Abstract
This study examines how acute and chronic stresses associated with functional declines in seniors and their spouses are moderated by their informal and formal support contexts. In the United States, states vary greatly in their support for home and community-based services (HCBS) for seniors with disabilities. This state-to-state variation allowed us to examine mental health effects of living in a society supportive of HCBS for the oldest old, who are at high risk for low or declining functions in daily activities and cognitive abilities. Using a ten-year panel study of a nationally representative sample of the oldest old (>=70 years old) covering the period 1993 to 2002, we conducted mixed-effects logistic regression analysis to incorporate time-varying characteristics of persons and states. As expected, low and declining functions in daily living and cognition constituted significant stressors among seniors and their spouse. Results demonstrated the important role of informal support available from non-spouse family/friends in lowering depression. Living in a state supportive of HCBS was associated with lower depression among seniors experiencing consistently low levels of function or recent functional declines, especially among those without informal support. Our findings were consistent with moderating or buffering models of formal support, suggesting that state HCBS support is effective mainly under conditions of high levels of stressors. Political will is needed to prepare US society to collectively support community-based long-term needs, given the difficulty of preparing ourselves fully for common, but often unexpected, functional declines in later life.
Keywords: USA, elderly, disabilities, depression, stress, social support, formal support, home and community-based services, geographic variation
Introduction
Declining physical and cognitive function poses a major threat for independent living for older adults and their spouses. In particular, rapid functional declines can invoke uncertainties and, possibly, hopelessness about independent living, with little time for adjustment to the situation. Having somebody to rely on when in need is likely to reduce the effects of stress associated with declining function. Previous research has established the association between declining function and depression (Lynch & George, 2002), but relatively little is known about whether and how social support contexts, such as long-term care (LTC) and family caregiving availability, could protect older adults from stress associated with functional declines.
While older Americans usually seek help from informal sources such as family and friends, people are increasingly seeking care from formal sources (Liu, Manton, & Aragon, 2000). In particular, home and community-based services (HCBS), such as personal help and adult day services, help people with disabilities live in the community. Each state has a mix of programs and funding sources, resulting in large state-to-state variation in generosity to support HCBS (Kane, Kane, Ladd, & Veazie, 1998; Kitchener, Carrillo, & Harrington, 2003). Such variation across 50 states and the District of Columbia provides an opportunity to examine mental health effects of living in a society supportive of community living for disabled seniors.
This study examined how functional declines among older Americans and their spouses, and informal and formal support contexts (non-spouse support availability and state HCBS support) were associated with depression, using a ten-year panel study of a nationally representative sample of the oldest old.
Background
Functional decline and depression
Previous research has established the association between depression and declines in functional abilities that are crucial for older adults' well-being (Lenze, Rogers, Martire, Mulsant, Rollman, Dew et al., 2001; Schulz, Heckhausen, & O'Brien, 1994; Taylor & Lynch, 2004). While low functional status has been mainly conceptualized as chronic stress that provides ongoing challenges to daily life, recent studies have recognized the importance of differentiating acute stress of rapid functional declines from chronic stress of relatively stable low functional status (Bruce, 2001; Kennedy, Kelman, & Thomas, 1990; Taylor & Lynch, 2004). While seniors tend to adapt themselves to functional declines over time by assimilative strategies (e.g. using assisted technology or modifying homes) and by accommodative strategies (e.g. modifying their life goals), seniors experiencing recent or rapid declines are not able to adopt such strategies in the short run (Schulz et al., 1994). Also, feelings of uncertainty and helplessness are likely to be acute among those who experience rapid functional declines (Schulz et al., 1994). Kennedy, et al. (1990) found that increasing disability and declining health preceded the emergence of depressive symptoms and showed that deterioration in health and disability over twenty-four months were more important than base-line poor health and functional status.
Researchers have increasingly focused on the dynamic relationships between functional limitations and depression using longitudinal panel data involving three or more waves of data (Fiske, Gatz, & Pedersen, 2003; Ormel, Rijsdijk, Sullivan, van Sonderen, & Kempen, 2002; Taylor & Lynch, 2004; Yang, 2007). For example, Taylor and Lynch (2004) modeled disability, social support and depressive symptoms using a four-wave dataset, and found that trajectories of disability were strongly related to trajectories of depressive symptoms. Those relationships were mediated by trajectories of perceived support, but not by those of received support. Ormel, et al. (2002) used three waves of panel data to examine the temporal character of the reciprocal effects between disability and depressive symptoms to show that disabilities and depressive symptoms mutually reinforce over time, suggesting changes in physical function have stronger and more immediate effects on depression than vice versa. However, there remain important research questions, including how changes in cognitive as well as daily living function are associated with depression, and how social support resources could buffer the impact of functional declines on depression.
One's health is influenced by his or her spouse's health (Christakis & Allison, 2006). Most longitudinal studies on functional declines and depression remain exclusively focused on the focal person. Although there are emerging studies that examine the effects of spouse disability on depressive symptoms among the young-old (Fultz, Jenkins, Østbye, Taylor, Kabeto, & Langa, 2005; Siegel, Bradley, Gallo, & Kasl, 2004; Szinovacz & Davey, 2004), spouse's cognitive and functional status and their changes have not been incorporated in research on depression in the oldest old, who are at high risk of functional declines.
Social support and depression
Social support has both direct and moderating effects on mental health (House, Landis, & Umberson, 1988). Only a few studies have examined how social support moderates or mediates the effects of disability on depression, cross-sectionally (Jang, Haley, Small, & Mortimer, 2002) or longitudinally (Taylor & Lynch, 2004). Those previous studies use general measures of social support focusing on informal support as a composite measure of instrumental, informational and emotional support or of availability of family or friends in times of trouble or to discuss problems. However, moderating effects tend to be detected when social support matches with stress (Cohen & Wills, 1985). Thus, we included measures of formal support reflected in states' generosity for HCBS and informal instrumental social support for functional disabilities.
State variation in HCBS
As key players in U.S. LTC policies, states vary greatly in their commitment to developing HCBS. Approximately 80% of publicly funded HCBS are financed by Medicaid, a federal/state entitlement program of medical assistance for certain individuals and families with low incomes and resources. Medicaid funds HCBS waiver programs for the aged/disabled and state plans that cover home health and personal care. Under Medicaid, states set eligibility criteria, determine payment levels, and define covered services subject to broad federal guidelines. The other HCBS funding sources include state general revenues and moneys allocated to states from the Older Americans Act and the Social Services Block Grant (Title XX). These non-Medicaid funds have accounted for a substantial proportion of HCBS expenditures in some states. In 1992 annual total HCBS expenditures from the Medicaid and non-Medicaid funds mentioned above ranged from $1,180 per person aged 65 and older in New York, to $369 in Oregon, down to $29 in Mississippi (Administration on Aging, 1995b; Ladd, Kane, Kane, & Nielsen, 1995). Between 1992 and 2002, Medicaid HCBS spending increased by more than 200% (CPI-adjusted), driven by the rapid increase (438%) in the Medicaid HCBS waiver program for the aged/disabled. The large inter-state variation remains today. Living in a state supportive of HCBS lowers the risk for nursing home admission among seniors (Muramatsu, Hoyem, Yin, & Campbell, 2008; Muramatsu, Yin, Campbell, Hoyem, Jacob, & Ross, 2007). However, whether state HCBS support affects older adults' psychological well-being is virtually unknown.
