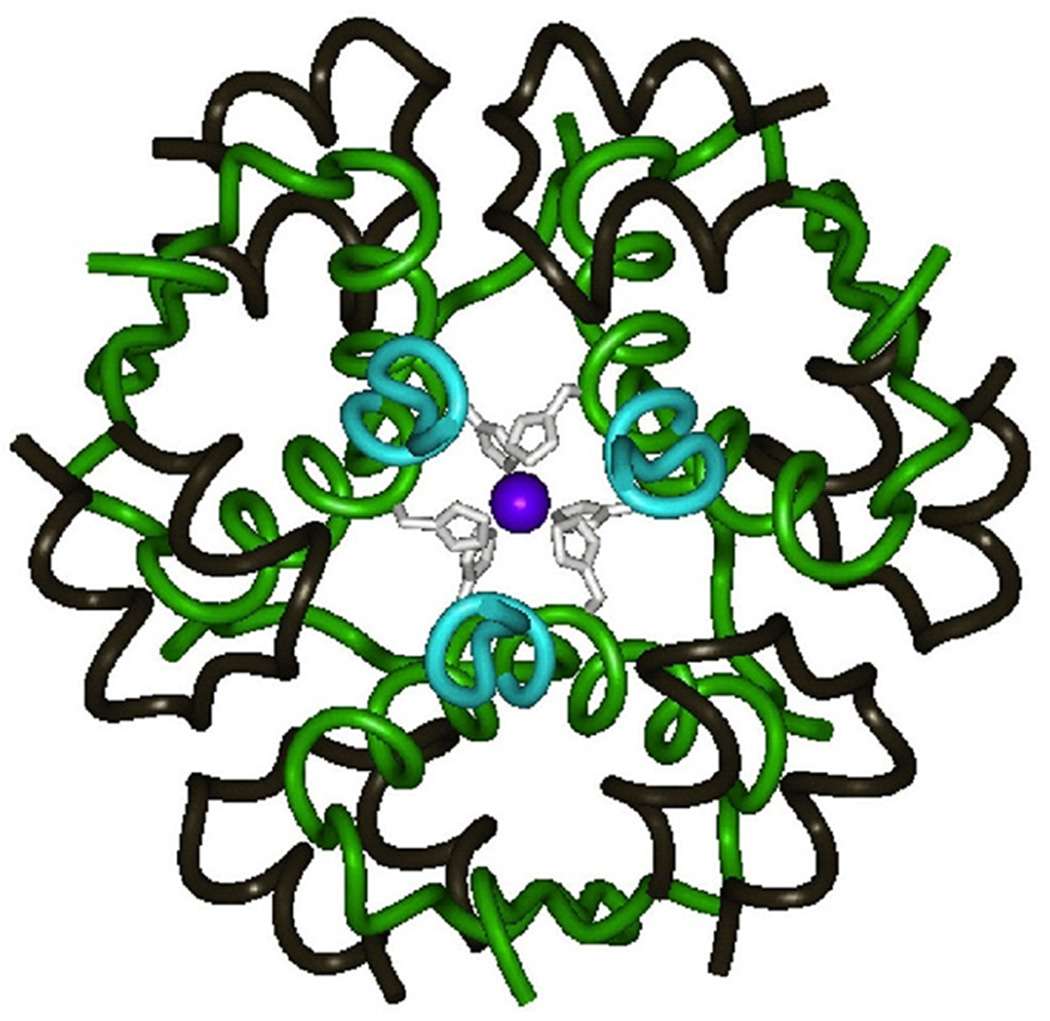
Figure 1.
Wild-type insulin hexamer. The A chain (residues A1–A21) is shown in black and the B chain in blue (residues B1–B6) or green (residues B7–B30). Two axial zinc ions (purple; overlaid at center) are coordinated by six histidine side chains (residue B10; white). The structure shown is the R6 hexamer form characteristic of a pharmaceutical formulation116; coordinates were obtained from Protein Databank entry 1EV3.
Table 1.
Current Insulin Analogs and Modes of Actiona
| Analog | Modification | Mechanism |
|---|---|---|
| A | ||
| Lispro (Humalog®) Eli Lilly and Co. |
ProB28→ Lys LysB28→ Pro |
IGF-I-related motif impairs dimerization |
| Aspart (NovoLog®) Novo-Nordisk |
ProB28→ Asp | charge repulsion at dimmer interface |
| Glulisine (Apidra®) Sanofi-Aventis |
AsnB3 → Lys LysB29 → Glu |
Decreased zinc-free self-association |
| B | ||
| Glargine (Lantus®) Sanofi-Aventis |
ArgB31–ArgB32 tag AspA21 → Gly |
Shift in pI to pH 7 leads to isoelectric precipitation on injection |
| Detemir (Levemir®) Novo-Nordisk |
modification of LysB29 by a tethered fatty acid | stabilization of hexamer and binding to serum albumin |
Panel A lists basal insulin analogs with protracted action whereas B describes rapid-acting analogs employed in prandial regimens and in insulin pumps.
The overarching therapeutic objective of insulin products, singly or in combination, is to recapitulate the physiologic pattern of insulin secretion by pancreatic β-cells in the course of metabolic homeostasis. The importance of tight glycemic control in Type 1 diabetes mellitus was shown by the landmark DCCT10 and its long-term follow-up in the Epidemiology of Diabetes Interventions & Complications Study.11 In long-established Type 2 diabetes mellitus, however, the safety of aggressive glycemic protocols in has been called into question by the recent Action to Control Cardiovascular Risk in Diabetes Study.12,13 Depending on individual metabolic and clinical features14, the United Kingdom Prospective Diabetes Study15 and ACCORD subgroup analysis nonetheless support the appropriateness of moderate glycemic targets with avoidance of hypoglycemic episodes.16 To achieve these clinical objectives, rapid- and basal insulin analogs have been designed based on classical crystal structures3 and general physico-chemical principles.17 In this review, we seek to relate therapeutic objectives to the physical chemistry of insulin and general principles of protein design.
Prandial insulin analogs
The design of insulin analogs has long provided a “molecular laboratory” for the development and application of general principles of protein folding and assembly. Such principles were first applied to the goal of accelerating hexamer disassembly.18,19 These efforts were based on the premise that more rapid disassembly in the subcutaneous depot would facilitate capillary absorption of zinc-free insulin monomers and dimers.6,20 Diverse amino-acid substitutions at subunit interfaces were characterized that weakened or prevented the formation of dimers and hexamers. Whereas mutational disruption of structure generally represents a straightforward task, a specific subset of such substitutions was sought based on three functional criteria: compatibility with high-affinity binding to the insulin receptor, retention of native biological activity in vivo, and amenability to stable pharmaceutical formulation. There are three such rapid-acting analogs in current use (Table 1B); in chronological order of clinical introduction, these are insulin lispro (the active component of Humalog®; Eli Lilly),21 insulin aspart (Novolog®; Novo-Nordisk),22,23 and insulin glulisine (Apidra®; Sanofi-Aventis).24,25 These products have been proven safe and effective in multi-injection regimens7,26 and for use in continuous subcutaneous infusion devices (insulin pumps).27 The diversity of molecular changes conferring more rapid insulin absorption reflects the multiple ways that the elegantly crafted structure of the wild-type insulin hexamer may be rendered less stable with maintenance of biological activity. Although current rapid-acting insulin analog products have met the threshold criteria for chemical and physical stability as set by the United States Food & Drug Administration (FDA), these formulations are in general more susceptible to physical and chemical degradation above room temperature than are comparable wild-type formulations.
X-ray crystallographic studies of insulin lispro and aspart28,29 have provided insight into their respective mechanisms of rapid action and led to a deeper insight into the structural determinants of classical dimerization.2,3 Hexamer assembly in each case required the binding of phenol or the related ligand meta-cresol, commonly employed in pharmaceutical formulations for their anti-microbial properties. Such ligands were previously found to induce a large-scale allosteric reorganization of the zinc insulin hexamer (Figure 2) designated the TR transition.30 Thus we see three families of structures: T6 (the original Hodgkin structure of 1969),1,2 T3Rf3 (which was first observed under high-salt conditions)31, and R6 (which contains six bound ligands per hexamer).32 Whereas the T-state protomer resembles the solution structure of an insulin monomer in solution,33–35 in the R-state protomer the B-chain undergoes a change in secondary structure to form an elongated B1–B19 α-helix; an isolated R-like conformation has not to date been observed. Comparison of these structures provided a pioneering model for the transmission of conformational change in protein assembly.3,32,36 The crystal structure of insulin lispro was determined as a T3Rf3 zinc hexamer containing three bound phenolic ligands (Fig. 3A),28 whereas the structure of insulin aspart was determined as an R6 hexamer containing six bound ligands (Fig. 3B).29 Comparison of their dimer contacts demonstrated retention of native-like anti-parallel β-sheets (residues B24–B28), with only subtle structural distortions near the sites of substitution (Fig. 3C and 3D).
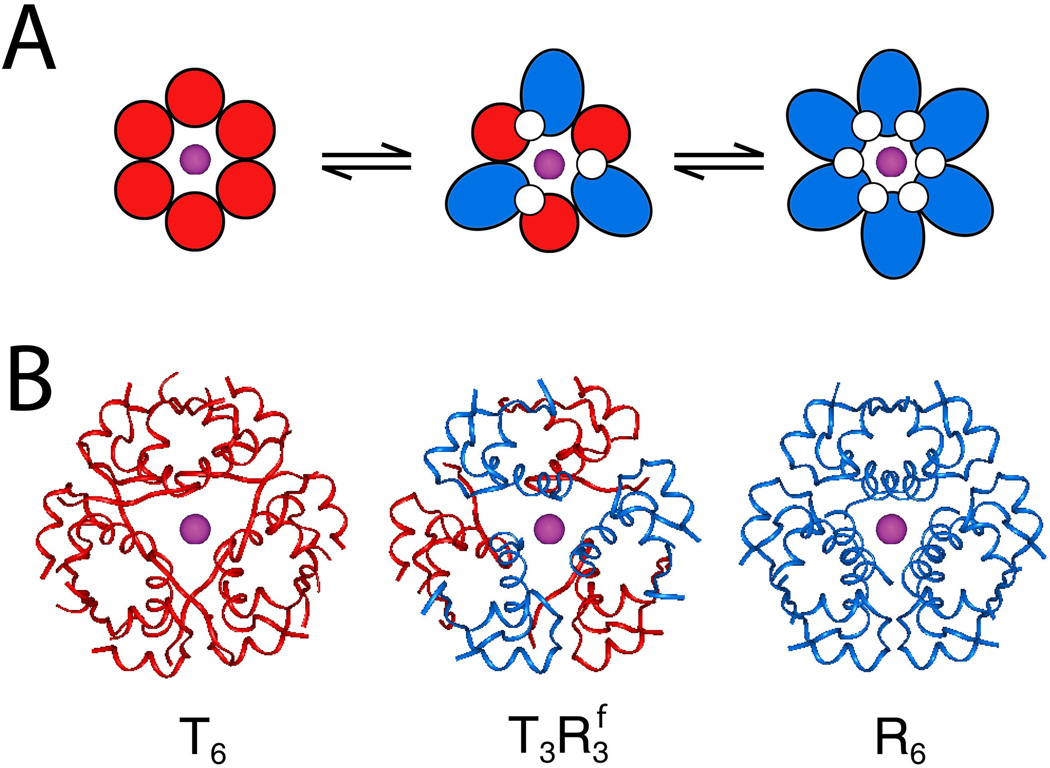
Figure 2.
