Abstract
The increased prevalence of obesity and the lack of treatment success both argue for the design and evaluation of strategies to prevent the development of overweight and obesity. To date, the role of resistance training (RT) in this regard is largely unexplored. RT may be effective for weight management as a result of increased fat-free mass (FFM), which may result in increased resting metabolic rate and increased physical activity energy expenditure. However, the literature relative to the efficacy of RT protocols recommended for healthy adults to alter the aforementioned parameters is inconsistent or inadequately evaluated. We will conduct a 9 month randomized controlled efficacy trial to compare changes in body composition (fat mass, FFM, % body fat) and energy balance in response to 2 volumes of RT (1 vs. 3 sets vs. non-exercise control) both at the completion of training (9 months) and 1 year later (body composition). This investigation will be conducted in a sample of healthy, normal and overweight, sedentary, young adult men and women; a group at high risk for development of overweight and obesity. Our results will provide information relative to the minimum volume of RT that may be associated with body weight/fat gain which may inform the development of guidelines for RT to prevent weight gain or to alter body composition.
Keywords: resistance training, weight management, obesity, training volume, body composition, gender
1. Introduction
Obesity is a highly prevalent chronic disease that is associated with numerous co-morbidities including cardiovascular disease, diabetes, hypertension and some cancers [1, 2]. Treatment for obesity has proven difficult with a high proportion of those who lose weight regaining much of the weight they have lost [3, 4]. Both the high prevalence of obesity and the lack of treatment success argue for the evaluation of strategies to prevent the development of overweight and obesity.
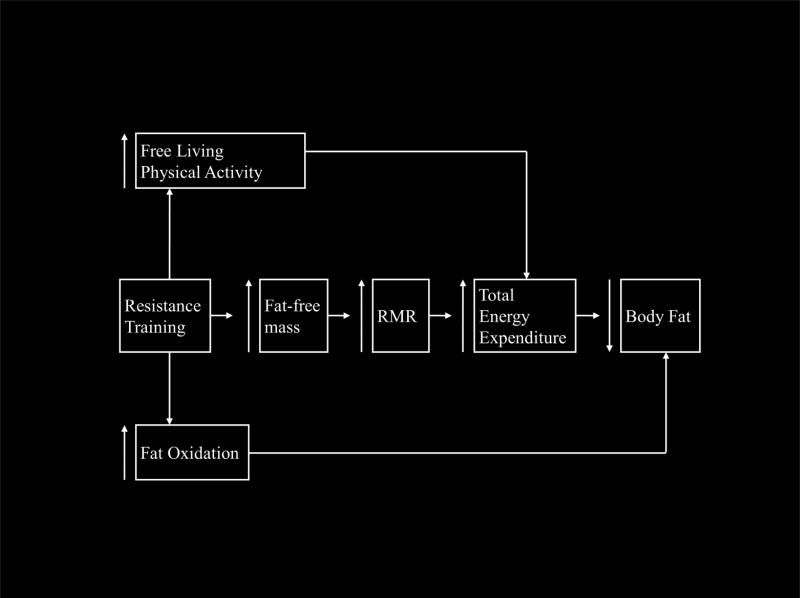
The Surgeon General, Centers for Disease Control, and the American College of Sports Medicine (ACSM) all recommend resistance training (RT) as an integral part of adult fitness programs [5-7]. However, the role of RT in the prevention of overweight and obesity is largely unexplored. As depicted in Figure 1, RT may have a positive impact on weight management as a result of increased fat-free mass (FFM) [8, 9] and increased fat oxidation [10-13]. Increased FFM may result in increased resting metabolic rate (RMR) [14, 15] and increased physical activity energy expenditure (PAEE) [16].
Figure 1.
Theoretical association: Resistance training and body composition
However, the literature relative to the efficacy of RT, to alter the aforementioned parameters is inconsistent or inadequately evaluated [16-26].
We completed a 6 month pilot randomized trial (NIH-DK62832) in overweight young adults [n = 32 RT, 23 control (C)], to evaluate the effect of a supervised minimal RT protocol (3 days/wk., 1 set, 3-6 repetitions maximum, 9 exercises) on body composition (dual energy x-ray absorptiometry-DXA), RMR and sleeping metabolic rate (SMR), and fat oxidation (whole-room calorimeter: sub-sample, (n = 22 RT, 17 C). Our pilot results suggested a positive impact of RT on body composition, energy expenditure, and fat oxidation [12, 13]. RT was associated with a significant decrease in % body fat resulting from a significant increase in FFM (RT = 2.7%, C = -0.6%) and a smaller increase in fat mass (FM) in RT (2.2%) compared with C (8.5%). Both RT and C showed increased 24-hr energy expenditure with a trend toward larger increases in RT (4%) vs. C (2.1%). Twenty-four- hour fat oxidation tended to decrease in C and increase with RT. RT resulted in a significant increase in metabolic rate and fat oxidation during sleep and a trend toward an increase in metabolic rate and fat oxidation during rest. No significant differences for change in body weight between RT and C were observed.
Based on the available literature and our pilot results we will conduct a randomized efficacy trial with 1 primary and 3 secondary aims: Primary aim: To determine the impact of the volume (1 vs. 3 sets) of RT on body composition (fat mass, fat free mass and % body fat) both at the completion of a 9 month RT protocol and 1 year later. Secondary aims will evaluate the impact of RT volume (1 vs. 3 sets) on energy balance and explore potential gender differences in the response of body composition to the RT protocols.
2. Methods and Materials
2.1. Study Overview
We will conduct a 9 month randomized controlled efficacy trial, with a 1 year post-training follow-up, to evaluate the impact of a progressive RT protocol as recommended by the ACSM for inducing muscular hypertrophy (1 set vs. 3 sets vs. non-RT control) on body composition, weight and energy balance. We will study a sample of (n = ~150) healthy, normal and overweight (BMI = 22 to <30), sedentary, young adult men and women (age 18-30), a group at high risk for the development of overweight and obesity. while consuming an ad libitum diet. Advice regarding physical activity outside the RT protocol and diet will not be provide as documenting any changes in energy balance, i.e. changes in physical activity and/or diet outside the study protocol, and how these changes may impact weight and body composition, is a goal of the study. The following variables will be assessed: height, weight, body composition (dual energy x-ray absorptiometry -DXA, waist circumference), free-living total daily energy expenditure (TDEE) and PAEE (doubly labeled water-DLW), RMR (ventilated hood), dietary intake (picture-plate-waste –PPW, 24 hr. recalls), muscular strength (1- repetition maximum-RM).The goal of our project is to prevent increases in weight/fat, therefore conducting the study in a young adult sample (age 18-30) before they become either overweight or obese (i.e., BMI 22 to <30), and where the rate of weight gain is high, increases the probability of detecting an effect of our intervention. US Census data indicates that in 2008 approximately 15.4 million individuals age 18-30 yrs. are enrolled in college [27]. Thus, if our intervention is successful there would be an available avenue for dissemination. Our results will provide information relative to the minimum volume of RT that may be associated with body weight/fat gain which may inform the development of guidelines for RT to alter body composition or prevent weight gain. If a 1-set RT has a favorable impact on energy balance and body composition, it may provide an attractive alternative to aerobic exercise for weight management for busy young adults, as RT requires minimal time, and no need to change clothes or shower (i.e., minimal or no sweating).
