Abstract
Background
Determining appropriate disposition for referred pediatric patients is difficult since it relies primarily on a telephone description of the patient. In this study, we evaluate the Transport Risk Assessment in Pediatrics (TRAP) score’s ability to assist in appropriate placement of these patients. This novel tool is derived from physiologic variables.
Objectives
To determine the feasibility of calculating a TRAP score and whether a higher score correlates with Pediatric Intensive Care Unit (PICU) admission.
Methods
We performed an observational study of pediatric patients transported by a specialized team to a tertiary care center and the feasibility of implementing the TRAP tool. Patients were eligible if transported by the pediatric specialty transport team for direct admission to the children’s hospital. The TRAP score was obtained either through chart review of transport team’s initial assessment or real-team by the transport team.
Results
A total of 269 patients were identified with 238 patients included in the study Using logistic regression, higher TRAP scores were associated with PICU admission (OR 1.40, p <0.001). Patients with a higher score were also less likely to leave the PICU within 24 hours (OR 0.79, p <0.001).
Conclusion
The TRAP score is a novel objective pediatric transport assessment tool where an elevated score is associated with PICU admission for greater than 24 hours. This score may assist with the triage decisions for transported pediatric patients.
Keywords: Pediatric, transport, disposition, score, intensive care
Background
The regionalization of care has been shown to reduce mortality and adverse outcomes in pediatric patients1–11, but creates heightened awareness around resource utilization in inter-facility transport. Thus, many tertiary care centers now use specialized transport teams that are specifically equipped to manage critically ill children during inter-facility transport. These teams have become direct extensions of the children’s hospital to provide stabilization and specialty critical care at the referring hospital and while en route to the accepting facility. Children are often transported from centers unaccustomed to assessing the severity of pediatric illness which can complicate transport decisions, specifically hospital disposition.
These disposition decisions may be facilitated with a standardized scoring system. In adults, the Rapid Acute Physiology Score (RAPS) has been shown to predict patient severity of illness and physiologic stability before and after critical care focused transport12. For neonatal patients, two similar objective scoring systems have been recently validated as predictors of mortality during transport13, 14. In contrast, no comparable standardized scoring system focuses specifically on the transport of pediatric patients. Only certain isolated pre-transport variables such as systolic blood pressure, respiratory rate, oxygen requirement, and altered mental status have been shown to be useful in predicting in-hospital mortality and major transport interventions for pediatric patients15. The current study evaluates the utility of a novel objective scoring tool, the Transport Risk Assessment in Pediatrics (TRAP) score, in determining the appropriate disposition of transported pediatric patients. We hypothesize that a higher TRAP score will correlate with the need for PICU admission.
Methods
Study approval was granted by the hospital investigational review board and informed consent was waived. The pediatric transport program was a unit-based team that completes 250 transports annually based at a pediatric tertiary care center. The center houses a 19 bed multi-subspecialty pediatric critical care unit, where the pediatric critical care attending physician functioned as medical control for the transport team. The transport team was led by a fellow level physician, pediatric critical care nurse practitioner or pediatric critical care nurse with advanced airway management and resuscitation skills. Other team members included critical care nurses and respiratory therapists, if needed. Medical control was available by telephone for direct communication with the team at all times. The transport team performed only ground transports for admission to the children’s hospital. The program supports 22 community based hospitals, of which approximately one quarter has inpatient pediatric services.
Patients were eligible if they were transported by the pediatric ground transport team and were directly admitted to the children’s hospital. Patients transported by air or by other ambulance crews were excluded. Trauma patients were also excluded since they were brought directly to the emergency department for trauma evaluation irrespective of their severity of illness.
