Abstract
Background
New care modes in primary care may affect patients’ experienced continuity of care.
Aim
To analyse whether experienced continuity for patients with chronic obstructive pulmonary disease (COPD) changes after different care modes are introduced, and to analyse the relationship between continuity of care and patients’ quality of life.
Design and setting
Randomised controlled trial with 2-year follow-up in general practice in the Netherlands.
Method
A total of 180 patients with COPD were randomly assigned to three different care modes: self-management, regular monitoring by a practice nurse, and care provided by the GP at the patient's own initiative (usual care). Experienced continuity of care as personal continuity (proportion of visits with patient's own GP) and team continuity (continuity by the primary healthcare team) was measured using a self-administered patient questionnaire. Quality of life was measured using the Chronic Respiratory Questionnaire.
Results
Of the final sample (n = 148), those patients receiving usual care experienced the highest personal continuity, although the chance of not contacting any care provider was also highest in this group (29% versus 2% receiving self-management, and 5% receiving regular monitoring). There were no differences in experienced team continuity in the three care modes. No relationship was found between continuity and changes in quality of life.
Conclusion
Although personal continuity decreases when new care modes are introduced, no evidence that this affects patients’ experienced team continuity or patients’ quality of life was found. Patients still experienced smooth, ongoing care, and considered care to be connected. Overall, no evidence was found indicating that the introduction of new care modes in primary care for patients with COPD should be discouraged.
Keywords: continuity of patient care; general practice; pulmonary disease, chronic obstructive; quality of life
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is highly prevalent and one of the leading causes of morbidity and mortality worldwide.1 Its prevalence is predicted to rise in the coming decades, which will result in an increased burden on healthcare systems.1,2
In primary care, new care modes are being introduced to improve quality and to cope with the increased workload of COPD in primary care globally. Practice nurses take over elements of COPD care and self-management programmes are introduced to increase patients’ self-care. There are concerns that the introduction of these new care modes may be a threat to patients’ experienced continuity in primary care, both in terms of personal continuity (seeing the same care provider) and team continuity (continuity by the primary healthcare team). Other studies have shown that decreased personal continuity is related to less confidence in care providers3,4 and less satisfaction with care.4–6 Moreover, patients’ adherence to treatment and prevention might decrease.7 The evidence is still inconclusive as to whether decreased levels of continuity are also related to reduced quality of life.8–11
In this study the experienced continuity of care of patients with COPD who were receiving different modes of care was compared. This was done to ascertain whether the level of experienced personal and team continuity of patients with COPD changes after the introduction of a self-management intervention or regular monitoring by a practice nurse, compared with usual GP care at the patient's own initiative. It was hypothesised that experienced personal and team continuity would decrease when receiving self-management or regular monitoring, compared with usual care, because patients contact an additional care provider and more care providers have to communicate and collaborate. The relationship between experienced continuity of care and quality of life was also examined.
METHOD
Design
In The Netherlands, patients with COPD are primarily treated in primary care. GPs act as gatekeepers to secondary care. This study was embedded in a 24-month, multicentre, single-blinded, parallel-group randomised controlled trial comparing three care modes for patients with COPD in primary care. The study is powered on the primary study outcome, which was quality of life. This article focuses on continuity of care as the outcome measure. The randomised controlled trial has been registered in the international clinical trial register, ClinicalTrial.gov (Identifier NCT00128765).
Participants
Between June 2004 and November 2006 15 general practices from the Nijmegen region (10 general practices of the academic network of the Department of Primary and Community Care of the Radboud University Nijmegen Medical Centre and five additional general practices from the Nijmegen/Achterhoek region) selected patients aged ≥35 years, who were considered to have COPD, based on recorded International Classification of Primary Care codes R95/R91, diagnostic labels, and prescription records for respiratory medication (Anatomical Therapeutic Chemical code R03). GPs excluded patients who:
had severe comorbid conditions with a reduced life expectancy;
were unable to communicate in Dutch;
obtained care by a lung specialist at baseline; or
should, according to the GP, not be included in the study for other reasons.
How this fits in
There are concerns that the introduction of a practice nurse or a self-management programme for patients with chronic obstructive pulmonary disease (COPD) may be a threat to patients’ experienced continuity of care. However, when introducing these new care modes, patients are more likely to be reviewed frequently, which is advised in several guidelines. Moreover, patients still experience their care to be smooth, ongoing and connected. Overall, this study found no evidence that the newly introduced care modes have a negative impact on patients with COPD.
