Abstract
Purpose
HIV/AIDS surveillance data are critical for monitoring epidemic trends, but can mask dynamic sub-epidemics, especially in vulnerable populations that under-utilize HIV testing. In this case study, we describe community-based epidemiologic data among injection drug users (IDU) and female sex workers (FSWs) in two northern Mexico-US Border States that identified an emerging HIV epidemic and generated a policy response.
Methods
We draw from quantitative and qualitative cross-sectional and prospective epidemiologic studies and behavioral intervention studies among IDUs and FSWs in Tijuana, Baja California and Ciudad Juarez, Chihuahua.
Results
Recognition that the HIV epidemic on Mexico’s northern border was already well established in subgroups where it had been presumed to be insignificant was met with calls for action and enhanced prevention efforts from researchers, NGOs and policy makers.
Conclusions
Successful policies and program outcomes included expansion of needle exchange programs, a nation-wide mobile HIV prevention program targeting marginalized populations, a successful funding bid from the Global Fund for HIV, TB and Malaria to scale up targeted HIV prevention programs and the establishment of binational training programs on prevention of HIV and substance use. We discuss how epidemiologic data informed HIV prevention policies and suggest how other countries may learn from Mexico’s experience.
Keywords: HIV, AIDS, surveillance, policy, Mexico, US border, epidemiology, injection drug use, sex work
I. Introduction
Surveillance data plays a critical role in monitoring epidemiologic trends and programmatic responses to infectious disease threats, both nationally and globally. There is a long history in public health disease control and prevention in which epidemiologic and surveillance data have informed policy and interventions to reduce or alter risk even in the absence of knowing the underlying mechanisms of disease transmission.1 In 1983, epidemiologic studies prior to the isolation of Human Immunodeficiency Virus (HIV) had already identified many risks factors for which control measure policies were subsequently developed.1,2 However, national and regional HIV/AIDS surveillance data can sometimes mask dynamic sub-epidemics that vary by country, region, sex or HIV transmission group, especially when HIV incidence is increasing in vulnerable populations that under-utilize HIV testing and treatment services. In many countries, HIV/AIDS surveillance data are limited to programmatic data from clinics testing antenatal women, those being screened for sexually transmitted infections (STI), or routine HIV testing among military personnel. The reliance on these types of sources, rather than HIV testing data drawn from community-based populations, can lead to erroneous conclusions about country-level HIV epidemic trends and the presumed impact of prevention interventions and policies.3
Among the country-level HIV prevalence estimates across the Americas, Mexico’s nationwide prevalence of 0.3% is among the lowest. By 2007, there were an estimated 200,000 HIV-positive persons living in Mexico, and at the end of 2008, a total of 124,505 reported AIDS cases, among whom the vast majority were attributed to homosexual/bisexual activity. Since the first AIDS case was reported in Mexico in 1983 until 2007, the male:female AIDS case ratio dropped from 10:1 to 3:5.4 Trends in national HIV prevalence data by gender and risk group were similar to AIDS incidence data, but among Mexico’s 32 states, Baja California –abutting California, USA-- has consistently had the highest cumulative AIDS incidence, second only to Mexico’s federal district, and the corresponding rate in the border state of Chihuahua has remained above the national average.5
In 2002, del Rio and Sepulveda reviewed and offered insights into Mexico’s HIV epidemic and the national response, concluding that Mexico had thus far averted a major HIV epidemic, in contrast to some of its neighbors (e.g., the U.S. and Honduras).6 They pointed to Mexico’s low national HIV prevalence, even among high risk populations such as female sex workers (FSWs), among whom available HIV prevalence estimates were <1%. They contended that unlike in the United States, the HIV epidemic in Mexico had remained 'nuclear', primarily affecting men who have sex with men (MSM) in urban settings such as Mexico City, Guadalajara, Monterrey and Tijuana.7 The proportion of AIDS cases attributed to the sharing of injection equipment among injection drug users (IDUs) in Mexico had consistently been <5%6 which was attributed to the relatively few number of IDUs in most cities.6 The authors further posited that this relative containment of the HIV epidemic was a consequence of multiple prevention efforts enacted by governmental and non-governmental organizations (NGOs). Since this review was published, epidemiologic data indicate that Mexico’s HIV epidemic has evolved, and that these assumptions require re-examination.
In this case study, we contrast Mexico’s national and state-level HIV epidemic profile with data drawn from cross-sectional and prospective cohort studies conducted in two northern Mexican cities bordering the United States (Tijuana in Baja California and Ciudad Juarez, Chihuahua). We then discuss how HIV/AIDS surveillance data initially perpetuated spurious assumptions about the HIV epidemic profiles in these states and in Mexico overall, which hampered timely responses for targeting appropriate prevention and treatment. We show how epidemiologic data used in conjunction with qualitative data led to the recognition that the HIV epidemic in the Mexico-US border region had already become well established in specific subgroups that had been presumed to be insignificant and isolated, many of whom were highly mobile. These data played a significant role in stimulating calls for action from researchers, NGOs and state policy makers. Several successful outcomes included formal endorsement and expansion of needle exchange programs as a critical component to a combined HIV prevention response and the creation of a nation-wide mobile HIV prevention program targeting marginalized populations. We discuss this experience in an international context and provide lessons learned to suggest ways in which other countries may benefit from how epidemiology played a key role in formulating policy for HIV prevention efforts. This case study also highlights the benefits of integrating research with training in a binational context, which is critical for capacity building and sustained policy responses in resource-limited settings.
II. Contextual Factors: A Conceptual Framework
As the HIV pandemic has unfolded, epidemiologic and behavioral research has identified the role that environments and social structures can play in the transmission process.8–10 While behaviors of individuals are central to HIV transmission, the non-random nature of HIV transmission suggests that disease spread is influenced not only by virus-host interactions, but by differences in cultural, political, economic, geographic and social conditions8–13
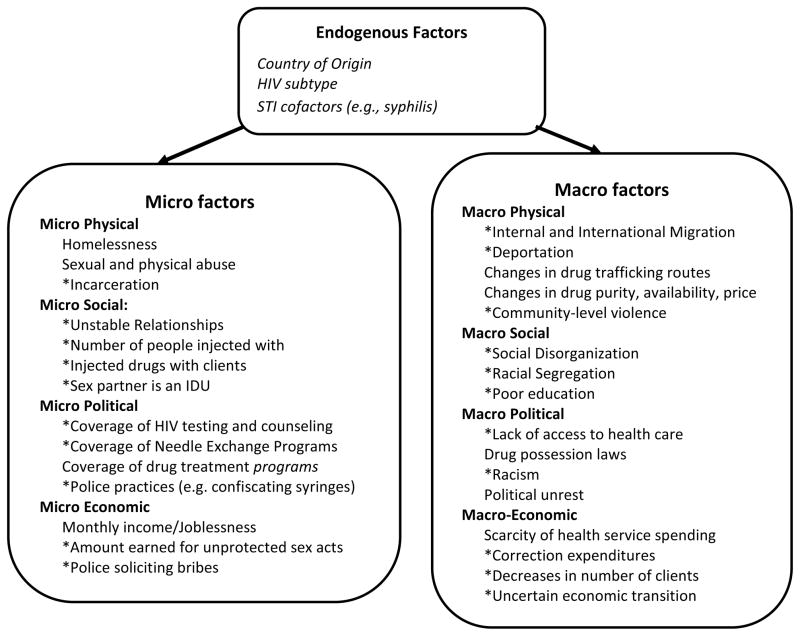
The underlying framework that best characterizes our perspective on the intersection between epidemiologic data and HIV prevention responses in an international context is that of risk environments10,14,15 and its corollary of risk clusters.16 Rhodes and colleagues14,17 describe the “HIV risk environment” as the space-- whether social or physical-- in which the interplay of factors exogenous to the individual increases their likelihood of engaging in risky behaviors that predispose to HIV infection, or decreases their likelihood of accessing HIV prevention or treatment.15,17 These exogenous factors can be categorized in terms of types (i.e., physical, social, economic, policy) that interact at the micro and macro levels of environmental influence. There are several important implications of this perspective.