Score development
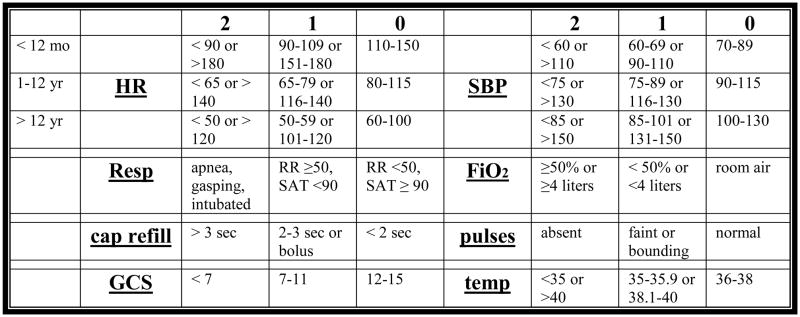
The TRAP score was derived to include previously identified pre-transport predictors of in-hospital mortality, which included systolic blood pressure, respiratory rate, oxygen requirement, and altered mental status15. Additionally, variables from other pediatric and neonatal scoring tools were added based on expert opinion at our institution13, 14, 16–18. The agreed upon tool contained eight components, each worth zero to two (0–2) points. As this was a feasibility study no weight was designated to individual components. The final transport scoring tool with all combined clinical fields ranged from a score of zero to 16, with 16 representing the most abnormal physiological variables (Figure 1).
Figure 1.
Transport Risk Assessment in Pediatrics (TRAP) score.
HR, heart rate; mo, month; yr, year; SBP, systolic blood pressure; Resp, respiratory; RR, respiratory rate; SAT, oxygen saturation; FiO2, fraction of inspired oxygen; cap, capillary; sec, second; GCS, Glasgow Coma Scale; temp, temperature in Celsius.
Study Design
This was an observational study of pediatric patients transported by a specialized ground transport team to a tertiary care center. Since this was a feasibility study, two time periods were selected that reflected the busiest months for our pediatric transport team. Transported patients were included between September 2008 and February 2009 and 1 year later between September 2009 and February 2010. Overall the goal was to evaluate the transport team’s first assessment and initial vital signs collected either through chart review or real time by the team. Patients had TRAP scores either retrospectively assigned based on the transport team’s medical chart documentation or in real time at the initial encounter with the patient. The score was completed by either a fellow level physician, advance practice nurse practitioner, or a lead critical care nurse. The pediatric critical care attending physician functioned as medical control for the transport team, and was blinded to the TRAP score. Final patient disposition decisions made by medical control were based on their clinical expertise and real-time discussions with the transport team.
Data were abstracted directly from medical records including transport flow sheets and notes. Information extracted was divided into categories consisting of patient characteristics, transport characteristics and outcome data. Patient characteristics included age, gender, weight, transport diagnosis category (respiratory, neurological, or other medical condition), and severity of illness measurements. The Pediatric Index of Mortality 2 (PIM2) score was used as a measure of severity of illness16.
Transport team composition and distance from the tertiary care center (one-way) were also evaluated. The relationship of the TRAP score and hospital disposition upon arrival to the hospital (i.e. PICU versus general pediatric ward) was the primary outcome of interest. Any change in disposition (defined as the transfer into or out of the PICU within 24 hours), in addition to PICU length of stay, hospital length of stay and mortality were evaluated as secondary outcomes.
Statistical Analysis
Descriptive statistics were done using chi-square and Fisher’s exact tests for categorical data and Student’s t-test or Mann-Whitney U test for continuous variables. In order to explore the relationship between the TRAP score and hospital disposition, logistic regression with the TRAP score as the main independent predictor was used. Similarly, a change in the disposition was analyzed using a logistic regression approach. We also evaluated if changes in level of care were to a higher level, for example to the PICU from the general care ward. As this was a feasibility study, the components of the TRAP score were not analyzed individually or weighted. Lastly, a receiver operating characteristic (ROC) curve was plotted to identify a TRAP score cut off point that maximizes sensitivity and specificity.
In all analyses, statistical significance was established using an alpha of 0.05. Statistical analyses were conducted using SAS 9.2 Software (SAS Institute Inc., Cary, NC) and SPSS Software Version 17 (IBM, Chicago, IL).
Results
Two hundred sixty-nine children were transported to a tertiary care center during the study period. Thirty-one children were excluded. Of those excluded, 9 were transported by air/other EMS crew, 3 were transported to another facility, 5 were canceled due to inclement weather, and 14 were brought directly to the emergency department for trauma evaluation.