Current Study
Drawing on stress theory, we examined how chronic and acute stress of functional declines in older Americans and their spouses were associated with depression. Depression is a global indicator of stress sensitive to the effects of undesired experience that is both enduring and resistant to efforts for changes (Pearlin, Lieberman, Menaghan, & Mullan, 1981). Our special focus was on the moderating effects of caregiving resources, including availability of non-spouse family/friends for help with daily activities and state generosity in HCBS, an important yet neglected social context for older adults with disabilities.
Our overarching hypothesis is that higher levels of caregiving resources protect older adults from depression. Knowing that relatives or friends are available to help with daily activities when in need provides a sense of security, control and hope. In particular, the acute stress of functional declines could heighten uncertainties about the future and enhance the relative role of informal care availability in psychological well-being. Thus we hypothesized that informal caregiving availability would be associated with lower depression among older adults, and the association would be stronger among those with higher functional disability and those with recent functional declines.
We also hypothesized that living in a state that generously supports HCBS would protect older adults with functional limitations from depression and that such protective state effects would be larger for those without informal support. Realizing that one is living in an environment that supports HCBS and promotes community living would protect one from depression and anxiety that accompany functional declines. On the other hand, learning that no such support is available could enhance feeling of uncertainty and hopelessness, especially among those with few informal caregiving resources. States generally target public HCBS to people with low income and assets. However, states' commitment to public HCBS may have spill-over effects, encouraging service providers to develop HCBS for those with higher economic status and enhancing the general availability of HCBS in the state. We did not expect state HCBS support to affect seniors with no immediate HCBS needs. One tends to be insensitive to, or unknowledgeable about, a distant, not-yet-relevant environment.
Methods
We conducted multi-level repeated measures analysis using Health and Retirement Study (HRS, http://hrsonline.isr.umich.edu/) data for 1993, 1995, 1998, 2000, and 2002 from cohorts born in 1923 or earlier. Person-level data were drawn from files produced by the Rand Center for the Study of Aging supplemented by other public data files, such as “exit interview”, “tracker”, “other person”, helper”, and “region” files. A restricted data file containing state identifiers permitted us to link state-level data to the person-level data.
Measures
The dependent variable, depression, was measured by a shortened 8-item Center for Epidemiologic Studies Depression Scale (CES-D), a commonly used self-rating scale of depression in the general population (Radloff, 1977). This HRS depression scale, based on a Yes(1)/No(0) response format (range: 0-8), represents depressed mood and somatic complaints factors. The validity and reliability of this measure have been extensively evaluated by the HRS group (Mills & Henretta, 2001; Steffick, 2000). Given the highly skewed distribution (i.e., few respondents have severe depression), we dichotomized the variable. We used the cut-off point of 4 or higher, which, according to the HRS research group, approximates the traditional cutoff point of 16 or higher for the original 20-item CES-D Scale that indicates a high likelihood of clinical depression (Wallace, Herzog, Ofstedal, Steffick, Fonda, & Langa, 2000).
Two dimensions of functional limitations were examined: daily living and cognitive abilities. The former indicates the number of basic and instrumental activities of daily living (ADL: bathing, dressing, eating, getting in/out of bed; IADL: using a telephone, taking medication, handling money, shopping, preparing meals) where the respondent reports any difficulty. Combining ADL and IADL items into a single scale has major advantages over separate measures in terms of its parsimony and ability to measure a large range of functional disability (Spector & Fleishman, 1998). HRS assessed cognitive function (immediate memory, working memory, knowledge, language and orientation) using the Telephone Interview of Cognitive Status, a validated screening instrument patterned on the Mini-Mental State Examination (Herzog & Wallace, 1997; Ofstedal, Fisher, & Herzog, 2005). The coding was reversed so that a higher score indicates more cognitive limitations (range:0-35).
To differentiate chronic and acute stress, we decomposed functional limitations into two: (1) each individual's mean score calculated across the period when the individual was observed; and (2) each individual's deviation from his/her own mean score assessed at each time point (Horney, Osgood, & Marshall, 1995). The former is in effect between-persons differences in the underlying level of functional status, representing stable components of one's function or a chronic stressor. The latter indicates within-person changes from one's underlying level of functional status, representing dynamic components or an acute stressor.
We created parallel measures of spouses' functional limitations. To retain unmarried respondents, all married respondents' mean values calculated over the entire study period were used for spouse characteristics for unmarried person, which, in conjunction with a marital status indicator, permits unbiased estimation of the effects of spouse factors in the full sample (Allison, 2002).
Two dimensions of support availability were assessed: state HCBS support and informal support. The former was measured as total state HCBS expenditures divided by the 65+ population (Administration on Aging, 1995b; Ladd, Kane, & Kane, 1999; Ladd et al., 1995). We captured HCBS expenditures funded not only by Medicaid (home health, personal care, and waiver expenditures for aged or disabled individuals) (Burwell, 2001, 2003; Harrington, Carillo, Wellin, & Norwood, 2000) but also by Older Americans Act (Administration on Aging, 1995a, 1996, 2004), Social Services Block Grant (U.S. Department of Health and Human Services, 1999, 2000-2004; U.S. Department of Health and Human Services. Office of Community Services, 2004) and state funds (Administration on Aging, 1995b; Kassner & Williams, 1997; Summer & Ihara, 2004) that provided HCBS to older adults. For multivariate analysis, we used the natural logarithm of the per-capita HCBS.
Non-spouse support availability indicates whether a respondent was receiving instrumental support from non-spouse family or friends or, if s/he was not receiving such support, whether s/he expected such informal support available when in need in the future. The respondents with ADL/IADL limitations were asked whether anyone ever helped them (with each limitation), who most often helped them (with any of the limitations), and if anyone else helped, who that was. Those who were not receiving help were asked the following question instead: “Suppose in the future, you needed help with basic personal care activities like eating or dressing. Do you have relatives or friends [besides your (husband/wife/partner)] who would be willing and able to help you over a long period of time?” Since this latter question was not asked of those who were receiving help, we could not measure anticipated support and received support separately (Krause, 1997). The role of non-spouse support could depend on the availability of spouse help. Thus we controlled for current receipt of help from spouse. HRS did not assess future availability of spouse help consistently over the observation period. We assessed informal support availability and depression concurrently, because support resources present at the time of depression assessment are likely to be more contemporaneous with the depression process than the resources reported at a prior wave two to three years earlier (Pearlin et al., 1981).