Exploiting the TR transition in supramolecular protein engineering. (A) Schematic representation of the three types of zinc insulin hexamers, designated T6, T3Rf3, and R6. Residues B1–B8 exhibit a change in secondary structure as shown in black. T-state protomers are otherwise shown in red, and R-state protomers in blue. (B) Corresponding ribbon representation of wild-type crystal structures. Axial zinc ions are shown in blue-gray. Coordinates were obtained from Protein Databank entries 4INS, 1TRZ, and 1ZNJ, respectively. This figure is reprinted by Wan and colleagues 117 with permission of the authors.
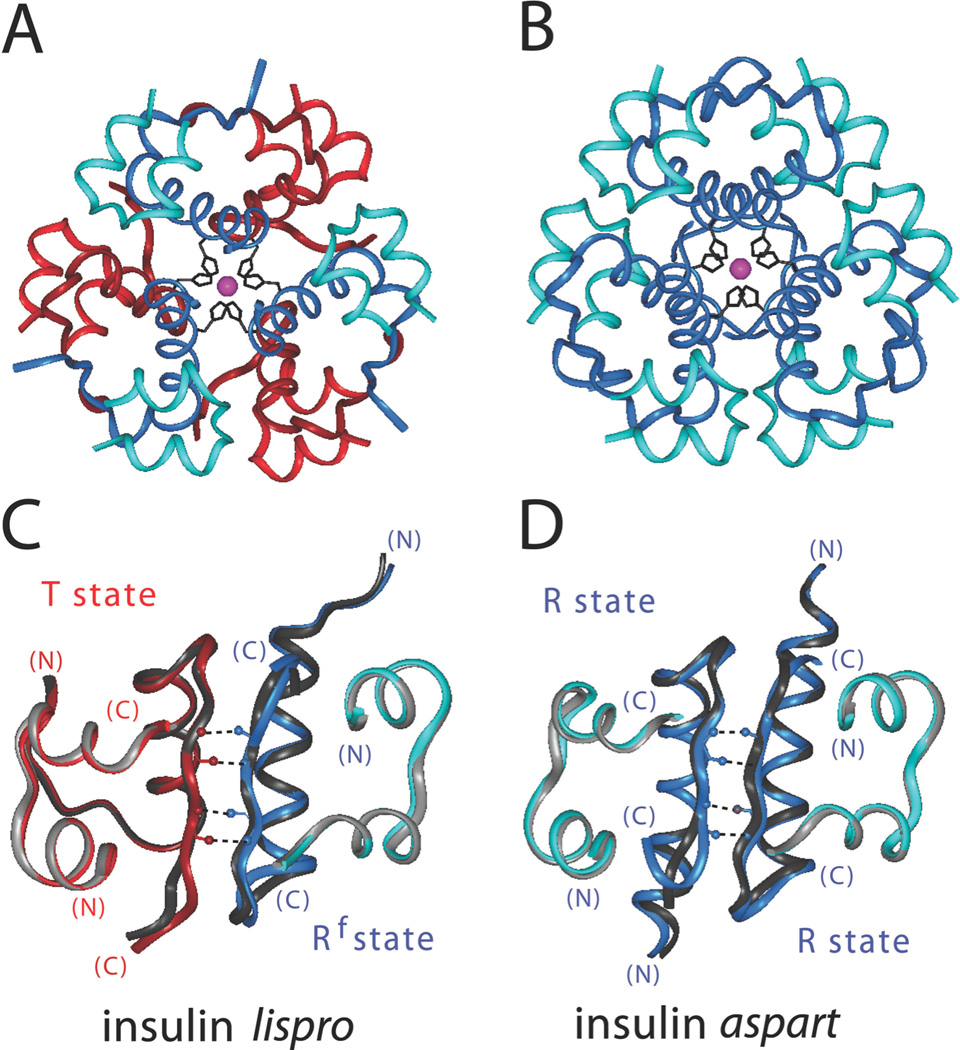
Figure 3.
Structure of prandial insulin analogs. (A) Ribbon model of insulin lispro (the active component of Humalog®) as a phenol-stabilized T3Rf3 zinc hexamer (PDB entry 1LPH). The A- and B-chains of T-state protomers are shown in light and dark red, respectively; the A- and B-chains of Rf-state protomers are show in light and dark blue, respectively. Axial zinc ions are shown as purple spheres. (B) Corresponding model of insulin aspart (the active component of Novolog®) as a phenol-stabilized R6 zinc hexamer (AspB28-insulin; PDB entry 1ZEG). The A- and B-chains of R-state protomers are shown in light and dark blue, respectively. (C and D) Expanded region of dimer contacts in prandial insulin analogs versus wild-type insulin: dimer-related β-sheet (residues B24–B28) and inter-strand hydrogen bonds (dotted lines). (C) Insulin lispro versus wild-type T3Rf3 zinc hexamer (PDB entry 1TRZ). The A- and B-chains of wild-type insulin are shown in light and dark gray, respectively; the color code is otherwise as in panel A. T-state of lispro are shown in light and dark red, and R state in light and dark blue. (D) Insulin aspart versus wild-type T3Rf3 zinc hexamer (PDB entry 1ZNJ). The wild-type shading is as in panel C, and color scheme as in panel B. In panels C and D the variant and wild-type structures were aligned according to the main-chain atoms of residues B3–B28 and A3–A20. Hydrogen-bond lengths and angles are given in Table 2.
The dual role of phenolic ligands as anti-microbial preservatives and allosteric effectors was central to the stable pharmaceutical formulation of insulins lispro and aspart. Although kinetic 1H-NMR studies have demonstrated that ligand dissociation occurs on the millisecond time scale,37 the TR transition stabilizes zinc binding38 and profoundly retards rates of subunit exchange between hexamers.39 On subcutaneous injection, the ligands are presumed to diffuse from the depot and partition into cellular membranes. The unliganded hexamers then rapidly disassembly to permit absorption into capillaries.6,20 How the mechanisms of assembly and disassembly of the insulin analog hexamers differ from those of wild-type insulin is not well understood. Although wild-type insulin forms monodisperse solutions of zinc hexamers in the presence or absence of phenolic ligands, ligand binding is required for monodisperse hexamer assembly of the analogs. Because the binding sites are distant from the amino-acid substitutions at positions B28 and/or B29, it is not known whether structural communication occurs between these sites or whether such ligand-dependent assembly reflects a purely formal thermodynamic linkage. While inter-strand hydrogen bonds in the R6 aspart hexamer are similar to those of wild-type insulin in the same crystal form (Fig. 3D and Table 2),29 G. D. Smith and colleagues have emphasized that the inter-strand hydrogen bonds in the T3Rf3 lispro hexamer are in part distorted (Fig. 3C; bold and underlined values in Table 2) and so might contribute to accelerated disassembly.28 Because subsequent spectroscopic studies have suggested that the actual structure of insulin lispro in a formulation is R6 and not T3Rf3 (based on d-d optical transitions in corresponding cobalt models),40 it is possible that the T3Rf3 crystal structure represents an intermediate state of the subcutaneous depot on partial dissociation of the bound phenolic ligands.
Table 2.
β-Sheet-Related Hydrogen Bonds in Insulin Dimers
| A. Wild-Type Zinc Hexamersa | |||||||
|---|---|---|---|---|---|---|---|
| T6 | T3Rf3 | R6 | |||||
| mol. 1 | mol. 2 | d | θ | d | θ | d | θ |
| PheB24.1 O | — TyrB26.2 NH | 1.86 | 177.84 | 1.78 | 170.63 | 1.62 | 170.50 |
| PheB24.1 NH | — TyrB26.2 O | 2.08 | 139.19 | 1.93 | 153.19 | 2.12 | 140.56 |
| TyrB26.1 O | — PheB24.2 NH | 2.16 | 149.78 | 1.97 | 151.80 | 2.08 | 148.00 |
| TyrB26.1 NH | — PheB24.2 O | 1.86 | 174.90 | 1.91 | 170.57 | 1.54 | 170.59 |
| B. Variant Zinc Hexamersb | |||||||
|---|---|---|---|---|---|---|---|
| lispro | aspart | zinc-stapled | |||||
| mol. 1 | mol. 2 | d | θ | d | θ | d | θ |
| PheB24.1 O | — TyrB26.2 NH | 1.69 | 164.88 | 1.88 | 166.78 | 1.79 | 171.08 |
| PheB24.1 NH | — TyrB26.2 O | 2.48 | 130.72 | 1.97 | 148.89 | 2.05 | 149.17 |
| TyrB26.1 O | — PheB24.2 NH | 2.21 | 172.18 | 1.89 | 156.32 | 1.82 | 152.10 |
| TyrB26.1 NH | — PheB24.2 O | 1.87 | 166.95 | 1.88 | 173.46 | 1.84 | 166.72 |
Coordinates were obtained from PDB entries 4INS (T6), 1TRZ (T3R3), and 1ZNJ (R6). Respective resolutions are 1.5, 1.6, and 2.0 Å.
Coordinates were obtained from PDB entries 1LPH (lispro), 1ZEG (aspart), and 3KQ6 (zinc-stapled analog). Respective resolutions are 2.3, 1.6, and 1.9 Å. In each case hydrogen bond length and angle are designated d and θ, respectively. Value in bold indicates anomalous lengthening of hydrogen bond at dimer interface of insulin lispro relative to any of the wild-type crystal forms28; underlined value indicates anomalous lengthening of hydrogen bond relative to corresponding T3Rf3 wild-type structure.
