Abstract
Background
Despite evidence that several colorectal cancer (CRC) screening strategies can reduce CRC mortality, screening rates remain low. This study aimed to determine whether the approach by which screening is recommended influences adherence.
Methods
We used a cluster randomization design with clinic time block as the unit of randomization. Persons at average risk for development of CRC in a racially/ethnically diverse urban setting were randomized to receive recommendation for screening by fecal occult blood testing (FOBT), colonoscopy, or their choice of FOBT or colonoscopy. The primary outcome was completion of CRC screening within 12 months after enrollment, defined as performance of colonoscopy, or 3 FOBT cards plus colonoscopy for any positive FOBT result. Secondary analyses evaluated sociodemographic factors associated with completion of screening.
Results
A total of 997 participants were enrolled; 58% completed the CRC screening strategy they were assigned or chose. However, participants who were recommended colonoscopy completed screening at a significantly lower rate (38%) than participants who were recommended FOBT (67%) (P< .001) or given a choice between FOBT or colonoscopy (69%) (P< .001). Latinos and Asians (primarily Chinese) completed screening more often than African Americans. Moreover, non-white participants adhered more often to FOBT, while white participants adhered more often to colonoscopy.
Conclusions
The common practice of universally recommending colonoscopy may reduce adherence to CRC screening, especially among racial/ethnic minorities. Significant variation in overall and strategy-specific adherence exists between racial/ethnic groups; however, this may be a proxy for health beliefs and/or language. These results suggest that patient preferences should be considered when making CRC screening recommendations.
Trial Registration
clinicals.gov Identifier: NCT00705731
Colorectal cancer (CRC) is a nearly ideal disease for screening. It is a prevalent condition that can be identified and definitively treated during an asymptomatic phase, thereby preventing the morbidity and mortality associated with the unscreened clinical course of the disease.1 Previous studies have illustrated the benefit of screening using fecal occult blood testing (FOBT),2–6 flexible sigmoidoscopy (FS),7–9 and colonoscopy10–12 to decrease the incidence and/or mortality from CRC. Some national guidelines leave the choice of screening test to the clinician and patient,13–15 while others recommend colonoscopy as the preferred screening test.16 However, adherence to CRC screening is suboptimal, especially among racial/ethnic minorities.17,18
Evidence suggests that the adherence rate to CRC screening is generally more important than which strategy is used.19 It is unknown, however, whether giving patients a choice of screening modalities improves or reduces adherence. Giving choices through shared decision making can improve adherence by increasing patient engagement and allowing for individual patient preferences.20,21 In contrast, evidence also illustrates that providing options of similar value and characteristics can sometimes have a negative impact on adherence due to people defaulting to inertia, presumably because of confusion or indecision between choices.22–24 A small pilot study supported the latter hypothesis, in which patients allowed to choose among colonoscopy, FS, and FOBT were less likely to adhere to CRC screening than those recommended a single strategy.25
No US clinical trial has compared patient adherence to competing CRC screening strategies. Using a cluster randomization design, we examined the effects of recommending (1) FOBT, (2) colonoscopy, or (3) giving patients the choice of FOBT or colonoscopy on completion of CRC screening in persons at average risk for CRC. Our hypothesis was that patients given a choice of screening strategies would have a lower rate of adherence than patients recommended a single strategy. Given reports of lower adherence in racial/ethnic minorities, we also aimed to compare how the approach to screening affected completion in 4 racial/ethnic groups: African Americans, Hispanics, whites, and Asians (the latter being predominantly Chinese).
METHODS
STUDY PARTICIPANTS
This study was conducted in the San Francisco Community Health Network (CHN), the public health care system of the City and County of San Francisco, California. Participants were aged between 50 and 79 years and at average risk for development of CRC. To capture the majority of patients served by the CHN, research materials were produced in, and research staff were fluent in, English, Spanish, Cantonese, and Mandarin. Exclusion criteria included (1) a family history of CRC in a first-degree relative; (2) a personal history of colonic adenomatous polyps, CRC, or inflammatory bowel disease, symptoms for which colonoscopy or sigmoidoscopy would otherwise be performed (hematochezia, new-onset diarrhea, constipation or abdominal pain); or (3) compliant with CRC screening (FOBT within preceding 12 months, sigmoidoscopy or barium enema within 5 years, or colonoscopy within 10 years). In addition, patients with comorbid illness precluding endoscopic evaluation (myocardial infarction within 6 months, unstable angina. or congestive heart failure, chronic obstructive pulmonary disease requiring home oxygen) were excluded, as were patients with other diseases that limited their life expectancy to less than 10 years, as assessed by their primary health care provider (PCP).
Participant Identification
Eligible patients were identified by screening the patient panels of participating PCPs using the computerized clinical databases of the CHN. Potential participants were verified to be candidates for CRC screening by their PCP.