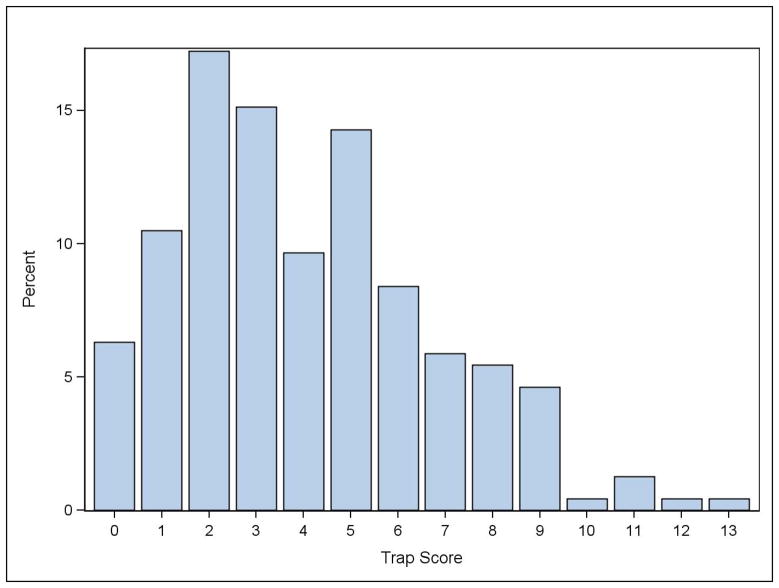
One hundred and eight patients (45%) had TRAP scores completed by the transport team leader at first encounter. The remaining scores were completed based on flow sheet documentation. The median age of transported patients was 2.8 years (IQR 0.7, 8.2). As expected, the majority of the children were transported for respiratory illnesses (58%). There were equal numbers of males and females. The median distance traveled to each referring institution was 33 miles (IQR 18, 41). The majority of the teams were physician led. The median predicted risk of mortality (as estimated by PIM2 score) was 0.9 % (IQR 0.2, 1.4). Further demographic and transport characteristics are reported in Table 1. The distribution of the TRAP score for the transported patients is shown in Figure 2A. The median score was 4.0 (IQR 2, 6), with no patient scoring higher than 13 points.
Table 1.
Baseline characteristics
| Characteristics | Transported Patients (n=238) |
|---|---|
| Age/years, Median (IQR) | 2.8 (0.7, 8.2) |
| Weight/kg, Median (IQR) | 15 (7.7, 28) |
| Sex, Male, n (%) | 128 (53.8%) |
| PIM2, Median (IQR) | 0.9 (0.2, 1.4) |
| Diagnosis, n (%) | |
| Respiratory | 137 (58%) |
| Neurologic | 45 (19%) |
| Other | 56 (24%) |
| Distance/miles, Median (IQR) | 33 (18, 41) |
| Team Composition, n (%) | |
| Physician lead | 146 (61%) |
| RN lead | 92 (39%) |
| TRAP Score, Median (IQR) | 4.0 (2, 6) |
Categorical data are reported with percentages in parentheses. For continuous data median values and interquartile ranges are reported. kg, kilograms; PIM2, Pediatric Index of Mortality 2; n, number; IQR, interquartile range; RN, registered nurse.
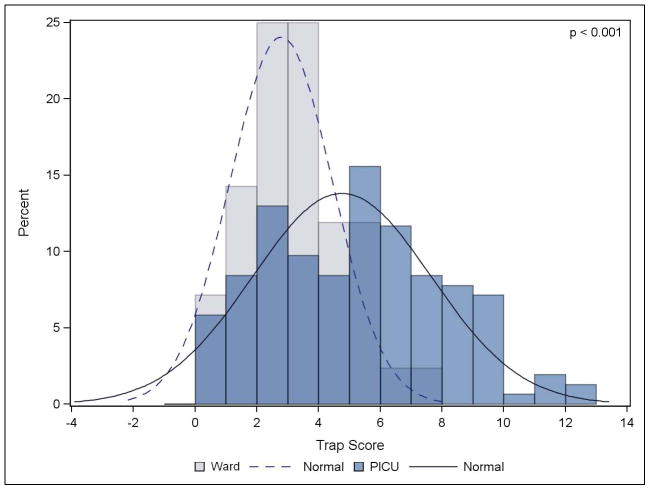
Figure 2.
