Abstract
Objective
This study aimed to investigate the longitudinal course of daily living skills in a large, community-based sample of adolescents and adults with autism spectrum disorders (ASD) over a 10-year period.
Method
Adolescents and adults with ASD (n=397) were drawn from an ongoing, longitudinal study of individuals with ASD and their families. A comparison group of 167 individuals with Down syndrome (DS) were drawn from a linked longitudinal study. The Waisman Activities of Daily Living Scale was administered 4 times over a 10-year period.
Results
We utilized latent growth curve modeling to examine change in daily living skills. Daily living skills improved for the individuals with ASD during adolescence and their early 20s, but plateaued during their late 20s. Having an intellectual disability was associated with lower initial levels of daily living skills and a slower change over time. Individuals with DS likewise gained daily living skills over time, but there was no significant curvature in the change.
Conclusions
Future research should explore what environmental factors and interventions may be associated with continued gains of daily living skills for adults with ASD.
Keywords: daily living skills, autism, adolescence, adulthood, trajectories
Introduction
Autism spectrum disorders (ASDs) are lifelong developmental disabilities that affect an estimated 1 in 110 children in the US.1 ASDs are characterized by impairments in communication and social interaction as well as the presence of repetitive behaviors. In recent years increasing attention has been given to understanding the behavioral phenotype of ASD during adolescence and adulthood. For instance, researchers have explored how autism symptoms and behavior problems change across adolescence and adulthood.2,3, 4 Other work has focused on measuring educational and occupational outcomes for adults with ASD, with results indicating that few individuals reach high levels of independence. 5,6 Virtually no studies, however, have explored the development of independence in daily living skills in adolescents and adults with ASD, even though such abilities are often cited as important factors for successful outcomes for adults with intellectual and developmental disabilities (IDD). 7,8 The present study addressed this gap by examining trajectories of daily living skills over a 10-year period in a large, community sample of adolescents and adults with ASD.
Daily Living Skills in Individuals with ASD
Daily living skills constitute a critical domain of adaptive behavior, which are defined as behaviors necessary for age-appropriate, independent functioning in social, communication, daily living, or motor areas. Past research suggests that the development of daily living skills may be particularly challenging for individuals with ASD. Children with autism often have significant impairments in daily living skills compared to well-matched controls9,10 and as early as 36 months of age such children display a greater discrepancy between their adaptive behavior and mental age than children with other developmental delays. 11 These delays in daily living skills may become more pronounced over time. In a validation study of the Vineland Adaptive Behavior Scales’ supplemental norms for autism, younger children with ASD had higher standard scores than older children with ASD in all adaptive behavior domains, including daily living skills, suggesting that as children with ASD grow, they increasingly lag behind their same-age peers. 12 Similarly, in sample of 1089 children and adolescents with ASD, Kanne and colleagues13 recently found that adolescents had a greater gap between their mental age and adaptive skills than younger children, suggesting that individuals with ASD may gain daily living skills at a pace slower than the rate of their intellectual growth. These cross-sectional findings highlight the need for longitudinal studies to elucidate how daily living skills change over time for individuals with ASD and what factors are associated with improvements in these skills.
Most studies that have examined within-person change in daily living skills for individuals with autism notably have focused on early childhood. For instance, Freeman and colleagues14 explored change in the Vineland Adaptive Behavior Scales in children with ASD and found that daily living skills improved with age. Additionally, results indicated that children with IQs at or above 70 improved at a faster rate than children whose IQs were below 70.14 Similarly, in a longitudinal study of daily living skills in preschoolers with ASD, Green and Carter15 found a linear increase in daily living skills over a three year period, with lower IQ scores and higher levels of autism symptoms associated with slower gains. In a recent study of children with high-functioning autism, daily living skills improved over time, although the rate of change slowed as children entered adolescence.16 Taken together, these studies suggest that daily living skills improve during early childhood and into adolescence, although the rate of change slows over time, and that the presence of an intellectual disability (ID) further slows the rate of growth. Questions remain, however, regarding whether daily living skills continue to improve through adolescence and adulthood and the extent to which ID may influence these later-life trajectories.
The literature on daily living skills for adults with other types of IDD may offer insights into possible patterns of change in daily living skills for those with ASD. For example, Esbensen and colleagues17 explored functional abilities (housekeeping, personal care, meal-related activities, and mobility domains) over a nine-year period in a sample of individuals with IDD, including a large subsample of individuals with Down syndrome (DS). Results indicated that housekeeping skills improved over time whereas personal care and mobility skills declined over the same period. Improvements in housekeeping skills were fastest for younger individuals and declines in personal care skills were fastest for older individuals.17 However, this study did not examine the possibility of curvilinear change. It may be that daily living skills improve for individuals with IDD during adolescence and early adulthood but decline later in adulthood. The present study examined this hypothesis by using latent growth curve modeling to test for linear and curvilinear change in daily living skills for adolescents and adults with ASD as well as for similarly-aged individuals with DS.
Present Study
The primary aim of the present study was to investigate the longitudinal course of daily living skills in a large, community sample of adolescents and adults with ASD. Daily living skills were measured on 4 occasions over a 10-year period, allowing for an examination of linear and curvilinear change. Further, due to the wide range of ages of participants in our study (10–52 years at Time 1), we were able to explore the effects of the age of the individual with ASD (termed “child age”) in addition to ID status on initial level of daily living skills as well as change in daily living skills over time. Residential status of the individual with ASD (living with parent vs. not living with parent) also was examined as a time-varying covariate. In order to provide a benchmark for interpreting trends among the adolescents and adults with ASD, a secondary aim of the present study was to examine change in daily living skills among similarly-aged individuals with DS, again measured on 4 occasions over a 10-year period. Although we did not conduct a direct comparison given differences in the age between samples, we explored change in the DS sample to provide additional context for interpreting scores in the ASD group.
