Abstract
Background
Management of cardiovascular risk includes adoption of healthy lifestyles. Uptake and completion rates for lifestyle programmes are low and many barriers and facilitators to lifestyle behaviour change have been reported in the literature. Clarity on which barriers and facilitators to target during consultations in primary care may support a more systematic approach to lifestyle behaviour change in those at high risk of cardiovascular events.
Aim
To identify the main barriers and facilitators to lifestyle behaviour change in individuals at high risk of cardiovascular events.
Design
A content synthesis of the qualitative literature reporting patient-level influences on lifestyle change.
Method
Qualitative studies involving patients at high risk of cardiovascular events were identified through electronic searching and screening against predefined selection criteria. Factors (reported influences) were extracted and, using a clustering technique, organised into categories that were then linked to key themes through relationship mapping.
Results
A total of 348 factors were extracted from 33 studies. Factors were organised into 20 categories and from these categories five key themes were identified: emotions, beliefs, information and communication, friends and family support, and cost/transport.
Conclusion
It is possible to organise the large number of self-reported individual influences on lifestyle behaviours into a small number of themes. Further research is needed to clarify which of these patient-level barriers and facilitators are the best predictors of uptake and participation in programmes aimed at helping people to change lifestyle.
Keywords: cardiovascular diseases, health behaviour, primary health care
INTRODUCTION
There is strong evidence supporting the role of healthy lifestyles in the prevention and management of a range of longer-term conditions, including cardiovascular disease, some cancers, and mental health and musculoskeletal problems.1,2 In the UK, where cardiovascular disease is responsible for 40% of all deaths,3 England's Department of Health vascular check programme is aiming to reduce morbidity and mortality rates by optimal management of those identified as being at high risk, targeting medical risk factors (such as blood pressure and cholesterol) and unhealthy lifestyle behaviours (for example, smoking, physical inactivity, poor diet, and excessive alcohol).4 Underpinning the initiative is the drive to reduce health inequalities, where the risk of developing cardiovascular disease through unhealthy lifestyles is significantly greater in groups of low socioeconomic status than those of high socioeconomic status.5
Targeting lifestyle behaviours requires both organisational and individual commitment and capacity. However, both may be in short supply; for example, only half of all eligible patients are offered cardiac rehabilitation and, of these, one-third choose not to participate.6 Likewise, early estimates of uptake for the Department of Health's vascular check programme suggest that almost 40% are declining screening, with up to 70% not attending in some areas.7,8 Subsequent referral, uptake, and completion rates for lifestyle programmes are not well recorded, due to poor integration between health and social care systems, but evidence from other programmes suggests that high drop-out rates are likely.6,9,10 Known barriers to delivery and uptake of lifestyle change relate to the availability of resources, structure, and skills within the organisation, and to social, cognitive, and emotional factors in the individual.11–13 To date, few primary care-based cardiovascular interventions incorporating lifestyle behaviour change have specifically and systematically targeted personal barriers to change,14–16 and none appears to have considered the role of barriers and facilitators in the design of care pathways.
Clarity on the main influences on uptake and participation in programmes for behaviour change would help to inform the development of referral systems to direct patients more efficiently to appropriate care pathways. In addition to working with patients’ own resources and capabilities, this more tailored approach would potentially free primary care to provide patient support where it is most needed.
As the first step in developing such a lifestyle referral system, this study reviewed and synthesised the qualitative literature to identify the main patient-perceived barriers and facilitators to lifestyle behaviour change among those at high risk of cardiovascular events. A major challenge of such work is to organise what seems like a bewildering number of potential influences into a manageable number of themes that could be used in clinical practice, and this paper reports the framework that was developed to achieve this aim.
How this fits in
There has been a lack of clarity about the main barriers and facilitators to lifestyle behaviour change in individuals at high risk of cardiovascular events. As a possible consequence, decisions on the type of lifestyle support to be provided in primary care are unsystematic, and lifestyle behaviours frequently remain unchanged. This review suggests that through targeting a small number of key barriers and facilitators, primary care could provide more tailored support that may help individuals to achieve lifestyle behaviour change.
METHOD
Selection criteria
The inclusion criteria were: empirical qualitative studies examining lifestyle behaviour change in adults (>18 years of age) who had experienced angina, myocardial infarction, or transient ischaemic attack, or were living with hypertension, hypercholesterolaemia, type 2 diabetes, or coronary artery disease. Studies were excluded if they: were focused on a selected population such as mental health patients; were culturally unrepresentative of the main ethnic groups residing in the UK; included only stroke, chronic obstructive pulmonary disease, peripheral artery disease, or heart failure patients (on the basis that physical limitations would have major influences on lifestyle choices), or studied only patients with type 1 diabetes patients.
