Abstract
Study Objective
Patients on warfarin or clopidogrel are considered at increased risk for traumatic intracranial hemorrhage (tICH) following blunt head trauma. The prevalence of immediate tICH and the cumulative incidence of delayed tICH in these patients, however, are unknown.
Methods
A prospective, observational study at two trauma centers and four community hospitals enrolled emergency department (ED) patients with blunt head trauma and pre-injury warfarin or clopidogrel use from April 2009 through January 2011. Patients were followed for two weeks. The prevalence of immediate tICH and the cumulative incidence of delayed tICH were calculated from patients who received an initial cranial computed tomography (CT) in the ED. Delayed tICH was defined as tICH within two weeks following an initially normal CT scan and in the absence of repeat head trauma.
Results
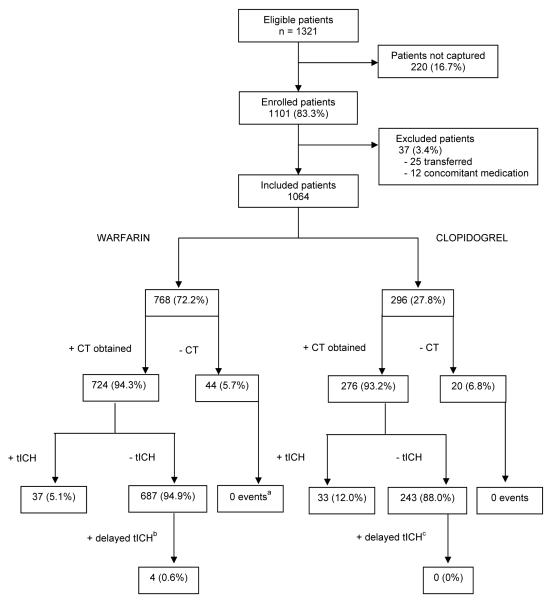
A total of 1,064 patients were enrolled (768 warfarin patients [72.2%] and 296 clopidogrel patients [27.8%]). There were 364 patients [34.2%] from Level 1 or 2 trauma centers and 700 patients [65.8%] from community hospitals. One thousand patients received a cranial CT scan in the ED. Both warfarin and clopidogrel groups had similar demographic and clinical characteristics although concomitant aspirin use was more prevalent among patients on clopidogrel. The prevalence of immediate tICH was higher in patients on clopidogrel (33/276, 12.0%; 95% confidence interval [CI] 8.4-16.4%) than patients on warfarin (37/724, 5.1%; 95%CI 3.6-7.0%), relative risk 2.31 (95%CI 1.48-3.63). Delayed tICH was identified in 4/687 (0.6%; 95%CI 0.2-1.5%) patients on warfarin and 0/243 (0%; 95%CI 0-1.5%) patients on clopidogrel.
Conclusion
While there may be unmeasured confounders that limit intergroup comparison, patients on clopidogrel have a significantly higher prevalence of immediate tICH compared to patients on warfarin. Delayed tICH is rare and occurred only in patients on warfarin. Discharging patients on anticoagulant or antiplatelet medications from the ED after a normal cranial CT scan is reasonable but appropriate instructions are required as delayed tICH may occur.
INTRODUCTION
Background
The use of anticoagulant and antiplatelet medications, specifically warfarin and clopidogrel, is steadily increasing in the population.1-3 Prior studies suggest patients on either of these medications are at increased risk for traumatic intracranial hemorrhage (tICH) following blunt head trauma, but the risk in a large, generalizable cohort is unknown.4-6
Importance
The majority of patients with tICH are identified on initial cranial computed tomographic (CT) scan. Limited data, however, suggest patients on warfarin are at increased risk for delayed tICH (tICH diagnosed within two weeks of injury following an initially normal cranial CT).7-9 This concern is highlighted by the not uncommon practice of reversing patients on warfarin following head trauma despite a normal cranial CT.10 The potential risk for both immediate and delayed tICH has generated guidelines recommending routine cranial CT imaging and hospital admission for neurological observation in head-injured patients taking warfarin.11-14 These recommendations, however, are not informed by rigorous, prospective, multicenter studies identifying the prevalence and incidence of immediate tICH and delayed tICH in patients on warfarin.
The evidence supporting an increased risk of tICH in patients on clopidogrel is more limited,11 despite this drug being one of the most commonly prescribed worldwide.15 Although small retrospective studies suggest an increased risk of tICH and mortality in head trauma patients on clopidogrel,6,16,17 current guidelines do not explicitly recommend routine CT imaging for these patients after blunt head trauma.11-13 In addition, the risk of delayed tICH in patients on clopidogrel is entirely unknown.
Goals of This Investigation
Knowledge of the true prevalence and incidence of immediate and delayed tICH in patients on warfarin or clopidogrel would allow clinicians to make evidence-based decisions regarding their initial patient evaluation and disposition. Therefore, we assessed the prevalence and incidence of immediate and delayed tICH in patients with blunt head trauma taking either warfarin or clopidogrel. Warfarin and clopidogrel cohorts were compared. We hypothesized that the prevalence for immediate tICH is similar between patients on clopidogrel and those on warfarin and that the cumulative incidence of delayed tICH in both groups is < 1%.
METHODS
Study Design
This is a prospective, observational, multicenter study conducted at two trauma centers and four community hospitals in Northern California. The study was approved by the Institutional Review Boards at all sites.
