Abstract
Background:
The WHO Global Burden of Disease study estimates that mental and addictive disorders are among the most burdensome in the world, and their burden will increase over the next decades. The mental and behavioral disorders account for about 12% of the global burden of disease. However, these estimates and projections are based largely on literature review rather than cross-national epidemiological surveys. In India, little is known about the extent, severity and unmet need of treatment mental disorders. Thus, there was a need to carry out rigorously implemented general population surveys that estimate the prevalence of mental disorders among urban population at Pune, Maharashtra. The study attempted to address unmet need and to form a basis for formulating the mental health need of the community.
Objective:
The study was undertaken to estimate the lifetime prevalence and 12 month prevalence of specific mental disorders in urban population, socio-demographic correlates of mental disorders and to assess the service utilization in individuals with mental disorders.
Materials and Methods:
The study was undertaken among adults aged 18 years and above living in house hold and in geographical area of Pune , Maharashtra. A minimum sample of 3000 completed interviews was planned using representative probabilities to population size (PPS) sampling method which ensured equal probability for every eligible member. Data listing was obtained from Census Office from recent census of 2001 data. The face to face interviews were undertaken in homes using fully structured interview schedule of World Mental Health Survey Initiative duly revised Version of WHO- Composite International Diagnostic Interview (CIDI 3.0) by trained investigators. Clinical reappraisal was carried out using Schedules for Clinical Assessment in Neuropsychiatry (SCAN) among ten percent of diagnosed cases selected randomly. Data were entered into DDE (Blaize Software) and analyzed using SPSS software package.
Results:
Overall lifetime prevalence of mental disorders was found to be 5.03%.Rates among males (5.30%) were higher as compared to females (4.73%). Among the diagnostic group , depression(3.14%) was most prevalent followed by substance use disorder (1.39%) and panic disorder (0.86%). Overall 12 month prevalence of mental disorder was found to be 3.18% which was 3.47% among males and 2.85% among females. Prevalence of depression (1.75%) was the most 12-month mental disorder, followed by substance use mental disorder (0.99%) and panic disorder (0.69%).Lifetime and twelve month prevalence of any mental disorder was the highest among employed group, followed by home makers and depression was more among married, followed by separated/divorced/widowed group and the least in unmarried group in the study. Treatment gap due to low prescription received indicated the most of the ill person did not acknowledge their need for treatment or do not received the appropriate care.
Conclusion:
The figure of 5.03% prevalence of diagnosable psychiatric disorders in adult population points to the great need to increase the prevention strategies both at primary and secondary level to overcome the disability and economic loss to society due to mental disorders.
Keywords: Mental disorders, psychiatry service utilization, sociodemographic correlates
Introduction
The WHO Global Burden of Disease study estimates that mental and addictive disorders are among the most burdensome in the world, and their burden will increase over the next few decades. The mental and behavioral disorders account for about 12% of the global burden of diseases. By 2020, it is likely to increase to 15%.(1) Depression, alcohol use disorders, schizophrenia and bipolar disorders constitute the top 10 conditions contributing to the global burden of disease among the age group of 15–44 years. Mental and behavioral disorders are present, in about 10% of the adult population, at any given point of time.(2) However, these estimates and projections are based largely on literature review rather than cross-national epidemiological surveys.
In India, little is known about the extent, severity and unmet need of treatment of mental disorders. Few studies on the epidemiology of mental disorders have focused on prevalence at their isolated sites. The metaanalysis of available Indian studies carried out by Reddy and Chandrasekhar(3) revealed the overall prevalence of mental disorders as 5.8% among the population. A review analysis of 15 epidemiological studies by Ganguli(4) on the prevalence of mental disorders in India estimated the national prevalence of all mental disorders as 70.5 per 1000 in the rural and 73 per 1000 in the urban population. Most of the Indian studies had limitations of properly selected study population based on scientifically valid sampling techniques, and selected the study population based on convenience due to availability of existing resources. Thus, there was a need to carry out rigorously implemented general population surveys to assess the prevalence of mental disorders among the urban population at Pune, Maharashtra. The study was undertaken to estimate the lifetime and 12-month prevalence rates of specific mental disorders (as per ICD-10 of WHO-1992 edition) among the urban population, sociodemographic correlates of mental disorders and to assess the service utilization in individuals with mental disorders. The study attempted to form a basis for formulating the mental health need of the community to address unmet care.
Materials and Methods
Study population
The study was conducted at Pune city of Maharashtra state. The catchment population in the study covered the urban population of Pune city, about 25,13,776 based on the year 2001 census data, residing in Pune Municipal Corporation with an area of 146.14 sq km. Administratively, the Pune Municipal Corporation is divided into four subdivision levels. There are 48 Prabhags (Khands) divided into 161 wards and 4269 census enumeration blocks.