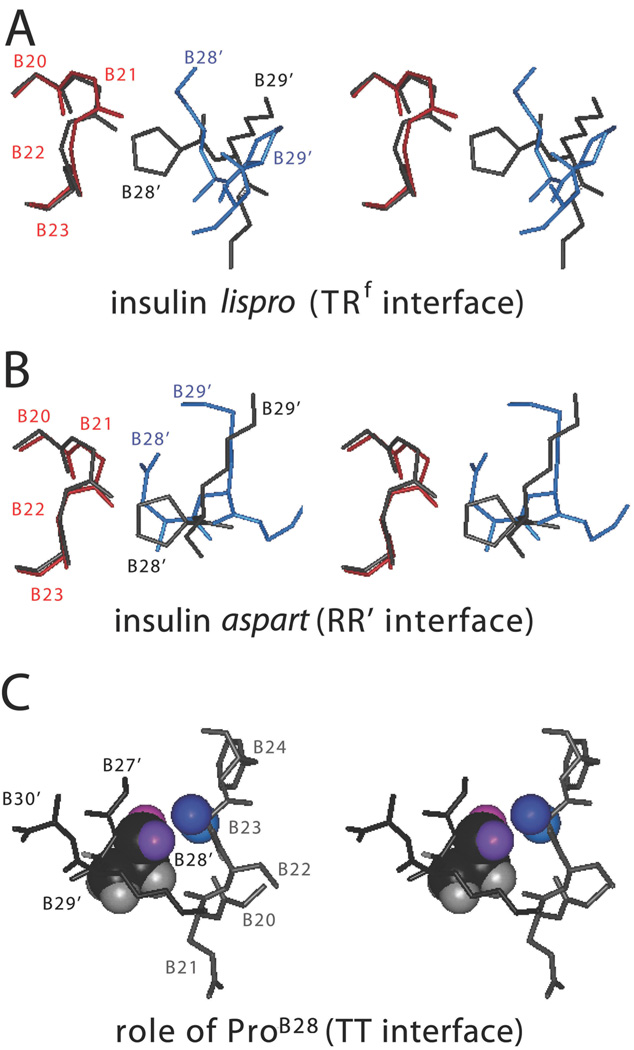
Although the original ideas underlying the design of insulin aspart emphasized the role of electrostatic repulsion at the dimer interface18, further mutagenesis studies highlighted the key role played by the absence of ProB28 and so by implication its cryptic contribution to the wild-type interface.19 Proline is conserved at this position among vertebrate insulins but had not previously been the focus of attention, in part because des-tripeptide[B28–B30]-insulin, des-tetrapeptide[B27–B30]-insulin, and des-pentapeptide[B26–B30]-insulin-amide each exhibit native activity.3,41,42 Comparison of the crystal structures of insulins lispro and aspart with wild-type insulin in corresponding crystal forms demonstrated a local distortion of the dimer interface associated with the absence of ProB28: the wild-type pyrrolidine ring contacts GlyB23 in the opposite β-turn (Fig. 4A and 4B). Thus informed by the structures of the analogs, this perspective highlighted for the first time the importance of the same contact in the classical T6 hexamer (Fig. 4C). This sequence of events exemplifies the power of mutagenesis to enhance the structural annotation of a wild-type structure even after decades of high-resolution study.
Figure 4.
Molecular details of B28-related dimer contact. (A) Stereo models of wild-type insulin and insulin lispro (in corresponding T3Rf3 hexamers): enlargement of the interface between the C-terminal residues of one B-chain (B28–B30) and the B20–B23 β-turn of the dimer-related B-chain. The wild-type B-chain is shown in dark gray; residues belonging to the T- or Rf-state protomers of insulin lispro are shown in red or blue, respectively. (B) Corresponding alignment of wild-type insulin and insulin aspart (in corresponding R6 hexamers). The coloring scheme is as in panel A. (C) Corresponding interface in classical wild-type T6 hexamer (PDB entry 4INS). The site of closest contact between the dimer-related B-chains at this site are shown in Corey-Pauling-Koltun (CPK) representation; respective residues belong to the A- and B-chains are otherwise shown as light and dark gray sticks. The side chain of PheB24 (which anchors the β-turn to the central B-chain α-helix) is also shown. The proteins were in each case aligned as in Figure 2.
Advances in “smart” insulin pumps – closed-loop systems in which control of the pump is controlled by an algorithm based on feedback from a continuous glucose monitor43,44 – have highlighted the need for insulin analogs even faster than current products (Table 1A).8,9,45,46 A wide variety of approaches are under investigation, including heating pads at the site of injection to increase local blood flow,47,48 co-injection of the enzyme hyaluronidase to break down connective tissue at the site of injection,49 fabrication of micro-needle patches,50 needle-free jet injection,51 and additives to current formulations that enhance rates of disassembly.52,53 The diversity of these approaches highlights the perception of clinical need.8 We anticipate that further structural analysis of insulin and its determinants of stability will also provide guidance for future design of ultra-fast analogs synergistic with existing approaches to accelerating insulin absorption from the subcutaneous depot.54,55 However, because insulin assembly ordinarily protects the hormone from degradation, a tradeoff may be encountered between structural strategies for rapid action and the stability requirements of regulatory agencies.
Basal insulin analogs
A complementary therapeutic objective in the treatment of diabetes mellitus is defined by the pharmacokinetics of a basal insulin analog formulation.56 Whereas fast-acting analogs are essential for the management of Type 1 diabetes mellitus and key to the operation of insulin pumps,43–45 basal insulin analogs enhance glycemic control in multi-injection regimens57 and are of overarching importance in Type 2 diabetes mellitus.58 In Type 2 patients controllable by either prandial or basal analogs alone, basal regimens are preferred to their simplicity and reduced risk of weight gain.59 Although the global need for such products may exceed that of rapid-acting formulations (given the emerging pandemic of the metabolic syndrome and Type 2 diabetes mellitus), the converse goal of targeted stabilization of the insulin hexamer poses a more subtle challenge to the protein engineer.5,60 Indeed, evolutionary optimization of the insulin hexamer and its exquisitely crafted self-assembly surfaces (well conserved among mammalian insulins3) renders inapparent possible structural routes to further improvement. Although pioneering efforts in this direction were proposed by Dodson and colleagues,3,5 current products have circumvented the need for detailed molecular analysis. Insulin glargine exploits a phenomenon that is robust to the details of molecular structure: isoelectric precipitation, a reversible transition to insolubility that classically occurs between pH 5 and 6 under which conditions wild-type insulin exhibits little or no net charge.61,62 Insulin glargine contains a two-residue basic extension of the B-chain (ArgB31 and ArgB32) whose positive charges result in a shift in the isoelectric point to neutrality. Injection of an unbuffered pH 4 formulation results in precipitation within the subcutaneous depot and hence protracted absorption.63 The di-arginyl extension is disordered and in part removed by endogenous exopeptidases. Lantus is the most widely-used long-acting insulin currently on the market.64 Related analogs containing additional basic residues N-terminal to GlyA1 have also been described but are not in clinical use.65 Insulin detemir contains a prosthetic fatty acyl group on LysB29, intended to mediate binding to serum albumin and hence provide a circulating depot.66 Although this mechanism is active, the tethered moiety serendipitously also enhances the stability of hexamers of the modified insulin.67 Levemir is often administered twice a day as its duration of action is less prolonged than that of Lantus Thus, non-standard modification of the insulin molecule in principle provides an opportunity to exploit chemical tactics beyond those made possible by the 20 naturally occurring amino acids – and so complement the structural strategies implicitly optimized by evolution.
Next-generation insulin analogs
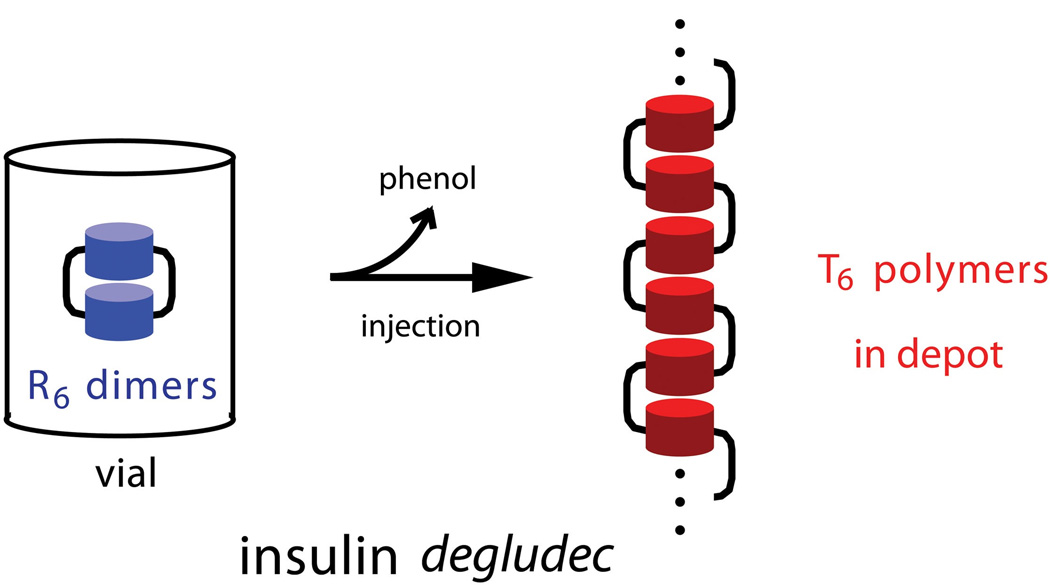
A next-generation basal insulin analog, designated insulin degludec, is under clinical investigation by Novo-Nordisk and a network of academic collaborators.68–71 Formulated as neutral pH solution containing a dimer of zinc hexamers linked by a novel acyl modification, this analog undergoes multi-hexamer assembly in the subcutaneous depot and thereby achieves protracted action. The name “degludec” refers to three chemical features: “de”, the absence of ThrB30 (i.e., des-B30), “glu”, side-chain addition of a glutamic acid residue via a non-standard peptide bond between its δ-carboxylate function and the ε-mino group of LysB29, and “dec”, referring to a dicarboxylic acid (HOOC-(CH2)n-COOH) in turn linked to the α-amino group of attached Glu. In this analog n = 14, corresponding to thapsic acid. Whereas insulin glargine contains two additional positive charges at neutral pH (ArgB31 and ArgB32; see above) and is insoluble, the net formal charge of insulin degludec differs from wild-type insulin by -2 (loss of the positive charge of LysB29 and gain of one negative charge from the peptide-linked thapsic acid), enabling its formulation as a clear solution at pH 7.4.
Higher-order assembly of insulin degludec is associated with a change in zinc hexamer conformation triggered by release of the bound phenolic preservative. Remarkably, supramolecular assembly is thus coupled to the rhombohedral TR transition as described above (Fig. 2).31,32 The transition among T6, T3R3, and R6 zinc hexamers is notable for displacements in the relative positions of atoms as large as 30 Å. Beyond its academic interest as a model of conformational change36, its application to the pharmacology of insulin degludec appears central. Whereas the vial or pen contains the R6 hexamer form, which is advantageous for stability and resistance to degradation, the depot presumably contains acyl-bridged stacks of T6 insulin hexamers, yielding linear polymers (Fig. 5). The modification also permits albumin binding in the bloodstream as achieved by insulin detemir. Because the pharmacokinetic profile of insulin degludec exceeds 24 hours, once-a-day dosing may provide a flatter pharmacodynamic profile and reduced risk of hypoglycemia relative to first-generation products.69–71 Acylated insulin analogs conferring protracted action have also been disclosed in patents awarded to the Lilly Research Laboratories.65,72–75 Although the physical state of proteins in a subcutaneous depot is not amenable to atomic-level characterization, the precise molecular architectures bridged by the acyl modification of insulin degludec may be extrapolated from analysis of crystal contacts. To the extent that such structural features were unanticipated, the favorable pharmacokinetic properties of this next-generation analog represent a combination of rational design and molecular serendipity.
Figure 5.
