Abstract
Optical coherence tomography (OCT) has transformed macular disease practices. This report describes the use of conventional OCT systems for peripheral retinal imaging. Thirty-six eyes with peripheral retinal pathology underwent imaging with conventional OCT systems. In vivo sectional imaging of lattice degeneration, snail-track degeneration, and paving-stone degeneration was performed. Differences were noted between phenotypes of lattice degeneration. Several findings previously unreported in histopathology studies were encountered. Certain anatomic features were seen that could conceivably explain clinical and intraoperative behavior of peripheral lesions. Peripheral OCT imaging helped elucidate clinically ambiguous situations such as retinal breaks, subclinical retinal detachment, retinoschisis, choroidal nevus, and metastasis. Limitations of such scanning included end-gaze nystagmus and far peripheral lesions. This first of its kind study demonstrates the feasibility of peripheral retinal OCT imaging and expands the spectrum of indications for which OCT scanning may be clinically useful.
Keywords: Choroidal nevus, in vivo, lattice degeneration, optical coherence tomography, peripheral retinal lesions, retinoschisis
Optical coherence tomography (OCT) has enabled in vivo near-histological imaging leading to better understanding of macular diseases. Peripheral retinal lesions have traditionally been considered inaccessible and remained unexplored hitherto. We describe the use of conventional OCT systems to image peripheral retinal lesions, with the twin objectives of elucidating their in vivo sectional structure and demonstration of the practical utility of such an exercise.
Materials and Methods
Institutional review board exemption was obtained for this study. Twenty-eight consecutive patients (36 eyes) with peripheral retinal lesions underwent imaging from November 2009 to April 2010. Cases with advanced cataract or non-dilating pupils were excluded. Subject age ranged from 18 to 74 years. Imaging was performed with time domain OCT (TD-OCT) (Stratus 3, Carl Zeiss, Dublin, CA) and spectral domain OCT (SD-OCT) (Cirrus, Carl Zeiss, Dublin, CA) instruments. No machine modifications or additional lenses were used. The dilated patient was seated as usual and instructed to look in the direction of the quadrant of interest. Acquisition protocol was chosen as per the clinical situation. Focusing was done to obtain as clear a retinal lesion image as possible in the fundus image window and the scan was performed. Cases where the fundus image was of poor quality and could not reliably confirm scan location were excluded (7 eyes).
Results
Image signal strength varied from 0 to 5. Retinal morphology was apparent even in images with zero signal strength. Lesions reported in our study were distributed in all quadrants and were equally accessible for imaging. Image quality and resolution were better with the Cirrus system. Imaging ease was higher with the Stratus system as it allowed greater freedom of movement. Sectional features of peripheral retinal entities are presented first. Subsequently, benefits of peripheral OCT in clinically ambiguous situations are described.
Peripheral retinal lesions
Both pigmented (5) and non-pigmented (7) lattice degeneration showed vitreous condensation at the edges of the two ends of lattice. Patchy retinal thinning was seen in pigmented lesions alone, with areas of increased reflectivity from pigment hyperplasia. Full thickness retinal defects were found in areas without clinically apparent holes, especially at the outer border of the ends of lattice degeneration [Fig. 1]. Non-pigmented lattice lesions did not demonstrate thinning of the retina, contrary to previous histopathology descriptions.[1] Edges of these lesions were thicker than the surrounding retina and demonstrated a triangular configuration of vitreous attachment [Fig. 2]. In addition to the edges, SD-OCT revealed high reflective dot echoes densely localized over the non-pigmented lattices. Clinically, this could explain adherent gel vitreous frequently encountered over lattices during vitrectomy, in contrast to the “liquefied vitreous” previously reported in histopathology.
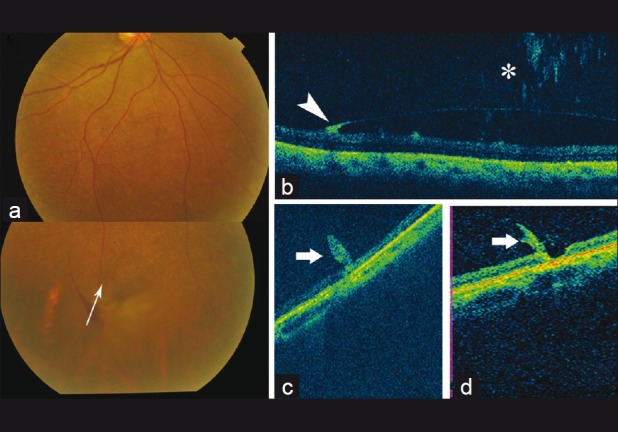
Figure 1.