Setting and Selection of Participants
Adult (≥ 18 years old) emergency department (ED) patients with blunt head trauma and pre-injury warfarin or clopidogrel use (within the previous seven days) were enrolled. We defined blunt head trauma as any blunt head injury regardless of loss of consciousness (LOC) or amnesia. We excluded patients with known injuries transferred from outside facilities, as their inclusion would falsely inflate the prevalence of tICH. Additionally, patients with concomitant warfarin and clopidogrel use were excluded.
Data Collection
The treating ED faculty physicians recorded patient history and medication use, injury mechanism, and clinical exam, including initial Glasgow Coma Scale score (GCS) and evidence of trauma above the clavicles (defined as trauma to the face, neck, or scalp) on a standardized data form prior to cranial CT (if obtained). Imaging studies were obtained at the discretion of the treating physician and not dictated by study protocol. At each site, approximately 10% of patients (non-randomly selected) had a separate, independent faculty physician assessment that was masked to and completed within 60 minutes of the initial assessment to evaluate the reliability of pre-selected clinical variables. Data on patients eligible but not enrolled (failures of the study screening process) during ED evaluation were abstracted from their medical records to assess for enrollment bias.
Outcome Measures
Immediate tICH was defined as the presence of any intracranial hemorrhage or contusion as interpreted by the faculty radiologist on the initial cranial CT scan. Patients without a cranial CT during initial ED evaluation were excluded from the immediate tICH calculation. Delayed tICH was defined as tICH on cranial CT scan, occurring within 14 days after an initial normal CT scan and in the absence of repeat head trauma. Neurosurgical intervention was defined as the use of intracranial pressure monitor or brain tissue oxygen probe, placement of burr hole, craniotomy/craniectomy, intraventricular catheter, or subdural drain, or the use of mannitol or hypertonic saline.
Follow Up
Patients were admitted to the hospital at the discretion of the ED physician. Patients with normal cranial CT scans and therapeutic international normalized ratio (INR) levels are not reversed at the participating centers. Electronic medical records (EMR) were reviewed in a standardized fashion by research coordinators and site investigators to assess INR results, CT scan results, ED disposition, and hospital course. Patients admitted to the hospital for at least 14 days were evaluated for the presence of delayed tICH through review of the EMR. Patients discharged from the ED or admitted to the hospital for less than 14 days received a consented, standardized telephone survey at least 14 days after the index ED visit. The 14-day follow up was deemed sufficient to identify clinically important delayed tICH.8,18,19 Repeat cranial imaging was obtained at the discretion of the patients’ treating physicians. If patients were unable to be contacted by telephone survey or the EMR, the Social Security Death Index was reviewed to evaluate for death.20
Statistical Analysis
Data were compared using STATA for Windows, Rel. 10.0 2007 (STATA Corp College Station, TX, USA). Normally distributed continuous data were reported as the mean ± standard deviations (SDs), and ordinal or non-normally distributed continuous data described as the median with interquartile (25-75%) ranges (IQR). For primary, stratified, and sensitivity analyses, proportions and relative risks were presented with 95% confidence intervals (CI). Categorical data were compared with chi-square test or Fisher’s exact test in cases of small cell size. Inter-rater reliability of independent variables recorded by initial and second physicians was reported as percent agreement.
To ensure that differences in outcome between cohorts were not secondary to differences in injury severity, we performed both stratified and sensitivity analyses. We compared the following strata: patients 65 years old or older, patients with minor head injury (GCS scores 13-15), patients with an initial GCS score of 15, patients with a ground level fall, patients with physical evidence of trauma above the clavicles, patients without concomitant aspirin use, and patients evaluated at a community hospital. In addition we stratified the analyses by degree of anticoagulation (INR ≥ 1.3 and INR ≥ 2.0). Sensitivity analyses were conducted assuming those patients without an initial cranial CT (1) had immediate tICH and (2) did not have tICH. Finally, we compared the cumulative incidence of delayed tICH assuming all patients lost to follow up had a delayed tICH.
Role of the Funding Source
The sponsors of the study had no role in study design, data collection and analysis, or manuscript preparation. The corresponding author had full access to all the data and had final responsibility for the decision to submit for publication.
RESULTS
Characteristics of Study Subjects
Between April 2009 and January 2011, 1101 patients were enrolled (83.3% of all eligible patients) (Figure). Comparison of patients enrolled and those eligible but not enrolled demonstrated similar characteristics (age, gender, medication use, ED cranial CT, and hospital admission) and outcomes (immediate tICH, neurosurgical intervention, and in-hospital mortality). Reasons for failures of the study screening process were unknown. Thirty-seven patients were excluded (25 transferred patients and 12 patients with concomitant clopidogrel and warfarin use), leaving 1064 patients for data analysis. Of the 1064 patients, 768 patients (72.2%) were taking warfarin and 296 patients (27.8%) were taking clopidogrel. There were 364 patients (34.2%) from two American College of Surgeons designated Level 1 or 2 trauma centers and 700 patients (65.8%) from four community hospitals. The most common mechanism of injury was a ground level fall (n=887, 83.3%) followed by direct blow (n=59, 5.6%) and motor vehicle collision (n=51, 4.8%).
Figure 1.