Sampling design
Data listing was obtained from the census office from recent census of 2001 data. All 161 wards and 4269 census enumeration blocks were included in the sampling frame. Each census enumeration block of Pune city, composed of about 43–207 households, was utilized for sampling purpose, adopting a stratified multistage systemic sampling scheme with probability proportion to size (PPS) measures,(2) which ensured an equal probability for every eligible individual in the target population to be selected in the sample. A minimum sample size of 3000 respondents, including 300 spouses, were planned (assuming the prevalence rate of mental disorders of 7% with 95% confidential level, deviation of 2 and keeping in mind the minimum drop out/nonresponse of 20%). All the blocks were serially numbered from 1 to 4269, of which 100 census enumeration blocks were selected by systematic sampling fractions. A sample fraction of 42.7 was obtained by dividing 4269 by 100. From the first random number, every 42.7th blocks were sampled. Location of each block sampled was traced back to ward location. From each census enumeration block sampled, 27 households were selected by computer-generated random numbers. From each household, one eligible individual was selected by the Kish method and interviewed. A total of 300 spouses were also selected by systematic random numbers and interviewed.
The study was undertaken among adults aged 18 years and above, living in household and in the geographical area of Pune, Maharashtra. After taking informed consent, the face-to-face interviews were undertaken in homes using a fully structured interview schedule of the World Mental Health Survey Initiative(2) duly revised version of the WHO-Composite International Diagnostic Interview (CIDI 3.0) by trained investigators from 1 April 2003 to 31 March 2004. The WHO CIDI schedule consisted of structured questions for assessment of mental disorders as per ICD-10, severity, treatment and some correlates regarding diagnosed individuals. The interview schedule consisted of two parts. Part 1 of the interview schedule was completed for all respondents and screened for the core diagnoses. All respondents who met the criteria of any diagnosis were administered Part II, which assessed specific mental disorders and a wide range of correlates. Paper and pencil version (PAPI) was used in the study, duly pretested and translated in local language by standardized translation and back-translation measures. Clinical reappraisal was carried out using Schedules for Clinical Assessment in Neuropsychiatry (SCAN) among 10% of the respondents selected randomly. SCAN consisted of four components, which included present state examination, item group check list, clinical history schedule and glossary of differential definitions. In addition, a random of 20% of the respondents who screened positive for lifetime disorders and all the respondents screened positive for psychosis were also reappraised by a qualified psychiatrist using SCAN. Data were entered into the PAPI Direct Data Entry Instrument (Blaize Software) and analyzed using SPSS software package. Ethical clearance for the study was obtained from the competent local institutional ethical board. Management of diagnosed patients was tied up with qualified psychiatrists in a reputed local hospital.
Results and Discussion
Sample characteristics
A total of 3023 respondents were interviewed in the study. Percent distribution of sample population by age group, sex, marital status, education and employment status were as shown in Table 1.
Table 1.
Sociodemographic profile of the study population
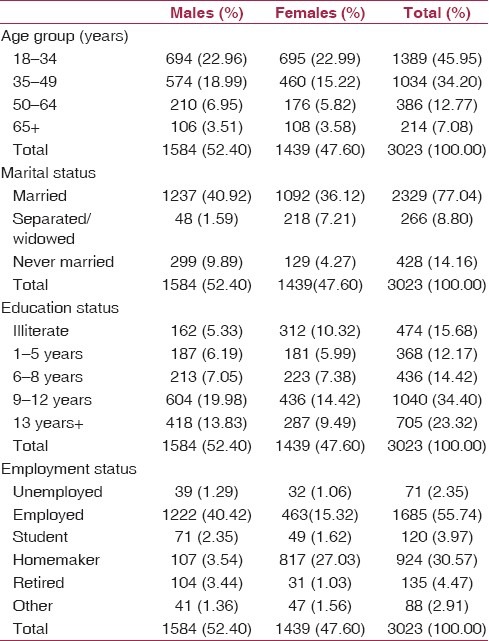
It is seen that about half of the respondents (45.95%) were in the young age group (18–34 years) and 7.08% above the age of 65 years. Males constituted 52.40% and females constituted 47.60% of the study population. A majority of the subjects were literate (84.32%) and employed (55.74%) in the study.
Prevalence of mental disorders
Lifetime and 12-month prevalence of mental disorders were found as depicted in Table 2.
Table 2.
