Abstract
Objective
Perceived barriers are one of the strongest determinants of health behavior. The current study presents a novel conceptualization of perceived barriers by testing the following hypotheses: (a) perceived barriers are multidimensional and thus should cluster into distinct factors; (b) practical barriers should be salient for individuals intending to engage in a particular health behavior, whereas global barriers should be salient for individuals not intending to enact the behavior; and (c) whereas global barriers should be negatively associated with behavioral intentions, practical barriers should be positively related to intentions.
Methods
The context for this investigation was young adult women’s perceived barriers to human papillomavirus (HPV) vaccination. Two months after viewing an educational video about HPV vaccination, women (aged 18-26) who had not initiated the series (n = 703) reported their perceived barriers to HPV vaccination and intentions to receive the vaccine.
Results
Relative to the conventional single factor approach, a five-factor model provided better fit to the data and accounted for a larger proportion of variance in vaccination intentions. The relative salience of different perceived barriers varied as a function of women’s intentions. Participants who were not intending to get vaccinated cited global concerns about vaccine safety and low perceived need for the vaccine. In contrast, participants intending to get vaccinated cited practical concerns (cost, logistical barriers) related to carrying out their intentions. Moreover, whereas global perceived barriers were associated with lower intentions, practical barriers were associated with higher intentions.
Conclusions
Perceived barriers are multidimensional and vary systematically as a function of people’s behavioral intentions.
Keywords: perceived barriers, theories of health behavior, sexually transmitted infections
When considering whether to engage in a particular health behavior, people are often quick to name the potential barriers that might prevent them from doing so. Consider, for example, common reasons people give for not exercising: “There aren’t enough hours in the day. It’s too cold outside. Exercising hurts. I can’t afford a gym membership. I’m healthy so I don’t need to exercise.” Indeed, most health behaviors are associated with a variety of social, psychological, economic, environmental, and logistical challenges that need to be overcome before the behavior can be initiated and, if necessary, maintained.
The construct of perceived barriers is an important component of most major theories of health behavior (Ajzen, 1988, 1991; Ajzen & Fishbein, 1980; Bandura, 1977; Fishbein & Ajzen, 1975; Prochaska & DiClemente, 1983; Rogers, 1975; Weinstein, 1988; Weinstein & Sandman, 1992). Indeed, in a comprehensive review of studies guided by the health belief model (Rosenstock, 1974), perceived barriers were identified as one of the strongest determinants of health behavior (Janz & Becker, 1984). Not surprisingly, greater perceived barriers are generally associated with a reduced likelihood of behavior change across a wide range of health behaviors (Abraham & Sheeran, 2005; Harrison, Mullen, & Green, 1992).
Despite the importance of perceived barriers, the existing literature is characterized by two important and related limitations. First, previous studies have not fully attended to the multidimensional nature of perceived barriers. Although studies typically assess a variety of barriers believed to hinder behavior change, those barriers are usually treated as a one-dimensional construct (Weinstein, 1993), typically by taking the average of multiple items to form a single composite (e.g., Allen, Mohllajee, Shelton, Othus, Fontenot, & Hanna, 2009; Schmiege, Aiken, Sander, & Gerend, 2007) or by summing the total number of barriers endorsed on a checklist (e.g., Reichert, Barros, Domingues, & Hallal, 2007). We propose that perceived barriers are inherently multidimensional and, as such, will cluster into distinct domains.
Second, previous research has not systematically attended to the possibility that specific perceived barriers are differentially salient for different people. This second limitation is tied to the first: treating barriers as a one-dimensional construct can obscure important variability in the specific barriers that are attended to by different individuals. We propose that people’s perceived barriers will vary as a function of whether or not they are planning to engage in a health behavior. Certain barriers may be especially important in discouraging people from wanting to change their behavior in the first place whereas other barriers may be important for people who have made the decision to engage in the behavior and are assessing how to implement their intentions. In sum, we propose that perceived barriers are multidimensional and that the salience of different perceived barriers should vary as a function of people’s intentions to engage in the health behavior.
This conceptual framework leads to several specific predictions. First, because most health behaviors are associated with perceived barriers from a variety of distinct domains (e.g., personal, environmental, logistical barriers) we hypothesize that perceived barriers should cluster into distinct themes. Although some scholars have pointed to the possibility that perceived barriers are multidimensional (Abraham & Sheeran, 2005; Glasgow, 2008), few empirical studies have systematically investigated the factor structure of perceived barriers. Some supporting evidence for our prediction is provided by a study that conducted an exploratory factor analysis of items assessing common perceived barriers to mammography and Pap testing (Glasgow, Whitlock, Valanis, & Vogt, 2000). Perceived barriers for both cancer screening tests clustered into three correlated factors: 1) Pessimism/Misinformation (e.g., Not necessary for my age), 2) Embarrassment/Mistrust (e.g., Test is embarrassing and uncomfortable), and 3) Logistics (e.g., Inconvenience of appointment). Other studies have cautioned against combining distinct perceived barriers into a single composite, and instead investigated the relationship between individual perceived barrier items and intentions or health behavior (e.g., Champion & Skinner, 2003; Zheng, Sait, Takahashi, Ishibashi, & Kai, 2006). Nevertheless, most studies have failed to conceptualize perceived barriers as a multidimensional construct, and even fewer have systematically investigated the multidimensional structure of perceived barriers or tested it against a one-dimensional structure.
This leads to our second prediction: we propose that the salience of different perceived barriers will vary as a function of whether or not a person is intending to engage in a given health behavior. More specifically, we hypothesize that the types of perceived barriers most salient to individuals who intend to engage in a particular health behavior will center on practical and concrete barriers related to carrying out those intentions. In contrast, perceived barriers for individuals who do not intend to engage in the behavior are expected to center on more global and abstract barriers. These hypotheses are based in theories of self-regulation and goal pursuit. Research suggests that when a goal is active (i.e., when an individual has formed an intention to achieve a particular goal), cognitions needed to achieve that goal become especially accessible (e.g., Förster, Liberman, & Higgins, 2005; Gollwitzer, 1990; Sheeran, 2002; Sheeran, Milne, Webb, & Gollwitzer, 2005). Thus, people who have decided to enact a particular health behavior are likely to focus on practical barriers (e.g., time constraints, cost, logistical barriers) that must be overcome in order to act on their intentions and perform the behavior. In contrast, behaviors that one has decided not to pursue are more psychologically distant, and research suggests that a distant-future time perspective is associated with abstract thinking (Förster, Friedman, & Liberman, 2004). Thus, people who do not intend to perform a health behavior are expected to focus on relatively global and abstract barriers, such as those related to whether or not the behavior is relevant or safe.