Other covariates include age (as of 1993), gender, education, race/ethnicity, marital status, household income, non-housing wealth, number of health conditions, living alone, having at least one living child, and spouse' age and health conditions. Income and wealth variables were logged except for $0 or negative values. In case of $0, the original value was kept. For negative wealth, the negative value of the logarithm of the absolute value, i.e., -log(|X|), was computed. Also included was a variable indicating whether the respondent lived in a rural area to control for within-state differences in LTC service availability. Two state-level variables derived from the 2000 census data, household income inequality measured in the GINI coefficient (Kawachi & Kennedy, 1997) and urbanization (percentage of urban population), were included to control for state characteristics that may affect policy priorities and residents' well-being. Median household income, an insignificant predictor correlated with HCBS (r=0.3, p<.0001).was excluded from the final models. Time was measured in years since the 1993 baseline survey. Inclusion of indicator variables for response patterns (panel attrition due to deaths, lost to follow-up/missed interviews) allowed us to estimate and control for the increased rates of depression among those with these types of missing data (Hedeker & Gibbons, 1997).
Analytic sample
Our analytic sample consisted of 6,535 respondents representing 18,770 observations. From the 1993 baseline sample of the 7,441 respondents (representing 26,542 observations through 2002), we excluded interviews conducted during nursing home stays (2,168 observations), proxy interviews (with no depression measures, 2,641 observations), observations after a respondent moved out of the baseline state (356), and observations with missing data in the variables included in the model (2607).
Analytic strategies
We conducted mixed-effects logistic regression analysis, involving three levels of data: states, persons, and time points (<=5). Mixed-effects regression models can account for the dependency inherent in the data due to repeated measurement and clustering within states and allow respondents with missing observations (Hedeker & Gibbons, 2006). Our data involved unequal time intervals between observations (2 years, except 3 years between 1995 and 1995), which could be easily incorporated into our three-level random intercept model, involving two random effects (subjects and states). We report the subject-specific results as opposed to the population-averaged (Neuhaus, Kalbfleisch, & Hauck, 1991), because we would like to know how the risk of depression increases when individuals experience functional declines and whether the relationship between function and depression is modified by state HCBS support. We treated state as a random effect because of our interest in generalizing the state HCBS effects beyond our given sample of states (N=41).
The HRS samples are drawn using a complex survey design in which African-Americans, Mexican-Hispanics and residents of the state of Florida are over-sampled. Indicator variables for the first two groups were included in our models along with many other variables such as age and income which account for similarity of cases within primary sampling units. Following Winship and Radbill (Winship & Radbill, 1994), we did not use sampling weights since they are reflected in our independent variables.
Results
Sample characteristics
Table 1 presents the characteristics of the respondents, their spouse, and the states of residence as of the 1993 baseline survey. Thirty-eight percent of the sample participated in all of the five surveys, 25 percent had only one observation, and the rest had 2-4 observations. Annual HCBS expenditure per person aged 65 and older in the states represented in our sample was, on average, $222 in 1993, ranging from $28 to $945. These expenditures grew considerably during the study period up to $524, ranging from $39 to $1303 in 2002.
Table 1. Sample characteristics as of 1993: Health and Retirement Study respondents born in 1923 or earlier and their states of residence.
| Variables | Mean (SD) |
|---|---|
| Respondents N=6101a | |
| Depression b,i | 0.17 |
| Sociodemographic Characteristics | |
| Age (years) | 77.36 (5.69) |
| Female | 0.63 |
| White (non-Hispanic)c | |
| African-American (non-Hispanic)c | 0.05 |
| Hispanicc | 0.13 |
| Education (years in school) | 10.93 (3.69) |
| Wealth, non -housing ($)i | 102,160 (288,783) |
| Income, total household ($)i | 25,739 (54,271) |
| Functional limitations & health | |
| ADL/IADL limitationsd,i | 0.70 (1.38) |
| Cognitive limitationse,i | 15.61 (5.85) |
| No. of health conditions (0 to 8)i | 1.49 (1.21) |
| Family characteristics | |
| Currently marriedc,i | 0.46 |
| Live alonec,i | 0.40 |
| Have any child alivec,i | 0.86 |
| Spouse characteristicsf | |
| Age (years) | 75.32 (4.78) |
| ADL/IADL limitationsd,i | 0.60 (0.86) |
| Cognitive limitationse,i | 14.08 (3.74) |
| No. of medical conditionsi | 1.61 (0.83) |
| Informal help availability | |
| Non-spouse – current/futurec,i | 0.54 |
| Spouse help – currentc,i | 0.10 |
| Rural residencec,i | 0.25 |
| Response patternsc | |
| Participated in all 5 waves | 0.38 |
| Died during the study period | 0.43 |
| Lost to follow-up or missed interview(s)g | 0.19 |
| States N=41 | |
| HCBS expenditures per 65+/year ($)i | 222 (225) |
| GINIh | 0.45 (0.03) |
| Urbanizationh | 79.32 (14.36) |
Notes: SD = standard deviation; HCBS=home and community-based services.
Additional 431 respondents included in our multivariate analysis had missing data or a proxy interview in 1993.
The depression score (8-item Center for Epidemiologic Studies Depression Scale, range:0-8) was recoded into an indicator variable (1 if the score >=4, 0 otherwise).
Indicator variable (coded 0/1). The mean value indicates the proportion of cases with the attribute indicated by the variable. Standard deviations were omitted.
The number of ADLs (activity of daily living) and IADLs (instrumental ADL) where the respondent had difficulties (range: 0-10).
Scale based on the Telephone Interview of Cognitive Status (range:0-35).
Based on those who had a spouse (N=2,825).
Did not participate in the last interview (2002) and were not reported dead; or participated in the first and last interviews but missed one or more interviews in between.
Source: 2000 Census. http://www.census.gov/main/www/cen2000.html.
Time-varying variables assessed at each survey wave.
On average, the respondents and their spouse had relatively high levels of function, and their functional abilities declined only slightly between 1993 and 2002. Lack of significant changes in the sample average, however, masks significant intra-person changes (Table 2). Between the first and last observations, 23.9% and 45.4% of the respondents experienced declines in daily function and cognitive abilities, respectively (not shown).