Flow of Patients in Study
Abbreviations: CT, computed tomography; tICH, traumatic intracranial hemorrhage
a One patient lost to follow-up
b Two patients lost to follow-up
c Two patients lost to follow-up and one patient died after discharge from the emergency department
The majority (n=932, 87.6%) of patients had a GCS of 15 and 752 (70.7%) patients had physical examination findings of head trauma above the clavicles. The primary indication for warfarin and clopidogrel use was atrial fibrillation (543/768, 70.7%) and coronary artery disease (158/296, 53.4%), respectively. Most patients reported taking their medication less than 24 hours prior to injury (warfarin group 660/768, 85.9%; clopidogrel group 252/296, 85.1%). In patients on warfarin, 603/768 (78.5%) had an INR measurement on initial evaluation in the ED (median INR 2.5; IQR 2.0-3.3). The majority of these patients (576/603, 95.5%) had an elevated INR (≥ 1.3) and 458/603 (76.0%) had an INR (≥ 2.0).
One thousand of the 1064 (94.0%; 95% CI 92.4-95.3%) received a cranial CT during initial ED evaluation. Hospitalization rates were similar for those on warfarin (271/768, 35.3%) and on clopidogrel (93/296, 31.4%). Patient clinical characteristics were similar in both groups, except for headache, concomitant aspirin use, and evidence of trauma to the neck and scalp laceration, which were more common in the clopidogrel group (Table 1).
Table 1.
Demographic and Clinical Characteristics of the Study Population
| No. (%) of Patients | |||
|---|---|---|---|
| Characteristic | Total (n = 1064) |
Warfarin (n = 768) |
Clopidogrel (n = 296) |
| Demographics | |||
| Age, mean (SD), y | 75.4 (12.7) | 75.3 (13.0) | 75.7 (11.9) |
| Male sex | 502 (47.1) | 362 (47.1) | 140 (47.3) |
| Mechanism of injury | |||
| Ground level fall | 887 (83.3) | 644 (83.9) | 243 (82.1) |
| Fall from height | 37 (3.5) | 23 (3.0) | 14 (4.7) |
| MVC, < 35 miles per hour | 18 (1.7) | 12 (1.6) | 6 (2.0) |
| MVC, ≥ 35 miles per hour | 24 (2.3) | 16 (2.1) | 8 (2.7) |
| MVC, unknown speed | 9 (0.8) | 4 (0.5) | 5 (1.7) |
| Pedestrian struck by automobile | 4 (0.4) | 4 (0.5) | 0 (0.0) |
| Bicyclist struck by automobile | 4 (0.4) | 3 (0.4) | 1 (0.3) |
| Direct blow | 59 (5.6) | 45 (5.9) | 14 (4.7) |
| Unknown mechanism | 16 (1.5) | 13 (1.7) | 3 (1.0) |
| Other mechanism | 6 (0.5) | 4 (0.5) | 2 (0.7) |
| Clinical history | |||
| Vomiting | 45 (4.2) | 34 (4.4) | 11 (3.7) |
| Headache | 357 (33.6) | 239 (31.1) | 118 (39.9) |
| Loss of consciousness or amnesia | 196 (18.4) | 136 (17.7) | 60 (20.3) |
| Concomitant aspirin use | 43 (4.0) | 19 (2.5) | 24 (8.1) |
| Physical exam | |||
| Alcohol intoxication | 33 (3.1) | 26 (3.4) | 7 (2.4) |
| Any evidence of trauma above the clavicles | 752 (70.7) | 531 (69.1) | 221 (74.7) |
| - Trauma to face | 406 (38.2) | 296 (38.5) | 110 (37.2) |
| - Trauma to neck | 36 (3.4) | 20 (2.6) | 16 (5.4) |
| - Basilar skull fracture | 2 (0.2) | 1 (0.1) | 1 (0.3) |
| - Scalp abrasion | 157 (14.8) | 110 (14.3) | 47 (15.9) |
| - Scalp contusion | 309 (29.0) | 221 (28.8) | 88 (29.7) |
| - Scalp laceration | 182 (17.1) | 117 (15.2) | 65 (22.0) |
| Normal mental status (GCS 15) | 932 (87.6) | 674 (87.8) | 258 (87.2) |
| Mild head injury (GCS 13-15) | 1035 (97.3) | 747 (97.3) | 288 (97.3) |
| Moderate head injury (GCS 9-12) | 18 (1.7) | 13 (1.7) | 5 (1.7) |
| Severe head injury (GCS 3-8) | 11 (1.0) | 8 (1.0) | 3 (1.0) |
| ED course | |||
| Initial cranial computed tomography | 1000 (94.0) | 724 (94.3) | 276 (93.3) |
| Admitted to hospital | 364 (34.2) | 271 (35.3) | 93 (31.4) |
Abbreviations: SD, standard deviation; MVC, motor vehicle collision; GCS, Glasgow coma scale
Main Results
Immediate tICH
Seventy of the 1000 patients had immediate tICH on ED CT scan. The prevalence of immediate tICH was higher in patients on clopidogrel (33/276, 12.0%; 95% CI 8.4-16.4%) than on warfarin (37/724, 5.1%; 95% CI 3.6-7.0%), relative risk = 2.31 (95% CI 1.48-3.63), p<0.001 (Table 2). Follow-up was obtained in 63/64 of patients not undergoing cranial CT during initial ED evaluation and none was subsequently diagnosed with tICH. Mortality and neurosurgical intervention rates after immediate tICH were not statistically different between cohorts (Table 2).
Table 2.
