Abstract
Aim:
To analyze the trends in clinicopathologic indications for enucleations over a 15-year period.
Materials and Methods:
Clinicopathologic details of all eyes that underwent enucleation from January 1996 to December 2010 were drawn up from a computerized database. The study was divided into three periods of 5 years each and comparison tables for each cause of enucleation during these periods were generated. Chi-square test was used to compare proportions.
Results:
Out of a total 1467 enucleations performed during the study period, 693 (46%) were attributable to retinoblastoma, 189 (12.5%) to uveal melanoma, 228 (15%) to trauma, and 149 (10%) to phthisis bulbi. Intraocular tumors accounted for more than 63% of all enucleations performed. Over the three time periods, proportion of enucleations secondary to retinoblastoma increased from 38% in the 1st period to 58% in the 3rd period (P < 0.001). Enucleations for trauma showed statistically significant reduction in trends over the three periods (24% in the 1st period vs. 4.4% in the 3rd period, P < 0.001). Similar trends were also seen in the proportion of enucleations due to intractable glaucoma and chronic uveitis. The absolute number of enucleations secondary to retinoblastoma out of the total cases seen during the study period did not change over the three periods (range 51–60%).
Conclusion:
Intraocular tumors were the commonest indications for enucleation in our patient population despite the availability of globe-conserving treatments such as chemotherapy and radioactive plaques. We observed increasing trends in the proportion of enucleations due to retinoblastoma and reduction of enucleations secondary to trauma, chronic uveitis, and glaucoma.
Keywords: Enucleation, India, indications, trends
Enucleation of the globe is a terminal therapeutic measure in many end-stage ocular diseases. The main goals of enucleation are to alleviate patient's symptoms, viz. pain in cases with intractable glaucoma, uveitis, and trauma, improve cosmetic appearance in phthisical eyes, and prevent extraocular spread of infection in eyes with endophthalmitis. It may also prevent extraocular extension and systemic metastasis of intraocular tumors such as retinoblastoma and choroidal melanomas. In cases of tumor, enucleation can be life saving as well as provides acceptable cosmetic results, especially in large choroidal melanomas of >16 mm thickness.
An analysis of the indications for enucleation over a large time period provides scope for its comparison between different points in time and different geographic locations. These assessments lead to emergence of trends which can retrospectively hint at success/failure of disease management protocols, especially of those with globe-salvaging potential. There are numerous studies in literature reporting on the spectrum of diseases leading to enucleation.[1–5] However, most of these are from the developed world where the variety and incidence of diseases may be entirely different from that in the developing world. Apart from data presented by Vemuganti et al., there is hardly any data from India comparing indications of enucleation.[6] The purpose of the present study is to review the indications for enucleation from a tertiary eye care center in South India and analyze the trends over the past 15 years.
Materials and Methods
A computerized database at the Department of Ocular Pathology of our institute was used to draw up clinicopathologic details of all eyes that underwent enucleation from January 1996 to December 2010. This time period was chosen as all the histopathologic slides were available for review in doubtful cases. Clinical history was obtained from standard pathology requisition forms completed by the enucleating physician and contained the demographics, relevant clinical history, and the clinical diagnosis. Specimens were fixed in paraffin and sectioned for examination under light microscopy. The final diagnosis was based on clinicopathologic correlation, i.e. both clinical and pathological findings were considered to arrive at a diagnosis. In case of a discrepancy, the pathologic diagnosis was considered as the mainstay.
The enucleated globes were divided into causes of enucleation: retinoblastoma, uveal melanoma, trauma, end-stage glaucoma, phthisis bulbi, staphyloma, other tumors, Coats’ disease, infection (including endophthalmitis and corneal ulcers), chronic uveitis, and others category. The underlying diseases for end-stage glaucoma were grouped into two categories: neovascular glaucoma (this included glaucoma related to vessel occlusion and diabetic neovascularization) and other intractable glaucomas. End-stage/intractable glaucoma was a clinical diagnosis obtained from information provided by the treating clinician. It was correlated with advanced cupping of the optic nerve head seen on histopathology. However, if the underlying cause of glaucoma was retinal vascular telangiectasias, then these eyes were grouped under Coats’ disease. Chronic uveitis was also a clinical diagnosis provided by the treating clinician and correlated histopathologically with inflammatory cell infiltration within the uveal tract. Eyes that were blind, painful, and/or cosmetically unacceptable as a result of acute or distant trauma, with no other known disease, were put in the trauma category including traumatic glaucomas. Disfigured eyes due to any etiology other than trauma were included in the phthisis bulbi group.