Exploiting the TR transition in supramolecular protein engineering: schematic representation of the mechanism of insulin degludec. Left, Insulin degludec is formulated at neutral pH as dimers of phenol- (or meta-cresol) stabilized R6 zinc insulin hexamers (blue). The acyl modification of LysB29 is shown in schematic form as a black bar (in principle 6 per hexamer); for simplicity only two are shown. Right, On subcutaneous injection, diffusion of the phenolic ligand into cellular membranes triggers the R →T transition, leading in turn to linear polymerization of T6 zinc hexamers (red). Classical hexamer reorganization is thus coupled to a change in mode of hexamer-hexamer assembly mediated in part by the B29-linked acyl group. Panels A and B are reprinted by Wan and colleagues 117 with permission of the authors.
The mechanism of protracted action of insulin degludec elegantly exploits the conformational repertoire of insulin hexamers. Although this repertoire (with its unusual thermodynamic linkage to the binding of phenolic ligands) is a particular feature of mammalian insulins, the mechanism nonetheless provides a model for the potential role of supramolecular chemistry in nanobiotechnology. Although nano-scale engineering efforts to date have employed simpler models, increased fidelity may likewise be achieved by taking advantage of the high degree of specificity conferred by complementary surfaces; a diversity of potential products may be selectively obtained by exploiting appropriate molecular compatibilities and combinations.76,77 This perspective focuses attention on the structure and organization of a subcutaneous insulin depot as a biomaterial in its own right.
Zinc-mediated assembly
Whereas the mechanism of insulin degludec is mediated by a complex prosthetic modification of the insulin molecule, an independent approach to the supramolecular “depot engineering” exploits design features of proteins that are ubiquitous in nature. Biological assemblies often contain hybrid inorganic-organic structures as mediated by the coordination of metal ions, especially divalent cations such as Ca2+ and Zn2+ (Fig. 6B). Examples range from association of the S100A12 protein into oligomers78 and construction of long cadherin-repeat chains to assembly of viral capsids (Fig. 6D).79 An example of clinical relevance is seen in the “zinc zipper” adhesion of staphylococcal biofilms; this zinc-mediated form of supramolecular assembly contributes to resistance in hospital bacterial strains.78,80–82 Such metal-ion-coordinated supramolecular assembly offers the important advantage that the ligand can act as a switch to alter the oligomeric state of a peptide or protein, thus permitting biological control through regulation of ion concentrations. This mechanism also provides a potential tool for nano-scale engineering.
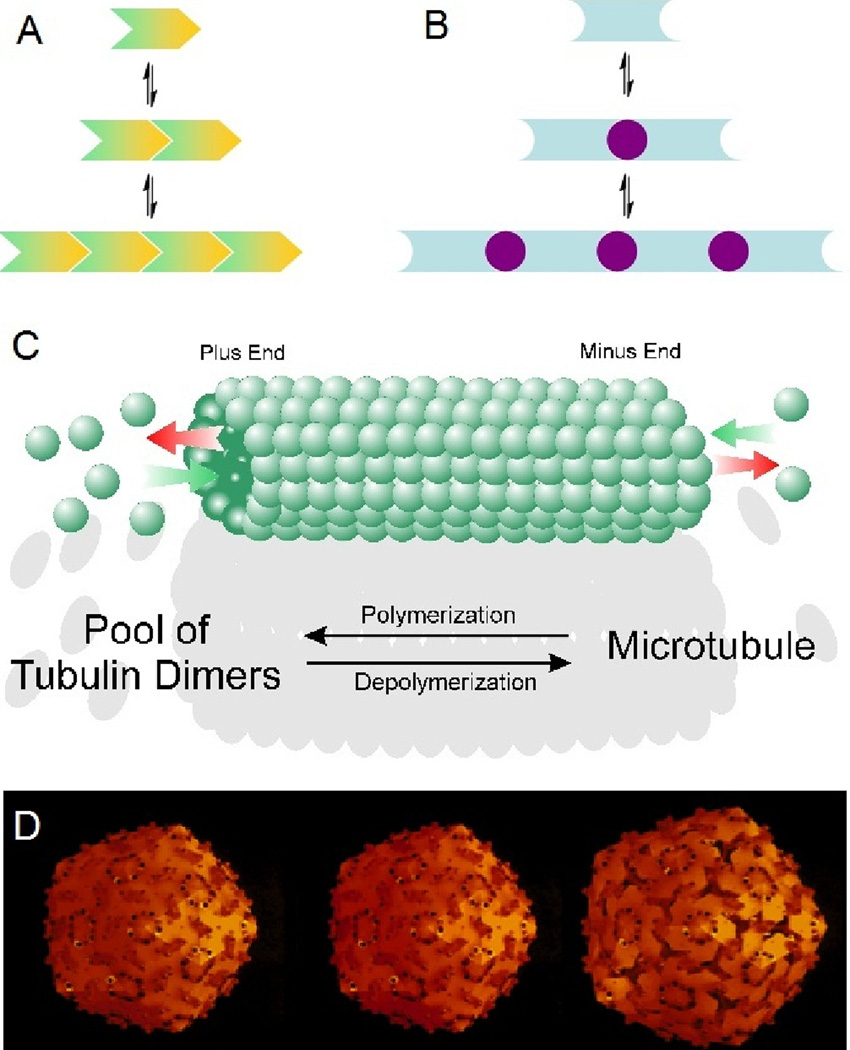
Figure 6.
Supramolecular assembly. (A) Schematic representation of supramolecular assembly of monomers, each containing complementary surfaces. Such assembly is often exploited in biology to form diverse architectures, including multi-layered ropes (as in the collagen of ligaments and tendons), hollow tubes (as in microtubules), and cages (as in viral assembly). (B) Ligand-linked mechanism of supramolecular assembly. One possible realization of this strategy is provided by metal ions. Each monomer (blue) presents half of a metal-ion binding site; successive coordination by metal ions (purple) mediates polymerization. (C) Assembly of a microtubule from tubulin monomers (this panel was kindly provided by Dr. Danton H. O’Day, Professor of Cell and Systems Biology, University of Toronto Mississauga, Ontario, Canada.) (D) Southern bean mosaic virus. Presence of divalent cations directs the swelling from left to right (this panel was kindly provided by Dr. Donald L. Caspar, Professor Emeritus of Biological Sciences, Florida State University, Tallahassee FL).
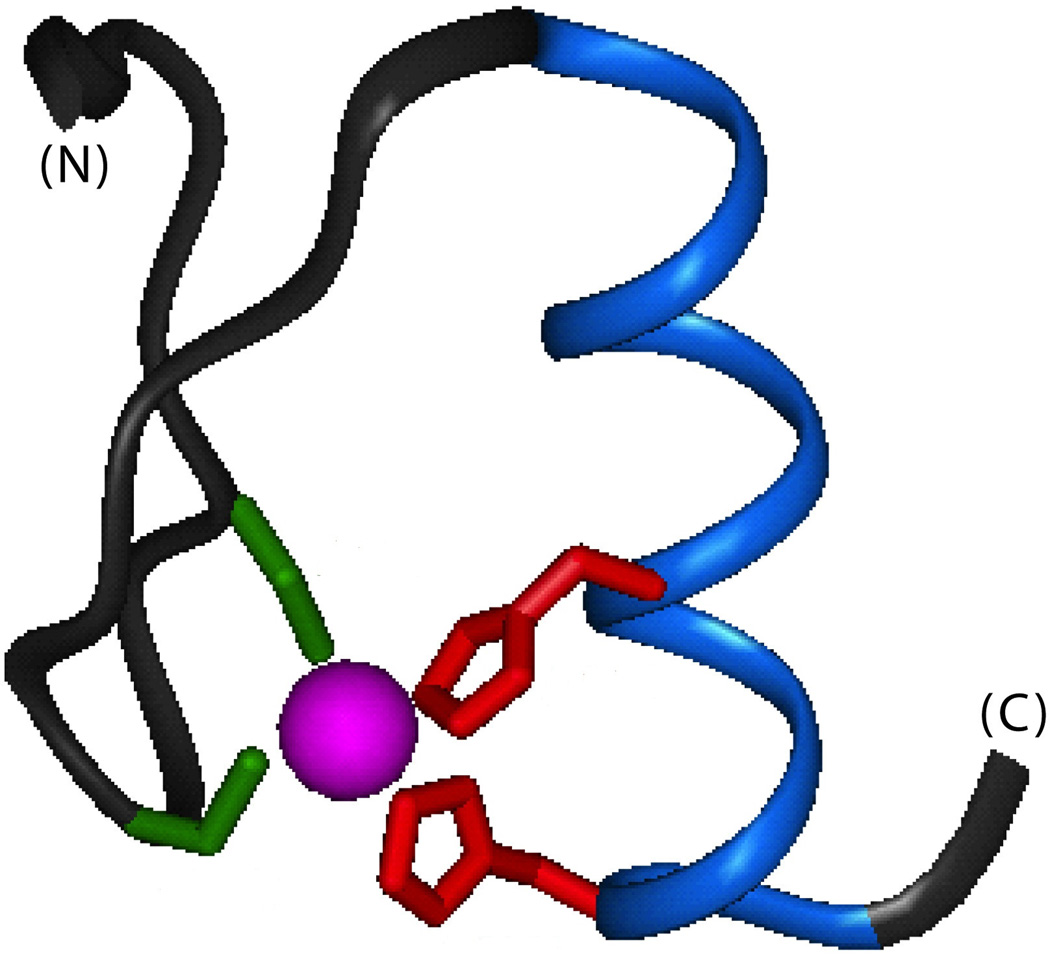
A straightforward method for introducing novel zinc-binding sites into proteins83 is by recapitulation of zinc finger motifs.84 Zinc fingers are ancient and highly conserved zinc-binding moieties that coordinate the Zn2+ with a combination of cysteine and histidine residues. Such binding is sensitive to pH as the cysteines function as thiolates and the imidizole ring must be unprotonated. The first zinc finger domain to be identified contained two cysteines (CX2,4C, where X2,4 represents intervening two or four residues) and two histidines (HX3,4H), together defining a C2H2 motif. The peptide backbone of a zinc finger consists of a small β-hairpin domain followed by an α-helix held in place by the encaged zinc ion (Fig. 7).84,85 Zinc fingers play a significant role in eukaryotic protein-nucleic acid interactions. The binding of individual zinc ions is associated with an increased rate of protein folding and in some cases dimerization.81 Zinc fingers typically form tandem arrays; in protein-DNA complexes successive fingers recognize particular DNA subsites.86 The widespread occurrence of zinc finger genes in eukaryotic genomes is likely a consequence of the high structural stability of the zinc-finger domains as a combinatorial platform for sequence-specific DNA and RNA recognition.
Figure 7.
Classical zinc-finger motif. The peptide backbone is shown in black (N-terminal β-hairpin and central loop) or blue (C-terminal α-helix); the encaged zinc ion is shown in magenta. The interior Zn2+ coordination site of the C2H2 motif comprises the thiolate groups of two cysteine side chains (green) and imidazole rings of two histidine side chains (red). The structure shown is domain 2 of Zif268;85 coordinates were obtained from Protein Databank entry 1ZAA.
