Abstract
Mild Cognitive Impairment (MCI) affects 25% of older African Americans and predicts progression to Alzheimer's disease. An extensive epidemiologic literature suggests that cognitive, physical, and/or social activities may prevent cognitive decline. We describe the methods of a randomized clinical trial to test the efficacy of Behavior Activation to prevent cognitive decline in older African Americans with the amnestic multiple domain subtype of MCI. Community Health Workers deliver 6 initial in-home treatment sessions over 2-3 months and then 6 subsequent in-home booster sessions using language, materials, and concepts that are culturally relevant to older African Americans during this 24 month clinical trial. We are randomizing 200 subjects who are recruited from churches, senior centers, and medical clinics to Behavior Activation or Supportive Therapy, which controls for attention. The primary outcome is episodic memory as measured by the Hopkins Verbal Learning Test-Revised at baseline and at months 3, 12, 18, and 24. The secondary outcomes are general and domain-specific neuropsychological function, activities of daily living, depression, and quality-of-life. The negative results of recent clinical trials of drug treatments for MCI and Alzheimer's disease suggest that behavioral interventions may provide an alternative treatment approach to preserve cognition in an aging society.
Keywords: Clinical Trial, Prevention, Cognitive Decline, Mild Cognitive Impairment, Alzheimer's disease, African Americans
1. Introduction
This clinical trial will determine whether increasing participation in cognitive, physical, and/or social activities prevents cognitive decline in older African Americans with Mild Cognitive Impairment (MCI). MCI is a transition state between normal aging and dementia that affects 10% to 20% of older persons and predicts progression to dementia, particularly Alzheimer's disease (AD).1-6 African Americans are more likely to have MCI and AD than Whites, possibly because comorbid medical problems (e.g., diabetes, hypertension), disparities in access to health care, fewer years of education of uncertain quality, scarce economic resources, and limited opportunities to pursue leisure activities increase their risk.7-10 One study found that nearly 1 in 4 older African Americans have a mild degree of cognitive dysfunction.11 Thus, there is a pressing need to develop interventions to prevent cognitive decline in this high risk population.
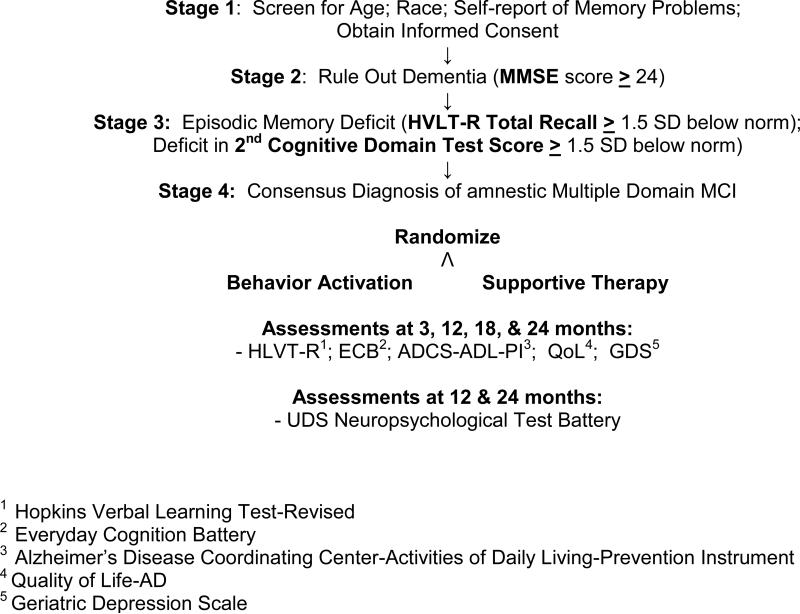
An extensive epidemiologic literature suggests that participation in stimulating activities in late life may prevent cognitive decline.12-32 However, no randomized controlled trials have demonstrated this. We are testing the efficacy of Behavior Activation (BA), which increases participation in self-identified meaningful activities, to prevent cognitive decline in older African Americans with the amnestic multiple domain subtype of MCI (aMCIMD).33-35 We are targeting persons with this MCI subtype because they are at high risk for progression to AD.36-42 We are recruiting subjects from multiple sites (e.g., churches, senior centers, senior high rise apartment houses, and primary care medical practices) that predominately serve older African Americans and will randomize 200 older African Americans with aMCI-MD to BA or Supportive Therapy (ST), which is an attention control treatment.43, 44 Community Health Workers will deliver 6 initial in-home BA or ST treatment sessions over 2-3 months and then 5 subsequent in-home booster sessions (one session every 3 months) using language, materials, and concepts that are culturally relevant to older African Americans during this 24 month clinical trial. Figure 1 depicts the study flow chart.
Figure 1.
Study Flow Chart
The primary outcome is preventing a decline in episodic memory as measured by the Hopkins Verbal Learning Test-Revised (HVLT-R) at baseline and at months 3, 12, 18, and 24.45 We will compare the proportion of subjects in the 2 treatment groups who decline by ≥ 6 points on the HVLT-R over 24-months. A 6-point decline on the HVLT-R translates clinically to the loss of ability to perform an instrumental activity of daily living task.46 We hypothesize that 20% of BA-treated subjects, compared to 40% of ST controls, will decline to that extent over 24 months. The assessments at months 3, 12, 18, and 24 will enable us to characterize rates and trajectories of cognitive change as a subsidiary approach to assess BA's efficacy. The secondary outcomes are general neuropsychological function, difficulty with instrumental activities of daily living, depression, and quality-of-life. We hypothesize that BA-treated subjects will have fewer declines in cognitive and functional abilities, fewer depressive symptoms, and better quality of life than ST-treated subjects at 24 months. In exploratory analyses we will determine whether increasing participation in activities mediates BA's treatment effect.
2. Study Design
The study design is innovative for several reasons: 1) it is the first rigorously designed RCT to determine whether participation in cognitive, physical, and/or social activities prevents cognitive decline; 2) it targets African Americans, whose risk for cognitive decline is especially high; and 3) it employs a prevention design,which is important given the high risk of progression from MCI to AD. Treatment for the latter is complex, costly, only partly effective, and more difficult for African Americans to access. Thus, preventing new cases may be more effective than waiting to treat patients who already have AD; 4) it tests a nonpharmacologic intervention that resonates with the coping strategies of older African Americans;47-49 5) it tests an intervention that increases participation in activities that subjects value. Whereas previous studies have prescribed specific cognitive or physical exercises, ours is the first that is tailored to meet individuals’ preferences;17,50, 51 6) it targets persons with the amnestic multiple domain subtype of MCI, who are at greatest risk for cognitive decline.36-42 7) it employs a community-based strategy to recruit subjects, deliver the intervention, and assess outcomes. This approach increases access to care and may lead to greater cooperation, better assessments of daily functioning, and lower attrition rates; and 8) it addresses the issue of equipoise in AD prevention research. Although epidemiological studies suggest that activities reduce the risk of cognitive decline, genuine uncertainty remains. This clinical trial will provide new knowledge on this issue as it employs both a rigorous research design and a practical care model that is standardized and reproducible.
