Abstract
Introduction
Mediastinal lymphadenopathy in patients with an extrathoracic malignancy is a common clinical scenario. Invasive sampling of intrathoracic lymph nodes may be performed by mediastinoscopy or endoscopic ultrasound-guided fine needle aspiration. Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is an alternative to mediastinoscopy and endoscopic ultrasound in patients with lung cancer and sarcoidosis. The utility of EBUS-TBNA in patients with extrathoracic malignancy was evaluated.
Methods
Consecutive patients who were suspected to have intrathoracic lymph node metastases from an extrathoracic malignancy underwent EBUS-TBNA. When EBUS-TBNA did not provide a specific diagnosis, patients underwent mediastinoscopy or clinical follow-up of at least 6 months duration.
Results
One hundred sixty-one patients meeting the inclusion criteria underwent EBUS-TBNA in five UK centers over a 3-year period. EBUS-TBNA diagnosed mediastinal or hilar metastases in 71 (44%) patients, new lung cancer in 20 (12%) patients, and sarcoidosis in 14 (9%) patients. The sensitivity, negative predictive value for malignancy, and overall accuracy for EBUS-TBNA were 87%, 73% and 88%, respectively. One hundred ten (68%) patients in the study had a final diagnosis of malignant intrathoracic lymphadenopathy.
Conclusion
Because of the high prevalence of alternative diagnoses, pathological evaluation is important in patients with extrathoracic malignancy and suspected mediastinal or hilar lymph node metastases. EBUS-TBNA is a safe and sensitive technique and may be considered a first-line investigation in these patients.
Keywords: Endobronchial ultrasound, Mediastinal lymphadenopathy, Breast cancer, Lung cancer
Mediastinal lymphadenopathy is a common finding in patients with extrathoracic malignancies and is a frequent diagnostic dilemma for respiratory physicians and oncologists. Enlarged mediastinal nodes are often discovered at the time of initial staging when the demonstration of mediastinal metastases may significantly alter treatment and prognosis. Alternatively, mediastinal lymphadenopathy may be discovered after treatment and require pathological evaluation to exclude or confirm disease recurrence.
Before the advent of endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), sampling of intrathoracic lymphadenopathy was most commonly performed by mediastinoscopy or endoscopic ultrasound-guided fine needle aspiration (EUS-FNA). However, mediastinoscopy is associated with a 1% complication rate1 and requirement for general anesthesia, whereas EUS-FNA does not allow access to the right paratracheal and hilar lymph nodes.2 EBUS-TBNA allows sampling of paratracheal, subcarinal, and hilar lymphadenopathy under sedation in the outpatient setting. The technique has an established role in the diagnosis and staging of lung cancer with a sensitivity of more than 90%, even early in the learning process.3 Prospective data are now available on the utility of EBUS-TBNA in the diagnosis of sarcoidosis,4,5 and a small series has also demonstrated a high diagnostic yield in patients with tuberculous lymphadenopathy.6 Limited data, however, exist on the role of EBUS-TBNA in the diagnosis of extrathoracic malignancies.7 In this large multicenter study, we describe the diagnostic utility of EBUS-TBNA for the clarification of intrathoracic lymphadenopathy in patients with extrathoracic malignancy.
PATIENTS AND METHODS
Participants
Consecutive patients with an active or previous diagnosis of extrathoracic malignancy and enlarged intrathoracic lymphadenopathy who underwent EBUS-TBNA between January 1, 2007, and December 1, 2010, were included. Patients were suspected to have intrathoracic lymph node metastases on the basis of computed tomography or positron emission tomography-computed tomography findings. The participating centers were University College London Hospital, Papworth Hospital, Cambridge, University Hospitals Birmingham, University Hospital of North Tees, and Lancashire Teaching Hospitals, Preston. The observational design of the study meant that ethical approval was not required.
Procedure
EBUS-TBNA was performed with a dedicated linear echo-endoscope (Olympus BF-UC160F-OL8) under moderate sedation with intravenous midazolam and fentanyl or midazolam alone. Systematic assessment of all EBUS accessible lymph nodes was made. Vascular structures were avoided using the Doppler function. Under direct ultrasound guidance, the lymph node was then aspirated using either a 21-gauge or 22-gauge needle. Samples were expelled both onto glass slides where air-dried smears were made for cytology and also into liquid fixative suitable for cell block preparations. In cases where core biopsies were obtained for histology, these were placed directly into formalin. The appropriate immunohistochemical staining with antibodies to the cytokeratins, thyroid transcription factor-1, prostate-specific antigen, estrogen and progesterone receptors, and neuroendocrine markers, was used when required.