The 15-year study period was divided into three periods of 5 years each and indications for enucleation over each period were compared. Data were entered into Microsoft Excel sheets and all statistical analyses were performed using commercially available statistical package (SPSS for Windows, version 14, Chicago, IL, USA). Period-wise comparison tables for each cause of enucleation were generated and χ2 test was used to compare proportions. All P-values were two-sided and were considered statistically significant when the values were less than 0.05.
Results
A total of 1467 enucleations were performed over the 15-year study period for a variety of indications [Table 1]. Fig. 1 shows the trends in the proportion of enucleation due to different etiologies over the three periods. Ocular tumors were the commonest indication for enucleation in our study population, with retinoblastoma and uveal melanoma constituting 46 and 12.5% of the cases, respectively. Table 2 shows the comparative percentages of different indications over the three different time periods. The percentage of enucleations due to retinoblastoma increased gradually from 38% in the 1st period to 58% in the 3rd period (P = 0.001, χ2 test). No differences were observed in the proportion of enucleations due to uveal melanomas over the three periods (P = 0.177).
Table 1.
Indications of enucleation
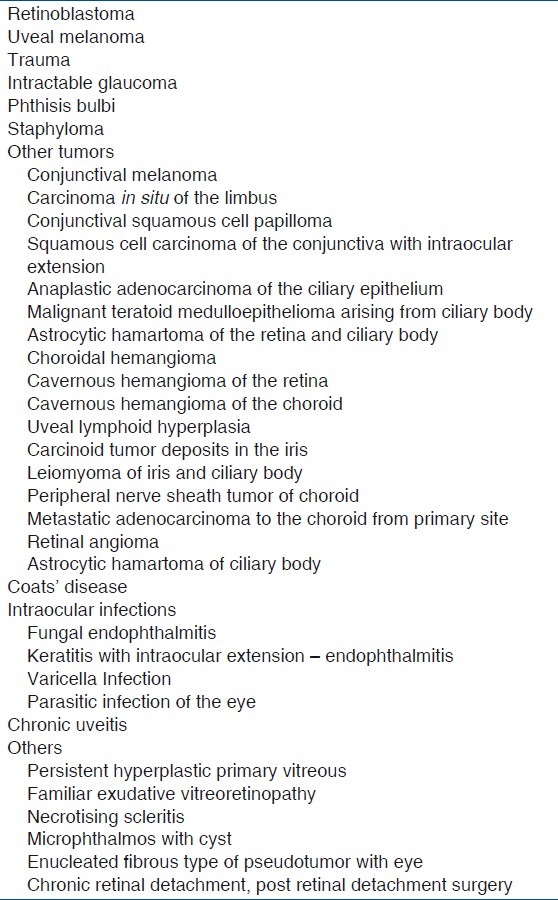
Figure 1.
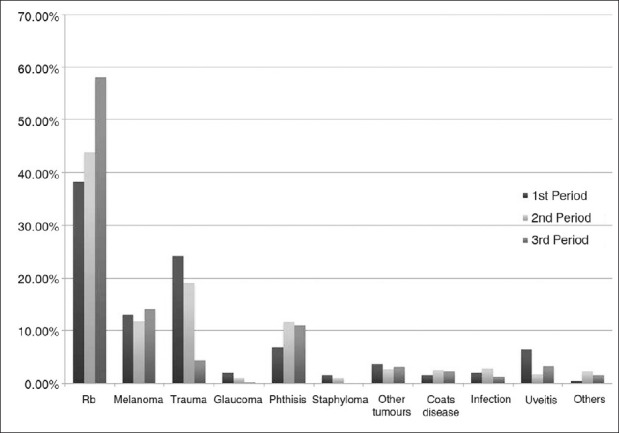
Trends in etiologies for enucleation over the three periods
Table 2.