Third, we propose the somewhat counterintuitive prediction that, because global barriers should be salient for people who do not intend to engage in a health behavior and practical barriers should be salient for people who do intend to engage in the behavior, global barriers should be negatively associated with intentions to act (as is typically observed), whereas practical barriers should actually be positively associated with intentions. Support for this prediction would stand in contrast to the traditional thinking that the link between barriers and behavioral intentions is uniformly negative. Although not the focus of their investigation, McCree, Brewer, Reiter, Gottlieb, and Smith (2010) provide some initial evidence for this hypothesis in a recent study of parental attitudes and beliefs about human papillomavirus (HPV) vaccine acceptability. The researchers observed an unexpected positive association between perceived barriers and intentions to vaccinate their daughters. Consistent with our theoretical framework, the perceived barriers measured by the authors reflected practical concerns associated with HPV vaccination (e.g., cost, access). In explaining the finding, the authors speculated that parents who were planning to vaccinate their daughters may have been more aware of the immediate practical barriers associated with HPV vaccination.
To test our hypotheses we examined young adult women’s barriers to initiating HPV vaccination. HPV is a common sexually transmitted infection (STI), with the highest rates of infection in young adults aged 20-24 (Markowitz et al., 2007). Certain oncogenic types of HPV (primarily types 16 and 18) can cause cervical cancer in women, while other non-oncogenic types (primarily types 6 and 11) can cause genital warts. A quadrivalent HPV vaccine (Gardasil, Merck & Co. Inc.) that prevents infection with these four types of HPV was introduced in the United States in 2006. A bivalent HPV vaccine (Cervarix, GlaxoSmithKline) targeting HPV types 16 and 18 was approved for use in females in late 2009. HPV vaccination is recommended for females ages 9-26, with special emphasis on 11- and 12-year-old girls (Markowitz et al., 2007). Both vaccines consist of three shots administered (ideally) over a six month period. HPV vaccines are most effective when given before an individual has become sexually active. Uptake has been decidedly low in the U.S. relative to other countries (e.g., UK, Australia) and falls well below the target goal of 80% coverage (Healthy People, 2020). HPV vaccine uptake (receipt of ≥ 1 doses) in 18-26 year-old females is currently estimated to be somewhere between 18% and 41% (Daley et al., 2010; Dempsey, Cohn, Dalton, & Ruffin, 2011).
Several perceived barriers to HPV vaccination have been identified. The most commonly reported barriers to HPV vaccination center on vaccine cost and vaccine safety (Brewer & Fazekas, 2007; Hopfer & Clippard, 2011; Zimet, Weiss, Rosenthal, Good, & Vichnin, 2010). Although HPV vaccination is covered by most major health insurers, the amount of coverage varies. For the uninsured, each dose of the 3-shot series can cost ≥ $130 per shot. Because HPV vaccines are relatively new, people sometimes raise concerns about their safety and unknown side effects (e.g., Constantine & Jerman, 2007; Zimet et al., 2010). Other perceived barriers include concerns about vaccine efficacy, duration of protection, and discomfort and pain associated with receiving an injection (e.g., Dempsey, Zimet, Davis, & Koutsky, 2006; Gerend, Lee, & Shepherd, 2007). An additional barrier is low perceived relevance of the vaccine, which can reflect relationship factors (e.g., being in a monogamous relationship) and perceived appropriateness to one’s lifestyle (e.g., not being sexually active; Constantine & Jerman, 2007; Slomovitz et al., 2006; Zimet et al., 2010). Finally, logistical barriers such as lack of time may prevent women from getting vaccinated (Hopfer & Clippard, 2011). We assessed each of these barriers in the current study.
To summarize, three hypotheses guided the current research. First, we hypothesized that women’s perceived barriers to HPV vaccination would cluster into multiple factors instead of a single factor. Second, we predicted that which barriers would be salient for a given woman would vary as a function of her intentions to receive the HPV vaccine. Women with low intentions to receive the HPV vaccine were expected to be concerned primarily about vaccine safety, side effects, relevance, and effectiveness. In contrast, women with high intentions to receive the HPV vaccine were expected to be concerned primarily about practical and logistical barriers to HPV vaccination such as vaccine cost, health insurance coverage, and time constraints. Third, because perceived barriers are expected to vary as a function of women’s intentions to receive the vaccine, we predicted that some barriers (e.g., vaccine safety concerns, low perceived need) would be negatively associated with HPV vaccination intentions, whereas other barriers (e.g., cost, logistical barriers) would be positively associated with intentions.
Method
Participants
Young adult women attending a large southeastern university in the U.S. were recruited into the study via flyers, announcements posted on the university’s web-based course management system, and the psychology department subject pool. Those interested in the study were directed to a webpage with the screening survey. A total of 2,782 respondents completed the screening survey, of whom 58% (n = 1,612) met eligibility criteria (female; aged 18-26 years; no prior receipt of any doses of the HPV vaccine; not currently pregnant). Most ineligible respondents (n = 1170) had already been vaccinated (n = 888) or fell outside the 18-26 age range (n = 222). All eligible participants were invited to enroll in the study. Invitations were sent via E-mail and data collection continued until we reached our target sample size of 735 participants. Enrollment was closed after 739 participants completed the baseline session.
Baseline data collection took place between March and August of 2009. Participants recruited from the general student body (n = 692) received $30 and participants recruited through the psychology department (n = 47) received course credit for completing the baseline session. The two-month follow-up assessment took place between May and October 2009. In all, 720 (97%) participants completed the follow-up survey, for which they received a $10 gift card.