TRAP score distribution: A, for all pediatric transports and B, by disposition. The P value represents the probability of a difference between the median TRAP scores distributed between the general pediatric ward vs. PICU.
Patient outcomes are listed in Table 2. Sixty-five percent of patients were admitted to the PICU. Forty-two percent of all patients changed their disposition within 24 hours of arriving to the hospital. However, only 3% of these patients required transfer from the general pediatric ward to the PICU, and all had TRAP scores ≤ 6. When TRAP scores were separated out based on disposition, the median score for general care ward patients was 3 (IQR 1, 5), whereas the median score for PICU patients was 5 (IQR 0, 10; P <0.001) (Figure 2B).
Table 2.
Outcome characteristics
| Characteristics | Transported Patients (n=238) |
|---|---|
| Disposition, n (%) | |
| PICU | 154 (65%) |
| Ward | 84 (35%) |
| Change Disposition in 24hrs, n (%) | |
| No | 139 (58%) |
| Yes | 99 (42%) |
| Higher Level of Care in 24hrs, n (%) | 7 (3%) |
| PICU stay/days, Median (IQR) | 2 (1, 4) |
| Hospital stay/days, Median (IQR) | 4 (3, 8) |
| In-hospital Mortality, n (%) | 4 (2%) |
Categorical data are reported with percentages in parentheses. For continuous data median values and intra-quartile ranges are reported. n, number; PICU, pediatric intensive care unit; IQR, interquartile range
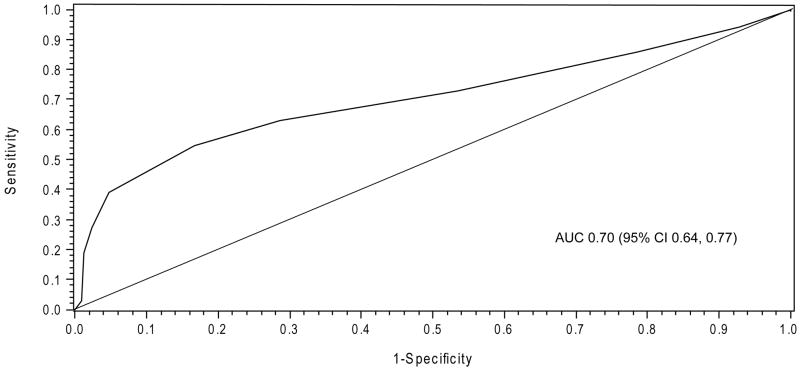
Bivariate analysis showed that higher TRAP scores were associated with admission to the PICU (OR 1.40, p <0.001) (Table 3). Longer distances were associated with lower odds of going to the PICU (OR 0.96, p<0.001). Bivariate analysis was also used to investigate if certain variables were associated with any change in disposition within 24 hours of admission (Table 4). A higher TRAP score was also found to be protective against any changes in level of care within 24 hours of admission (OR 0.79, p<0.001). In this analysis, high PIM2 scores were also protective against changes in disposition (OR 0.84, p<0.001). No additional patient characteristics were found to be associated with the need for higher level of PICU care in the patients initially admitted to the general care ward. The ROC curve for PICU admission using TRAP score as a predictor is shown in Figure 3. The area under the curve was 0.70 (95% CI 0.64, 0.77).
Table 3.
Bivariate associations between patient and transport characteristics and disposition to the PICU
| Characteristic | OR (95% CI) | P-value |
|---|---|---|
| Sex | 1.26 (0.74, 2.16) | 0.388 |
| Age, days | 1.00 (1.00, 1.00) | 0.675 |
| Weight, kg | 1.01 (0.99, 1.02) | 0.255 |
| TRAP | 1.40 (1.23, 1.60) | <0.001 |
| PIM2 | 1.15 (0.97, 1.35) | 0.099 |
| Diagnosis | ||
| Respiratory | Reference | |
| Neurologic | 1.01 (0.50, 2.04) | 0.929 |
| Other | 1.09 (0.56, 2.09) | 0.819 |
| Distance, miles | 0.96 (0.93, 0.98) | <0.001 |
CI, confidence interval; OR, odds ratio; kg, kilograms; TRAP, transport risk assessment in pediatrics; PIM2, Pediatric Index of Mortality 2.