2.2. Design Justification
2.2.1. Age/Gender
We have chosen to study 18-30 year olds as they represent a group at high risk for the development of overweight and obesity. Recent data from the National Health and Nutrition Examination survey 2009-2012 indicted that combined prevalence of overweight and obesity among 20-39 year olds was 67.1% [28] while 33.6% of those age 12-19 had a BMI ≥ 85th percentile [29]. Young adulthood also represents a period on increased potential for weight gain [30-33]. For example, in the CARDIA study, a 7-year longitudinal follow-up of 5,115 black and while young adults, age 18-30 at baseline, the average weight gain over the 7-year follow-up ranged from a low of 5.2 kg in white women to a high of 8.5 kg in African American women [34]. The risk of adult obesity is more strongly associated with overweight during late adolescence than is being overweight earlier in life [35-37]. Guo et al. [35] reported that in 18 year olds, with a BMI exceeding the 60th percentile, the risks for adult overweight were 34% for men and 37% for women. To enhance the generalizability of our results equal numbers of men and women will be randomized to each of the 3 study groups
2.2.2. Intervention Length
A trial length of 9 months was selected based on our 2003 review on RT and weight management [8], more recent investigations of RT and body composition, as well as results from our pilot study [13]. Our 2003 review included only 3 studies in young adults of at least 6 months duration, and no studies in young adults longer than 6 months [8]. More recent studies on RT and body composition in young adults tend to be 6 months or less [18, 19, 21, 22, 38]. A meta-analysis by Wolfe et al. [39] indicated greater increases in muscular strength with training durations 17-40 weeks vs. 6-16 weeks. In our pilot (DK62832) data from 11 resistance trained men with measures of body composition at baseline, 3, and 6 months indicated beneficial changes only between months 3 and 6: FFM (+2.9%), fat mass (-3.5%), % body fat (-3.7%). Body weight increased in both RT and control groups, the magnitude of weight change with RT was less between months 3 and 6 (+0.7%) than from baseline to month 3 (+3.2%). This is in contrast to the change in weight in controls: baseline -3 months (+ 1.5%); 3 month-6 months (+ 2.8%). The difference in the rate of weight change between RT and control suggests that increased FFM and the potential for increased TDEE (PAEE + RMR) elicited by RT may require a training protocol longer than 6 months before the magnitude of decreased fat mass exceeds that of increased FFM and results in decreased body weight. The benefit of RT on body weight/composition observed from months 3 to 6 in our pilot study justifies a longer trial (9 months) to determine if these benefits would plateau or continue to accrue.
2.2.3. Training volume- One vs. 3 sets
We chose to examine 1 vs. 3 sets based on our pilot data, and suggestions in the literature of the superiority of 3 over 1 set RT protocols on strength and hypertrophy with longer term RT (> 3 months). Results from our pilot study indicated a potential for a time efficient 1 set RT protocol (11 minutes to complete) to favorably impact body composition, SMR, RMR, and fat oxidation [12, 13]. The impact of a higher volume RT protocol (i.e., 3 sets) on body composition and energy balance is unknown. The majority of the literature comparing 1 vs. 3 set RT protocols examines the impact on strength and hypertrophy. In untrained participants, as will be used in this project, a number of studies show similar increases in strength with 1 vs. 3 set RT protocols, whereas others show 3 sets to be superior [40]. A meta-analysis by Wolfe et al. [39], suggests that during initial training in untrained individuals (months 1-3) strength gains with single and multiple set protocols may be similar, but over the longer term (>3 months) 3 set protocols result in greater improvements in strength and hypertrophy. There is limited information available regarding the differential impact of 1 vs. 3 set RT on body composition. The only available study assessing body composition by DXA in a small sample (n = 12, 1 set, n = 16, 3 sets) of older (age = 65-78 yrs.) untrained men and women over 20 wks., reported no significant differences for change in fat mass, FFM or % body fat, however; decreases in fat mass and % body fat tended to be greater in the 3 vs. the one set groups [20]. Studies of body composition in individuals with previous experience with RT, using skinfold and bio-electric impedance assessments, have shown no differences in body composition between 1 and 3 set protocols in younger men (20 yr.) [41] and older men and women (40 & 56 yr. olds) [42, 43] who trained for 12 [43], 13 [42], or 14 wks. [41]. Comparisons of 1 vs. 3 set RT protocols on body composition and strength across studies are complicated by differences in assessment techniques [20, 41, 42, 44, 45], training intensity [20, 41, 42, 46], muscle groups trained and tested [20, 44, 45, 47], and participant prior experience with RT [20, 41, 42, 44]. Therefore, considering the documented superiority of 3 set vs. 1 set RT for increasing muscular strength and hypertrophy with longer duration training (> 3 months) and the potential for 3 set protocols to produce superior effects on body composition in untrained participants, we chose to compare a 1 vs. 3 set RT protocol on body composition and energy balance. One set RT, as recommended by the American College of Sports Medicine (ACSM) for general adult fitness [5] represents a time efficient (approximately 15 minutes to complete) approach that is appealing to the sedentary young adult population. It is important to determine if this approach will result in changes in body composition and energy balance when performed for 9 months, and if these changes are of a similar or superior magnitude to a more time consuming 3 set RT protocol (30-40 minutes). Thus, our results will provide information relative to the minimum volume of RT that may be associated with body weight/fat gain.
2.2.4. BMI
The goal of our study is to prevent the development of overweight and obesity, thus both normal (BMI = 22 to <25) and overweight (BMI = 25 to <30) individuals will be evaluated. Obese individuals (BMI ≥ 30) require weight loss, which is not the focus of our study, thus they will not be included. Individuals with BMI <22 may be genetically predisposed to resist weight gain, unhealthy, or have eating disorders, thus they will not be included.
2.3. RT interventions
2.3.1. RT program overview
All RT will be supervised and completed in The Energy Balance Laboratory (EBL), Center for Physical Activity and Weight Management at the University of Kansas. The exercise room will be available 6 hours/day on weekdays, and 3 hours on Saturday. We will use a 9 month, progressive, periodized RT protocol (4 week cycles) as recommended by the ACSM [5]. This approach has been shown to maximize gains in both muscular strength and FFM in both trained and untrained individuals [48]. Participants will complete 9 resistance exercises using Paramount Advanced Performance equipment (Paramount Fitness Corp. Los Angeles, CA): bench press, shoulder press, lat pull, triceps pushdown, back extension, leg press, leg curl, calf raise, and abdominal crunch.
2.3.1. RT- Progression/periodization
The progression of the 9 month RT program is outlined in Table 1. Training load and repetitions will be identical for the 1 and 3 set conditions.
Table 1.
Resistance training, Energy Balance and Weight Management Trial: Progression of the Resistance Training Protocol.
| Training Cycle (weeks) | Sets | Reps | Intensity (% 1 RMa) | |
|---|---|---|---|---|
| Cycle 1. | 1-2 | 1 or 3 | 15 | Self- selected |
| 3-4 | 50% | |||
| Cycle 2. | 5-8 | 1 or 3 | 12 | 60% |
| Cycle 3. | 9-12 | 1 or 3 | 10 | 60% |
| Cycle 4. | 13-16 | 1 or 3 | 8 | 75% |
| Cycle 5. | 17-20 | 1 or 3 | 6 | 90% |
| Cycle 6. | 21-24 | 1 or 3 | 10 | 60% |
| Cycle 7. | 25-28 | 1 or 3 | 8 | 75% |
| Cycle 8. | 29-32 | 1 or 3 | 6 | 75% |
| Cycle 9. | 33-36 | 1 or 3 | 6 | 90% |
RM – repetition maximum; Reps = Repetitions
The initial 4 week cycle is intentionally light to allow participants to accommodate to the equipment and the un-accustomed exercise, and progresses gradually to reduce muscular soreness, and prevent injury. Each RT session will be preceded by a 5-10 minute warm up of light cardiovascular exercise (bike, treadmill, elliptical trainer), followed by stretching of the major muscle groups utilized for RT. The order of exercises will be randomly assigned for each participant each week. Participants assigned to the 3 set protocol will be allowed a 30-60 second rest between sets, and 2 minutes rest between exercises. To decrease the likelihood that momentum is used to lift the weight, and to provide maximal muscle loading, all lifts will be performed in approximately 6 seconds (2 seconds concentric, 4 seconds eccentric). During the first 2 weeks of training (6 sessions) participants will perform all exercises using a self-selected minimal resistance. At the beginning of week 3, participants will be evaluated for maximal strength (1-RM) for all exercises to determine initial training load (50% 1-RM). The data for leg press and bench press will also be used as the baseline strength measure. One-RM will be determined for each exercise at the beginning of each 4 week training cycle to adjust training load. Participants will train 3 days/week and will not be allowed to complete more than one training session every 48 hrs.
