Abstract
Rationale: The National Quality Forum recently endorsed in-hospital mortality and intensive care unit length of stay (LOS) as quality indicators for patients in the intensive care unit. These measures may be affected by transferring patients to long-term acute care hospitals (LTACs).
Objectives: To quantify the implications of LTAC transfer practices on variation in mortality index and LOS index for patients in academic medical centers.
Methods: We used a cross-sectional study design using data reported to the University HealthSystem Consortium from 2008–2009. Data were from patients who were mechanically ventilated for more than 96 hours.
Measurements and Main Results: Using linear regression, we measured the association between mortality index and LTAC transfer rate, with the hospital as the unit of analysis. Similar analyses were conducted for LOS index and cost index. A total of 137 hospitals were analyzed, averaging 534 transfers to LTAC per hospital during the study period. Mean ± SD in-hospital mortality was 24 ± 6.4%, and observed LOS was 30.4 ± 8.2 days. The mean LTAC transfer rate was 15.7 ± 13.7%. Linear regression demonstrated a significant correlation between transfer rate and mortality index (R2 = 0.14; P < 0.0001) and LOS index (R2 = 0.43; P < 0.0001).
Conclusions: LTAC hospital transfer rate has a significant impact on reported mortality and LOS indices for patients requiring prolonged acute mechanical ventilation. This is an example of factors unrelated to quality of medical care or illness severity that must be considered when interpreting mortality and LOS as quality indicators.
Keywords: National Quality Forum, American Thoracic Society, quality improvement
At a Glance Commentary
Scientific Knowledge on the Subject
Rising health care costs, increased demand for quality health care, and emphasis on pay-for-performance measures have led to the creation of benchmarks to measure quality. In-hospital mortality and length of stay have recently been endorsed as publicly reported quality measures for care of patients in the intensive care unit. However, these measures may be influenced by factors unrelated to medical care or illness severity.
What This Study Adds to the Field
This study suggests that transfer of ventilated patients to long-term acute care hospitals significantly impacts variations between hospitals in measures of mortality and length of stay.
Rising health care costs, increased demand for quality health care, and emphasis on pay-for-performance measures have led to the creation of benchmarks to measure quality. Recently, the National Quality Forum (NQF) endorsed the measures of in-hospital mortality rates and intensive care unit (ICU) length of stay (LOS) as quality indicators for patients receiving care in acute hospital ICUs (1). These measures have been questioned by several professional organizations, such as the American Thoracic Society, the American College of Chest Physicians, and the American Association of Critical Care Nurses, because they may be subject to bias from individual hospital characteristics unrelated to medical practice (2). One example is variation in transfer patterns to long-term acute care (LTACs) hospitals.
Since the 1980s, LTACs have provided care to patients with prolonged acute care needs, such as weaning from mechanical ventilation, prolonged intravenous antibiotics, or complex wound care (3). Throughout the United States, LTAC transfer rates vary considerably among large hospitals (4). Although this is partly explained by heterogeneous LTAC distribution, LTAC transfer rates frequently differ greatly among hospitals in the same region.
Previous studies using modeled data suggest that standardized mortality ratios can be improved by increasing transfer of ICU patients directly to other acute hospitals (5, 6). Mechanically ventilated patients transferred to LTACs have a mean LOS at the LTAC of 25 days and 69% mortality at 1 year (7). For patients transferred to LTAC, referring hospitals have 0% documented mortality for the patients’ hospitalization regardless of risk of death during the full episode of acute care, and they are credited with none of the additional days of acute care. It is not known how much of a real impact this has on reported quality indicators. The objective of this study was to measure the impact of LTAC transfer rate on reported quality indicators for patients requiring prolonged mechanical ventilation. We hypothesize that the mortality index (observed or expected mortality) and LOS index (observed or expected LOS) reported to hospitals in the University HealthSystem Consortium (UHC) are significantly affected by LTAC transfer rates for patients in the “ventilator support product line.” Some of the results of this study have been previously reported in the form of an abstract (8).