Table 4.
Bivariate associations between patient and transport characteristics and changes in disposition within 24 hours
| Characteristic | OR (95% CI) | P-value |
|---|---|---|
| Sex | 1.61 (0.95, 2.71) | 0.075 |
| Age, days | 1.00 (1.00, 1.00) | 0.603 |
| Weight, kg | 1.01 (1.00, 1.02) | 0.231 |
| TRAP | 0.79 (0.71, 0.89) | <0.001 |
| PIM2 | 0.84 (0.71, 0.99) | 0.032 |
| Diagnosis | ||
| Respiratory | Reference | |
| Neurologic | 1.71 (0.87, 3.37) | 0.200 |
| Other | 1.23 (0.65, 2.31) | 0.841 |
| Distance, miles | 1.00 (0.98, 1.02) | 0.942 |
CI, confidence interval; OR, odds ratio; kg, kilograms; TRAP, transport risk assessment in pediatrics; PIM2, Pediatric Index of Mortality 2.
Figure 3.
Receiver Operator Curve for PICU admission.
AUC, area under the curve; CI, confidence interval.
Discussion
Patient disposition decisions have always proved difficult especially since these decisions impact both resource and funding allocations19. To assist or evaluate these decisions, some departments utilize scoring tools in their clinical decision making process. Thus far, existing scoring tools have led to an underestimation of the need for intensive care or major interventions when used solely for transport evaluation20. In this study, the TRAP score was designed to evaluate the potential for assisting disposition decisions for pediatric patients transported from one center to another. The TRAP score is a simplified tool that can be completed quickly by any member of the transport team at initial patient contact. Interestingly, during this study period our center was transitioning to a specialized nurse-led transport team. Over the last decade several studies have demonstrated that specialized teams improve outcomes whether led by specially trained nurses or physicians21–23. However, having an objective tool to assist with triage decisions previously made by the physician-led team may become more valuable.
The TRAP score which is based on the transport team’s initial assessment was evaluated both retrospectively through chart review and in real-time at team’s first contact. While this may have introduced bias it demonstrated the ease and availability of the variables used to calculate the TRAP score. It also minimized possible temporal phenomenon influencing transport decisions, such as a pandemic illness or transport personnel changes.
In this study we found a higher TRAP score associated with increased odds of admission to the PICU (OR 1.40, p<0.001). This translated to a 40% increase in odds of PICU admission for every point increase in the TRAP score. A higher TRAP score was also protective against changing disposition within 24 hours (OR 0.79, p<0.001). This can be interpreted to mean that patients with higher TRAP scores were appropriately triaged to the PICU since they remained for greater than 24 hours. We did not perform further adjusted analyses, since the other predictors needed for modeling were highly correlated. The area under the receiver operator curve demonstrated a fair predictive value of the TRAP score for PICU admission (AUC 0.704). It is clear from the ROC curve that this current un-weighted scoring tool will not substitute clinical judgment. Instead, it may provide additional information to assist the clinician’s disposition decision making.
Interestingly, the distance traveled from the referral center was also significantly associated with disposition. A shorter distance traveled was associated with PICU admission, while longer distances were linked to lower odds of PICU admission (OR 0.96, p<0.001). It is tempting to speculate that the remote referring institutions preferred modes of transportation different from ground transportation for critically ill patients. Though, only 9 patients were excluded from this study for transport by another team, whether by air or other EMS crew. Another possibility is that the remote referring centers did not have pediatric in-patient facilities, prompting the transfer of all pediatric patients even for low acuity. This will have to be further investigated.