Based on past studies documenting that autism symptoms and behavior problems tend to become less severe during adolescence and adulthood2, we hypothesized that there would be concomitant improvements in daily living skills over the course of the study. However, based on recent work by Taylor and Seltzer3 indicating that the rate of improvement in autism symptoms and behavior problems slows after entering adulthood, we also hypothesized that the change in daily living skills would be curvilinear; that is that the rate of change would decrease over time. Next, consistent with past studies showing that daily living skills improve with age for children with ASD, 14,15 we hypothesized that there would be a significant association between age and initial level of daily living skills. Given the association between intelligence and daily living skills in other samples, 10,13,18 we hypothesized that having an ID would be associated with a lower initial level of daily living skills. Based on the association between ID and growth in daily living skills in studies of younger children with ASD, 14,15 we hypothesized that having an ID would be associated with slower change in daily living skills for adolescents and adults with ASD.
Regarding our secondary aim, based on past work showing gains over time in functional abilities for individuals with ID, 17 we hypothesized that there would be improvements in daily living skills for individuals with DS. We also hypothesized that individuals with DS would display curvilinear change, or a slowing of improvement, consistent with findings that individuals with DS are at risk for dementia as they age. 19,20
Method
Autism Sample Participants
Participants were drawn an ongoing, multi-wave, longitudinal study of 406 individuals with ASD and their families, the Adolescents and Adults with Autism study (AAA). 21 The present study focused on four of eight points of data collection, Times 1, 4, 7, and 8. Families were recruited via agencies, schools, diagnostic clinics, and media announcements. At entry into the AAA study, families met three criteria: (a) the family included a child 10 years of age or older; (b) the child had received a diagnosis of ASD from a medical, psychological, or educational professional; and (c) scores on the Autism Diagnostic Interview-Revised (ADI-R) 22 were consistent with the parental report of an ASD.
Of the original sample of 406, 9 were excluded from the present study as they did not have complete data on activities of daily living at Time 1. Excluded cases were not significantly different from the full sample in child age, sex, family income, or parental education. The individuals with ASD in the present study ranged from 10 to 52 years of age at the beginning of the study (Time 1 M=21.84 years, SD=9.32; Time 4 M=26.25 years, SD=9.36; Time 7 M=29.87 years, SD=9.19; Time 8 M=31.23 years, SD=9.02). The majority of the sample was male (73%) and 70% of the sample had a comorbid diagnosis of ID.
When the AAA study began in 1998, 65% of the individuals with ASD lived with their families and 35% lived away from home. An increasing proportion of individuals moved away from the family home at each subsequent point of data collection, such that at Times 4, 7, and 8, 56%, 45%, and 47% were co-residing with their families, respectively. About half (52.2%) of parent respondents had at least a bachelor’s degree and the median annual household income was $50,000–$59,000 in 1998–1999. The majority of participants (93%) were White. Most respondents were mothers (96.5%), with 14 fathers participating (3.5%).
There were no significant differences between families who participated in all waves of data collection and families with missing data in child sex or ID status. However, consistent with age-related morbidity and mortality, families of older individuals were more likely to end study participation than their younger counterparts (F=3.78, p= .05). Importantly, there were no significant associations between complete study participation and daily living skill scores at Time 1.
Down Syndrome Sample Participants
To benchmark changes in daily living skills in individuals with ASD, a sample of individuals with DS was drawn from a linked longitudinal study of 461 individuals with ID. 23 Families were included in the study if they met two criteria: the mother was between 55 and 85 years of age and the son or daughter lived at home with her. Of the 461 target children in the study, 169 of the sons or daughters had a diagnosis of DS. Of these cases, 2 were excluded from the present study as they had missing data on activities of daily living at Time 1. The individuals with DS in the present study ranged from 15 to 56 years of age at Time 1 (M= 31.61 years, SD= 7.19). The majority were daughters (60.5%) and 28.8% of mothers had at least a bachelor’s degree. The majority of participants (92%) were White.
When this longitudinal study began, all of the individuals with DS lived at home with their families. However, some individuals changed residences at each subsequent point of data collection, such that at Time 4, 7, and 8, 94%, 81%, and 92% were co-residing with their families, respectively. Families who participated in all waves of data collection were not significantly different from families with missing data in child sex, but families of older individuals were more likely to end study participation than families of younger individuals (F=6.94, p < .05). As with the ASD sample, there was no association between complete study participation and Time 1 daily living skills scores.
Procedure and Measures
Procedures and measures were identical for both the ASD and DS samples. At each time point (Times 1, 4, 7, and 8), mothers completed self-administered questionnaires and participated in a 2- to 3- hour in-home interview. For the ASD sample, data collection between Times 1 and 4 occurred an average of 5.00 years apart. Approximately 3.45 years occurred between Times 4 and 7, and 1.99 years occurred between Times 7 and 8. For the DS sample, an average of 4.44 years elapsed between Times 1 and 4, 4.47 years between Times 4 and 7, and 1.72 years between Times 7 and 8.