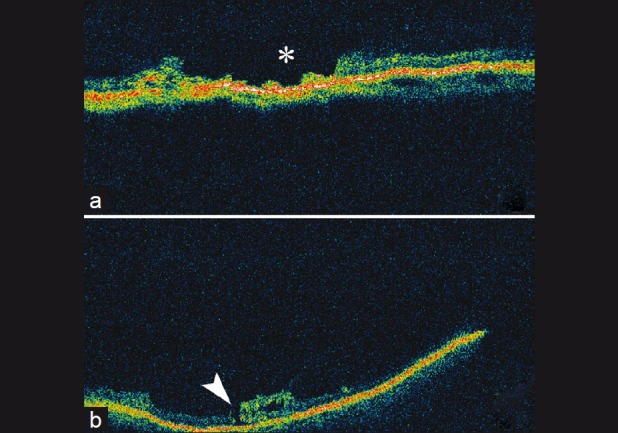
(a and b) Optical coherence tomography scan through pigmented lattice degeneration demonstrating irregularly thinned retina and full thickness defects (asterisk). (b) Full thickness hole at the edge of the lesion (arrowhead)
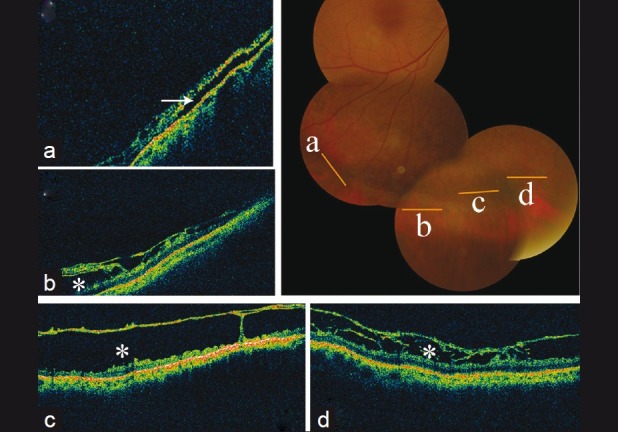
Figure 2.
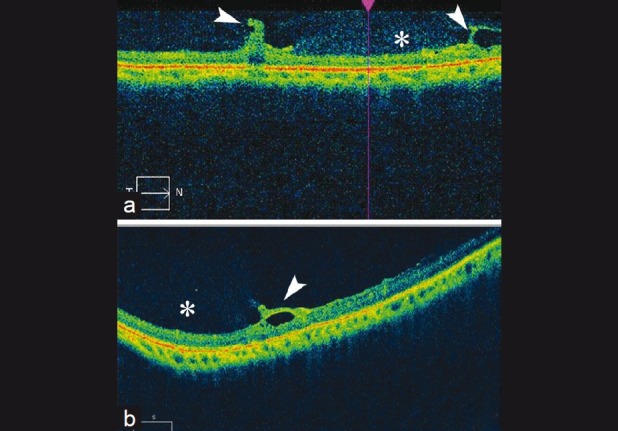
(a and b) Optical coherence tomography image of non-pigmented lattice degeneration demonstrating triangular attachment of vitreous (arrowheads) and dense hyper-reflective dots over lesion (asterisk). The retinal thickness within the lesion is similar to adjoining retina
Configuration of peripheral atrophic holes resembled that of macular holes, including the presence of cystoid changes in surrounding retina, with additional vitreous attachment to one edge in a few cases [Fig. 3].
Figure 3.