Methods
The study used a cross-sectional study with analysis of an existing database. Hospitals reporting to the UHC's Clinical Database–Resource Manager (CDB-RM) were the unit of analysis. The UHC is an alliance of approximately 90% of the academic and affiliated nonprofit hospitals in the United States (http://www.uhc.edu). The CDB-RM is a patient-level on-line interactive, transparent resource used by database participants for performance improvement. The database is populated by participating hospitals’ reporting outcome and resource information on all hospital discharges. Ratios of observed to expected outcome (mortality, LOS, and cost indices) facilitate interpretation of performance as favorable or unfavorable. Calculation of expected values is performed using UHC risk adjustment models generated by multiple regression on a range of variables including patient demographics, diagnosis and procedure codes, and admission source. Patients who are transferred to acute care hospitals other than LTACs are excluded from data used for UHC mortality risk adjustment model development. Patients who are transferred to another acute hospital within 2 days of admission are excluded from LOS and cost prediction models. However, when hospital-specific mortality and LOS are reported for the ventilator support product line, patients who are transferred to acute care hospitals including LTACs are included in those analyses and incorporated into the comparisons of outcomes. The study included patients discharged during calendar years 2008–2009. The patients were mapped to the UHC CDB-RM's ventilator support product line, which includes patients who received mechanical ventilation for greater than 96 hours at the institution. Hospitals with less than 100 beds were excluded. Hospitals were also excluded if less than eight quarters of data were available or if qualifying information was not reported to the UHC during the study period.
Variables and Measurements
Linear regression was used for the analysis. The primary outcomes were hospital mortality index and LOS index reported by the UHC for each hospital. The primary independent variable was hospital LTAC transfer rate. Hospital costs were measured as a secondary dependent variable. Descriptive variables for the hospitals and descriptive variables for patients who were transferred to LTACs were also recorded.
Analysis
Descriptive data are expressed as mean ± SD for continuous variables or as proportions for categorical variables. Simple regression was used to measure the association between continuous variables, including between mortality index and LOS index and LTAC transfer rate. To measure the relative contributions of illness severity and LTAC transfer rates on observed mortality and LOS, multiple linear regression was performed with mortality or LOS as the dependent variable and LTAC transfer rate and expected mortality or expected LOS as the independent variables. In a secondary analysis we created a similar model with hospital costs as the outcome variable and LTAC transfer rate and expected cost as dependent variables. Five extreme outlier hospitals were excluded from the analysis, as recommended by Porter (9), to prevent an individual atypical hospital with data well outside the normal (greater than 3 SD above or below the mean in this case) from exerting disproportionate influence. The analysis was performed using Stata version 8.0 (Stata Corp, College Station, TX).
The protocol was reviewed by the University of North Carolina institutional review board, who determined that the protocol was exempt from institutional review board approval because of use of existing de-identified data. A copy of all the final manuscripts was provided to the UHC before submission to ensure compliance with UHC data reporting standards.
Results
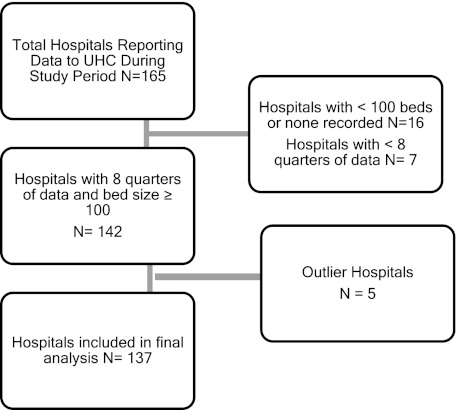
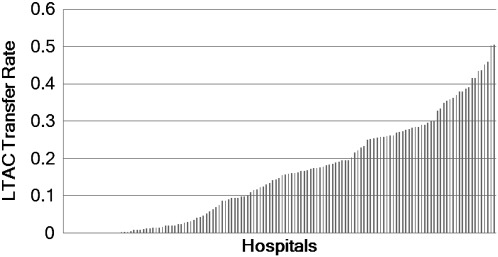
One hundred and sixty-five hospitals reported data to the UHC during the study period, and 137 hospitals were included in the final analysis (Figure 1). The mean bed size of hospitals included in the analysis was 493, averaging 534 qualifying patients during the study period (Table 1). Mean ± SD in-hospital mortality for these patients was 24 ± 6.4% and LOS was 30.4 ± 8.2 days. The LTAC transfer rate was 15.7 ± 13.7%. The mean mortality and LOS indices were 0.90 ± 0.20 and 1.12 ± 0.26, respectively. The distribution of LTAC transfer rates by hospital is listed in Figure 2, and Table 2 lists the distribution of LTAC transfers by region.