GPs invited selected patients to their general practice for an intake visit. During this visit pre- and post-bronchodilator lung function was measured. All patients who fulfilled the following inclusion criteria were asked to participate in the study:
post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC)<0.7, according to the Global initiative for chronic Obstructive Lung Disease (GOLD) criteria — COPD is diagnosed below this threshold;12 and
post-bronchodilator FEV1≥30% predicted.
Patients were excluded if they had objections to more than one of the disease management modes in the study.
Before the start of the study all patients received usual GP care. After signed, informed consent was given, patients were allocated to one of the three study arms using a computer-generated, two-block randomisation procedure with stratification on COPD severity according to GOLD classification (mild or moderate versus severe), smoking status (current versus former smoker), and exacerbation frequency in the previous 24 months (<2 versus ≥2 exacerbations). All investigators were blinded for individual treatment allocation.
Interventions
Usual care
Patients received care at their own initiative, provided by their GP. Most patients visited their GP only when symptoms were aggravated.
Self-management as an adjunct to usual care
A Dutch translation of the Canadian COPD-specific self-management programme Living Well with COPD was provided to all patients in this group.13 The programme consisted of the following topics: COPD disease knowledge; use of medication and breathing techniques; managing exacerbations; maintaining a healthy lifestyle; managing stress and anxiety; and home exercise. Using motivational interviewing techniques, the practice nurses of each practice gave the programme to patients in four individual sessions of 60 minutes each. During the 2-year follow-up, the practice nurses followed up with the patients with telephone calls to reinforce the intended behaviour changes. In case of an exacerbation, patients contacted their GP.
Regular monitoring as an adjunct to usual care
Patients were invited to participate in structured controls by the practice nurse and the GP. The frequency of these provider-initiated visits (minimum twice a year, maximum four times a year, of which one was a GP visit) depended on the severity of both airflow obstruction and dyspnoea. The content of the monitoring programme was based on national and international COPD guidelines14,15 and included spirometry, inhalation instructions, and assessment of dyspnoea and quality of life. In case of an exacerbation, patients contacted their GP.
Outcome and measurements
All patients visited the lung-function department of the Radboud University Nijmegen Medical Centre at baseline, 1 year, and 2 years for spirometry and an assessment of demographic characteristics, smoking history, and continuity of care.
Continuity of care
Continuity of care was defined as a three-dimensional concept including personal continuity from the same care provider, team continuity from the primary care team, and cross-boundary continuity across primary–secondary care settings.16 Cross-boundary continuity was not measured as patients were excluded when treated by a lung specialist.
Personal continuity was measured using the Usual Provider of Continuity (UPC) index,18 which measures the proportion of visits with the usual care provider, that is the GP. The UPC index was calculated for each patient as:
The score of the UPC index varies between 0 (low personal continuity) and 1 (high personal continuity). A patient questionnaire was used at 1 year and 2 years after baseline to obtain the number of visits during the last year that were used to calculate the UPC index.
Team continuity was then measured using a questionnaire including the following six items on team continuity:
the treatment of my lung disease in primary care goes smoothly;
the care of the different providers in primary care for my lung disease is connected;
the care providers in primary care often give me contradictory advice about my lung disease;
the care providers in primary care involved in the care for my lung disease communicate well with each other;
the care providers in primary care involved in the care for my lung disease have knowledge of my medical record; and
the care providers in primary care involved in the care for my lung disease have knowledge of previous visits.
This questionnaire, based on 30 patient interviews that were conducted as part of a study on continuity of care,19 was tested among six GPs/senior researchers and eight patients (content validity) to make sure that no significant items were missing and that all items were understood correctly. After this testing was done, minor changes to the questionnaire were made. Responses were to be recorded on a five-point scale (1 = never, 5 = always). The questionnaire was tested on a sample of Dutch patients with COPD, heart failure, or a mental illness; principal factor analysis was subsequently performed, which confirmed this presumed factor (construct validity).
Quality of life
Disease-specific health-related quality of life was measured with the self-administered Chronic Respiratory Questionnaire (CRQ).20 This instrument consists of 20 questions that are scored on a seven-point Likert-scale. The minimal clinically important difference of the CRQ has been established at 0.5 points.21 The CRQ was assessed at baseline, 6 months, 12 months, 18 months, and 24 months.