The study inclusion criteria are: 1) African-American race; 2) Age ≥ 65 years; and 3) Amnestic MCI-Multiple Domain. To meet the latter criterion subjects will have self-reported memory decline, preserved general cognition, no functional disability due to memory impairment, scores less than 1.5 standard deviations (SD) on age-, education-, and race-adjusted norms on the HVLT-R, and scores ≤ 7th percentile or ≤ 1.5 SD on neuropsychological tests assessing a second cognitive domain. We use the Uniform Data Set neuropsychological test battery to identify possible deficits in language, executive function, and/or visuospatial perception.52 For language, the battery includes the Boston Naming and Category Fluency Tests;53 for executive function, Trailmaking Test Part B;54 and for visuospatial skills WAIS-R Digit Symbol55 and Trailmaking Test Part A.54 The exclusion criteria are: 1) Axis I DSM-IV psychiatric diagnosis (e.g., Major Depression, Dementia); 2) sensory deficits that preclude neuropsychological testing; 3) reduced life expectancy; and 4) institutional residence.
We are recruiting 200 subjects from 3 large senior centers, senior high rise apartment buildings, area churches that serve older African Americans, and Jefferson's homecare network and family medicine and internal medicine clinics. The senior centers and high rise apartment buildings serve over 10,000 older African Americans and the medical and home care programs include about 2,000 more. Available literature suggests that about 20% of persons at these sites have MCI, yielding a sufficient number for study.3,42 To recruit the sample, community health workers and community partners at senior centers and churches deliver memory awareness programs, set up information booths and posters, and screen interested persons. We also advertise in local newspapers and mail introductory letters to patients who attend the medical clinics and who receive homecare. We also take the following steps to promote recruitment: 1) Community Health Workers (CHW) who are concordant to subjects in language, race/ethnicity, and community of origin conduct recruitment; and 2) we offer $20 to subjects to complete the baseline and follow-up assessments at months 3, 12, 18, and 24. To identify the sample we conduct a 4-stage screening process:
Stage 1
We identify persons who report memory problems and recall fewer than 5 of 12 items on Trial 1 of the HVLT-R (immediate recall). The average score for African Americans ages 60-71 is 4.4 (SD 1.3).56 For these potential subjects, a community health worker schedules an in-home visit to obtain the subject's informed consent. During the informed consent process we state that the study's purpose is to learn more about ways to prevent memory loss in older African Americans who are already starting to notice mild memory problems, and that we are comparing BA and ST to determine whether one or both of these treatments are effective. We indicate that BA aims to increase participation in activities and that ST provides subjects an opportunity to talk about one's life and issues of aging. Jefferson's Institutional Review Board approved this approach to contacting and consenting patients for research participation.
Stage 2
To rule out global cognitive impairment, the CHW administers the Mini-Mental Status Examination (MMSE).57 Callahan et al (2002) found that a MMSE ≤ 24 had a negative predictive value of 99.9% in an urban community sample of AAs.58 The CHW also administers the Alzheimer's Disease Cooperative Study Activities of Daily Living–Prevention Instrument97 to confirm that subjects have no substantial impairment in activities of daily living due to cognitive problems before proceeding to Stage 3 Screening.
Stage 3
To identify persons with possible amnestic multiple domain MCI, the CHW administers the HVLTR, the Uniform Data Set neuropsychological test battery, and other clinical measures (see ahead).
Stage 4
To confirm the diagnosis of aMCI-MD, the investigators review all clinical information to determine whether a subject meets eligibility criteria. We then randomize eligible subjects to the 2 study interventions.
Randomization follows a fixed scheme with a 1:1 allocation ratio to the 2 study groups. We use a random numbers table to assign subjects and base the schedule on a permuted random block design (with randomly chosen block sizes) to ensure balance between treatment groups on enrollment time.
3. Conceptual Framework
We based this trial on the Disablement Process Model, which is a sociomedical model that describes how medical diseases affect functioning in specific body systems and lead to disability.59 The model posits that disability is part of a complex relationship between health conditions and contextual (i.e. environmental and personal) factors. In this model, aMCI-MD, as a possible preclinical AD state, reflects a physiologic dysfunction that results in diminished memory and initiative (disability), where environmental factors (i.e., activity participation) may “speed up” or “slow down” this core pathway. We propose to increase activity levels and thereby “slow down” progression to disability.
4. Sample Size Calculation
The primary outcome is a ≥ 6 point decline in Total Recall on the Hopkins Verbal Learning Test-Revised (HVLT-R) by month 24. To power this study we first estimated the expected rate of decline in African American controls. Two previous studies reported that 34.6% and 41.8% of older, cognitively normal African Americans experienced a clinically significant cognitive decline over 2 and 3 years, respectively.10, 60 We anticipate a higher rate of decline in subjects with aMCI-MD because their already impaired cognition confers a greater risk of further decline. Based on these data, we project that 40% of controls will decline by ≥ 6 points over 2 years on HVLT-R Total Recall measure. To estimate the rate reduction associated with BA, we looked to published effect sizes of behavioral interventions to improve cognition in persons with MCI. The effect sizes ranged from 0.55 – 1.12.61-64 Based on these data we hypothesize that BA-treated subjects will experience half the rate of decline as controls. Assuming an incidence rate of cognitive decline of 40% in controls, a relative risk of 0.5 (20% incidence in the BA group) is equivalent to an effect size of approximately 0.45. This translates to a number needed to treat of 5 subjects to prevent 1 case of cognitive decline (1/ (40% - 20%) =5.0).
We powered the study to detect an overall 50% reduction in risk of decline (RR=0.5) for the primary outcome using a generalized linear model for binomial data with a log link. We anticipate an attrition rate of 20% over 2 years. Drawing from the same recruitment sites as we propose in this study, the attrition rate in a previous study of an in-home behavioral intervention was 6% at 6 months and 11% at 12 months.65 In Fried et al's (2004) “Experienced Corps Intervention”, which was a volunteer program to increase physical and cognitive activity of older African Americans, the attrition rate was 11.4% over 7 months.66 In a related program for older African American women, the attrition rate was 15.5% over 3 years.67 These data suggest that stimulating activity programs, particularly for older African Americans, have relatively low attrition rates even out to 3 years. Allowing for a 20% attrition rate by 24 months, we are randomizing 200 subjects and expect to have complete data on 160 subjects at 24 months. With an expected rate of decline in the ST group of 40% at 24 months, we will have 80% power to detect a relative risk of 0.5 using a two-sided test with alpha=0.05.
5. Study Treatments
A. Behavior Activation (BA)
BA is a manual-based, behavioral treatment that helps people increase activity levels through goal setting, activity scheduling, graded task assignment, identifying avoidant behaviors, and rating one's sense of accomplishment.33-35 We designed the BA treatment protocol to specifically counter the behavioral and cognitive deficits of aMCI-MD. The latter include memory dysfunction plus language, executive, and/or visuospatial dysfunction. These deficits lead to difficulty recalling recent events, grasping explanations, solving practical problems, and finding one's way in familiar environments. These deficits also compromise one's ability to capably pursue cognitive, social, and physical activities. MCI's behavioral deficits (e.g., apathy, depression) further diminish activity participation as initiative, self confidence, and mood decline.
BA prevents this downward spiral by providing a structured approach to compensate for MCI symptoms. Using visual cues, written schedules, and step-by-step sequencing, BA may enable persons with MCI to increase activity levels with beneficial effects on memory. BA does not specify what behaviors to activate; instead it encourages patients to choose activities based on their interest, access, and feasibility. This flexibility allows patients to develop treatment plans that accord with their specific values and beliefs, and thereby enhances BA's cultural relevance. BA may be especially relevant to low-income African Americans whose life circumstances necessitate a present-time oriented, practical, and problem-centered treatment approach.68--70 Although different subjects may choose different activities, BA delivers an identical treatment approach to all subjects.