First, this heuristic implies that HIV prevention is not merely a function of an individual’s behavior, but also a function of social, economic and policy environments that act as ‘risk regulators’ to present constraints and/or opportunities that shape individual behaviors.18 This approach therefore shifts of the onus of responsibility for behavior change away from the individual, towards governments and policymakers who should be tasked with creating and sustaining environmental conditions that promote safer behaviors.11,17
Second, the concept that HIV risk stems from a confluence of environmental factors operating at multiple spheres of influence requires that epidemiologists go beyond a narrow characterization of individual behaviors that confer protection or risk, to measure contextual circumstances that can help uncover the interactions, processes and pathways that explain disease risk.11 Mixed methods approaches that integrate classical epidemiologic data collection with social science methodologies (e.g., ethnographic and qualitative data collection) are especially useful, and can be incorporated into case-control studies, prospective cohorts or randomized controlled trials.19
Finally, the risk environment heuristic is consistent with the notion that HIV infections do not occur randomly within a population, and are prone to clustering.16 It is not just a matter of which environmental factors are operating, but the fact that some subpopulations are more likely than others to experience a social structure in which risk factors intersect and cluster to potentiate HIV spread within a network.13 Farley’s conceptual model of risk clustering suggests that it is not each risk factor itself that creates risk for HIV infection, but rather the circumstances of how they cluster together to create an almost inescapable vulnerability.16 Below and in Figure 1, we describe factors at the physical, social, economic, and policy environment that appear to influence the HIV risk environment and risk clustering on the Mexico-US border, based on the cumulative body of research.
Figure 1.
Conceptual Framework Depicting Factors in the HIV Risk Environment Operating in the Mexico-US Border Region
* Factors supported by research in Mexico
Unique Features of the HIV Risk Environment in the Mexico-US Border region
The geographic and social landscape helps explain why the Mexico-U.S. border region is at heightened risk for infectious diseases such as HIV. Like many border regions, it is characterized by an economically disadvantaged population, and exists as a nexus for drug use, prostitution and mobility, as described below.
Place
The 2,000 mile border between the U.S. and Mexico, which is the most extensive land frontier separating a developed and developing country, is a study in contrasts. The gap in median incomes between inhabitants of Mexico and the U.S. is the largest between any two contiguous countries.20 Of the 12.5 million people living in the Mexico-US border region, 5.7 million live in Mexico, of whom, more than one quarter live below the poverty index and only 41% of those aged 25 years and older have completed elementary school education.20 If this border region were to constitute the 51st U.S. state, it would rank last in health care access and per capita income. It would also rank first in the number of school children living in poverty and without health care.21 Among the 6 Mexican-U.S. border states, Baja California has among the highest number of physicians per capita (125 per 100,000), but the lowest number of hospitals/clinics (8.4 per 100,000).20
The inhabitants of the Mexico-US border region tend to be young; 28.0% of Mexican border inhabitants are less than 13 years old.20 The large youth population in Mexico combined with their HIV-related vulnerabilities is one of the concerning factors that should drive prevention efforts. A significant percentage of Mexican youth (81%) start drinking by the age of 1422,23 and come into contact with drugs or psychoactive substances between the ages of 12 and 29 years of age.22,24
Drug Trafficking and Drug Use
After Colombia, Mexico is the second most important source of heroin entering the U.S;25 90% of all methamphetamine entering the USA is produced in Mexico, and 70% of all cocaine entering the U.S. passes through Mexico26 en route from South America. As a consequence, Tijuana and Cd. Juarez are situated on major drug trafficking corridors.25 Illicit drug use—particularly injection drug use—has increased in Mexico over the past 10 years as local consumption markets emerged along these trafficking routes. In 1988, the first National Addictions Survey (NAS) reported that 0.1% of the Mexican population used heroin, of whom 17,000 reported use in the previous year. By the time NAS was conducted in 1993, 30,000 Mexicans reported heroin use in the previous year.27
The highest consumption of illegal drugs in Mexico is in Baja California. The proportion of the general population in Tijuana aged 12–65 years who reported having ever used an illegal drug was 15%, almost three times the national average.28 In Mexico overall, men were 13 times more likely than women to have ever used an illicit drug, but in Tijuana the ratio was 6:1.28 Tijuana has one of the fastest growing IDU populations in Mexico. By 2002, heroin was the primary reason for seeking treatment for those attending drug treatment facilities in Tijuana;29 among those, nearly half reported that their onset of illicit drug use was between 10–14 years of age. Officials estimate there were ~6000 IDUs attending shooting galleries in Tijuana in 2003, but the total number of IDUs in the city is thought to be closer to 10,000.30
Among Mexican cities, Cd. Juarez is ranked second only to Tijuana in the number of illicit drug users, which is twice the national average. In 2001, it was estimated that there were ~6,000 ‘heavy heroin users’ in Cd. Juarez and as many as 186 ‘picaderos’ [shooting galleries]31 where IDUs rent and/or buy used needles. At least 200 picaderos were known to authorities in Tijuana in 2003.30 Shooting galleries are uncommon in Western U.S. cities but are well known in the eastern U.S. and Puerto Rico, which experienced dramatic IDU-associated HIV epidemics linked to needle sharing in these establishments.32 But addiction and infectious diseases are not the only health problem Mexico experiences related to drug use. Since 2007, over 20 000 drug-related fatalities occurred nationwide in Mexico in association with warring drug trafficking organizations. Ciudad Juarez and Tijuana have borne a disproportionate number of these deaths.
Legal and Social Context of Sex Work
Sex work is quasi-legal in Mexico. Sex with FSWs is encouraged as a display of virility and “machismo” at all socioeconomic levels.33 Many Mexican-U.S. border cities have thriving prostitution districts, or zona rojas (red light districts), frequented by thousands of U.S. and foreign tourists each year. Qualitative research suggests that most sex workers enter prostitution out of economic necessity, perhaps due to a failed relationship or poor working conditions in maquiladoras (manufacturing plants), and 95% have children.34 In some cities, such as Tijuana, a registration permit is required to practice sex work in the zona roja, but in practice, about half of the city’s estimated 9000 FSWs work without permits35 and less than 5% of FSWs who inject drugs have permits. In other cities, such as Ciudad Juarez, the zona rojas exist less formally and many sex workers have been recently displaced due to gentrification.
In Tijuana, FSWs who work in bars, motels, massage parlors and street corners are typically highly concentrated within the zona roja, and a spatial epidemiology study indicated that relatively few sex work venues accounted for a large proportion of the STI burden.36 In addition, FSWs working at high risk venues were more likely to speak English, to report drug use during sex, and were less likely to be registered with the health department. The zona roja in Tijuana also overlaps the Zona Norte, a border neighborhood known for its high density of IDUs, which leads to overlapping risks. In a recent study, nearly half of FSWs who injected drugs in Tijuana and Ciudad Juarez had initiated sex work before age 18, and those that did so were more likely to report that their initiation into injection drug use had been through force.37 In our study of 400 male U.S. and Mexican men who had paid for sex with FSWs in Tijuana, half reported having unprotected sex with FSWs within the last four months,38 which was associated with drug use during sex.39
Migration, Cross-border Mobility and Deportation
Vast economic disparities between the US and Mexico have fueled a major migration boom, drawing Mexican migrants to the US and its border cities in search of employment. The number of manufacturing plants in the region exploded after North American Free Trade Agreement; by 2001, 2,700 maquiladoras were operational predominantly from US businesses. Between 1990 and 2000, the Mexico-US border region experienced a 21% increase in population size,40 more than double the US national average.40
The Mexico-US border region is also characterized by high levels of cross-border mobility. In 2008 alone, there were 44 million registered northbound crossings from Tijuana to San Diego County,41 making this the busiest land border crossing in the world. Mobile populations are often at higher risk of acquiring HIV, due to changing social networks in the context of social isolation, loneliness and the lure of anonymity.42 Our study of U.S. male clients of FSWs who had paid for sex in Tijuana in the last year found that they had crossed the border to pay for sex a mean number of 26 times.38 Tijuana and Ciudad Juarez are also primary corridors for migrants and truckers traveling from Central America and Southern Mexico en route to the U.S. Similar dynamics of truck routes as major corridors for HIV/STI transmission have been seen in South Africa43 and in the US with drug users from the Northeast traveling to the South via I-95.44,45
US immigration policies pose a considerable challenge to HIV prevention efforts in the US and in Mexico. In the US, undocumented persons are ineligible for health care, and unable to access HIV testing and treatment. Between 1999-2007, the U.S. deported ~4.8 million migrants to Mexico; of these, ≥1.1 million migrants (~23%) were deported to Tijuana.46,47 Many deportees stay in Tijuana to await U.S. re-entry; in 2010, over half of those detained at the U.S.-Mexico border had been detained previously. Deportees are typically left at the border with no identification, few possessions, and no source of income. Many turn to drug dealing, substance use or sex work out of desperation.48
High levels of voluntary and involuntary mobility have influenced the socio-demographic profile of populations at high risk for HIV infection, along with their drug use and HIV risks. Among female sex workers (FSWs) and IDUs in Tijuana and Ciudad Juarez, more than two-thirds are migrants, primarily from southern Mexican states and Central America.49,50 Nearly half of migrants voluntarily returning to Mexico have ever used illicit drugs.51 Among male IDUs in Tijuana, those who had been deported from the US were more likely to have inject drugs daily, but were less likely to receive medical care, to have ever been tested for HIV or to have attempted drug treatment.50
Cross-border HIV transmission is bi-directional. Across Mexico, 12.7% of Mexico’s accumulated HIV cases reported through 2000 were migrants to the U.S.52 On the other hand, the proportion of reported AIDS cases of Hispanic origin in San Diego County more than doubled from 19% during 1985–1989 to 44% during 2000–2004.53 Without proper context, these statistics can spark a ‘blame game’ through which each country feels that its HIV cases are the fault of the other, undermining efforts to improve HIV prevention and treatment on both sides of the border.
