Abstract
External work was utilized to measure differences between the unaffected and the affected limb in patients with unilateral peripheral arterial disease compared to healthy controls. Patients with unilateral peripheral arterial disease have shown deficits in peak joint powers during walking in the unaffected and affected legs. However, no research has detailed the amount of work that is being performed by each leg compared to healthy controls even though such an analysis would provide valuable information on the energy output from the affected and the unaffected legs. Two hypotheses were tested: a) the unaffected and affected leg would perform less work than healthy controls in a pain-free state, and b) the onset of symptomatic claudication pain would result in further changes in the external work. Results showed that during a pain-free state, both the unaffected and affected legs perform less work than the healthy controls. After onset of claudication pain, the work output by the affected limb becomes further decreased while the unaffected limb experiences changes in negative external work. These findings combined with recent evidence of decreased peak powers in both legs in unilateral peripheral arterial disease patients reflects altered pathomechanics in both limbs compared to healthy controls.
Keywords: gait, locomotion, arterial disease, atherosclerosis, biomechanics
Introduction
An inverted pendulum model has been used to describe simple human locomotion(1). In this model, the body’s center of mass moves over the stance leg before reaching the end of the stance phase when there is a period of transition to the other limb which serves as a subsequent inverted pendulum. This period of transition coincides with a push-off for the trailing stance leg, which is performing positive work to raise the center of mass, and a collision for the leading stance leg, a time when the leading stance leg is doing negative work to further redirect the center of mass upwards (2, 3). Positive work is calculated as the integral of the power-time curve above the abscissa. It occurs when the acting force is causing the center of mass to move in a parallel direction. Negative work is calculated as the integral of the power-time curve below the abscissa. It occurs when the acting forces are parallel but opposite the direction of the movement of the center of mass.
The primary contributors to positive work during push-off are the ankle plantar flexors (4). In our laboratory, we have studied patients with peripheral arterial disease (PAD); a condition of decreased blood flow to the affected limb which results in a significant neuromyopathy. They are found to ambulate with decreased peak ankle plantar flexor powers during push-off (5) which variably worsens during peak activity and pain(5, 6).
Peripheral arterial disease is a slowly progressive, chronic disease characterized by atherosclerotic stenoses and occlusions of the arteries supplying the legs. By far, the most common clinical manifestation of symptomatic PAD is claudication. Claudication is defined as walking-induced leg muscle pain and gait dysfunction relieved by rest. When claudicating patients start walking, their leg muscles have adequate perfusion and they experience no pain. With continued walking the metabolic needs of the exercising limb rapidly increase but the blood flow required to support these needs cannot be delivered due to blockages in the arterial system. As exercise continues, the muscles become progressively more ischemic and painful forcing the patient to eventually stop walking.
In addition to the plantar flexor weakness, we have found an overall theme of decreased peak joint power throughout the lower limb(5, 6). Furthermore, we have found that patients affected unilaterally by PAD show similar peak power impairments in both the affected and unaffected limbs (6). The mechanisms through which the unaffected limb is impaired are not fully understood and thus warrant further biomechanical investigation.
The individual limbs method of calculating external work (i.e. work on the body’s center of mass) has recently been used as a means for analyzing work done to move the body through the stance phase(4). This technique has been shown to be more accurate in the estimation of external work than the previously used combined limbs method(3). The individual limbs method for calculating external work calculates the work done on the body’s center of mass by the resultant force for each leg(3). The resultant force is the ground reaction force generated through the leg. This is in contrast to the traditional combined limbs method that did not separate the ground reaction force under each leg but rather combined into a single reaction force from the two legs(7). The combined limbs method would not permit comparison between legs.
The individual limbs method was first used to examine the cost of transition between legs during locomotion, initially in healthy individuals and then recently expanded into pathological gait. For instance, Houdijk et al.(8) utilized the individual limbs method for calculating external work in amputees. Their results showed altered amounts of work through the gait cycle with no difference in absolute total work performed compared to unaffected controls(8). Although they did not study differences between the unaffected and affected leg of their amputee population, a qualitative difference in work output can be observed in their graphs between the affected and unaffected legs of their unilateral amputees(8). They noted that the increased metabolic cost of amputee gait seems to correspond well with decreased positive work at push-off and an increased negative work in early stance loading, resulting in more substantial energy loss from the system during transition between the amputated and the intact limb(8).