Participant Solicitation
Research assistants approached patients while they were waiting to be seen by their PCP. Participants provided written consent allowing completion of a study survey and follow-up through medical record review and contact with study personnel 12 months after enrollment.
Random Assignment Of CRC Screening Strategy
In randomly allocated 3-month blocks, PCPs in each clinic were assigned to provide their patients an initial recommendation for CRC screening by (1) FOBT, (2) colonoscopy, or (3) a choice of FOBT or colonoscopy (Choice arm). The sequence of 3-month blocks was randomly assigned by blinded draw of sequentially numbered containers. Because enrollment took place over an 18-month period, each clinic was assigned each strategy twice. To ensure PCPs did not adjust scheduling of patients to allow discussion of specific strategies, PCPs were blinded to the strategy until the first day that a block change occurred.
INITIAL STUDY ENCOUNTER
Clinic Visits With PCP
The PCP was responsible for counseling eligible patients about CRC screening. During time blocks in which a single strategy was assigned, PCPs recommended only this strategy and did not offer the alternative strategy to patients at the initial visit. Fecal occult blood testing cards were not available for distribution during the time in which colonoscopy was being recommended, and colonoscopy appointments for screening were not available during periods in which FOBT was being recommended. Additional measures to ensure PCPs recommended the correct strategy included changing written material regarding CRC screening in the waiting and examination rooms to depict only the strategy being offered, and changing the verbal scripts used by the PCPs when discussing CRC screening with participants. Since FOBT was the sole means of CRC screening in the CHN outside the study setting, patients assigned FOBT did not have the opportunity to undergo colonoscopy; however, patients assigned to the colonoscopy arm had the opportunity to receive FOBT at subsequent PCP visits if they continued to refuse colonoscopy.
Primary health care providers discussed both FOBT and colonoscopy screening with their patients assigned to the Choice arm. The PCPs were instructed to refrain from recommending a particular CRC screening strategy and allow participants to choose which strategy they wished to pursue. To facilitate choice, the principal investigator (J.M.I) held training sessions prior to study initiation and met with PCPs regularly during the study to emphasize the USP reventive Services Task Force recommendations that did not describe a preferred strategy for CRC screening.14
Conduct of CRC Screening Tests
For participants assigned or who chose FOBT, testing kits were given to the patient for home administration with instructions in their preferred language, which was documented to be English, Spanish, Cantonese, or Mandarin. The cards were mailed back to research staff to ensure accurate assessment of adherence prior to submission to the clinical laboratory for standard processing. For colonoscopy, standard information about the procedure and directions for the bowel preparation were delivered to the participants in their preferred language. No additional reminders to promote screening were provided in this study.
The presence of occult blood on any of the 3 FOBT samples prompted a recommendation for colonoscopy. The participant’s PCP was notified about the positive test result, and the PCP contacted the participant to schedule a colonoscopy.
Reduction of System Barriers to Screening
This study focused on the patient factors associated with adherence to CRC screening tests; therefore, we attempted to reduce health care system barriers to screening. All recommendations and instructions (verbal and written) were provided to participants in their preferred language. Participants agreeing to undergo colonoscopy were directly scheduled for the procedure, thus bypassing a preprocedure gastroenterology visit. Procedural wait times have been associated with reduced adherence; thus, all colonoscopies were scheduled to occur within 2 weeks of enrollment. If necessary, participants were provided postprocedure rides to their residence. Finally, the health care initiative passed by the residents of San Francisco (Healthy San Francisco) ensured colonoscopy was available to all patients regardless of insurance status or ability to pay for this service.
STUDY OUTCOMES
The primary outcome of the study was completion of a CRC screening strategy within 12 months of enrollment in the study defined as the following:
FOBT: Receipt of 3 test cards containing stool specimens. A positive FOBT test result (presence of occult blood on any test card) required documented performance of a colonoscopy in order for the strategy to be completed.
Colonoscopy: Documented performance of colonoscopy.
Completion was prospectively assessed through count of FOBT kits mailed back to the research office and direct observation of participants completing colonoscopy. If there was no documentation of FOBT or colonoscopy the participant was contacted 12 months after enrollment to verify noncompletion. If the participant stated that CRC screening was completed outside of the study site, the research assistant contacted the institution to verify procedure performance.
Research assistants recorded information solicited from participants including age, sex, race/ethnicity, language preference (English, Spanish, Cantonese or Mandarin), level of education, income, employment status, and type of insurance.
DATA ANALYSIS
The primary outcome was comparison of the proportion of participants who completed the CRC screening strategy they were assigned (FOBT or colonoscopy arms) or chose (Choice arm). In addition, the proportions completing FOBT and colonoscopy strategies were calculated separately in the Choice arm. Racial/ethnic differences in overall completion and in completion of specific screening strategies were examined. Completion rates were compared using the χ2 test and adjusted for multiple comparisons using a level of statistical significance of .01. In addition, all analyses adjusted for potential within-PCP clustering using a generalized linear mixed-effect model with logit link.