The Role of Religion
Almost 95% of Mexicans are Roman Catholics.22 The strong influence of the Catholic Church has thwarted attempts to make condoms widely accessible.54 In Mexico, some of those most vulnerable to the risk of HIV infection are those engaging in survival sex. Advocating for the use of a condom to prevent HIV transmission may seem reasonable, but this kind of leadership is largely lacking in Mexico. This opposition by the Church makes it difficult if not impossible in some areas to freely distribute condoms as a part of HIV prevention. For example, Church leaders in Tijuana have vehemently opposed harm reduction measures.54 In both Tijuana and Ciudad Juarez, various religious groups frequently operate drug treatment programs, some of which are not regulated by the state and have been accused of human rights violations.55
Access to Sterile Syringes
The U.S. Congressional ban on federal support for needle exchange programs (NEPs) and the U.S. lobby to prevent neighboring countries from supporting harm reduction contributed to Mexico’s slow adoption of NEPs. Until the mid-2000s, the only active Mexican NEP was operated by a nongovernmental organization (NGO) in Ciudad Juarez, which began in the late 1980s and was unofficially sanctioned by Chihuahua’s Secretary of Health. In 2004, Tijuana opened the second NEP in the country, operated by Prevencasa A.C.56,57 Meanwhile, CENSIDA and the National drug program (CONADIC) published a position paper supporting harm reduction, including NEP, in 2003,57 but its impact was limited until epidemiologic data spurred health officials to enact them more broadly (see timeline, Table 1).
Table 1.
Timeline Depicting HIV Epidemiology Surveillance and Research in Mexico and the Response in the Mexico-US Border Region
| 1983 | First AIDS case reported in Mexico |
| 1986 | First heterosexual case of HIV among an IDU reported to the Mexican Federal health authorities |
| 1988 | Needle exchange began informally in Ciudad Juarez by an NGO (Programa Compañeros) |
| 1990 | Federal epidemiological HIV Surveillance in IDUs began in Baja California |
| 2000 | CONASIDA and the NGO Programa Compañeros published the first harm reduction manual |
| 2003 | The Mexican federal government published a position paper with the first open endorsement of the harm reduction programs |
| 2004 | The Mexican federal government develops workshops in Mexican border states for the implementation of harm reduction activities |
| 2005 | Baja California, Chihuahua and Sonora formally begin needle exchange programs |
| 2006 | Conasida began to distribute syringes to state level AIDS programs |
| 2007 | Conasida commissioned a fleet of ‘condonetas’ for all Mexican states, inspired by Tijuana’s Prevemovihl and the NGO Colectivo Sol's Condomovil in Mexico City |
| 2007 | Needle exchange programs now formally operating in 7 Mexican states (Baja California, Chihuahua, Coahuila, Nuevo Leon, Oaxaca, Sonora, Zacatecas) |
| 2007–2008 | Mexican federal government establishes the first free-standing HIV/AIDS clinics in Tijuana and Ciudad Juarez (CAPACITS clinics) |
| 2008 | During the International AIDS Conference in Mexico City CONASIDA and Baja California authorities presented the first harm reduction video with BC minister of health promoting harm reduction |
| 2009 | Possession of small amounts of illicit drugs were de-criminalized across Mexico Mexico was awarded $76M in Global Fund resources in response to the HIV epidemiological data presented |
| 2010 | Mexican federal authorities signed the Vienna Declaration (www.viennadeclaration.com) |
| 2010 | Baja California Secretary of Health and federal Mexican health authorities publish Lancet commentary embracing harm reduction and decriminalization |
II. Epidemiologic Studies of HIV and STIs among IDUs and FSWs in Tijuana and Ciudad Juarez
The first sign that drug use was more closely linked to HIV infection in the Mexico-US border region than early surveillance data had suggested arose from a study of >1000 pregnant women in Tijuana in 2003.58 HIV prevalence was 1% overall and 6% among those who used drugs; all HIV cases were previously unidentified. Although Mexico reports low numbers of HIV-infected infants, Baja California and Chihuahua have had among the highest rates of congenital syphilis in Mexico,59 which was an early warning that untreated syphilis could be serving as a cofactor of HIV transmission.
From 2004–2006, baseline results from a study of 924 FSWs in Tijuana and Cd. Juarez found that HIV prevalence was 8%; correlates of HIV infection included injection of cocaine and snorting/smoking methamphetamine.60 HIV prevalence was 12% among the sub-sample of FSWs who inject drugs in these cities, among whom nearly half had at least one active STI.61 HIV incidence among FSWs randomized to the control group of a subsequent behavioral intervention was 2 per 100 person-years.62
In 2004, a qualitative study of IDUs in Tijuana and Ciudad Juarez was conducted through a partnership between UCSD researchers (authors SS, TP and CMR), Mexican NGOs (Programa Companeros and ProComuSIDA), and Mexican health officials at the municipal, state and federal levels. This study found that in both cities, needle sharing was normative, and that problematic police practices such as confiscating syringes and arresting the IDUs based on their disheveled appearance led IDUs to resort to injecting in shooting galleries (i.e., places where IDUs inject drugs in groups with syringes that are rented or bought).30,63 Despite the fact that it was legal to purchase syringes at pharmacies without a prescription in Mexico, in-depth interviews found that pharmacists often refused to sell syringes to IDUs, or charged them exorbitant prices, taking advantage of their desperate need to assuage their withdrawal symptoms.30,64
Drawing from these observations, a cross-sectional study subsequently recruited 207 IDUs in Tijuana and 197 in Ciudad Juarez through respondent driven sampling (RDS). In Tijuana, recruitment of street-based IDUs was facilitated by the use of a modified recreational vehicle donated by the UCSD research team to one of the NGO partners. This ‘prevemovihl’ (HIV prevention mobile) successfully accessed high risk participants in the callejones (alleys), and in the rural colonias (neighborhoods). In both cities, HIV prevalence was low at 3%,65 but HCV prevalence was 95%.66 These data suggested that sharing of needles and other injection equipment in these cities could support an HIV epidemic, since parenteral transmission of HCV and HIV is highly efficient. In particular, police confiscation of used and sterile syringes was associated with three-fold higher odds of receptive needle sharing in both cities.67
A subsequent prospective study of 1056 Tijuana IDUs funded by the National Institute on Drug Abuse found that HIV prevalence among male IDUs remained low at 4% from 2006–2008, but had risen to 10% among female IDUs.68 Social and structural factors were more closely associated with HIV infection than individual-level behaviors. Specifically, among male IDUs, factors independently associated with HIV infection included injecting in groups, deportation from the U.S. and being arrested for carrying used syringes, whereas among female IDUs, HIV risk was independently associated with living in Tijuana for longer durations.68 A spatial analysis of HIV infections also found that these HIV infections were initially clustered in the Zona Norte, but incident HIV infections became dispersed after 2006, which coincided approximately with the escalation of violence and federal army presence that displaced many IDUs.69 A later study among FSWs who injected drugs in Tijuana and Cd. Juarez found that police confiscation of syringes and sharing needles with clients were both independently associated with HIV infection.70
In addition to identifying environmental factors that exacerbated HIV risk behaviors, we found low coverage of HIV and STI testing and treatment programs, which appeared to be due in part to their centralized locations outside of the highest risk neighborhoods. In Tijuana and Ciudad Juarez, data from 2004–2006 suggested that only 49% of FSWs and 30–38% of IDUs had ever had an HIV test.71 Syphilis was consistently identified as being independently associated with HIV infection among IDUs, FSWs and their clients.38,60,72 This was not surprising since approximately half of these syphilis infections had titers > 1:8, which is consistent with active infections that facilitate HIV transmission. Collectively, these studies suggest that factors operating at various levels in the HIV risk environment were central to shaping individual HIV risk behaviors in both cities.