2.3.2. RT-Compliance
Compliance with the RT guidelines is crucial in an efficacy study, thus we have proposed direct supervision of all RT sessions. We feel that direct supervision of the RT program is essential and has been shown to elicit greater gains in muscular strength when compared with non-supervised programs [49]. Participants will report to the training supervisor prior to the initiation of any exercise and will remain under their supervision throughout the exercise session. The training supervisor is responsible for verification that the subject completes RT sessions and adheres precisely to the exercise prescription. Training supervisors will complete an Excel spread sheet documenting the exercise, sets, repetitions, and load for each participant at each supervised RT session. Participants will be dismissed from the study if attendance falls below 80% of scheduled supervised RT sessions during any 3 month period (months 1-3, 4-6, or 7-9), and will not be allowed to miss more than 4 consecutive scheduled training sessions. Participants will receive weekly reports regarding their attendance status. During extended breaks in the academic calendar (Thanksgiving, Winter, Spring Break) participants will be permitted to complete an “at-home” RT protocol using resistance tubing and a video/DVD (developed by the study staff) provided to them or to complete RT at a fitness center. The DVD/video will demonstrate the proper technique for all prescribed exercises. The at-home protocols will be individualized to reflect the current training prescription. To encourage completion of RT at a fitness center, participants will be reimbursed for a maximum of 5 day passes over the course of the 9 month RT protocol. To minimize the potential for participants to accumulate missed training days and using them all during the Winter break we will allow a maximum of 12 unsupervised RT sessions to satisfy attendance requirements over the course of the 9 month RT protocol. Therefore if a participant uses the maximum available unsupervised RT sessions we would still provide direct supervision of approximately 90% of scheduled sessions.
2.4. Participants
2.4.1. Recruitment pool/rate
We will recruit 3 cohorts of approximately 50-52 men and women (age 18-30 yrs.) attending the University of Kansas and/or living in the Lawrence community, over 4 years for a total of approximately 150 participants. The most recent available demographic information indicates that non-whites comprise 20% of the University of Kansas student population and 16.2% of the Lawrence community. We will recruit 20% non-whites for this study with both ethnic and racial distribution to equal or exceed that of the Lawrence community (3.6% Hispanic or Latino, 2.9% American Indian/Alaska Native, 3.8% Asian, 5.1% Black/African American). We will recruit 152 participants to allow for a post-enrollment attrition rate of ~20%. The proposed 20% attrition rate includes attrition for failure to comply with the resistance training protocol. Although the attrition rate in our pilot study was only 13%, we feel that a 20% attrition rate is a realistic projection given the increased study length and the inclusion of more frequent, time consuming assessments (including a 1 year follow-up) required of the proposed study. There are over 29,000 students currently attending the University of Kansas at Lawrence, and approximately 30,000 individuals, age 18-30, living in the Lawrence community. It is estimated that approximately 43% of this population are normal weight and 29% are overweight [28], thus approximately 25,000 normal weight and 17,000 overweight potential participants (6,800 minorities) will be available. Not all 42,000 potential normal and overweight participants will meet other inclusion/exclusion criteria (Table 2) nor will all of these potential participants volunteer for the study.
Table 2.
Resistance training volume, energy balance and weight management trial: Inclusion/exclusion criteria.
| Inclusion criteria |
|---|
| • Age 18 to 30. |
| • BMI 22 to < 30. |
| • No resistance training in the past 12 months. |
| • Sedentary except for casual recreation such as softball, bowling, etc. This will be determined < 500 kcal per wk. of exercise physical activity as estimated by the Minnesota Leisure Time Physical Activity Questionnaire. |
| • Weight stable (± 2.27 kg) for 3 months prior to intake. This will be determined by phone/web screen and self-report on the health history questionnaire. |
| • Willing to take three meals per day for 3, 1- wk. periods throughout the study at The University of Kansas Cafeteria. |
| • Willing to be randomized to one of the three study groups: control, 1 set RT, 3 set RT. |
| • Determined to be healthy and capable of participation in RT based on a review of the health history and results of the 24 item blood panel by our study physician. |
| • Females: a negative pregnancy test at baseline. Pregnancy during the study will result in dismissal. In addition to baseline, pregnancy status will be assessed at all subsequent DXA assessments (4.5 and 9 months, 1-yr follow up). |
| • Females currently using oral/hormonal contraceptives: No change in oral/hormonal contraceptive use in the past year. |
| • Females not currently using oral/hormonal contraceptives: No use of oral/hormonal contraceptives within the past year, normal and regular menstrual cycles of 25-32 days for the past 6 months, and 5-6 menstrual cycles in the past 6 months. |
| • lanning to be in Lawrence for the duration of the 9 month study and to be available for a 1- yr., follow-up. |
| Exclusion criteria |
|---|
| • Individuals with contraindications based on the review of the health history and results from the 24 item blood panel (glucose, insulin, lipids, electrolytes, liver function etc.) by the study physician will be excluded. Individuals with abnormal lab values will be referred to their personal physician. |
| • Cardiovascular disease and metabolic disorders: dyslipidemia- lipids (cholesterol > 240 mg/L; triglycerides >500 mg/L), hypertension- systolic blood pressure > 140 mmHG or diastolic blood pressure > 90 mmHG, diabetes – fasting glucose > 126 mg/dL. |
| • Medications that could affect metabolism such as cardiac drugs, thyroid, steroids, insulin, beta blockers, SSRI's, etc. |
| • Weight altering products such as Dexitrim, Metabolife, creatine, etc. |
| • Current use of smoking/tobacco products or initiation of smoking/tobacco during the study. |
| • Alcohol consumption exceeding 3 drinks per day or a total of 18 per wk. This will diminish the number of subjects who are binge drinkers (Health Risk Behaviors of Kansans, 2002). |
| • Eating disorders as determined by the Eating Attitudes Test using a score of 20 or greater. |
| • Center for Epidemiological Studies Depression Scale scores of 35 or greater at baseline. |
| • Treatment for psychiatric illness or chemical dependency within the previous 6 months. |
| • Pregnancy, lactation or amenorrhea (lack of a natural menstrual period > 6 months). |
| • Initiation of, or change in oral/hormonal contraceptives within the past 6 months, or have less than 4 or greater than 6 menstrual cycles within the past 6 months. |
| • Orthopedic contraindications to participation in resistance training as determined from review of the health history by the study physician. |
| • Excessive exposure to radiation (x-rays, CT, PET, Fluroscopic or nuclear medicine studies) in the past 12 months as determined from review of the health history form by the study physician. |
Reducing the number of potential participants by 75% to account for those who do not meet the inclusion criteria, or do not care to participate leaves a pool of 10,500 potential participants. Recruiting the 152 participants necessary to achieve our desired statistical power would require a recruitment rate of 1.4%. We recognize that it may be perceived that participants will not accept randomization to a sedentary control condition. We will offer controls an identical RT program the following year, however; our experience is that few actually initiate this offer. All participants will receive monetary compensation. In addition to the monetary incentives, we believe the opportunity to receive a professionally designed and supervised 9 month RT program will be of interest to the young adult population.