The BA CHW meets with subjects in their homes to help subjects develop strategies to: 1) maintain participation in activities that they currently pursue; 2) encourage participation in activities that they are withdrawing from; 3) renew participation in activities that they have given up; or 4) engage in new activities. Although the CHW encourages subjects to formulate their own goals, the CHW will ensure that they are feasible. For example, the CHW may break down goals to smaller, more manageable tasks. He/she may suggest strategies for task modification or substitution when physical limitations interfere with a desired activity (e.g., reorganize kitchen to allow for navigating with a walker). Because all subjects have memory deficits, the CHW provides visual cues and reminders (e.g., lists of treatment goals from session to session) and recommend organizational strategies (e.g., put keys, wallet in same place) to support initiation, sequencing, and integration. The CHW also creates charts depicting the sequence of steps to follow to achieve a goal. For subjects with language deficits, the CHW teaches visual cueing techniques to aid verbal expression.
1) Session 1
In the first session the CHW establishes rapport, explains the intervention, and helps the subject formulate initial activity goals. The CHW begins by introducing the importance of activity engagement, healthy lifestyle behaviors, and maintaining optimal brain health. The CHW presents this material in a culturally sensitive format, with careful consideration of subject's cultural preferences, literacy, and cognitive capabilities. The CHW then reviews the subject's life long interests, hobbies, social relationships, physical activity levels, spiritual and religious activities, and intellectual pursuits using a semi-structured questionnaire. Then the CHW asks the subject to describe how he or she now spends a typical day. The CHW then encourages the subject to set new specific Activity Goals. The goals need to be activity-based (i.e., knit half an hour per day, go to church), readily observable, and quantifiable. In selecting activity goals, the CHW reviews the activity programs at local senior centers although subjects may choose activities elsewhere. When setting the activity goals, the CHW encourages subjects to participate in the activity at least twice weekly (either the same activity twice weekly or 2 distinct activities once weekly) and more often if possible. We based this minimum activity dose on previous studies that have found that twice weekly activity is the minimum level necessary to strengthen cognitive reserve.12-14 The Activity Goals are recorded and monitored on a Master Activity Log. This Log lists: 1) each activity the subject will pursue; 2) the ideal number of times to engage in the activity each week; and 3) the actual number of times and when the subject engaged in the activity; and rates: 4) how she/he felt while doing the activity; and 5) the activity's degree of difficulty. In this way the Master Activity Log provides a weekly summary of all activities for the subject and CHW to review in subsequent treatment sessions.
Next the CHW helps the subject delineate the steps he or she will take to implement the Activity Goal. For example, if the goal is “getting together with a friend” the steps may include: 1) choose whom to call; 2) pick a date and time; 3) look up phone number; and 4) make the call. Reminders are embedded in the steps (e.g., set timer to ring 30 minutes before social event, write upcoming tasks on calendar).
2) Sessions 2-6
The CHW begins subsequent sessions by assessing subjects’ progress towards achieving their goals from previous sessions. Reviewing the Master Activity Log standardizes this process. The CHW provides positive reinforcement for goals that subjects achieved. The CHW asks subjects to describe their feelings in meeting their goals in order to link activity with positive affect. The CHW encourages the subject to increase, if possible, the amount of time that he/she participates in an activity (e.g., walk 5X /week instead of 3X, go to senior center 2X/week instead of once), or to target new activities in other domains. If goals were not met (or partially met), the CHW and subject discuss barriers and problem-solve ways to overcome them. If the CHW determines that the goal was unrealistic, he/she suggests similar yet easier activities (e.g., puzzle with fewer pieces, more simple knitting pattern, less strenuous exercise). The CHW reinforces the basic principles of BA, especially the importance of an active life style. Then the CHW and subject update the Master Activity Log to set new goals for the upcoming week.
3) Maintenance (“Booster”) Sessions (Months 6, 9, 12, 15, 18, and 21)
To optimize treatment effects, the CHW administers 6 in-home maintenance sessions during the study to reinforce continued participation in activities. At each maintenance session, the CHW reviews the previous Master Activity Log and updates the upcoming Master Activity Log to document activity plans for the next 3 months. Scheduling future appointments, meeting regularly over time, and remaining engaged with subjects increase the likelihood that they will sustain behavioral changes (i.e., remain active) and will also reduce attrition. If new or worsening cognitive or physical deficits arise and/or significant changes to a subject's social milieu occur (e.g., death of a spouse), the CHW suggests strategies to make task completion easier or suggest new activities.
B. Supportive Therapy (ST)
ST controls for the nonspecific elements of the CHWs’ contact with subjects in the BA treatment group. It is a fully-structured, nondirective, supportive psychological treatment that facilitates personal expression and conveys empathy, respect, and optimism.43,44 ST resembles BA in all ways but for BA's activation strategies. Both BA and ST are fully manualized, similar in dose and intensity of attention (i.e. number and duration of sessions), and delivered by rigorously trained therapists. Unlike BA, ST contains no active elements beyond its nonspecific components. Its techniques include active listening, open questioning, reflecting back, and summation. Although social attention itself may have benefits, we nevertheless consider ST a placebo because it has no theoretical basis or lasting effects to prevent memory decline.43,44
1) ST In-Home Visits 1-6 and Booster Sessions
In the first session, the CHW discusses ST's purpose, which is to explore the impact of aging and memory loss on the subject's life. The goals are to facilitate discussion of the subject's life situation in relation to growing older and relevant issues such as illness, disability, retirement, and social isolation. In contrast to the BA intervention, the CHW does not discuss the importance of activities or make any attempt to increase them. In subsequent sessions, ST facilitates and deepens knowledge about the subject's life situation in relation to his or her memory and other life difficulties. Therapists create an accepting, non-judgmental, empathic environment, by using supportive statements, reflective listening, and empathic communications. Direct suggestions about ways to stay active or preserve cognition are prohibited. Although ST is an activity during the time that it is delivered, its effects are transient and not associated with meaningful improvement.43,44
6. Study Measures
A. Personal Characteristics
At baseline we obtain data on age, sex, education, marital status, living arrangements, occupation, socioeconomic status, and alcohol use. We ask subjects whether they identify themselves as “African American,” “black”, “black American”, or black/Caribbean”. We also assess literacy, which is defined as reading level and measured using the Reading Recognition Subtest of the Wide Range Achievement Test-Version 3.71 Manly et al (2004) have argued that literacy, as a proxy for education quality and cognitive reserve, strongly influences cognitive test results and may be a risk factor for cognitive decline.7
B. Medical Status
We use the Chronic Disease Score and the Multilevel Assessment Inventory Health Conditions Check List to quantify medical comorbidity at baseline and at months 3, 12, 18, and 24.72, 73 We also use these instruments to identify changes in health status and medical treatments during the study.
C. Outcome Measures
We selected outcome measures with known reliability and validity, sensitivity to change and, for the neuropsychological tests, normative scores for African Americans. A CHW administers these measures at baseline and months 3, 12, 18, and 24 masked to treatment assignment.