Lifetime prevalence and 12-month prevalence of mental disorders
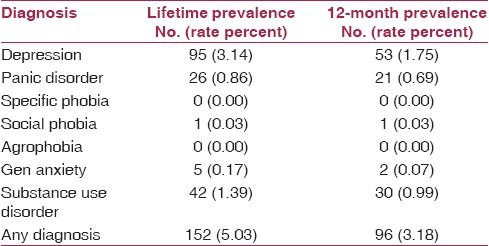
The overall lifetime prevalence of mental disorders was found to be 5.03%. Among the diagnosable group, depression (3.14%) was most prevalent, followed by substance use disorder (1.39%) and panic disorder (0.86%). Overall, the 12-month prevalence of mental disorder was found to be 3.18%. The prevalence of depression (1.75%) was the most 12-month mental disorder, followed by substance use mental disorder (0.99%) and panic disorder (0.69%). A metaanalysis of 13 studies consisting of 33,572 persons carried out by Reddy and Chandrasekar(3) reported a total mental disorder morbidity of 5.82%, while Ganguli(4) estimated the same as 7.3% from his metaanalysis of 15 Indian studies. A survey carried out in Karnataka by Barua et al.(5) determined one-point prevalence of psychiatric disorders as 39.9%, which was quite high as compared with various studies and the present study. Studies in developed countries, such as the NIMH-Epidemiological Catchment Area Study of USA by Regier et al.(6) reported the lifetime prevalence as 32.2%. Compared with these studies, the prevalence of metal disorders in the present Indian study was very low. This might be due to various factors like difference in religious, culture and social and family support system.
Mental disorders as per sociodemographic correlates
Lifetime mental disorders and 12-month mental disorders as per sociodemographic correlates were found as depicted in Tables 3 and 4, respectively.
Table 3.
Lifetime mental disorders as per sociodemographic correlates
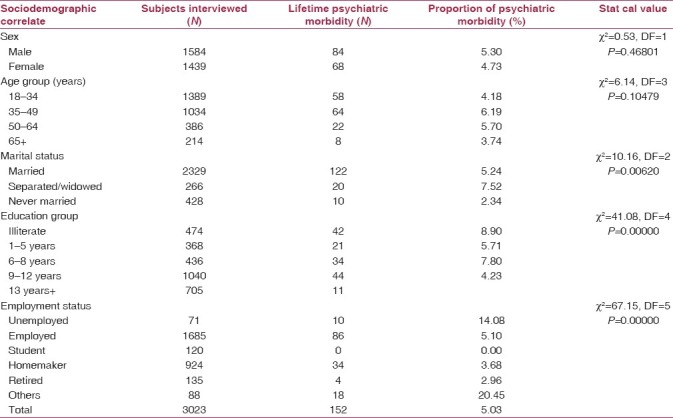
Table 4.
Twelve-month mental disorders as per sociodemographic correlates
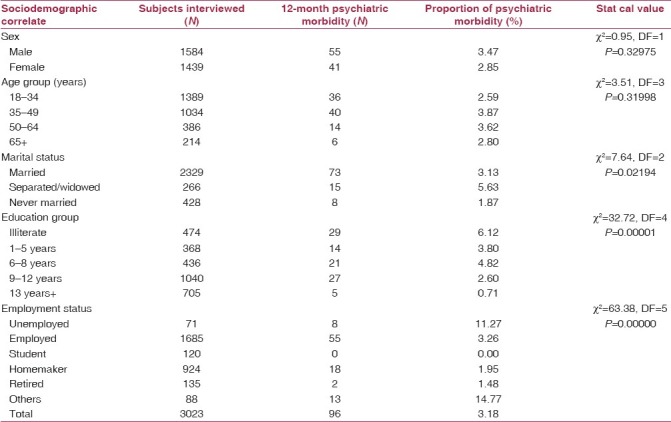
Results in this study found that the lifetime and 12-month prevalence of depressive episode, panic disorder, general anxiety and substance abuse disorders had a higher prevalence in the married group, followed by the separated/divorced/widowed group, and the least in the unmarried group. Lifetime and 12-month prevalence rates of any mental disorder were the highest among the married group (4.04%) and the least among those never married (0.33%). Similar results were reported by Kassler et al.(7) from their study done in the USA. Barua et al.(5) among a rural community in Karnataka reported that women had significantly higher symptoms of somatic disorders and anxiety than men, and this was strongly associated with the lack of education, poverty, low socioeconomic status and also among unmarried or widowed/divorced individuals as compared with their married counterparts. The difference in the results of the study compared with this study may be due to the different setting and sociodemographic attributes of urban and rural settings.
The present study revealed that the lifetime and 12-month prevalence of affective disorders had a gradient across the years of education, i.e. the highest prevalence in group with 0–5 years of education and the least prevalence in the group with 13 years and above years of education. Similarly, panic disorder also had the same trend, with maximum prevalence in the 0–5 years education group and the least prevalence among the 13 years and above education group. General anxiety disorder, specific phobia, any anxiety disorders and substance use disorders were also found to have the highest prevalent in the 0–5 years educated group. Overall, the lifetime prevalence rate of mental disorders was found to be higher among those with 0–5 years of education as compared with higher educated persons. Alex Cohen(8) has described a similar association between female illiteracy and poor mental health. In a study carried out by a community-based psychiatric survey by Carstairs and Kapur,(9) they determined that women had higher rates of psychiatric disorders and that the higher levels of education had a positive effect on the wellbeing of both genders.