Searching
An electronic search strategy was developed (details from authors) and run in MEDLINE®, Health Management Information Consortium, OVID Nursing, PsycINFO® and Embase, from 1980 to February 2010. The start date of 1980 was selected as a reflection of influential public health policies such as the 1984 British Medical Association (BMA) drivers to commence NHS smoking cessation programmes alongside existing and expanding telephone help lines. Likewise, secondary-care-based cardiac rehabilitation programmes began to be routinely offered in the NHS in the 1980s.17 Search results were imported into Endnote (Version X2) and screened against predefined selection criteria. Papers underwent four phases of screening (titles, abstracts [twice], and full papers), with each phase involving four independent reviewers.
Data extraction: identification of factors
Relevant factors reported in individual studies were identified as those that described a patient-reported influence (barrier or facilitator) on the likelihood of taking up some lifestyle behaviour change. Papers were read by a second reviewer if the reported factors appeared ambiguous. Discordant factor ratings were resolved by consensus between reviewers. Each agreed factor was entered as an individual record into an Excel 2007 spreadsheet, along with contextual data relating to the health condition under investigation, whether the factor was reported as a facilitator or barrier, and whether it related to uptake, participation, or maintenance of lifestyle change. Decisions about uptake, participation, and maintenance were made by one reviewer, with a sample of the records undergoing checking by a second reviewer.
Aggregation of factors into categories
Extracted factors were transcribed onto individual notes and organised into categories using a group clustering method.18 This involved four reviewers simultaneously, and without consultation, placing the notes to a blank wall initially and later to congruent categories. Factors could be moved without discussion, until each reviewer was satisfied with the allocation. Towards the end of the exercise, the emergent categories were interpreted and labelled through group discussion. Detailed additional analysis of the contents of each category was performed to ensure unambiguous interpretation of the factors and thus correct allocation.
Identification of key themes
Finally, individual factors within each category were reviewed to identify overlaps or links with other categories. Overlaps were then used to create a relationship map showing clusters of linked and disparate categories. The final clusters or themes were based on a balance between the number of links, the size of the category (number of factors within), and the frequency of uptake factors within the category.
Quality assessment
The quality of the studies was assessed using a combination of the consolidated criteria for reporting qualitative research (COREQ)19 and a tool devised by Long and Godfrey.20 The total number of items in the adapted tool was 43. Each item scored 2, 1, or 0, representing criterion met, partially met (applicable for some items), or not met, respectively. The maximum possible score was 86. As an arbitrary measure of quality, studies were categorised as good (>65%), fair (35–65%), or poor (<35%).
RESULTS
The electronic search strategy generated 16 802 hits (after de-duplication) and, following screening, 49 full papers were obtained. Eight were rejected through failure to explore experiences of behaviour change or because the study population was not clinical. Of the remaining 41 papers, eight focused on healthcare professionals only. Of the 33 studies that were eventually included,13,21–52 21 underwent data extraction by one reviewer and 12 (36%) required two reviewers. Initial agreement between reviewers about reported factors from the 12 papers was 59% (n = 66/112) and all discrepancies were resolved.
Summary of the studies
In total, there were 947 patient participants (range: 5–88 per study). Participants’ ages ranged from 24 to 88 years, with durations of illness from 2 weeks up to 20 years. There was a broad ethnic mix of participants. Sixteen studies were conducted in the US, 13 in Europe (three of which were outside the UK), and two in both Canada and Australia. The majority reported collecting data through individual interviews, with two using additional telephone interviews and seven using focus groups, either alone or in conjunction with individual interviews. The main stated method for sampling participants was purposive (n = 13), with grounded theory, framework analysis, and content analysis reported as the most common analytic frameworks. In nine studies, only females were included and in one, only males. Of the 30 studies that reported the sex make-up of their sample, 384 (40%) participants were male. Half the studies (n = 16) concentrated on a single lifestyle behaviour (Table 1). Moderation of alcohol intake was not examined in any study.
Table 1.
Main characteristics of included studies
| Study characteristic | Number of studiesa | Study reference numbers |
|---|---|---|
| Conditions | ||
| Heart disease | 24 | 13, 22, 23, 25–27, 29–32, 35, 37–39, 41–48, 51 |
| Diabetes | 8 | 21, 24, 28, 34, 46, 49, 52 |
| Hypertension | 2 | 28, 40 |
| Multiple (>2 conditions) | 1 | 33 |
| Behaviours | ||
| Smoking | 9 | 13, 22, 28, 30–33, 37, 41 |
| Diet | 21 | 13, 21, 22, 24–26, 28, 30, 32–43, 36–38, 40, 41, 45, 47–49, 52 |
| Exercise | 24 | 13, 22, 25–30, 32, 34–39, 41, 44–48, 50–52 |
| Medication | 6 | 13, 28, 30, 32, 33, 41 |
| General (unspecified) | 3 | 23, 42, 43 |
| Source of participants | ||
| Hospital (outpatients or inpatients) | 15 | 21–26, 29, 35–37, 39, 40, 42, 44, 48 |
| Community health services | 11 | 27, 28, 32, 33, 37, 38, 41, 43, 46, 47, 52 |
| Other study | 6 | 13, 30, 31, 34, 45, 51 |
| Otherb | 4 | 28, 49–51 |
Some studies included patients with comorbid conditions, examined multiple conditions behaviours, and used multiple sources of participants.