Comparative percentages of different indications over the three different periods
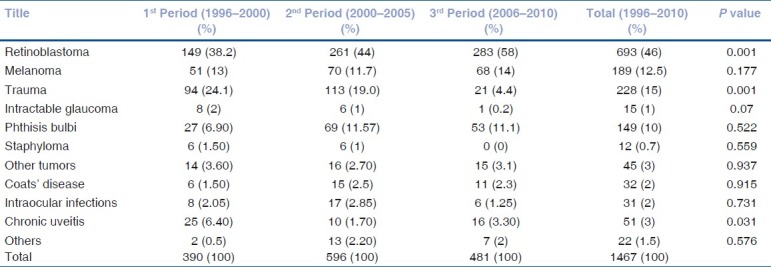
In the trauma group, the main types of injury included road traffic accidents, burst injury (mainly firecracker and bottles), and sharp object perforating injury. In the 1st period (1996–2000), 24% of the enucleations were attributable to trauma. This reduced to around 4.5% in the 3rd period (2006–2010). This reducing trend seen in the proportion of enucleations due to trauma over the three periods was statistically significant (P = 0.001, χ2 test). A similar trend was seen in enucleations due to intractable glaucoma, reducing from 2% in the 1st period to 0.2% in the 3rd period (P = 0.07). Chronic uveitis constituted 6.4% of all enucleations in the 1st period and this reduced by half in the 3rd period (3.3%) (P = 0.031). Other indications such as phthisis bulbi, Coats’ disease, and other intraocular tumors showed similar trends over the study periods. Eyes with Coats’ disease were enucleated due to the presence of intractable glaucoma with painful blind eye. Very few diagnostic surprises were encountered and these were in the group of other ocular tumors and retinoblastoma being mistaken for Coats’ disease (approximately 2%).
In terms of percentage of enucleations for retinoblastoma, out of the total cases seen during the entire study period, there was no difference between the three periods and ranged from 51.5% (149/289) in the 1st period to 61.4% (261/425) in the 2nd period and 57.3% (283/494) in the 3rd period.
Discussion
The rate and clinical causes leading to ocular enucleation reflect the spectrum of severe ocular disorders within geographic confines. The efficacy of eye-salvaging treatment modalities such as sophisticated vitreoretinal surgery for ocular trauma and chemotherapy of ocular tumors such as retinoblastoma can also be indirectly evaluated, and for these reasons, it is essential to review data from enucleation specimens on a periodic basis. Vemuganti et al. reported retrospectively analyzed data from 151 eyes that presented to them between January 1995 and July 1998.[6] To the best of our knowledge, there has been no similar study from India over the past decade, evaluating the etiologies responsible for enucleations.
Increasing number of globe-salvaging techniques are now available for retinoblastoma; however, the proportion of enucleations due to retinoblastoma seems to be increasing.[1,7] In our study, we found an increasing trend in the proportion of enucleations due to retinoblastoma over a 15-year period, from 38% to nearly 60%. However, the proportion of enucleations out of the total number of retinoblastoma cases seen during the study period has remained fairly constant, ranging from 50 to 60%. We performed enucleation for stage IV (International Classification of Intraocular retinoblastoma) retinoblastoma in unilateral cases and for Stage V retinoblastoma (worse eye) in bilateral cases. Hence, the indication for enucleation in retinoblastoma cases did not change over time and changing practice patterns did not contribute to increasing proportion of enucleations due to retinoblastoma. Neoplasia has become the more common cause of enucleation through the years, and as the total number of enucleations for all other causes steadily decreases, neoplasia represents an increasingly larger proportion. Another plausible explanation for increasing enucleations due to neoplasia could be increased awareness of intraocular tumors amongst ophthalmologists and pediatricians, leading to more cases being diagnosed and referred to tertiary care centers like ours. Globe salvage has been introduced in the management of intraocular tumors, but their applicability in developing countries is limited due to late presentation in the course of the disease, poor socioeconomic conditions, and lack of education as evidenced by the fairly stable proportion of retinoblastoma enucleations out of total cases seen. Setlur et al. reviewed the changing causes of enucleation over a 60-year period and reported similar trends, with tumors accounting for 51% of all enucleations in this decade.[1] In the series reported by Vemuganti et al., tumors were the commonest etiologies for enucleation, amounting for 49%.[6] In comparison, our series demonstrated a significant increase in enucleations due to intraocular tumors (including retinoblastoma, melanomas, and others), which accounted for 63%.
Enucleations for trauma, glaucoma, and chronic uveitis are on the decline.[1,3,4] Our series showed a decline by nearly 20% in the proportion of enucleation due to trauma over the past 15 years. Also, enucleation due to glaucoma reduced tenfold and that due to chronic uveitis reduced by half in our study. Probable explanation for this is the availability of improved surgical techniques to treat trauma, reduced incidence of trauma due to more public awareness, and better medical treatment of glaucomas and uveitic entities over the past decade.