Mean age of participants at baseline was 21 years old (SD = 1.8; range 18-26). Sixteen percent were Hispanic or Latina. The majority of participants self-identified as White (68%) or Black/African American (19%). The remaining participants self-identified as multi-racial (5%), Asian/Asian American (3%), Native Hawaiian/Pacific Islander (<1%), or American Indian/Alaska Native (<1%). Race was unknown or not reported for 3% and 2% of the sample, respectively. The majority of participants were in their junior (24%) or senior (37%) year of college. Median annual income for this student population fell within the range of $1-$5,000 per year. Most (91%) reported that they had some form of health insurance, with over two thirds covered by their parents’ health insurance. Nearly 80% had ever had sex. See Gerend & Shepherd (2011) for additional information about the sample.
Procedure
This study was approved by the University Human Subjects Committee. Data for the current study were drawn from an HPV vaccination intervention study. After providing informed consent, participants completed a baseline session and an online follow-up assessment approximately two months later. At baseline, participants viewed an educational video about HPV vaccination. The video provided detailed information about HPV infection (its prevalence, transmission, consequences, diagnosis, treatment, risk factors, and association with cervical cancer and genital warts) and the quadrivalent HPV vaccine (its efficacy, safety profile, dosing schedule, cost, etc). We also varied subtle aspects of how information about HPV vaccination was framed (gain-framed, loss-framed, no frame control). The framing manipulation, however, had no effect on participants’ HPV vaccination intentions and thus is not discussed further in this paper. Approximately two months after the baseline session, participants received an email invitation with a secure link to the online follow-up survey. Participants who had not completed the survey after four additional reminder emails were contacted by phone by a research assistant.
Measures
Behavioral intentions
Participants who had not initiated HPV vaccination as of the follow-up (n = 703) reported their intentions for HPV vaccination in the future. Behavioral intentions were assessed with both a single categorical item and a 5-item continuous scale. The categorical question read: Are you planning to get vaccinated for HPV sometime in the future? (No, Yes, Not sure). The intentions scale consisted of five questions assessing participants’ HPV vaccination intentions for the next year (e.g., “How likely is it that you’ll actually get the HPV vaccine?” 1 = very unlikely to 7 = very likely, α = .96). Items had been validated in previous research (Gerend & Shepherd, 2007; Gerend, Shepherd, & Monday, 2008).
Perceived barriers to HPV vaccination
Participants who had not initiated HPV vaccination as of the follow-up (n = 703) reported their barriers to HPV vaccine uptake. Perceived barriers were assessed with an open-ended question followed by several closed-ended questions. The open-ended question assessed perceived barriers to HPV vaccination (“What factors have prevented you from getting the HPV vaccine?). Afterward participants completed 19 closed-ended barriers questions, which were introduced with the following instructions: “How much did the following factors prevent you from getting vaccinated for HPV?” (1 = not at all; 2 = a little; 3 = somewhat; 4 = a lot; 5 = a great deal). Theory (health belief model, Rosenstock, 1974) and previous research (Brewer & Fazekas, 2007; Constantine & Jerman, 2007; Gerend et al., 2007, 2008; Gerend & Shepherd, 2007; Slomovitz et al., 2006; Zimet et al., 2000) guided the development of these items. Items referenced the following barriers to HPV vaccination: vaccine cost, health insurance issues, logistical barriers (e.g., time), fear of shots, concerns about vaccine safety, effectiveness, and side effects, limited sexual behavior (e.g., plans to be abstinent until marriage), and low perceived need for the vaccine.
A codebook for scoring participants’ open-ended responses was developed based on the literature and a preliminary assessment of participants’ responses. Each barriers theme was assigned a code (e.g., 1 = vaccine expense, 2 = insurance issues, etc.). Participants’ responses were coded by three trained raters. Raters were instructed to code each barrier that was mentioned, assigning up to four codes per participant. Miscellaneous factors that did not fall into an existing category and were mentioned by only one person were assigned a special code, as were statements that were too vague to be categorized (e.g., “current situation”). For this question, 26 participants received the miscellaneous code, 18 participants received the “uncodeable” code, and 52 participants said “none.” The overall percent agreement score for the three raters was 97%. Any remaining discrepancies were discussed and resolved.
Data Analyses
Descriptive statistics were computed for all demographic characteristics, open-ended barriers codes, and categorical HPV vaccination intentions. We used t tests and chi-square analyses to compare participants who completed versus did not complete the two-month follow-up survey on demographics, background characteristics, and sexual history variables.
To test the first hypothesis regarding the multidimensional structure of perceived barriers, we randomly split the sample into two halves. In the first half (n = 352) we conducted an exploratory factor analysis (EFA) of the 19 closed-ended barriers items using principal axis factoring with promax rotation. Based on the assumption that some overlap would be expected among perceived barriers (Glasgow et al., 2000), factors were allowed to correlate. Factors with eigenvalues > 1 that were also above the notable bend in the scree plot were retained. In the second half (n = 351) we first conducted a confirmatory factor analysis (CFA) to test a single factor model in which all of the perceived barrier items loaded on one latent factor. Second, we tested whether the factor structure observed in the EFA could be replicated using a more rigorous CFA approach. Each perceived barrier item was constrained to load on its respective factor and latent factors were allowed to correlate. Model fit was assessed with chi-square, the comparative fit index (CFI), the root-mean-square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). CFI values ≥ .90, RMSEA values < .06, and SRMR values < .08 indicate close fit (Hu & Bentler, 1998). Composite scores were created for each latent factor by averaging items associated with each factor.
To test the second hypothesis regarding the differential salience of perceived barriers, we conducted a one-way multivariate analysis of variance (MANOVA) to compare composite-level perceived barrier scores for participants (a) who were intending to receive the HPV vaccine sometime in the future (referred to as “intenders”), (b) who were not intending to receive the vaccine (“non-intenders”), and (c) who were “not sure” about whether they would receive the HPV vaccine (“undecided”). The MANOVA was followed by univariate one-way analysis of variance (ANOVA) tests and post hoc comparisons using Tukey’s Honestly Significant Difference test. To address the issue of family-wise error due to multiple comparisons, we applied a Bonferroni correction. With this correction, p values ≤ .01 represented statistically significant differences. An additional test of the second hypothesis was conducted by examining participants’ open-ended responses as a function of vaccination intentions.