Independence in activities of daily living was measured using the Waisman Activities of Daily Living Scale (W-ADL; Maenner, Smith, Hong, Makuch, Greenberg, and Seltzer, unpublished material, 2011). See Table 1. Parent respondents rated their son or daughter’s level of independence on 17 items covering the domains of personal care, housekeeping, and meal-related activities. Each item was rated on a 3-point scale of independence 0 (does not perform the task at all), 1 (performs the task with help), or 2 (performs the task independently); and items were summed. Coefficient alphas for the total score in the ASD sample ranged from .90 to .94 for Times 1, 4, 7, and 8; for the DS sample, the alphas ranged from .91 to .93.
Table 1.
Waisman Activities of Daily Living Scale
| 1. Making his/her own bed |
| 2. Doing household tasks, including picking up around the house, putting things away, light housecleaning, etc. |
| 3. Doing errands, including shopping in stores |
| 4. Doing home repairs, including simple repairs around the house, non-technical in nature; for example, changing light bulbs or repairing a loose screw |
| 5. Doing laundry, washing and drying |
| 6. Washing/bathing |
| 7. Grooming, brushing teeth, combing and/or brushing hair |
| 8. Dressing and undressing |
| 9. Toileting |
| 10. Preparing simple foods requiring no mixing or cooking, including sandwiches, cold cereal, etc. |
| 11. Mixing and cooking simple foods, fry eggs, make pancakes, heat food in microwave, etc. |
| 12. Preparing complete meal |
| 13. Setting and clearing table |
| 14. Drinking from a cup |
| 15. Eating from a plate |
| 16. Washing dishes (including using a dishwasher) |
| 17. Banking and managing daily finances, including keeping track of cash, checking account, paying bills, etc. (Note: if he/she can do a portion but not all circle ‘1’ with help.) |
Note: Instructions that accompanied the items: “Next we would like to know about your son or daughter’s current level of independence in performing activities of daily living. For each activity please tell me the number which best describes your son/daughter’s ability to do the task. For example, Independent would mean your son/daughter is able to do the task without any help or assistance.”
2 = independent or does on own; 1 = does with help; 0 = does not do at all.
Child characteristics of age (continuous) and ID status (1=yes, 0=no) were included as predictors of daily living skills scores in the ASD sample analyses. Procedures for assessing the presence of ID in our sample have been reported in detail in previous studies24 and involved a clinical consensus process utilizing information drawn from sources including direct cognitive testing and educational records. Residential status (0=co-residing with parent, 1 = not co-residing with parent) was also included as a time-varying covariate.
Data Analysis
To address our primary aim, we utilized latent growth curve (LGC) modeling to examine daily living skills over a 10-year period. LGC modeling integrates individual growth modeling (i.e. hierarchical linear modeling) and structural equation modeling (SEM) approaches25 and provides estimates of mean structure (intercept and slope), reflecting the average starting point for all individuals and average rate of change. 26 It is also possible to model nonlinear change; by adding a quadratic parameter to a model which already includes an intercept and linear slope, the growth trajectory becomes curvilinear. In a purely linear model, the rate of change is presumed to be constant over time; in contrast, a quadratic latent curve model allows the rate of change either to increase or decrease over time. As an example, the magnitude of change in repeated measures may be larger in earlier years than in later years. 26 The addition of a quadratic trend also alters the interpretation of the linear slope, such that the linear slope coefficient is changed to reflect the instantaneous rate of change at a specific point in time. 25 If the coefficient for the quadratic factor is negative, then the trajectory is concave to the time axis. Conversely, the presence of a positive quadratic trend indicates that the trajectory is convex to the time axis.25
After preliminary analyses using ANOVAs confirmed the presence of change over time in daily living skills without controlling for age and ID status, a multivariate LCG model was assessed in which age and ID status were included as time-invariant predictors and residential status was included as a time-varying covariate. To address our secondary aim of providing an illustrative benchmark for interpreting the patterns of daily living skills observed in our ASD sample, we used LGC modeling to assess change in daily living skills in a sample of individuals with DS over a similar period of time. All models were evaluated in terms of measures of goodness-of-fit using the Mplus modeling program. 27 A satisfactory fit is indicated by a comparative fit index (CFI) close to one and a root mean square error of approximation (RMSEA) less than or equal to .08.