Prevalence of Traumatic Intracranial Hemorrhage, Neurosurgical Intervention, and Mortality
| No. (%) [95% CI] of Patients | Differences in proportions, % (95% CI) |
|||
|---|---|---|---|---|
| Outcome measures | Total (n = 1064) |
Warfarin (n = 768) |
Clopidogrel (n = 296) |
|
| Immediate tICHa,b | 70/1000 (7.0) [5.5 to 8.8] |
37/724 (5.1) [3.6 to 7.0] |
33/276 (12.0) [8.4 to 16.4] |
6.8 (2.7 to 11.0) |
| In-hospital mortality after immediate tICH |
15/70 (21.4) [12.5 to 32.9] |
8/37 (21.6) [9.8 to 38.2] |
7/33 (21.2) [9.0 to 38.9] |
−0.4 (−19.7 to 18.8) |
| Neurosurgical intervention after immediate tICH |
12/70 (17.1) [9.2 to 28.0] |
5/37 (13.5) [4.5 to 28.8] |
7/33 (21.2) [9.0 to 38.9] |
7.6 (−10.1 to 25.5) |
| Delayed tICHc,d | 4/930 (0.4) [0.1 to 1.1] |
4/687 (0.6) [0.2 to 1.5] |
0/243 (0.0) [0.0 to 1.5] |
−0.6 (−1.1 to 0.0) |
Abbreviations: CI, confidence interval; tICH, traumatic intracranial hemorrhage; CT, computed tomography
Immediate tICH is defined as the presence of tICH on initial cranial CT
Sixty-four patients did not receive initial cranial CT
Delayed tICH is defined as the presence of tICH on cranial CT or autopsy after negative initial cranial CT without new head trauma
Four patients were lost to follow-up (two warfarin and two clopidogrel) and one patient died after discharge from the emergency department (clopidogrel)
The majority of patients with immediate tICH (45/70, 64.3%) had a normal mental status (GCS = 15), with similar proportions between the warfarin (23/37, 62.2%) and clopidogrel (22/33, 66.7%) cohorts. Furthermore, in those with immediate tICH, 4/37 (10.8%) in the warfarin cohort and 6/33 (18.2%) in the clopidogrel cohort had no LOC, a normal mental status, and no evidence of trauma above the clavicles.
The prevalence of immediate tICH varied by participating center. The prevalence of tICH was highest at the Level 1 trauma center (12.6%; 95% CI 8.1-18.3%) compared to the Level 2 trauma center (5.0%; 95% CI 2.3-9.2%) and the four community centers (5.4%; 95% CI 3.9-7.4%). All clinical variables measured for inter-rater reliability had substantial agreement (range 87-100%).21
Delayed tICH
The cumulative incidence of delayed tICH was assessed in the 930 patients with an initial normal cranial CT scan by telephone survey (843, 90.6%) or EMR review (83, 8.9%). Of the four patients lost to follow-up, none was identified in the Social Security Death Index.
Delayed tICH was identified in 4/687 (0.6%; 95% CI 0.2-1.5%) patients on warfarin and 0/243 (0%; 95% CI 0-1.5%) patients on clopidogrel (Figure). Two of these four patients were deemed non-operable and died from extensive tICH. The characteristics of the four patients who suffered a delayed tICH are represented in Table 3. One additional patient on clopidogrel died at home from unknown causes eight days after initial ED visit and did not present to hospital at time of death.
Table 3.
Patients With Delayed Traumatic Intracranial Hemorrhage (all with pre-injury warfarin use)
| Patient | Mechanism of Injury |
Initial GCS |
Initial INR |
Repeat cranial CT findings (days after initial cranial CT) |
Neurosurgical intervention/In- hospital mortality (days after initial cranial CT) |
Comments |
|---|---|---|---|---|---|---|
| 63 year old female |
Ground level fall, isolated head injury |
15 | 1.15 | Massive subdural hematoma with uncal herniation (3) |
Mannitol/Died (3) | Patient was discharged home from initial ED visit. She was found obtunded at home three days later. She was taken emergently to ED and died in hospital the same day. |
| 63 year old male |
Ground level fall, isolated head injury |
15 | 1.50 | Small intraparenchymal contusion and subarachnoid hemorrhage (1) |
No/No | Patient was admitted to hospital. Routine repeat cranial CT showed a small tICH. Discharged home HD#4. |
| 79 year old male |
Ground level fall, isolated head injury |
15 | 4.95 | Small intraventricular hemorrhage (7) |
No/No | Patient was admitted to hospital. Repeat cranial CT obtained for a change in mental status on HD#7. Patient improved and was discharged home on HD#8. |
| 91 year old male |
Ground level fall, isolated head injury |
15 | 1.90 | Large intraparenchymal, subarachnoid, and intraventricular hemorrhage with midline shift of 9.3 mm (3) |
No/Died (7) | Patient was admitted to hospital. On HD#3, repeat cranial CT was obtained for a change in mental status demonstrated a large tICH and patient was made DNR. Died on HD#7. |
Abbreviations: GCS, Glasgow coma scale; INR, international normalized ratio; ED, emergency department; CT, computed tomography; tICH, traumatic intracranial hemorrhage; HD, hospital day; DNR, Do-Not-Resuscitate
Stratified and Sensitivity Analyses
We performed both stratified and sensitivity analyses to assess the validity of our results (Table 4). The stratified analyses confirm an increased risk of tICH in those patients on clopidogrel compared with warfarin across all strata. Likewise, the sensitivity analyses also confirm the increased risk of tICH in those patients on clopidogrel.
Table 4.