To test the third hypothesis regarding the predictive pattern of perceived barriers, we conducted two separate multiple regression analyses predicting the continuous intentions scale score. In the first analysis, intentions were predicted from the composite factors derived from the CFA. In the second analysis, intentions were predicted from the most frequently mentioned open-ended barriers to HPV vaccination (i.e., barriers mentioned by at least 30 participants). Predictor variables were coded as “1” if the barrier was mentioned; “0” if not mentioned.
Finally, to further test whether a multidimensional approach outperforms the conventional “single factor” barriers score, we conducted a regression analysis in which the continuous intentions scale score was predicted from a single perceived barriers composite that was created from the average of all of the closed-ended barrier items.
Results
Participant Attrition
The response rate for the two-month follow-up survey was 97%. With one exception, non-completers (n = 19) were similar to completers (n = 720) on all demographic and background characteristics (age, education, race, annual income, relationship status, religion, political affiliation) and sexual history variables (sexual orientation, history of sexual intercourse, number of lifetime sexual partners, age of sexual debut). Latina/Hispanic participants were less likely to complete the two-month follow-up survey relative to non-Latina/Hispanic participants (94% vs. 98%), χ2 (1, N = 739) = 5.97, p = .024.
HPV Vaccine Uptake and Intentions
Two months after the intervention, 17 participants reported that they had received at least one shot of the HPV vaccine. Of the 703 participants who had not initiated HPV vaccination as of the two-month follow-up, 27% (n = 187) indicated that they were planning to get vaccinated for HPV sometime in the future, 30% (n = 209) indicated that they were not planning to get vaccinated, and 44% (n = 307) were undecided.
Exploratory Factor Analysis (EFA) of Closed-Ended Barriers
The EFA of the 19 close-ended barrier items resulted in a five factor solution reflecting the following factors: Safety (26% of the variance), Cost (17%), Shots (11%), No Need (9%), and Logistics (6%). Factor loadings, coefficient alpha, and correlations among the five factors are given in Table 1. Notably, one item did not load strongly (≥ .40) on any of the five factors (“The vaccine only protects against some types of HPV.”) and thus was not retained in the CFA.
Table 1. Exploratory Factor Analysis of the 19 Closed-ended Barrier Items: Factor Loadings and Correlations among the Factors.
| Code | Perceived Barrier Item | Factor 1 Safety α = .91 |
Factor 2 Cost α = .88 |
Factor 3 Shots α = .78 |
Factor 4 No Need α = .75 |
Factor 5 Logistics α = .56 |
|---|---|---|---|---|---|---|
| S1 | I have concerns about whether the HPV vaccine is safe. (8) | .854 | −.025 | −.002 | −.024 | −.010 |
| S2 | I have concerns about whether the HPV vaccine is effective. (9) | .559 | .003 | −.014 | −.076 | .222 |
| S3 | I have concerns about possible side effects of the HPV vaccine. (10) | .922 | .012 | −.006 | −.042 | −.019 |
| S4 | The HPV vaccine may have long-term side effects. (13) | .930 | .033 | −.064 | .074 | −.063 |
| S5 | There has not been enough research done on the HPV vaccine. (14) | .894 | .008 | −.040 | .060 | −.018 |
| S6 | My parents don’t want me to get the HPV vaccine. (15) | .475 | −.023 | .091 | −.008 | −.137 |
| -- | The vaccine only protects against some types of HPV. (17) | .320 | −.050 | .069 | −.042 | .224 |
| C1 | Vaccine cost (it’s too expensive). (1) | .000 | .738 | −.054 | −.121 | .079 |
| C2 | My insurance does not cover HPV vaccine. (2) | −.025 | .876 | .020 | .055 | −.049 |
| C3 | My insurance does not cover enough of the vaccine. (3) | .006 | .956 | −.009 | .004 | −.095 |
| C4 | I’m not sure how to file the insurance claim to get reimbursed. (4) | .021 | .642 | .038 | .043 | .162 |
| Sh1 | I’ve heard it hurts a lot to receive the HPV shot. (7) | −.042 | −.029 | .821 | .012 | .104 |
| Sh2 | I have concerns about fainting if I get the HPV shot. (11) | .338 | .042 | .586 | −.020 | −.048 |
| Sh3 | Fear of shots and needles. (16) | −.070 | .003 | .843 | −.002 | −.047 |
| N1 | I don’t think I need the HPV vaccine. (12) | .159 | −.080 | −.068 | .614 | .055 |
| N2 | I plan to be abstinent (not have sex) until marriage. (18) | −.103 | .028 | .020 | .748 | .045 |
| N3 | I plan to only have one sexual partner in my lifetime. (19) | −.020 | .026 | .030 | .867 | −.036 |
| L1 | Getting the HPV shot takes too much time. (5) | −.059 | .026 | −.029 | .001 | .692 |
| L2 | I’m not sure where to get the HPV shot. (6) | .002 | .048 | .058 | .071 | .555 |
|
| ||||||
| Factor 1: Safety | -- | |||||
| Factor 2: Cost | −.03 | -- | ||||
| Factor 3: Shots | .30 | −.07 | -- | |||
| Factor 4: No Need | .15 | −.28 | .02 | -- | ||
| Factor 5: Logistics | .29 | .15 | .53 | −.06 | -- | |
Note. Each barrier item has been assigned a code (e.g., S1) to denote its presence in Figure 1. The numbers in parentheses after each item represent the order in which the item was given on the survey.
Confirmatory Factor Analysis (CFA) of Closed-Ended Barriers
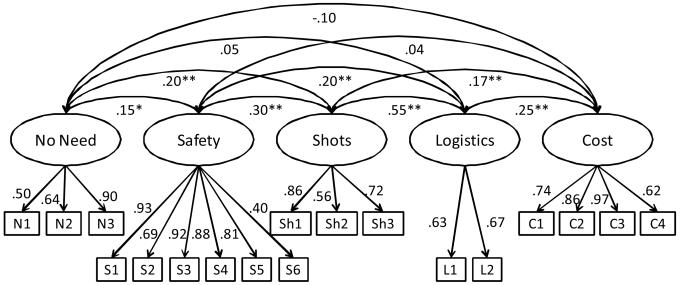
First, we conducted a CFA in which all 18 closed-ended perceived barrier items were specified to load on a single latent factor. Results suggested a very poor fitting model, χ2 (135, N = 327) = 1641.61, p < .001; CFI = .51; RMSEA = .19; SRMR = .17. Second we conducted a CFA in which the 18 barrier items were specified to load on five latent factors, consistent with the results of the EFA. Results suggested that the model provided good fit to the data, χ2 (125, N = 327) = 388.48, p < .001; CFI = .91; RMSEA = .08; SRMR = .08. All factors loadings were statistically significant (p < .001). Factor loadings and correlations among the five latent variables are given in Figure 1. Composite scores were created for each latent factor by taking the average of the items associated with each factor.