Table 2. Functional limitations: Sample means, individual means over time, and intra-individual changes.
| Respondent ADL/IADL | Respondent Cognitive Limitations | Spouse ADL/IADL | Spouse Cognitive Limitations | |
|---|---|---|---|---|
| 1993 Sample meansa (SD) [Min; Max] | .70 (1.38) [0; 10] |
15.61 (5.85) [0; 35] |
.59 (1.26) [0; 10] |
14.15 (5.50) [0; 35] |
| 2002 Sample meansa (SD) [Min; Max] | .85 (1.64) [0; 10] |
15.78 (5.50) [0; 35] |
.69 (1.63) [0; 10] |
14.81 (5.32) [0; 35] |
| Individual means over timeb (SD) [Min; Max] N=6,535 | 1.00 (1.53) (0; 10) |
15.47 (4.93) [0; 35] |
.72 (.86) (0; 10) |
14.10 (3.07) [0;35] |
| Intra-individual changesc (SD) [Min; Max] | -.24 (1.15) [-7.50; 7.40] |
-0.14 (2.86) [-13.75; 19.00] |
-.11 (.63) [-8.00; 7.20] |
-.07 (1.82) [-13; 19] |
| Percent of people who had any changesd | 42.02 | 72.74 | 33.43 | 68.77 |
Based on the number of respondents and their spouse in 1993 (6,101 and 2,825) and 2002 (1,902, and 686).
Calculated for each individual across time points when s/he participated in the survey (N=6,535 respondents; N=3,069 spouses).
Deviation of the person's functional level from his/her individual mean at each time point (N=18,770 observations for respondents; N=8,153 observations for spouses).
Based on N=6,535 respondents and 3,069 spouses. 25% of the sample had one observation (and thus no change in functional status); 20% had two observations, 20% had three, 15% had four, and 21% had five.
Main effects of functional limitations, informal support, and state HCBS support
Not surprisingly, ADL/IADL limitations had strong associations with depression. The coefficient of individual means indicates that those with systematically high levels of limitations had systematically high levels of depression (Table 3, p≤.01). The coefficient of intra-individual changes indicates significant association between recent declines in daily living function and depression (p≤.01). The effects of spouse's ADL/IADL limitations on depression were much smaller: those whose spouse experienced recent functional declines had higher levels of depression (p≤.10), but spouse's underlying ADL/IADL limitations (individual means) had no effects. Interestingly and understandably, spouse cognition had large effects on depression: the effect of spouse's underlying cognitive level (p≤.01) was even larger than that of his/her own, and spouse's cognitive decline was significantly associated with depression (p≤.05).
Table 3. Mixed-effects logistic regression of depression: Main effects model (Model 1).
| Variables | Coefficients | (SE) | Odds Ratio | |
|---|---|---|---|---|
| Individual-level variables | ||||
| Age as of 1993 | -0.0233 | (0.0067) | 0.9769 | *** |
| Female | 0.1547 | (0.0550) | 1.1673 | *** |
| African-American - non-Hispanic | -0.0904 | (0.0952) | 0.9135 | |
| Hispanic | 0.3154 | (0.1669) | 1.3708 | * |
| Education (years in school) | -0.0347 | (0.0089) | 0.9659 | *** |
| Wealth, non-housing (logged) | -0.0132 | (0.0064) | 0.9869 | ** |
| Income, total household (logged) | -0.0437 | (0.0255) | 0.9572 | * |
| Rural | -0.1132 | (0.1032) | 0.8929 | |
| ADL/IADL limitations – individual means | 0.3273 | (0.0138) | 1.3873 | *** |
| – change | 0.2138 | (0.0204) | 1.2384 | *** |
| Cognitive limitations – individual means | 0.0318 | (0.0054) | 1.0323 | *** |
| – change | 0.0082 | (0.0089) | 1.0083 | |
| No. Medical conditions | 0.2341 | (0.0212) | 1.2638 | *** |
| Married | -0.5896 | (0.0965) | 0.5545 | *** |
| Live alone | 0.2081 | (0.0639) | 1.2314 | *** |
| Have any child alive | 0.0271 | (0.0720) | 1.0275 | |
| Spouse: Age (in months) | 0.0130 | (0.0065) | 1.0131 | * |
| ADL/IADL limitations – individual means | 0.0375 | (0.0351) | 1.0382 | |
| – change | 0.0732 | (0.0406) | 1.0760 | * |
| Cognitive limitations – individual means | 0.0492 | (0.0129) | 1.0505 | *** |
| – change | 0.0229 | (0.0114) | 1.0232 | ** |
| # Medical Conditions | 0.1150 | (0.0374) | 1.1218 | *** |
| Non-spouse informal help availability | -0.4329 | (0.0650) | 0.6486 | *** |
| Spouse help – current | 0.1877 | (0.0985) | 1.2065 | * |
| Response pattern: Died during the study period | 0.3045 | (0.0615) | 1.3559 | *** |
| Lost-to follow-up/missed interviews | -0.0233 | (0.0817) | 1.2380 | *** |
| State-level variable | ||||
| HCBS expenditures per 65+ Person (logged) | -0.0056 | (0.0343) | 0.9944 | |
| Income inequalitya | 0.1780 | (0.0531) | 1.1948 | *** |
| Urbanization level | 0.0020 | (0.0033) | 1.0020 | |
| Time | ||||
| Time (years since 1993 interview) | -0.2416 | (0.0474) | 0.7854 | *** |
| Time Square | 0.0732 | (0.0142) | 1.0759 | *** |
| Time Cubic | -0.0052 | (0.0011) | 0.9948 | *** |
| _Constant | -5.4936 | (1.0410) | 0.0041 | *** |
p ≤ 0.10
p ≤ 0.05
p ≤ 0.01 (two-tailed tests).
SE=Standard errors, adjusted for clustering in states. ADL = activity of daily living; IADL = instrumental ADL; HCBS=Home and community-based services. The analytic data include18,880 observations represented by 6,535 respondents who lived in 41 states.
The GINI coefficient. The effect is expressed in terms of a one standard deviation unit of change.
Availability of help with functional limitations from non-spouse family/friends was strongly associated with lower depression (p≤.01), whereas current receipt of help from spouse was marginally associated with higher depression (p≤.10). Not surprisingly, state HCBS support had no statistically significant main effects, whether included as the only state-level factor (not shown) or together with the state-level control variables (Table 3). Interestingly, state income inequality was significantly associated with depression (p≤.01).
Does state HCBS and informal support availability moderate the effects of functional limitations?