Data accumulating from these epidemiologic studies were among the first estimates of HIV prevalence among FSWs and IDUs in the Mexico-US border region, and began to challenge assumptions that had been made about the context of the Mexican HIV epidemic. First, these data underscored the extent to which Mexico’s HIV epidemic was not a single epidemic, but had become regional sub-epidemics. Second, HIV prevalence among FSWs and female IDUs in Tijuana and Ciudad Juarez was much higher than expected based on HIV surveillance data. Third, it was now indisputable that there was considerable overlap between communities engaged in sex work and drug use. Finally, the importance of the HIV risk environment in shaping individual-level HIV risk behaviors could not be ignored, indicating that the responsibility for change should rest more on the shoulders of policy makers and program planners, rather than individuals themselves or the small under-resourced NGOs that served them.
III. Leveraging Data to Influencing Policy: The Role of Epidemiology
How could these epidemiologic data be leveraged to generate thoughtful policy changes without the US or Mexico blaming each other for its HIV epidemic? Members of our binational team, which included federal and state health officials, NGO leaders and researchers, spent long hours contemplating this problem and embarked on a strategy to elicit a binational response. Based on available HIV prevalence and census data, we conducted a modeling exercise to estimate the number of HIV-infected persons in Tijuana using a ‘low risk’ and a ‘high risk’ scenario. In the high risk scenario, models were generated based on the upper end of the 95% confidence intervals for each HIV prevalence estimate, which suggested that one in 125 persons aged 15–49 in Tijuana was HIV-infected in 2005.73 These data indicated that that the city’s HIV epidemic had moved from low-level to concentrated, according to UNAIDS categorizations. Epidemiologic data were used to demonstrate the extent to which mobility was bi-directional among high risk populations at the Mexico-US border, which emphasized the potential for cross-border transmission of HIV and STIs from north to south or vice versa. Coinciding with its publication in 2006, the findings from this paper were prepared in a press release in Spanish and English, shared with municipal, state and federal health officials in Mexico before the press embargo was lifted, and released simultaneously to media in both countries. The findings received widespread coverage in both countries, and the research team was subsequently invited to present policy recommendations to the Governor of Baja California and the Mayor of San Diego in a joint meeting. Meanwhile, the Secretary of Health of Baja California, who had formerly served as the Health Commissioner in Tijuana stated publicly that he endorsed NEPs as a critical component of a comprehensive strategy to prevent HIV infection. By 2008, dedicated HIV clinics (CAPACITS) were established in Tijuana and Ciudad Juarez. However, in Tijuana, local pressures from some religious and political figures forced the clinic to be located away from colonias where HIV was most concentrated, which remains a barrier to HIV care for vulnerable populations without means of transportation.
In 2007, following the example of using mobile vans for HIV prevention service delivery that had been employed both in Mexico City and by our NGO partner’s Prevemovihl in Tijuana, federal and state health officials in Mexico commissioned a fleet of customized mobile vans that would later be delivered to every Mexican state. Equipped with a loudspeaker on the roof, a TV screen in the rear, adequate space for outreach workers to provide condoms and exchange syringes, and painted neon green with caricatures of dancing condoms, the condoneta was born. In conjunction, the national guidelines supporting harm reduction that had been published by CENSIDA without fanfare in 2005 now had ample epidemiologic data to justify the implementation of NEPs across Mexico. By 2007, there were small-scale NEPs supported by Mexico’s federal government operating in seven states–Baja California, Chihuahua, Coahuila, Nuevo Leon, Oaxaca, Sonora, Zacatecas, and by 2010, nine Mexican states had NEPs.
The team also learned that the press could wield a double-edged sword. In 2008, a study of the male clients of FSWs in Tijuana showed that HIV prevalence was 5%, and was equivalent among the clients who lived in the U.S. versus Mexico.38 More than two thirds of FSWs in Tijuana and Ciudad Juarez reported being patronized by clients from the U.S.; these FSWs reported a greater tendency to inject drugs, have syphilis and engage in unprotected sex for higher pay.74 However, the highly politicized nature of these data proved difficult to manage; the headline from the San Diego Tribune read: “Sex with Americans Risky for Mexican Hookers.”
A more successful approach was met by working with U.S. health officials at the National Institute of Health to identify research questions that were of public health significance to both Mexico and the U.S, which subsequently led to six successful peer-reviewed R01 grant applications with Mexican Co-PIs. In addition to funding received by the National Institute on Drug Abuse (NIDA) to study risk factors for HIV infection among IDUs at the individual, social and environmental level, both NIDA and the National Institute of Mental Health funded behavioral intervention studies aimed at increasing condom use and reducing drug-related risk behaviors among FSWs and their clients. One such study demonstrated that a brief intervention incorporating motivational interviewing and role play surrounding condom use negotiation was associated with a 40% reduction in HIV/STI incidence among FSWs in Tijuana and Ciudad Juarez.62 A subsequent project was recently funded by NIMH with support from the Mexican federal government to study the organizational factors that promote or impede the scale-up of this intervention in twelve Mexican cities.
In 2010, NIDA funds were awarded to study the impact of drug policy reform on drug use behaviors in Tijuana, following Mexico’s enactment of an unprecedented law that deregulates possession of small specified amounts of cocaine, heroin, methamphetamine, and marijuana for personal use.75 The law specifies that police who apprehend individuals who possess sub-threshold amounts of these drugs will not pursue penal action until a third apprehension, when such individuals will be required to enter drug treatment or jail. This law is intended to re-direct law enforcement to drug dealers and traffickers, while embracing more of a harm reduction approach with the scale-up of NEPs and methadone maintenance treatment programs. Whether these reforms will have an impact on risk behaviors and HIV incidence is an open question, but in a high-profile Lancet commentary, national and state-level policy makers publicly pledged to ensure that their future health and drug policy decisions are evidence-based and grounded in a human rights approach.76
Mexico’s evolving HIV epidemic also garnered an international response. In 2009, Mexico was successful in its bid to secure funds from the Global Fund for HIV, TB and Malaria for the first time. HIV prevalence and incidence data from the epidemiologic studies conducted on Mexico’s northern border were instrumental in showing that HIV prevalence had surpassed 5% in more than one risk group, which was a requirement for Global Fund eligibility. Accordingly, $76M USD was awarded to scale up HIV prevention programs, which includes support for IDUs in Tijuana and Ciudad Juarez, as well as two cities where HIV prevalence among IDUs had recently begun to rise (i.e., Hermosillo and Guadalajara).
Central to the success of these studies is a commitment to recognizing binational partnerships. Study findings were published following guidelines for publication that were generated by the team that were included both US and Mexican partners. NIDA, the Fogarty International Center, Hispanic Serving Health Professions Schools and USAID also provided funding to support training programs to develop research skills and programmatic capacity-building for both U.S. and Mexican students and fellows. The majority of the team’s publications to date have been led by students and fellows, many of whom are Mexican or Mexican-American.
IV. Lessons Learned
Textbox 1 contrasts our experience in Mexico to an international case example that has been reported upon extensively in the HIV prevention literature: 1) The 100% Condom Campaign in Bangkok, Thailand. In the Thai example, epidemiologic data were used to generate political will for a structural HIV prevention intervention enforcing brothels to comply to consistent condom use or suffer closure. This was shown to be a highly effective policy for controlling HIV transmission in brothel-based FSWs.
Text Box 1.