Stratified and Sensitivity Analyses For Immediate Traumatic Intracranial Hemorrhage
| Analysesa | No. (%) [95% CI] of Patients | Relative Risk (95% CI) |
||
|---|---|---|---|---|
| Warfarin (n = 768) |
Clopidogrel (n = 296) |
Differences in proportions, % (95% CI) |
||
| Primary analysis | 37/724 (5.1) [3.6 to 7.0] | 33/276 (12.0) [8.4 to 16.3] | 6.8 (2.7 to 11.0) | 2.31 (1.48 to 3.63) |
| Patients 65 years or older | 33/594 (5.6) [3.9 to 7.7] | 24/217 (11.1) [7.2 to 16.0] | 5.5 (3.7 to 7.4) | 1.99 (1.20 to 3.29) |
| Patients with GCS 13-15 | 30/703 (4.3) [2.9 to 6.0] | 29/268 (10.8) [7.4 to 15.2] | 6.6 (2.5 to 10.6) | 2.54 (1.55 to 4.14) |
| Patients with GCS 15 | 23/631 (3.6) [2.3 to 5.4] | 22/239 (9.2) [5.9 to 13.6] | 5.6 (2.2 to 9.5) | 2.53 (1.44 to 4.44) |
| Patients with ground level fall |
30/608 (4.9) [3.4 to 7.0] | 27/225 (12.0) [8.1 to 17.0] | 7.1 (2.5 to 11.6) | 2.43 (1.48 to 4.00) |
| Patients with evidence of trauma above the clavicles |
29/502 (5.7) [3.9 to 8.2] | 21/205 (10.2) [6.4 to 15.2] | 4.5 (−0.2 to 9.1) | 1.77 (1.04 to 3.04) |
| Patients without concomitant aspirin use |
36/705 (5.1) [3.6 to 7.0] | 29/252 (11.5) [7.8 to 16.1] | 6.4 (2.1 to 10.7) | 2.25 (1.41 to 3.60) |
| Patients evaluated at community hospitals |
21/485 (4.3) [2.7 to 6.5] | 17/161 (10.6) [6.3 to 16.4] | 6.2 (1.1 to 11.3) | 2.44 (1.32 to 4.51) |
| Warfarin patients with INR ≥ 1.3 |
35/556 (6.3) [4.4 to 8.6] | 33/276 (12.0) [8.4 to 16.3] | 5.7 (1.3 to 10.0) | 1.90 (1.21 to 2.99) |
| Warfarin patients with INR ≥ 2.0 |
31/441(7.0) [4.8 to 9.8] | 33/276 (12.0) [8.4 to 16.3] | 4.9 (0.4 to 9.4) | 1.70 (1.07 to 2.71) |
| Assume patients without cranial CT imaging did not have immediate tICH |
37/768 (4.8) [3.4 to 6.6] | 33/296 (11.1) [7.8 to 15.3] | 6.3 (2.4 to 10.2) | 2.31 (1.48 to 3.63) |
| Assume patients without cranial CT imaging had immediate tICH |
81/768 (10.5) [8.5 to 12.9] | 53/296 (17.9) [13.7 to 22.8] | 7.4 (2.5 to 12.2) | 1.70 (1.23 to 2.34) |
Abbreviations: CI, confidence interval; GCS, Glasgow coma score; INR, international normalized ratio; CT, computed tomography; tICH, traumatic intracranial hemorrhage
Based on patients who received a cranial CT scan on initial evaluation after head injury
The final sensitivity analysis assessed the four patients lost to follow-up and the one death from unknown causes. Assuming all patients had a delayed tICH, the cumulative incidence of delayed tICH would increase to 6/687 patients (0.9%; 95% CI 0.3-1.9%) in the warfarin group and 3/243 (1.2%; 95% CI 0.3-3.6%) in the clopidogrel group.
LIMITATIONS
Our results should be interpreted in the context of several limitations. This was an observational study, thus CT scans were not obtained on all patients and ethical considerations prevented CT scanning solely for study purposes. Some patients not undergoing CT scan during initial ED visit potentially had an undiagnosed tICH, although none was identified in follow-up. Furthermore, some patients with a negative initial CT scan may have eventually developed an undiagnosed delayed tICH. We did, however, obtain clinical follow-up, which is a reasonable method to evaluate for clinically important outcomes when the definitive test is not ethical or feasible.39 The increased risk of immediate tICH in the clopidogrel cohort may be attributed to the higher prevalence of concomitant aspirin use compared to the warfarin cohort (8.1% vs. 2.5%). However, we conducted a subgroup analysis excluding patients with concomitant aspirin use and the clopidogrel cohort maintained a significant increased risk for immediate tICH compared to the warfarin cohort. We did not collect data on patients with isolated pre-injury aspirin use40 or patients without pre-injury anti-platelet or anti-coagulation use. Finally, patients on warfarin may be more acutely aware of the bleeding risks associated with their medication than those taking clopidogrel. Therefore, patients on warfarin may be more apt to seek emergency care, even with trivial head trauma, and thus have less severe mechanisms of injury compared to patients on clopidogrel. We were unable, however, to identify such behavior, as the clinical characteristics, mechanism of injury, and CT scan rate were similar overall between the warfarin and clopidogrel groups.
DISCUSSION
Contrary to our hypothesis, the prevalence of immediate tICH in patients with clopidogrel was significantly higher compared with those on warfarin despite the cohorts having similar characteristics. Additionally, we determined in a large and generalizable cohort of patients on warfarin or clopidogrel that the development of a delayed tICH after a negative initial cranial CT is rare and does not warrant routine hospitalization for observation or immediate anticoagulation reversal with blood products.