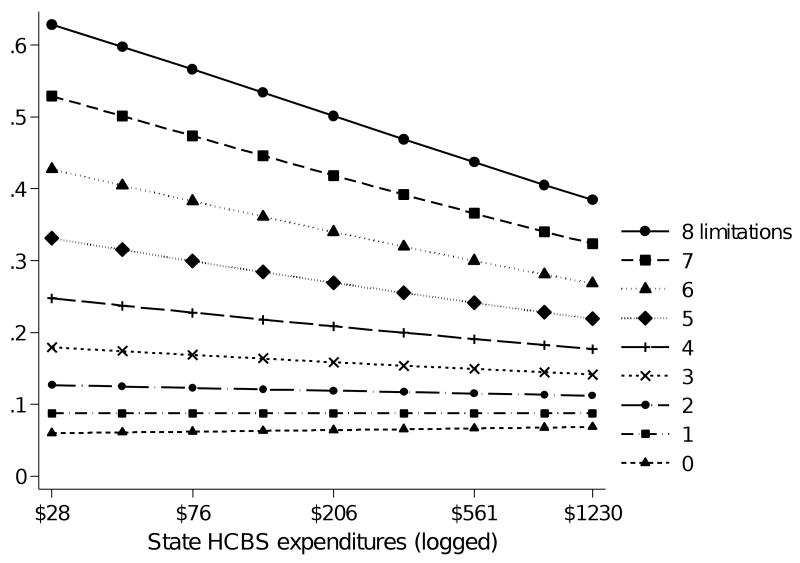
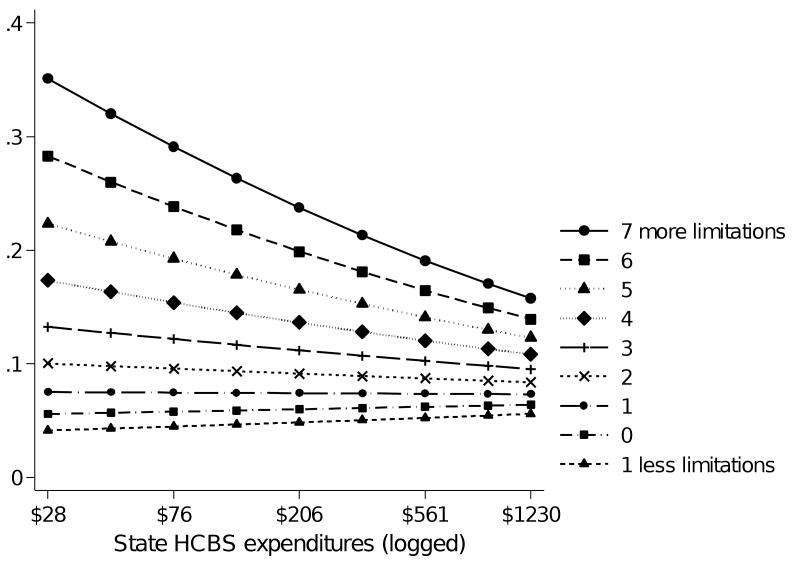
We tested two-way interactions between functional limitations and caregiving contexts to investigate whether supportive contexts moderate the effects of functional limitations. Significant two-way interactions between ADL/IADL limitations (intra-individual means and changes) and state HCBS support emerged (p<.01, Table 4 Model 2). Figures 1 and 2 graphically illustrate these moderating effects for an “average” white married woman. Higher and steeper lines for persons with more ADL/IADL limitations on average (Figure 1) indicate that those with systematically higher levels of ADL/IADL limitations were more likely to be depressed and that they benefited more from living in a state with higher HCBS expenditures. Similarly, Figure 2 illustrates that those who recently experienced more dramatic declines in daily living functions benefited even more from living in a state with higher HCBS support. The models with two-way interactions involving cognitive limitations did not yield any statistically significant interaction effects.
Table 4. Mixed-effects logistic regression of depression: Interaction effects models.
| Model 2 ADL/IADL 2-way Interactions | Model 3 Cognitive Limitations 3-way Interactiona | |
|---|---|---|
| Variables | Coefficients (SE) | Coefficients (SE) |
| ADL/IADL (means) by HCBS | -0.0371 *** (0.0108) | |
| ADL/IADL (changes) by HCBS | -0.0449 *** (0.0128) | |
| Cognitive limitations (means) by HCBS by Non-spouse informal help | 0.0268 (0.0118) ** | |
| Cognitive limitations (means) by HCBS | -0.0238 (0.0058) *** | |
| Cognitive limitations (means) by non-spouse informal help | -0.1578 (0.0616) ** | |
| HCBS by non-spouse informal help | -0.4630 (0.2355) ** | |
p ≤ 0.05
p ≤ 0.01 (two-tailed tests).
Each model included all the independent variables shown in Table 3.
The 3-way interaction model included all the 2-way interactions between the variables included in the 3-way interactions.
Figure 1.
Interaction between state HCBS and intra-individual means of daily activity limitations (Based on Model 2)
Notes: HCBS=Home and Community-Based Services. The x-axis indicates a log scale of the level of states' annual expenditures on HCBS per person aged 65+, ranging from the lowest level to the highest level in our analytic sample. The y-axis indicates the predicted probability of depression for an “average” married white woman, fixing the values of independent variables at mean levels for continuous variables (Table 1) and 0 for dichotomous variables.
Figure 2.
Interaction between state HCBS support and intra-individual changes in daily activity limitations (Based on Model 2)
Notes: See Figure 1.
Are the protective effects of HCBS support more salient for people without informal support?
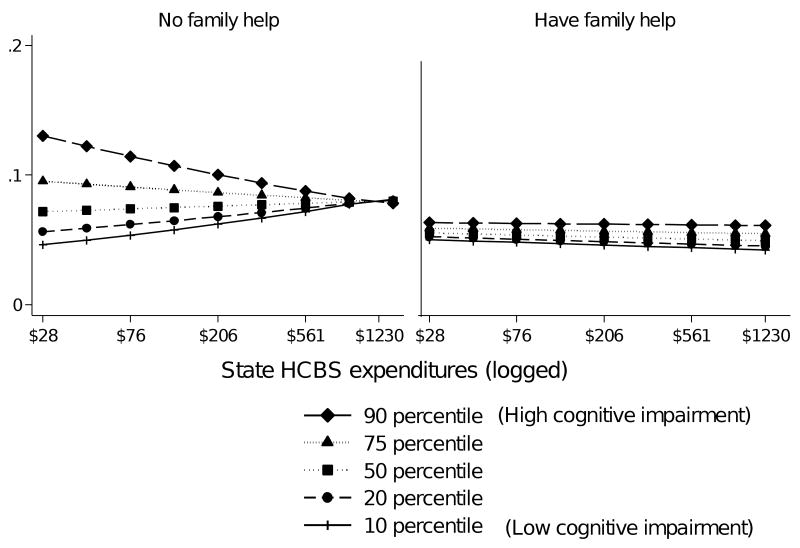
We then examined three-way interactions among functional limitations, state HCBS and informal support availability. We found significant interaction effects among state HCBS, informal help and underlying cognitive limitations (individual means, Table 4). The left panel of Figure 3 illustrates the case for those with no current or anticipated help from non-spouse family/friends, and the right panel, those with such help. In both panels, people with higher levels of cognitive problems had higher rates of depression. The right panel indicates that, for those with non-spouse family help, state HCBS support did not make much difference in the relationship between cognitive problems and depression. The left panel (those without non-spouse help) shows that, among those with severe cognitive problems (i.e., 90 percentile), higher state HCBS was associated with lower depression (p=.002), as indicated by the steeper downward slope; among those with higher cognitive function, state HCBS support had no or positive relationships with depression, somewhat unexpectedly. The left panel also indicates that the relationship between cognitive status and depression is stronger if the state HCBS support is low. Figure 3 as a whole illustrate that living in a state that generously supports HCBS would protect older adults from stressful effects of severe cognitive problems, when no informal support was available. We did not find three-way interactions involving ADL/IADL limitations or intra-individual changes in cognitive limitations.