Secondary outcomes included comparison of the proportion of participants in each arm who completed any CRC screening strategy regardless whether this was the strategy the participant was assigned or originally chose. In addition, sociodemographic data were used as independent variables to assess the impact of each on completion of CRC screening. Predictor variables significantly associated in crude analyses with completion status (P< .05) were entered into a logistic model to identify independent variables associated with noncompletion of CRC screening. Interactions between study arm and various predictors, such as race/ethnicity, on completion were also examined by introducing the product of potential interaction terms into the model.
SAMPLE SIZE CALCULATIONS
The study was designed to have 90% power to detect a difference in CRC completion proportions of 20% between the Choice and single-recommendation arms (.05 [2-sided] significance level, assuming an intraclinic correlation coefficient of 0.05). Assuming at most a 15% dropout, the recruitment goal was set at 990 participants in order to assure a final sample size of 842 or more. This study was approved by the University of California, San Francisco, institutional review board and was registered prior to participant enrollment through ClinicalTrials.gov (NCT00705731).
RESULTS
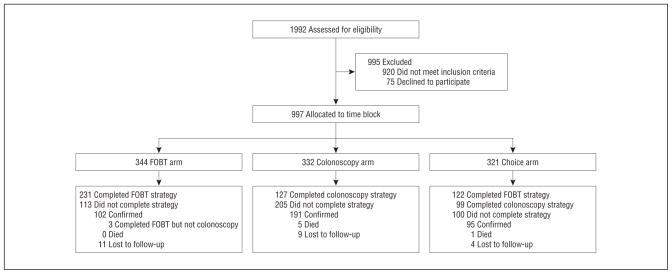
Of 1072 eligible patients identified, 997 (93%) were enrolled in the study, of whom 973 (98%) were successfully followed to the primary end point (completion of a CRC screening strategy or 12 months of follow-up). Enrollment initiated in April 2007, and follow-up was completed March 2010. Details of the study solicitation, enrollment, and follow-up are outlined in Figure 1. The characteristics of the study participants are presented in Table 1. The mean age of the participants was 58.4 years (range, 50–79 years), and 53% were women. The group was racially/ethnically diverse with excellent representation of Latino and Asian patients, and there was no significant difference in participation between racial or ethnic groups. English was the preferred language by 55% of participants, while 27% preferred Spanish and 18% preferred either Cantonese or Mandarin. While the majority had annual incomes of less than $20 000, with 57% having incomes of less than $10 000, 67% had attained a high school diploma or general equivalency diploma, and 39% had attended college. While only 17% stated no insurance, the majority had public insurance including the San Francisco health access plan.
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) diagram. FOBT indicates fecal occult blood testing.
Table 1.
Baseline Sociodemographic Characteristics of the Participants by Study Arm
| Characteristic | FOBT Arm (n = 344) | Colonoscopy Arm (n = 332) | Choice Arm (n = 321) | Total (n = 997) | P Value | |
|---|---|---|---|---|---|---|
| Age, y | ||||||
| Mean (SD) | 58.7 (7.3) | 58.6 (6.7) | 57.8 (6.4) | 58.4 (6.9) | .16 | |
| Median (Range) | 57 (50–79) | 57.5 (50–78) | 57 (50–78) | 57 (50–79) | ||
| Sex, No. (%) | ||||||
| Female | 190 (55) | 173 (52) | 170 (53) | 533 (53) | .70 | |
| Race/Ethnicity, No. (%) | ||||||
| African American | 57 (17) | 61 (18) | 59 (18) | 177 (18) | .36 | |
| White | 51 (15) | 38 (11) | 60 (19) | 149 (15) | ||