To our knowledge, this is the first large, prospective study of head-injured patients with pre-injury warfarin or clopidogrel use. We identified ten warfarin and three clopidogrel studies that reported a prevalence of immediate tICH.4,6,22-30 The prevalence for immediate tICH in patients with pre-injury warfarin use ranged from 0% to 65%.4,22-30 The three studies evaluating immediate tICH in patients with pre-injury clopidogrel use demonstrated a prevalence of tICH ranging from 36-71%.6,23,24 The overall quality of these studies however was limited, as the majority of studies were small (<100 patients), retrospective, and registry studies. These studies suffer from significant inclusion bias as the sampled population originates from a trauma registry (patients admitted to a trauma center) and excludes not only patients evaluated and discharged from the trauma center ED but also all patients evaluated at community hospitals. In addition, the prevalence of tICH is likely falsely elevated due to the inclusion of patients transferred to a trauma center. Our study is unique in that a majority of patients were evaluated at community hospitals. Furthermore, we included all patients with any degree of head trauma. Thus, the current study identifies the prevalence of tICH in a more generalizable population than those sampled from trauma registries. Numerous case reports and case series describe delayed tICH though no prior study evaluates the cumulative incidence of delayed tICH.7-9
Current guidelines recommend that patients with head trauma and pre-injury warfarin undergo routine cranial CT imaging.11-14 These recommendations are based on theoretical risk and retrospective data, as large, prospective studies excluded anti-coagulated patients or did not specifically study patients on warfarin.31-34 Despite the lower prevalence rate of tICH in this study, the results confirm the substantial risk of tICH in patients with blunt head trauma on warfarin and the benefit of routine cranial CT imaging, even in community hospitals. Prior guidelines, however, do not consider pre-injury clopidogrel an indication for cranial imaging,11-13 despite retrospective data suggesting an increased risk for tICH.6,16,17 The current results indicate that the approach to the head-injured patient with pre-injury clopidogrel should be similar to the approach to the head-injured patient with pre-injury warfarin use – liberal cranial imaging. As delayed diagnosis of tICH increases morbidity and mortality, early diagnosis of tICH is important in order to initiate treatment, including coagulopathy reversal and/or neurosurgical intervention.35-37
The prevalence of immediate tICH in well-appearing patients is also very concerning. Over 60% of patients with immediate tICH in both warfarin and clopidogrel cohorts had a normal mental status (GCS=15). Additionally, a significant proportion of patients (11% in warfarin cohort and 18% in the clopidogrel cohort) had no LOC, a normal mental status, and no physical evidence of trauma above the clavicles. Current National Institute for Health and Clinical Excellence head injury guidelines (updated 2007) recommend urgent (< 1 hour) CT imaging in patients with head injury and pre-injury warfarin use, provided they sustain LOC or amnesia.12 In our study, 49 of 70 (70%) patients with immediate tICH did not sustain LOC or amnesia. We recommend routine urgent CT imaging in head-injured patients with prior warfarin or clopidogrel use, even in well-appearing patients without a history of LOC or amnesia.
The concern for delayed tICH in patients with warfarin use stems from case reports and case series,7-9 leading guidelines to recommend routine admission for all head-injured patients on warfarin despite a normal cranial CT.14 Moreover, a survey of clinical practices among North American trauma surgeons indicated that 74% of respondents reverse patients on warfain with blunt head trauma despite a normal cranial CT.10 Furthermore, 66% of respondents reverse these patients with fresh frozen plasma.10 Our results indicate that delayed tICH occurs very infrequently (<1%) in both populations. Thus patients on warfarin or clopidogrel with a normal cranial CT and no other indications for admission may be discharged home, albeit with explicit discharge instructions and close follow-up. More importantly, these patients do not need to have their therapeutic anticoagulation aggressively reversed with blood products. In patients with supratherapeutic INR levels, we recommend appropriate medical treatment following current guidelines.38
In summary, ED patients with blunt head trauma and pre-injury clopidogrel use have a significantly higher prevalence of immediate tICH compared to those with pre-injury warfarin use. Routine cranial CT imaging is generally indicated in patients with blunt head trauma on clopidogrel or warfarin regardless of the clinical findings. The cumulative incidence of delayed tICH is very low for both groups, suggesting that in patients with a normal cranial CT anticoagulation reversal is unnecessary and discharging them home from the ED may be reasonable. As delayed tICH may rarely occur, routine follow-up and appropriate discharge instructions are necessary.