Figure 1.
Results from the confirmatory factor analysis of perceived barriers to HPV vaccination,?2 (125, N = 327) = 388.48, p < .001; CFI=.91; RMSEA=.08; SRMR=.08. All factor loadings are statistically significant, p < .001. Correlations among the five factors are depicted. Individual perceived barrier items are labeled by code, e.g., C1 = Vaccine cost (it’s too expensive). See Table 1 for the full list of codes and items. * p < .05 ** p < .01
Mean Barrier Ratings by Intentions to Receive the HPV Vaccine
Next we compared mean levels of the five perceived barrier composites for participants who were intending to receive the vaccine, not intending to receive the vaccine, and those who were undecided (Table 2). Results from the MANOVA indicated that perceived barriers differed by intentions to receive the vaccine, F (10, 1316) = 20.11, p < .001; Wilk’s λ = 0.753, η2 = .133. Based on the ANOVAs, significant mean differences were observed for the three intentions groups on every composite except for Shots, F (2, 662) = .391, p = .676, η2 = .001, and Logistics, F (2, 662) = .983, p = .375, η2 = .003. Consistent with predictions, non-intenders reported the highest safety concerns, followed by undecided participants, F (2, 662) = 23.24, p < .001, η2 = .066. Intenders’ concerns about vaccine safety were significantly lower than both non-intenders and undecided participants. Mean levels for the perceived lack of need composite also clearly demarcated the three intentions groups, F (2, 662) = 55.31, p < .001, η2 = .143, with strongest endorsement observed for non-intenders. Concerns about vaccine expense were stronger for both intenders and undecided participants relative to non-intenders, F (2, 662) = 27.44, p < .001, η2 = .077. Mean differences between intenders vs. non-intenders were the same whether undecided participants were included with non-intenders or excluded from the analyses entirely.
Table 2. Mean (Standard Deviation) Barrier Ratings for the Five Composite Scores by HPV Vaccination Intentions.
| Barrier composite | Intenders (n = 187) |
Undecided (n = 307) |
Non-intenders (n = 209) |
|---|---|---|---|
| No need | 1.7 (0.9)a | 2.3 (1.2)b | 2.9 (1.4)c |
| Safety | 1.8 (0.9)c | 2.3 (1.1)b | 2.6 (1.3)c |
| Shots | 1.6 (0.9)a | 1.5 (0.8)a | 1.6 (1.0)a |
| Cost | 2.8 (1.3)a | 2.7 (1.3)a | 2.0 (1.2)b |
| Logistics | 1.6 (0.7)a | 1.6 (0.7)a | 1.5 (0.8)a |
Note. Means that do not share a superscript are significantly different from one another, p < .01.
Barriers to HPV Vaccination: Open-ended Responses
The most commonly reported perceived barriers to HPV vaccination are given in Table 3. Perceived barriers varied systematically as a function of participants’ intentions to receive the HPV vaccine. Concerns about vaccine safety were more common among non-intenders and undecided participants than intenders. Relative to the other groups, non-intenders were more likely to mention low perceived need for the vaccine and the fact that they did not need the vaccine because they were not sexually active or were currently in a monogamous relationship. Although vaccine expense was the most frequently mentioned barrier in all three categories, it was mentioned more often by participants who were undecided or intended to receive the vaccine, than by participants who did not intend to receive the vaccine. The perceived barrier of time constraints followed a similar pattern to vaccine cost. Finally, intenders were more likely to mention logistical constraints, than were non-intenders or undecided participants.
Table 3. Most Frequently Mentioned Perceived Barriers to HPV Vaccination by HPV Vaccination Intentions.
| Perceived barriers | Intenders n (%) |
Undecided n (%) |
Non-intenders n (%) |
|---|---|---|---|
| No need | |||
| Low need for vaccine | 5 (3%) | 14 (5%) | 24 (12%) |
| Not sexually active | 6 (3%) | 20 (7%) | 24 (12%) |
| Monogamous relationship | 3 (2%) | 23 (8%) | 21 (10%) |
| Safety | |||
| Safety concerns | 3 (2%) | 34 (11%) | 31 (15%) |
| Not enough research; vaccine too new |
3 (2%) | 16 (5%) | 21 (10%) |
| Cost | |||
| Vaccine cost | 103 (55%) | 183 (60%) | 70 (34%) |
| Insurance issues | 35 (19%) | 36 (12%) | 10 (5%) |
| Logistics | |||
| Logistical barriers | 33 (18%) | 15 (5%) | 3 (2%) |
| Time constraints | 60 (32%) | 60 (20%) | 20 (10%) |
Note. Table reflects participants’ coded responses to the following open-ended question: “What factors have prevented you from getting the HPV vaccine?” Entries in this table include those perceived barriers mentioned by ≥ 30 participants. Barriers mentioned by ≥ 10% of participants in each column are printed in bold font. Responses concerning the perceived barrier Shots were made by less than 30 participants and thus are not included in the table.
Multiple Regression Analyses Predicting Intentions from Perceived Barriers
In the first regression analysis we predicted the continuous HPV vaccination intentions scale from the five closed-ended barrier composites based on the CFA. Four of the five factors were significant predictors of HPV vaccination intentions. However, as predicted, the sign of those relationships differed across predictor variables. Safety, β = −.19, t (655) = −5.38, p < .001, partial r (pr) = −.20, and No Need, β = −.38, t (655) = −10.76, p < .001, pr = −.39, emerged as negative predictors of intentions, whereas Cost, β = .17, t (655) = 4.73, p < .001, pr = .18, and Logistics, β = .08, t (655) = 2.11, p = .036, pr = .08, emerged as positive predictors of intentions. Shots was not significantly related to intentions (p = .309). Overall, the five factors accounted for 26% of the variance in HPV vaccination intentions.