Figure 1.
Schematic of study sample with exclusions from analysis. UHC = University HealthSystem Consortium.
TABLE 1.
HOSPITAL CHARACTERISTICS (N = 137) AND QUALITY INDICATORS REPORTED FOR PATIENTS IN THE UHC VENTILATOR SUPPORT PRODUCT LINE*
| Characteristic | N |
| Number of beds per hospital | 493 ± 245 |
| Ventilator support product line patients per hospital | 534 ± 345 |
| In-hospital mortality rate, % | 24 ± 6.4 |
| Hospital LOS, d | 30.4 ± 8.2 |
| Mean LTAC transfer rate, % | 15.7 ± 13.7 |
| Mortality index | 0.90 ± 0.20 |
| LOS index | 1.12 ± 0.26 |
Definition of abbreviations: LOS = length of stay; LTAC = long-term acute care; UHC = University HealthSystem Consortium.
Values expressed as mean ± SD.
Patients receiving greater than 96 hours of mechanical ventilation.
Figure 2.
Distribution of long-term acute care (LTAC) transfer rate by hospital.
TABLE 2.
CHARACTERISTICS OF HOSPITALS AND QUALITY INDICATOR OUTCOMES BY REGION
| Region | Number of Hospitals | Number of Beds | Number of Product Line Cases | LTAC Transfer Rate | Mortality Index | LOS Index |
| Western | 18 | 487 ± 171 | 449 ± 184 | 5.2 ± 6.2 | 0.93 ± 0.21 | 1.32 ± 0.19 |
| Mid-Atlantic | 29 | 568 ± 210 | 592 ± 330 | 8.9 ± 10.7 | 0.98 ± 0.19 | 1.28 ± 0.24 |
| Southeastern | 21 | 571 ± 208 | 786 ± 369 | 16.2 ± 10.5 | 0.96 ± 0.21 | 1.13 ± 0.20 |
| New England | 22 | 331 ± 214 | 303 ± 299 | 16.6 ± 14.7 | 0.87 ± 0.16 | 1.01 ± 0.24 |
| Midwestern | 30 | 456 ± 265 | 487 ± 320 | 22.2 ± 14 | 0.80 ± 0.19 | 0.97 ± 0.26 |
| Mid-Continent | 17 | 551 ± 315 | 598 ± 366 | 25.3 ± 14.1 | 0.84 ± 0.19 | 1.06 ± 0.19 |
Definition of abbreviations: LOS = length of stay; LTAC = long-term acute care.
Values expressed as mean ± SD.
Table 3 lists the characteristics of patients transferred to LTACs. The mean age was 62.7 ± 8.4 and 6,185 (54.9%) were female.
TABLE 3.
CHARACTERISTICS OF PATIENTS TRANSFERRED TO LTACS (N = 11,276)
| Age | 62.7 ± 8.4 |
| Female | 6,185 (54.9) |
| Race | |
| Unknown | 233 (2.1) |
| White | 7,464 (66.1) |
| Black | 2,368 (21) |
| Hispanic | 412 (3.7) |
| Native American/Eskimo | 58 (0.5) |
| Asian | 164 (1.5) |
| Other | 575 (5.1) |
| Hawaiian/Pacific Islander | 2 (<0.1) |
| Number of comorbidities | 5 ± 2.3 |
| Number of complications | 1.1 ± 1.2 |
| Total cost of hospital stay | $124,782 ± 69,074 |
| Expected costs | $112,760 ± 18,396 |
| Readmissions within 30 d | 1,548 (13.8) |
| LOS for readmissions | 34 ± 12.3 |
| Hospital cost for readmissions | $141,391 |
Definition of abbreviations: LOS = length of stay; LTAC = long-term acute care.