1. Primary Outcome Measure
We chose episodic memory as the primary outcome because deficits in this domain predict dementia in persons with MCI and small clinical trials suggest that behavioral interventions preserve episodic memory;36-42, 74, 75 To measure episodic memory, we administer the Hopkins Verbal Learning Test-Revised (HVLT-R). The HVLT is a widely used, brief, word-list learning and memory test that has age, education, and gender-adjusted norms for older African Americans.45, 56, 76 Benedict et al (1998) and others have established its test-retest reliability and validity in patients with AD, MCI, and normal controls.45, 77-79 Longitudinal studies demonstrate its sensitivity to change.78, 79 Six equivalent forms are used to reduce practice effects.45 We administer HVLT version #1 at baseline and alternate versions thereafter so no single version is administered on consecutive test occasions.
The HVLT-R consists of a 12 item-word list presented in 3 consecutive learning trials. The Total Recall score is the sum of the 3 learning trials; scores range from 0 – 36. The Delayed Recall score is the number of correctly recalled words 20 minutes later; scores range from 0 – 12. We use a decline ≥ 6 in Total Recall score as the primary outcome measure and will compare the proportion of subjects in the 2 treatment groups who decline to that extent over 24 months. A decline of ≥ 6 in Total Recall translates clinically to an important functional decline (i.e., the loss of ability on a medication, telephone, or financial management task).46 In the inception sample to develop the HVLT, a 6 point change also represented the Reliable Change Score (i.e., a significant change over and above measurement error and practice effects).45 In patients with Clinical Dementia Rating scores of 0.5 (which is often taken to represent MCI), their average HVLT-R Total Recall score was 13.95 (6.11).45 This indicates that at study entry subjects will have a sufficient range of scores to avoid floor effects in the detection of a decline of ≥ 6 in Total Recall score by 24 months. We also plan subsidiary analyses to assess BA's efficacy using mixed effects models to compare rates and trajectories of change in HVLT-R scores over time in the 2 treatment groups. As a continuous measure, a 1 standard deviation (SD) change in Total Recall score is associated with a 1.58% decline in function over 5 years.45
2. Secondary Outcome Measures
a. Uniform Data Set (UDS) Neuropsychological Battery
The National Institute on Aging-funded Alzheimer's Disease Centers developed this battery to distinguish individuals with MCI and mild AD from non-demented older persons.52 Data on over 1,300 subjects attest to its feasibility and validity. The battery assesses the cognitive domains necessary to identify MCI subtypes, provides a uniform, stable threshold for MCI and dementia over time, and facilitates comparisons with other subjects. Most tests have age- and education-adjusted normative scores for African Americans.80-83 We administer the UDS battery at baseline and months 12 and 24. At these time points, we compute standardized scores (z scores) for each test in each cognitive domain (e.g., Attention, Semantic Memory/Language, Psychomotor Speed, Visuospatial Function, Executive Function) using the baseline population means and standard deviations. For domains that include more than one test, we average the standardized scores to yield a single composite score. We also average the standardized scores of all tests into a single composite measure of global cognition.
b. Everyday Cognition Battery (ECB)84
This objective performance-based memory test assesses medication use, financial management, and nutrition and food preparation. The test includes 2 standardized stimuli for each of 3 domains (e.g., a sample medication label for medication use; a checking account statement for financial management; food label for nutrition/food preparation). Scores range from 0 to 30 with higher scores indicating better function. Participants first study real-world printed material such as a medication label or a food label. After the material is removed, the examiner asks, “What dosage should have been taken?” or “How many calories does this product have per serving?” An item is scored 1 if correctly answered and 0 if incorrectly answered. The mean score within each domain produces a domain-specific subscale score.
c. Alzheimer's Disease Cooperative Study Activities of Daily Living–Prevention Instrument (ADL-PI)
We also assess participants’ subjective ratings of daily functioning using the ADL-PI, which contains 15 ADL and 5 physical function questions.85 The latter assess physical factors (e.g., vision and hearing) that may affect function. The ADLs cover performance of complex instrumental activities over the past 3 months (e.g., handling money, shopping, preparing food, doing housework). The ADL-PI uses a standardized, symmetrical set of descriptions of each level of performance for each activity, with higher scores representing better performance.
d. Quality-of-Life (QOL)
We are using the Quality of Life-AD, which is a reliable and valid measure of QOL that has been used in subjects with normal cognition, MCI, and AD.86 On a 4-point scale (excellent to poor), subjects rate 13 QOL domains (e.g., physical health, energy level and mood). Total scores range from 13 to 52, with higher scores indicating better life quality.
e. Depression and Neuropsychiatric Symptoms
We assess these symptoms to determine if BA prevents worsening noncognitive symptomotology. We administer the Geriatric Depression Scale and questions to assess self-reported symptoms such as hallucinations and delusions.87
3. Mediating Variable (Activity Participation)
We assess subjects’ participation in cognitive, physical, and/or social activities over the 2 year study period using the Florida Cognitive Activities Scale,_the Barnes et al (2004) social activities items, and the Sturman et al (2005) physical activity items.19, 27, 88 We gather these data at baseline and months 3, 12, 18, and 24 to track activity participation and change over time. We have not powered this study to address whether specific types of activity have specific treatment effects. BA's intent is to increase activity in any of the 3 domains. We will have the ability, however, to compare the relative benefits of increases in one type of activity with another.
4. Process Variables
Both the BA and ST therapists will document the number and duration of treatment sessions, subject adherence, and the extent and quality of family involvement. The BA therapist will record details of each treatment session on a Master Activity Log. This includes the subject's treatment goals, the frequency the subject plans to engage in the goal, steps to achieve each goal, and actual goal completion. Subjects in both treatment groups will also rate their satisfaction with the respective treatments they receive.
7. Procedures to Maintain Masking
Behavioral intervention trials differ from other clinical trials in medicine in that double-blind administration of treatments is impossible: therapists are aware of what treatment they deliver as are the subjects. Recognizing this, procedures have been developed to ensure structural equivalence of treatments and to assess and maintain treatment fidelity and differentiability. A CHW who is masked to treatment assignment obtains all outcome data during in-home interviews. The CHW instructs subjects to reveal nothing about the treatments they may have received. We require that central data collection, measurement, and data entry procedures are made by persons masked to treatment assignment; only the project director, statistician, and therapists are aware of treatment assignment.
8. Treatment Fidelity
We have developed extensive training protocols to ensure proper implementation of the study interventions. Both interventions are manual driven; thus training concentrates on adhering to the respective manuals. The training protocols include didactic sessions, reviewing the treatment manuals, and supervised role-playing and actual training cases. We record all treatment sessions and review the audio-tapes of 30% of randomly selected subjects for treatment fidelity assessments. We ensure that the BA and ST therapists do not discuss with each other their respective interventions. The CHW therapists all have bachelor's level education and deliver both treatment interventions. This approach avoids confounding treatment outcomes with therapist traits; close fidelity monitoring prevents bias due to contamination in the delivery of the respective treatments.