Included non-hospital registers; advertising; churches.
Factors, categories and key themes
In total, 348 (range = 3 to 20 per study) factors were extracted and these were organised into 20 categories (Table 2). There were 194 (56%) reported barriers to behaviour change and 154 facilitators (44%) (Table 3). Factors influencing the uptake of lifestyle change were the most frequent (n = 141; 40%), followed by maintenance (n = 134; 38%), and then participation (n = 66; 19%) with the remaining seven addressing more than one stage.
Table 2.
Summary description of factors within each category
| Category | Description |
|---|---|
| Transport | Difficulties with access to specific centres to undertake rehabilitation; relates to both private and public transport |
| Referrals | Lack of referral or not being informed/offered formal support |
| Language barriers | Inability to communicate directly with providers |
| Cost | Costs associated with transport and daily costs of living |
| Physical environment | Mainly problems exercising due to lack of equipment,a weather,a safety,a and cultural issuesa |
| Physical wellbeing | Physical ill-health, lack of energy, and perceived age and physical limitations as barriers to exercise |
| Balancing and integrating healthcare needs with life | Commitments,a time conflicts,a and lack of flexibility of programmes,a mainly barriers to taking up rehabilitation; evidence of good and poor problem-solving skillsa |
| Social environment | Mainly about the temptations that individuals face in changing and maintaining their health lifestyle |
| Culture | Programmes with exercise may lack cultural sensitivity |
| Friends and family support | Close social support appears to impact on attempts to change and maintain healthy lifestyles; also influence attendance at rehabilitation |
| Social support | Support derived from new network of friends made at rehabilitation programmes |
| Formal programme delivery | Preferences for group and individual exercise activities shown to be influenced by the the composition of groups in formal programmes |
| Emotions | Barriers mostly relating to motivation,a fear,a stress,a confidence,a and embarrassmenta |
| Role of the healthcare professional | Providing encouragement,a being told what to do,a acting as role models,a patient relationships,a and changing for othersa all appear to influence decisions on change |
| Formal support | Ways in which the healthcare provider supports patients during change |
| Attitudes to rehabilitation | Perceptions about role of rehabilitation in recovery |
| Attitudes to exercise | Mainly perceived mental and physical benefits of exercise |
| Information and communication | Lack of knowledgea and misperceptionsa about the purpose of rehabilitation, lifestyle, condition, poor communication about risks and diet |
| Psychological and spiritual beliefs | Beliefs about the role of health behaviours and extent of physical recovery influencing decision making about change |
| Personal choices and cultural preferences | Unwillingness to change (diet/smoking) leading to a perception that adoption of a healthier lifestyle may leave them feeling deprived |
Factors that were reported across a number of studies.
Table 3.
Five key themes and 20 categories
| Categories | Number of papers | Factors (all) | Barriers | Facilitators | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Transport (key theme with cost) | 11 | 12 | 3 | 12 | 100 | 0 | 0 |
| Referrals | 6 | 6 | 2 | 6 | 100 | 0 | 0 |
| Personal choices and cultural preferences | 9 | 11 | 3 | 11 | 100 | 0 | 0 |
| Language barriers | 3 | 4 | 1 | 4 | 100 | 0 | 0 |
| Social environment | 5 | 9 | 3 | 8 | 89 | 1 | 11 |
| Cost (key theme with transport) | 11 | 13 | 4 | 11 | 85 | 2 | 15 |
| Physical environment | 7 | 12 | 3 | 10 | 83 | 2 | 17 |
| Physical wellbeing | 14 | 22 | 6 | 18 | 82 | 4 | 18 |
| Emotions (key theme) | 19 | 27 | 8 | 21 | 78 | 6 | 22 |
| Balancing and integrating healthcare needs with life | 19 | 30 | 9 | 19 | 63 | 11 | 37 |
| Information and communication (key theme) | 17 | 25 | 7 | 14 | 56 | 11 | 44 |
| Formal programme delivery | 10 | 20 | 6 | 10 | 50 | 10 | 50 |
| Culture | 1 | 2 | 1 | 1 | 50 | 1 | 50 |
| Psychological and spiritual beliefs (key theme) | 14 | 31 | 9 | 15 | 48 | 16 | 52 |
| Friends and family support (key theme) | 17 | 35 | 10 | 16 | 46 | 19 | 54 |
| Role of the healthcare professional | 16 | 27 | 8 | 8 | 30 | 19 | 70 |
| Attitudes to rehabilitation | 10 | 11 | 3 | 4 | 36 | 7 | 64 |
| Social support | 15 | 20 | 6 | 4 | 20 | 16 | 80 |
| Attitudes to exercise | 8 | 20 | 6 | 2 | 10 | 18 | 90 |
| Formal support | 7 | 11 | 3 | 0 | 0 | 11 | 100 |
| Total | 348 | 193 | 154 | ||||
See Figure 2 for a diagrammatic explanation of links between categories within key themes.