Values expressed as mean ± SD or n (%)
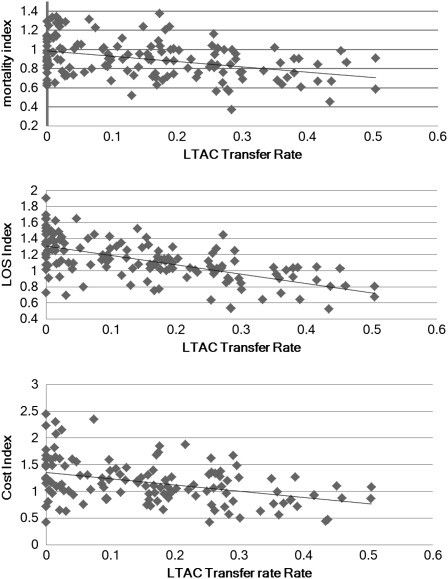
Multivariate regression analysis results are listed in Table 4. LTAC transfer rate is a significant predictor of in-hospital mortality, and it has a significant impact on the hospital mortality index (R2 = 0.14; P < 0.0001). LTAC transfer rate is also a significant predictor of observed LOS, and it has significant impact on hospital LOS index (R2 = 0.37; P < 0.0001). Additionally, LTAC transfer rate significantly impacts hospital cost index (R2 = 0.13; P < 0.0001). Similar analyses were performed with outliers included, and results were not significantly affected (R2 = 0.11, P < 0.0001 for mortality index; R2 = 0.36, P < 0.0001 for LOS index; and R2 = 0.13, P < 0.0001 for cost index). Figure 3 is a scatter plot representing the relationship between LTAC transfer rate and LOS, mortality, and cost indices.
TABLE 4.
ASSOCIATION OF QUALITY INDICES AND LTAC TRANSFER RATES
| Outcome | Variable | Coefficient | P Value | R2 |
| Mortality rate | LTAC transfer rate | −15.3 (−21.4, −9.3) | <0.0001 | 0.43 |
| Expected mortality | 0.86 (0.67, 1.04) | <0.0001 | ||
| Intercept | 3.4 | |||
| Mortality index | LTAC transfer rate | −0.57 (−0.77, −0.31) | <0.0001 | 0.14 |
| Intercept | 0.98 | |||
| LOS | LTAC transfer rate | −30 (−36.1, 23.2) | <0.0001 | 0.60 |
| Expected LOS | 1.4 (1.2, 1.7) | <0.0001 | ||
| Intercept | −3.8 | |||
| LOS index | LTAC transfer rate | −1.14 (−1.4, 0.89) | <0.0001 | 0.37 |
| Intercept | 1.3 | |||
| Cost | LTAC transfer rate | −104,638 (−150,701, 58,576) | <0.0001 | 0.39 |
| Expected cost | 1.6 (1.2, 2) | |||
| Intercept | 23,679 | |||
| Cost index | LTAC transfer rate | −1.12 (−1.6, −0.6) | <0.0001 | 0.13 |
| Intercept | 1.3 |
Definition of abbreviations: LOS = length of stay; LTAC = long-term acute care.
Figure 3.
Linear regression of long-term acute care (LTAC) transfer rate and mortality index, length of stay (LOS) index, and cost index.
Discussion
Our data indicate that LTAC transfer rate explains 14% of the variation in hospital mortality index and 37% of variation in LOS index for patients requiring more than 96 hours of mechanical ventilation, an important and resource-intensive patient group. Based on these data, increasing an LTAC transfer rate from the 25th percentile (2%) to the 75th percentile (26%) would improve a hospital's mortality index from 0.97 to 0.83 and LOS index from 1.28 to 1.00. This suggests that data from patients who are transferred to LTACs should not be included in reports of mortality and LOS used for quality comparison. Ideally, the quality of care for patients transferred to LTACs should be measured across the entire episode of illness, using data from the acute hospital and LTAC. Benchmark data for mortality and LOS can be valuable for hospitals as a screening tool to identify areas that may require performance-improvement interventions (10). However, these findings provide an important example of how mortality and LOS data should be interpreted carefully because factors that are unrelated to quality of medical care or illness severity can have a significant impact on variation between centers. This is especially relevant if data are to be reported publicly as endorsed by the NQF.