A decreased push-off corresponds to an increased amount of negative work at collision for the contralateral leg(3). The amount of negative work during the transition between legs in the gait cycle, or the early stance loading, is associated with increased metabolic cost(9). Individuals with PAD walk with increased energy expenditure and a walking economy that deteriorates with the onset of claudication pain(10, 11). Kurz et al.(12) noted that shifts in the amount of work at different stages in the stance phase may contribute to the increased energy for walking in cerebral palsy children. Performing increased work during the single support phase of gait would require more effort from the hip extensors and would be less energy efficient than if this work was performed in late stance during push-off(13). Therefore, it is possible that a similar mechanical inefficiency is contributing to the increased metabolic cost in PAD patients.
External work calculations have an advantage over internal joint and segmental work calculations by revealing the amount of work being done on the body’s center of mass and therefore can be considered the amount of work being performed to move the person from point “A” to “B”. Thus, it gives a holistic measurement of the individual’s mechanical energy expenditure to get from point “A” to “B”. In the case of a unilaterally affected PAD patient, it can reveal how much mechanical work is being performed by the affected limb and unaffected limb during locomotion and was thus utilized for this study. In addition to PAD limbs, external work was calculated for healthy controls to use as an optimal reference point to compare the amount of work throughout different parts of the stance phase. Finally, in order to further understand the changes that occur with the onset of intermittent claudication, patients were tested in both a pain-free state and a pain state. Two hypotheses were tested: 1) positive and negative work of the affected limb, unaffected limb, and healthy control are different during the pain-free state, and 2) the onset of claudication pain results in further changes in work output of the unaffected limb and affected limb compared to the healthy control.
Methods
Subjects
Sixteen subjects (Table 1) diagnosed with unilateral symptomatic PAD were recruited through the clinics at the Nebraska Western Iowa Veterans Affairs Medical Center and the University of Nebraska Medical Center. In addition, 16 healthy individuals were selected for comparison. PAD patients and healthy controls were screened by a board-certified vascular surgeon. Screening evaluations included resting Ankle-brachial index measurements; levels below 0.9 were necessary for inclusion as a PAD subject. Ankle-brachial index is the ratio of systolic blood pressure at the dorsal pedis and posterior tibialis arteries over the systolic pressure in the brachial artery. Detailed history, physical examination, and visual observation and assessment of walking impairment were also performed. Those subjects with any cardiac, pulmonary, neuromuscular, or musculoskeletal conditions affecting gait were excluded. Subjects also experiencing any pain during ambulation other than claudication were also excluded. No PAD patient had a history of previous revascularization. Control subjects underwent similar screening to the PAD patients. All subjects signed informed consent forms consistent with guidelines set forth by the Institutional Review Boards at the respective medical centers.
Table 1.
Group characteristics for healthy controls and peripheral arterial disease patients. Only age was significantly different.
| Healthy Controls (n=16) mean(SD) | PAD (n=16) mean(SD) | |
|---|---|---|
| Age (yr) | 52.4 (13.1)* | 61.6 (8.4)* |
| Height (cm) | 172.6 (8.3) | 172.1 (7.4) |
| Weight (kg) | 82.4 (23.0) | 88.6 (18.8) |
| Velocity (m/s) (Pain-Free) | 1.15 (0.21) | 1.08 (0.17) |
| Velocity (m/s) (Pain) | 1.07 (0.21) | |
| Ankle-Brachial Index | n/a | 0.54 (0.28) |
Significant at p<0.05
Experimental Design and Procedures
For data collections, subjects presented to the laboratory and wore a tight fitting spandex uniform and athletic shoes. Retroreflective markers were placed at the sacrum, heel, and top of the second metatarsal phalangeal joint. All PAD patients were initially tested in a pain-free state. Three dimensional marker positions were recorded with an 8-camera motion capture system (Motion Analysis, Santa Rosa, CA, USA) sampling at 60 Hz. PAD subjects were tested bilaterally with the order of affected limb (AL) and unaffected limb (UL) randomized. Subjects walked across a 10 meter walkway with an embedded force platform (Kistler Instruments, Winterthur, Switzerland) for five successful trials for each leg. A successful trial was defined as one in which only the leg of interest contacted the force platform and landed entirely within the perimeter of the force platform. Three dimensional ground reaction forces were collected at 600 Hz while subjects walked at a self-selected speed. During the pain-free testing, PAD subjects were required to take a one minute rest between trials to prevent the onset of claudication pain.