In addition, we found that patients with higher severity of illness (PIM2) scores tended to stay in the PICU longer than 24 hours (OR 0.84, p=0.03). This score has been validated in the pediatric critical care population to predict mortality based on data collected within the first hour of admission16. And while initially validated in Australia, New Zealand and the United Kingdom, the PIM2 has since been used as a measurable predictor of mortality in the United States24, 25. This tool has not been validated specifically for transported patients, but was similarly used in a study involving specialized pediatric transport teams in England and Wales22. Since our transport team functions as a direct extension of the critical care unit, we felt that the PIM2 was an appropriate tool to standardize severity of illness among transported patients.
Surprisingly, we found a low overall PIM2 score predicting a mortality rate of 0.9% among our transported patient population. This was especially surprising given that 65% of the transported patients were subsequently admitted to the PICU. Over utilization of our PICU is the simplest explanation of this discrepancy. Further supporting this theory was the relatively high percentage of patients transferred out of the PICU within 24 hours of admission. Sixty percent of the 154 patients admitted initially to the PICU were transferred to the ward within 24 hours. Additionally, unpublished data from our institution showed an average mortality rate in our PICU as 2% compared to the published national average of 5%26. This also seemed apparent when we looked specifically at the TRAP score. There were 22 patients (14%) admitted to the PICU who had a TRAP score of 0 or 1. Of these, 73% were transferred out of the PICU within 24 hours. However, it is important to note that our institution does not have a step-down unit and hospital policy regarding monitoring often prevents some of these patients from being admitted to the general pediatric ward. For example, of the patients with low TRAP scores who required a longer than 24 hour admission in our PICU, none had a deterioration in clinical status, but all 6 patients required a level of monitoring higher than allowed on our general pediatric ward (Table 5). Furthermore, we found several patients with neurologic diagnoses and low TRAP scores admitted to the PICU for monitoring, indicating that the neurologic components of the score may need to be further explored.
Table 5.
Patients with low TRAP scores and PICU length of stay > 24 hours
| Patient | TRAP Score | Diagnosis | Reason For PICU Stay |
|---|---|---|---|
| 1 | 0 | Transverse Myelitis (T10 level) | Neurological Monitoring |
| 2 | 1 | Hemolytic Uremic Syndrome | Neurological Monitoring |
| 3 | 1 | End Stage Pontine Glioma/Bradycardia | Continuous Cardiovascular Monitoring & Neurological Monitoring |
| 4 | 1 | New Onset Partial Seizures/Status Epilepticus | Neurological Monitoring |
| 5 | 1 | Complex Partial Seizure/Prolonged Seizures | Neurological Monitoring |
| 6 | 1 | Deep Vein Thrombosis and Radiologic Evidence of Pulmonary Embolism | Heparin Drip and Increased Monitoring |
Finally, there are some additional limitations to our study that are worth mentioning. First, our transport program is currently growing but our geographical catchment area limits the amount of patients that can be included in this study. Cognizant of this, we attempted to enroll patients during our busiest transport months over a two-year period. However, this may have added unintended bias. Second, we did not collect data on the nine patients who were excluded due to alternative means of transport. Perhaps these patients had higher risks of mortality and biased our results. Third, disposition or changes in disposition are not standardized outcome measures even within the same institution. Fourth, patients who were admitted directly to the pediatric ward had PIM2 scores retrospectively calculated based on medical record documentation. We recognize that the PIM2 score has not been validated for general ward patients and this may have introduced bias. Lastly, we examined the feasibility and ease of TRAP score application in this observational study. Future studies examining outcomes with less institution variability and score component weighting, are warranted to test if the TRAP score is suitable for assisting with transport patient disposition at other centers. Furthermore, additional validation is needed prior to using the TRAP score to determine transport team composition or as an Emergency Medical Service triage tool.
We emphasize that this is a feasibility study and while the TRAP score may assist with triage decisions, aid in resource allocation, or assist with quality improvement assessments, it was not designed to make individual patient decisions. Those final decisions should remain in the hands of medical control.
Conclusion
In a busy critical care transport setting, standardized objective tools to match transported children with the appropriate level of care are necessary. The TRAP score is designed to assist with transport decisions, specifically patient disposition upon arrival to the accepting facility. We find high TRAP scores to be positively associated with the level of care a patient requires, as well as significantly associated with PICU admission lasting greater than 24 hours. Future studies are necessary to evaluate if this tool can appropriately assist with patient placement and whether it is applicable to additional transport programs.