| Latino | 117 (34) | 123 (37) | 97 (30) | 337 (34) | ||
| Asian | 107 (31) | 97 (29) | 94 (29) | 298 (30) | ||
| Othera | 12 (3) | 13 (4) | 11 (3) | 36 (4) | ||
| Language,b No. (%) | ||||||
| English | 184 (54) | 187 (56) | 178 (55) | 549 (55) | .85 | |
| Spanish | 101 (29) | 87 (26) | 82 (26) | 270 (27) | ||
| Cantonese or Mandarin | 59 (17) | 57 (17) | 60 (19) | 176 (18) | ||
| Other | 0 | 1 (0) | 1 (0) | 2 (0) | ||
| Race/ethnicity–language, No. (%) | ||||||
| African American–English | 57 (17) | 61 (18) | 59 (18) | 177 (18) | .04 | |
| White–English | 51 (15) | 38 (12) | 60 (19) | 149 (15) | ||
| Latino–English | 16 (5) | 36 (11) | 15 (5) | 67 (7) | ||
| Latino–Spanish | 101 (29) | 87 (26) | 82 (26) | 270 (27) | ||
| Asian–English | 48 (14) | 39 (12) | 33 (10) | 120 (12) | ||
| Asian–Cantonese or Mandarin | 59 (17) | 57 (17) | 60 (19) | 176 (18) | ||
| Other–English | 12 (3) | 13 (4) | 11 (3) | 36 (4) | ||
| Education level, No. (%) | ||||||
| No high school diploma or GED | 133 (39) | 111 (33) | 88 (27) | 332 (33) | .08 | |
| High school diploma or GED | 96 (28) | 93 (28) | 92 (29) | 281 (28) | ||
| Some college or technical school | 56 (16) | 62 (19) | 71 (22) | 189 (19) | ||
| ≥College degree | 59 (17) | 66 (20) | 70 (22) | 195 (20) | ||
| Annual household income, No. (%) | ||||||
| <$10 000 | 204 (60) | 186 (56) | 176 (55) | 566 (57) | .29 | |
| $10 000–$19 999 | 107 (32) | 99 (30) | 109 (34) | 315 (32) | ||
| $20 000–$29 999 | 20 (6) | 34 (10) | 24 (8) | 78 (8) | ||
| ≥$30 000 | 8 (2) | 13 (4) | 9 (3) | 30 (3) | ||
| Employed, No. (%) | 116 (34) | 103 (31) | 121 (38) | 340 (34) | .20 | |
| Insurance, No. (%) | ||||||
| None | 52 (15) | 68 (21) | 49 (15) | 169 (17) | .12 | |
| Publicc | 290 (84) | 257 (78) | 268 (84) | 815 (82) | ||
| Private | 2 (1) | 6 (2) | 3 (1) | 11 (1) | ||
Abbreviations: GED, general equivalency diploma; FOBT, fecal occult blood testing.
“Other” race includes Native Americans, those who listed more than 1 race, and those who declined to state.
Preferred language for interview, including survey completion.
Public includes Medicare, Medicaid, Healthy San Francisco, and the San Francisco Healthy Worker Health Plan.
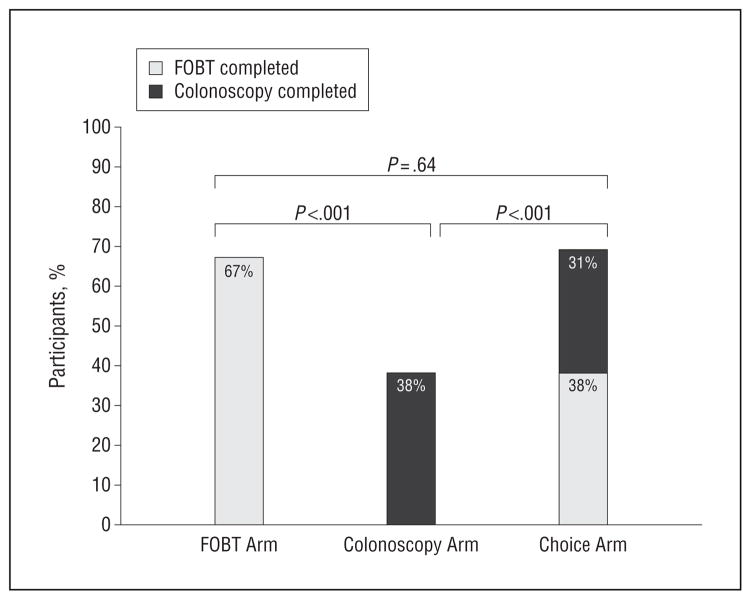
Within 12 months of enrollment, 58% of participants completed the CRC screening strategy they were assigned or chose. A significantly lower proportion of participants in the colonoscopy arm completed colonoscopy (38.2%) compared with participants in the FOBT arm completing FOBT (67.2%) (P < .001) or participants who were allowed to choose their screening strategy (68.8%) (P < .001) (Figure 2). Moreover, the proportion of participants who completed either CRC screening strategy after being recommended colonoscopy (58.1%, including those who completed FOBT) was significantly lower compared with participants recommended FOBT or participants who were allowed to choose their screening strategy (67.2% [P = .01] and 68.8% [P = .004], respectively).
Figure 2.
Completion rates by study arm. Participants recommended colonoscopy completed screening at a significantly lower rate than participants recommended fecal occult blood testing (FOBT) or a choice between colonoscopy or FOBT. The level of statistical significance was reduced to .01 to adjust for multiple comparisons.