9. Data Analysis
We will use an intent-to-treat approach for all analyses in that we include all subjects with follow-up data regardless of the extent to which they received treatment. The primary outcome measure is a dichotomous variable based on the HVLT-R Total Recall measure (i.e., loss of ≥ 6 points) at 3, 12, 18, and 24 months. The primary research question of BA's efficacy drives our decision to use a categorical index of cognitive change rather than a continuous measure of cognitive symptoms as the primary outcome measure. The categorical approach seems best suited to assess the efficacy of a clinical treatment, generating, as it does, an outcome with discernable prognostic implications. Were we to rely on a gradation of symptoms as the primary outcome measure, we would obtain only a relative, not an explicit, sense of the efficacy of BA that may lack clinical meaning. Thus, we hypothesize that BA-treated subjects will have a lower risk of decline at all post-treatment measurements compared to ST-treated subjects. We will use a generalized linear model for binomial outcomes assuming a log link function to directly model the relative risk of BA vs. ST. We will use Generalized Estimating Equations (GEE) methods to account for correlation among the 4 repeated post-treatment measurements for each subject. We will also examine whether BA slows the progression of cognitive decline by month 24, regardless of whether an individual subject exhibits a particular level of decline. We will evaluate this by examining the slopes of HVLT-R Total Recall scores over time using a repeated measures mixed effects linear regression model. To determine whether increasing participation in activities mediates BA's treatment effects, we will use Baron and Kenny's 3-step approach to test for mediation effects.89
10. Discussion
MCI is a serious public health problem for everyone. As a possible prelude to AD, it portends increasing caregiver burden, costly and complicated medical care, and nursing home placement.90 There is no effective treatment for MCI and new drug development faces substantial scientific obstacles.91, 92 An extensive epidemiologic literature, however, suggests that cognitive, physical, and social activities may prevent cognitive decline.12-32 This clinical trial is the first large-scale study to determine whether increasing activity participation prevents cognitive decline in older African Americans. Although this initial step is promising, additional work will be needed to define how best to disseminate and implement activity interventions to prevent cognitive decline if this trial is positive. Nevertheless, a positive finding would have broad significance to the field. To African American community leaders, it w ould demonstrate their capacity to improve their populations’ health status through formal linkages w ith the medical community. To neurobiologists, it would highlight the environment's effect on cognition and spur efforts to define the cerebral mechanisms that underlie cognitive reserve (i.e., brain's use of compensatory cognitive processes). To public health researchers, it would provide a model for culturally relevant interventions to address other diseases that disproportionately affect African Americans such as asthma and hypertension. Finding ways to prevent cognitive decline, even temporarily, are needed to address a public health crisis that is now upon us and to avert the larger one that awaits us.93 An estimated 5.3 million Americans currently have AD and many millions more have MCI.90 Their numbers will increase dramatically as the population ages. Besides getting older, our society is also getting more diverse racially and culturally. For older African Americans, who comprise one of the fastest growing minority groups, the diagnosis of AD comes at more advanced stages when care is costlier and outcomes less promising.94, 95 Given the enormous personal and societal costs of AD, especially as it affects older African Americans, demonstrating that a culturally relevant, nonpharmacological intervention prevents cognitive decline would boost public health efforts to encourage all older persons to pursue active lifestyles. The importance and impact of such an effort are magnified by the negative results of recent clinical trials of drug treatments for MCI and AD.91, 92, 96 In light of these facts, behavioral interventions currently may hold the best hope for preserving cognition in an aging society.
Acknowledgement
This research is supported by grant 1R01AG035025-01A1 from the National Institute on Aging. ClinicalTrials.gov Identifier: NCT01299766
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: None of the authors have any conflicts to report.
Bibliography and References Cited
- 1.Petersen RC, Roberts RO, Knopman DS, Boeve BF, Geda YE, Ivnik RJ, Smith GE, Jack CR. Mild cognitive impairment: ten years later. Arch Neurol. 2009;66:1447–1455. doi: 10.1001/archneurol.2009.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manly JJ, Bell-McGinty S, Tang M-X, Schupf N, Stern Y, Mayeux R. Implementing diagnostic criteria and estimating frequency of mild cognitive impairment in an urban community. Arch Neurol. 2005;62:1739–1746. doi: 10.1001/archneur.62.11.1739. [DOI] [PubMed] [Google Scholar]
- 3.Unverzagt FW, Gao S, Lane KA, Callahan C, Ogunniyi A, Balyewu O, Gurieje O, Hall KS, Hendrie HC. Mild cognitive dysfunction: An epidemiological perspective with an emphasis on African Americans. J Geriatr Psychiatry Neurol. 2007;20:215–226. doi: 10.1177/0891988707308804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plassman BL, Langa KM, Fisher GG, Heeringa SG, Weir DR, Ofstedal MB, Burke JR, Hurd MD, Potter GG, Rodgers WL, Steffens DC. Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med. 2008;148:427–434. doi: 10.7326/0003-4819-148-6-200803180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitchell AJ, Shiri-Feshki M. Temporal trends in the long term risk of progression of mild cognitive impairment: a pooled analysis. J Neurol Neurosurg Psychiatry. 2008;79:1386–1391. doi: 10.1136/jnnp.2007.142679. [DOI] [PubMed] [Google Scholar]
- 6.Farias S, Mungas D, Reed B, Harvey D, DeCarli C. Progression of mild cognitive impairment to dementia in clinic-vs community-based cohorts. Arch Neurol. 2009;66(9):1151–1157. doi: 10.1001/archneurol.2009.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manly JJ, Byrd D, Touradji P, Sanchez D, Stern Y. Literacy and cognitive change among ethnically diverse elders. International Journal of Psychology. 2004;39:47–60. [Google Scholar]
- 8.Demirovic J, Prineas R, Loewenstein D. Prevalence of dementia in three ethnic groups: The South Florida Program on Aging and Health . Ann Epidemiol. 2003;13:472–478. doi: 10.1016/s1047-2797(02)00437-4. [DOI] [PubMed] [Google Scholar]
- 9.Mehta KM, Simonsick EM, Rooks R, Newman AB, Pope SK, Rubin SM, Yaffe K. Black and White differences in cognitive function test scores: What explains the difference? J Am Geriatr Soc. 2004;52:2120–2127. doi: 10.1111/j.1532-5415.2004.52575.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shadlen MF, Siscovick D, Fitzpatrick AL, Duhlberg C, Kuller LH, Jackson S. Education, cognitive test scores, and black-white differences in dementia risk. J Am Geriatr Soc. 2006;54:898–905. doi: 10.1111/j.1532-5415.2006.00747.x. [DOI] [PubMed] [Google Scholar]