Analysis
Patient and disease characteristics were calculated and compared between the three groups using analysis of variance and χ2 tests; a P-value of <0.05 determined statistical significance. The UPC index was calculated over the total 2 years of the study; however, if data on the second year were missing the UPC index over the first year was calculated.
The answers on the items measuring team continuity at baseline were described, then the total score of team continuity in the three care modes at baseline, after 1 year, and after 2 years calculated and compared. If ≥3 or more questions on team continuity were missing from a case, that case was excluded. All remaining missing values were imputed by patient's mean. The answers on the negatively keyed question were recoded.
A general linear model was used to compare the UPC index between the three care modes and to assess the difference in team continuity score between baseline and 1 year, and between baseline and 2 years between the three care modes. In this model, care mode was included and controlled for age, sex, GOLD stage, and existence of comorbidity (cancer, heart failure, and anxiety and/or depression).
The relationship between continuity of care and quality of life was analysed; the difference between CRQ score (ΔCRQ) at baseline and in the second trial year (mean score measured at 18 and 24 months) was calculated. Differences in ΔCRQ in different levels of personal and team continuity were examined, and the Pearson's correlation coefficient (r) of ΔCRQ and personal and team continuity were calculated.
Data including and excluding patients who reported that they did not see any care provider in primary care in the last year were analysed. As the results of these two analyses did not differ, this article presents the analyses including these patients’ data. SPSS (version 16.0) was used for all statistical analyses.
RESULTS
Patient selection
A sample of 180 patients was randomly assigned to the three care modes (Figure 1). After 2 years, 148 patients had completed the study. The overall drop-out rate was 18%; reasons for drop-out were consent withdrawal, miscellaneous medical conditions, and loss to follow-up, and were comparable between the three study groups. Patients who dropped out did not statistically significantly differ in age (P = 0.94), sex (P = 0.91), post-bronchodilator FEV1 (P = 0.295), or CRQ score (P = 0.06) from patients who did not drop out.
Figure 1.
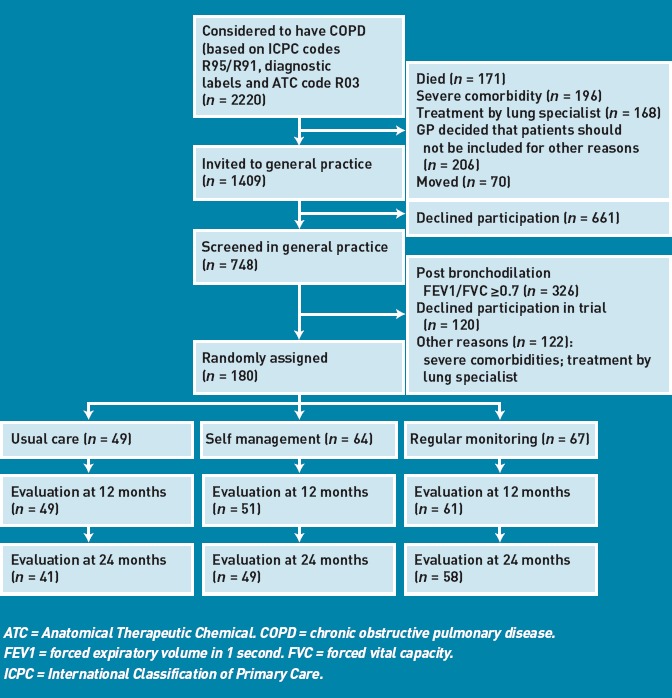
Study flow diagram.
Patient characteristics
At baseline, patients’ mean age was 64.5 years and 63% were male. In total, 18% of patients were classified as being in GOLD stage I, 64% in GOLD stage II, and 18% in GOLD stage III or IV. A breakdown of patient characteristics by care mode is given in Table 1.
Table 1.