2.4.2 Recruitment strategies/randomization
We will contact potential participants by a variety of media and public announcements. We will advertise our study in the University Daily Kansan (UDK), the campus newspaper that has a wide readership. Eleven thousand five hundred UDK's are printed daily and distributed throughout campus. We will post flyers on the KU campus including classroom buildings, dormitories, and the Kansas Student Union. We will have a recruitment booth in the Kansas Student Union on the main entry floor and we will have a second booth in the university cafeteria where over 5,000 students obtain their meals. We will announce the study in large service classes containing several hundred students per class and post a description of the study on our laboratory web site. In addition, we will use both the campus and Lawrence radio stations to air public service messages regarding the study. All forms of advertising will include our dedicated study phone number as well as our web site and study e-mail address to provide multiple options for potential participants to contact study staff. Potential participants will be asked to complete a web-based initial eligibility screener regarding height and weight to determine BMI, use of medications, smoking and drinking habits, and current levels of physical activity (including RT). Those without web access will be asked to complete the initial screener by hard copy or telephone interview. Individuals considered eligible based on the initial eligibility screen will be scheduled to meet with the project coordinator. At the orientation meeting requirements for study participation will be explained, questions will be answered, informed consent will be obtained, and appointments will be scheduled for blood sampling, and assessment of height and weight to determine final eligibility. Randomization will be stratified by gender (50% women, 50% men) and BMI (22-24.9/ 25-29.9) under the supervision of our study statistician. For each gender and BMI category, participants will be sequentially randomized (1:1:1) into one of three groups: control, 1 set RT, 3 set RT.
2.5. Outcomes
2.5.1. Outcome assessment schedule/methods
A schedule for outcome assessments is presented in Table 3. All laboratory assessed outcomes will be obtained with at least 48 hours separating the assessment and the completion of an RT session. Two laboratory visits will be required at baseline, 4.5, and 9 months. Height/weight and body composition will be assessed at visit 1 and RMR at visit 2. Muscular strength assessments (baseline, 4.5, 9 months) will be performed in conjunction with the RT program and will not require additional laboratory visits. Dietary intake (PPW) will be assessed at baseline, 4.5, and 9 months, while free living energy expenditure (14 d-DLW) and RMR will be assessed at baseline and 9 months. Dietary intake by 24-hr. recall will be assessed at months 2.25 and 6.75. Laboratory testing visits are anticipated to require approximately 45-60 minutes. Outcome assessments for females with normal menstrual cycles will be obtained on days 5-10 of the cycle (early follicular phase). Outcome assessments will be conducted during the “placebo” period, i.e. days 22-28 for females taking oral/hormonal contraceptives.
Table 3.
Resistance training, energy balance and weight management trial: Outcome assessment schedule.
| Month |
||||||
|---|---|---|---|---|---|---|
| Baseline | 2.25 | 4.5 | 6.75 | 9 | 21 | |
| Anthropometrics | ||||||
| Height | X | X | X | X | ||
| Weight | X | X | X | X | ||
| Body Composition (DXA) | X | X | X | X | ||
| Waist Circumference | X | X | X | X | ||
| Energy Expenditure/PA | ||||||
| Doubly Labeled Water | X | X | ||||
| Resting Metabolic Rate | X | X | ||||
| PA (Accelerometry) | X | X | ||||
| Exercise Session | X | |||||
| Energy Intake | ||||||
| Picture-plate waste | X | X | X | |||
| 24-hour recalls | X | X | ||||
| Muscular Strength | X | X | X | |||
Note: DXA (Dual-energy X-ray absorptiometry), PA (physical activity)
2.5.2. Blinding/Attention
Research staff conducting all assessments, data entry, and data analysis will be blind to participant group assignment. We realize that the control group (no RT) will not have similar weekly contact hours with the research staff and are aware, that in some study designs, contact is an important variable. However, we do not expect differential contact between RT and control will influence the outcome of the current study. We have previously demonstrated that control groups of young adults will remain sedentary and likely will gain weight [50]. In similar fashion, it is unlikely that the RT groups will maintain or lose weight solely due to contact with research staff. RT and control groups will participate in identical assessment protocols.
2.5.3. Body height/weight and body composition
Body weight will be recorded at baseline, 4.5 and 9 months using a digital scale accurate to ± 0.1 kg (Befour Inc. Model #PS6600, Saukville, WI). Participants will report to the EBL between the hours of 7 and 9 a.m., after an overnight fast, and will be weighed prior to breakfast after attempting to void. Participants will wear a standard hospital gown at the time of weighing. Height will be measured using a stadiometer (Model PE-WM-60-84, Perspective Enterprises, Portage, MI) and BMI (kg/m2) will be calculated. Fat-free mass, fat mass and % body fat will be assessed by DXA (Prodigy Advance Plus, GE, Madison, WI) at baseline, 4.5, and 9 months. Women will undergo pregnancy testing prior to each DXA test. Participants will wear a hospital gown during DXA scans to standardize clothing. We will also use DXA to estimate visceral adipose using existing equations [51]. Skeletal muscle mass from DXA derived appendicular lean soft tissue mass will be calculated using the equation of Kim et al. [52]. Waist circumference will be assessed using procedures described by Lohman et al. [53]. We will obtain 2 measurements per site within 2 cm.
2.5.4. Resting metabolic rate (RMR)
RMR will be assessed at baseline and 9 months by open circuit indirect calorimetry with the participant in the supine position [54]. In addition to serving as an outcome measure, RMR assessed at baseline and 9 months will be used for the determination of PAEE obtained from DLW measurements (Section 2.5.5). Participants will report to the EBL between 6 and 10 a.m. after a 12 hour fast and 48 hour abstention from RT or aerobic exercise [55, 56]. Following 30 minutes of rest in an isolated, temperature controlled (21-24 °C) room participants will be placed in a ventilated hood for a minimum of 30 minutes. Expired gases will be analyzed with a ParvoMedics TrueOne 2400 indirect calorimetry system (ParvoMedics Inc, Sandy, UT). Criteria for a valid RMR will be a minimum of 15 minutes of steady state with steady state determined as less than 10% fluctuation in minute ventilation and oxygen consumption and less than 5% fluctuation in respiratory quotient (Sensormedics Corporation, Yorba Linda, CA). RMR (kcal/day) will be calculated using the equations of Weir [57].