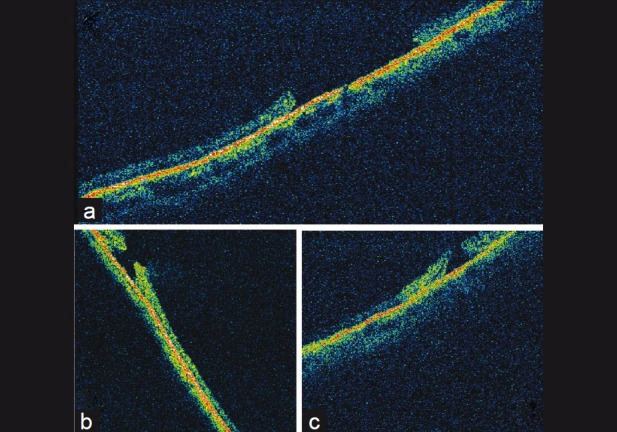
(a–c) Optical coherence tomography images of peripheral retinal holes demonstrating similarity to idiopathic macular holes. (a) Flattened edges of the hole. (b) and (c) Everted edges, vitreous attachment and cystoid changes in surrounding retina
Snail-track degeneration (2 eyes) demonstrated irregular thinning with a wrinkled curvilinear inner retinal surface [Fig. 4]. No changes (traction, condensation) were seen in the overlying vitreous. Paving-stone degeneration (2 eyes) demonstrated uniform marked thinning of the retina over the lesion with choroidal hyperreflectivity.
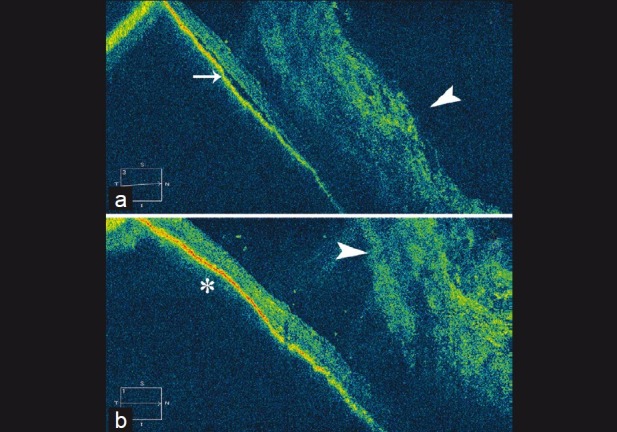
Figure 4.
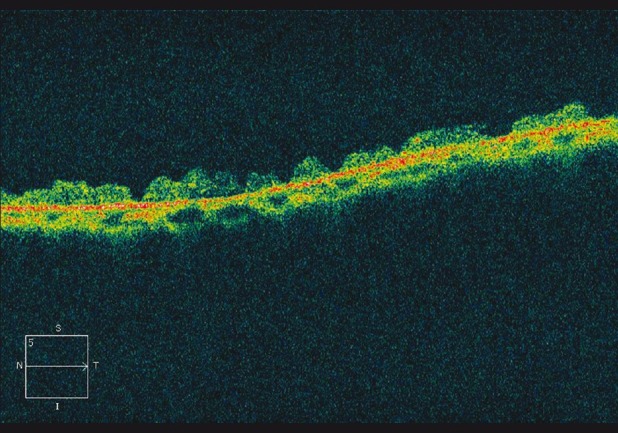
Optical coherence tomography image of snail-track degeneration demonstrating thinning with markedly wrinkled inner retinal surface and no vitreoretinal abnormalities
Clinical application
SD-OCT scanning was done in three patients with persistent flashes and clinical difficulty in ruling out suspected tears due to subhyaloid blood. OCT through the suspected area demonstrated retinal continuity in two patients and an occult break in the third. Two eyes with suspected small horseshoe flaps were scanned. One of these demonstrated a partial thickness defect alone [Fig. 5].
Figure 5.
(a) Color fundus photograph of a patient with posterior vitreous detachment (PVD), small subhyaloid hemorrhage, and persistent flashes. Arrow demonstrates scan direction of Optical coherence tomography (OCT) in (b); (b) OCT through suspected area demonstrates vitreous hemorrhage (asterisk), edge of PVD with hyperreflective subhyaloid hemorrhage (arrowhead), and underlying intact retina; (c) OCT of suspected retinal flap demonstrates retinal tag with intact retina; (d) OCT demonstrating partial thickness retinal defect along with retinal flap. This case was kept under observation
Three patients with senile retinoschisis with suspected retinal detachment underwent scanning (TD-OCT). The presence of subretinal fluid (SRF) under the retinoschisis was revealed in two cases [Fig. 6]. The third demonstrated presence of outer retinal breaks without a detachment.