Statistical Analysis
Standard definitions of sensitivity, negative predictive value (NPV), and diagnostic accuracy were used. Positive malignant findings on EBUS-TBNA were not confirmed, and specificity was assumed to be 100%. Nonmalignant findings at EBUS-TBNA were subject to surgical confirmation or at least 6 months of radiological and clinical follow-up. Predictors of malignant lymphadenopathy were modeled using logistic regression. Continuous variables were not categorized in the regression analyses. Significant variables in univariate analysis (at the 10% level) or those deemed clinically important were included in the multivariate model. Analysis was carried out with STATA version 10 (Stata corporation). This study conforms to the standards for the reporting of diagnostic accuracy studies initiative.8
RESULTS
All 161 patients successfully underwent EBUS-TBNA and no complications were observed. The median age of the patients was 64 (range 19 – 86) years. The most common extrathoracic malignancies observed were breast, colorectal, and esophageal carcinomas. The patient characteristics are summarized in Table 1.
TABLE 1.
Patient Characteristics
| Total No. of Patients | 161 |
| Male | 73 (45%) |
| Median age (range), yr | 64 (19–86) |
| Median lymph node size (range), mm | 25 (6–48) |
| Extrathoracic malignancy primary site | |
| Breast | 40 |
| Colorectal | 25 |
| Esophagus | 13 |
| Melanoma | 12 |
| Head and neck | 11 |
| Renal cell | 10 |
| Prostate | 9 |
| Bladder | 8 |
| Lymphoma | 7 |
| Ovarian | 5 |
| Sarcoma | 4 |
| Testis | 3 |
| Cervix | 3 |
| Stomach | 3 |
| Endometrial | 2 |
| Penis | 2 |
| Teratoma, anus, vulva, schwannoma | 1 each |
The median size of lymph nodes seen at EBUS-TBNA was 25 (range 6 – 48) mm and each node underwent a median of 4 passes (range 2– 6). One hundred ninety-six nodes were sampled in 160 patients, with no samples taken in one patient. The subcarinal or right paratracheal lymph node stations were the site of aspiration in 100 (62%) patients. Twenty-eight (17%) patients had only hilar lymph nodes sampled. The sensitivity, NPV for malignancy, and overall accuracy for EBUS-TBNA were 87%, 73% and 88%, respectively. The final diagnosis was unknown in six patients. If we assume that the intrathoracic lymph nodes in these patients harbored extrathoracic malignancy (undiagnosed by EBUS-TBNA), the sensitivity, NPV, and accuracy are 78%, 61%, and 84%. Overall, 110 (68%) of the patients in the study were known to have had malignant intrathoracic lymphadenopathy. EBUS-TBNA did not obtain a diagnosis in 13 patients with metastases to intrathoracic nodes from an extrathoracic malignancy. Four patients had breast cancer, one bladder cancer, one renal cell carcinoma, one seminoma, one leiomyosarcoma, three melanoma, one head and neck carcinoma, and one patient had lymphoma.
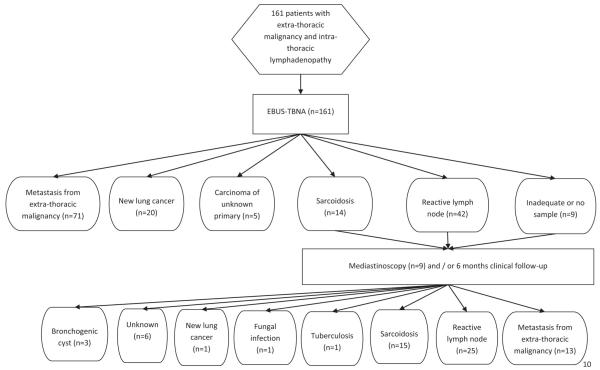
In 14 (9%) patients, EBUS-TBNA demonstrated granulomas alone and the final diagnosis in each of these patients was sarcoidosis. Of the 51 cases, in which EBUS-TBNA did not provide a malignant or alternative diagnosis, surgery was performed in 9 (18%), and a median of 15 months of clinical and radiological follow-up was used in the remainder (Figure 1).
FIGURE 1.
Flowchart of patients.