- 11.Unverzagt FW, Gao S, Baiyewu O, Ogunniyl AO, Gueje O, Perkins A, Emsley CT, Dickens J, Evans R, Musick B, Hall KS, Hui SL, Hendrie HC. Prevalence of cognitive impairment: data from the Indianapolis study of health and aging. Neurology. 2001;57:1655–1662. doi: 10.1212/wnl.57.9.1655. [DOI] [PubMed] [Google Scholar]
- 12.Akbaraly TN, Portet F, Fustinoni S, Dartigues JF, Artero S, Rouand O, Touchon J, Ritchie K, Berr C. Leisure activities and the risk of dementia in the elderly. Results from the Three-City Study. Neurology. 2009;73:854–861. doi: 10.1212/WNL.0b013e3181b7849b. [DOI] [PubMed] [Google Scholar]
- 13.Fabrigoule C, Letenneur L, Dartigues JF, Commenges D, Barberger-Gateau P. Social and leisure activities and risk of dementia: A prospective longitudinal study. J Am Geriatr Soc. 1995;43:485–490. doi: 10.1111/j.1532-5415.1995.tb06093.x. [DOI] [PubMed] [Google Scholar]
- 14.Fratiglioni L, Paillard-Borg S, Winblad B. An active and socially integrated lifestyle in late life might protect against dementia. Lancet Neurol. 2004;3:343–53. doi: 10.1016/S1474-4422(04)00767-7. [DOI] [PubMed] [Google Scholar]
- 15.Rockwood K, Middleton L. Physical activity and the maintenance of cognitive function. Alzheimer's & Dementia. 2007;3:S38–S44. doi: 10.1016/j.jalz.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Kramer A, Erickson K. Effects of physical activity on cognition, well-being, and brain: Human interventions. Alzheimer's and Dementia. 2007;3:S45–S51. doi: 10.1016/j.jalz.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 17.Lautenschlager N, Cox K, Flicker L. Effect of physical activity on cognitive function in older adults at risk for alzheimer's disease. A randomized trial. JAMA. 2008;300:1027–1037. doi: 10.1001/jama.300.9.1027. [DOI] [PubMed] [Google Scholar]
- 18.Larson EB. Physical activity for older adults at risk for alzheimer disease. JAMA. 2008;300:1077–1079. doi: 10.1001/jama.300.9.1077. [DOI] [PubMed] [Google Scholar]
- 19.Sturman MT, Morris MC, Mendes de Leon C, Biennis JL, Wilson RS, Evans DA. Physical activity, cognitive activity, and cognitive decline in a biracial community population. Arch Neurol. 2005;62:1750–1754. doi: 10.1001/archneur.62.11.1750. [DOI] [PubMed] [Google Scholar]
- 20.Verghese J, LeValley A, Derby C, Kuslansky G, Katz M, Hall C, Buschke H, Lipton RB. Leisure activities and the risk of amnestic mild cognitive impairment in the elderly. Neurology. 2006;66:821–827. doi: 10.1212/01.wnl.0000202520.68987.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carlson M, Helms M, Steffens DC, Burke JR, Potter GG, Plassman BL. Midlife activity predicts risk of dementia in older male twin pairs. Alzheimers & Dementia. 2008;4:324–331. doi: 10.1016/j.jalz.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson R, Mendes deLeon C, Barnes L, Barnes LL, Evans DA, Bennett DA. Participation in cognitively stimulating activities and risk of incident Alzheimer's disease. JAMA. 2002;287:742–748. doi: 10.1001/jama.287.6.742. [DOI] [PubMed] [Google Scholar]
- 23.Wilson RS, Bennett DA, Bienias JL, Mendes deLeon CF, Morris MC, Evans DA. Cognitive activity and cognitive decline in a biracial community population. Neurology. 2003;61:812–16. doi: 10.1212/01.wnl.0000083989.44027.05. [DOI] [PubMed] [Google Scholar]
- 24.Wilson RS, Bennett DA, Bienias JL, Aggarwal NT, Mendes de Leon CF, Morris MC, Schneider JA, Evans DA. Cognitive activity and incident Alzheiner's disease in a population-based sample of older persons. Neurology. 2002;59:1910–14. doi: 10.1212/01.wnl.0000036905.59156.a1. [DOI] [PubMed] [Google Scholar]
- 25.Wilson RS, Scherr PA, Schneider JA, Tang Y, Bennett DA. Relation of cognitive activity to risk of developing Alzheimer's disease. Neurology. 2007;69:1911–20. doi: 10.1212/01.wnl.0000271087.67782.cb. [DOI] [PubMed] [Google Scholar]
- 26.Barnes LL, Wilson RS, Mendes De Leon CF, Bennett DA. The relation of lifetime cognitive activity and lifetime access to resources to late-life cognitive function in older African Americans. Aging, Neuropsychology, and Cognition. 2006;13:516–528. doi: 10.1080/138255890969519. [DOI] [PubMed] [Google Scholar]
- 27.Barnes LL, Mendes de Leon CF, Wilson RS, Bienias JL, Evans DA. Social resources and cognitive decline in a population of older African Americans and whites. Neurology. 2004;63:2322–2326. doi: 10.1212/01.wnl.0000147473.04043.b3. [DOI] [PubMed] [Google Scholar]
- 28.Karp A, Paillard-Borg S, Wand H-X, Silverstein M, Winblad B, Fratiglioni L. Mental, physical and social components in leisure activities equally contribute to decrease dementia risk. Dement Geriatr Cogn Disord. 2006;21:65–73. doi: 10.1159/000089919. [DOI] [PubMed] [Google Scholar]
- 29.Niti M, Yap K-B, Kua E-H, Tan C-H, Ng T-P. Physical, social and productive leisure activities, cognitive decline and interaction with APOE-ε4 genotype in Chinese older adults. International Psychogeriatrics. 2008;20:237–251. doi: 10.1017/S1041610207006655. [DOI] [PubMed] [Google Scholar]
- 30.Kramer AF, Willis SL. Enhancing the cognitive vitality of older adults. Curr Dir Psychol Sci. 2002;11:173–176. [Google Scholar]
- 31.Baker LD, Frank LL, Foster-Schubert K, Green PS, Wilkinson CW, McTiernan A, Plymate SR, Fishel MA, Watson GS, Cholerton BA, Duncan GE, Mehta PD, Craft S. Effects of aerobic exercise on mild cognitive impairment. Arch Neurol. 2010;67:71–79. doi: 10.1001/archneurol.2009.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lackman ME, Agrigoroaei S, Murphy C, Tun PA. Frequent cognitive activity compensates for education differences in episodic memory. Am J Geriatr Psychiatry. 2010;18:4–10. doi: 10.1097/JGP.0b013e3181ab8b62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kanter JW, Manos RC, Bowe WM, Baruch DE, Busch AM, Rusch LC. What is behavioral activation? A review of the empirical literature. Clin Psychol Rev. 2010;30:608–620. doi: 10.1016/j.cpr.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 34.Cuijpers P, van Straten A, Warmerdam L. Behavioral activation treatments of depression: A meta-analysis. Clinical Psychology Review. 2007;27:318–326. doi: 10.1016/j.cpr.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 35.Quijano L, Stanley M, Petersen N. Healthy IDEAS: A depression intervention delivered by community-based case managers serving older adults. J Applied Gerontology. 2007;26:139–156. [Google Scholar]
- 36.Tyas SL, Salazar JC, Snowdon DA, Desrosiers MF, Riley KP, Mendiondo MS, Kryscio RJ. Transitions to mild cognitive impairments, dementia, and death: Findings from the nun study. Am J Epidemiol. 2007;165:1231–1238. doi: 10.1093/aje/kwm085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bäckman L, Jones S, Berger A-K, Laukka EJ, Small BJ. Cognitive impairment in pre-clinical Alzheimer's disease: A meta-analysis. Neuropsychology. 2005;19:520–531. doi: 10.1037/0894-4105.19.4.520. [DOI] [PubMed] [Google Scholar]