Acknowledgments
This work was supported by The Garfield Memorial Fund (Kaiser Permanente). DN was supported through a Mentored Clinical Research Training Program Award (K30 and KL2), Grant Number UL1 RR024146 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The Garfield Memorial Fund, NCRR, NIH had no role in the design and conduct of the study, in the analysis or interpretation of the data, or in the preparation of the data. The views expressed in this article are solely the responsibility of the authors and do not necessarily represent the official view of NCRR, NIH, or Kaiser Permanente. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Footnotes
Presented as an oral presentation at the SAEM National Meeting, Boston, MA, June 4th, 2011
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Quintero-Gonzalez JA. Fifty years of clinical use of warfarin. Invest Clin. 2010;51(2):269–287. [PubMed] [Google Scholar]
- 2.Virjo I, Makela K, Aho J, et al. Who receives anticoagulant treatment with warfarin and why? A population-based study in Finland. Scand J Prim Heath Care. 2010;28(4):237–241. doi: 10.3109/02813432.2010.514138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ostini R, Hegney D, Mackson JM, Williamson M, Tett SE. Why is the use of clopidogrel increasing rapidly in Australia? An exploration of geographical location, age, sex and cardiac stenting rates as possible influences on clopidogrel use. Pharmacoepidemiol Drug Saf. 2008;17(11):1077–1090. doi: 10.1002/pds.1638. [DOI] [PubMed] [Google Scholar]
- 4.Li J, Brown J, Levine M. Mild head injury, anticoagulants, and risk of intracranial injury. Lancet. 2001;357(9258):771–772. doi: 10.1016/S0140-6736(00)04163-5. [DOI] [PubMed] [Google Scholar]
- 5.Mina AA, Knipfer JF, Park DY, Bair HA, Howells GA, Bendick PJ. Intracranial complications of preinjury anticoagulation in trauma patients with head injury. J Trauma. 2002;53(4):668–672. doi: 10.1097/00005373-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Jones K, Sharp C, Mangram AJ, Dunn EL. The effects of preinjury clopidogrel use on older trauma patients with head injuries. Am J Surg. 2006;192(6):743–745. doi: 10.1016/j.amjsurg.2006.08.037. [DOI] [PubMed] [Google Scholar]
- 7.Cohen DB, Rinker C, Wilberger JE. Traumatic brain injury in anticoagulated patients. J Trauma. 2006;60(3):553–557. doi: 10.1097/01.ta.0000196542.54344.05. [DOI] [PubMed] [Google Scholar]
- 8.Itshayek E, Rosenthal G, Fraifeld S, Perez-Sanchez X, Cohen JE, Spektor S. Delayed posttraumatic acute subdural hematoma in elderly patients on anticoagulation. Neurosurgery. 2006;58(5):E851–856. doi: 10.1227/01.NEU.0000209653.82936.96. discussion E851-856. [DOI] [PubMed] [Google Scholar]
- 9.Reynolds FD, Dietz PA, Higgins D, Whitaker TS. Time to deterioration of the elderly, anticoagulated, minor head injury patient who presents without evidence of neurologic abnormality. J Trauma. 2003;54(3):492–496. doi: 10.1097/01.TA.0000051601.60556.FC. [DOI] [PubMed] [Google Scholar]
- 10.Coimbra R, Hoyt DB, Anjaria DJ, Potenza BM, Fortlage D, Hollingsworth-Fridlund P. Reversal of anticoagulation in trauma: a North-American survey on clinical practices among trauma surgeons. J Trauma. 2005;59(2):375–382. doi: 10.1097/01.ta.0000174728.46883.a4. [DOI] [PubMed] [Google Scholar]
- 11.Jagoda AS, Bazarian JJ, Bruns JJ, Jr., et al. Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Ann Emerg Med. 2008;52(6):714–748. doi: 10.1016/j.annemergmed.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 12.Head injury: Triage, assessment, investigation and early management of head injury in infants, children, and adults. National Collaborative Centre for Acute Care and National Institute for Health and Clinical Excellence; [Accessed February 24, 2012]. Available at: http://www.nice.org.uk/nicemedia/pdf/CG56NICEGuideline.pdf. [Google Scholar]
- 13.Servadei F, Teasdale G, Merry G. Defining acute mild head injury in adults: a proposal based on prognostic factors, diagnosis, and management. J Neurotrauma. 2001;18(7):657–664. doi: 10.1089/089771501750357609. [DOI] [PubMed] [Google Scholar]
- 14.Vos PE, Battistin L, Birbamer G, et al. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurol. 2002;9(3):207–219. doi: 10.1046/j.1468-1331.2002.00407.x. [DOI] [PubMed] [Google Scholar]
- 15.IMS [Accessed February 24, 2012];Top 20 Global Products, 2010, Total Audited Markets. Available at: http://imshealth.com/deployedfiles/imshealth/Global/Content/StaticFile/Top_Line_Data/Top_20_Global_Products.pdf.