The largest categories were ‘friends and family support’ and ‘balancing and integrating healthcare needs with (other aspects of daily) life’ (Table 3). Four categories included only factors that were barriers: ‘transport’, ‘personal choices and cultural preferences’, ‘referrals’ and ‘language barriers’. The uptake, participation, and maintenance distributions (Figure 1) indicate that the categories ‘transport’, ‘referrals’, ‘psychological and spiritual beliefs’, ‘attitudes to rehabilitation’, ‘information and communication’, and ‘emotions’ contained mainly barriers to uptake of lifestyle behaviour change, whereas the categories ‘social environment’, ‘physical environment’, and ‘personal choices and cultural preferences’ appear more relevant to maintenance of lifestyle change.
Figure 1.
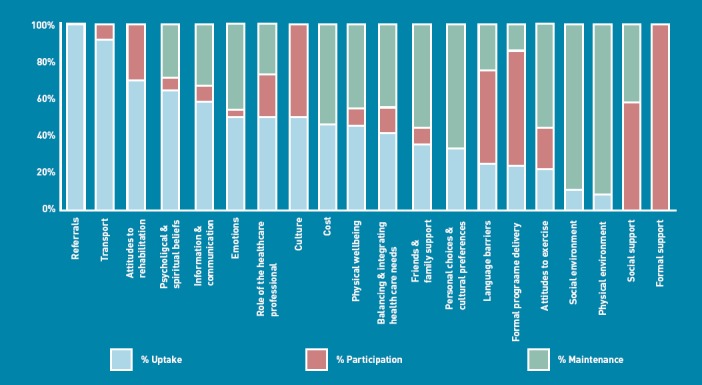
Uptake, participation and maintenance distributions of factors within each category.
Some factors were reported across multiple papers and some categories contained types of factors, for example, ‘balancing and integrating healthcare needs with (other aspects of daily) life’, included commitments, conflicts (time clashes with formal programmes), problem solving (both practical and psychological), and inflexibility (of programmes). ‘Emotions’ included factors that related to motivation, fear, stress, and confidence. ‘Information and communication’ comprised information, communication, misperceptions, and knowledge. Misperceptions about particular programmes or behaviours appeared to influence decisions on uptake and maintenance. The ‘role of the healthcare professional’ category, which was predominantly facilitative, included five main factors: encouragement (and support), being told (that is: accepted paternalistic delivery of care), role models, relationships, and doing it for others.
Analysis of overlap between factors across categories revealed five potential key themes (Figure 2): ‘emotions’, ‘psychological and spiritual beliefs’, ‘information and communication’, ‘friends and family support’, and ‘cost/transport’. Of note is the disparate nature of the cost/transport cluster in comparison to the other clusters.
Figure 2.
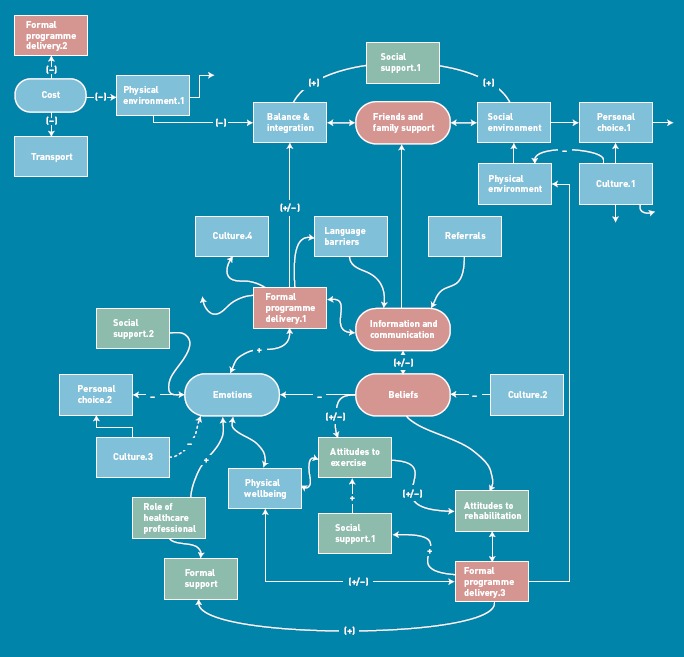
Potential clusters of categories arising from analysis of overlapping factors. Green boxes: categories with <40% barrier type factors. Blue boxes: categories with between 40–59% barriers. Red boxes: categories with ≥60% barriers.
Quality assessment
None of the studies was poor in quality; 28 were fair and five were good. The median score was 48 out of a total possible score of 86 (55%; range 36% to 68%). Studies scored least well in providing information about the relationship between the study participants and the researcher (Table 4). Likewise, certain aspects of the study design such as describing data analysis, and evidence of effort to establish study validity, also scored low. Most of the studies scored well in the ethics section of the tool but over half the studies failed to report whether ethical approval had been granted.
Table 4.