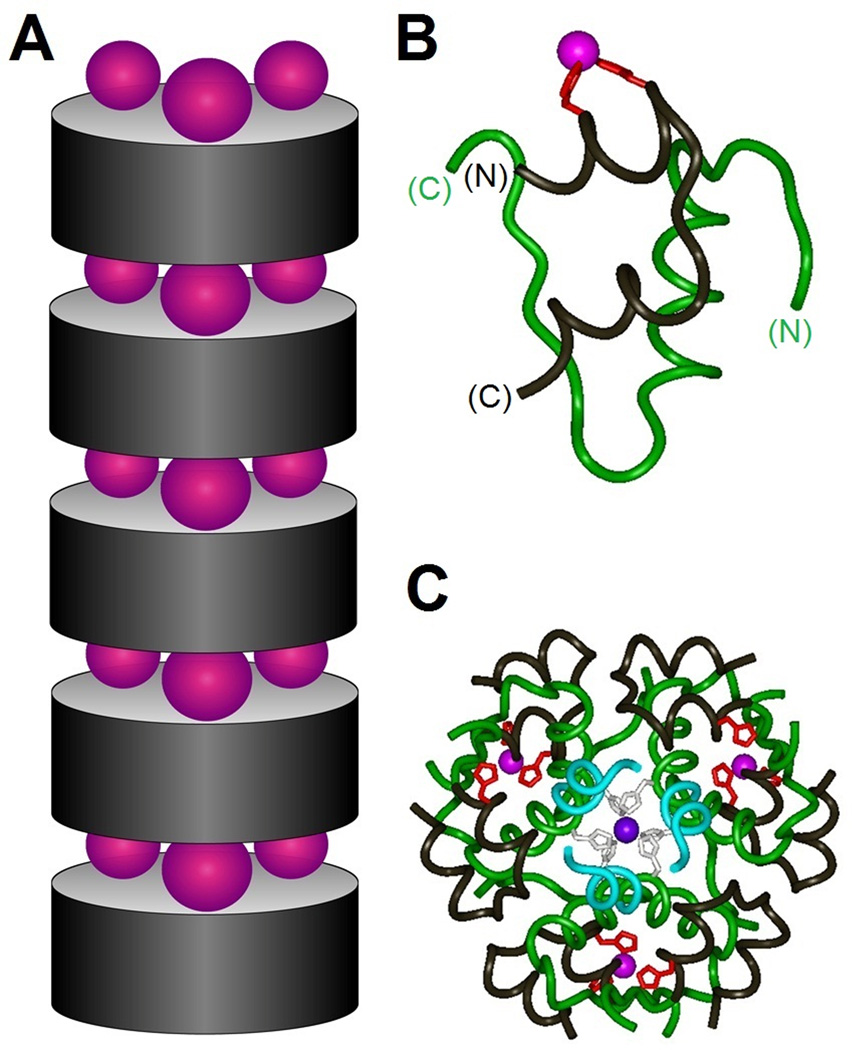
The physico-chemical principles of designed metal-ion-binding sites83 may be applied to insulin: a portion of the classical zinc finger motif was introduced by substituting histidine residues at positions (i, i + 4) on the surface of an A chain α-helix. This scheme employed the paired substitutions GluA4→His and ThrA8→His. In hexamers of this disubstituted insulin, three insulin molecules have the engineered partial zinc-binding sites facing up while three have them facing down. The half binding sites on the top face of one hexamer align with the half sites on the bottom face of the next hexamer to recapitulate the full zinc finger motifs; the tetrahedral coordination site may be completed by a chloride ion. One Zn2+ion can fit into each of the three zinc-binding moieties at the hexamer-hexamer interface, where the cation can stabilize hexamer-hexamer interactions and thus promote supramolecular assembly. Substitutions GluA4→His and ThrA8→His thus maintain insulin’s tertiary structure. The introduced HX3H element hinders neither binding of the analog to the insulin receptor nor native self-assembly into a zinc-insulin hexamer (Fig. 8).
Figure 8.
Zinc-stapled insulin analogs. (A) Schematic model showing successive stacking of insulin hexamers (gray cylinders) bridged by layers of zinc ions (purple spheres). Upper and lower surfaces of insulin analog hexamer present three α-helix-related HX3H half-coordination sites; each site recapitulates the C-terminal half of the classical zinc finger (see Fig. 3). (B) Ribbon model of variant insulin monomer showing designed HX3H sites (red) at residue positions A4 (left) and A8 (right) in the N-terminal A-chain α-helix. The A chain is otherwise shown in black, and the B chain in green. (C) Crystal structure of variant R6 insulin hexamer. The three novel interfacial zinc ions are shown in magenta whereas the two classical axial zinc ions (coordinated by HisB10; black) are shown in purple (overlaid in center). The color code is otherwise as in Figure 1 with the A chain in black and B chain in blue (residues B1–B6) or green (residues B7–B30). In the crystal lattice successive insulin hexamers are stacked as in panel A with intervening layers of zinc ions.78 Coordinates were obtained from Protein Databank entry 3KQ6.
Zinc-stapled insulin carries several potential therapeutic advantages. As in insulin glargine, substitution by basic amino acids (in this case histidine) raises the isoelectric point; the pI is further raised by removal of the negative charge of GluA4. Therefore, this novel disubstituted insulin can be freely formulated as a monomer at pH 4, where protonation of the A4 and A8 histidines also prevents coordination with either axial or bridging zinc ions. At neutral pH, however, the insulin loses its net charge and deprotonation of the imidazole rings unshields zinc-binding sites. The protein thus associates into zinc-coordinated hexamers and then zinc-stapled polymers of hexamers, promoting precipitation of stable supramolecules upon injection into the subcutaneous compartment. The crystalline deposit formed can then act as a stable and ultra-long acting insulin reservoir. The extended pharmacokinetics of this formulation has been demonstrated in preliminary studies in rodents. With fine-tuning, it is expected that the pharmacokinetics of zinc-stapled insulin will closely match the constant basal level of insulin in non-diabetic human beings. Whether this approach will make possible equivalent or superior glycemic control awaits clinical trials.78
Like insulin degludec, a feature of this novel insulin analog of potential importance in relation to insulin glargine is its more stringent receptor specificity. One of the principle public health concerns regarding insulin glargine is its sixfold-increased affinity relative to human insulin for the mitogenic IGF-1R. In vitro studies on human cells have found an almost eightfold increase in mitogenic potential.87–89 Follow-up studies in diabetic patients found that those using insulin glargine at high doses or for many years appeared to have increased rates of breast, colon, prostate, pancreas, and lung cancers90,91 Although the association between use and insulin glargine and risk of cancer is controversial92–94 (in part due to the statistical methods employed in the original analysis)95, the A4, A8 di-substituted insulin may address this potential concern because it discriminates 30-fold more than insulin glargine between the IR and IGF-1R. Thus, this novel insulin may both prolong action and (to the extent that effects of insulin analogs on carcinogenesis may be validated or invalidated)91,96 enhance patient safety.78 Additional population-based studies of cancer prevalence in long-term users of insulin products (ideally prospective and randomized) will be required to address the issue of carcinogenicity and its potential relationship to in vitro properties of insulin analogs.
Supramolecular protein engineering
The molecular lessons provided by the engineering of insulin analogs promise to illuminate broader principles. An overview of this field provides a general context. There are two principal approaches for creating nanoscale technology. The first, design of an assembly from the top-down, involves the synthesis and organization of nanoscopic products using large-scale technology, as exemplified by the manufacturing of computer chips. Top-down design typically employs explicit rules and criteria for optimization. By contrast, bottom-up assembly reflects the intrinsic tendency of some materials to amalgamate via complex and yet well-organized molecular mechanisms for self-recognition. Physico-chemical interactions that mediate molecular recognition at complementary surfaces include hydrogen bonding, donor-acceptor interactions, van der Waals forces, and the hydrophobic effect (Fig. 6A). Bottom-up assembly of supramolecular structures in principle offers distinct advantages over traditional top-down approaches, including heightened nano-scale control and fidelity. Complex chemical surfaces can be regarded as building blocks to organize hierarchical assembly, ideally in predictable ways.
Zinc stapling promises to provide a general approach to the rational design of protein deposits as a therapeutic nanobiotechnology.97 Engineered zinc binding sites that promote supramolecular assembly may thus have a wide-ranging impact in protein therapeutics. A rapidly expanding field in medicine, protein therapeutics includes more than 130 FDA-approved polypeptides or proteins targeted for treatment of cancer, infertility, hemophilia, and various metabolic disorders in addition to diabetes. Protein therapeutic formulations, however, must generally be delivered subcutaneously and face many challenges both in the supply chain and in delivery. Several key impediments to improving protein therapeutics are denaturing, temperature-dependent deamidation, agglomeration and amyloid formation, enzymatic digestion, and poor pharmacokinetics.98 Zinc staple motifs may provide a solution to some of these problems by stabilizing the protein. Additional research will be needed to investigate the pharmacokinetic properties of zinc-stapled insulin formulations in human subjects and the application of this nanobiotechnology to other protein therapeutics.
Nature is rich with biological systems that employ bottom-up self-assembly with exquisite precision. The cell’s ability to regulate polymerization and depolymerization of cytoskeletal microfilaments and microtubules, for example, underlies cell motility and mitosis (Fig. 6C). The growing database of biological structures and their nanoscale organization within the cell and extracellular matrix provides a catalog of what may in principle be achieved through bottom-up protein engineering. The principles of supramolecular chemistry extend beyond peptides and proteins to other classes of polymers and heteropolymers. A long-standing vision for the treatment of diabetes mellitus has been the notion of a “smart insulin depot” from which the hormone would be released when and only when blood glucose concentration is high, thus mitigating the risk of hypoglycemia.99,100 As in an algorithm-controlled closed-loop pump system, an ideal glucose-responsive depot would provide regulated insulin release as a function of extent of hyperglycemia and so mimic the function of pancreatic β-cells as mediated by glucokinase-coupled measurement of the ambient tissue glucose concentration.101 The pioneering embodiment of this idea consisted of an oligoglycoslyated insulin bound to the lectin Concanavalin A.99,100 Competition between free glucose and bound insulin adducts resulted in displacement of the hormone. A related mechanism employed a polymer containing Concanavalin A bound to dextran molecules; binding of exogenous glucose molecules to the dextran induce a gel-sol transition that in turn enabled the encapsulated insulin to diffuse out.102 A pH-sensitive hydrogel has also been described whose volume decreases at higher glucose concentrations: glucose oxidase incorporated into the matrix thereupon oxidizes the entering glucose to gluconic acid, lowering the pH of the gel and in turn causing its pH-sensitive polymers to contract and expel its contents.103 Although to our knowledge none of these possibilities has entered clinical trials, “smart” glucose-responsive insulin/polymer reservoirs in principle define a new frontier of supramolecular chemistry in human therapeutics.