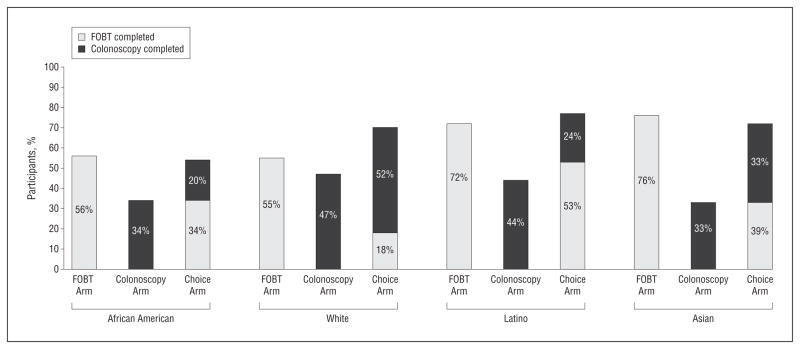
There were significant differences between racial/ethnic groups with regard to completion of CRC screening strategies. African Americans had the lowest CRC screening completion rate (48.0%), while Asians (60.7%) and Latinos (62.9%) had the highest rates (Table 2). Moreover, there were differences between racial/ethnic groups in completion of FOBT vs colonoscopy strategies. Nonwhites were more likely to complete FOBT, while whites were significantly more likely to complete colonoscopy than nonwhites (Figure 3). Correspondingly, among participants in the Choice arm, completion varied by race/ethnicity, with nonwhites completing FOBT significantly more often and white participants being more likely to complete colonoscopy.
Table 2.
Adherence to Colorectal Cancer Screening Strategiesa
| Variable | No./Total No. (%) | OR (95% CI)
|
|
|---|---|---|---|
| Crude Analysis | Multivariable Analysisb | ||
| Study arm | |||
| Colonoscopy | 127/332 (38) | 1 [Reference] | 1 [Reference] |
| FOBT | 231/344 (67) | 3.46 (2.48–4.82) | 3.50 (2.48–4.93) |
| Choice | 221/321 (69) | 3.69 (2.63–5.16) | 3.93 (2.77–5.57) |
| Age category, y | |||
| 50–59 | 337/616 (55) | 1 [Reference] | 1 [Reference] |
| 60–69 | 186/301 (62) | 1.35 (1.01–1.80) | 1.38 (1.00–1.89) |
| 70–79 | 56/80 (70) | 1.94 (1.16–3.24) | 1.61 (0.92–2.80) |
| Sex | |||
| Female | 312/533 (58) | 1 [Reference] | NA |
| Male | 267/464 (58) | 0.95 (0.74–1.23) | NA |
| Race/ethnicity | |||
| African American | 85/177 (48) | 1 [Reference] | 1 [Reference] |
| White | 88/149 (59) | 1.54 (0.99–2.41) | 1.34 (0.82–2.18) |
| Latino | 181/337 (63) | 1.83 (1.26–2.66) | 1.29 (0.70–2.39) |
| Asian | 212/298 (61) | 1.66 (1.14–2.44) | 1.08 (0.64–1.80) |
| Otherc | 13/36 (36) | 0.61 (0.29–1.29) | 0.55 (0.25–1.22) |
| Languaged | |||
| English | 284/549 (52) | 1 [Reference] | 1 [Reference] |
| Spanish | 179/270 (66) | 1.86 (1.36–2.54) | 1.42 (0.77–2.63) |
| Cantonese or Mandarin | 115/176 (65) | 1.78 (1.24–2.55) | 1.78 (1.04–3.02) |
| Other | 1/2 (50) | 0.98 (0.06–16.35) | 0.90 (0.05–17.03) |
| Education level | |||
| No high school diploma or GED | 217/332 (65) | 1 [Reference] | 1 [Reference] |
| High school diploma or GED | 145/281 (52) | 0.56 (0.40–0.78) | 0.64 (0.44–0.93) |
| Some college or technical school | 100/189 (53) | 0.60 (0.41–0.86) | 0.78 (0.51–1.21) |
| College degree or higher | 117/195 (60) | 0.80 (0.55–1.16) | 1.06 (0.68–1.65) |
| Annual household income, $ | |||
| <10 000 | 326/566 (58) | 1 [Reference] | NA |
| 10 000–19 999 | 188/315 (60) | 1.09 (0.82–1.45) | NA |
| 20 000–29 999 | 44/78 (56) | 0.94 (0.58–1.54) | NA |
| ≥30 000 | 18/30 (60) | 1.10 (0.51–2.35) | NA |
| Insurance | |||
| None | 84/169 (50) | 1 [Reference] | 1 [Reference] |
| Publice | 486/815 (60) | 1.51 (1.08–2.12) | 1.43 (0.99–2.07) |
| Private | 8/11 (73) | 2.68 (0.67–10.68) | 3.35 (1.01–18.06) |
| Employment | |||
| Not working | 371/657 (56) | 1 [Reference] | NA |
| Working | 208/340 (61) | 1.20 (0.92–1.58) | NA |
Abbreviations: GED, general equivalency diploma; FOBT, fecal occult blood testing; NA, not applicable.
All analyses adjusted for potential primary health care provider clustering.
Model includes all variables that were significant in crude analysis.
“Other” race includes Native Americans, those who listed more than 1 race, and those who declined to state.
Preferred language for interview, including survey completion.