Summary of quality assessment of 33 included studies
| Section and subsection of tool | Number of items | Item most often addressed (number of studiesa) | Item least often addressed (number of studiesa) |
|---|---|---|---|
| Background | 2 | Is it clear what is being studied? (33) | Is sufficient detail given of the nature of the phenomena under study? (33b) |
| Research team and reflexivity | |||
| Personal characteristics | 5 | Is the sex of the researcher clear? (23) | Is the researcher's experience/training reported? (2) |
| Relationships established | 3 | Only one study addressed any of these items | — |
| Study design | |||
| Theoretical framework | 1 | Was a methodological orientation used to underpin the study? (21) | Not applicable |
| Participant selection | 6 | Does the study state how many took part? (32) | Does the study state how many refused or dropped out and does it provide reasons? (14b) |
| Setting | 4 | Was the sample appropriate in terms of depth and width? (33) | Are the important characteristics of the sample reported (demographics, dates)? (9b) |
| Data collection | 7 | Does the author say how many interviews were carried out? (32) | Was data saturation discussed? (5) |
| Data analysis and findings | |||
| Data analysis | 6 | Does the author state if themes were identified in advance or from the data? (29) | Did the authors report checking back with informants over interpretation? (5) |
| Reporting | 4 | Do the quotations reflect the findings? (32) | Do the quotations represent a range of participants? (13b) |
| Ethics | 3 | Is the study ethically sound? (33b) | Does the study report if ethical approval was obtained? (14) |
| Implications | 2 | Are the study findings likely to be transferable to another setting or population? (33b) | Are the conclusions of the study justified, given the conduct of the study? (33b) |
The number of studies completely or partially addressing each item.
Some studies partially addressed this item.
DISCUSSION
Summary
To the authors’ knowledge, this is the first reported synthesis of qualitative studies into patient-reported barriers to and facilitators of lifestyle behaviour change, in individuals with clinical risk factors for, or established, cardiovascular disease. This report is timely, given the recent introduction of the vascular checks programme in England.4 Individuals found to be at high risk of cardiovascular disease through this programme require both medical and lifestyle management in accordance with existing guidelines and resources. However, the barriers reported in the current review demonstrate the challenges that individuals experience in changing lifestyle behaviours.
Despite the paucity of trials evidence, there is a strong rationale and some evidence to support more tailored approaches to lifestyle behaviour change.53–55 What might an effective programme look like? The present study identified both practical and psychological influences on behaviour change, indicating the need for a broad approach to lifestyle assessment and delivery of support. Some categories, such as transport, cost, and education, suggest relatively straightforward responses. Others, such as integrating healthcare needs with other challenges of daily living, and tackling negative beliefs and emotions, will require skilled support staff and some level of organisational commitment. In addition to barriers, the study also sought to identify facilitators to lifestyle behaviour change. In particular, the categories of ‘friends and family support’ and ‘social support’, in which over half the themes were facilitators, suggest the importance of involving significant others wherever possible during lifestyle-change attempts.
The relationship map (Figure 2) shows that, from the patient perspective, many of these categories are linked, and some tentative causal pathways are suggested. However as this review demonstrates, both practical and psychological issues will probably be included in a lifestyle assessment. Targeting a small number of key barriers and facilitators may be feasible in clinical practice and lead to increased attempt and success rates at lifestyle change. As a start, it is suggested that it would be useful for clinicians discussing behaviour change with patients, to consider the influences on their likely response in five key areas:
beliefs about the need to change and likely success of attempts;
knowledge about lifestyles and options;
support from friends and family;
current emotional state, especially anxiety and depression; and
practical problems with finance and travel.
Strengths and limitations
This review has some limitations. Categorisation of factors to uptake, participation, or maintenance was subjective, as many studies did not link experiences of change to any particular period of time or event. A further limitation was that many of the studies focused on physical activity and diet in the context of formal cardiac rehabilitation. Barriers and facilitators across a broader range of behaviours and conditions may indicate different trajectories that would reflect more closely the experiences of those going through the Department of Health vascular check process. Finally, the qualitative nature of the data means that it is not possible to determine which of the self-reported influences are, in reality, the best predictors of behaviour. However, the richness of the data has offered insight into why individuals fail or succeed in their attempts at lifestyle behaviour change, in a way that the quantitative data cannot address. An important next step will be to identify more robustly the categories that predict behaviours, through a complementary review of the quantitative literature.
Comparison with existing literature
Systematic identification and approaches to remove barriers to lifestyle behaviour change have been reported in a limited number of primary care studies.14–16 The interventions were complex, comprising between seven and nine components, and none indicated how chosen barriers were selected, what number of barriers was identified, or how and if they were resolved. Thus, the impact of systematic approaches to identifying and tackling individual barriers to lifestyle behaviour change remains unclear.
Implications for practice and research
The findings from this review suggest that consideration of a core set of psychological and practical issues could help healthcare practitioners to consider a more tailored approach to lifestyle change for individuals at high risk of cardiovascular events. This account of the qualitative literature will be supplemented by a comprehensive review of quantitative research in the area. It will then be possible to develop an assessment procedure based upon research evidence of key influences on lifestyle behaviour change. Subsequent to this, the authors plan to evaluate the effectiveness of this assessment on the use of programmes to which at-risk patients are referred.