Although an intuitive measure, some maintain that mortality is a poor indicator of hospital quality because it measures all hospital deaths, when performance-improvement measures ideally address preventable deaths. Thomas and Hofer (11) determined in a metaanalysis of 18 papers that quality of care has only a small correlation with outcome measures, such as mortality. Little association has been seen between process measures and outcomes for heart attack (12), hip fracture (13), and stroke (14). Although the fraction of preventable deaths in any given hospital is debatable, Brennan and coworkers (15) demonstrated that only 0.25% of admissions result in preventable death. In a recent editorial, Lilford and Pronovost (16) suggested that, using the data of Brennan and coworkers (15), 19 out of 20 hospital deaths are unavoidable in modern hospitals.
Standardized mortality is widely considered to be more reliable as a quality indicator than observed mortality (17). However, standardized mortality ratios use complex algorithms that need constant refining to reflect changing populations and trends in care. Heterogeneous patient populations, differences in documentation, and available resources can render these algorithms imprecise and quickly obsolete. Risk-adjusted mortality ratios were shown by Pitches and coworkers (17) in a recent metaanalysis to be neither consistent nor reliable as a marker of quality care.
Our data show that increased LTAC transfers can also contribute significantly to a decreased LOS index. LOS is problematic as a quality measure. Like mortality, ICU LOS is a low-signal (hospital days accrued because of preventable causes), high-noise (unpreventable hospital days) metric. Many maintain that ICU LOS measures resource use, not quality care (18). Variations between hospitals are dependent on a number of factors, such as stepdown bed availability, payor source, family resources that could support care at home, and hospital census. Inaccuracies are common, because LOS is usually recorded in days, when ICU hours or midnight bed occupancy are more effective measurements (19). The prevalence of outlier patients can greatly affect the mean measurements, especially among small hospitals. Finally, mortality and LOS are likely collinear, as demonstrated by Jencks and coworkers (20) in a comparison of LOS and hospital mortality between New York and California for several common medical conditions.
NQF measures can be targeted by the Centers for Medicare and Medicaid Services as performance measures that are linked to financial incentives for hospitals (21). Our data suggest that expected hospital LOS and mortality for ICU patients should be adjusted for LTAC transfer rates. If the current NQF measures are adapted by the Centers for Medicare and Medicaid Services and adjustments for LTAC transfer rates are not made, then hospitals will receive further incentives to increase transfer to LTACs. For hospitals, increased transfer to LTACs is already thought to be a financially prudent decision because it likely reduces patient care costs for the hospital (22) and opens acute care beds for new patients that provide higher reimbursement (23). Our analysis confirms that LTAC transfer decreases the hospital cost index for mechanically ventilated patients. Despite these incentives to transfer patients to LTACs, there is no evidence that transfer to LTAC improves patient outcomes (24), and recent data indicate that LTAC transfer may be associated with longer LOS for the entire episode (25, 26).
In a previous study, applying a Monte Carlo simulation to a dataset of 131,618 ICU admissions, Kahn and coworkers (5) showed that increasing transfers by 2% and 6% improved standardized mortality ratios by 0.10 and 0.14, respectively. In a retrospective study using data from patients in 35 California ICUs, Vasilevskis and coworkers (6) produced models that demonstrated that varying discharge practices by 1% would affect standardized mortality ratios by 0.021. Our study advances these concepts by demonstrating the impact that a modifiable, nonmedical practice has on variation in actual reported measures that are used to indicate quality of care.
Our data also indicate that there is significant regional variation in LTAC transfer rates, related in part to geographic availability (27). Ongoing studies are evaluating the important question of why there is variation in transfer rates within regions and whether this has an impact on patient outcome.