Concluding remarks
The discovery of insulin in 1922 was a transformational event in the development of molecular medicine and its broad public support.104 The pioneering efforts of the late D. C. Hodgkin to decipher the atomic-level structure of insulin and its conformational repertoire extended over six decades and engaged an international network of laboratories,3 notably including research teams in the People’s Republic of China during its years of isolation from the West.105,106 Given this long history, it seems remarkable that this small globular protein continues to inspire molecular innovation, motivated by clinical urgency. Unmet needs in the pharmacology of insulin relate directly to risks faced by patients with diabetes mellitus. Short-term risks reflect daily steering between treatment-related hypoglycemia (with its neurocognitive and adrenergic symptoms), on the one hand, and hyperglycemic excursions on the other. In addition to acute metabolic decompensation (diabetic ketoacidosis in Type 1 diabetes mellitus and hyperosmolar coma in Type 2), hyperglycemic excursions are associated with omnipresent long-term risks of microvascular, macrovascular, and neurologic complications. Next-generation insulin analogs in affluent societies seek to enhance the convenience and safety by which patients can navigate their daily lives to achieve metabolic control. The design and development of ultra-rapid insulin analog formulations and ultra-flat basal insulin analog formulations promise to enable patients to mimic with greater precision endogenous mechanisms of hormonal regulation. The cost-effectiveness of such technologies, a general issue of increasing societal concern107–109, will require population-based analysis of relative impact on rates of complications leading to expensive interventions and long-term disability.110
Principles of protein dynamics and stability will come to the fore in yet another dimension of the diabetes challenge: the emerging pandemic of diabetes mellitus in the developing world.111 The insulin analogs discussed in this review, including those under investigation, were designed to meet standards of stability appropriate in the developed world. Whereas for patients in affluent societies thermal degradation of insulin and insulin analogs is uncommon, the majority of patients in the coming decades will be living in underprivileged regions of the developing world. In such regions intertwined scientific, technical, and societal challenges are posed by the cold chain of insulin delivery, storage, and use in the absence of refrigeration or a reliable electrical grid.112–114 Given this humanitarian need and its growing scale, we anticipate that third-generation insulin analogs must combine ultra-stability with optimized pharmacokinetic properties. Such efforts are likely to require the present understanding of the native state of insulin to be extended to non-native states, including metastable partial folds and amyloid.55 Because the susceptibility of insulin analogs to chemical and physical degradation correlates with their propensity to undergo conformational fluctuations,115 structural studies of the rugged landscape of protein folding and misfolding, a foundational topic in biophysics, thus promise to define a new frontier of translational research with application to global health. At this frontier design of insulin analogs – and their self-organization within a subcutaneous depot – will require the integration of biochemical principles with the emergent perspective of nanotechnology. We anticipate that such molecular technologies will enable patients in both the developed and developing to navigate with ever-increasing safety between the Scylla of hyperglycemia and Charybdus of hypoglycemic episodes.
Acknowledgements
We thank Ms. Martha Raymond and Ms. Crista Moeller with assistance in the preparation of the manuscript. This work was supported by grants from the National Institutes of Health and American Diabetes Association to one of the authors (M.A.W.). We thank Profs. D.H. O’Day and D.L. Caspar for their kind permission to use images in Figure 2 and gratefully acknowledge Dr. N. Phillips and Dr. Z.L. Wan for helpful discussion. D.F.B. and A.R.W. respectively thank R.W. Berenson (Chief Operating Officer, Thermalin Diabetes, LLC, Cleveland, OH) and Dr. T. Heller (NIDDK Liver Diseases Branch, National Institutes of Health, Bethesda, MD) for their encouragement. This article is a contribution from the Cleveland Center for Membrane and Structural Biology and CWRU Comprehensive Cancer Center.
Footnotes
Conflict of Interest Statement
The intellectual property pertaining to [HisA4, HisA8]-human insulin and its long-acting formulation is owned by Case Western Reserve University and licensed to Thermalin Diabetes, LLC. M.A.W. holds shares in and is Chief Scientific Officer of Thermalin Diabetes, LLC.; he has also been a consultant to Merck, Inc. and the DEKA Research and Development Corp. A.R.W. is the daughter of M.A.W. D.F.B. is the son of R. Berenson, Chief Executive Office of Thermalin Diabetes, LLC; D.F.B. has an ownership interest in Venzyme Catalyst, LLC, which holds shares in Thermalin Diabetes, LLC. The authors otherwise declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Adams MJ, Blundell TL, Dodson EJ, et al. Structure of rhombohedral 2 zinc insulin crystals. Nature. 1969;224:491–495. [Google Scholar]
- 2.Blundell TL, Cutfield JF, Cutfield SM, et al. Atomic positions in rhombohedral 2-zinc insulin crystals. Nature. 1971;231:506–511. doi: 10.1038/231506a0. [DOI] [PubMed] [Google Scholar]
- 3.Baker EN, Blundell TL, Cutfield JF, et al. The structure of 2Zn pig insulin crystals at 1.5 Å resolution. Philos. Trans. R. Soc. Lond. B Biol. Sci. 1988;319:369–456. doi: 10.1098/rstb.1988.0058. [DOI] [PubMed] [Google Scholar]
- 4.Brange J, Skelbaek-Pedersen B, Langkjaer L, et al. Galenics of insulin: the physico-chemical and pharmaceutical aspects of insulin and insulin preparations. Berlin: Springer-Verlag; 1987. [Google Scholar]
- 5.Dodson GG, Dodson EJ, Turkenburg JP, et al. Molecular recognition in insulin assembly. Biochem. Soc. Trans. 1993;21:609–614. doi: 10.1042/bst0210609. [DOI] [PubMed] [Google Scholar]
- 6.Brange J. The new era of biotech insulin analogues. Diabetologia. 1997;40:S48–S53. doi: 10.1007/s001250051400. [DOI] [PubMed] [Google Scholar]
- 7.Freeman JS. Insulin analog therapy: Improving the match with physiologic insulin secretion. Journal of the American Osteopathic Association. 2009;109:26–36. [PubMed] [Google Scholar]
- 8.NIDDK, N.I.o.D.a.D.a.K.D. Advances and emerging opportunities in diabetes research: a Strategic Planning report of the DMICC. Committee, D. M. I. C., Ed. Washington, D.C.: 2011. [Google Scholar]
- 9.ADA, A.D.A. American Diabetes Association Scientific Sessions 2011. San Diego, California: 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Diabetes Control Group and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl. J. Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 11.Nathan DM, Cleary PA, Backlund JY, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N. Engl. J. Med. 2005;353:2643–2653. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gerstein HC, Miller ME, Genuth S, et al. Long-term effects of intensive glucose lowering on cardiovascular outcomes. N. Engl. J. Med. 2011;364:818–828. doi: 10.1056/NEJMoa1006524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riddle MC. Effects of intensive glucose lowering in the management of patients with type 2 diabetes mellitus in the Action to Crontrol Cardiovascular Risk in Diabetes (ACCORD) trial. Circulation. 2010;122:844–846. doi: 10.1161/CIRCULATIONAHA.110.960138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saltiel AR. New perspectives into the molecular pathogenesis and treatment of type-2 diabetes. Cell. 2001;104:517–529. doi: 10.1016/s0092-8674(01)00239-2. [DOI] [PubMed] [Google Scholar]
- 15.Nicollerat JA. Implications of the United Kingdom Prospective Diabetes Study (UKPDS) results on patient management. Diabetes Educ. 2000;26(Suppl):8–10. [PubMed] [Google Scholar]
- 16.Ismail-Beigi F, Moghissi E, Tiktin M, et al. Individualizing glycemic targets in type 2 diabetes mellitus: implications of recent clinical trials. Ann. Intern. Med. 2011;154:554–559. doi: 10.7326/0003-4819-154-8-201104190-00007. [DOI] [PubMed] [Google Scholar]
- 17.Creighton TE. Protein Structure: a Practical Approach. Oxford: IRL Press at Oxford University Press; 1997. [Google Scholar]
- 18.Brange J, Hansen JF, Havelund S, et al. Studies of insulin fibrillation process. In: Brunetti P, Waldhäusl WK, editors. Advanced models for the therapy of insulin-dependent diabeses. New York: Raven Press; 1987. pp. 85–90. [Google Scholar]
- 19.Brems DN, Alter LA, Beckage MJ, et al. Altering the association properties of insulin by amino acid replacement. Protein Eng. 1992;5:527–533. doi: 10.1093/protein/5.6.527. [DOI] [PubMed] [Google Scholar]
- 20.DeFelippis MR, Chance RE, Frank BH. Insulin self-association and the relationship to pharmacokinetics and pharmacodynamics. Crit. Rev. Ther. Drug Carrier Syst. 2001;18:201–264. [PubMed] [Google Scholar]
- 21.DiMarchi RD, Chance RE, Long HB, et al. Preparation of an insulin with improved pharmacokinetics relative to human insulin through consideration of structural homology with insulin-like growth factor I. Horm. Res. 1994;41(Suppl. 2):93–96. doi: 10.1159/000183967. [DOI] [PubMed] [Google Scholar]
- 22.Heinemann L, Heise T, Jorgensen LN, et al. Action profile of the rapid acting insulin analogue: human insulin B28 Asp. Diabet. Med. 1993;10:535–539. doi: 10.1111/j.1464-5491.1993.tb00116.x. [DOI] [PubMed] [Google Scholar]
- 23.Owens D, Vora J. Insulin aspart: a review. Expert Opin. Drub Metab. Toxicol. 2006;2:793–804. doi: 10.1517/17425255.2.5.793. [DOI] [PubMed] [Google Scholar]
- 24.Barlocco D. Insulin glulisine. Aventis Pharma. Curr. Opin. Investig. Drugs. 2003;4:1240–1244. [PubMed] [Google Scholar]
- 25.Helms KL, Kelley KW. Insulin glulisine: an evaluation of its pharmacodynamic properties and clinical application. Ann. Pharmacother. 2009;43:658–668. doi: 10.1345/aph.1E662. [DOI] [PubMed] [Google Scholar]