Univariate analysis of lymph node size, number of passes per node, and number of lymph nodes sampled revealed that there was a statistically significant association between lymph node size and presence of metastatic lymphadenopathy (p = 0.03). In the logistic regression multivariate model, lymph node size remained significantly associated with malignant lymphadenopathy (OR 1.04, 95% confidence interval 1.00 –1.08). This implies that for every increase in lymph node size of 1 mm, the probability of the lymph node being malignant increases by 4%. Univariate analysis demonstrated that there was no association between lymph node size and yield from EBUS-TBNA (p = 0.279).
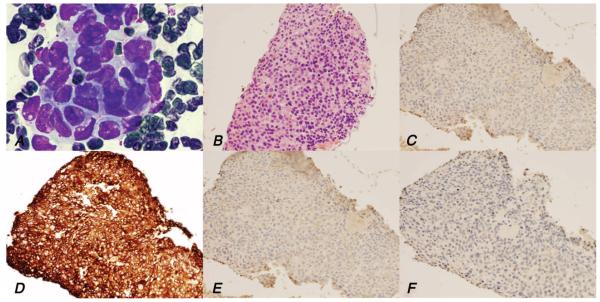
Of the 71 patients with extrathoracic malignancy diagnosed by EBUS-TBNA, morphological appearances alone were sufficient in 17 (24%). Immunohistochemistry was successfully performed in 54 (76%) patients whose EBUS-TBNA had diagnosed malignancy, elucidating the primary origin of the tumor (Figure 2).
FIGURE 2.
EBUS-TBNA samples demonstrating metastatic breast cancer. A, FNA smear shows malignant cells (MGG). B, Cell block preparation contains numerous malignant cells (HE). C, TTF-1 negative staining. D, CK7 positive staining. E, CK20 negative staining. F, ER staining negative. EBUS-TBNA, endobronchial ultrasound-guided transbronchial needle aspiration; MGG, May Grunwald Giemsa stain; HE, hematoxylin and eosin; TTF-1, thyroid transcription factor-1; CK, cytokeratin; ER, estrogen receptor.
DISCUSSION
This multicenter study of 161 patients is the largest to date to demonstrate the role of EBUS-TBNA in the diagnosis of intrathoracic lymphadenopathy in patients with extrathoracic malignancy. EBUS-TBNA demonstrated a sensitivity of 87% with an overall diagnostic accuracy of 88% and therefore is an important alternative to other techniques for the diagnosis of intrathoracic lymphadenopathy in patients with extrathoracic malignancy.
Clarification of mediastinal lymphadenopathy in the context of a known or suspected extrathoracic malignancy is a common scenario faced by physicians and may have profound effects on the patient’s treatment and prognosis. Although mediastinoscopy is considered the gold standard investigation in this clinical scenario, mediastinoscopy is associated with risks due to general anesthesia, a serious complication rate of 1% and increased healthcare costs compared with minimally invasive techniques. Standard cervical mediastinoscopy also only provides access to the paratracheal and anterior subcarinal lymph nodes. Evidence of the utility of alternatives to mediastinoscopy in this patient group is beginning to emerge. A recent report of conventional TBNA in five patients with extrathoracic malignancy9 showed that the procedure is able to provide suitable material for the diagnosis of extrathoracic malignancy. A large study of 75 patients undergoing EUS-FNA demonstrated a sensitivity of 86%,10 whereas Tournoy et al.7 also showed a sensitivity of 85% for EBUS-TBNA in 61 patients with malignant intrathoracic lymphadenopathy.
In this study of 161 patients with suspected metastases from extrathoracic malignancy, only 84 (52%) had a final diagnosis of intrathoracic lymph node metastases, highlighting the importance of pathological confirmation in this clinical scenario. The NPV obtained in this cohort was low at 73%, emphasizing the need for further investigation if EBUS-TBNA did not yield a malignant or other specific diagnosis.
Of note in this study, EBUS-TBNA demonstrated non-caseating granulomas in 14 cases, in all of whom a sarcoid-like reaction was the final diagnosis. Previous studies of granulomas in mediastinal lymph nodes in patients with early-stage non-small cell lung cancer have suggested that this finding reliably excludes malignancy and suggested that clinical follow-up rather than further invasive sampling may be justified in this context.11 The statement that the presence of granulomas may reliably exclude malignancy is questionable. The coexistence of granulomas and malignant cells in metastatic lymph nodes has been described,12 and, although we did not encounter this phenomenon in any of our patients initially diagnosed with sarcoid on EBUS TBNA, we would recommend further investigation when granulomas only are observed in EBUS-TBNA and the suspicion of malignancy remains.