There are some limitations of our study. Data are from nonprofit academic and affiliated nonprofit institutions, and the analysis was restricted to hospitals with more than 100 beds. Teaching hospitals are more likely to be high referrers to LTACs because of the concentration of LTACs in urban areas (27). However, most LTAC patients come from nonteaching hospitals because of their higher number. Because geographic location is likely to be the most important factor affecting LTAC transfer rate, this issue is relevant to both types of hospitals. It should also be noted that hospital reporting of LTAC transfers is not always accurate (28). The dataset consisted of patients who had received greater than or equal to 96 hours of mechanical ventilation. Nonventilated ICU patients or patients receiving shorter periods of mechanical ventilation are less likely to be referred to LTACs, so mortality and LOS indices measured for all ICU patients should be less affected by LTAC transfer rates. However, patients included in the study are part of an established subset of patients for which quality data are reported for a very large consortium of major hospitals. They are also a subset of patients with high mortality and very high resource requirement, making them an important focus of quality benchmarking. The contribution of LTAC transfer rate to variation in LOS index may be less if ICU rather than hospital outcomes are reported, as currently recommended by the NQF. However, hospital LOS is the more relevant patient outcome and is the parameter currently provided by the UHC to individual hospitals.
Conclusions
LTAC transfer practice has a significant impact on mortality and LOS indices that are reported as quality benchmarks for patients requiring prolonged acute mechanical ventilation. This is an example of a factor unrelated to medical care or illness severity that must be considered when interpreting mortality and LOS as quality indicators. This also questions the NQF endorsement of mortality and LOS as publicly reported quality indicators for ICU medical care.
Supplementary Material
Acknowledgments
The authors acknowledge Sam Hohmann, Ph.D., for his assistance in review of this manuscript.
Footnotes
Supported by the NHLBI (5T32HL007106-33).
Author Contributions: W.B.H. contributed to the design of the study, data analysis, and manuscript preparation. S.S.C. contributed to the design of the study, data analysis, and manuscript preparation. L.E.W. contributed to data analysis and manuscript preparation. S.M. provided data for analysis and assisted in manuscript review.
Originally Published in Press as DOI: 10.1164/rccm.201106-1084OC on September 22, 2011
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Aebersold A NQF endorses patient outcome measures for high-impact conditions. Washington, DC: National Quality Forum; 2010 [Google Scholar]
- 2.Peterson KGK, Schraufnagel D. Letter to the NQF Steering Committee. Washington, DC: National Quality Forum; 2010. p. 3 [Google Scholar]
- 3.Hotes LS, Kalman E. The evolution of care for the chronically critically ill patient. Clin Chest Med 2001;22:1–11 [DOI] [PubMed] [Google Scholar]
- 4.Medicare program: prospective payment system for long-term care hospitals RY 2007: annual payment rate updates, policy changes, and clarification. Final rule. Fed Regist 2006;71:27797–27939 [PubMed] [Google Scholar]
- 5.Kahn JM, Kramer AA, Rubenfeld GD. Transferring critically ill patients out of hospital improves the standardized mortality ratio: a simulation study. Chest 2007;131:68–75 [DOI] [PubMed] [Google Scholar]
- 6.Vasilevskis EE, Kuzniewicz MW, Dean ML, Clay T, Vittinghoff E, Rennie DJ, Dudley RA. Relationship between discharge practices and intensive care unit in-hospital mortality performance: evidence of a discharge bias. Med Care 2009;47:803–812 [DOI] [PubMed] [Google Scholar]
- 7.Kahn JM, Benson NM, Appleby D, Carson SS, Iwashyna TJ. Long-term acute care hospital utilization after critical illness. JAMA 2010;303:2253–2259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall WB, Willis B, Medvedev S, Carson SS. Long term acute care hospital transfer rate is independently associated with in-hospital mortality and length of stay [abstract]. Proc Am Thorac Soc 2011;8:A2370 [Google Scholar]