In the second regression analysis we predicted the continuous HPV vaccination intentions scale from the most commonly mentioned open-ended barriers to HPV vaccination (i.e., the nine barriers given in Table 3). All nine barriers were significant predictors of vaccination intentions. However, as in the previous analysis, the sign of those relationships differed across predictors. Safety concerns, β = −.09, t (689) = −2.59, p = .01, pr = −.10, not sexually active, β = −.10, t (689) = −3.00, p = .003, pr = −.11, low need for vaccine, β = −.16, t (689) = −4.71, p < .001, pr = −.18, not enough research, β = −.08, t (689) = −2.28, p = .023, pr = −.09, and monogamous relationship, β = −.11, t (689) = −3.10, p = .002, pr = −.12, all emerged as negative predictors of intentions, whereas vaccine cost, β = .13, t (689) = 3.63, p < .001, pr = .14, insurance issues, β = .13, t (689) = 3.74, p < .001, pr = .14, logistics, β = .17, t (689) = 4.93, p < .001, pr = .19, and time constraints, β = .18, t (689) = 5.07, p < .001, pr = .19, emerged as positive predictors of intentions. Predictors accounted for 21% of the variance in HPV vaccination intentions.
Comparison of the Conventional Barriers Scale to the Multidimensional Approach
In our final analysis we created a single composite score from all 18 closed-ended barriers items (M = 2.13; SD = 0.63) and then predicted HPV vaccination intentions from that score. The single composite score was negatively associated with vaccination intentions (β = −.18, t (659) = −4.57, p < .001) and accounted for 3% of the variance in vaccination intentions.
Discussion
The current paper presents a novel conceptualization of perceived barriers, a central construct in most theories of health behavior. Findings suggest that, rather than reflecting a single unified construct, perceived barriers clustered into multiple domains. Moreover, factors perceived to interfere with the adoption of a health behavior (HPV vaccination) varied systematically as a function of whether or not people intended to adopt the behavior. Participants who did not intend to receive the HPV vaccine cited relatively global concerns about vaccine safety and low perceived need for the vaccine. In contrast, participants who were intending to receive the vaccine cited more practical concerns (e.g., vaccine cost, logistical barriers) related to carrying out their intentions. This pattern was also reflected in the relationships observed between perceived barriers and vaccination intentions: whereas global perceived barriers demonstrated the usual negative relationship with intentions, practical barriers displayed a positive relationship with intentions. Participants’ open-ended reasons for not receiving the HPV vaccine provided additional support for the hypothesis that the types of perceived barriers most salient to individuals depend on their intentions to adopt the health behavior.
Findings from the present study support a multidimensional conceptualization of perceived barriers. Although others have noted the potential value of viewing barriers as a multi-faceted construct (Abraham & Sheeran, 2005; Glasgow, 2008), few have systematically examined this possibility. Our results illustrate the value of attending more fully to the heterogeneous nature of perceived barriers. Results from the CFA demonstrated that women’s perceived barriers to HPV vaccination clustered into five distinct but correlated themes that reflected global and practical barriers. Relative to the conventional single factor approach, the five-factor model provided much better fit to the data. In addition, the analysis predicting vaccination intentions from the five perceived barrier composites not only accounted for a substantially larger proportion of the variance in intentions than a single composite, but also revealed barriers that were differentially (positively and negatively) associated with intentions. This analysis further supports the utility of conceptualizing barriers as multidimensional. Combining perceived barrier items into a single composite, as others studies have done, would have obscured these important findings.
One possible interpretation of the current findings is that different perceived barriers may be more or less relevant as people progress through different stages of the health behavior change process. Those barriers that prevent people from intending to engage in a health behavior may be different from those barriers that prevent people from actually carrying out their intentions once they have decided to enact the behavior. Indeed, findings from the present study are consistent with construal level theory (Trope & Liberman, 2003), which proposes that the temporal distance of future events affects people’s mental representation of those events. Distant-future events tend to be represented in abstract terms (high-level construals), whereas near-future events tend to be represented in more concrete terms (low-level construals). Drawing on construal level theory, one might predict that early in the behavior change process, when people are contemplating whether or not to change their behavior, they should focus on relatively abstract barriers associated with the behavior because it is temporally distant. In contrast, after people have made the commitment to change their behavior, people should focus on more concrete barriers associated with enacting the behavior because the event is psychologically nearer. Because the current work did not include a temporal component, it cannot provide direct support for this interpretation; thus future studies are needed to assess directly the extent to which barriers vary as a function of people’s stage of change.
Previous studies have explored differences in perceived barriers by stages of change from the transtheoretical model (TTM; Prochaska & DiClemente, 1983). Nevertheless, in the majority of those studies, perceived barriers were treated as a one-dimensional construct. Therefore, analyses have largely been limited to examining whether perceived barriers as a whole increase or decrease across different stages. Several studies, for instance, have examined differences in women’s perceived barriers to mammography screening as a function of their stage of mammography adoption (e.g., Brenes & Skinner, 1999; Skinner, Champion, Gonin, & Hanna, 1997). Those studies typically show that women in the action stage (i.e., those who have recently received a mammogram) report significantly lower perceived barriers to mammography than women in the precontemplation or contemplation stages. This confirms the intuitive hypothesis that perceived barriers to mammography generally decrease as an individual enacts the behavior. However, this approach provides little information about which barriers in particular are important when women are deciding whether or not to receive a mammogram. Similarly, recent research that applied the TTM to young women’s adoption of HPV vaccination found that women who had been vaccinated reported lower barriers than women who had decided not to receive the vaccine (Allen et al., 2009). Yet, again, perceived barriers were operationalized as a single composite consisting of a mix of different barriers (vaccine cost, pain, safety, side effects, need for multiple doses). This approach obscures the possibility that certain barriers may have been more or less relevant at different stages of the adoption process. The current findings suggest that attending to the multidimensionality of perceived barriers provides critical information about the differential salience of specific barriers. Whether different perceived barriers are salient at different stages of change is an important area for future research.