2.5.5. Free-living energy expenditure by doubly labeled water (DLW)/Physical activity (accelerometry)
DLW will be used to assess average 24-hour energy expenditure over a 14 day period at baseline and 9 months using the procedures used in our completed (DK41981) [50] and on-going (DK49181-06) long term aerobic exercise trials. The end of study assessment (9 month) will be conducted during the last 2 weeks of the RT protocol. Participants will report to the EBL between 8:00 and 9:00 a.m. after an overnight fast. Two baseline urine specimens will be collected from each participant prior to oral dosing with a mixed solution of 2H218O. The isotope given to each participant will contain approximately 0.10g/kg body weight of 2H2O and 0.15g/kg of H218O. After administration of the isotope dose, participants will be given a rinse solution of 100ml of tap water. For each participant's dose, a weighed 1:400 dilution of the dose will be prepared and a sample of the tap water will be stored at -70°C for later analysis. Additional urine samples will be collected on days 1 and 14. On these days 2 urine samples will be collected at least 3 hours apart. All urine samples will be stored in sealed containers at -70°C and shipped in dry ice to the Clinical Research Core Laboratory at the University of Alabama-Birmingham for analysis. Samples will be analyzed in duplicate for 2H2O and H218O by isotope ratio mass spectrometry as previously described by Herd et al. [58]. Total daily energy expenditure (TDEE) will be estimated using the equation of Elia [59]: Total EE (Mj/d) = (15.48/RQ + 5.55) × rCO2 (L/d). Physical activity energy expenditure (PAEE) will be estimated from TDEE and RMR (PAEE = (TDEE *0.9) – RMR [26]. This approach assumes that the thermic effect of food represents 10% of TDEE [60]. To assess the impact of the RT intervention on TDEE irrespective of the energy expenditure associated with the RT program, we will measure the energy expenditure of the RT protocol by portable indirect calorimetry (CosMed K4b2 –Rome, Italy) twice during the 14 day DLW period. The average energy expenditure across the 2 measures will be subtracted from the PAEE to determine if any changes in PAEE from baseline to 9 months were associated with changes in PAEE outside the RT program. We will also examine the impact of the energy expenditure of RT on changes in weight and body composition. To determine between and within day variation in physical activity (i.e., compare exercise/ non-exercise days, exercise time/non-exercise time), and to estimate time spent in a range of PA intensities (sedentary/light/moderate/vigorous), participants will wear an ActiGraph GT3X+ (ActiGraph, LLC, Pensacola, FL) for 7 consecutive days at baseline, 3 and 9 mos. Data collection interval will be 1-min. with a minimum of 10 hrs. constituting a valid day. We will use NHANES intensity cut-points as described by Troiano et al [61].
2.5.6. Measurement of energy intake and macronutrient composition by picture plate waste and 24 hr. recalls
We will assess energy intake and macronutrient composition during ad libitum eating in our research cafeteria using picture plate waste (PPW), and 24 hour recalls. PPW uses standardized digital photographs of meals before and after consumption. The research staff observes the photos and records consumption. We have previously documented our ability to precisely measure energy intake in our research cafeteria using weighed plate waste methodology [62]. To reduce participant burden we have modified our weighed plate waste methodology and now use a PPW technique. We will document 7 consecutive days of dietary intake in our research cafeteria using PPW at 3 time points (baseline, 4.5, and 9 months). We have previously demonstrated that 7 days of dietary intake data adequately characterize usual energy intake in young adults [63]. We have shown an average difference of 2.2% between daily energy intake over 7 days assessed by PPW and daily energy expenditure assessed by DLW in a sample of 68 young adults. We also will obtain 24 hour dietary recalls on 3 non-consecutive days, including 1 week end and 2 week days, during months 2.25 and 6.75 (midway between PPW assessments). The 24 hour recalls will be obtained by the study dietitian when participants report for a RT session. The energy and macronutrient content of both PPW and 24 hr. recall data will be determined using Nutrition Data System for Research (NDS-R, version 2011, University of Minnesota, Minneapolis, MN).
2.5.7. Dietary staff training and quality control
All staff will complete standardized training for PPW, 24-hr. recalls, and NDS-R coding, prior to the beginning of data collection, with refresher sessions every 2 months, thereafter. After initial training, all dietary assessment staff will be required to complete ten 24-hr. recalls obtained from non-study subjects, and ten weighed and measured sample PPW meals, and enter this data directly into NDS-R. The recalls will be evaluated according to a published dietary recall documentation checklist [64]. Agreement > 95% on this checklist and on NDS-R coding will be required before interviewers will be allowed to collect and process dietary recall data. During the study, all dietary recalls will be evaluated by our study dietician using the recall documentation checklist before entry into the study database. Any recall with greater than 5% error will be eliminated and another recall obtained. The PPW results will be compared with the actual weighed and measured data. Study staff demonstrating agreement of < 95% or greater for either energy intake or macronutrient composition, will be required to obtain further training and repeat assessment of accuracy described previously. We will also conduct routine monitoring of the accuracy and reliability of our staff on dietary assessment techniques (PPW, 24-hour recall, NDS-R data entry) every 2 months throughout the 9 month study in conjunction with refresher training. Staff not meeting our criteria for accuracy at any time during the study following 3 attempts will not be permitted to collect or process dietary data.
2.5.8. Muscular strength
One RM strength for the bench and leg press will be assessed at baseline, 4.5, and 9 months using the protocol described by Lemmer et al.[24]. Baseline strength will be assessed following a 2 week period of resistance training (6 sessions) against minimal resistance. The order of testing will be randomized at baseline (bench vs. leg press), and remain the same for all further testing. All strength assessment will be preceded by a light 3-min warm-up on a cycle ergometer and supervised stretching of all major muscle groups, followed by 5 repetitions of the exercise to be evaluated, against minimal resistance. A resistance estimated by the participant and study staff to be just below the participant's 1-RM will be chosen and the participant will be asked to lift the weight one time. If the lift is completed successfully through the full range of motion, the resistance will be increased (minimum increment 2.5 lbs.), and another attempt made following a rest period of at least 1 minute. This process will be continued until the subject is unable to lift the prescribed resistance. The highest weight lifted will be recorded as the 1-RM. At baseline only, participants will complete 1-RM evaluations for the remaining 7 RT exercises included in the training program to determine initial training load.
2.6. Analysis plan and statistical power
2.6.1. Analysis plan
Baseline measures and demographic characteristics will be summarized using means and standard deviations for continuous variables, and frequencies, percentages, and cross-tabulations for categorical variables. Differences in means at the midpoint (4.5 months), end of RT (9 months) and 1 year follow-up will be assessed by general linear models for continuous variables. To address our primary aim (changes in weight and body composition), we will examine the differences between the groups at the selected time point (4.5 and 9 months, 1 year post RT) using an analysis of covariance with the baseline measure as the covariate. Significant differences between the groups will be further examined using pair-wise difference tests to determine which groups differ from each other. Similar analyses of covariance will be performed to address secondary aim 1 (between group differences for energy intake, TDEE, PAEE, RMR). If between group differences in these variables are observed we will explore their role as simple covariates or as possible mediators or moderators of the effect of RT on our primary outcome (fat mass) [65, 66]. Other potential covariates (age, gender) will be explored using the same procedures by extending the model to include age/gender by treatment interaction terms. If the interaction effect for gender is significant, we will explore gender differences by evaluating differences between males and females in each treatment and for differences between treatments effects with gender groups. Similarly, if the age by treatment effect is significant, we will examine the effect of age within treatment condition. Effect sizes will be calculated for all gender comparisons to determine the magnitude of possible gender differences and to inform sample size estimates for future studies. Variables, other than the treatment, that are shown to be significantly associated with outcomes will be included in the final models used for the estimation of treatment effects. This information will be important in understanding the effects of RT, and for informing the design of subsequent studies, particularly if variables are determined to have moderating effects, or are shown to act as mediators. Statistical significance will be defined at p < 0.05 for all omnibus tests with follow-up tests conducted using appropriate p value adjustments (Tukey) to control Type I error. The analyses of covariance will allow us to determine if one treatment protocol is more effective than another at specific time points (4.5 and 9 months, 1 year post RT). We will also examine the rates of change for each of the experimental groups using general linear mixed models with the time of observation (baseline, 4.5, and 9 months) as a within-subjects factor and treatment group as a between subjects factor. The advantage of the general linear mixed model over traditional repeated measures analysis is increased flexibility in modeling the covariance structures and, the ability to include all cases, even those of participants with incomplete data, provided data are missing at random. Because of the limited number of observations, we will be able to fit only a random linear slope. A significant group x time (slope) interaction will indicate that the treatment groups are not changing at the same rate. Follow-up tests will allow us to determine the rate of change for each group and which groups differ in their rates of change. A similar change-over-time analysis will be conducted using the 1 year follow-up as the final data point and either baseline or 9 month data as the initial data point. These analyses will include the 2 treatment groups and controls. Data analysis will be performed using PC-SAS (Cary, NC).