- 16.Ohm C, Mina A, Howells G, Bair H, Bendick P. Effects of antiplatelet agents on outcomes for elderly patients with traumatic intracranial hemorrhage. J Trauma. 2005;58(3):518–522. doi: 10.1097/01.ta.0000151671.35280.8b. [DOI] [PubMed] [Google Scholar]
- 17.Wong DK, Lurie F, Wong LL. The effects of clopidogrel on elderly traumatic brain injured patients. J Trauma. 2008;65(6):1303–1308. doi: 10.1097/TA.0b013e318185e234. [DOI] [PubMed] [Google Scholar]
- 18.Diaz FG, Yock DH, Jr., Larson D, Rockswold GL. Early diagnosis of delayed posttraumatic intracerebral hematomas. J Neurosurg. 1979;50(2):217–223. doi: 10.3171/jns.1979.50.2.0217. [DOI] [PubMed] [Google Scholar]
- 19.Poon WS, Rehman SU, Poon CY, Li AK. Traumatic extradural hematoma of delayed onset is not a rarity. Neurosurgery. 1992;30(5):681–686. [PubMed] [Google Scholar]
- 20.Quinn J, Kramer N, McDermott D. Validation of the Social Security Death Index (SSDI): An Important Readily-Available Outcomes Database for Researchers. West J Emerg Med. 2008;9(1):6–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 22.Claudia C, Claudia R, Agostino O, Simone M, Stefano G. Minor head injury in warfarinized patients: indicators of risk for intracranial hemorrhage. J Trauma. 2011;70(4):906–909. doi: 10.1097/TA.0b013e3182031ab7. [DOI] [PubMed] [Google Scholar]
- 23.Brewer ES, Reznikov B, Liberman RF, et al. Incidence and predictors of intracranial hemorrhage after minor head trauma in patients taking anticoagulant and antiplatelet medication. J Trauma. 70(1):E1–5. doi: 10.1097/TA.0b013e3181e5e286. [DOI] [PubMed] [Google Scholar]
- 24.Pieracci FM, Eachempati SR, Shou J, Hydo LJ, Barie PS. Degree of anticoagulation, but not warfarin use itself, predicts adverse outcomes after traumatic brain injury in elderly trauma patients. J Trauma. 2007;63(3):525–530. doi: 10.1097/TA.0b013e31812e5216. [DOI] [PubMed] [Google Scholar]
- 25.Franko J, Kish KJ, O’Connell BG, Subramanian S, Yuschak JV. Advanced age and preinjury warfarin anticoagulation increase the risk of mortality after head trauma. J Trauma. 2006;61(1):107–110. doi: 10.1097/01.ta.0000224220.89528.fc. [DOI] [PubMed] [Google Scholar]
- 26.Ivascu FA, Howells GA, Junn FS, Bair HA, Bendick PJ, Janczyk RJ. Rapid warfarin reversal in anticoagulated patients with traumatic intracranial hemorrhage reduces hemorrhage progression and mortality. J Trauma. 2005;59(5):1131–1137. doi: 10.1097/01.ta.0000189067.16368.83. discussion 1137-1139. [DOI] [PubMed] [Google Scholar]
- 27.Gittleman AM, Ortiz AO, Keating DP, Katz DS. Indications for CT in patients receiving anticoagulation after head trauma. Am J Neuroradiol. 2005;26(3):603–606. [PMC free article] [PubMed] [Google Scholar]
- 28.Mina AA, Bair HA, Howells GA, Bendick PJ. Complications of preinjury warfarin use in the trauma patient. J Trauma. 2003;54(5):842–847. doi: 10.1097/01.TA.0000063271.05829.15. [DOI] [PubMed] [Google Scholar]
- 29.Garra G, Nashed AH, Capobianco L. Minor head trauma in anticoagulated patients. Acad Emerg Med. 1999;6(2):121–124. doi: 10.1111/j.1553-2712.1999.tb01048.x. [DOI] [PubMed] [Google Scholar]
- 30.Major J, Reed MJ. A retrospective review of patients with head injury with coexistent anticoagulant and antiplatelet use admitted from a UK emergency department. Emerg Med J. 2009;26(12):871–876. doi: 10.1136/emj.2008.068643. [DOI] [PubMed] [Google Scholar]
- 31.Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM. Indications for computed tomography in patients with minor head injury. N Engl J Med. 2000;343(2):100–105. doi: 10.1056/NEJM200007133430204. [DOI] [PubMed] [Google Scholar]
- 32.Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian CT Head Rule and the New Orleans Criteria for CT scanning in patients with minor head injury. JAMA. 2005;294(12):1519–1525. doi: 10.1001/jama.294.12.1519. [DOI] [PubMed] [Google Scholar]
- 33.Stiell IG, Clement CM, Rowe BH, et al. Comparison of the Canadian CT Head Rule and the New Orleans Criteria in patients with minor head injury. JAMA. 2005;294(12):1511–1518. doi: 10.1001/jama.294.12.1511. [DOI] [PubMed] [Google Scholar]
- 34.Stiell IG, Wells GA, Vandemheen K, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357(9266):1391–1396. doi: 10.1016/s0140-6736(00)04561-x. [DOI] [PubMed] [Google Scholar]
- 35.Cohen JE, Montero A, Israel ZH. Prognosis and clinical relevance of anisocoria-craniotomy latency for epidural hematoma in comatose patients. J Trauma. 1996;41(1):120–122. doi: 10.1097/00005373-199607000-00019. [DOI] [PubMed] [Google Scholar]
- 36.Haselsberger K, Pucher R, Auer LM. Prognosis after acute subdural or epidural haemorrhage. Acta Neurochir (Wien) 1988;90(3-4):111–116. doi: 10.1007/BF01560563. [DOI] [PubMed] [Google Scholar]
- 37.Seelig JM, Becker DP, Miller JD, Greenberg RP, Ward JD, Choi SC. Traumatic acute subdural hematoma: major mortality reduction in comatose patients treated within four hours. N Engl J Med. 1981;304(25):1511–1518. doi: 10.1056/NEJM198106183042503. [DOI] [PubMed] [Google Scholar]
- 38.Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133(6 Suppl):160S–198S. doi: 10.1378/chest.08-0670. [DOI] [PubMed] [Google Scholar]
- 39.Jaeschke R, Guyatt G, Sackett DL. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA. 1994;271(5):389–391. doi: 10.1001/jama.271.5.389. [DOI] [PubMed] [Google Scholar]
- 40.Hensrud DD, Engle DD, Scheitel SM. Underreporting the use of dietary supplements and nonprescription medications among patients undergoing a periodic health examination. Mayo Clin Proc. 1999;74(5):443–447. doi: 10.4065/74.5.443. [DOI] [PubMed] [Google Scholar]