Patient characteristics at baseline
| Usual care (n = 49) | Self-management (n = 64) | Regular monitoring (n = 67) | P-value | |
|---|---|---|---|---|
| Age in years, mean (SD) | 63.5 (± 10.3) | 64.3 (± 11.2) | 65.3 (± 9.3) | 0.65 |
| Male sex, n (%) | 25 (51.0) | 42 (65.6) | 47 (70.1) | 0.10 |
| GOLD stage, n (%) | 0.32 | |||
| GOLD I | 11 (22.4) | 13 (20.3) | 8 (11.9) | |
| GOLD II | 29 (59.2) | 42 (65.6) | 45 (67.2) | |
| GOLD III/IV | 9 (18.4) | 9 (14.1) | 14 (20.9) | |
| Lung function, mean (SD)a | ||||
| FEV1 % predicted | 67.0 (± 18.0) | 65.8 (± 16.3) | 62.6 (± 15.3) | 0.32 |
| FEV1 (L) | 1.96 (± 0.68) | 1.98 (± 0.61) | 1.94 (± 0.62) | 0.94 |
| FEV1/FVC | 0.57 (± 0.12) | 0.58 (± 0.10) | 0.56 (± 0.12) | 0.74 |
| Smoking status, n (%) | 0.47 | |||
| Smoker | 14 (30.4) (n = 46) | 22 (37.3) (n = 59) | 19 (30.6) (n = 62) | |
| Former smoker | 26 (56.5) (n = 46) | 28 (47.5) (n = 59) | 37 (59.7) (n = 62) | |
| GP-diagnosed exacerbations in previous 24 months, mean (SD) | 0.8 (± 1.1) | 1.5 (± 2.0) | 1.0 (± 1.2) | 0.08 |
| Pulmonary medication, n (%) | ||||
| No medication | 19 (38.8) | 12 (18.8) | 18 (26.9) | 0.06 |
| Long-acting bronchodilators | 25 (51.0) | 35 (54.7) | 39 (58.2) | 0.80 |
| Inhaled corticosteroids | 19 (38.8) | 41 (64.1) | 34 (50.7) | 0.04 |
Post-bronchodilator measurements. FEV1 = forced expiratory volume in 1 second. FVC = forced vital capacity. GOLD = Global initiative for chronic Obstructive Lung Disease. SD = standard deviation. Denominators vary owing to missing values
Personal continuity
Of 24 (17%) patients, data on the second trial year were missing, so the UPC index of these patients was calculated over the first year. Data on both the first and second trial year were missing of 24 patients. Table 2 shows the estimated marginal means (controlled for age, sex, GOLD stage, and existence of comorbidity) of the UPC score during the trial in the different study groups. Personal continuity was significantly higher for patients receiving usual care compared with patients in the other care modes: the mean UPC score was 0.74 for patients receiving usual care, compared with 0.50 for those receiving regular monitoring and 0.36 for patients who were self-managing. The UPC index was >0.80 in 44% of the patients in the usual care group, compared with 23% of those receiving regular monitoring and 6% of those self-managing.
Table 2.
Mean score of personal continuity and difference in team continuity in the different study groups
| Intervention group | Mean UPC index during trial4 (95% CI) | Mean difference in team continuity between baseline and 1 yeara (95% CI) | Mean difference in team continuity between baseline and 2 yearsa (95%CI) |
|---|---|---|---|
| Usual careb | 0.74 (0.61 to 0.86) | 0.31 (–1.14 to 1.76) | –0.05 (–1.84 to 1.74) |
| Self management | 0.36 (0.25 to 0.47) (P = 0.00) | 0.02 (–0.37 to 2.20) (P = 0.500) | –0.21 (–1.66 to 1.25) (P = 0.883) |
| Regular monitoring | 0.50 (0.39 to 0.61) (P = 0.02) | 0.87 (–0.45 to 2.19) (P = 0.528) | 0.12 (–1.43 to 1.68) (P = 0.873) |
Estimated marginal mean controlled for age, sex, GOLD-stage, and existence comorbidity.
Reference group. GOLD = Global initiative for chronic Obstructive Lung Disease. UPC = Usual Provider of Continuity (range: 0–1; team continuity range: 6–30).
In the usual care group, 13/45 (29%) patients did not contact any care provider at all for their COPD during the study (UPC index was missing), compared with one (2%) patient who was self-managing, and 3/60 (5%) patients who received regular monitoring.