Example of the Thai Government’s Effective HIV Prevention Policies and Strategies and their Impact - 1991–1993
| Policy/Strategy | Impact |
|---|---|
| Early recognition of HIV as a national health problem by both the Public Health Community and Government | Early coordinated collaboration and call to action by two influential public sector partners focusing on the urgency of the problem88 |
| Careful analysis of the epidemiological data and trends, especially among sub populations | Early identification of and focus on the more urgent impact and problem of HIV among sex workers and their clients89 |
| Focus on HIV as a Public Health/Medical issue | Key partners were able to sidestep issues of morality and religion and focus on “high risk behaviors” instead of “high risk groups” to prevent HIV infections88 |
| Deliberate and focused plan to recruit key community stakeholders, using evidenced based data and information on the current and future impact of HIV on the country | |
| Ongoing epidemiological surveillance and evidence based risk reduction interventions among sex workers and their clients. | Initiated the 100% condom use program in brothels. 87,90 Increase in the use of condoms by sex workers from 14% in 1989 to 90% by 1992.90
|
Reliance on HIV/AIDS Surveillance Data Can Mask Emerging Regional Trends
Our case study illustrates how Mexico’s early reliance on national and state-level HIV/AIDS surveillance data masked an emerging HIV sub-epidemic on the Mexico-US border. HIV/AIDS surveillance data from India have also generated mis-leading results when inappropriately extrapolated to the regional level, which led the estimated number of HIV-infected persons in India to be revised significantly downward.77 In a review of the quality of HIV/AIDS surveillance data from 127 low and middle-income countries,78 a fully functioning surveillance system was operating in only 40 countries. The authors recommended that countries with low-level and concentrated epidemics should focus on collecting serologic and behavioral data from all high risk populations, which would provide an early warning signal if HIV prevalence and incidence begins to escalate.
Simple Epidemiologic Data Can Generate Powerful Responses
Often, epidemiologic researchers rely on large scale studies such as longitudinal cohort studies which require significant time and resource investments to determine solutions. As demonstrated in this case study, descriptive data, such as estimates of HIV prevalence, incidence and associated risk behaviors, can sometimes be sufficient for stimulating an effective policy response. By showing that HIV prevalence among some sub-populations in the Mexico-US border region had surpassed the critical threshold of 5%, we demonstrated that the HIV epidemic in this region had shifted from ‘low level’ to ‘concentrated’, making Mexico eligible to receive a large contract from the Global Fund. Coupled with qualitative data to provide context, simple epidemiologic data collected from multiple sub-groups was also used to generate an epidemic profile that informed policy makers and program planners. This implies the need for community-based partnerships that facilitate the development of trust and sharing of information especially when working with marginalized populations that typically fall outside the health care system, and across borders.
The Importance of Risk Environments
Traditionally, epidemiologists are concerned with how individuals behave and focus interventions at the individual level. In this case study, environmental factors appeared to be the most important drivers of individual level risk behaviors68,70 which is consistent with the HIV risk environment heuristic8,11,17 and incident HIV cases appeared to cluster69 which supports Farley’s conceptual framework.16 Moreover, systems and structural factors were found to inhibit some subpopulations from accessing prevention programs. As shown in Table 2, factors operating in the physical environment (voluntary and involuntary migration), social environment (police and pharmacists’ practices that limited access to sterile syringes), economic environment (poverty, coupled with economic disparities between the U.S. and Mexico), and policy environment (low coverage of HIV and STI testing and treatment) were important underlying factors driving HIV transmission, consistent with Rhodes’ heuristic of the HIV risk environment.14,17 These findings exemplify how epidemiologic data were used to shift the responsibility for interventions towards governments and policy makers and away from individuals. The research studies presented in this case study were also informed by theory, which aided in their application to theory-based interventions. Embedding qualitative research in epidemiologic study designs was also shown to provide invaluable context and insights into potential mechanisms of risk and protection.
Table 2.
Environmental HIV Risk Factors operating in the Mexico-US Border Region: Implemented Interventions and Recommendations
| HIV Risk Environment Concept A | Environmental HIV Risk Factors Identified | Recommended Intervention | Interventions Implemented |
|---|---|---|---|
| Physical | |||
| Macro Physical |
|
|
-- |
| Macro Physical |
|
-- | |
| Macro Physical |
|
-- | |
| Macro Physical |
|
|
|
| Micro Physical |
|
||
| Social | |||
| Micro Social |
|
|
|
| Macro Social |
|
-- | |
| Micro Social |
|
|
|
| Economic | |||
| Macro Economic |
|
|
|
| Micro Political |
|
|
-- |
| Micro Economic |
|
-- | |
| Policy | |||
| Micro Policy |
|
||
| Micro Policy |
|
|
|
| Macro Policy |
|
|
|
| Macro Policy |
|
-- | |
| Macro Policy |
|
Mobilizing Key Stakeholders is Critical for Generating Timely Policy Responses
This case study illustrates how involvement of policymakers and partners at all levels from inception is critical for developing trust, which in turn facilitates an appropriate and timely policy response. In this context, the team sought to include both Mexican and U.S. researchers, and local NGOs. We engaged Mexican health officials at the municipal, state and federal levels who not only were passive actors in terms of receiving information, but at times played an active role in disseminating study results and interpreting it for the public. For example, Baja California’s Secretary of Health presented results from our study at the International AIDS Conference in Mexico City in 2008,79 and was lead author on a commentary in Lancet that outlined his strategy for preventing HIV and other drug-related harms,76 setting an example for other Mexican states. The case study also showed the benefits of a well-executed communication plan, by jointly issuing press releases in the US and Mexico in English and Spanish, to ensure that communities on both side of the border had equal access to study results which were used to justify the development of HIV prevention policies.
V. Conclusion
This case study illustrates how epidemiologic data were used to develop HIV prevention policies directed at the Mexico-US border region. The body of research presented identified several avenues for intervention that address structural factors that potentiate HIV risks, some of which have been met with action, whereas others have yet to be addressed (see Table 2). For example, police continue to confiscate syringes from drug injectors in both Tijuana and Ciudad Juarez, which undermines harm reduction initiatives such as NEPs. While curricula have been developed to sensitize police to harm reduction, it has yet to be incorporated widely into police trainings across Mexico. Elsewhere in the U.S. and in South Asia, success has been met with police trainings that integrate HIV prevention with occupational safety (i.e., prevention of needle-stick injuries) to help align law enforcement with public health goals.80,81
Religious opposition to the promotion of condoms and sterile syringes in Mexico is another persistent barrier. In South Africa, advocating for the use of a condom not for contraceptive purposes, but to prevent the transmission of HIV has been endorsed by an Archbishop.82 In a 2010 interview,83 Pope Benedict openly stated that condom use for HIV prevention may be “justifiable in certain situations.” While there has been much debate by religious leaders regarding what the Pope actually meant, this was the first time the qualified endorsement of condom use for HIV prevention has come directly from a Pope, marking an apparent, albeit subtle, policy shift in the Vatican’s thinking. This may prove useful for Catholic prelates and pastors in Mexico and other countries for supporting local efforts in the use of condoms to prevent HIV infections. Further development of HIV prevention policies in the Mexico-US border region will therefore need to engage leaders outside the health sector.
Increased awareness of the value and benefits of considering an ecological approach to assessing “environments of risk” for HIV infection, not just individual behaviors, and the subsequent training of epidemiologists, public health scientists and other professional and lay workers on the ecological model and approach should lead to more efficient and targeted HIV prevention interventions throughout the world. Ongoing critical examination of effective and innovative evidence-based approaches to HIV prevention and the sharing of successful policies and strategies with those on the frontlines should be a high priority in the struggle against the HIV pandemic.
Acknowledgments
The authors would like to thank Ross Brownson, Ph.D. for his vision of the overall project as well as the Policy Board of the American College of Epidemiology and Peter Hartsock, Ph.D. of the Division of Epidemiology, Service, Prevention and Research at the National Institute of Drug Abuse for his keen insights. Work on this manuscript was supported by the American College of Epidemiology and the following grants from the National Institutes of Health: R37DA019829, R01DA023877, R01MH065849, D43TW008633 and R01DA20826. We thank Jessica Hutchinson for assistance with manuscript preparation. All of the ideas expressed in the manuscript are those of the authors and should not be attributed to the funding agencies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Steffanie A. Strathdee, Division of Global Public Health, Department of Medicine, University of California, San Diego, La Jolla, California.