2.6.2. Power and sample size
Statistical power for this study was based on the results from our pilot study [12, 13] indicating a moderate to large effect size (Cohen's delta = 0.67) [67] for the response of one of our primary outcomes (fat mass) to a 1 set, 6 month RT protocol and results from the literature on changes in fat mass as a result of 3 set RT protocols with durations of 8-18 weeks [18, 21, 68]. We used the SAS fpower macro (Friendly M, SAS Macro Programs (1995, updated 2006), SAS Institute, Cary, NC) for a design with one between-subjects factor (Control, RT-1set, RT-3 sets) and one within-subjects factor (time: 3 levels, baseline, 4.5, and 9 months). Our primary aim is to detect differences in fat mass among the study groups at the mid and endpoints and to examine the differences in the rate of change in fat mass over the 9 month intervention. A sample size of 40 participants per group, with an alpha level of 0.05, and assuming a correlation between repeated measures as high as 0.60 will provide power of 0.80 to detect a moderate effect-size (Cohen's delta = 0.60) for differences in fat mass among groups. For all analyses conducted, we will calculate observed effect sizes for differences between control and 1 set RT, control and 3 set RT, and between 1 and 3 set RT for the total sample, as well as within genders. Calculation of effect size will allow us to evaluate the clinical importance of any observed differences, and to inform sample size estimates for any similar future studies. We have projected a conservatively high attrition rate (~ 20%) and will recruit 152 participants at baseline to assure our final sample size requirements are met (40 completers/group). We have powered the study to detect between group changes in our primary outcome (fat mass), however; the proposed sample size (40 per group) should be adequate to detect at least moderate between group effects for changes in secondary outcomes (TDEE, RMR and FFM) based on the results from our pilot study where the following effect sizes were observed: 24-hr energy expenditure (Cohen's delta = .30) RMR (Cohen's delta = .60), FFM (Cohen's delta = 1.10) study [12, 13]. We will conduct an efficacy trial; therefore our analyses will include only participants who complete RT protocol and all outcome assessments.
2.7. Discussion
The specific aims of this project are to determine the impact of the volume (1 vs. 3 sets) of a progressive RT protocol for inducing muscular hypertrophy, as recommended by the ACSM, on body weight and body composition (fat and lean mass), and energy balance. We will conduct an efficacy study to answer the question, “What happens when participants complete a protocol as intended,” (i.e. efficacy). This is opposed to an effectiveness study which answers the question “what happens if participants will complete a protocol as intended”. This study will be conducted in both normal and overweight, sedentary, young adult men and women. Our results will provide information relative to the minimum volume of RT that may be associated with body weight/fat gain which may inform the development of guidelines for RT to prevent weight gain or to alter body composition. If a 1-set RT protocol has a favorable impact on energy balance and body composition, it may provide an attractive alternative to aerobic exercise for weight management for busy young adults, as resistance training requires minimal time, and no need to change clothes or shower (i.e., minimal or no sweating). If shown to be effective in young adults, additional studies in other populations will be necessary to provide evidence for generalizability. In addition, studies involving less rigorous supervision of the RT protocol would be useful to determine the potential for dissemination.
Acknowledgments
Funding: National Institutes of Diabetes, Digestive and Kidney Diseases (R01- DK80832)
Abbreviations
- ACSM
American College of Sports Medicine
- DLW
Doubly labeled water
- DXA
Dual energy X-ray absorptiometry
- EBL
Energy balance laboratory
- FFM
Fat free mass
- PAEE
Physical activity energy expenditure
- PPW
Picture plate waste
- RMR
Resting metabolic rate
- RT
Resistance training
- SMR
Sleeping metabolic rate
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kopelman P. Health risks associated with overweight and obesity. Obes Rev. 2007;8(Suppl 1):13–7. doi: 10.1111/j.1467-789X.2007.00311.x. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303:241–9. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 3.Meckling KA, O'Sullivan C, Saari D. Comparison of a low-fat diet to a low-carbohydrate diet on weight loss, body composition, and risk factors for diabetes and cardiovascular disease in free-living, overweight men and women. J Clin Endocrinol Metab. 2004;89:2717–23. doi: 10.1210/jc.2003-031606. [DOI] [PubMed] [Google Scholar]
- 4.Borg P, Kukkonen-Harjula L, Fogelholm M, Pasanen M. Effects of walking or resistance training on weight loss maintenance in obese, middle-aged men: a randomized trial. Int J Obes. 2002;26:676–83. doi: 10.1038/sj.ijo.0801962. [DOI] [PubMed] [Google Scholar]
- 5.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Medicine and Science in Sports & Exercise. 2011;43:1334–59. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 6.Pate RR, Blair SN, Haskell WL, Macera CA, Bouchard C, Bruchner D, et al. Physical activity and public health: A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–7. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 7.Pollock ML, Franklin BA, Balady GJ, Chaitman BL, Fleg JL, Fletcher B, et al. AHA Science Adivsory, Resistance exercise in individuals with and without cardiovascular disease benefits, rationale, safety, and prescription. An advisory from the committee on exercise, rehabilitation, and prevention, council on clinical cardiology, American heart association. Circulation. 2000;101:828–33. doi: 10.1161/01.cir.101.7.828. [DOI] [PubMed] [Google Scholar]
- 8.Donnelly JE, Jakicic JM, Pronk NP, Smith BK, Kirk EP, Jacobsen DJ, et al. Is resistance training effective for weight management? Evidence-Based Preventive Medicine. 2003;1:21–9. [Google Scholar]
- 9.Rabelo HT, Bezerra LA, Terra DF, Lima RM, silva MA, Leite TK, et al. Effects of 24 weeks of progresive resistance training on knee extensors peak torque and fat-free mass in older women. Journal of Strength and Conditioning Research. 2011;25:2298–303. doi: 10.1519/JSC.0b013e3181e86106. [DOI] [PubMed] [Google Scholar]
- 10.Ormsbee MJ, Choi MD, Medlin JK, Geyer GH, Trantham LH, Dubis GS, et al. Regulation of fat metabolism during resistance exercise in sedentary lean and obese men. Journal of Applied Physiology. 2009;106:1529–37. doi: 10.1152/japplphysiol.91485.2008. [DOI] [PubMed] [Google Scholar]