Acknowledgments
This publication was made possible by CTSA Grant Number UL1 RR024139 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. This research is also partially supported by a NIH Training Grant, NIH T32 HL07272, The development of cardiovascular and pulmonary function (SK). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
We would like to thank all of the Yale-New Haven PICU nurses, therapists and physicians for their continued efforts with the Pediatric Transport Team.
Abbreviations
- TRAP
Transport Risk Assessment in Pediatrics
- PICU
Pediatric Intensive Care Unit
- PIM2
Pediatric Index of Mortality
- IQR
Interquartile Range
- OR
Odds Ratio
- CI
Confidence Interval
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Usher RH. The role of the neonatologist. Pediatric Clinics of North America. 1970;17(1):199–202. doi: 10.1016/s0031-3955(16)32386-0. [DOI] [PubMed] [Google Scholar]
- 2.Swyer PR. The regional organisation of special care for the neonate. Pediatric Clinics of North America. 1970;17(4):761–776. doi: 10.1016/s0031-3955(16)32479-8. [DOI] [PubMed] [Google Scholar]
- 3.Pollack MM, Alexander SR, Clarke N, Ruttimann UE, Tesselaar HM, Bachulis AC. Improved outcomes from tertiary center pediatric intensive care: A statewide comparison of tertiary and nontertiary care facilities. Critical Care Medicine. 1991;19(2):150–159. doi: 10.1097/00003246-199102000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Perloff WH, Brill J, Ackerman A, Briglia F, Dimand R, Flores R, et al. Consensus report for regionalization of services for critically ill or injured children. Pediatrics. 2000;105(1 I):152–155. [PubMed] [Google Scholar]
- 5.Usher R. Changing mortality rates with perinatal intensive care and regionalization. Semin Perinatol. 1977;1(3):309–319. [PubMed] [Google Scholar]
- 6.Tilford JM, Simpson PM, Green JW, Lensing S, Fiser DH. Volume-outcome relationships in pediatric intensive care units. Pediatrics. 2000;106(2 Pt 1):289–294. doi: 10.1542/peds.106.2.289. [DOI] [PubMed] [Google Scholar]
- 7.Consensus report for regionalization of services for critically ill or injured children. Council of the Society of Critical Care Medicine. Crit Care Med. 2000;28(1):236–239. doi: 10.1097/00003246-200001000-00040. [DOI] [PubMed] [Google Scholar]
- 8.Phibbs CS, Baker LC, Caughey AB, Danielsen B, Schmitt SK, Phibbs RH. Level and volume of neonatal intensive care and mortality in very-low-birth-weight infants. N Engl J Med. 2007;356(21):2165–2175. doi: 10.1056/NEJMsa065029. [DOI] [PubMed] [Google Scholar]
- 9.Potoka DA, Schall LC, Gardner MJ, Stafford PW, Peitzman AB, Ford HR. Impact of pediatric trauma centers on mortality in a statewide system. Journal of Trauma - Injury, Infection and Critical Care. 2000;49(2):237–245. doi: 10.1097/00005373-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Odetola Folafoluwa O, Miller William C, Davis Matthew M, Bratton Susan L. The Relationship between the Location of Pediatric Intensive Care Unit Facilities and Child Death from Trauma: A County-level Ecologic Study. The Journal of Pediatrics. 2005;147(1):74–77. doi: 10.1016/j.jpeds.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Johnson DL, Krishnamurthy S. Send severely head-injured children to a pediatric trauma center. Pediatr Neurosurg. 1996;25(6):309–314. doi: 10.1159/000121145. [DOI] [PubMed] [Google Scholar]