Following collection of the AL and UL in a pain-free state, subjects then walked back and forth 15.25 meters continuously in a hallway until the onset of claudication. After patients reported the onset of claudication pain, patients returned for the walking trials in the pain state. Similar procedures were performed except no rest periods were allowed from the moment the patient finished walking in the hallway to the end of the final trial. This was collected as the pain state. For all trials, patients walked at a self-selected speed.
Healthy controls performed the same collection procedure however no trials were performed in the pain state. Healthy controls walked at a self-selected speed as well. The calculation of external work is dependent on velocity of the center of mass, which when averaged over time is the average walking speed for an individual. This limitation makes it necessary to have subjects ambulating at similar self-selected walking speeds. In order to accomplish this, we selected 16 healthy controls with a similar self-selected walking velocity as our 16 unilateral PAD patients. Controls were selected from our database used with our two most recent studies examining PAD gait that utilized the same procedures for the healthy controls with the exception of more retroreflective markers(5, 6). Accordingly, only the sacral, heel, and second matatarsal phalangeal markers were utilized for this study. The right legs of the sixteen healthy controls with the closest matching velocities were used for analyses.
Data Analysis
External work was calculated as the integral of the dot product of the three dimensional ground reaction force of the limb during stance phase in contact with the force platform and the three dimensional velocity of the body’s center of mass.
The vertical ground reaction force was utilized to determine stance phase at a threshold above 10 Newtons. Stance phase was divided into three separate periods(14): initial double support, single support, and terminal double support. Initial double support coincided with the time that the foot came in contact with the force platform while the contralateral limb was still in contact with the floor. During this time the foot is the lead leg and experiences early stance loading resulting in negative work. During single support, the contralateral limb is in swing phase. The terminal double support was the period when the foot was still in contact with the ground and the contralateral foot came into contact with the ground. The leg is now the trailing leg and performing push-off, resulting in a large burst of positive work. These time periods within the stance phase were determined through heel and toe marker kinematic data using techniques described by O’Connor et al.(15). The O’Connor et al.(15) algorithm has been calculated with absolute error rates of 7 ± 6 ms for detecting heel strike and 23 ± 10 ms for toe-off. The velocity of the body’s center of mass was estimated as the derivative of the sacral marker position. It has been shown that the motion of the sacral marker can serve as an accurate estimate for the body’s center of mass in individuals ambulating at speeds below 1.4 m/s(16), which was true for all of our subjects.
For each leg, the periods of initial double support, single support, and terminal double support were analyzed for positive and negative work. In addition, total positive and negative work over the entire stance phase were compared for each leg. Work was normalized to each individual’s body mass(17). All calculations and normalizations were done through custom software in Matlab (Matlab 2009, Mathworks Inc., Concord, MA, USA).
Statistical Analysis
Significant differences for the pain-free and pain states were tested through separate one-way ANOVAs. First comparisons were made for the pain-free state between the AL, UL, and healthy control legs for the following dependent variables: positive work initial double support (PWDS1), negative work initial double support (NWDS1), positive work single support (PWSS), negative work single support (NWSS), positive work terminal double support (PWDS2), negative work terminal double support (NWDS2), total positive work (TotPW), and total negative work (TotNW). The AL, UL, and healthy control legs were then compared for differences in the pain state for the same dependent variables. Tukey post-hoc analyses were utilized for any significant differences. Dependent t-tests were utilized to test for differences in work output by each limb from the pain-free to the pain state. Demographics were compared through independent t-tests between the healthy controls and the PAD patients. A separate ANOVA was used to verify similarity in gait velocity. Significance was set at the 0.05 level.
Results
Only age was significantly different between groups (Table 1). The healthy controls were slightly younger than the PAD patients. Statistical tests confirmed walking velocity was similar for all conditions (healthy controls, PAD pain-free, and PAD pain).