- 11.Chatzinikolaou A, Fatouros I, Petridou A, Jamurtas A, Avloniti A, Douroudos I, et al. Adipose tissue lipolisis is upregulated in lean and obese men during acute resistance exercise. Diabetes Care. 2008;31:1397–9. doi: 10.2337/dc08-0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Washburn RA, Kirk EP, Smith BK, Honas JJ, LeCheminant J, Bailey BW, et al. One set resistance training: Effect on body composition in overweight young adults. J Sports Med Phys Fitness. In press. [PubMed] [Google Scholar]
- 13.Kirk EP, Donnelly JE, Smith BK, Honas J, LeCheminant JD, Bailey BW, et al. Minimal resistance training improves daily energy expenditure and fat oxidation. Med Sci Sports Exerc. 2009;41:1122–9. doi: 10.1249/MSS.0b013e318193c64e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alpert SS. The cross-sectional and longitudinal dependence of the resting metabolic rate on the fat-free mass. Metabolism. 2007;56:363–72. doi: 10.1016/j.metabol.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 15.Fatouros IG, Tournis S, Leontsini D, Jamurtas AZ, Sxina M, Thomakos M, et al. Leptin and adpnectin responses in overweight inactive elderly following resistance traiing and detraining are intensity related. The Journal of Clinical Endocrinology & Metabolism. 2005;90:5970–7. doi: 10.1210/jc.2005-0261. [DOI] [PubMed] [Google Scholar]
- 16.Ades PA, Savage PD, Broucha M, Tischler MD, Lee NM, Poehlman ET. Resistance training increases total daily energy expenditure in disabled older women with coronary heart disease. Journal of Applied Physiology. 2005;98:1280–5. doi: 10.1152/japplphysiol.00360.2004. [DOI] [PubMed] [Google Scholar]
- 17.Schmitz KH, Jensen MD, Kugler JC, Jeffery RW, Leon AS. Strength training for obesity prevention in midlife women. Int J Obes. 2003;27:326–33. doi: 10.1038/sj.ijo.0802198. [DOI] [PubMed] [Google Scholar]
- 18.Shaibi GQ, Cruz ML, Ball GDC, Weigensberg mJ, Salem GJ, Crespo NE, et al. Effects of resistance training on insulin sensitivity in overweight Latino adolescent males. Med Sci Sports Exerc. 2006;38:1208–15. doi: 10.1249/01.mss.0000227304.88406.0f. [DOI] [PubMed] [Google Scholar]
- 19.Glowacki SP, Martin SE, Maurer A, Baek W, Green JS, Crouse SF. Effects of resistance, endurance, and concurrent exercise on training outcomes in men. Med Sci Sports Exerc. 2004;36:2119–27. doi: 10.1249/01.mss.0000147629.74832.52. [DOI] [PubMed] [Google Scholar]
- 20.Galvao DA, Taaffe DR. Resistance exercise dosage in older adults: Single-versus multiset effects on physical performance and body composition. J Am Geriatr Soc. 2005;53:2090–7. doi: 10.1111/j.1532-5415.2005.00494.x. [DOI] [PubMed] [Google Scholar]
- 21.Shaw I, Shaw BS. Consequences of resistance training on body composition and coronary artery disease risk. Cardiovasc J S Afr. 2006;17:111–6. [PubMed] [Google Scholar]
- 22.Dionne IJ, Melancon MO, Brochu M, Ades PA, Poelhman ET. Age-related difference in metabolic adaptations following resistance training in women. Exp Gerontol. 2004;39:133–8. doi: 10.1016/j.exger.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 23.Cullinen K, Caldwell M. Weight training increases fat-free mass and strength in untrained young women. J Am Diet Assoc. 1998;98:414–8. doi: 10.1016/S0002-8223(98)00094-7. [DOI] [PubMed] [Google Scholar]
- 24.Lemmer JT, Ivey FM, Ryan AS, Martel GF, Hurlbut DE, Metter JE, et al. Effect of strength training on resting metabolic rate and physical activity: age and gender comparisons. Med Sci Sports Exerc. 2001;33:532–41. doi: 10.1097/00005768-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Broeder CE, Burrhus KA, Svanevik LS, Volpe J, Wilmore JH. Assessing body composition before and after resistance or endurance training. Med Sci Sports Exerc. 1997;29:705–12. doi: 10.1097/00005768-199705000-00019. [DOI] [PubMed] [Google Scholar]
- 26.Hunter GR, Wetzstein CJ, Fields DA, Brown A, Bamman MM. Resistance training increases total energy expenditure and free-living physical activity in older adults. J Appl Physiol. 2000;89:977–84. doi: 10.1152/jappl.2000.89.3.977. [DOI] [PubMed] [Google Scholar]
- 27.Davis JW, Bauman K. School Enrollment in the United States: 2008. US Census Bureau; 2011. pp. 20–564. [Google Scholar]
- 28.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2012. Journal of the American Medical Association. 2012;307(5) doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 29.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. Journal of the American Medical Association. 2012;307(5) doi: 10.1001/jama.2012.40. doi:10:1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lloyd-Richardson EE, Bailey S, Fava JL, Tobacco Etiology Research Network A prospective study of weight gain during the college freshman and sophomore years. Preventive Medicine. 2009;48:256–61. doi: 10.1016/j.ypmed.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gropper SS, Newton A, Harrington P, Simmons KP, Connell LJ, Ulrick P. Body composition changes during the first two years of university. Preventive Medicine. 2011;52:20–2. doi: 10.1016/j.ypmed.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 32.Crombie AP, Illich JZ, Dutton GR, Panton LB, Abood DA. The freshman weight gain phenomenon revisited. Nutrition Reviews. 2009;67:83–94. doi: 10.1111/j.1753-4887.2008.00143.x. [DOI] [PubMed] [Google Scholar]
- 33.Vella-Zarb RA, Elgar FJ. The “Freshman 5”: A meta-analysis of weight gain in the freshman year of college. Journal of American College Health. 2009;58:161–6. doi: 10.1080/07448480903221392. [DOI] [PubMed] [Google Scholar]
- 34.Lewis CE, Smith DE, Wallace DD, Williams OD, Bild DE, Jacobs DR., Jr Seven-year trends in body weight and associations with lifestyle and behavioral characteristics in black and white young adults: The CARDIA Study. American Journal of Public Health. 1997;87:635–42. doi: 10.2105/ajph.87.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guo SS, Roche AF, Chumlea WC, Gardner JD, Siervogel RM. The predictive value of childhood body mass index values for overweight at age 35 y. American Journal of Clinical Nutrition. 1994;59:810–9. doi: 10.1093/ajcn/59.4.810. [DOI] [PubMed] [Google Scholar]
- 36.Guo SS, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. American Journal of Clinical Nutrition. 2002;76:653–8. doi: 10.1093/ajcn/76.3.653. [DOI] [PubMed] [Google Scholar]
- 37.Guo SS, Huang C, Maynard LM, Demerath E, Towne B, Chumlea WC, et al. Body mass index during childhood, adolescence and young aduthood in relation to adult overweight and adiposity: the Fels Longitudinal Study. International Journal of Obesity. 2000;24:1628–35. doi: 10.1038/sj.ijo.0801461. [DOI] [PubMed] [Google Scholar]
- 38.Abe T, Kojima K, Yohena H, Fukuda J. Whole body muscle hypertrophy from resistance training: distribution and total mass. Br J Sports Med. 2003;37:543–5. doi: 10.1136/bjsm.37.6.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wolfe BL, LeMura LM, Cole PJ. Quantative analysis of single- vs. multiple-set programs in resistance training. J Strength Cond Res. 2004;18:35–47. doi: 10.1519/1533-4287(2004)018<0035:qaosvm>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 40.Kraemer WJ, Ratamess NA. Fundamentals of resistance training: Progression and exercise prescription. Med Sci Sports Exerc. 2004;36:674–88. doi: 10.1249/01.mss.0000121945.36635.61. [DOI] [PubMed] [Google Scholar]