Team continuity
At baseline, most patients scored high on the items measuring team continuity (Table 3). No great differences were seen in the team continuity scores at baseline among the three care modes (P = 0.693) and, after 1 and 2 years, no clear differences in the score of team continuity were seen at group level (Table 4). Most patients showed no or only small differences (0–2 points) in experienced team continuity after 1 year; these differences seemed to become even smaller after 2 years. Patients in the usual care group show the smallest difference in team continuity (data not shown).
Table 3.
Experienced team continuity in primary care at baseline (n = 162)
| Questionnaire item | Never, n (%) | Seldom, n (%) | Sometimes, n (%) | Often, n (%) | Always, n (%) |
|---|---|---|---|---|---|
| The treatment of my lung disease in primary care goes smoothly | 2 (1.2) | 3 (1.9) | 7 (4.3) | 33 (20.4) | 117 (72.2) |
| The care of the different care providers in primary care for my lung disease is connected | 5 (3.1) | 1 (0.6) | 15 (9.3) | 44 (27.2) | 97 (59.9) |
| The care providers in primary care often give me contradictory advice about my lung disease | 132 (81.5) | 22 (13.6) | 3 (1.9) | 3 (1.9) | 2 (1.2) |
| The care providers in primary care involved in the care for my lung disease communicate well with each other | 4 (2.5) | 9 (5.6) | 7 (4.3) | 54 (33.3) | 88 (54.3) |
| The care providers in primary care involved in the care for my lung disease have knowledge of my medical record | 4 (2.5) | 5 (3.1) | 18 (11.1) | 46 (28.4) | 89 (54.9) |
| The care providers in primary care involved in the care for my lung disease have knowledge of previous visits | 5 (3.1) | 6 (3.7) | 10 (6.2) | 50 (30.9) | 91 (56.2) |
Table 4.
Total score of experienced team continuity in general practice in the three care modes at baseline, after 1 year, and after 2 years
| Score of team continuity by care modea | Baseline, % | After 1 year, % | After 2 years, % |
|---|---|---|---|
| Usual care | n = 40 | n = 30 | n = 27 |
| 30 | 30 | 30 | 30 |
| 24–29 | 53 | 57 | 48 |
| 18–23 | 10 | 10 | 15 |
| 12–17 | 5 | 0 | 4 |
| 6–11 | 3 | 3 | 4 |
| Self-management | n = 59 | n = 45 | n = 43 |
| 30 | 31 | 38 | 33 |
| 24–29 | 58 | 49 | 54 |
| 18–23 | 9 | 13 | 9 |
| 12–17 | 3 | 0 | 5 |
| 6–11 | 0 | 0 | 0 |
| Regular monitoring | n = 63 | n = 52 | n = 41 |
| 30 | 35 | 35 | 29 |
| 24–29 | 44 | 56 | 46 |
| 18–23 | 16 | 8 | 24 |
| 12–17 | 2 | 2 | 0 |
| 6–11 | 3 | 0 | 0 |
Total score of team continuity range: 6–30.
Continuity and quality of life
Table 5 shows the relationship between continuity of care and changes in quality of life. No clinically relevant difference in CRQ score (>0.50) was seen for different UPC scores. Pearson's correlation coefficient of ΔCRQ and personal continuity was 0.117. A slightly higher quality of life was found after 2 years when the UPC score exceeded 0.60, however this difference was not clinically relevant. The experienced quality of life did not change for patients who saw no care provider at all during the trial; in addition no clinically relevant difference was found between different levels of team continuity and quality of life. Pearson's correlation coefficient of ΔCRQ and team continuity was –0.041.
Table 5.
Changes in CRQ score between baseline and the second trial year in different continuity classes
| Personal continuity: UPC index | ΔCRQa | SD | n |
|---|---|---|---|
| 0.00–0.20 | 0.06 | ± 0.51 | 31 |
| 0.21–0.40 | 0.01 | ± 0.51 | 27 |
| 0.41–0.60 | 0.04 | ± 0.61 | 27 |
| 0.61–0.80 | 0.28 | ± 0.48 | 23 |
| 0.81–1.00 | 0.16 | ± 0.59 | 28 |
| No care provider at all during trial | –0.01 | ± 0.59 | 16 |
| Team continuity: difference between baseline and 2 years | |||
| ≤–2 | –0.01 | ± 0.52 | 20 |
| −1.99 to 1.99 | 0.09 | ± 0.43 | 53 |
| ≥2 | 0.19 | ± 0.59 | 29 |
Difference in CRQ score between baseline and the second trial year. CRQ = Chronic Respiratory Questionnaire. SD = standard deviation. UPC = Usual Provider of Continuity.