Results
Primary Aim: Daily Living Skills in Adolescents and Adults with ASD
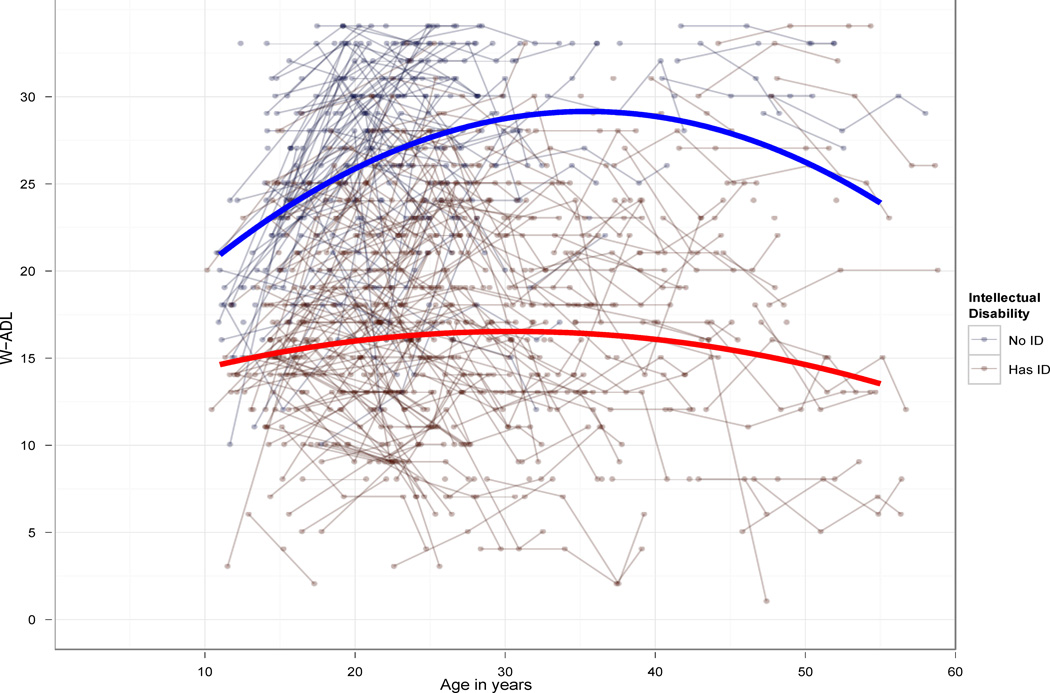
Activities of daily living were assessed at 4 time points (Times 1, 4, 7, and 8) in the ASD sample. We present means, standard deviations, ranges, and intercorrelations among study variables in Table 2. Figure 1 depicts a mixed-effects regression model showing individual scores by age and intellectual disability status. By the end of the study, the average score for the group was 20.59 (SD=8.08) on a scale in which a score of 34 reflects complete independence. Only 16.5% of the sample had scores of 30 or above at Time 8. Scores at each time point were significantly correlated with scores at all other time points.
Table 2.
Descriptive statistics and intercorrelations among study variables for autism sample.
| Time 1 W-ADL |
Time 4 W-ADL |
Time 7 W-ADL |
Time 8 W-ADL |
Child Age | ID Status | |
|---|---|---|---|---|---|---|
| Time 1 | 1 (n = 385) | |||||
| W-ADL | ||||||
| Time 4 | .85*** | 1 | ||||
| W-ADL | (n = 267) | (n = 278) | ||||
| Time 7 | .81*** | .90*** | 1 | |||
| W-ADL | (n = 235) | (n = 228) | (n = 245) | |||
| Time 8 | .78*** | .87*** | .94*** | 1 | ||
| W-ADL | (n = 221) | (n = 217) | (n = 216) | (n = 230) | ||
| Child Age | .16** | −.04 | −.09 | −.09 | 1 | |
| (n = 385) | (n = 278) | (n = 245) | (n = 230) | (n = 397) | ||
| ID Status | −.45*** | −.58*** | −.62*** | −.61*** | .23*** | 1 |
| (n = 385) | (n = 278) | (n = 245) | (n = 230) | (n = 397) | (n = 397) | |
| M/SD | 19.62 (6.65) | 20.66 (7.51) | 20.53 (7.87) | 20.59 (8.08) | 21.84 (9.32) | .70 (.46) |
| Range | 3–34 | 2–34 | 1–34 | 3–34 | 10–52 | 0–1 |
Note: ID = intellectual disability; W-ADL = Waisman Activities of Daily Living
p < .001
Figure 1.
Change in Waisman Activities of Daily Living scores over time for autism spectrum disorder sample, individual and group trajectories. Note: Quadratic (age2) mixed−model paramaterizations displayed.
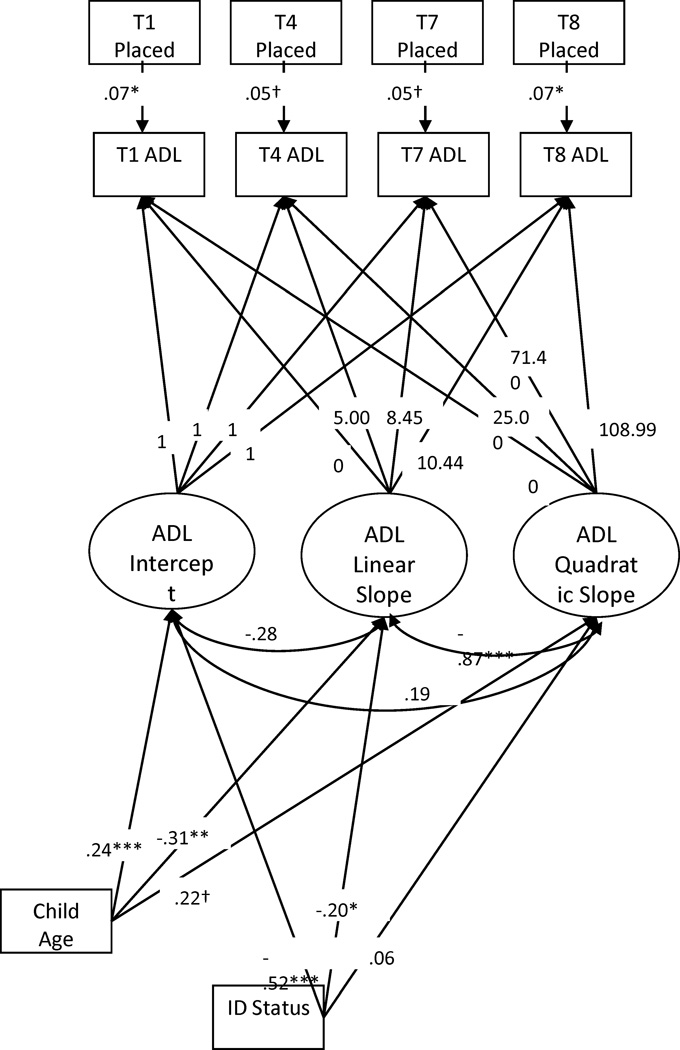
We evaluated a LGC model of daily living skills that specified quadratic growth over time and included child age and ID status as predictors of all latent factors. Residential status (co-residing vs not co-residing) also was included as a time-varying covariate (see Figure 2). In this model, the latent intercept, linear slope, and quadratic trend were indicated by daily living scores at Times 1, 4, 7, and 8. The factor loadings for the intercept factor were all set to 1. The loadings for the linear slope factor were fixed at 0, 5.0, 8.45, and 10.44, reflecting the average length of time between waves of data collection. The loadings for the quadratic slope factor were the linear values squared.