- 41.Kramer JB, Stone MH, O'Bryant HS, Conley MS, Johnson RL, Nieman DC, et al. Effects of single vs. multiple sets of weight traininig: Impact of volume, intensity, and variation. J Strength Cond Res. 1997;11:143–7. [Google Scholar]
- 42.Hass CJ, Garzarella L, De Hoyos D, Pollock ML. Single versus multiple sets in long-term recreational weightlifters. Med Sci Sports Exerc. 2000;32:235–42. doi: 10.1097/00005768-200001000-00035. [DOI] [PubMed] [Google Scholar]
- 43.Kemmler WK, Lauber D, Engelke K, Weineck J. Effects of single-vs. multiple -set resistance training on maximum strength and body composition in trained postmenopausal women. J Strength Cond Res. 2004;18:689–94. doi: 10.1519/R-16164.1. [DOI] [PubMed] [Google Scholar]
- 44.Ronnestad BR, Egeland W, Kvamme NH, Refsnes PE, Kadi F, Raastad T. Dissimilar effects of one- and three-set strength training on strength and muscle mass gains in upper and lower body in untrained subjects. J Strength Cond Res. 2007;21:157–63. doi: 10.1519/00124278-200702000-00028. [DOI] [PubMed] [Google Scholar]
- 45.McBride JM, Blaak JB, Triplett-McBride T. Effect of resistance exercise volume and complexity on EMG, strength, and regional body compositon. Eur J Appl Physiol. 2003;90:626–32. doi: 10.1007/s00421-003-0930-3. [DOI] [PubMed] [Google Scholar]
- 46.Marx JO, Ratamess NA, Nindl BC, Gotshalk LA, Volek JS, Doi K, et al. Low-volume circuit versus high-volume periodized resistance training in women. Med Sci Sports Exerc. 2001;33:635–43. doi: 10.1097/00005768-200104000-00019. [DOI] [PubMed] [Google Scholar]
- 47.Ryan AS, Pratley RE, Elahi D, Goldberg AP. Resistive training increases fat-free mass and maintains RMR despite weight loss in postmenopausal women. J Appl Physiol. 1995;79:818–23. doi: 10.1152/jappl.1995.79.3.818. [DOI] [PubMed] [Google Scholar]
- 48.Fleck SJ, Kraemer WJ. Designing resistance training programs. Human Kinetics; Champaign, IL: 2003. [Google Scholar]
- 49.Mazzetti SA, Kraemer WJ, Volek JS, Duncan ND, Ratamess NA, Gomez AL, et al. The influence of direct supervision of resistance training on strength performance. Med Sci Sports Exerc. 2000;32:1175–84. doi: 10.1097/00005768-200006000-00023. [DOI] [PubMed] [Google Scholar]
- 50.Donnelly JE, Hill JO, Jacobsen DJ, Potteiger JA, Sullivan D,K, Johnson SL, et al. Effects of a 16-month randomized controlled exercise trial on body weight and composition in young, overweight men and women. Arch Intern Med. 2003;163:1343–50. doi: 10.1001/archinte.163.11.1343. [DOI] [PubMed] [Google Scholar]
- 51.Treuth MS, Hunter GR, Kekes-Szabo T. Estimating intraabdominal adipose tissue in women by dual-energy X-ray absorptiometry. Am J Clin Nutr. 1995;62:527–32. doi: 10.1093/ajcn/62.3.527. [DOI] [PubMed] [Google Scholar]
- 52.Kim J, Heshka S, Gallagher D, Kotler DP, Mayer L, Albu J, et al. Intermuscular adipose tissue-free skeletal muscle mass: estimation by dual-energy X-ray absorptiometry in adults. J Appl Physiol. 2004;97:655–60. doi: 10.1152/japplphysiol.00260.2004. [DOI] [PubMed] [Google Scholar]
- 53.Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Human Kinetics Books; Champaign,Ill: 1988. [Google Scholar]
- 54.Consolazio CF, Matoush LO, Nelson RA, Torres JB, Isaac GJ. Environmental temperature and energy expenditures. J Appl Physiol. 1963;18:65–8. doi: 10.1152/jappl.1963.18.1.65. [DOI] [PubMed] [Google Scholar]
- 55.Berke EM, Gardner AW, Goran MI, Poehlman ET. Resting metabolic rate and the influence of pretesting environment. Am J Clin Nutr. 1992;55:626–9. doi: 10.1093/ajcn/55.3.626. [DOI] [PubMed] [Google Scholar]
- 56.Haugen HA, Melanson EL, Tran ZV, Kearney JT, Hill JO. Variability of measured resting metabolic rate. Am J Clin Nutr. 2003;78:1141–4. doi: 10.1093/ajcn/78.6.1141. [DOI] [PubMed] [Google Scholar]
- 57.Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9. doi: 10.1113/jphysiol.1949.sp004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Herd S, Vaughn W, Goran M. Comparison of zinc reduction with platinum reduction for analysis of deuterium-enriched water samples for the doubly-labeled water technique. Obes Res. 1999;8:302–8. doi: 10.1038/oby.2000.36. [DOI] [PubMed] [Google Scholar]
- 59.Elia M. Converting carbon dioxide production to energy expenditure. In: Prentice AM, editor. The doubly-labeled water method for measuring energy expenditure Technical recommendations for use in humans A consensus report by the IDECG working group. NAHRES-4; Vienna: 1990. pp. 193–211. [Google Scholar]
- 60.Westrate JA. Resting metabolic rate and diet-induced thermogenesis: a methodological appraisal. Am J Clin Nutr. 1993;58:592–601. doi: 10.1093/ajcn/58.5.592. [DOI] [PubMed] [Google Scholar]
- 61.Troiano RP, Berrigan D, Dodd K, Masse LC, Tilert T, MacDowell M. Physical activity in the United States measured by accelerometer. Medicine & Science in Sports & Exercise. 2008;40:181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 62.Hise ME, Sullivan DK, Jacobsen DJ, Johnson SL, Donnelly JE. Validation of energy intake measurements determined from observer-recorded food records and recall methods compared with the doubly labeled water method in overweight and obese individuals. Am J Clin Nutr. 2002;75:263–7. doi: 10.1093/ajcn/75.2.263. [DOI] [PubMed] [Google Scholar]
- 63.Grunwald GK, Sullivan D,K, Hise M, Donnelly JE, Jacobsen DJ, Johnson SL, et al. Number of days, number of subjects, and sources of variation in longitudinal intervention or crossover feeding trials with multiple days of measurement. Br J Nutr. 2003;90:1087–95. doi: 10.1079/bjn2003989. [DOI] [PubMed] [Google Scholar]
- 64.Tillotson JL, Gorder DD, DuChene AG, Grambsch PV, Wenz J. Quality control in the Multiple Risk Factor Intervention Trial Nutrition Modality. Control Clin Trials. 1986;7:66S–90S. doi: 10.1016/0197-2456(86)90160-1. [DOI] [PubMed] [Google Scholar]
- 65.Edwards JR, Lamebert LS. Methods for integrating moderation and mediation: a general analytic framework using moderated path analysis. Psychological Methods. 2007;12:1–22. doi: 10.1037/1082-989X.12.1.1. [DOI] [PubMed] [Google Scholar]
- 66.Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behav Res. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- 67.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Second Edition ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- 68.Van Etten LMLA, Westerterp KR, Verstappen FTJ, Boon BJB, Saris WHM. Effect of an 18-wk weight-training program on energy expenditure and physical activity. J Appl Physiol. 1997;82:298–304. doi: 10.1152/jappl.1997.82.1.298. [DOI] [PubMed] [Google Scholar]