Enucleations in Coats’ disease were performed for symptomatic relief of pain rather than as a result of confusion with retinoblastoma, though we did experience a few diagnostic surprises. Eyes with chronic uveitis and retinal detachment were enucleated for similar reasons. Eyes with phthisis bulbi underwent enucleation with orbital ball implantation and socket reconstruction if indicated. Trends in enucleation due to these conditions did not change significantly with time.
The changing demographics of South India, in general, and referral patterns to our institute, in particular, may have contributed to the change in causes of enucleation over the 15-year study period. This makes a direct comparison with other enucleation studies difficult. A higher proportion of enucleations due to intraocular tumors in our study has already been highlighted previously. The availability of a specialist ocular oncologist at our center may have led to increased tumor referrals. Huang et al. reported a decrease in pediatric non-retinoblastoma enucleations over time, possibly attributable to better diagnostic capabilities, surgical techniques, and public health interventions.[7] The increase in retinoblastoma enucleations over time in their study was likely due to the result of institutional referral bias, similar to our experience. A pattern of increasing retinoblastoma was also seen by Stiebel et al. in their 1960–1989 enucleation study.[8] Cheng et al. reviewed 1375 enucleations from Beijing, China, in 2007 and found trauma to be the commonest cause for enucleation (62%).[2] In their series, tumors accounted for 28% and were the second commonest cause contrary to ours. Setlur et al. have demonstrated similar trends to ours, in the declining proportion of glaucoma and trauma and increasing neoplasm-related enucleations over time in their study.[1]
The strength of our study is the large sample size and time duration sufficient enough to demonstrate changing trends in the etiologies responsible for enucleation. A drawback of the study is its retrospective nature and selection bias due to our institute being a referral center.
In conclusion, we observed increasing trends in the proportion of enucleations due to retinoblastoma and reduction of enucleations attributable to trauma, chronic uveitis, and glaucoma. To the best of our knowledge, this is the largest such data available from an Indian scenario and shows increasing proportion of enucleations due to neoplasia compared to previous studies.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Setlur VJ, Parikh JG, Rao NA. Changing causes of enucleation over the past 60 years. Graefes Arch Clin Exp Ophthalmol. 2010;248:593–7. doi: 10.1007/s00417-009-1262-8. [DOI] [PubMed] [Google Scholar]
- 2.Cheng GY, Li B, Li LQ, Gao F, Ren RJ, Xu XL, et al. Review of 1375 enucleations in the TongRen Eye Centre, Beijing. Eye (Lond) 2008;22:1404–9. doi: 10.1038/sj.eye.6702919. [DOI] [PubMed] [Google Scholar]
- 3.Gunalp I, Gunduz K, Ozkan M. Causes of enucleation: A clinicopathological study. Eur J Ophthalmol. 1997;7:223–8. doi: 10.1177/112067219700700304. [DOI] [PubMed] [Google Scholar]
- 4.Hansen AB, Petersen C, Heegaard S. Review of 1028 bulbar eviscerations and enucleations. Changes in aetiology and frequency over a 20-year period. Acta Ophthalmol Scand. 1999;77:331–5. doi: 10.1034/j.1600-0420.1999.770317.x. [DOI] [PubMed] [Google Scholar]
- 5.Saeed MU, Chang BY, Khandwala M. Twenty year review of histopathological findings in enucleated/eviscerated eyes. J Clin Pathol. 2006;59:153–5. doi: 10.1136/jcp.2005.029744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vemuganti GK, Jalali S, Honavar SG, Shekar GC. Enucleation in a tertiary eye care centre in India: Prevalence, current indications and clinicopathological correlation. Eye (Lond) 2001;15:760–5. doi: 10.1038/eye.2001.245. [DOI] [PubMed] [Google Scholar]
- 7.Huang S, Crawford JB, Porco T, Rutar T. Clinicopathologic review of pediatric enucleations during the last 50 years. J AAPOS. 2010;14:328–33. doi: 10.1016/j.jaapos.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 8.Stiebel H, Sela M, Péer J. Changing indications for enucleations in Hadassah University Hospital, 1960–1989. Ophthalmic Epidemiol. 1995;2:123–7. doi: 10.3109/09286589509057093. [DOI] [PubMed] [Google Scholar]