DISCUSSION
Summary
Although personal continuity — that is, the proportion of visits with patient's own GP — was found to be highest when receiving usual care and lowest when self-managing (which would be expected from the organisation of the care modes), in contrast to this study's hypothesis, no differences in experienced team continuity in primary care among the three care modes were found. Patients in all three care modes, independent of the number of care providers seen, felt that their care went smoothly, was connected, and that care providers communicated well and knew them.
Although the proportion of visits with the patient's own GP was highest when receiving usual care, it was found that the chance of not contacting any care provider at all was also highest in this care mode (almost 30%). There was no evidence that a decreasing (personal) continuity affects patients’ quality of life.
Strengths and limitations
One limitation to be aware of is that the study is powered on the quality-of-life outcome measure and not on continuity of care. It could be that too few patients were included to find differences in experienced team continuity.
Another limitation is the high level of experienced team continuity at baseline, which makes it difficult to show an increase in team continuity during the study. However, as it was hypothesised that the experienced continuity would decrease when patients were self-managing or receiving regular monitoring because they need to contact an additional care provider in these care modes, it is not thought that this limitation negatively influenced these results.
A considerable number of patients saw no care provider at all for their COPD during the trial, especially in the group of patients receiving usual care. Some of these, however, did answer the questions about team continuity, which can make the reliability of the answers doubtful. Data including and excluding patients who reported that they did see any care provider for their COPD were analysed; the results of these two analyses did not differ.
Many patients thought to have COPD did not participate in the trial, which could lower the generalisability of the results. However, the age, sex, and severity of COPD (according to the GOLD stage) of those patients who were included are comparable with the same characteristics of primary care patients with COPD who have participated in other studies.22,23 To the authors’ knowledge, this is the first study analysing changes in experienced personal and team continuity after the introduction of new care modes.
Comparison with existing literature
The relationship between continuity of care and quality of life has been investigated in previous studies. Chien et al9 also found no relationship between the UPC index and quality of life, but Hanninen et al10 found a positive correlation between seeing the same GP for at least 2 years and quality of life in patients with diabetes. Adair et al8 and King et al11 investigated the relationship between a multidimensional definition of continuity of care and quality of life: King et al performed a cross-sectional study in patients with cancer and found no relationship, whereas Adair et al performed a prospective study in patients with severe mental illness and found a positive relationship between continuity and quality of life.
Implications for practice
Regular monitoring by a practice nurse and self-management are increasingly introduced in primary care to anticipate the growing load of this chronic disease in primary care. As patients contact an additional care provider (practice nurse) in these new care modes, they experience less personal continuity. However, as guidelines advise the review of patients with COPD regularly to provide high levels of quality of care,14,15 these new care modes reduce the chance of not being reviewed at all. Although patients contact an additional care provider, they still experience that their care goes smoothly, is connected, and that care providers communicate well and know their patients. Overall, no evidence was found that the newly introduced care modes have a negative impact on patients with COPD.
Funding
None.