Acknowledgments
We thank the National Institute for Health Research Collaborations for Leadership in Applied Health Research and Care (NIHR CLAHRC) for LYB (Leeds, York and Bradford) — a collaboration between two universities, the NHS, and Social Services. We also thank the Leeds York Bradford Collaboration for Applied Health Research and Care (CLAHRC) vascular theme collaborators: Professors Bob Lewin, Simon Gilbody, Ian Watt at the University of York, and Lucy Jackson at NHS Leeds. The views and opinions expressed in this paper are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Funding
National Institute for Health Research Collaborations for Leadership in Applied Health Research and Care.
Ethical approval
Approval was not required for this study.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Blair S. Physical inactivity: the biggest public health problem of the 21st century. Br J Sports Med. 2009;43(1):1–2. [PubMed] [Google Scholar]
- 2.Gillies C, Abrams K, Lambert P, et al. Pharmacological and lifestyle interventions to prevent or delay type 2 diabetes in people with impaired glucose tolerance: systematic review and meta-analysis. BMJ. 2007;334(7588):299. doi: 10.1136/bmj.39063.689375.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Allender S, Foster C, Scarborough P, Rayner M. The burden of physical activity related ill health in the UK. J Epidemiol Community Health. 2007;61(4):344–348. doi: 10.1136/jech.2006.050807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Department of Health. Putting prevention first. Vascular checks: risk assessment and management. London: Department of Health; 2008. [Google Scholar]
- 5.Gerber Y, Koton S, Goldbourt U, et al. Poor neighbourhood socioeconomic status and risk of ischaemic stroke after myocardial infarction. Epidemiology. 2011;22(2):162–169. doi: 10.1097/EDE.0b013e31820463a3. [DOI] [PubMed] [Google Scholar]
- 6.British Heart Foundation. The National Audit of Cardiac Rehabilitation. Annual statistical report 2009. London: British Heart Foundation; 2009. [Google Scholar]
- 7.Dalton A, Bottle A, Okoro C, et al. Uptake of the NHS Health Checks programme in a deprived, culturally diverse setting: cross-sectional study. J Public Health. 2011;33(3):422–429. doi: 10.1093/pubmed/fdr034. [DOI] [PubMed] [Google Scholar]
- 8.Free NHS health check. http://www.healthcheck.nhs.uk/ (accessed 27 Feb 2012)
- 9.Tsai A, Wadden T. Systematic review: an evaluation of major commercial weight loss programs in the United States. Ann Intern Med. 2005;142(1):56–66. doi: 10.7326/0003-4819-142-1-200501040-00012. [DOI] [PubMed] [Google Scholar]
- 10.Williams NH, Hendry M, France B, et al. Effectiveness of exercise-referral schemes to promote physical activity in adults. Br J Gen Pract. 2007;57(545):979–986. doi: 10.3399/096016407782604866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Macintosh MJ, Lacey EA, Tod AM. Secondary prevention for coronary heart disease: a qualitative study. Br J Nurs. 2003;12(8):462–469. doi: 10.12968/bjon.2003.12.8.11272. [DOI] [PubMed] [Google Scholar]
- 12.Summerskill WSM, Pope C. ‘I saw the panic rise in her eyes, and evidence-based medicine went out of the door.’: an exploratory qualitative study of the barriers to secondary prevention in the management of coronary heart disease. Fam Pract. 2002;19(6):605–610. doi: 10.1093/fampra/19.6.605. [DOI] [PubMed] [Google Scholar]
- 13.Jones MI, Greenfield S, Jolly K, BRUM Trial Steering Committee Patients’ experience of home and hospital based cardiac rehabilitation: a focus group study. Eur J Cardiovasc Nurs. 2009;8(1):9–17. doi: 10.1016/j.ejcnurse.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 14.Litaker D, Mion L, Planavsky L, et al. Physician–nurse practitioner teams in chronic disease management: the impact on costs, clinical effectiveness, and patients’ perception of care. J Interprof Care. 2003;17(3):223–237. doi: 10.1080/1356182031000122852. [DOI] [PubMed] [Google Scholar]
- 15.California Medi-Cal Type 2 Diabetes Study Group. Closing the gap: effect of diabetes case management on glycemic control among low-income ethnic minority populations: the California Medi-Cal type 2 diabetes study. Diabetes Care. 2004;27(1):95–103. doi: 10.2337/diacare.27.1.95. [DOI] [PubMed] [Google Scholar]