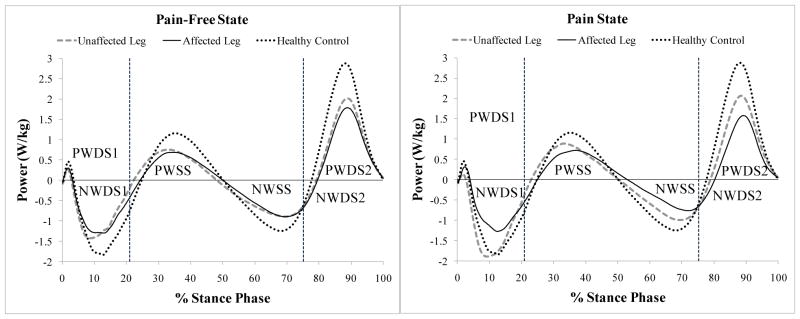
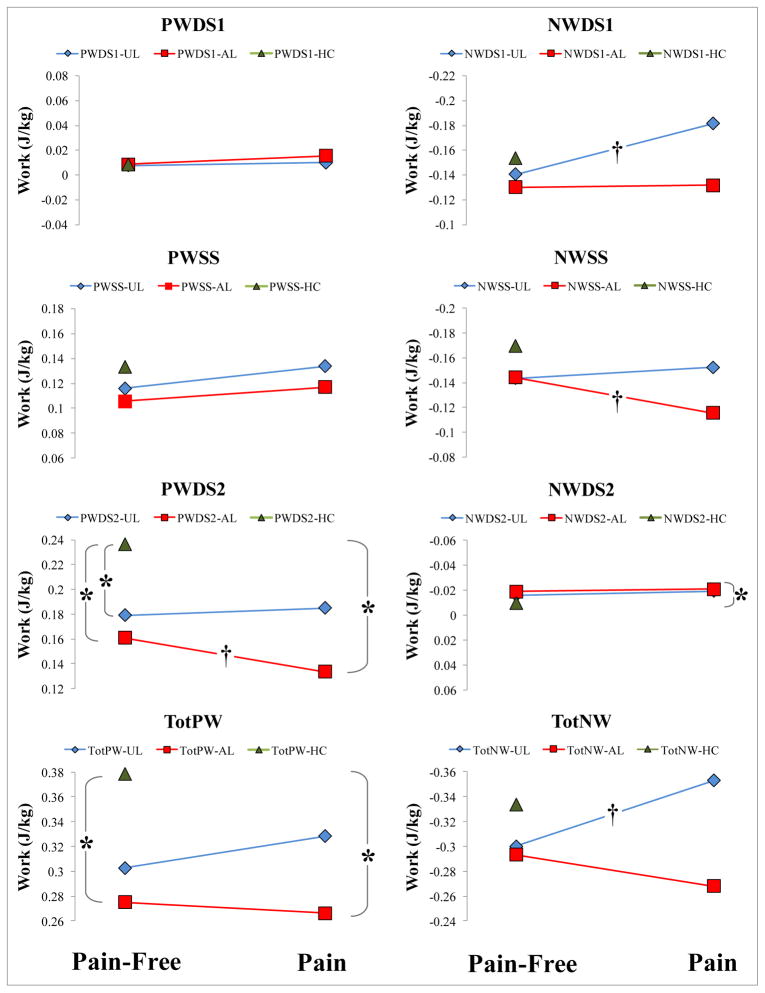
The mean ensemble curves present a descriptive picture of the work output during stance phase for the AL and UL compared to the healthy controls (Figure 1). For the pain-free state, the AL and UL perform significantly less positive work during the terminal double support period (i.e. push-off) compared to the healthy control (Table 2, Figure 2). The AL performs significantly less total positive work than the healthy control during the entire stance phase (Table 2, Figure 2). The difference between the total positive work of the UL and healthy controls did not reach statistical significance.
Figure 1.
Mean ensemble curves for external work (integral of power-time plot). Plots have been normalized to 100% stance phase. Power is normalized to body mass. Vertical dashed lines denote average timing for end of initial double support and beginning of terminal double support. In the pain state, the unaffected leg is doing more work throughout the stance phase as the affected leg takes on less work.
PWDS1, positive work initial double support; NWDS1, negative work initial double support; PWSS, positive work single support; NWSS, negative work single support; PWDS2, positive work terminal double support; NWDS2, negative work terminal double support; TotPW, total positive work through entire stance; TotNW, total negative work through entire stance.
Initial double support corresponds to early stance loading for lead leg. Terminal double support corresponds to push-off for trailing leg.
Table 2.