Public includes Medicare, Medicaid, Healthy San Francisco, and the San Francisco Healthy Worker Health Plan.
Figure 3.
Adherence by study arm and race/ethnicity. Among participants offered a choice of screening tests, white participants adhered more often to colonoscopy than nonwhite participants (odds ratio [OR], 3.2; 95% CI, 1.7–6.1), and less often to fecal occult blood testing (FOBT) (OR, 0.3; 95% CI, 0.1–0.6). Among participants offered FOBT, Asians (OR, 2.6; 95% CI, 1.2–5.3) and Latinos (OR, 2.1; 95% CI, 1.0–4.2) adhered more often than whites.
Of the 226 participants who underwent colonoscopy, 74 (32.7%) had adenomatous polyps: 34 participants (15.0%) had a single adenoma, 19 (8.4%) had 2, 8 (3.5%) had 3, 7 (3.1%) had 4, and 6 (2.7%) had 5 or more removed. No cancers were detected. Of 8 participants who had positive FOBT test results, 5 underwent colonoscopy and 3 were nonadherent (2 refused colonoscopy and 1 missed her scheduled appointment multiple times).
Several sociodemographic factors were associated with adherence to CRC screening. In addition to age and race/ethnicity, language preference affected adherence (Table 2). Participants who preferred to conduct their interviews in Spanish, Cantonese, or Mandarin were significantly more likely to adhere to CRC screening than participants of the same race/ethnicity who preferred to conduct the interview in English. Patients with private or public insurance more often completed screening compared with those without insurance. Patients without high school diplomas had greater adherence than those with diplomas. Clustering by PCP was examined but not found to be significant.
A multivariable model examining the study arm, age, race/ethnicity, and language revealed that completion of CRC screening among participants recommended colonoscopy remained significantly lower than other groups. However, the differences in completion between different race/ethnicity categories were eliminated when language was introduced (Table 2). Specifically, participants who preferred to conduct their interview in Cantonese or Mandarin completed screening more often than participants who preferred to speak English. No significant interaction between race/ethnicity and study arm on completion was noted.
COMMENT
In this randomized clinical trial of competing CRC screening strategies in a racially/ethnically diverse population, we found that patients for whom colonoscopy was recommended were less likely to complete CRC screening than those recommended FOBT or offered a choice between FOBT and colonoscopy. There were significant racial/ethnic differences in screening completion, however, with whites more often completing colonoscopy and nonwhites more often completing FOBT. Moreover, some of these differences were driven by language preference, in that Latinos preferring to speak Spanish and Asians preferring Cantonese or Mandarin completed screening at a higher rate than patients of the same racial/ethnic group who preferred to speak English.
Adherence to different CRC screening strategies has been examined through large population-based studies outside the United States. One Italian study found no difference in adherence between strategies,26 while a second study reported adherence to colonoscopy was significantly lower than to FOBT or FS.27 However, the infrastructure for test access was not standardized and outcomes were not stratified by race/ethnicity. In addition, adherence to any test was low (26%–32%), suggesting substantial differences in patient populations and/or access to CRC screening.
Prior studies reported low CRC screening rates among racial/ethnic minorities, especially among Asians,28 Latinos,28,29 and African Americans.29,30 While the present study confirms the disparity among African Americans, we observed higher adherence among Asians and Latinos than for whites. Our population had established access to health care, which may have reduced these racial differences. In addition, patients without high school diplomas adhered more often than those with diplomas. This unexpected result may indicate less variation and skewing toward lower education in our population.
Participants whose preferred language was not English adhered more often than participants of the same race/ethnicity who preferred to speak English. In fact, after adjusting for language, the racial differences were eliminated. Previous research has found that recent immigrants can suffer less from disparities and social problems than their offspring, or even fair better than nonimmigrants, especially when provided adequate access to resources and opportunity.31
Our hypothesis that giving patients a choice between CRC screening methods would decrease adherence was not supported by this study. However, evidence in decision psychology suggests that providing multiple choices can often lead to confusion, uncertainty, and a default to doing nothing.23,32,33 It may be that 2 options are insufficient to induce decisional conflict. Alternatively, the influence of the PCP may have reduced the need for decision making by the patient; however, this is unlikely, since a bias favoring colonoscopy as the preferred method for CRC screening was voiced by the majority of our PCPs (data not shown), strengthening our conclusion of a preference for FOBT among nonwhite participants.
Additional limitations to this study include a single-point observation of adherence and potential residual system barriers to colonoscopy performance. Results from a single safety-net health care system may not be generalizable to other populations. If we were successful in eliminating access barriers to screening tests this may reduce generalizability to nonstudy settings; however, this would imply potentially lower adherence to colonoscopy in settings where these access barriers were intact. Also, we did not formally test language fluency and assumed language preference based on what participants preferred to speak during the enrollment and survey process. Finally, there may be behavioral aspects of our PCPs or infrastructure factors that may be different from other health care systems.