Carlos Magis-Rodriguez, Programa de SIDA de la Ciudad de México, Mexico City, Mexico.
Vickie M. Mays, Departments of Psychology and Health Services, University of California, Los Angeles and UCLA Center for Research, Education, Training and Strategic Communication on Minority Health Disparities.
Richard Jimenez, School of Public Health, College of Health Sciences, Walden University, Minneapolis, MN.
Thomas L. Patterson, Department of Psychiatry, University of California, San Diego, La Jolla, California.
References
- 1.Catchpole MA. The role of epidemiology and surveillance systems in the control of sexually transmitted diseases. Genitourin Med. 1996;72(5):321–329. doi: 10.1136/sti.72.5.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prevention of acquired immune deficiency syndrome (AIDS): report of inter-agency recommendations. MMWR Morb Mortal Wkly Rep. 1983;32(8):101–103. [PubMed] [Google Scholar]
- 3.Walker N, Garcia-Calleja JM, Heaton L, Asamoah-Odei E, Poumerol G, Lazzari S, et al. Epidemiological analysis of the quality of HIV sero-surveillance in the world: how well do we track the epidemic? AIDS. 2001;15(12):1545–1554. doi: 10.1097/00002030-200108170-00012. [DOI] [PubMed] [Google Scholar]
- 4.Magis-Rodriguez C, De Luca M, Bravo-Garcia E, Rivera-Reyes P, Ortiz-Mondragon R, Gayet C. The AIDS epidemics in Mexico up to 2008. Gaceta Med Mex. 2010;146(1):45–49. [PubMed] [Google Scholar]
- 5.Strathdee SA, Magis-Rodriguez C. Mexico's evolving HIV epidemic. JAMA. 2008;300(5):571–573. doi: 10.1001/jama.300.5.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.del Rio C, Sepulveda J. AIDS in Mexico: lessons learned and implications for developing countries. AIDS. 2002;16(11):1445–1457. doi: 10.1097/00002030-200207260-00001. [DOI] [PubMed] [Google Scholar]
- 7.Tapia-Conyer R. Epidemiology of AIDS in Mexico, 1983–1996 [in Spanish] Gaceta Med Mex. 1996;132(supl 1):41–45. [Google Scholar]
- 8.Rhodes T, Ball A, Stimson GV, Kobyshcha Y, Fitch C, Pokrovsky V, et al. HIV infection associated with drug injecting in the newly independent states, Eastern Europe: the social and economic context of epidemics. Addiction. 1999;94(9):1323–1336. doi: 10.1046/j.1360-0443.1999.94913235.x. [DOI] [PubMed] [Google Scholar]
- 9.Poundstone KE, Strathdee SA, Celentano DD. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiol Rev. 2004;26:22–35. doi: 10.1093/epirev/mxh005. [DOI] [PubMed] [Google Scholar]
- 10.Rhodes T, Simic M. Transition and the HIV risk environment. BMJ. 2005;331(7510):220–223. doi: 10.1136/bmj.331.7510.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, et al. HIV and risk environment for injecting drug users: the past, present, and future. Lancet. 2010;376(9737):268–284. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Degenhardt L, Mathers B, Guarinieri M, Panda S, Phillips B, Strathdee SA, et al. Meth/amphetamine use and associated HIV: implications for global policy and public health. Int J Drug Policy. 2010;21(5):347–358. doi: 10.1016/j.drugpo.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 13.Mays VM, Maas R, Ricks J, Cochran SD. HIV and African American Women in the south: employing a population-level HIV prevention and intervention efforts. In: Baum A, Revenson T, Singer J, editors. Handbook of Health Psychology. New York, NY: Oxford Press; 2011. pp. 781–801. [Google Scholar]
- 14.Rhodes T. The 'risk environment': a framework for understanding and reducing drug-related harm. Int J Drug Policy. 2002;13:85–94. [Google Scholar]
- 15.Rhodes T. Risk environments and drug harms: a social science for harm reduction approach. Int J Drug Policy. 2009;20(3):193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Farley TA. Sexually transmitted diseases in the Southeastern United States: location, race, and social context. Sex Transm Dis. 2006;33(7 Suppl):S58–64. doi: 10.1097/01.olq.0000175378.20009.5a. [DOI] [PubMed] [Google Scholar]
- 17.Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 18.Bernays S, Rhodes T, Barnett T. Hope: a new way to look at the HIV epidemic. AIDS. 2007;21 (Suppl 5):S5–11. doi: 10.1097/01.aids.0000298097.64237.4b. [DOI] [PubMed] [Google Scholar]
- 19.Rhodes T, Wagner KD, Strathdee SA, Shannon K, Davidson PJ, Bourgois P. Structural violence and structural vulnerability within the risk environment: theoretical and methodological perspectives for a social epidemiology of HIV risk among injection drug users and sex workers. In: O'Campo P, Dunn JR, editors. Rethinking social epidemiology: towards a science of change. Springer; 2011. [Google Scholar]
- 20.National Alliance of State & Territorial AIDS Directors (NASTAD) [Accessed: 10/03/2011];HIV/AIDS en la frontera: US-Mexico border epidemiologic profile. 2009 Mar;2009;I http://nastad.org/Docs/Public/InFocus/200951_NASTAD_Border_Vol1_alpha.pdf. [Google Scholar]
- 21.Commission US-MBH. [Accessed: 10/11/2011];About the United States - México Border Health Commission. 2011 http://www.borderhealth.org/about_us.php.
- 22.Givaudan M, Pick S. A preventive program for substance abuse in Mexico: best practices. Mentor Foundation; pp. 1–13. [Google Scholar]
- 23.Instituto Nacional de Psiquiatra Ramn de la Fuente. Student Drug Consumption Surveys II. 2000. [Google Scholar]
- 24.Galván-Reyes J, Ortiz-Castro A, González-Uribe L. El sistema de registro de informacin sobre drogas. Un auxiliar diagnstico en la evaluacin de la farmacodependencia [The drug information registration system. A helpful diagnostic in evaluation of pharmaceutical dependency] Salud Publica Mex. 1997;39(1):61–68. [PubMed] [Google Scholar]
- 25.Bucardo J, Brouwer KC, Magis-Rodriguez C, Ramos R, Fraga M, Perez SG, et al. Historical trends in the production and consumption of illicit drugs in Mexico: implications for the prevention of blood borne infections. Drug Alcohol Depend. 2005;79(3):281–293. doi: 10.1016/j.drugalcdep.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brouwer KC, Case P, Ramos R, Magis-Rodriguez C, Bucardo J, Patterson TL, et al. Trends in production, trafficking, and consumption of methamphetamine and cocaine in Mexico. Subst Use Misuse. 2006;41(5):707–727. doi: 10.1080/10826080500411478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Magis-Rodríguez C, Ruiz-Badillo A, Ortiz-Mondragón R, Loya-Sepúlveda M, Bravo-Portela MJ, Lozada-Romero R. de Tijuana BC, editor. Estudio sobre prácticas de riesgo de infección para VIH/SIDA en inyectores de drogas de la cd. [Accessed: 12/05/2011];Biblioteca Virtual en Salud VIH/SIDA. 2002 http://bvssida.insp.mx/articulos/2382.pdf.