Results for external work performed by each leg in unilaterally affected peripheral arterial disease (PAD) patients as well as the right leg for sixteen healthy controls ambulating at similar velocity. Values are normalized to body mass.
| Healthy Control (n=16) | PAD patients
|
||||
|---|---|---|---|---|---|
| Pain Free | Pain | ||||
|
| |||||
| Unaffected Leg (n=16) | Affected Leg (n=16) | Unaffected Leg (n=16) | Affected Leg (n=16) | ||
| PWDS1 | 0.0086 ± 0.0054 | 0.0078 ± 0.0057 | 0.0086 ± 0.0050 | 0.0099 ± 0.0076 | 0.0156 ± 0.0169 |
| NWDS1 | −0.1537 ± 0.0648 | −0.1406 ± 0.0573b | −0.1303 ± 0.0465 | −0.1814 ± 0.0797b | −0.1317 ± 0.0684 |
| PWSS | 0.1332 ± 0.0627 | 0.1159 ± 0.0827 | 0.1056 ± 0.0661 | 0.1337 ± 0.0962 | 0.1170 ± 0.0659 |
| NWSS | −0.1698 ± 0.0538 | −0.1435 ± 0.0627 | −0.1440 ± 0.0837a | −0.1524 ± 0.0858 | −0.1156 ± 0.0960a |
| PWDS2 | 0.2367 ± 0.0642 | 0.1790 ± 0.0503* | 0.1607 ± 0.0564*a | 0.1848 ± 0.0743 | 0.1336 ± 0.0649*a |
| NWDS2 | −0.0099 ± 0.0116 | −0.0160 ± 0.0108 | −0.0190 ± 0.0141 | −0.0192 ± 0.0119* | −0.0208 ± 0.0136 |
| TotPW | 0.3785 ± 0.0796 | 0.3027 ± 0.1109 | 0.2749 ± 0.0870* | 0.3284 ± 0.1446 | 0.2662 ± 0.0822* |
| TotNW | −0.3334 ± 0.0815 | −0.3001 ± 0.0952b | −0.2933 ± 0.1069 | −0.3530 ± 0.1420b | −0.2682 ± 0.1371 |
Units = W*s/kg
PWDS1, positive work initial double support; NWDS1, negative work initial double support; PWSS, positive work single support; NWSS, negative work single support; PWDS2, positive work terminal double support; NWDS2, negative work terminal double support; TotPW, total positive work through stance; TotNW, total negative work through stance.
Initial double support corresponds to early stance loading for lead leg. Terminal double support corresponds to push-off for trailing leg.
Significant difference from healthy control (p<0.05)
Significant difference affected leg pain-free vs. pain states (p<0.05)
Significant difference unaffected leg pain-free vs. pain states (p<0.05)
Figure 2.
Average external work by the peripheral arterial disease patients’ unaffected and affected legs during pain-free and pain walking as well as the healthy controls’ legs normalized to body mass. Primary differences occurred with the positive work output in terminal double support for both the unaffected and affected limbs. The onset of pain led to further decreased work output for the affected limb.
UL, unaffected limb; AL, affected limb; PWDS1, positive work initial double support; NWDS1, negative work initial double support; PWSS, positive work single support; NWSS, negative work single support; PWDS2, positive work terminal double support; NWDS2, negative work terminal double support; TotPW, total positive work through entire stance; TotNW, total negative work through entire stance.
Initial double support corresponds to early stance loading. Terminal double support corresponds to push-off.
* Significant vs healthy control, p<0.05
†Significant pain-free vs pain state, p<0.05
For the pain state notable changes occur. During the terminal double support, the AL performs significantly less positive work compared to the healthy control (Table 2, Figure 2). The AL does more negative work during the terminal double support compared to healthy controls (Table 2, Figure 2). The AL still performs significantly less total positive work during the entire stance phase than the healthy control (Table 2, Figure 2).
For the unaffected limb, the increased amount of negative work in the initial double support following onset of claudication pain was significant (Table 2, Figure 2). The amount of negative work over the entire stance phase also significantly increased (Table 2, Figure 2).
For the affected limb, the decreased amount of negative work in single support following onset of claudication pain was significant (Table 2, Figure 2). The increased amount of positive work in terminal double support was also significant (Table 2, Figure 2).
Discussion
This study is the first to investigate the total work of ambulation during stance phase for patients with limbs both affected and unaffected by peripheral arterial disease. PAD is a manifestation of atherosclerosis affecting the arteries supplying the lower extremities with a result of limited blood flow to the leg musculature. Our group has been able to identify patients with unilateral PAD and to evaluate them with advanced biomechanical analysis. Our laboratory has recently shown that unilateral PAD patients produce decreased peak joint powers not only in the affected limb but also the unaffected limb(6). These decreased peak joint powers further decrease with the onset of intermittent claudication. We sought to determine whether the altered peak joint powers in the unaffected and affected limbs are leading to changes in external work in PAD patients. Specifically, we utilized the individual limbs method for calculating the external work that is expended by the affected limb and the unaffected limb in PAD and compared this to healthy controls walking at similar self selected speed. We hypothesized that the unaffected limb and affected limb would exhibit reduced amounts of external work compared to healthy controls in the pain-free state and that the onset of claudication pain would generate further alterations.