In summary, this study found that limiting the recommendation for CRC screening to colonoscopy can result in a lower completion rate for CRC screening compared with providing a choice between FOBT or colonoscopy, especially among ethnic/racial minorities. Furthermore, we found significant differences in adherence to competing CRC screening tests between racial/ethnic groups. Moreover, these differences in utilization may be culturally based, specifically with regard to language or acculturation. Finally, at least in the population studied, this study demonstrated that a relatively high level of adherence to CRC screening can be achieved in low-income racial/ethnic minorities when barriers to access are reduced. Further research will determine whether these single-point observations can be translated to programmatic adherence and whether shared decision making or decision aids may increase screening completion.
Acknowledgments
Funding/Support: This work was supported by grant R01CA106773 from the National Cancer Institute at the National Institutes of Health, grant K24DK080941 from the National Institutes of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health, and grant UL1 RR024131 from the National Center for Research Resources at the National Institutes of Health.
Footnotes
Author Contributions: Study concept and design: Inadomi, Vijan, Janz, Fagerlin, Thomas, El-Nachef, and Hayward. Acquisition of data: Inadomi, Thomas, Lin, Muñoz, and Lau. Analysis and interpretation of data: Inadomi, Vijan, Janz, Fagerlin, Thomas, Somsouk, El-Nachef, and Hayward. Drafting of the manuscript: Inadomi, Thomas, Lin, and El-Nachef. Critical revision of the manuscript for important intellectual content: Inadomi, Vijan, Janz, Fagerlin, Muñoz, Lau, Somsouk, and Hayward. Statistical analysis: Inadomi, Vijan, Thomas, Somsouk, and Hayward. Obtained funding: Inadomi, Vijan, Janz, and Hayward. Administrative, technical, and material support: Inadomi, Thomas, Lin, Muñoz, Lau, and El-Nachef. Study supervision: Inadomi and Thomas.
Financial Disclosure: None reported.
References
- 1.Wilson JMG, Jungner F. Principles and Practice of Screening for Disease. Geneva, Switzerland: World Health Organization; 1968. [Google Scholar]
- 2.Hardcastle JD, Chamberlain JO, Robinson MH, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348(9040):1472–1477. doi: 10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- 3.Kronborg O, Fenger C, Olsen J, Jørgensen OD, Søndergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996;348(9040):1467–1471. doi: 10.1016/S0140-6736(96)03430-7. [DOI] [PubMed] [Google Scholar]
- 4.Mandel JS, Bond JH, Church TR, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood: Minnesota Colon Cancer Control Study. N Engl J Med. 1993;328(19):1365–1371. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- 5.Mandel JS, Church TR, Bond JH, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343(22):1603–1607. doi: 10.1056/NEJM200011303432203. [DOI] [PubMed] [Google Scholar]
- 6.Selby JV, Friedman GD, Quesenberry CPJ, Jr, Weiss NS. Effect of fecal occult blood testing on mortality from colorectal cancer: a case-control study. Ann Intern Med. 1993;118(1):1–6. doi: 10.7326/0003-4819-118-1-199301010-00001. [DOI] [PubMed] [Google Scholar]
- 7.Newcomb PA, Norfleet RG, Storer BE, Surawicz TS, Marcus PM. Screening sigmoidoscopy and colorectal cancer mortality. J Natl Cancer Inst. 1992;84(20):1572–1575. doi: 10.1093/jnci/84.20.1572. [DOI] [PubMed] [Google Scholar]
- 8.Selby JV, Friedman GD, Quesenberry CPJ, Jr, Weiss NS. A case-control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992;326(10):653–657. doi: 10.1056/NEJM199203053261001. [DOI] [PubMed] [Google Scholar]
- 9.Atkin WS, Edwards R, Kralj-Hans I, et al. UK Flexible Sigmoidoscopy Trial Investigators. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010;375(9726):1624–1633. doi: 10.1016/S0140-6736(10)60551-X. [DOI] [PubMed] [Google Scholar]
- 10.Winawer SJ, Zauber AG, Ho MN, et al. The National Polyp Study Workgroup. Prevention of colorectal cancer by colonoscopic polypectomy. N Engl J Med. 1993;329(27):1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 11.Müller AD, Sonnenberg A. Protection by endoscopy against death from colorectal cancer: a case-control study among veterans. Arch Intern Med. 1995;155 (16):1741–1748. doi: 10.1001/archinte.1995.00430160065007. [DOI] [PubMed] [Google Scholar]
- 12.Müller AD, Sonnenberg A. Prevention of colorectal cancer by flexible endoscopy and polypectomy: a case-control study of 32,702 veterans. Ann Intern Med. 1995;123(12):904–910. doi: 10.7326/0003-4819-123-12-199512150-00002. [DOI] [PubMed] [Google Scholar]