Figure 2.
Latent growth curve model of Waisman Activities of Daily Living (ADL) scores for individuals with autism spectrum disorders (N = 397). Note: ID = intellectual disability. * p < .05, ** p < .01, *** p < .001, † p < .10,
This model displayed excellent fit, χ2 15, N= 406)= 12.69, p = .63; RMSEA= .00; CFI = 1.0. There was a significant positive linear slope (est.= 1.25, SE= .19, p < .001) and a significant negative quadratic trend (est.= −.07, SE= .02, p < .001). However, the linear trend in a model that includes a quadratic trend is interpreted as the instantaneous rate of change. This means that for different snapshots of time, the rate of change may be different. As such, in order to determine how daily living skills were changing across time, we additionally examined the values for the linear slope when time was centered at Times 4, 7, and 8, respectively. At Time 4, the linear trend was positive (est.= .56, SE= .07, p<.001) but at Time 7 the linear trend was non-significant (est.= .07, SE=.15, p=.57). At Time 8, however, there was a significant negative linear trend (est.= −.89, SE= .27, p=.001). Taken together, these findings suggest that, on average, scores were increasing at Times 1 and 4 but were no longer significantly changing at Time 7. By Time 8, scores were beginning to decrease. In other words, daily living skills were improving during adolescence and the early 20s, plateaued around the time of the late 20s, and started to decline during the early 30s. However, we encourage some caution in interpreting the exact nature of change for older individuals since the majority of the sample was under the age of 30 at the end of the study.
There also were significant relationships between child age, ID status, and the latent factors. Child age was positively associated with the intercept of daily living skills, with older individuals having higher scores at the start of the study, β=.24, p<.001. Child age also was associated with the linear factor, β=-.31, p<.01, and the quadratic factor, β=.22, p<.10, although this association with the quadratic factor was not significant at the .05 level. These age effects suggest that older individuals displayed a faster rate of curvature; that is, they were declining at a faster rate. Additionally, ID status was a significant predictor of the intercept of daily living skills, with individuals with ID having lower initial levels of daily living skills at the start of the study, β= −.52, p<.001. Having an ID was also negatively associated with the linear factor, β= −.20, p<.01, suggesting that individuals with ID were gaining skills at a slower rate than individuals without ID. Residential status was a statistically significant covariate of daily living skills at Times 1 and 8, with coresidence between parent and child associated with lower scores.
Secondary Aim: Daily Living Skills in Individuals with Down Syndrome
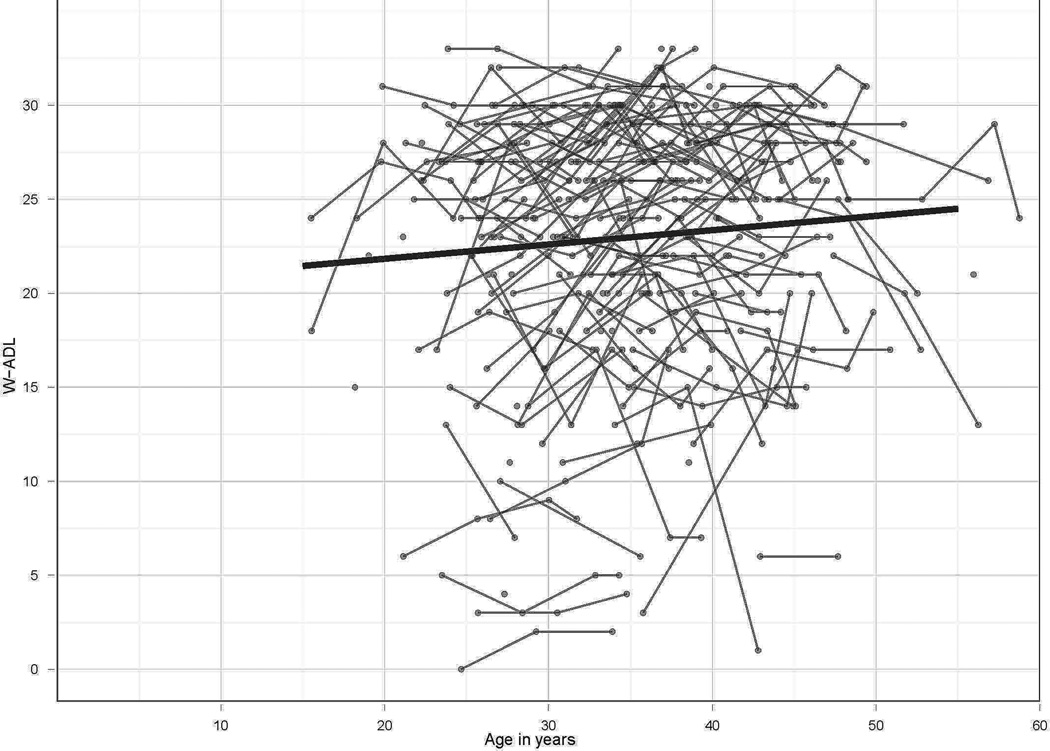
To explore trajectories of daily living skills in the DS sample, daily living skills were assessed at 4 time points (Times 1, 4, 7, and 8). We present means, standard deviations, ranges, and intercorrelations among study variables in Table 3. Figure 3 depicts a mixed-effects regression model showing individual scores by age. By the end of the study, the average score for the group was 23.83 (SD=6.33) on a scale in which a score of 34 reflects complete independence. Only 19.6% of the sample had scores of 30 or above at Time 8. Scores at each time point were significantly correlated with scores at all other time points.