- 16.Bosworth HB, Olsen MK, Neary A, et al. Take Control of Your Blood Pressure (TCYB) study: a multifactorial tailored behavioral and educational intervention for achieving blood pressure control. Patient Educ Couns. 2008;70(3):338–347. doi: 10.1016/j.pec.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Green V, Stansfield B, Davidson C. Cardiac rehabilitation in the United Kingdom 1985/86: a questionnaire survey. Physiotherapy. 1988;74:363–365. [Google Scholar]
- 18.Backoff RW, Nutt PC. A Process for strategic management with specific application for the non-profit organisation. In: Bryson J, Einsweiler R, editors. Strategic planning: threats and opportunities for planners. Chicago: Planners Press; 1988. pp. 134–135. [Google Scholar]
- 19.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 20.Long AF, Godfrey M. An evaluation tool to assess the quality of qualitative research studies. Int J Soc Res Methodol. 2004;7(2):181–196. [Google Scholar]
- 21.Levine SP, Shah JH, Bell LP, Ritchie TA. Psychological factors affecting adherence to diet in male diabetic patients. Psychol Rep. 1986;59(2 Pt 1):439–445. doi: 10.2466/pr0.1986.59.2.439. [DOI] [PubMed] [Google Scholar]
- 22.Frenn MD, Borgeson DS, Lee HA, Simandl G. Life-style changes in a cardiac rehabilitation program: the client perspective. J Cardiovasc Nurs. 1989;3(2):43–55. doi: 10.1097/00005082-198902000-00006. [DOI] [PubMed] [Google Scholar]
- 23.McSweeney JC. Making behavior changes after a myocardial infarction. West J Nurs Res. 1993;15(4):441–455. doi: 10.1177/019394599301500404. [DOI] [PubMed] [Google Scholar]
- 24.Schlundt DG, Rea MR, Kline SS, Pichert JW. Situational obstacles to dietary adherence for adults with diabetes. J Am Diet Assoc. 1994;94(8):874–876. doi: 10.1016/0002-8223(94)92367-1. [DOI] [PubMed] [Google Scholar]
- 25.Moore SM. Women's views of cardiac rehabilitation programs. J Cardiopulm Rehabil. 1996;16(2):123–129. doi: 10.1097/00008483-199603000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Thornhill M, Stevens JA. Client perceptions of a rural-based cardiac rehabilitation program: a grounded theory approach. Aust J Rural Health. 1998;6(2):105–111. doi: 10.1111/j.1440-1584.1998.tb00293.x. [DOI] [PubMed] [Google Scholar]
- 27.Mitchell R, Muggli M, Sato A. Cardiac rehabilitation: participating in an exercise program in a quest to survive. Rehabil Nurs. 1999;24(6):236–239. doi: 10.1002/j.2048-7940.1999.tb02189.x. [DOI] [PubMed] [Google Scholar]
- 28.Weiss J, Hutchinson SA. Warnings about vulnerability in clients with diabetes and hypertension. Qual Health Res. 2000;10(4):521–537. doi: 10.1177/104973200129118615. [DOI] [PubMed] [Google Scholar]
- 29.McSweeney JC, Crane PB. An act of courage: women's decision-making processes regarding outpatient cardiac rehabilitation attendance. Rehabil Nurs. 2001;26(4):132–140. doi: 10.1002/j.2048-7940.2001.tb01935.x. [DOI] [PubMed] [Google Scholar]
- 30.Wiles R, Kinmonth AL. Patients’ understandings of heart attack: implications for prevention of recurrence. Patient Educ Couns. 2001;44(2):161–169. doi: 10.1016/s0738-3991(00)00187-7. [DOI] [PubMed] [Google Scholar]
- 31.Parry O, Thomson C, Fowkes G. Cultural context, older age and smoking in Scotland: qualitative interviews with older smokers with arterial disease. Health Promot Int. 2002;17(4):309–316. doi: 10.1093/heapro/17.4.309. [DOI] [PubMed] [Google Scholar]
- 32.Crane PB, McSweeney JC. Exploring older women's lifestyle changes after myocardial infarction. Medsurg Nurs. 2003;12(3):170–176. [PubMed] [Google Scholar]
- 33.Durack-Bown I, Giral P, d'Ivernois J-F, et al. Patients’ and physicians’ perceptions and experience of hypercholesterolaemia: a qualitative study. Br J Gen Pract. 2003;53(496):851–857. [PMC free article] [PubMed] [Google Scholar]
- 34.Hall RF, Joseph DH, Schwartz-Barcott D. Overcoming obstacles to behavior change in diabetes self-management. Diabetes Educ. 2003;29(2):303–311. doi: 10.1177/014572170302900221. [DOI] [PubMed] [Google Scholar]
- 35.Jensen BO, Petersson K. The illness experiences of patients after a first time myocardial infarction. Patient Educ Couns. 2003;51(2):123–131. doi: 10.1016/s0738-3991(02)00196-9. [DOI] [PubMed] [Google Scholar]
- 36.Jones LW, Farrell JM, Jamieson J, Dorsch KD. Factors influencing enrollment in a cardiac rehabilitation exercise program. Can J Cardiovasc Nurs. 2003;13(1):11–15. [PubMed] [Google Scholar]