- 12.Rhee KJ, MacKenzie JR, Burney RE, Willits NH, O’Malley RJ, Reid N, et al. Rapid acute physiology scoring in transport systems. Critical Care Medicine. 1990;18(10):1119–1123. doi: 10.1097/00003246-199010000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Lee SK, Zupancic JAF, Pendray M, Thiessen P, Schmidt B, Whyte R, et al. Transport risk index of physiologic stability: A practical system for assessing infant transport care. Journal of Pediatrics. 2001;139(2):220–226. doi: 10.1067/mpd.2001.115576. [DOI] [PubMed] [Google Scholar]
- 14.Broughton SJ, Berry A, Jacobe S, Cheeseman P, Tarnow-Mordi WO, Greenough A. The mortality index for neonatal transportation score: A new mortality prediction model for retrieved neonates. Pediatrics. 2004;114(4):e424–e428. doi: 10.1542/peds.2003-0960-L. [DOI] [PubMed] [Google Scholar]
- 15.Orr RA, Venkataraman ST, McCloskey KA, Janosky JE, Dragotta M, Bills D, et al. Measurement of pediatric illness severity using simple pretransport variables. Prehospital Emergency Care. 2001;5(2):127–133. doi: 10.1080/10903120190939986. [DOI] [PubMed] [Google Scholar]
- 16.Slater A, Shann F, Pearson G. PIM2: A revised version of the Paediatric Index of Mortality. Intensive Care Medicine. 2003;29(2):278–285. doi: 10.1007/s00134-002-1601-2. [DOI] [PubMed] [Google Scholar]
- 17.Duncan H, Hutchison J, Parshuram CS. The pediatric early warning system score: A severity of illness score to predict urgent medical need in hospitalized children. Journal of Critical Care. 2006;21(3):271–278. doi: 10.1016/j.jcrc.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Pollack MM, Ruttimann UE, Getson PR. Pediatric risk of mortality (PRISM) score. Crit Care Med. 1988;16(11):1110–1116. doi: 10.1097/00003246-198811000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Meena Patel, Ian Maconochie. Triage in children. Trauma: Sage Publications, Ltd; 2008. pp. 239–245. [Google Scholar]
- 20.Orr RA, Venkataraman ST, Cinoman MI, Hogue BL, Singleton CA, McCloskey KA. Pretransport Pediatric Risk of Mortality (PRISM) score underestimates the requirement for intensive care or major interventions during interhospital transport. Critical Care Medicine. 1994;22(1):101–107. doi: 10.1097/00003246-199401000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Orr RA, Felmet KA, Han Y, McCloskey KA, Dragotta MA, Bills DM, et al. Pediatric specialized transport teams are associated with improved outcomes. Pediatrics. 2009;124(1):40–48. doi: 10.1542/peds.2008-0515. [DOI] [PubMed] [Google Scholar]
- 22.Ramnarayan P, Thiru K, Parslow RC, Harrison DA, Draper ES, Rowan KM. Effect of specialist retrieval teams on outcomes in children admitted to paediatric intensive care units in England and Wales: a retrospective cohort study. Lancet. 376(9742):698–704. doi: 10.1016/S0140-6736(10)61113-0. [DOI] [PubMed] [Google Scholar]
- 23.King BR, King TM, Foster RL, McCans KM. Pediatric and neonatal transport teams with and without a physician: a comparison of outcomes and interventions. Pediatr Emerg Care. 2007;23(2):77–82. doi: 10.1097/PEC.0b013e318030083d. [DOI] [PubMed] [Google Scholar]
- 24.Lacroix J, Cotting J. Severity of illness and organ dysfunction scoring in children. Pediatric Critical Care Medicine. 2005;6(3 SUPPL):S126–S134. doi: 10.1097/01.PCC.0000161287.61028.D4. [DOI] [PubMed] [Google Scholar]
- 25.Marcin JP, Pollack MM. Review of the acuity scoring systems for the pediatric intensive care unit and their use in quality improvement. Journal of Intensive Care Medicine. 2007;22(3):131–140. doi: 10.1177/0885066607299492. [DOI] [PubMed] [Google Scholar]
- 26.Pollack MM, Cuerdon TC, Getson PR. Pediatric intensive care units: results of a national survey. Crit Care Med. 1993;21(4):607–614. doi: 10.1097/00003246-199304000-00023. [DOI] [PubMed] [Google Scholar]