- 28.CENSIDA - Secretaría de Salud. Encuesta nacional de adicciones. 2002. [Google Scholar]
- 29.CENSIDA - Secretaría de Salud. Sistema de vigilancia epidemiológica de las adicciones (SISVEA) 2002. [Google Scholar]
- 30.Strathdee SA, Fraga WD, Case P, Firestone M, Brouwer KC, Perez SG, et al. "Vivo para consumirla y la consumo para vivir" ["I live to inject and inject to live"]: high-risk injection behaviors in Tijuana, Mexico. J Urban Health. 2005;82(3 Suppl 4):iv58–73. doi: 10.1093/jurban/jti108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cravioto P. Chihuahua. 2003. La magnitud y la naturaleza del problema de la heroina en Ciudad Juárez. [Google Scholar]
- 32.Deren S, Kang SY, Colon HM, Andia JF, Robles RR. HIV incidence among high-risk Puerto Rican drug users: a comparison of East Harlem, New York, and Bayamon, Puerto Rico. J Acquir Immune Defic Syndr. 2004;36(5):1067–1074. doi: 10.1097/00126334-200408150-00010. [DOI] [PubMed] [Google Scholar]
- 33.Carrier JM. Sexual behavior and spread of AIDS in Mexico. Med Anthropol. 1989;10(2–3):129–142. doi: 10.1080/01459740.1989.9965958. [DOI] [PubMed] [Google Scholar]
- 34.Bucardo J, Semple SJ, Fraga-Vallejo M, Davila W, Patterson TL. A qualitative exploration of female sex work in Tijuana, Mexico. Arch Sex Behav. 2004;33(4):343–351. doi: 10.1023/B:ASEB.0000028887.96873.f3. [DOI] [PubMed] [Google Scholar]
- 35.Sirotin N, Strathdee SA, Lozada R, Nguyen L, Gallardo M, Vera A, et al. A comparison of registered and unregistered female sex workers in Tijuana, Mexico. Public Health Rep. 2010;125 (Suppl 4):101–109. doi: 10.1177/00333549101250S414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rusch ML, Brouwer KC, Lozada R, Strathdee SA, Magis-Rodriguez C, Patterson TL. Distribution of sexually transmitted diseases and risk factors by work locations among female sex workers in Tijuana, Mexico. Sex Transm Dis. 2010;37(10):608–614. doi: 10.1097/OLQ.0b013e3181deaa0f. [DOI] [PubMed] [Google Scholar]
- 37.Goldenberg SM, Rangel G, Vera A, Patterson TL, Abramovitz D, Silverman JG, et al. Exploring the impact of underage sex work among female sex workers in two Mexico-US border cities. AIDS Behav. 2011 doi: 10.1007/s10461-011-0063-3. (e-pub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patterson TL, Goldenberg S, Gallardo M, Lozada R, Semple SJ, Orozovich P, et al. Correlates of HIV, sexually transmitted infections, and associated high-risk behaviors among male clients of female sex workers in Tijuana, Mexico. AIDS. 2009;23(13):1765–1771. doi: 10.1097/QAD.0b013e32832f08a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goldenberg SM, Gallardo Cruz M, Strathdee SA, Nguyen L, Semple SJ, Patterson TL. Correlates of unprotected sex with female sex workers among male clients in Tijuana, Mexico. Sex Transm Dis. 2010;37(5):319–324. doi: 10.1097/OLQ.0b013e3181c5334f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.US Census Bureau. [Accessed: 12/05/2011];Population change and distribution: 1990 to 2000. 2001 http://www.census.gov/prod/2001pubs/c2kbr01-2.pdf.
- 41.US Department of Transportation. [Accessed: 07/29/2009];Statistics on US border crossing. 2009 http://www.transtats.bts.gov/bordercrossing.aspx.
- 42.Rachlis B, Brouwer KC, Mills EJ, Hayes M, Kerr T, Hogg RS. Migration and transmission of blood-borne infections among injection drug users: understanding the epidemiologic bridge. Drug Alcohol Depend. 2007;90(2–3):107–119. doi: 10.1016/j.drugalcdep.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 43.Bwayo J, Plummer F, Omari M, Mutere A, Moses S, Ndinya-Achola J, et al. Human immunodeficiency virus infection in long-distance truck drivers in east Africa. Arch Intern Med. 1994;154(12):1391–1396. [PubMed] [Google Scholar]
- 44.Cook RL, Royce RA, Thomas JC, Hanusa BH. What's driving an epidemic? The spread of syphilis along an interstate highway in rural North Carolina. Am J Public Health. 1999;89(3):369–373. doi: 10.2105/ajph.89.3.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McCoy HV, Correa R, Fritz E. HIV diffusion patterns and mobility: gender differences among drug users. Population Research and Policy Review. 1996;15(3):249–264. [Google Scholar]
- 46.Consejo Nacional de la Poblacion. Población mexicana devuelta por la patrulla fronteriza por diversas características sociodemográficas, según año de levantamiento de la EMIF NORTE 1995, 1999–2007. 2011. Cuadro IV.3.1. [Google Scholar]
- 47.Consejo Nacional de la Poblacion. Población mexicana devuelta por la patrulla fronteriza por características de devolución, según año de levantamiento de la EMIF NORTE, 1995, 1999–2007. 2011. Cuadro IV.3.5. [Google Scholar]
- 48.Robertson AM, Rangel MG, Lozada R, Vera A, Ojeda VD. Male injection drug users try new drugs following U.S. deportation to Tijuana. Mexico Drug Alcohol Depend. 2012;120(1–3):142–148. doi: 10.1016/j.drugalcdep.2011.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Patterson TL, Semple SJ, Fraga M, Bucardo J, de la Torre A, Salazar J, et al. A sexual risk reduction intervention for female sex workers in Mexico: design and baseline characteristics. J HIV/AIDS Soc Serv. 2006;5(2):115–137. [Google Scholar]
- 50.Brouwer KC, Lozada R, Cornelius WA, Firestone Cruz M, Magis-Rodriguez C, Zuniga de Nuncio ML, et al. Deportation along the U.S-Mexico border: its relation to drug use patterns and accessing care. J Immigr Minor Health. 2009;11(1):1–6. doi: 10.1007/s10903-008-9119-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Borges G, Medina-Mora ME, Orozco R, Fleiz C, Cherpitel C, Breslau J. The Mexican migration to the United States and substance use in northern Mexico. Addiction. 2009;104(4):603–611. doi: 10.1111/j.1360-0443.2008.02491.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.CENSIDA - Secretaría de Salud. 25 Años de SIDA en México. [Accessed: 12/06/2011];Logros, desaciertos, y retos. 2008 http://www.censida.salud.gob.mx/descargas/SIDA25axos-26mar.pdf.
- 53.County of San Diego. [Accessed: 12/06/2011];HIV/AIDS epidemiology report 2006. 2006 http://www.sdcounty.ca.gov/hhsa/programs/phs/documents/AnnualReport2006.pdf.
- 54.Philbin MM, Mantsios A, Lozada R, Case P, Pollini RA, Alvelais J, et al. Exploring stakeholder perceptions of acceptability and feasibility of needle exchange programmes, syringe vending machines and safer injection facilities in Tijuana, Mexico. Int J Drug Policy. 2009;20(4):329–335. doi: 10.1016/j.drugpo.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Syvertsen J, Pollini RA, Lozada R, Vera A, Rangel G, Strathdee SA. Managing la malilla: exploring drug treatment experiences among injection drug users in Tijuana, Mexico, and their implications for drug law reform. Int J Drug Policy. 2010;21(6):459–465. doi: 10.1016/j.drugpo.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.CENSIDA - Secretaría de Salud. El consumo de drogas inyectadas y la epidemia del VIH/SIDA en Mexico. [Accessed: 09/03/2007];Un problema de salud publica: documento de posicion. 2003 http://www.salud.gob.mx/conasida/noticias/vihsidacarceles/posicion.doc.
- 57.Magis-Rodriguez C, Ortiz Ruiz L, Ortiz Mondragon R. [Accessed: 11/02/2007];Actividades de reddución del daño en usuarios de drogas: informe interno. 2007 http://www.salud.gob.mx/conasida.
- 58.Viani RM, Araneta MR, Ruiz-Calderon J, Hubbard P, Lopez G, Chacon-Cruz E, et al. Perinatal HIV counseling and rapid testing in Tijuana, Baja California, Mexico: seroprevalence and correlates of HIV infection. J Acquir Immune Defic Syndr. 2006;41(1):87–92. doi: 10.1097/01.qai.0000174657.71276.9f. [DOI] [PubMed] [Google Scholar]
- 59.CENSIDA - Secretaría de Salud. [Accessed: 12/06/2011];Panorama epidemiologico del VIH/SIDA e ITS en Mexico. 2007 http://www.censida.salud.gob.mx/descargas/2007/panoepide30jun2007.pdf.