Findings have important practical implications for behavioral interventions promoting health behavior. Because different barriers are central for different people, health interventions that adopt an individualized tailored approach may be particularly effective in promoting behavior change (Glasgow, 2008; Noar, Benac & Harris, 2007). Future HPV vaccination interventions, for instance, could benefit from tailoring psychoeducational materials to women’s specific perceived barriers. If a woman were to express general concerns about the safety or effectiveness of HPV vaccines, intervention materials could focus on reducing those barriers. If, on the other hand, more practical concerns were raised regarding time constraints or inability to pay for the vaccine, messages could be aimed at helping the woman find a convenient time to receive the vaccine or directing her to clinics that offer the vaccine at a reduced rate.
Limitations of the present study provide useful directions for future research. We noted earlier that although the present findings are generally consistent with a stage-based approach, we did not measure perceived barriers across time or use a particular stage model (e.g., Precaution Adoption Process Model, Weinstein, 1988; Weinstein & Sandman, 1992; TTM, Prochaska & DiClemente, 1983) to guide this research. Future studies may benefit from the longitudinal assessment of perceived barriers, as well as from the application of a specific stage model to help fine-tune hypotheses about which perceived barriers are most relevant at different stages. Future research would also benefit from use of longitudinal designs to examine the extent to which the endorsement of specific barriers at one point in time predicts transitions to later stages. Moreover, as the current study assessed only intentions rather than a behavioral outcome, it will be important for future studies to investigate whether it is possible to predict who adopts versus does not adopt a behavior based on their perceived barriers at a given point in time.
A broader limitation of the current research is that we examined perceived barriers to only one health behavior (HPV vaccination). An important question for future research is whether the current findings generalize to other health behaviors. It is likely that the specific types of perceived barriers applicable to a given health behavior will vary somewhat as a function of the behavior under consideration. Thus, it is important for future studies to assess whether the focus on global barriers versus practical barriers replicates across different health behaviors. Future research should also investigate those perceived barriers that are particularly relevant for people who are trying to maintain (as opposed to initiate) a health behavior.
In closing, perceived barriers to behavior change are one of the most influential determinants of health behavior. The current study demonstrates that perceived barriers are multidimensional and that the relative salience of different perceived barriers varies as a function of people’s intentions to engage in the health behavior. Conceptualizing perceived barriers as a one-dimensional construct, as many studies have, may obscure important information about which barriers are most salient, and thus lead to missed opportunities for intervention. Findings have important implications for theories of health behavior and behavioral interventions aimed at promoting health protective behavior.
Acknowledgments
This research was supported in part by a grant from the National Cancer Institute of the National Institutes of Health (R03-CA138069). We thank members of the Women’s Health research team (Khadija Andrews, Kristina Banda, Kathleen Burns, Michelle DiMarco, Sophia Harvey, Elizabeth Howe, Jessica Kraich, Lisa Langenderfer, Meghan McLeod, Mallory McRoberts, Kristina Martinez, Shella Mesa, Samantha O’Hara, Virginia Parker, Victoria Patronis, Michelle Poole, Alana Resmini, Jennifer Rice, Stephanie Urena, and Becky Wiesenfeld) for their assistance with this project. Helpful comments from Jon Maner are gratefully acknowledged.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/hea.
References
- Abraham C, Sheeran P. Health belief model. In: Conner M, Norman P, editors. Predicting health behavior: Research and practice with social cognition models. 2nd edn. Open University Press; Buckingham, UK: 2005. [Google Scholar]
- Ajzen I. Attitudes, personality, and behavior. Open University Press & Chicago, IL: Dorsey Press; Milton-Keynes, England: 1988. [Google Scholar]
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50:179–211. [Google Scholar]
- Ajzen I, Fishbein M. Englewood Cliffs. Prentice-Hall; NJ: 1980. Understanding attitudes and predicting behavior. [Google Scholar]
- Allen JD, Mohllajee AP, Shelton RC, Othus MK, Fontenot HB, Hanna R. Stage of adoption of the human papillomavirus vaccine among college women. Preventive Medicine. 2009;48(5):420–425. doi: 10.1016/j.ypmed.2008.12.005. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Learning Theory. General Learning Press; New York: 1977. [Google Scholar]
- Brenes GA, Skinner CS. Psychological factors related to stage of mammography adoption. Journal of Women’s Health & Gender-Based Medicine. 1999;8:1313–1321. doi: 10.1089/jwh.1.1999.8.1313. [DOI] [PubMed] [Google Scholar]
- Brewer NT, Fazekas KI. Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Preventive Medicine. 2007;45:107–114. doi: 10.1016/j.ypmed.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Champion VL, Skinner CS. Differences in perceptions of risk, benefits, and barriers by stage of mammography adoption. Journal of Women’s Health. 2003;12:277–286. doi: 10.1089/154099903321667618. [DOI] [PubMed] [Google Scholar]
- Constantine NA, Jerman P. Acceptance of human papillomavirus vaccination among Californian parents of daughters: A representative statewide analysis. Journal of Adolescent Health. 2007;40:108–115. doi: 10.1016/j.jadohealth.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Daley EM, Vamos CA, Buhi ER, Kolar SK, McDermott, Hernandez N, Fuhrmann HJ. Influences on human papillomavirus vaccination status among female college students. Journal of Women’s Health. 2010;19(10):1885–1891. doi: 10.1089/jwh.2009.1861. [DOI] [PubMed] [Google Scholar]
- Dempsey A, Cohn L, Dalton V, Ruffin M. Worsening disparities in HPV vaccine utilization among 19-26 year old women. Vaccine. 2011;29(3):525–534. doi: 10.1016/j.vaccine.2010.10.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempsey AF, Zimet GD, Davis RL, Koutsky L. Factors that are associated with parental acceptance of human papillomavirus vaccines: A randomized intervention study of written information about HPV. Pediatrics. 2006;117:1486–1493. doi: 10.1542/peds.2005-1381. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention, and behavior. Addison-Wesley; Reading, MA: 1975. [Google Scholar]