- 26.Garg S, Ampudia-Blasco FJ, Pfohl M. Rapid-acting insulin analogues in Basal-bolus regimens in type 1 diabetes mellitus. Endocr. Pract. 2010;16:486–505. doi: 10.4158/EP09294.RA. [DOI] [PubMed] [Google Scholar]
- 27.Colquitt J, Royle P, Waugh N. Are analogue insulins better than soluble in continuous subcutaneous insulin infusion? Results of a meta-analysis. Diab. Med. 2003;20:863–866. doi: 10.1046/j.1464-5491.2003.01018.x. [DOI] [PubMed] [Google Scholar]
- 28.Ciszak E, Beals JM, Frank BH, et al. Role of C-terminal B-chain residues in insulin assembly: the structure of hexameric LysB28ProB29-human insulin. Structure (Lond.) 1995;3:615–622. doi: 10.1016/s0969-2126(01)00195-2. [DOI] [PubMed] [Google Scholar]
- 29.Whittingham JL, Edwards DJ, Antson AA, et al. Interactions of phenol and m-cresol in the insulin hexamer, and their effect on the association properties of B28 pro --> Asp insulin analogues. Biochemistry. 1998;37:11516–11523. doi: 10.1021/bi980807s. [DOI] [PubMed] [Google Scholar]
- 30.Brader ML, Dunn MF. Insulin hexamers: new conformations and applications. Trends Biochem. Sci. 1991;16:341–345. doi: 10.1016/0968-0004(91)90140-q. [DOI] [PubMed] [Google Scholar]
- 31.Bentley G, Dodson E, Dodson G, et al. Structure of insulin in 4-zinc insulin. Nature. 1976;261:166–168. doi: 10.1038/261166a0. [DOI] [PubMed] [Google Scholar]
- 32.Derewenda U, Derewenda Z, Dodson EJ, et al. Phenol stabilizes more helix in a new symmetrical zinc insulin hexamer. Nature. 1989;338:594–596. doi: 10.1038/338594a0. [DOI] [PubMed] [Google Scholar]
- 33.Hua QX, Shoelson SE, Kochoyan M, et al. Receptor binding redefined by a structural switch in a mutant human insulin. Nature. 1991;354:238–241. doi: 10.1038/354238a0. [DOI] [PubMed] [Google Scholar]
- 34.Hua QX, Hu SQ, Frank BH, et al. Mapping the functional surface of insulin by design: structure and function of a novel A-chain analogue. J Mol. Biol. 1996;264:390–403. doi: 10.1006/jmbi.1996.0648. [DOI] [PubMed] [Google Scholar]
- 35.Olsen HB, Ludvigsen S, Kaarsholm NC. Solution structure of an engineered insulin monomer at neutral pH. Biochemistry. 1996;35:8836–8845. doi: 10.1021/bi960292+. [DOI] [PubMed] [Google Scholar]
- 36.Chothia C, Lesk AM, Dodson GG, et al. Transmission of conformational change in insulin. Nature. 1983;302:500–505. doi: 10.1038/302500a0. [DOI] [PubMed] [Google Scholar]
- 37.Jacoby E, Hua QX, Stern AS, et al. Structure and dynamics of a protein assembly. 1H-NMR studies of the 36 kDa R6 insulin hexamer. J. Mol. Biol. 1996;258:136–157. doi: 10.1006/jmbi.1996.0239. [DOI] [PubMed] [Google Scholar]
- 38.Brader ML, Kaarsholm NC, Lee RW, et al. Characterization of the R-state insulin hexamer and its derivatives. The hexamer is stabilized by heterotropic ligand binding interactions. Biochemistry. 1991;30:6636–6645. doi: 10.1021/bi00241a002. [DOI] [PubMed] [Google Scholar]
- 39.Hassiepen U, Federwisch M, Mulders T, et al. The lifetime of insulin hexamers. Biophys. J. 1999;77:1638–1654. doi: 10.1016/S0006-3495(99)77012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Richards JP, Stickelmeyer MP, Flora DB, et al. Self-association properties of monomeric insulin analogs under formulation conditions. Pharm. Res. 1998;15:1434–1441. doi: 10.1023/a:1011961923870. [DOI] [PubMed] [Google Scholar]
- 41.Cosmatos A, Ferderigos N, Katsoyannis PG. Chemical synthesis of [des(tetrapeptide B27--30), Tyr(NH2)26-B] and [des(pentapeptide B26--30), Phe(NH2)25-B] bovine insulins. Int. J. Protein Res. 1979;14:457–471. doi: 10.1111/j.1399-3011.1979.tb01957.x. [DOI] [PubMed] [Google Scholar]
- 42.Fischer WH, Saunders D, Brandenburg D, et al. A shortened insulin with full in vitro potency. Biol. Chem. Hoppe Seyler. 1985;366:521–525. doi: 10.1515/bchm3.1985.366.1.521. [DOI] [PubMed] [Google Scholar]
- 43.Elleri D, Dunger DB, Hovorka R. Closed-loop insulin delivery for treatment of type 1 diabetes. BMC Med. 2011;9:120. doi: 10.1186/1741-7015-9-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schaepelynck P, Darmon P, Molines L, et al. Advances in pump technology: insulin patch pumps, combined pumps and glucose sensors, and implanted pumps. Diabetes Metab. 2011;37(Suppl 4):S85–S93. doi: 10.1016/S1262-3636(11)70972-7. [DOI] [PubMed] [Google Scholar]
- 45.Brown L, Edelman ER. Optimal control of blood glucose: the diabetic patient or the machine? Sci. Transl. Med. 2010;2 doi: 10.1126/scitranslmed.3001083. 27ps18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Scutcher M, Vasilakis-Scaramozza C, Sullivan K. Group DR. Diabetic Complications. Vital Biopharmaceutical Insights and Analytics for Experts from Experts. 2011 [Google Scholar]
- 47.Raz I, Weiss R, Yegorchikov Y, et al. Effect of a local heating device on insulin and glucose pharmacokinetic profiles in an open-label, randomized, two-period, one-way crossover study in patients with type 1 diabetes using continuous subcutaneous insulin infusion. Clin. Ther. 2009;31:980–987. doi: 10.1016/j.clinthera.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 48.Jakobsen LA, Jensen A, Larsen LE, et al. Effect of cutaneous blood flow on absorption of insulin: a methodological study in healthy male volunteers. Int. J. Physiol. Pathophysiol. Pharmacol. 2011;3:257–265. [PMC free article] [PubMed] [Google Scholar]
- 49.Vaughn DE, Muchmore DB. Use of recombinant human hyaluronidase to accelerate rapid insulin analogue absorption: experience with subcutaneous injection and continuous infusion. Endocr. Pract. 2011;17:914–921. doi: 10.4158/EP11297.RA. [DOI] [PubMed] [Google Scholar]
- 50.Pettis RJ, Ginsberg B, Hirsch L, et al. Intradermal microneedle delivery of insulin lispro achieves faster insulin absorption and insulin action than subcutaneous injection. Diabetes Technol Ther. 2011;13:435–442. doi: 10.1089/dia.2010.0184. [DOI] [PubMed] [Google Scholar]
- 51.Engwerda EE, Abbink EJ, Tack CJ, et al. Improved pharmacokinetic and pharmacodynamic profile of rapid-acting insulin using needle-free jet injection technology. Diabetes Care. 2011;34:1804–1808. doi: 10.2337/dc11-0182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hompesch M, McManus L, Pohl R, et al. Intra-individual variability of the metabolic effect of a novel rapid-acting insulin (VIAject) in comparison to regular human insulin. J. Diabetes Sci. Technol. 2008;2:568–571. doi: 10.1177/193229680800200406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Heinemann L, Nosek L, Flacke F, et al. U-100, pH-Neutral formulation of VIAject((R)) : faster onset of action than insulin lispro in patients with type 1 diabetes. Diabetes Obes. Metab. 2011 doi: 10.1111/j.1463-1326.2011.01516.x. [DOI] [PubMed] [Google Scholar]
- 54.Hua QX, Nakagawa SH, Jia W, et al. Design of an active ultrastable single-chain insulin analog: synthesis, structure, and therapeutic implications. J. Biol. Chem. 2008;283:14703–14716. doi: 10.1074/jbc.M800313200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang Y, Petkova A, Huang K, et al. An Achilles' Heel in an amyloidogenic protein and its repair. Insulin dynamics, misfolding, and therapeutic design. J. Biol. Chem. 2010;285:10806–10821. doi: 10.1074/jbc.M109.067850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pollock RF, Erny-Albrecht KM, Kalsekar A, et al. Long-acting insulin analogs: a review of "real-world" effectiveness in patients with type 2 diabetes. Curr. Diab. Rev. 2011;7:61–64. doi: 10.2174/157339911794273892. [DOI] [PubMed] [Google Scholar]
- 57.King AB, Armstrong DU. Basal bolus dosing: a clinical experience. Curr. Diabetes Rev. 2005;1:215–220. doi: 10.2174/1573399054022794. [DOI] [PubMed] [Google Scholar]
- 58.Baxter MA. The role of new basal insulin analogues in the initiation and optimization of insulin therapy in type 2 diabetes. Acta. Diabetol. 2008;45:253–268. doi: 10.1007/s00592-008-0052-9. [DOI] [PubMed] [Google Scholar]
- 59.Pontiroli AE, Miele L, Morabito A. Increase of body weight during the first year of intensive insulin treatment in type 2 diabetes: systematic review and meta-analysis. Diabetes Obes. Metab. 2011;13:1008–1019. doi: 10.1111/j.1463-1326.2011.01433.x. [DOI] [PubMed] [Google Scholar]
- 60.Markussen J, Diers I, Hougaard P, et al. Soluble, prolonged-acting insulin derivatives. III. Degree of protraction, crystallizability and chemical stability of insulins substituted in positions A21, B13, B23, B27 and B30. Protein Eng. 1988;2:157–166. doi: 10.1093/protein/2.2.157. [DOI] [PubMed] [Google Scholar]
- 61.Owens DR, Griffiths S. Insulin glargine (Lantus) Int. J. Pract. 2002;56:460–466. [PubMed] [Google Scholar]
- 62.Goykhman S, Drincic A, Desmangles JC, et al. Insulin Glargine: a review 8 years after its introduction. Expert Opin Pharmacother. 2009;10:705–718. doi: 10.1517/14656560902775677. [DOI] [PubMed] [Google Scholar]
- 63.Heinemann L, Linkeschova R, Rave K, et al. Time-action profile of the long-acting insulin analog insulin glargine (HOE901) in comparison with those of NPH insulin and placebo. Diab. Care. 2000;23:644–649. doi: 10.2337/diacare.23.5.644. [DOI] [PubMed] [Google Scholar]
- 64.Maggon K. Global Diabetes Market Review 2008 & World Top Ten Diabetes drugs:World Top Ten diabetic drug brands, market trends and top companies 2008. Vol. 93. Guild (KPG), Knol Publishing; 2011. [Google Scholar]
- 65.Kohn WD, Micanovic R, Myers SL, et al. pI-shifted insulin analogs with extended in vivo time action and favorable receptor selectivity. Peptides (N. Y.) 2007;28:935–948. doi: 10.1016/j.peptides.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 66.Havelund S, Plum A, Ribel U, et al. The mechanism of protraction of insulin detemir, a long-acting, acylated analog of human insulin. Pharm. Res. 2004;21:1498–1504. doi: 10.1023/b:pham.0000036926.54824.37. [DOI] [PubMed] [Google Scholar]
- 67.Whittingham JL, Jonassen I, Havelund S, et al. Crystallographic and solution studies of N-lithocholyl insulin: a new generation of prolonged-acting human insulins. Biochemistry. 2004;43:5987–5995. doi: 10.1021/bi036163s. [DOI] [PubMed] [Google Scholar]
- 68.Markussen J, Jonassen I, Havelund S, et al., inventors. 6,620,780. U. S. A. patent. 2003 Date of application: Sept. 16, 2003.