Our first hypothesis was supported. In the pain-free state, we found that the unaffected limb and affected limb were both underperforming compared to the healthy controls during the terminal double support when the limb is generating power and producing positive work for push-off. Interestingly though, it was only the affected limb that performed less positive work for the entire stance phase. Although there were no statistical differences between the affected limb and unaffected limb, the comparisons with the healthy controls indicate that the unaffected limb is contributing more energy to the maintenance of locomotion than the affected limb. Compromised performance by both affected and unaffected limbs during pain free ambulation seems to highlight previously demonstrated myopathic changes in the skeletal muscles in both limbs(18) of patients with unilateral PAD. Specifically Bhat et al.(18) reported mitochondrial damage was present in both the affected and unaffected limbs of patients with unilateral PAD. Although the damage was appreciably lower in the unaffected limb compared to the affected one, both limbs had evidence of significantly higher damage than controls.
When the level of exertion had reached such a point that the individual began to suffer from ischemic pain, we noted increased asymmetry in external work in support of our second hypothesis. In the pain state, the affected limb exhibits a decreased magnitude of negative work in single support and less positive work in terminal double support during push-off. To compensate for this the unaffected limb increases positive work in terminal double support to enhance push-off energy. From a mechanical perspective, it is energetically more economical for decreased force production to be maintained over increased time(9). This may indicate that the decreased peak joint powers within the unaffected limb found in Koutakis et al.(6) are partially an adaptation to balance work and minimize energetics.
The finding of decreased external work at various points in the gait cycle from both the affected and unaffected limbs seems to coincide well with previous biomechanical findings of decreased peak joint power output in both limbs of unilaterally affected PAD patients compared to healthy controls(6). In our study, increased physical activity leads to exercise-induced ischemia and increasing workload and they in return produce progressively worsening ischemic muscle pain and restriction of the lower extremity bioenergetics. The affected limb, already malperforming during pain-free walking due to myopathy (19, 20), decreased its work output in the pain-induced condition due to exercise-induced ischemia (blockages in the arteries supplying the affected limb) and increasing workload. The unaffected limb, although malperforming during pain-free walking, does not experience the same decreased work output as the affected limb first because its myopathy is milder than the one of the affected limb(18) and second because it does not have exercise-induced ischemia (there are no blockages in the arteries supplying the unaffected limb). The unaffected limb, therefore, is able to increase its work performance and compensate for the affected limb but never reaches the levels of work output seen with control limbs. This is likely due to its endogenous myopathy and the biomechanics of compensation for a contralateral affected limb. The only significant difference in external work for the unaffected limb from the pain-free to pain states is the negative work during initial double support leading to an increased total amount of negative work through stance phase (Table 2). However, importantly, the initial double support of the unaffected limb is also the terminal double support of the affected limb which has been reported as highly coupled(3). Thus an increased amount of negative work in initial double support for the unaffected limb likely occurs as a byproduct of the decreased positive work during terminal double support from the affected leg in the pain state. A finding consistent with our previous studies(5, 6, 21).
While external work calculation has the distinct advantage of giving an overall performance measure for locomotion, our study does have limitations. First, external work does not account for which muscle groups are performing the work. Although studies have reported the ankle plantar flexors are primarily active and responsible for generating push-off(2–4, 13, 22–26), in a diseased state such as PAD the plantar flexors may not be accountable for a similar percentage of work as established in healthy populations. As such, we do not know the distribution of work within the joints of the lower limbs, thus making it difficult to target exercise or strength rehabilitation towards a single muscle or joint. However, considering the results from our previous studies strongly indicating decreased performance from the ankle plantar flexors(5, 6, 21, 27, 28), the plantar flexors should be considered a major cause behind the decreased positive work by the affected limb during push-off as well as overall for the entire stance phase. Second, the individual limbs method for calculating external work was initially used for comparing the transition between steps (9). This requires capture of the trailing leg and leading leg in the same trial through multiple force platforms. Our study used a single force platform, which can measure work by the limb in contact with the force platform, but it cannot assess the transition period between limbs. However, the purpose of our study was to assess the performance of each limb through the stance phase rather than the transition between legs and thus it served to effectively quantify this. The limitation of a single force platform also required the use of kinematic data for detection of heel strike and toe-off in order to divide stance into the three phases which is not as accurate as force platform data. Finally, PAD patients were assessed in a pain state after they informed the investigator that they had begun feeling claudication pain. Future work should implement a pain scale to relate levels of pain with external work.