Ethical approval
Medical Ethics Committee of the Radboud University Nijmegen Medical Centre.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765–773. doi: 10.1016/S0140-6736(07)61380-4. [DOI] [PubMed] [Google Scholar]
- 2.Rabe KF, Beghe B, Luppi F, Fabbri LM. Update in chronic obstructive pulmonary disease 2006. Am J Respir Crit Care Med. 2007;175(12):1222–1232. doi: 10.1164/rccm.200704-586UP. [DOI] [PubMed] [Google Scholar]
- 3.Heller KS, Solomon MZ. Continuity of care and caring: what matters to parents of children with life-threatening conditions. J Pediatr Nurs. 2005;20(5):335–346. doi: 10.1016/j.pedn.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Schers H, van den Hoogen H, Bor H, et al. Familiarity with a GP and patients’ evaluations of care. A cross-sectional study. Fam Pract. 2005;22(1):15–19. doi: 10.1093/fampra/cmh721. [DOI] [PubMed] [Google Scholar]
- 5.Hjortdahl P, Laerum E. Continuity of care in general practice: effect on patient satisfaction. BMJ. 1992;304(6837):1287–1290. doi: 10.1136/bmj.304.6837.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Saultz JW, Albedaiwi W. Interpersonal continuity of care and patient satisfaction: a critical review. Ann Fam Med. 2004;2(5):445–451. doi: 10.1370/afm.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gray DP, Evans P, Sweeney K, et al. Towards a theory of continuity of care. J R Soc Med. 2003;96(4):160–166. doi: 10.1258/jrsm.96.4.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adair CE, McDougall GM, Mitton CR, et al. Continuity of care and health outcomes among persons with severe mental illness. Psychiatr Serv. 2005;56(9):1061–1069. doi: 10.1176/appi.ps.56.9.1061. [DOI] [PubMed] [Google Scholar]
- 9.Chien CF, Steinwachs DM, Lehman A, et al. Provider continuity and outcomes of care for persons with schizophrenia. Ment Health Serv Res. 2000;2(4):201–211. [Google Scholar]
- 10.Hanninen J, Takala J, Keinanen-Kiukaanniemi S. Good continuity of care may improve quality of life in type 2 diabetes. Diabetes Res Clin Pract. 2001;51(1):21–27. doi: 10.1016/s0168-8227(00)00198-4. [DOI] [PubMed] [Google Scholar]
- 11.King M, Jones L, Richardson A, et al. The relationship between patients’ experiences of continuity of cancer care and health outcomes: a mixed methods study. Br J Cancer. 2008;98(3):529–536. doi: 10.1038/sj.bjc.6604164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (updated 2010) http://www.goldcopd.org/uploads/users/files/GOLDReport_April112011.pdf (accessed 4 Apr 2012)
- 13.Bourbeau J, Julien M, Maltais F, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Arch Intern Med. 2003;163(5):585–591. doi: 10.1001/archinte.163.5.585. [DOI] [PubMed] [Google Scholar]
- 14.National Collaborating Centre for Chronic Conditions. Chronic obstructive pulmonary disease. National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. Thorax. 2004;59(Suppl 1):1–232. [PMC free article] [PubMed] [Google Scholar]
- 15.Smeele IJM, van Weel C, van Schayck CP, et al. NHG standaard COPD (Tweede herziening) Huisarts Wet. 2007;8:362–379. [Google Scholar]
- 16.Freeman G, Hughes J. Continuity of care and the patient experience. An inquiry into the quality of general practice in England. London: The King's Fund; 2010. [Google Scholar]
- 17.Uijen AA, Schers HJ, Schellevis FG, van den Bosch WJ. How unique is continuity of care? A review of continuity and related concepts. Fam Pract. 2011 doi: 10.1093/fampra/cmr104. doi: 10.1093/fampra/cmr104. [DOI] [PubMed] [Google Scholar]
- 18.Jee SH, Cabana MD. Indices for continuity of care: a systematic review of the literature. Med Care Res Rev. 2006;63(2):158–188. doi: 10.1177/1077558705285294. [DOI] [PubMed] [Google Scholar]
- 19.Schers HJ. Continuity of care in general practice. Exploring the balance between personal and informational continuity. Nijmegen: Radboud Universiteit; 2004. [Google Scholar]
- 20.Schunemann HJ, Goldstein R, Mador MJ, et al. A randomised trial to evaluate the self-administered standardised chronic respiratory questionnaire. Eur Respir J. 2005;25(1):31–40. doi: 10.1183/09031936.04.00029704. [DOI] [PubMed] [Google Scholar]
- 21.Schunemann HJ, Puhan M, Goldstein R, et al. Measurement properties and interpretability of the chronic respiratory disease questionnaire (CRQ) COPD. 2005;2(1):81–89. doi: 10.1081/copd-200050651. [DOI] [PubMed] [Google Scholar]
- 22.Bourbeau J, Sebaldt RJ, Day A, et al. Practice patterns in the management of chronic obstructive pulmonary disease in primary practice: the CAGE study. Can Respir J. 2008;15(1):13–19. doi: 10.1155/2008/173904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Afonso AS, Verhamme KM, Sturkenboom MC, Brusselle GG. COPD in the general population: prevalence, incidence and survival. Respir Med. 2011;105(12):1872–1884. doi: 10.1016/j.rmed.2011.06.012. [DOI] [PubMed] [Google Scholar]