- 69.Zinman B, Fulcher G, Rao PV, et al. Insulin degludec, an ultra-long-acting basal insulin, once a day or three times a week versus insulin glargine once a day in patients with type 2 diabetes: a 16-week, randomised, open-label, phase 2 trial. Lancet. 2011;377:924–931. doi: 10.1016/S0140-6736(10)62305-7. [DOI] [PubMed] [Google Scholar]
- 70.Birkeland KI, Home PD, Wendisch U, et al. Insulin degludec in type 1 diabetes: a randomized controlled trial of a new-generation ultra-long-acting insulin compared with insulin glargine. Diabetes Care. 2011;34:661–665. doi: 10.2337/dc10-1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Heise T, Tack CJ, Cuddihy R, et al. A new-generation ultra-long-acting basal insulin with a bolus boost compared with insulin glargine in insulin-naive people with type 2 diabetes: a randomized, controlled trial. Diabetes Care. 2011;34:669–674. doi: 10.2337/dc10-1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Flora DB, inventor. 6,444,641. U. S. A. patent. 2002 Date of application: Sept. 3, 2002.
- 73.Baker JC, Hanquier JM, inventors. 5,922,675. U. S. A. patent. 1999 Date of application: July 13, 1999.
- 74.Beals JM, DeFelippis MR, DiMarchi RD, et al., inventors. 2005/0014679. U. S. A. patent. 2005 Date of application: Jan. 20, 2005.
- 75.Kohn WD, Zhang L, DiMarchi RD, inventors. 2006/0217290. U. S. A. patent. 2006 Date of application: Sept. 28, 2006.
- 76.Seeman NC, Belcher AM. Emulating biology:building nanostructures from the bottom up. Proc. Natl. Acad. Sci. USA. 2002;99(Suppl. 2):6451–6455. doi: 10.1073/pnas.221458298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kurth DG. Metallo-supramolecular modules as a paradigm for materials science. Sci. Tech. Adv. Materials. 2008;Vol. 9 doi: 10.1088/1468-6996/9/1/014103. 014103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Phillips NB, Wan ZL, Whittaker L, et al. Supramolecular protein engineering: design of zinc-stapled insulin hexamers as a long acting depot. J. Biol. Chem. 2010;285:11755–11759. doi: 10.1074/jbc.C110.105825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Caspar DL, Namba K. Switching in the self-assembly of tobacco mosaic virus. Adv. Biophys. 1990;26:157–185. doi: 10.1016/0065-227x(90)90011-h. [DOI] [PubMed] [Google Scholar]
- 80.Sotomayor M, Schulten K. The allosteric role of the Ca2+ switch in adhesion and elasticity of C-cadherin. Biophys J. 2008;94:4621–4633. doi: 10.1529/biophysj.107.125591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Conrady DG, Brescia CC, Horii K, et al. A zinc-dependent adhesion module is responsible for intercellular adhesion in staphylococcal biofilms. Proc. Natl. Acad. Sci. USA. 2008;105:19456–19461. doi: 10.1073/pnas.0807717105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chuan YP, Fan YY, Lua LH, et al. Virus assembly occurs following a pH- or Ca2+-triggered switch in the thermodynamic attraction between structural protein capsomeres. J. R. Soc. Interface. 2010;7:409–421. doi: 10.1098/rsif.2009.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Regan L. The design of metal-binding sites in proteins. Annu. Rev. Biophys. Biomol. Struct. 1993;22:257–281. doi: 10.1146/annurev.bb.22.060193.001353. [DOI] [PubMed] [Google Scholar]
- 84.Berg JM. Proposed structure for the zinc-binding domains form transcription factor IIIA and related proteins. Proc. Natl. Acad. Sci. USA. 1988;85:99–102. doi: 10.1073/pnas.85.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pavletich NP, Pabo CO. Zinc finger-DNA recognition: crystal structure of a Zif268-DNA complex at 2.1 A. Science. 1991;252:809–817. doi: 10.1126/science.2028256. [DOI] [PubMed] [Google Scholar]
- 86.Ravasi T, Huber T, Zavolan M, et al. Systematic characterization of the zinc-finger-containing proteins in the mouse transcriptome. Genome Res. 2003;13:1430–1432. doi: 10.1101/gr.949803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zib I, Raskin P. Novel insulin analogues and its mitogenic potential. Diab. Obes. Metab. 2006;8:611–620. doi: 10.1111/j.1463-1326.2005.00567.x. [DOI] [PubMed] [Google Scholar]
- 88.Nagel JM, Staffa J, Renner-Muller I, et al. Insulin glargine and NPH insulin increase to a similar degree epithelial cell proliferation and aberrant crypt foci formation in colons of diabetic mice. Horm. Cancer. 2010;1:320–330. doi: 10.1007/s12672-010-0020-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Teng JA, Hou RL, Li DL, et al. Glargine promotes proliferation of breast adenocarcinoma cell line MCF-7 via AKT activation. Horm. Metab. Res. 2011;43:519–523. doi: 10.1055/s-0031-1280780. [DOI] [PubMed] [Google Scholar]
- 90.Dawson LK, Hamilton LA. Risk of cancer in patients receiving insulin glargine. Am. J. Health. Syst. Pharm. 2010;67:2025–2031. doi: 10.2146/ajhp100109. [DOI] [PubMed] [Google Scholar]
- 91.Suissa S, Azoulay L, Dell'Aniello S, et al. Long-term effects of insulin glargine on the risk of breast cancer. Diabetologia. 2011;54:2254–2262. doi: 10.1007/s00125-011-2190-9. [DOI] [PubMed] [Google Scholar]
- 92.Lind M, Fahlen M, Eliasson B, et al. The relationship between the exposure time of insulin glargine and risk of breast and prostate cancer: An observational study of the time-dependent effects of antidiabetic treatments in patients with diabetes. Prim. Care Diabetes. 2011 doi: 10.1016/j.pcd.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 93.Blin P, Lassalle R, Dureau-Pournin C, et al. Insulin glargine and risk of cancer: a cohort study in the French National Healthcare Insurance Database. Diabetologia. 2012 doi: 10.1007/s00125-011-2429-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ruiter R, Visser LE, van Herk-Sukel MP, et al. Risk of cancer in patients on insulin glargine and other insulin analogues in comparison with those on human insulin: results from a large population-based follow-up study. Diabetologia. 2012;55:51–62. doi: 10.1007/s00125-011-2312-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Simon D. Diabetes treatment with insulin glargine and risk of malignancy: methodological pitfalls and ethical issues. Diabetologia. 2010;59:1732–1744. doi: 10.1007/s00125-009-1572-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Renehan AG. Insulin analogues and cancer risk: the emergence of second-generation studies. Diabetologia. 2012;55:7–9. doi: 10.1007/s00125-011-2352-9. [DOI] [PubMed] [Google Scholar]
- 97.Berenson D, Weiss AR, Weiss MA. Zinc-stapled insulin: therapeutic application of supramolecular protein engineering. Biotech International. 2011 [Google Scholar]
- 98.Leader B, Baca QJ, Golan DE. Protein therapeutics: a summary and pharmacological classification. Nat. Rev. Drug Discov. 2008;7:21–39. doi: 10.1038/nrd2399. [DOI] [PubMed] [Google Scholar]
- 99.Brownlee M, Cerami A. A glucose-controlled insulin-delivery system: semisynthetic insulin bound to lectin. Science. 1979;206:1190–1191. doi: 10.1126/science.505005. [DOI] [PubMed] [Google Scholar]
- 100.Brownlee M, Cerami A. Glycosylated insulin complexed to Concanavalin A. Biochemical basis for a closed-loop insulin delivery system. Diabetes. 1983;32:499–504. doi: 10.2337/diab.32.6.499. [DOI] [PubMed] [Google Scholar]
- 101.Matschinsky F, Liang Y, Kesavan P, et al. Glucokinase as pancreatic beta cell glucose sensor and diabetes gene. J. Clin. Invest. 1993;92:2092–2098. doi: 10.1172/JCI116809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Taylor MJ, Tanna S, Sahota TS. UV cross-linked dextran methacrylate--concanavalin A methacrylamide gel materials for self-regulated insulin delivery. Drug. Dev. Ind. Pharm. 2008;34:73–82. doi: 10.1080/03639040701542101. [DOI] [PubMed] [Google Scholar]
- 103.You JO, Almeda D, Ye GJ, et al. Bioresponsive matrices in drug delivery. J Biol. Eng. 2010;4:15. doi: 10.1186/1754-1611-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bliss M. The Discovery of Insulin: twenty-fifth anniversary edition. Chicago: University of Chicago Press; 2007. [Google Scholar]
- 105.Rao Z. History of protein crystallography in China. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 2007;362:1035–1042. doi: 10.1098/rstb.2007.2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hua Q. Insulin: a small protein with a long journey. Protein Cell. 2010;1:537–551. doi: 10.1007/s13238-010-0069-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Radermecker RP, Scheen AJ. Continuous subcutaneous insulin infusion with short-acting insulin analogues or human regular insulin: efficacy, safety, quality of life, and cost-effectiveness. Diabetes Metab. Res. Rev. 2004;20:178–188. doi: 10.1002/dmrr.447. [DOI] [PubMed] [Google Scholar]
- 108.Hirsch IB. Insulin analogues. N. Engl. J. Med. 2005;352:174–183. doi: 10.1056/NEJMra040832. [DOI] [PubMed] [Google Scholar]
- 109.Leichter S. Is the use of insulin analogues cost-effective? Adv. Ther. 2008;25:285–299. doi: 10.1007/s12325-008-0043-9. [DOI] [PubMed] [Google Scholar]
- 110.Cameron CG, Bennett HA. Cost-effectiveness of insulin analogues for diabetes mellitus. CMAJ. 2009;180:400–407. doi: 10.1503/cmaj.081180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hua QX, Jia W, Weiss MA. Conformational dynamics of insulin. Front. Endocrin. 2011;2 doi: 10.3389/fendo.2011.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Osei K. Global epidemic of type 2 diabetes: implications for developing countries. Ethn. Dis. 2003;13:S102–S106. [PubMed] [Google Scholar]
- 113.Osei K, Schuster DP, Amoah AG, et al. Pathogenesis of type 1 and type 2 diabetes mellitus in sub-Saharan Africa: implication for transitional populations. J. Cardiovasc. Risk. 2003;10:85–96. doi: 10.1097/01.hjr.0000060841.48106.a3. [DOI] [PubMed] [Google Scholar]
- 114.Lefebvre P, Pierson A. The global challenge of diabetes. World Hosp. Health Serv. 2004;40:37–40. 42. [PubMed] [Google Scholar]
- 115.Brange J, Langkjoer L. Insulin structure and stability. Pharm. Biotechnol. 1993;5:315–350. doi: 10.1007/978-1-4899-1236-7_11. [DOI] [PubMed] [Google Scholar]
- 116.Derewenda U, Derewenda Z, Dodson GG, et al. Molecular structure of insulin: the insulin monomer and its assembly. Br. Med. Bull. 1989;45:4–18. doi: 10.1093/oxfordjournals.bmb.a072320. [DOI] [PubMed] [Google Scholar]
- 117.Wan Z, Huang K, Whittaker J, et al. The structure of a mutant insulin uncouples receptor binding from protein allostery. An electrostatic block to the TR transition. J. Biol. Chem. 2008;283:21198–21210. doi: 10.1074/jbc.M800235200. [DOI] [PMC free article] [PubMed] [Google Scholar]