- 37.Clark AM, Barbour RS, White M, MacIntyre PD. Promoting participation in cardiac rehabilitation: patient choices and experiences. J Adv Nurs. 2004;47(1):5–14. doi: 10.1111/j.1365-2648.2004.03060.x. [DOI] [PubMed] [Google Scholar]
- 38.Heid HG, Schmelzer M. Influences on women's participation in cardiac rehabilitation. Rehabil Nurs. 2004;29(4):116–121. doi: 10.1002/j.2048-7940.2004.tb00327.x. [DOI] [PubMed] [Google Scholar]
- 39.Hird C, Upton C, Chesson RA. ‘Getting back to normal’: patients’ expectations of cardiac rehabilitation. Physiotherapy. 2004;90(3):125–131. [Google Scholar]
- 40.Horowitz CR, Tuzzio L, Rojas M, et al. How do urban African Americans and Latinos view the influence of diet on hypertension? J Health Care Poor Underserved. 2004;15(4):631–644. doi: 10.1353/hpu.2004.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McSweeney JC, Coon S. Women's inhibitors and facilitators associated with making behavioral changes after myocardial infarction. Medsurg Nurs. 2004;13(1):49–56. [PubMed] [Google Scholar]
- 42.MacInnes JD. The illness perceptions of women following acute myocardial infarction: implications for behaviour change and attendance at cardiac rehabilitation. Women Health. 2005;42(4):105–121. doi: 10.1300/j013v42n04_06. [DOI] [PubMed] [Google Scholar]
- 43.Woodard LD, Hernandez MT, Lees E, Petersen LA. Racial differences in attitudes regarding cardiovascular disease prevention and treatment: a qualitative study. Patient Educ Couns. 2005;57(2):225–231. doi: 10.1016/j.pec.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 44.Hagan NA, Botti MA, Watts RJ. Financial, family, and social factors impacting on cardiac rehabilitation attendance. Heart Lung. 2007;36(2):105–113. doi: 10.1016/j.hrtlng.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 45.Jones M, Jolly K, Raftery J, et al. ‘DNA’ may not mean ‘did not participate’: a qualitative study of reasons for non-adherence at home and centre-based cardiac rehabilitation. Fam Pract. 2007;24(4):343–357. doi: 10.1093/fampra/cmm021. [DOI] [PubMed] [Google Scholar]
- 46.Sriskantharajah J, Kai J. Promoting physical activity among South Asian women with coronary heart disease and diabetes: what might help? Fam Pract. 2007;24(1):71–76. doi: 10.1093/fampra/cml066. [DOI] [PubMed] [Google Scholar]
- 47.Vishram S, Crosland A, Unsworth J, Long S. Engaging women from South Asian communities in cardiac rehabilitation. Br J Community Nurs. 2007;12(1):13–18. doi: 10.12968/bjcn.2007.12.1.22686. [DOI] [PubMed] [Google Scholar]
- 48.Astin F, Atkin K, Darr A. Family support and cardiac rehabilitation: a comparative study of the experiences of South Asian and White-European patients and their carer's living in the United Kingdom. Eur J Cardiovasc Nurs. 2008;7(1):43–51. doi: 10.1016/j.ejcnurse.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 49.Beverly EA, Miller CK, Wray LA. Spousal support and food-related behavior change in middle-aged and older adults living with type 2 diabetes. Health Educ Behav. 2008;35(5):707–720. doi: 10.1177/1090198107299787. [DOI] [PubMed] [Google Scholar]
- 50.Ferrand C, Perrin C, Nasarre S. Motives for regular physical activity in women and men: a qualitative study in French adults with type 2 diabetes, belonging to a patients’ association. Health Soc Care Community. 2008;16(5):511–520. doi: 10.1111/j.1365-2524.2008.00773.x. [DOI] [PubMed] [Google Scholar]
- 51.Traywick LS, Schoenberg NE. Determinants of exercise among older female heart attack survivors. J Appl Gerontol. 2008;27(1):52–77. [Google Scholar]
- 52.Malpass A, Andrews R, Turner KM. Patients with type 2 diabetes experiences of making multiple lifestyle changes: A qualitative study. Patient Educ Couns. 2009;74(2):258–263. doi: 10.1016/j.pec.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 53.Sturt JA, Whitlock S, Fox C, et al. Effects of the Diabetes Manual 1:1 structured education in primary care. Diabet Med. 2008;25(6):722–731. doi: 10.1111/j.1464-5491.2008.02451.x. [DOI] [PubMed] [Google Scholar]
- 54.Schroeder K, Fahey T, Hollinghurst S, Peters TJ. Nurse-led adherence support in hypertension: a randomized controlled trial. Fam Pract. 2005;22(2):144–151. doi: 10.1093/fampra/cmh717. [DOI] [PubMed] [Google Scholar]
- 55.Groeneveld Y, Petri H, Hermans J, Springer M. An assessment of structured care assistance in the management of patients with type 2 diabetes in general practice. Scand J Prim Health Care. 2001;19(1):25–30. doi: 10.1080/028134301300034585. [DOI] [PubMed] [Google Scholar]