Table 3.
Descriptive statistics and intercorrelations among study variables for Down syndrome sample.
| Time 1 W-ADL |
Time 4 W-ADL |
Time 7 W-ADL |
Time 8 W-ADL |
Child Age | |
|---|---|---|---|---|---|
| Time 1 | 1 | ||||
| W-ADL | (n = 166) | ||||
| Time 4 | .88*** | 1 | |||
| W-ADL | (n = 124) | (n = 125) | |||
| Time 7 | .83*** | .88*** | 1 | ||
| W-ADL | (n = 98) | (n = 92) | (n = 99) | ||
| Time 8 | .85*** | .86*** | .92*** | 1 | |
| W-ADL | (n = 66) | (n = 63) | (n = 60) | (n = 66) | |
| Child Age | .12 | .03 | −.02 | .01 | 1 |
| (n = 166) | (n = 125) | (n = 99) | (n = 66) | (n = 167) | |
| M/SD | 22.55 (6.37) | 23.69 (6.56) | 23.37 (7.41) | 23.83 (6.33) | 31.61 (7.19) |
| Range | 3–33 | 2–33 | 1 – 32 | 5 – 33 | 15–56 |
Note: W-ADL = Waisman Activities of Daily Living.
Figure 3.
Change in Waisman Activities of Daily Living scores over time for Down syndrome sample, individual and group trajectories. Note: Linear mixed−model paramaterization displayed.
We evaluated a LGC model of daily living skills that specified linear and quadratic growth over time and included child age as a predictor of all latent factors and residential status included as a time-varying covariate. Since all individuals in the DS sample had a diagnosis of ID, disability status was not included in this model. In this model, the latent intercept and linear slope were indicated by daily living scores at Times 1, 4, 7, and 8. The factor loadings for the intercept factor were all set to 1. The loadings for the linear slope factor were fixed at 0, 4.44, 8.91, and 10.63, reflecting the average length of time between waves of data collection. The loadings for the quadratic slope factor were the linear values squared.
This model displayed good fit, χ2 (11, N= 167) =16.84, p= .11; RMSEA= .06; CFI= .99. There was a positive linear slope (est.=.86, SE= .45), indicating improvement in daily living skills over time, although this effect only approached statistical significant (p = .058). Importantly, the average increase of .86 points per year is a clinically significant change. The quadratic slope factor was non-significant (est.=−.04, SE= .04, p =.42), indicating that there was no curvature in the change in daily living skills over time. There was a trend for child age to be positively associated with the intercept of daily living skills (p= .10). There were no significant associations between child age and the other latent factors. Residential status was not a significant covariate at any of the time points.
Discussion
The present study utilized LGC modeling to investigate trajectories of daily living skills for adolescents and adults with ASD. Past research examined trajectories of daily living skills for individuals with ASD during childhood and early adolescence but not across adolescence and adulthood. In contrast, the present study included a large, community-based sample of individuals with ASD with a wide age-range (10–52 years), which enabled us to examine the influence of age as well as ID status on change in daily living skills well into adulthood. The longitudinal design of the current study addressed another gap in the literature by allowing for an examination of curvilinear change over a 10-year period. Finally, the present study included an additional analysis of trajectories of daily living skills in a linked longitudinal study of individuals with DS, providing a unique opportunity to understand patterns of change in two different groups of individuals with IDD.
Most notably, the present study found significant quadratic change in daily living skills for individuals with ASD, indicating that skills improved during adolescence and the early twenties, plateaued around the late 20s, and began to decline in the early 30s. This is consistent with our hypothesis that there would be improvements in skills for individuals with ASD but that the rate of change would slow as individuals aged. Recently, Taylor and Seltzer3 documented that the rate of improvement in autism symptoms and behavior problems for adolescents with ASD slowed down (or even stopped) after the individuals with ASD exited the secondary school system (typically during the early 20s). Taken together, these findings suggest that adolescence is a time of growth and improvement for individuals with ASD in a variety of domains, but that, on average, the period of improvement ends by the time such individuals reach 30 years of age. The slowing of improvement in daily living skills is particularly concerning given that the plateau in gains was not due to ceiling effects or a mastery of skills (Maenner et al., unpublished material, 2011). In fact, by the end of the study period, on average, the individuals with ASD were failing to complete over a third of the measured daily living skills independently.