In summary, through detailed calculations of external work during walking in patients with unilateral PAD, we have shown that the unaffected limb and affected limb are both performing at a reduced capacity compared to healthy controls. Furthermore, these results suggest that with the onset of claudication, there is a further increase in the impairment of the affected limb secondary to limited blood flow in the setting of increased metabolic need. This reduction in external work is not seen in the unaffected limb. Further studies will be needed in order to determine if successful restoration of blood flow to the affected limb will improve the mechanics of both limbs and to what extent the deficits identified are reversible.
Acknowledgments
The authors kindly acknowledge Mr. Jeffrey Kaipust and Mr. Neil Huben for their assistance with data collection. This work was partly funded through a College of Public Health fellowship through the University of Nebraska Medical Center, National Institute on Aging F31 National Research Service Award, National Institute on Aging R01 Research Award, the Nebraska Research Initiative, and a National Institute on Disability and Rehabilitation Research Field Initiated Award.
Footnotes
Conflict of interest statement
None of the authors have any conflict of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Saunders JB, Inman VT, Eberhart HD. The major determinants in normal and pathological gait. J Bone Joint Surg Am. 1953 Jul;35-A(3):543–58. [PubMed] [Google Scholar]
- 2.Donelan JM, Kram R, Kuo AD. Mechanical work for step-to-step transitions is a major determinant of the metabolic cost of human walking. J Exp Biol. 2002 Dec;205(Pt 23):3717–27. doi: 10.1242/jeb.205.23.3717. [DOI] [PubMed] [Google Scholar]
- 3.Donelan JM, Kram R, Kuo AD. Simultaneous positive and negative external mechanical work in human walking. J Biomech. 2002 Jan;35(1):117–24. doi: 10.1016/s0021-9290(01)00169-5. [DOI] [PubMed] [Google Scholar]
- 4.Kuo AD, Donelan JM, Ruina A. Energetic consequences of walking like an inverted pendulum: Step-to-step transitions. Exerc Sport Sci Rev. 2005 Apr;33(2):88–97. doi: 10.1097/00003677-200504000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Koutakis P, Johanning JM, Haynatzki GR, Myers SA, Stergiou N, Longo GM, et al. Abnormal joint powers before and after the onset of claudication symptoms. J Vasc Surg. 2010 Aug;52(2):340–7. doi: 10.1016/j.jvs.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koutakis P, Pipinos II, Myers SA, Stergiou N, Lynch TG, Johanning JM. Joint torques and powers are reduced during ambulation for both limbs in patients with unilateral claudication. J Vasc Surg. 2010 Jan;51(1):80–8. doi: 10.1016/j.jvs.2009.07.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cavagna GA, Saibene FP, Margaria R. External work in walking. J Appl Physiol. 1963 Jan;18:1–9. doi: 10.1152/jappl.1963.18.1.1. [DOI] [PubMed] [Google Scholar]
- 8.Houdijk H, Pollmann E, Groenewold M, Wiggerts H, Polomski W. The energy cost for the step-to-step transition in amputee walking. Gait Posture. 2009 Jul;30(1):35–40. doi: 10.1016/j.gaitpost.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 9.Kuo AD. A simple model of bipedal walking predicts the preferred speed-step length relationship. J Biomech Eng. 2001 Jun;123(3):264–9. doi: 10.1115/1.1372322. [DOI] [PubMed] [Google Scholar]
- 10.Gardner AW, Ritti-Dias RM, Stoner JA, Montgomery PS, Scott KJ, Blevins SM. Walking economy before and after the onset of claudication pain in patients with peripheral arterial disease. J Vasc Surg. 2010 Mar;51(3):628–33. doi: 10.1016/j.jvs.2009.09.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marconi C, Ferretti G, Anchisi S, Catalano M, Scandale G, Antico A, et al. Energetics of walking in patients with peripheral arterial disease: A proposed functional evaluation protocol. Clin Sci (Lond) 2003 Jul;105(1):105–11. doi: 10.1042/CS20020310. [DOI] [PubMed] [Google Scholar]