Limitations of this study are recognized. The retrospective nature means that only patients who were clinically selected for EBUS-TBNA were included. Although consecutive patients were included to minimize this bias, the characteristics of patients who were directly referred for mediastinoscopy outside of the study are unknown. The multicenter collaboration strengthens conclusions about the generalizability of the data; however, due to differing pathology practices, standardized immunohistochemistry protocols were not followed.
In conclusion, pathological evaluation is important for diagnosis and staging of patients with extrathoracic malignancy and suspected mediastinal or hilar lymph node metastases. EBUS-TBNA is a safe and sensitive technique and may be considered a first-line investigation in these patients.
ACKNOWLEDGMENTS
N.N. is an MRC Clinical Research Training Fellow. S.M.J. is a Wellcome Trust Senior Fellow in Clinical Science. This study was partly undertaken at UCLH/UCL who received a proportion of funding from the Department of Health’s NIHR Biomedical Research Centers funding scheme (N.N., S.M.J.). This study was also partly undertaken at Papworth Hospital, Cambridge, who were funded by the Department of Health’s NIHR Biomedical Research Centers funding Scheme (R.C.R.) and the Cambridge Experimental Cancer Medicines Center.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Lemaire A, Nikolic I, Petersen T, et al. Nine-year single center experience with cervical mediastinoscopy: complications and false negative rate. Ann Thorac Surg. 2006;82:1185–1189. doi: 10.1016/j.athoracsur.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 2.Navani N, Spiro SG, Janes SM. Mediastinal staging of NSCLC with endoscopic and endobronchial ultrasound. Nat Rev Clin Oncol. 2009;6:278–286. doi: 10.1038/nrclinonc.2009.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Navani N, Nankivell M, Nadarajan P, et al. The learning curve for EBUS-TBNA. Thorax. 2011;66:352–353. doi: 10.1136/thx.2010.146407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tremblay A, Stather DR, Maceachern P, et al. A randomized controlled trial of standard vs endobronchial ultrasonography-guided transbronchial needle aspiration in patients with suspected sarcoidosis. Chest. 2009;136:340–346. doi: 10.1378/chest.08-2768. [DOI] [PubMed] [Google Scholar]
- 5.Navani N, Booth HL, Kocjan G, et al. Combination of endobronchial ultrasound-guided transbronchial needle aspiration with standard bron-choscopic techniques for the diagnosis of stage I and stage II pulmonary sarcoidosis. Respirology. 2011;16:467–472. doi: 10.1111/j.1440-1843.2011.01933.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hassan T, McLaughlin AM, O’Connell F, et al. EBUS-TBNA performs well in the diagnosis of isolated thoracic tuberculous lymphadenopathy. Am J Respir Crit Care Med. 2011;183:136–137. doi: 10.1164/ajrccm.183.1.136. [DOI] [PubMed] [Google Scholar]
- 7.Tournoy KG, Govaerts E, Malfait T, et al. Endobronchial ultrasound-guided transbronchial needle biopsy for M1 staging of extrathoracic malignancies. Ann Oncol. 2011;22:127–131. doi: 10.1093/annonc/mdq311. [DOI] [PubMed] [Google Scholar]
- 8.Bossuyt PM, Reitsma JB, Bruns DE, et al. Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. BMJ. 2003;326:41–44. doi: 10.1136/bmj.326.7379.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bruno P, Pisani L, Ricci A, et al. Cytology on transbronchial needle aspiration (TBNA): not only for lung cancer. Anticancer Res. 2010;30:4769–4772. [PubMed] [Google Scholar]
- 10.Peric R, Schuurbiers OC, Veselic M, et al. Transesophageal endoscopic ultrasound-guided fine-needle aspiration for the mediastinal staging of extrathoracic tumors: a new perspective. Ann Oncol. 2010;21:1468–1471. doi: 10.1093/annonc/mdp578. [DOI] [PubMed] [Google Scholar]
- 11.Steinfort DP, Irving LB. Sarcoidal reactions in regional lymph nodes of patients with non-small cell lung cancer: incidence and implications for minimally invasive staging with endobronchial ultrasound. Lung Cancer. 2009;66:305–308. doi: 10.1016/j.lungcan.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 12.Trisolini R, Cancellieri A, Patelli M. May sarcoidal reaction and malignant features coexist in regional lymph nodes of non-small cell lung cancer patients? Lung Cancer. 2009;66:272–273. doi: 10.1016/j.lungcan.2009.08.005. [DOI] [PubMed] [Google Scholar]