Consistent with our hypothesis and with other studies demonstrating an association between age and daily skills, 14,15 we found that being older at the start of the study was associated with higher levels of initial daily living skills. Findings also indicated that older individuals displayed a faster rate of curvature; that is the older an individual was at the start of the study, the sooner he or she started to display a plateau and eventual decline in daily living skills. Also consistent with past studies of daily living skills in children with ASD, 14,15 having an ID was associated with lower initial levels of daily living skills and with slower rates of change.
A secondary aim of the present study was to examine the pattern of change in daily living skills among individuals with DS in order to provide a context for interpreting the pattern of change observed in our ASD sample. Past research has shown that adults with DS have higher levels of daily living skills than individuals with other intellectual disabilities, 17,16 including individuals with ASD and ID. 7,28 Findings from the present study indicated that individuals with DS show a different pattern of change in daily living skills, with these adults continuing to gain skills across adulthood. The slowing of improvement in daily living skills for adults with ASD may contribute to the poorer adult outcomes observed in individuals with ASD compared to peers with DS who had similar levels of intellectual functioning. 7
The limitations of the present study point to areas for future research. The majority of individuals in our sample were White and middle-class, highlighting a need to examine these skills in more diverse groups. Similarly, although we controlled for residential status, it may be that other environmental contexts (e.g., type of day activity) also influence change in daily living skills. It also is important to note that the sample size for the DS group was small for conducting growth curve analyses, which leaves the possibility that more nuanced patterns of change may be observed in larger groups of adults with DS. Additionally, the majority of the DS sample were already adults at the start of the study, thus limiting the extent to which direct comparisons between the two samples would be informative; a sharper increase in skills may have been observed in the DS group had we measured these skills earlier in development. Although our observation of differences between the ASD and DS groups was entirely exploratory and descriptive, it does raise an intriguing question for future investigation. Finally, the present study is limited by the use of use of a categorical variable measuring ID status, as IQ scores were not available for all participants.
This study has important implications for future research and clinical practice. By the end of the study period, all individuals with ASD were adults but, on average, these adults had not achieved independence in many of the daily living skills we measured. However, as other researchers have noted, 13,29 daily living skills are less tied to the core symptoms of autism than other aspects of functioning such as socialization or communication and thus may be more amenable to change. The improvement in daily living skills for individuals with ASD into the late 20s likewise suggests that it may be possible for daily living skills to be gained at later points in development, even as skills in other areas plateau. It will be critical for future research to explore what environmental factors may be associated with continued gains of daily living skills for adults with ASD as well as the best practices for teaching these skills. Although some attention has been given to developing behavioral and pharmacological interventions to improve daily living skills in younger children with ASD, 30,31 new research is needed to develop strategies for supporting gains in daily living skills for individuals with ASD at later points in the life course.
Acknowledgments
This research was supported by National Institute of Health (NIH) grants R01 AG08768 (MMS) and P30 HD03352 (MMS).
We are extremely grateful to the families who participated in this study; without their generous commitment, our research would not be possible.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Drs. Smith, Maenner, and Seltzer report no biomedical financial interests or potential conflicts of interest.
References
- 1.Prevalence of autism spectrum disorders - Autism and Developmental Disabilities Monitoring Network, United States, 2006. MMWR. Surveillance summaries : Morbidity and mortality weekly report. Surveillance summaries. CDC. 2009;58(10):1–20. [PubMed] [Google Scholar]
- 2.Shattuck PT, Seltzer MM, Greenberg JS, et al. Change in autism symptoms and maladaptive behaviors in adolescents and adults with an autism spectrum disorder. J Autism Dev Disord. 2007;37(9):1735–1747. doi: 10.1007/s10803-006-0307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taylor JL, Seltzer MM. Changes in the autism behavioral phenotype during the transition to adulthood. J Autism Dev Disord. 2010;40(12):1431–1446. doi: 10.1007/s10803-010-1005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson DK, Maye MP, Lord C. Changes in maladaptive behaviors from midchildhood to young adulthod in autism spectrum disorder. Am J Intellect Dev Disab. 2011;116:381–397. doi: 10.1352/1944-7558-116.5.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. J Child Psychol and Psychiatry. 2004;45(2):212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- 6.Taylor JL, Seltzer MM. Employment and post-secondary educational activities for young adults with autism spectrum disorders during the transition to adulthood. J Autism Dev Disord. 2011;41(5):566–574. doi: 10.1007/s10803-010-1070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esbensen AJ, Bishop S, Seltzer MM, Greenberg JS, Taylor JL. Comparisons Between Individuals With Autism Spectrum Disorders and Individuals With Down Syndrome in Adulthood. Am J Intellect Dev Disab. 2010;115(4):277–290. doi: 10.1352/1944-7558-115.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Woolf S, Woolf CM, Oakland T. Adaptive Behavior Among Adults With Intellectual Disabilities and Its Relationship to Community Independence. Intellect Dev Disab. 2010;48(3):209–215. doi: 10.1352/1944-7558-48.3.209. [DOI] [PubMed] [Google Scholar]