- 38.Howieson DB, Carlson NE, Moore MM, Wasserman D, Abendroth CD, Payne-Murphy J, Kaye JA. Trajectory of mild cognitive impairment onset. J International Neuropsychological Society. 2008;14:192–198. doi: 10.1017/S1355617708080375. [DOI] [PubMed] [Google Scholar]
- 39.Tabert MH, Manly JJ, Liu X, Pelton GH, Rosenblum S, Jacobs M, Zamora D, Goodkind M, Bell K, Stern Y, Devanand DP. Neuropsychological prediction of conversion to Alzheimer's disease in patients with mild cognitive impairment. Arch Gen Psychiatry. 2006;63:916–24. doi: 10.1001/archpsyc.63.8.916. [DOI] [PubMed] [Google Scholar]
- 40.Blacker D, Lee H, Muzikansky A, Martin EC, Tanzi R, McArdle JJ, Moss M, Albert M. Neuropsychological measures in normal individuals that predict subsequent cognitive decline. Arch Neurol. 2007;64:862–871. doi: 10.1001/archneur.64.6.862. [DOI] [PubMed] [Google Scholar]
- 41.Arnaiz E, Almkvist O, Ivnik RJ, Tangalos EG, Wahlund LO, Winblad B, Petersen RC. Mild cognitive impairment: A cross-national comparison. J Neurol Neurosurg Psychiatry. 2004;75:1275–1280. doi: 10.1136/jnnp.2003.015032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Manly JJ, Ming X-T, Schupf N, Stern Y, Vonsattel JP, Mayeux R. Frequency and course of mild cognitive impairment in a multiethnic community. Ann Neurol. 2008;63:494–506. doi: 10.1002/ana.21326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Borkovec T, Newman M, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. J Consulting & Clin Psych. 2002;70:288–298. [PubMed] [Google Scholar]
- 44.Noavalis PN, Rojcewicz SJ, Peele R. Clinical Manual of Supportive Psychotherapy. American Psychiatric Press; Washington, D.C.: 1993. [Google Scholar]
- 45.Benedict RHB, Brandt J. Manual: Hopkins verbal learning test-revised/Brief visuospatial memory test-revised. Psychological Assessment Resources; Lutz, FL: 1998. [Google Scholar]
- 46.Gross AL, Rebok GW, Unverzagt FW, Willis SL, Brandt J. Word list memory predicts everyday function and problem-solving in the elderly: results from the ACTIVE cognitive intervention trial. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. Mar. 2011;18(2):129–46. doi: 10.1080/13825585.2010.516814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bryant L, Corbett K, Kutner J. In their own words: a model of healthy aging. Social Science and Medicine. 2001;53:927–941. doi: 10.1016/s0277-9536(00)00392-0. [DOI] [PubMed] [Google Scholar]
- 48.Arean P, Ayalon LL, Hunkeler E, Lin EH, Tang L, Harpole L, Hendrie H, Williams JW, Jr, Unutzer J. Improving depression care for older, minority patients in primary care. Medical Care. 2005;43:381–390. doi: 10.1097/01.mlr.0000156852.09920.b1. [DOI] [PubMed] [Google Scholar]
- 49.Gitlin L, Houck W, Dennis M. Depressive symptoms in older African Americans and White adults with functional difficulties: the role of control strategies. J Am Geriatr Soc. 2007;55:1023–1030. doi: 10.1111/j.1532-5415.2007.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Willis SL, Tennstedt SL, Marsiske M, Ball K, Elias J, Koepke KM, Morris JN, Rebok GW, Unverzagf FW, Stoddard AM, Wright E, the ACTIVE study group Long-term effects of cognitive training on everyday functional outcomes in older adults. JAMA. 2006;296:2805–2814. doi: 10.1001/jama.296.23.2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Geda YE, Roberts RO, Knopman DS, Christianson TJ, Pankratz VS, Ivnik RJ, Boeve BF, Tangalos EG, Petersen RC, Rocca WA. Physical exercise, aging, and mild cognitive impairment. Arch Neurol. 2010;67(1):80–86. doi: 10.1001/archneurol.2009.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morris J, Weintraub S, Chui H, Cummings J, DeCarli C, Ferris S, Foster N, Galasko D, Graff-Radford N, Peskind E, Beekly D, Ramos E, Kukull W. The Uniform Data Set (UDS): Clinical and cognitive variables and descriptive data from Alzheimer's disease centers. Alzheimer Dis Assoc Disord. 2006;20:210–216. doi: 10.1097/01.wad.0000213865.09806.92. [DOI] [PubMed] [Google Scholar]
- 53.Welsh K, Butters N, Mohs R, et al. The consortium to establish a registry for Alzheimer's disease (CERAD). Part-V; A normative study of the neuropsychological battery. Neurology. 1994;44:609–614. doi: 10.1212/wnl.44.4.609. [DOI] [PubMed] [Google Scholar]
- 54.Armitage SSG. An analysis of certain psychological tests used in the evaluation of brain injury. Psych Mono. 1946;60:1–48. [Google Scholar]
- 55.Weschler D. Wechsler memory scale-revised. Psychological Corporation; New York: 1992. [Google Scholar]
- 56.Friedman M, Schinka J, Mortimer J, et al. Hopkins verbal learning test revised: norms for elderly African-Americans. The Clinical Neuropsychologist. 2002;16:356–372. doi: 10.1076/clin.16.3.356.13857. [DOI] [PubMed] [Google Scholar]
- 57.Folstein MF, Folstein SC, McHugh PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinicians. J. Psychiatric Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 58.Callahan C, Unverzagt F, Hui S. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 59.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 60.Black SA, Rush RD. Cognitive and functional decline in adults ages 75 and older. J Am Geriatr Soc. 2002;50:1978–1986. doi: 10.1046/j.1532-5415.2002.50609.x. [DOI] [PubMed] [Google Scholar]
- 61.Belleville S, Gilbert S, Fontaine F. Improvement of episodic memory in persons with mild cognitive impairment and healthy older adults: Evidence from a cognitive intervention program. Dement Geriatr Cogn Disord. 2006;22:486–499. doi: 10.1159/000096316. [DOI] [PubMed] [Google Scholar]
- 62.Greenaway MC, Hanna SM, Lepore SW, Smith GE. A behavioral rehabilitation intervention for amnestic mild cognitive impairment. Alzheimer Dis Assoc Disord. 2008;21:451–461. doi: 10.1177/1533317508320352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ishizaki J, Meguro K, Ohe K. Therapeutic psychosocial intervention for elderly subjects with very mild Alzheimer's Disease in a community: The Tajiri Project. Alzheimer Dis Assoc Disord. 2002;16:261–269. doi: 10.1097/00002093-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 64.Yi-jung Tsai A, Yang M-J, Lan C-F, Chen C-S. Evaluation of effect of cognitive intervention programs for the community-dwelling elderly with subjective memory complaints. Int J Geriatr Psychiaatry. 2008;23:1172–1174. doi: 10.1002/gps.2050. [DOI] [PubMed] [Google Scholar]
- 65.Gitlin LLN, Corcoran DM, Schinfeld S, Hauck WA. A randomized trial of multi-component home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc. 2006;54:809–816. doi: 10.1111/j.1532-5415.2006.00703.x. [DOI] [PubMed] [Google Scholar]
- 66.Fried LP, Carlson MC, Freedman M, Frick KD, Glass TA, Hill J, McGill S, Rebok GW, Seeman T, Tielsch J, Wasik BA, Zeger S. A social model for health promotion for an aging population: Initial evidence on the experience corps model. J Urban Health. 2004;81:64–78. doi: 10.1093/jurban/jth094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tan EJ, Rebok GW, Yu Q, Frangakis CE, Tang T, Ricks M, Tanner EK, McGill S, Fried LP. The long-term relationship between high-intensity volunteering and physical activity in older African American women. J Gerontol B Psychol Sci Soc Sci. 2009;64:304–11. doi: 10.1093/geronb/gbn023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ayalon L, Arean PA. Knowledge of Alzheimer's disease in four ethnic groups of older adults. Int J Geriatr Psychiatry. 2004;19:51–57. doi: 10.1002/gps.1037. [DOI] [PubMed] [Google Scholar]