Figure 3.
Three-way interaction among state HCBS, intra-individual means of cognitive limitations, and availability of help from non-spouse relatives or friends (Based on Model 3)
Notes: See Figure 1.
Discussion
We examined how chronic and acute stresses of functional declines were associated with depression, with special focus on the role of social support contexts in ameliorating such stress in oldest old Americans. Caregiving resources varied greatly. Almost half of older adults did not receive or anticipate personal care support from non-spouse relatives or friends. The states where they resided varied greatly in the level of support for HCBS.
Our results confirmed that low and declining functions were major stressors associated with depression among older Americans and their spouses. Those who were consistently low in function, both physically and cognitively, and those who recently experienced declines in daily living functions were significantly more likely to be depressed. Spouse's function, particularly low and declining cognitive function, had large associations with depression.
Family caregiving contexts were important determinants of depression. Those who were receiving help with daily activities from non-spouse relatives or friends or who expected to receive such help for an extended period of time in the future had lower rates of depression than those without such help available. Knowing that help is, or will be, available when in need may reduce the anxiety associated with loss of independence, hindering depression. Current receipt of spouse help, on the other hand, was marginally associated with higher depression, consistent with the literature (Bolger & Amarel, 2007; Krause, 1997). Dependence on a spouse who is becoming older and frailer may threaten self-esteem and lead to feeling loss of control over important life outcomes, arousing anxiety and, eventually, depression.
Consistent with stress-buffering or stress-moderating models of formal support, state HCBS support seemed to be effective for mental health among seniors with consistently low or rapidly declining daily functions. It is likely that seniors with such functional problems may have learned their current and future needs for HCBS and service availability in their community. Knowing that they live in an environment where HCBS support is available may help maintain their mental health, while learning that they are on their own or solely dependent on their family and friends may be demoralizing. State HCBS support had no effects among “average” seniors or among those with less functional limitations. This finding was not surprising, because seniors with few or no functional limitations may not even be aware of state LTC contexts. State HCBS contexts may be irrelevant for their mental health.
The protective effects of non-spouse informal support, on the other hand, did not depend on the level of functional limitations. Perhaps, people generally have a sense of informal support availability, regardless of their current functional status.
Results buttress the notion that state HCBS support has a stronger effect on depression among those who lack informal support. The significant three-way interaction among depression, underlying cognitive problems, and state HCBS support suggests that state HCBS support is effective in protecting older adults from depression if they have severe cognitive problems and lack informal support. Somewhat unexpected was the finding that cognitively intact seniors without non-spouse family support were more depressed if living in a state with high HCBS. Even in the state with the highest level of HCBS, public HCBS support is limited, usually available only for the poor or those who have spent down their own assets. Recognizing this prospect may be especially depressing for cognitively intact seniors without family support. This feeling can be intensified if living in a state with high HCBS support bolsters initial expectation for public HCBS support and if HCBS resources are disproportionately allocated to those who are cognitively impaired.
Our findings on state HCBS moderating effects contribute to our understanding of the role of formal support contexts in the stress process. Numerous studies have consistently demonstrated that informal support promotes mental health (House et al., 1988). However, few studies incorporated formal sources of support into the study of stress and mental health in the elderly (Krause, 1990). We found that state HCBS support may not directly affect mental health, but may be effective only for those with acute and chronic stress of functional declines, especially when informal support is unavailable. Different from informal support that may serve various needs, services from formal sources, whether state LTC support or medical care, tends to be specialized. Only when specific needs arise, people seek specific services and appreciate their availability and potential benefits. On the other hand, learning that such support is not available, people remain anxious and demoralized about their declining functions, especially when they do not have alternative informal help to turn to.
Our findings also add to the emerging evidence from recent observational studies indicating the benefits of states' increased spending on HCBS for seniors' well-beings, such as reduced risks for nursing home admission and increased chances of living in the community at the end of life (Muramatsu et al., 2008; Muramatsu et al., 2007). Our study extends the literature to show that state HCBS contributes to mental health for people with limited and/or declining physical and cognitive functions, especially when informal support is not available.
A major strength of this study lies in the use of a 10-year longitudinal multilevel dataset, allowing up to 5 observation points for each person. However, this sample consisted of the oldest old at risk for deaths and declining health. Because of the inevitable panel attrition, each participant had fewer observation points than ideal. This limited our ability to capture intra-individual changes in functions. Thus there are uncertainties in assessing the effects of intra-individual changes. Furthermore, those with severe cognitive and health problems are less likely to participate in the survey and more likely to have proxy respondents. HRS did not assess depression among seniors with proxy respondents, and thus we excluded them from our analysis. This limits our ability to generalize our findings to people with severe cognitive and health problems. Because of this potential sample bias towards healthier seniors, we may have underestimated the moderating effects of state HCBS for people with functional limitations. Another limitation is that, due to the HRS complex sampling design, our sample did not include all the states. The states included in the sample had higher HCBS expenditures than those excluded. The implications of this are difficult to assess, and caution is needed to generalize our findings.
We incorporated spouse functional declines in our analytic model, but examined only their main effects to retain both married and unmarried seniors in the sample. Future research can examine whether and how state HCBS support may moderate the effects of spouse functional declines in a sample of married couples.
Conclusions
This is one of the first studies to demonstrate that societal level support for LTC needs is important for the psychological well-being of the elderly, especially when the elderly face common, but often unexpected loss of functions without support from family or friends. Developing functional limitations is a common risk for anybody getting older. Americans who live up to 70 are expected to live until 85 on average (Kochanek & Smith, 2004). Among 85 years and older who live in the community, one half are estimated to have ADL limitations, and another 20% IADL limitations (Medicare Current Beneficiary Survey). Functional declines can come randomly to anybody at any time, and LTC can be costly. However, Americans are not prepared for this common risk mentally or financially. Many mistakenly believe that their LTC is covered by Medicare, the federal health insurance program for the elderly and the disabled that generally covers medical and subacute care.
This article provides evidence for the importance of continued state and federal efforts to sustain and increase HCBS funding. The United States has made significant progress towards expanding HCBS, but the efforts have been mostly through Medicaid HCBS waiver programs available for those with few economic resources. LTC expenditures are one of the “largest uninsured financial risks” in the United States (Brown & Finkelstein, 2004). While public education is needed to help people understand their future LTC care needs and prepare themselves, there is a limit to what individuals can do. It is critical to establish a system at a societal level to protect seniors from unexpected, yet common, functional declines. The proportion of childless women is increasing over time, and baby boomers have fewer children, potential sources of informal support, than their predecessors (U.S. Census Bureau). The number of people aged 65 and older will double between 2000 and 2030. Facing rapid population aging and serious concerns about increasing caregiving burden, other countries implemented universal and equitable access to LTC regardless of socioeconomic status or family availability (Tsutsui & Muramatsu, 2007). Political will is needed to prepare the society for increasing LTC needs for the elderly, especially at this time of economic hardship.