- 9.Liss M, Harel B, Fein D, et al. Predictors and Correlates of Adaptive Functioning in Children with Developmental Disorders. J Autism Dev Disord. 2001;31(2):219–230. doi: 10.1023/a:1010707417274. [DOI] [PubMed] [Google Scholar]
- 10.Perry A, Flanagan HE, Dunn Geier J, Freeman NL. Brief report: the Vineland Adaptive Behavior Scales in young children with autism spectrum disorders at different cognitive levels. J Autism Dev Disord. 2009;39(7):1066–1078. doi: 10.1007/s10803-009-0783-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stone WL, Ousley OY, Hepburn SL, Hogan KL, Brown CS. Patterns of adaptive behavior in very young children with autism. Am J Ment Retard. 1999;104(2):187–199. doi: 10.1352/0895-8017(1999)104<0187:POABIV>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Carter AS, Volkmar FR, Sparrow SS, et al. The Vineland Adaptive Behavior Scales: Supplementary Norms for Individuals with Autism. J Autism Dev Disord. 1998;28(4):287–302. doi: 10.1023/a:1026056518470. [DOI] [PubMed] [Google Scholar]
- 13.Kanne SM, Gerber AJ, Quirmbach LM, Sparrow SS, Cicchetti DV, Saulnier CA. The role of adaptive behavior in autism spectrum disorders: implications for functional outcome. J Autism Dev Disord. 2011;41(8):1007–1018. doi: 10.1007/s10803-010-1126-4. [DOI] [PubMed] [Google Scholar]
- 14.Freeman BJ, Del'Homme M, Guthrie D, Zhang F. Vineland Adaptive Behavior Scale Scores as a Function of Age and Initial IQ in 210 Autistic Children. J Autism Dev Disord. 1999;29(5):379–384. doi: 10.1023/a:1023078827457. [DOI] [PubMed] [Google Scholar]
- 15.Green SA, Carter AS. Predictors and Course of Daily Living Skills Development in Toddlers with Autism Spectrum Disorders [published online ahead of print May 2011] J Autism Dev Disord. doi: 10.1007/s10803-011-1275-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Szatmari P, Bryson S, Duku E, et al. Similar developmental trajectories in autism and Asperger syndrome: from early childhood to adolescence. J child psychol psychiatry allied disciplines. 2009;50(12):1459–1467. doi: 10.1111/j.1469-7610.2009.02123.x. [DOI] [PubMed] [Google Scholar]
- 17.Esbensen AJ, Seltzer MM, Krauss MW, MacLean JWE. Stability and Change in Health, Functional Abilities, and Behavior Problems Among Adults With and Without Down Syndrome. Am J Ment Retard. 2008;113(4):263–277. doi: 10.1352/0895-8017(2008)113[263:SACIHF]2.0.CO;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ray-Subramanian CE, Huai N, Ellis Weismer S. Brief report: adaptive behavior and cognitive skills for toddlers on the autism spectrum. J Autism Dev Disord. 2011;41(5):679–684. doi: 10.1007/s10803-010-1083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holland AJ, Hon J, Huppert FA, Stevens F. Incidence And Course Of Dementia In People With Down's Syndrome: Findings From A Population-Based Study. J Intellect Disab Research. 2000;44(2):138–146. doi: 10.1046/j.1365-2788.2000.00263.x. [DOI] [PubMed] [Google Scholar]
- 20.Zigman WB, Schupf N, Sersen E, Silverman W. Prevalence of dementia in adults with and without Down syndrome. Am J Ment Retard. 1996 Jan;100(4):403–412. [PubMed] [Google Scholar]
- 21.Seltzer MM, Greenberg JS, Hong J, et al. Maternal cortisol levels and behavior problems in adolescents and adults with ASD. J Autism Dev Disord. 2010 Apr;40(4):457–469. doi: 10.1007/s10803-009-0887-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994 Oct;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 23.Krauss MW, Seltzer MM. An unanticipated life: The impact of lifelong caregiving. In: Bersani H, editor. Responding to the challenge: International trends and current issues in developmental disabilities. Brookline, MA: Brookline Books; 1999. [Google Scholar]
- 24.Smith LE, Greenberg JS, Seltzer MM, Hong J. Symptoms and behavior problems of adolescents and adults with autism: effects of mother-child relationship quality, warmth, and praise. Am J Ment Retard. 2008;113(5):387–402. doi: 10.1352/2008.113:387-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Willett JB, Sayer AG. Using Covariance Structure-Analysis to Detect Correlates and Predictors of Individual Change over Time. Psychol Bull. 1994;116(2):363–381. [Google Scholar]
- 26.Bollen KA, Curran PJ. Latent Curve Models: A Structural Equation Perspective. Hoboken, NJ: John Wiley and Sons; 2006. [Google Scholar]
- 27.Muthen LK, Muthen BO. Mplus user's guide. 2nd ed. Los Angeles: Muthen and Muthen; 2001. [Google Scholar]
- 28.Matson JL, Dempsey T, Fodstad JC. The effect of Autism Spectrum Disorders on adaptive independent living skills in adults with severe intellectual disability. Research Develop Disab. 2009;30(6):1203–1211. doi: 10.1016/j.ridd.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 29.Kraijer D. Review of Adaptive Behavior Studies in Mentally Retarded Persons with Autism/Pervasive Developmental Disorder. J Autism Dev Disord. 2000;30(1):39–47. doi: 10.1023/a:1005460027636. [DOI] [PubMed] [Google Scholar]
- 30.Drahota A, Wood J, Sze K, Van Dyke M. Effects of Cognitive Behavioral Therapy on Daily Living Skills in Children with High-Functioning Autism and Concurrent Anxiety Disorders. J Autism Dev Disord. 2011;41(3):257–265. doi: 10.1007/s10803-010-1037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williams SK, Scahill L, Vitiello B, et al. Risperidone and adaptive behavior in children with autism. J Am Acad Child Adolesc Psychiatry. 2006;45(4):431–439. doi: 10.1097/01.chi.0000196423.80717.32. [DOI] [PubMed] [Google Scholar]