- Förster J, Liberman N, Higgins ET. Accessibility from active and fulfilled goals. Journal of Experimental Social Psychology. 2005;41:220–239. [Google Scholar]
- Förster J, Friedman R, Liberman N. Temporal construal effects on abstract and concrete thinking: Consequences for insight and creative cognition. Journal of Personality and Social Psychology. 2004;87:177–189. doi: 10.1037/0022-3514.87.2.177. [DOI] [PubMed] [Google Scholar]
- Gerend MA, Lee SC, Shepherd JE. Predictors of human papillomavirus vaccination acceptability among underserved women. Sexually Transmitted Diseases. 2007;34:468–71. doi: 10.1097/01.olq.0000245915.38315.bd. [DOI] [PubMed] [Google Scholar]
- Gerend MA, Shepherd JE. Using message framing to promote acceptance of the human papillomavirus vaccine. Health Psychology. 2007;26:745–752. doi: 10.1037/0278-6133.26.6.745. [DOI] [PubMed] [Google Scholar]
- Gerend MA, Shepherd JE. Correlates of HPV knowledge in the era of HPV vaccination: A study of unvaccinated young adult women. Women & Health. 2011;51:25–40. doi: 10.1080/03630242.2011.540744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerend MA, Shepherd JE, Monday KA. Behavioral frequency moderates the effects of message framing on HPV vaccine acceptability. Annals of Behavioral Medicine. 2008;35:221–229. doi: 10.1007/s12160-008-9024-0. [DOI] [PubMed] [Google Scholar]
- Glasgow RE. Perceived barriers to self-management and preventative behaviors. Retrieved from U. S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute website; 2008. http://cancercontrol.cancer.gov/brp/constructs/barriers/index.html. [Google Scholar]
- Glasgow RE, Whitlock EP, Valanis BG, Vogt TM. Barriers to mammography and Pap smear screening among women who recently had neither, one or both types of screening. Annals of Behavioral Medicine. 2000;22:223–228. doi: 10.1007/BF02895117. [DOI] [PubMed] [Google Scholar]
- Gollwitzer PM. Action phases and mindsets. In: Higgins ET, Sorrentino JRM, editors. The Handbook of Motivation and Cognition. Vol. 2. Guilford; New York: 1990. p. 5392. [Google Scholar]
- Harrison JA, Mullen PD, Green LW. A meta-analysis of studies of the health belief model with adults. Health Education Research. 1992;7:107–116. doi: 10.1093/her/7.1.107. [DOI] [PubMed] [Google Scholar]
- Healthy People Immunization and Infectious Diseases. 2020 http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=23.
- Hopfer S, Clippard JR. College women’s HPV vaccine decision narratives. Qualitative Health Research. 2011;21(2):262–277. doi: 10.1177/1049732310383868. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Janz NK, Becker MH. The health belief model: A decade later. Health Education & Behavior. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER. Quadrivalent Human Papillomavirus Vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP) Morbidity and Mortality Weekly Report: Recommendations and Reports. 2007;56:1–24. [PubMed] [Google Scholar]
- McCree AL, Brewer NT, Reiter PL, Gottlieb SL, Smith JS. The Carolina HPV Immunization Attitudes and Beliefs Scale (CHIAS): Scale development and associations with intentions to vaccinate. Sexually Transmitted Diseases. 2010;37:234–239. doi: 10.1097/OLQ.0b013e3181c37e15. [DOI] [PubMed] [Google Scholar]
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin. 2007;133:673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change in smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology. 1983;51:390–405. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Reichert FF, Barros AJD, Domingues MR, Hallal PC. The role of perceived personal barriers to engagement in leisure-time physical activity. American Journal of Public Health. 2007;97:515–519. doi: 10.2105/AJPH.2005.070144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RW. A protection motivation theory of fear appeals and attitude change. Journal of Psychology. 1975;91:93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. Historical origins of the health belief model. Health Education Monographs. 1974;2:328–335. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- Schmiege SJ, Aiken LS, Sander JL, Gerend MA. Osteoporosis prevention among young women: Psychosocial models of calcium consumption and weight-bearing exercise. Health Psychology. 2007;26(5):577–87. doi: 10.1037/0278-6133.26.5.577. [DOI] [PubMed] [Google Scholar]
- Sheeran P. Intention-behavior relations: A conceptual and empirical review. In: Strobe W, Hewstone M, editors. European Review of Social Psychology. Vol. 12. Wiley; Chichester: 2002. pp. 1–30. [Google Scholar]
- Sheeran P, Milne S, Webb TL, Gollwitzer PM. Implementation intentions and health behaviour. In: Conner M, Norman P, editors. Predicting health behavior: Research and practice with social cognition models. 2nd edn. Open University Press; Buckingham, UK: 2005. [Google Scholar]
- Skinner CS, Champion RG, Hanna M. Do perceived barriers and benefits vary by mammography stage? Psychology, Health & Medicine. 1997;2:65–75. [Google Scholar]
- Slomovitz BM, Sun CC, Frumovitz M, Soliman PT, Schmeler KM, Pearson HC, Berenson A, Bodurka DC. Are women ready for the HPV vaccine? Gynecological Oncology. 2006;103:151–154. doi: 10.1016/j.ygyno.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Trope Y, Liberman N. Temporal construal. Psychological Review. 2003;110:403–421. doi: 10.1037/0033-295x.110.3.403. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. The precaution adoption process. Health Psychology. 1988;7(4):355–386. doi: 10.1037//0278-6133.7.4.355. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. Testing four competing theories of health-protective behavior. Health Psychology. 1993;12(4):324–333. doi: 10.1037//0278-6133.12.4.324. [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Sandman PM. A model of the precaution adoption process: Evidence from home radon testing. Health Psychology. 1992;11(3):1970–180. doi: 10.1037//0278-6133.11.3.170. [DOI] [PubMed] [Google Scholar]
- Zheng YF, Sait T, Takahashi M, Ishibashi T, Kai I. Factors associated with intentions to adhere to colorectal cancer screening follow-up exams. BMC Public Health. 2006;6:272. doi: 10.1186/1471-2458-6-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet GD, Weiss TW, Rosenthal SL, Good MB, Vichnin MD. Reasons for non-vaccination against HPV and future vaccination intentions among 19-26 year-old women. BMC Women’s Health. 2010;10:27. doi: 10.1186/1472-6874-10-27. doi:10.1186/1472-6874-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]