- 69.Roberts JS, Connell CM, Cisewski D, Hipps YG, Demissie S, Green RC. Differences between African-Americans and Whites in their perceptions of Alzheimer's disease. Alzheimer's Disease and Associated Disorders. 2003;17:19–26. doi: 10.1097/00002093-200301000-00003. [DOI] [PubMed] [Google Scholar]
- 70.Hinton L, Franz CE, Yeo G, Levkof F. Conceptions of dementia in a multiethnic sample of family caregivers. J Am Geriatr Soc. 2005;53:1405–1410. doi: 10.1111/j.1532-5415.2005.53409.x. [DOI] [PubMed] [Google Scholar]
- 71.Wilkinson GS. Wide-Range Achievement Test. 3rd Edition Wide-Range, Inc.; Wilmington, DE: 1993. [Google Scholar]
- 72.Von Korff M, Wagner EH, Saunders K. A chronic disease score from automated pharmacy data. J Clin Epidemiol. 1992;45:197–203. doi: 10.1016/0895-4356(92)90016-g. [DOI] [PubMed] [Google Scholar]
- 73.Clark DO, Von Korff M, Saunders K, Baluch WM, Simon GE. A chronic disease score with empirically derived weights. Medical Care. 1995;33:783–795. doi: 10.1097/00005650-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 74.Unverzagt FW, Monahan PO, Moser LR. Effect of memory impairment on training outcomes in ACTIVE. J International Neuropsychological Society. 2007;13:799–806. doi: 10.1017/S1355617707071512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Belleville S, Chetrkow H, Gauthier S. Working memory and control of attention in persons with Alzheimer's disease and mild cognitive impairment. Neuropsychology. 2007;21:456–469. doi: 10.1037/0894-4105.21.4.458. [DOI] [PubMed] [Google Scholar]
- 76.Shapiro A, Benedict R, Schretlen D, Brandt J. Construct and concurrent validity of the Hopkins Verbal Learning Test-revised. The Clinical Neuropsychologist. 1999;13:348–358. doi: 10.1076/clin.13.3.348.1749. [DOI] [PubMed] [Google Scholar]
- 77.Kuslansky G, Katz M, Verghese J, Hall C, Lapuerta P, LaRuffa G, Lipton R. Detecting dementia with the hopkins verbal learning test and the mini-mental state examination. Arch Clin Neuropsychology. 2004;19:89–104. [PubMed] [Google Scholar]
- 78.Schrijnenaekers A, DeJager C, Hogrvorst E, et al. Cases with mild cognitive impairment and Alzheimer's disease fail to benefit from repeated exposure to episodic memory tests as compared with control. Journal of Clinical and Experimental Neuropsychology. 2006;23:438–455. doi: 10.1080/13803390590935462. [DOI] [PubMed] [Google Scholar]
- 79.de Jager CA. Changes over time in memory, processing speed and clock drawing tests help to discriminate between vascular cognitive impairment, mild cognitive impairment and Alzheimer's disease. Neurol Res. 2004;26:481–487. doi: 10.1179/016164104225016209. [DOI] [PubMed] [Google Scholar]
- 80.Lucas JA, Invik RJ, Smith GE, Ferman TJ, Willis FB, et al. Mayo's older African-American's normative studies: Norms for Boston naming test, controlled oralword association, category fluency, animal naming, token test, WRAT-3 reading, trail making test, stroop test, and judgment of line orientation. The Clinical Neuropsychologist. 2005;19:243–269. doi: 10.1080/13854040590945337. [DOI] [PubMed] [Google Scholar]
- 81.Unverzagt FW, Hall KS, Torke AM, et al. Effects of age, education, and gender on CERAD neuropsychological test performance in an African-American sample. Clin Neuropsychol. 1996;10:180–190. [Google Scholar]
- 82.Fillenbaum GG, Heyman A, Huber MS, Ganguli M, Unverzagt FW. Performance of elderly African American and White community residents on the CERAD neuropsychological battery. J International Neuropsychological Society. 2001;7:502–509. doi: 10.1017/s1355617701744062. [DOI] [PubMed] [Google Scholar]
- 83.Marcopulos BA, McLain C. Are our norms “normal”?: A 4-year follow-up study of a biracial sample of rural elders with low education. The Clinical Neuropsychologist. 2003;17:19–33. doi: 10.1076/clin.17.1.19.15630. [DOI] [PubMed] [Google Scholar]
- 84.Allaire JC, Gamaldo A, Ayotte BJ, Sims R, Whitfield K. Mild cognitive impairment and objective instrumental everyday functioning: the everyday cognition battery memory test. J Am Geriatr Soc. 2009;57(1):120–125. doi: 10.1111/j.1532-5415.2008.02054.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Galasko G, Bennett D, Sano M, Marson D, Kaye J, Edland SD. ADCS prevention instrument project: assessment of instrumental activities of daily living for community-dwelling elderly individuals in dementia prevention clinical trials. Alzheimer Dis & Assoc Disord. 2006;20:S152–S169. doi: 10.1097/01.wad.0000213873.25053.2b. [DOI] [PubMed] [Google Scholar]
- 86.Logsdon R, Gibbons L, McCurry M, et al. Quality of life in Alzheimer's disease: patient and caregiver forms. J Ment SCI. 1999;5:21–32. [Google Scholar]
- 87.Yesavage JA. Geriatric Depression Scale. Psychopharmacol Bull. 1988;24:709–711. [PubMed] [Google Scholar]
- 88.Dotson VM, Schinka JA, Brown LM, Mortimer J, Borenstein A. Characteristics of the Florida cognitive activities scale in older African Americans. Assessment. 2008;15:72. doi: 10.1177/1073191107307509. [DOI] [PubMed] [Google Scholar]
- 89.Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: Conceptual strategic and statistical considerations. J Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 90.2009 Alzheimer's Disease Facts and Figures. Alzheimer's and Dementia. 2009;5:234–70. doi: 10.1016/j.jalz.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 91.Green RC, Schneider LS, Amato DA, Beelen AP, Wilcock G, Swabb EA, Zavitz KH. Effect of tarenflurbil on cognitive decline and activities of daily living in patients with Alzheimer's disease. JAMA. 2009;203:2557–2564. doi: 10.1001/jama.2009.1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schneider LS, Sano M. Current Alzheimer's disease clinical trials: methods and placebo outcomes. Alzheimers and Dementia. 2009;5:388–397. doi: 10.1016/j.jalz.2009.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Brookmeyer R, Gray S. Methods for projecting the incidence and prevalence of chronic diseases in aging populations: Application to Alzheimer's disease. Statistics in Medicine. 2000;19:1481–1493. doi: 10.1002/(sici)1097-0258(20000615/30)19:11/12<1481::aid-sim440>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 94.Lilienfeld DE, Perl DP. Projected neurodegenerative disease mortality among minorities in the United States, 1990-2040. Neuroepidemiology. 1994;13:179–186. doi: 10.1159/000110377. [DOI] [PubMed] [Google Scholar]
- 95.Stephenson J. Racial barriers may hamper diagnoses: care of patients with Alzheimer's disease. JAMA. 2001;286:779–780. [PubMed] [Google Scholar]
- 96.Peterson RC, Thomas RG, Grundman M, Bennett D, Doody R, Ferris S, Galasko D, Jin S, Kaye J, Levey A, Pfeiffer E, Sano M, van Dyck CH, Thai LJ. Vitamin E and donepezil for the treatment of mild cognitive impairment. N Engl J Med. 2005;352:2379–2388. doi: 10.1056/NEJMoa050151. [DOI] [PubMed] [Google Scholar]