Acknowledgments
Author Comments: The research reported here was supported by the National Institute on Aging (R01 AG021648). The authors thank Richard T. Campbell and Paul D. Allison for their inputs on statistical issues; Robert L. Kane, Charlene Harrington and Marshall H. Chin for their comments on earlier versions of this paper; and Ruby Hoyem, Martha Jacob, Brian Burwell, and other people at various agencies and organizations for their help in our state data compilation process.
Footnotes
An earlier version of this paper was presented at the 59th Annual Scientific Meeting of the Gerontological Society of America, Dallas, Texas, November 18, 2006. This paper was presented in part at the Annual Research Meeting of AcademyHealth, Chicago, Illinois, June 28, 2009.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Administration on Aging. 1995 State Program Report for Titles III and VII of the Older Americans Act. Washington, D.C.: Department of Health and Human Services; 1995a. [Google Scholar]
- Administration on Aging. Infrastructure of Home and Community Based Services for the Functionally Impaired Elderly--State Source Book. Washington, D.C.: Administration on Aging, U.S. Department of Health and Human Services; 1995b. [Google Scholar]
- Administration on Aging. 1996 State Program Report for Titles III and VII of the Older Americans Act. Washington, D.C.: Department of Health and Human Services; 1996. [Google Scholar]
- Administration on Aging. Titles III and VII State Program Reports. 2004. Retrieved October 1, 2004, from http://www.aoa.gov/prof/agingnet/NAPIS/SPR/spr_reports.asp.
- Allison PD. Missing data Sage University Papers Series on Quantitative Applications in the Social Sciences, 07-136. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Bolger N, Amarel D. Effects of social support visibility on adjustment to stress: Experimental evidence. J Pers Soc Psychol. 2007;92(3):458–475. doi: 10.1037/0022-3514.92.3.458. [DOI] [PubMed] [Google Scholar]
- Brown JR, Finkelstein A. Supply or demand: Why is the market for long-term care insurance so small? National Bureau of Economic Research Working Paper Series. 2004. Retrieved September 29, 2008, from http://www.nber.org/papers/w10782.
- Bruce ML. Depression and disability in late life: Directions for future research. American Journal of Geriatric Psychiatry. 2001;9(2):102–112. [PubMed] [Google Scholar]
- Burwell B. Medicaid long term care expenditures in FY 2000. 2001. Retrieved February 13, 2004, from http://www.hcbs.org/htmlFile.php/fid/280/did/127/ [DOI] [PubMed]
- Burwell B. Medicaid long term care expenditures, fy 2002. 2003. Retrieved February 13, 2004, from http://www.hcbs.org/files/5/248/2002LTCExpenditures.xls. [DOI] [PubMed]
- Christakis NA, Allison PD. Mortality after the hospitalization of a spouse. New England Journal of Medicine. 2006;354(7):719–730. doi: 10.1056/NEJMsa050196. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310–357. [PubMed] [Google Scholar]
- Fiske A, Gatz M, Pedersen NL. Depressive symptoms and aging: The effects of illness and non-health-related events. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2003;58B(6):320–328. doi: 10.1093/geronb/58.6.p320. [DOI] [PubMed] [Google Scholar]
- Fultz NH, Jenkins KR, Østbye T, Taylor DH, Jr, Kabeto MU, Langa KM. The impact of own and spouse's urinary incontinence on depressive symptoms. Social Science & Medicine. 2005;60(11):2537–2548. doi: 10.1016/j.socscimed.2004.11.019. [DOI] [PubMed] [Google Scholar]
- Harrington C, Carillo HM, Wellin V, Norwood F. 1915(c) Medicaid Home and Community Based Waiver Participants, Services, and Expenditures, 1992-1997. San Francisco, CA: University of California San Francisco, Department of Social and Behavioral Sciences; 2000. [Google Scholar]
- Hedeker D, Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods. 1997;2(1):64–78. [Google Scholar]
- Hedeker D, Gibbons RD. Longitudinal Data Analysis. Hoboken, NJ: John Wiley & Sons, Inc.; 2006. [Google Scholar]
- Herzog AR, Wallace RB. Measures of cognitive functioning in the ahead study. Journal of Gerontology: Social Sciences. 1997;52B(special):37–48. doi: 10.1093/geronb/52b.special_issue.37. [DOI] [PubMed] [Google Scholar]
- Horney J, Osgood DW, Marshall IH. Criminal careers in the short-term: Intra-individual variability in crime and its relation to local life circumstances. American Sociological Review. 1995;60(5):655–673. [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Jang Y, Haley WE, Small BJ, Mortimer JA. The role of mastery and social resources in the associations between disability and depression in later life. Gerontologist. 2002;42(6):807–813. doi: 10.1093/geront/42.6.807. [DOI] [PubMed] [Google Scholar]
- Kane RL, Kane RA, Ladd RC, Veazie WN. Variation in state spending for long-term care: Factors associated with more balanced systems. Journal of Health Politics, Policy and Law. 1998;23(2):364–390. doi: 10.1215/03616878-23-2-363. [DOI] [PubMed] [Google Scholar]
- Kassner E, Williams L. Taking Care of Their Own: State-Funded Home and Community-based Care Programs for Older Persons. Washington, D.C.: The Public Policy Institute, American Association of Retired Persons; 1997. [Google Scholar]
- Kawachi I, Kennedy BP. The relationship of income inequality to mortality: Does the choice of indicator matter? Social Science & Medicine. 1997;45(7):1121–1127. doi: 10.1016/s0277-9536(97)00044-0. [DOI] [PubMed] [Google Scholar]
- Kennedy GJ, Kelman HR, Thomas C. The emergence of depressive symptoms in late life: The importance of declining health and increasing disability. J Community Health. 1990;15(2):93–104. doi: 10.1007/BF01321314. [DOI] [PubMed] [Google Scholar]
- Kitchener M, Carrillo H, Harrington C. Medicaid community-based programs: A longitudinal analysis of state variation in expenditures and utilization. Inquiry. 2003;40:375–389. doi: 10.5034/inquiryjrnl_40.4.375. [DOI] [PubMed] [Google Scholar]
- Kochanek K, Smith B. Deaths: Preliminary data for 2002. National vital statistics reports. 2004;52(13) Retrieved September 28, 2008, from http://www.cdc.gov/nchs/data/nvsr/nvsr52/nvsr52_13.pdf. [PubMed] [Google Scholar]
- Krause N. Perceived health problems, formal/informal support, and life satisfaction among older adults. Journal of Gerontology. 1990;45(5):S193–205. doi: 10.1093/geronj/45.5.s193. [DOI] [PubMed] [Google Scholar]
- Krause N. Anticipated support, received support, and economic stress among older adults. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 1997;52B(6):284–293. doi: 10.1093/geronb/52b.6.p284. [DOI] [PubMed] [Google Scholar]
- Ladd RC, Kane RL, Kane RA. State Long Term Care Profiles Report, 1996. Washington, D.C.: Balancing Long-Term Care, Division of Health Services Research and Policy, School of Public Health, University of Minnesota; 1999. [Google Scholar]
- Ladd RC, Kane RL, Kane RA, Nielsen WJ. State Long Term Care Profiles Report. National LTC Mentoring Program, Institute for Health Services Research, School of Public Health, University of Minnesota; 1995. [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, et al. The association of late-life depression and anxiety with physical disability: A review of the literature and prospectus for future research. American Journal of Geriatric Psychiatry. 2001;9(2):113–135. [PubMed] [Google Scholar]
- Liu K, Manton KG, Aragon C. Changes in home care use by disabled elderly persons: 1982-1994. Journal of Gerontology: Social Sciences. 2000;55B(4):S245–S253. doi: 10.1093/geronb/55.4.s245. [DOI] [PubMed] [Google Scholar]
- Lynch SM, George LK. Interlocking trajectories of loss-related events and depressive symptoms among elders. Journal of Gerontology: Social Sciences. 2002;57B(2):S117–S125. doi: 10.1093/geronb/57.2.s117. [DOI] [PubMed] [Google Scholar]
- Medicare Beneficiary Survey. National Center for Health Statistics, Health Data Interactive. 2006. Retrieved January 19, 2010, Available from: www.cdc.gov/nchs/hdi.htm.