Lifetime and 12-month prevalence of depression, panic disorder, generalized anxiety, substance abuse and any mental disorder were the highest among the employed group, followed by the homemaker group and the lowest among the retired group in this study. These findings were concordant with those of the study carried out by Bromet et al.(10) in Ukraine. Mental disorders were reported to be differentially distributed across group of populations with different sociodemographic variable like education, marital status and employment.(9)
All the patients diagnosed with mental disorders were referred to a qualified psychiatrist for management, which was already tied up.
Service utilization
In this study, the 12-month prescription treatment received by 12-month prevalence of mental disorders found the overall prescription as 5.09%, which was very low. Individuals suffering from panic disorder had the highest percentage (11.55%) of treatment received. Specific phobia was the least treated disorder (1.66%). In the study, factors responsible for the treatment gap and main barriers for not utilizing the psychiatry services were stigma attached to mental disorders, shortage of mental health services, shortage of medicines and equipments and shortage of qualified psychiatric professionals in the vicinity. In addition to these, it was largely believed that mental disorders were the result of supernatural forces and not a medical problem; hence, seeking help from spiritual healers.
Treatment gap due to low prescription received indicated the most of the ill persons did not acknowledge their need for treatment or did not receive the appropriate care. Similar conditions prevailing in other countries have been reported by Kessler.(11)
Conclusion
The figures of 5.03% prevalence of diagnosable psychiatric disorders in the adult population and very low level (5.09%) of treatment received by ill individuals point to the great need to increase the prevention strategies both at primary and secondary levels to overcome the disability and economic loss to society due to mental disorders. This calls for concerted efforts to develop community-based mental health services in India on a priority basis. Useful guidelines to scale up the mental health services have been drafted by the Global Mental Health Group(12) to be followed by various countries worldwide as suited to their unmet need.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.New hope. Geneva: WHO; 2001. WHO. World Health Report 2001-Mental Health: A new understanding. [Google Scholar]
- 2.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity and unmet need for treatment of mental disorders in the World Health Organisation World Mental Health Surveys. JAMA. 2004;291:2581–90. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 3.Reddy MV, Chandrasekar CR. Prevalence of mental and behavioral disorders in India: A meta-analysis. Indian J Psychiatry. 1998;40:149–57. [PMC free article] [PubMed] [Google Scholar]
- 4.Ganguli HC. Epidemiological findings on prevalence of mental disorders in India. Indian J Psychiatry. 2000;42:14–20. [PMC free article] [PubMed] [Google Scholar]
- 5.Barua A, Jacob GP, Mahmood SS, Udupa S, Naidu M, Roopa PS, et al. A study on screening for psychiatric disorders in adult population. Indian J Community Med. 2007;32:65–6. [Google Scholar]
- 6.Regier DA, Myers JK, Kramer M, Robins LN, Blazer DG, Hough RL, et al. The NIMH Epidemiological Catchment Area program, historical context, major objectives and study population characteristics. Arch Gen Psychiatry. 1984;41:934–41. doi: 10.1001/archpsyc.1984.01790210016003. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the national co-morbidity survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 8.Alex Cohen. Our lives were covered in darkness. In: Cohen A, Kleinman A, Saraceno B, editors. The work of the national literacy mission in Northern India. Chapter 5, World Mental Health Case Book. New York: Kluwer Academic/Plenum Publishers; 2000. [Google Scholar]
- 9.Carstairs GM, Kapur RL. London: The Hogarth Press; 1976. The great universe of Kota; Stress, change and mental disorders in an Indian village. [Google Scholar]
- 10.Bromet EJ, Gluzman SF, Paniotto VI, Webb CP, Tintle NL, Zakhozha V, et al. Epidemiology of psychiatric and alcohol disorders in Ukraine; Findings from the Ukraine World Mental Health survey. Soc Psychiatry Psychiatr Epidemiol. 2005;40:681–90. doi: 10.1007/s00127-005-0927-9. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC. Psychiatric Epidemiology: Selected recent advances and future directions. Bull World Health Organ. 2000;78:464–74. [PMC free article] [PubMed] [Google Scholar]
- 12.Chisholm D, Flisher AJ, Lund C, Patel V, Saxena S, et al. Lancet Global Mental Health Group. Scale up services for mental disorders: A call for action. Lancet. 2007;370:1241–52. doi: 10.1016/S0140-6736(07)61242-2. [DOI] [PubMed] [Google Scholar]