- 12.Kurz MJ, Stuberg WA, DeJong SL. Mechanical work performed by the legs of children with spastic diplegic cerebral palsy. Gait Posture. 2010 Mar;31(3):347–50. doi: 10.1016/j.gaitpost.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Kuo AD, Donelan JM. Dynamic principles of gait and their clinical implications. Phys Ther. 2010 Feb;90(2):157–74. doi: 10.2522/ptj.20090125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Watkins J. An introduction to biomechanics of sport and exercise. China: Elsevier; 2007. [Google Scholar]
- 15.O’Connor CM, Thorpe SK, O’Malley MJ, Vaughan CL. Automatic detection of gait events using kinematic data. Gait Posture. 2007 Mar;25(3):469–74. doi: 10.1016/j.gaitpost.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 16.Gard SA, Miff SC, Kuo AD. Comparison of kinematic and kinetic methods for computing the vertical motion of the body center of mass during walking. Hum Mov Sci. 2004 Apr;22(6):597–610. doi: 10.1016/j.humov.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Vanezis A, Lees A. A biomechanical analysis of good and poor performers of the vertical jump. Ergonomics. 2005 Sep-Nov;48(11–14):1594–603. doi: 10.1080/00140130500101262. [DOI] [PubMed] [Google Scholar]
- 18.Bhat HK, Hiatt WR, Hoppel CL, Brass EP. Skeletal muscle mitochondrial DNA injury in patients with unilateral peripheral arterial disease. Circulation. 1999 Feb 16;99(6):807–12. doi: 10.1161/01.cir.99.6.807. [DOI] [PubMed] [Google Scholar]
- 19.Pipinos II, Judge AR, Selsby JT, Zhu Z, Swanson SA, Nella AA, et al. The myopathy of peripheral arterial occlusive disease: Part 1. functional and histomorphological changes and evidence for mitochondrial dysfunction. Vasc Endovascular Surg. 2007 Dec-2008 Jan;41(6):481–9. doi: 10.1177/1538574407311106. [DOI] [PubMed] [Google Scholar]
- 20.Pipinos II, Judge AR, Selsby JT, Zhu Z, Swanson SA, Nella AA, et al. The myopathy of peripheral arterial occlusive disease: Part 2. oxidative stress, neuropathy, and shift in muscle fiber type. Vasc Endovascular Surg. 2008 Apr-May;42(2):101–12. doi: 10.1177/1538574408315995. [DOI] [PubMed] [Google Scholar]
- 21.Chen SJ, Pipinos I, Johanning J, Radovic M, Huisinga JM, Myers SA, et al. Bilateral claudication results in alterations in the gait biomechanics at the hip and ankle joints. J Biomech. 2008 Aug 7;41(11):2506–14. doi: 10.1016/j.jbiomech.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 22.Kuo AD. The six determinants of gait and the inverted pendulum analogy: A dynamic walking perspective. Hum Mov Sci. 2007 Aug;26(4):617–56. doi: 10.1016/j.humov.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 23.Kuo AD. Energetics of actively powered locomotion using the simplest walking model. J Biomech Eng. 2002 Feb;124(1):113–20. doi: 10.1115/1.1427703. [DOI] [PubMed] [Google Scholar]
- 24.Griffin TM, Roberts TJ, Kram R. Metabolic cost of generating muscular force in human walking: Insights from load-carrying and speed experiments. J Appl Physiol. 2003 Jul;95(1):172–83. doi: 10.1152/japplphysiol.00944.2002. [DOI] [PubMed] [Google Scholar]
- 25.Sawicki GS, Ferris DP. Mechanics and energetics of level walking with powered ankle exoskeletons. J Exp Biol. 2008 May;211(Pt 9):1402–13. doi: 10.1242/jeb.009241. [DOI] [PubMed] [Google Scholar]
- 26.Sawicki GS, Ferris DP. Mechanics and energetics of incline walking with robotic ankle exoskeletons. J Exp Biol. 2009 Jan;212(Pt 1):32–41. doi: 10.1242/jeb.017277. [DOI] [PubMed] [Google Scholar]
- 27.Scott-Pandorf MM, Stergiou N, Johanning JM, Robinson L, Lynch TG, Pipinos II. Peripheral arterial disease affects ground reaction forces during walking. J Vasc Surg. 2007 Sep;46(3):491–9. doi: 10.1016/j.jvs.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 28.Celis R, Pipinos II, Scott-Pandorf MM, Myers SA, Stergiou N, Johanning JM. Peripheral arterial disease affects kinematics during walking. J Vasc Surg. 2009 Jan;49(1):127–32. doi: 10.1016/j.jvs.2008.08.013. [DOI] [PubMed] [Google Scholar]