- Mills TL, Henretta JC. Racial, ethnic, and sociodemographic differences in the level of psychosocial distress among older Americans. Research on Aging. 2001;23(2):131–152. [Google Scholar]
- Muramatsu N, Hoyem RL, Yin H, Campbell RT. Place of death among older americans: Does state spending on home- and community-based services promote home death? Medical Care. 2008;46(8):829–838. doi: 10.1097/MLR.0b013e3181791a79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muramatsu N, Yin H, Campbell RT, Hoyem RL, Jacob MA, Ross CO. Risk of nursing home admission among older americans: Does states' spending on home and community-based services matter? Journal of Gerontology: Social Sciences. 2007;62B(3):169–178. doi: 10.1093/geronb/62.3.s169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuhaus JM, Kalbfleisch JD, Hauck WW. A comparison of cluster-specific and population-averaged approaches for analyzing correlated binary data. International Statistical Review / Revue Internationale de Statistique. 1991;59(1):25–35. [Google Scholar]
- Ofstedal MB, Fisher GG, Herzog AR. Documentation of Cognitive Functioning Measures in the Health and Retirement Study. Ann Arbor, MI: Survey Research Center, University of Michigan; 2005. [Google Scholar]
- Ormel J, Rijsdijk F, Sullivan M, van Sonderen E, Kempen GI. Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2002;57B(4):P338–P347. doi: 10.1093/geronb/57.4.p338. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. Journal of Health & Social Behavior. 1981;22(4):337–356. [PubMed] [Google Scholar]
- Radloff LS. The ces-d scale: A self-report depression scale for research in the general population. Applied Psychological Measurement Vol 1(3) Sum 1977. 1977:385–401. [Google Scholar]
- Schulz R, Heckhausen J, O'Brien AT. Control and the disablement process in the elderly. Journal of Social Behavior & Personality Vol 9(5) 1994. 1994:139–152. [Google Scholar]
- Siegel MJ, Bradley EH, Gallo WT, Kasl SV. The effect of spousal mental and physical health on husbands' and wives' depressive symptoms, among older adults: Longitudinal evidence from the health and retirement survey. Journal of Aging and Health. 2004;16(3):398–425. doi: 10.1177/0898264304264208. [DOI] [PubMed] [Google Scholar]
- Spector WD, Fleishman JA. Combining activities of daily living with instrumental activities of daily living to measure functional disability. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 1998;53B(1):S46–S57. doi: 10.1093/geronb/53b.1.s46. [DOI] [PubMed] [Google Scholar]
- Steffick DC. Documentation of Affective Functioning Measures in the Health and Retirement Study. HRS/AHEAD Documentation Report dr-005. 2000. Retrieved April 18, 2008, from http://hrsonline.isr.umich.edu/docs/userg/dr-005.pdf.
- Summer LL, Ihara ES. State Funded Home and Community Based Service Programs for Older People. Washington, DC: AARP Public Policy Institute; 2004. [Google Scholar]
- Szinovacz ME, Davey A. Retirement transitions and spouse disability: Effects on depressive symptoms. Journal of Gerontology: Social Sciences. 2004;59(6):S333–342. doi: 10.1093/geronb/59.6.s333. [DOI] [PubMed] [Google Scholar]
- Taylor MG, Lynch SM. Trajectories of impairment, social support, and depressive symptoms in later life. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2004;59B(4):S238–S246. doi: 10.1093/geronb/59.4.s238. [DOI] [PubMed] [Google Scholar]
- Tsutsui T, Muramatsu N. Japan's universal long-term care system reform of 2005: Containing costs and realizing a vision. Journal of the American Geriatrics Society. 2007;55(9):1458–1463. doi: 10.1111/j.1532-5415.2007.01281.x. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Table sf2. Distribution of women 40 to 44 years old by number of children ever born and marital status: Selected years, 1970 to 2006. Retrieved September 28, 2008, from http://www.census.gov/population/www/socdemo/fertility.html.
- U.S. Department of Health and Human Services. Social Services Block Grant Program: Analysis of Expenditure and Recipient Data 1995-1997. Washington, D.C.: U.S. Government Printing Office; 1999. Administration for Children and Families, Office of Community Services. [Google Scholar]
- U.S. Department of Health and Human Services. Social Services Block Grant Program Annual Report. Washington D.C.: US Government Printing Office; 2000-2004. Administration for Children and Families, Office of Community Services. [Google Scholar]
- U.S. Department of Health and Human Services. Social Services Block Grant Program Annual Report 2002. Washington D.C.: US Government Printing Office; 2004. Office of Community Services. [Google Scholar]
- Wallace RB, Herzog AR, Ofstedal MB, Steffick DC, Fonda S, Langa K. Documentation of Affective Functioning Measures in the Health and Retirement Study. Ann Arbor: Survey Research Center, University of Michigan; 2000. [Google Scholar]
- Winship C, Radbill L. Sampling weights and regression analysis. Sociological Methods and Research. 1994;23:230–257. [Google Scholar]
- Yang Y. Is old age depressing? Growth trajectories and cohort variations in late-life depression. Journal of Health and Social Behavior. 2007;48(1):16–32. doi: 10.1177/002214650704800102. [DOI] [PubMed] [Google Scholar]