- 9.Porter AM. Misuse of correlation and regression in three medical journals. J R Soc Med 1999;92:123–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iezzoni LI. Assessing quality using administrative data. Ann Intern Med 1997;127:666–674 [DOI] [PubMed] [Google Scholar]
- 11.Thomas JW, Hofer TP. Research evidence on the validity of risk-adjusted mortality rate as a measure of hospital quality of care. Med Care Res Rev 1998;55:371–404 [DOI] [PubMed] [Google Scholar]
- 12.Mant J, Hicks N. Detecting differences in quality of care: the sensitivity of measures of process and outcome in treating acute myocardial infarction. BMJ 1995;311:793–796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Freeman C, Todd C, Camilleri-Ferrante C, Laxton C, Murrell P, Palmer CR, Parker M, Payne B, Rushton N. Quality improvement for patients with hip fracture: experience from a multi-site audit. Qual Saf Health Care 2002;11:239–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McNaughton H, McPherson K, Taylor W, Weatherall M. Relationship between process and outcome in stroke care. Stroke 2003;34:713–717 [DOI] [PubMed] [Google Scholar]
- 15.Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, Newhouse JP, Weiler PC, Hiatt HH. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. N Engl J Med 1991;324:370–376 [DOI] [PubMed] [Google Scholar]
- 16.Lilford R, Pronovost P. Using hospital mortality rates to judge hospital performance: a bad idea that just won't go away. BMJ 2010;340:c2016. [DOI] [PubMed] [Google Scholar]
- 17.Pitches DW, Mohammed MA, Lilford RJ. What is the empirical evidence that hospitals with higher-risk adjusted mortality rates provide poorer quality care? A systematic review of the literature. BMC Health Serv Res 2007;7:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shojania KG, Showstack J, Wachter RM. Assessing hospital quality: a review for clinicians. Eff Clin Pract 2001;4:82–90 [PubMed] [Google Scholar]
- 19.Marik PE, Hedman L. What's in a day? Determining intensive care unit length of stay. Crit Care Med 2000;28:2090–2093 [DOI] [PubMed] [Google Scholar]
- 20.Jencks SF, Williams DK, Kay TL. Assessing hospital-associated deaths from discharge data. The role of length of stay and comorbidities. JAMA 1988;260:2240–2246 [PubMed] [Google Scholar]
- 21.Kahn JM, Scales DC, Au DH, Carson SS, Curtis JR, Dudley RA, Iwashyna TJ, Krishnan JA, Maurer JR, Mularski R, et al. An official American Thoracic Society policy statement: pay-for-performance in pulmonary, critical care, and sleep medicine. Am J Respir Crit Care Med 2010;181:752–761 [DOI] [PubMed] [Google Scholar]
- 22.Gracey DR, Hardy DC, Koenig GE. The chronic ventilator-dependent unit: a lower-cost alternative to intensive care. Mayo Clin Proc 2000;75:445–449 [DOI] [PubMed] [Google Scholar]
- 23.Seneff MG, Wagner D, Thompson D, Honeycutt C, Silver MR. The impact of long-term acute-care facilities on the outcome and cost of care for patients undergoing prolonged mechanical ventilation. Crit Care Med 2000;28:342–350 [DOI] [PubMed] [Google Scholar]
- 24.Defining long-term care hospitals. MedPAC Report to the Congress: new approaches in Medicare; June 2004. [Google Scholar]
- 25.Votto JJ, Scalise PJ, Barton RW, Vogel CA. An analysis of clinical outcomes and costs of a long term acute care hospital. J Media Econ 2011;14:141–146 [DOI] [PubMed] [Google Scholar]
- 26.Kandilov A, Dalton K. Utilization and payment effects of Medicare referrals to long-term care hospitals (LTCHS). Final report. Falls Church, VA: Kennell and Associates, Inc.; 2011 [Google Scholar]
- 27.Monitoring post-acute care. MedPAC Report to Congress: variation and innovation in Medicare; June 2003. [Google Scholar]
- 28.Kahn JM, Iwashyna TJ. Accuracy of the discharge destination field in administrative data for identifying transfer to a long-term acute care hospital. BMC Res Notes. 2010;3:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.