- 60.Patterson TL, Semple SJ, Staines H, Lozada R, Orozovich P, Bucardo J, et al. Prevalence and correlates of HIV infection among female sex workers in 2 Mexico-US border cities. J Infect Dis. 2008;197(5):728–732. doi: 10.1086/527379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Strathdee SA, Philbin MM, Semple SJ, Pu M, Orozovich P, Martinez G, et al. Correlates of injection drug use among female sex workers in two Mexico-U.S. border cities. Drug Alcohol Depend. 2008;92(1–3):132–140. doi: 10.1016/j.drugalcdep.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Patterson TL, Mausbach B, Lozada R, Staines-Orozco H, Semple SJ, Fraga-Vallejo M, et al. Efficacy of a brief behavioral intervention to promote condom use among female sex workers in Tijuana and Ciudad Juarez, Mexico. Am J Public Health. 2008;98(11):2051–2057. doi: 10.2105/AJPH.2007.130096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Miller CL, Firestone M, Ramos R, Burris S, Ramos ME, Case P, et al. Injecting drug users' experiences of policing practices in two Mexican-U.S. border cities: public health perspectives. Int J Drug Policy. 2008;19(4):324–331. doi: 10.1016/j.drugpo.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Pollini RA, Rosen PC, Gallardo M, Robles B, Brouwer KC, Macalino GE, et al. Not sold here: limited access to legally available syringes at pharmacies in Tijuana, Mexico. Harm Reduct J. 2011;8(1):13. doi: 10.1186/1477-7517-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Frost SD, Brouwer KC, Firestone Cruz MA, Ramos R, Ramos ME, Lozada RM, et al. Respondent-driven sampling of injection drug users in two U.S-Mexico border cities: recruitment dynamics and impact on estimates of HIV and syphilis prevalence. J Urban Health. 2006;83(6 Suppl):i83–97. doi: 10.1007/s11524-006-9104-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.White EF, Garfein RS, Brouwer KC, Lozada R, Ramos R, Firestone-Cruz M, et al. Prevalence of hepatitis C virus and HIV infection among injection drug users in two Mexican cities bordering the U. S Salud Publica Mex. 2007;49(3):165–172. doi: 10.1590/s0036-36342007000300001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pollini RA, Brouwer KC, Lozada RM, Ramos R, Cruz MF, Magis-Rodriguez C, et al. Syringe possession arrests are associated with receptive syringe sharing in two Mexico-US border cities. Addiction. 2008;103(1):101–108. doi: 10.1111/j.1360-0443.2007.02051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Strathdee SA, Lozada R, Ojeda VD, Pollini RA, Brouwer KC, Vera A, et al. Differential effects of migration and deportation on HIV infection among male and female injection drug users in Tijuana, Mexico. PLoS One. 2008;3(7):e2690. doi: 10.1371/journal.pone.0002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Brouwer KC, Rusch ML, Weeks JR, Lozada R, Vera A, Magis-Rodríguez C, et al. Spatial epidemiology of HIV among injection drug users in Tijuana, Mexico. Ann Assoc Amer Geog. doi: 10.1080/00045608.2012.674896. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Strathdee SA, Lozada R, Martinez G, Vera A, Rusch M, Nguyen L, et al. Social and structural factors associated with HIV infection among female sex workers who inject drugs in the Mexico-US border region. PLoS One. 2011;6(4):e19048. doi: 10.1371/journal.pone.0019048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Moyer LB, Brouwer KC, Brodine SK, Ramos R, Lozada R, Cruz MF, et al. Barriers and missed opportunities to HIV testing among injection drug users in two Mexico--US border cities. Drug Alcohol Rev. 2008;27(1):39–45. doi: 10.1080/09595230701710845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Strathdee SA, Lozada R, Pollini RA, Brouwer KC, Mantsios A, Abramovitz DAA, et al. Individual, social, and environmental influences associated with HIV infection among injection drug users in Tijuana, Mexico. J Acquir Immune Defic Syndr. 2008;47(3):369–376. doi: 10.1097/QAI.0b013e318160d5ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brouwer KC, Strathdee SA, Magis-Rodriguez C, Bravo-Garcia E, Gayet C, Patterson TL, et al. Estimated numbers of men and women infected with HIV/AIDS in Tijuana, Mexico. J Urban Health. 2006;83(2):299–307. doi: 10.1007/s11524-005-9027-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Strathdee SA, Lozada R, Semple SJ, Orozovich P, Pu M, Staines-Orozco H, et al. Characteristics of female sex workers with US clients in two Mexico-US border cities. Sex Transm Dis. 2008;35(3):263–268. doi: 10.1097/OLQ.0b013e31815b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Consejo Nacional contras las Adicciones (CONADIC) [Accessed: 12/06/2011];Normatividad y legislación. 2010 http://www.conadic.salud.gob.mx/interior/normas.html.
- 76.Moreno JG, Licea JA, Ajenjo CR. Tackling HIV and drug addiction in Mexico. Lancet. 2010;376(9740):493–495. doi: 10.1016/S0140-6736(10)60883-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pandey A, Reddy DC, Ghys PD, Thomas M, Sahu D, Bhattacharya M, et al. Improved estimates of India's HIV burden in 2006. Indian J Med Res. 2009;129(1):50–58. [PubMed] [Google Scholar]
- 78.Lyerla R, Gouws E, Garcia-Calleja JM. The quality of sero-surveillance in low- and middle-income countries: status and trends through 2007. Sex Transm Infect. 2008;84 (Suppl 1):i85–i91. doi: 10.1136/sti.2008.030593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moreno JGB, Philbin MM, Lozada R, Mantsios A, Alvelais J, Case P, et al. Stakeholder attitudes towards and feasibility of needle exchange programs to reduce drug-related harm in Tijuana, Mexico. 2008 International Conference on AIDS; 2008 August 3–8; Mexico City, Mexico. 2008. [Google Scholar]
- 80.Beletsky L, Agrawal A, Moreau B, Kumar P, Weiss-Laxer N, Heimer R. Police training to align law enforcement and HIV prevention: preliminary evidence from the field. Am J Public Health. 2011;101(11):2012–2015. doi: 10.2105/AJPH.2011.300254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.UNAIDS. Regional Consultation on Role of Police and Law Enforcement in AIDS. 2009. [Google Scholar]
- 82.Coleman SJ. Bishop Kevin Dowling: AIDS and condoms. America: The National Catholic Weekly; New York, NY: America Press Inc; 2009. [Accessed: 12/07/2011]. http://www.americamagazine.org/blog/entry.cfm?id=24947991-3048-741E-1288626171072423. [Google Scholar]
- 83.Pope's statement on condom use applies to heterosexuals, spokesman says. [Accessed: 12/08/2011];CatholicCulture.org: Trinity Communications. 2010 http://www.catholicculture.org/news/headlines/index.cfm?storyid=8371.
- 84.Larios SE, Lozada R, Strathdee SA, Semple SJ, Roesch S, Staines H, et al. An exploration of contextual factors that influence HIV risk in female sex workers in Mexico: the Social Ecological Model applied to HIV risk behaviors. AIDS Care. 2009;21(10):1335–1342. doi: 10.1080/09540120902803190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Philbin MM, Lozada R, Zuniga de Nuncio ML, Mantsios A, Case P, Magis-Rodriguez C, et al. A qualitative assessment of stakeholder perceptions and socio-cultural influences on the acceptability of harm reduction programs in Tijuana, Mexico. Harm Reduct J. 2008;5:36. doi: 10.1186/1477-7517-5-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sirotin N, Strathdee SA, Lozada R, Abramovitz DA, Semple SJ, Bucardo J, et al. Effects of government registration on unprotected sex amongst female sex workers in Tijuana; Mexico. Int J Drug Policy. 2010;21(6):466–470. doi: 10.1016/j.drugpo.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Munoz FA, Pollini RA, Zuniga ML, Strathdee SA, Lozada R, Martinez GA, et al. Condom access: associations with consistent condom use among female sex workers in two northern border cities of Mexico. AIDS Educ Prev. 2010;22(5):455–465. doi: 10.1521/aeap.2010.22.5.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Levine R. Case studies in global health: millions saved. Boston, MA: Jones & Bartlett; 2007. [Google Scholar]
- 89.Levine R Thailand Ministry of Public Health. Case studies in global health: millions saved. Boston, MA: Jones & Bartlett; [Accessed: 01/12/2007]. 2007. Results of HIV sero-surveillance, Thailand 1989–2004 (round 1–22) http://epid.moph.go.th/Aids/Round6month/R6mtab1html. [Google Scholar]
- 90.Rojanapithayakorn W, Hannenberg R. The 100% condom program in Thailand. AIDS. 1996;10(1):1–7. doi: 10.1097/00002030-199601000-00001. [DOI] [PubMed] [Google Scholar]