- 13.Pignone M, Rich M, Teutsch SM, Berg AO, Lohr KN. Screening for colorectal cancer in adults at average risk: a summary of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2002;137(2):132–141. doi: 10.7326/0003-4819-137-2-200207160-00015. [DOI] [PubMed] [Google Scholar]
- 14.US Preventive Services Task Force. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149(9):627–637. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 15.Levin B, Lieberman DA, McFarland B, et al. American Cancer Society Colorectal Cancer Advisory Group; US Multi-Society Task Force; American College of Radiology Colon Cancer Committee. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134(5):1570–1595. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 16.Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM American College of Gastroenterology. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [published correction appears in Am J Gastroenterol. 2009 Jun;104(6):1613] Am J Gastroenterol. 2009;104(3):739–750. doi: 10.1038/ajg.2009.104. [DOI] [PubMed] [Google Scholar]
- 17.Maxwell AE, Crespi CM, Antonio CM, Lu P. Explaining disparities in colorectal cancer screening among five Asian ethnic groups: a population-based study in California. BMC Cancer. 2010 May 19;10:214. doi: 10.1186/1471-2407-10-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Doubeni CA, Laiyemo AO, Klabunde CN, Young AC, Field TS, Fletcher RH. Racial and ethnic trends of colorectal cancer screening among Medicare enrollees. Am J Prev Med. 2010;38(2):184–191. doi: 10.1016/j.amepre.2009.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vijan S, Hwang EW, Hofer TP, Hayward RA. Which colon cancer screening test? a comparison of costs, effectiveness, and compliance. Am J Med. 2001;111 (8):593–601. doi: 10.1016/s0002-9343(01)00977-9. [DOI] [PubMed] [Google Scholar]
- 20.Heisler M, Cole I, Weir D, Kerr EA, Hayward RA. Does physician communication influence older patients’ diabetes self-management and glycemic control? results from the Health and Retirement Study (HRS) J Gerontol A Biol Sci Med Sci. 2007;62(12):1435–1442. doi: 10.1093/gerona/62.12.1435. [DOI] [PubMed] [Google Scholar]
- 21.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 22.Anderson CJ. The psychology of doing nothing: forms of decision avoidance result from reason and emotion. Psychol Bull. 2003;129(1):139–167. doi: 10.1037/0033-2909.129.1.139. [DOI] [PubMed] [Google Scholar]
- 23.Redelmeier DA, Shafir E. Medical decision making in situations that offer multiple alternatives. JAMA. 1995;273(4):302–305. doi: 10.1001/jama.1995.03520280048038. [DOI] [PubMed] [Google Scholar]
- 24.Jones RM, Vernon SW, Woolf SH. Is discussion of colorectal cancer screening options associated with heightened patient confusion? Cancer Epidemiol Biomarkers Prev. 2010;19(11):2821–2825. doi: 10.1158/1055-9965.EPI-10-0695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Inadomi JM, Kuhn L, Vijan S, Fendrick AM, McMahon LF, Hayward RA. Adherence to competing colorectal cancer screening strategies. Am J Gastroenterol. 2005;100:S387–S388. [Google Scholar]
- 26.Segnan N, Senore C, Andreoni B, et al. SCORE2 Working Group-Italy. Randomized trial of different screening strategies for colorectal cancer: patient response and detection rates. J Natl Cancer Inst. 2005;97(5):347–357. doi: 10.1093/jnci/dji050. [DOI] [PubMed] [Google Scholar]
- 27.Segnan N, Senore C, Andreoni B, et al. SCORE3 Working Group-Italy. Comparing attendance and detection rate of colonoscopy with sigmoidoscopy and FIT for colorectal cancer screening. Gastroenterology. 2007;132(7):2304–2312. doi: 10.1053/j.gastro.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 28.Ioannou GN, Chapko MK, Dominitz JA. Predictors of colorectal cancer screening participation in the United States. Am J Gastroenterol. 2003;98(9):2082–2091. doi: 10.1111/j.1572-0241.2003.07574.x. [DOI] [PubMed] [Google Scholar]
- 29.Seeff LC, Nadel MR, Klabunde CN, et al. Patterns and predictors of colorectal cancer test use in the adult US population. Cancer. 2004;100(10):2093–2103. doi: 10.1002/cncr.20276. [DOI] [PubMed] [Google Scholar]
- 30.O’Malley AS, Forrest CB, Feng S, Mandelblatt J. Disparities despite coverage: gaps in colorectal cancer screening among Medicare beneficiaries. Arch Intern Med. 2005;165(18):2129–2135. doi: 10.1001/archinte.165.18.2129. [DOI] [PubMed] [Google Scholar]
- 31.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11(3):496–518. [PubMed] [Google Scholar]
- 32.Schwartz B. The Paradox of Choice: Why More Is Less. New York, NY: Ecco; 2004. [Google Scholar]
- 33.Iyengar S. The Art of Choosing. New York, NY: Twelve; 2010. [Google Scholar]