Figure 6.
Color fundus photograph of case with senile retinoschisis with optical coherence tomography scans taken through areas as depicted. (a) Shallow subretinal fluid (line arrow); (b-d) retinoschisis (asterisk) alone without subretinal fluid
One patient had residual SRF with suspected communication to the break following non-drainage scleral buckling for traumatic retinal detachment. Altered vitreous hemorrhage prevented a clear clinical assessment. SD-OCT revealed minimal SRF over the posterior slope of the buckle not communicating with the break [Fig. 7]. In another patient with an avulsed vessel and underlying retinal break, TD-OCT demonstrated a clinically unapparent thin layer of SRF extending far posterior to the break that required considerably wider laser treatment.
Figure 7.
Postoperative optical coherence tomography (OCT) images of patient who underwent scleral buckling for inferior retinal detachment and vitreous hemorrhage following trauma. There was minimal subretinal fluid (SRF) seen hazily through the hemorrhage running toward the break in the immediate postoperative period. (a) OCT scan through the area showing SRF (line arrow) and overlying vitreous hemorrhage (arrowhead); (b) Beyond the region shown in (a), no subretinal fluid was seen. A gentle indentation of the buckle can be made out (asterisk) with overlying vitreous hemorrhage (arrowhead)
Two patients with large naevi in the periphery demonstrated a minimally elevated convex hyperreflective echo from the RPE-choriocapillaris complex with lack of SRF or changes in the overlying retina [Fig. 8]. One patient with known recently diagnosed metastatic lung carcinoma and an elevated cream-white retinal lesion in the nasal periphery underwent TD-OCT imaging that demonstrated a choroidal lesion [Fig. 9]. A provisional diagnosis of choroidal metastasis was made. On a subsequent visit after chemotherapy, the elevation had disappeared.
Figure 8.
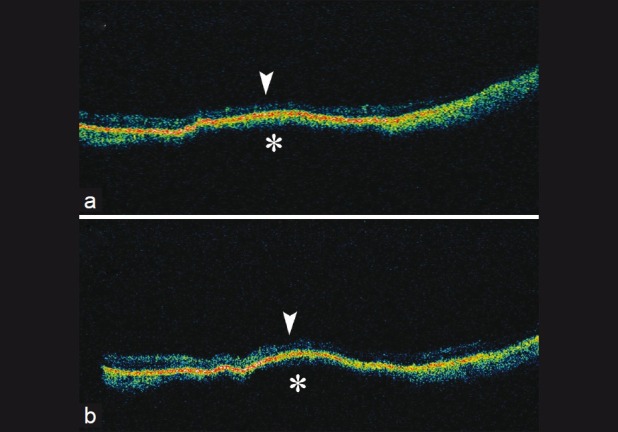
(a and b) Optical coherence tomography images of nevus demonstrating choroidal elevation with hyperreflectivity (asterisk) and normal architecture of overlying retina (arrowhead)
Figure 9.
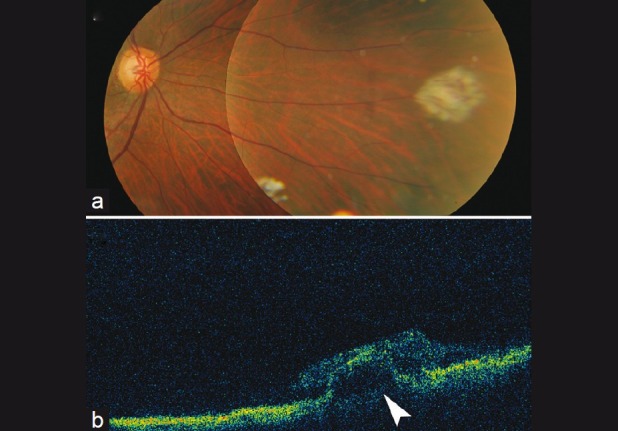
(a) Color fundus photograph of lesion in a patient with metastatic pulmonary carcinoma; (b) Optical coherence tomography scan through the lesion demonstrated an elevated choroidal lesion with thickening of overlying retina
Limitations of peripheral OCT imaging included end-gaze nystagmus and far peripheral location of lesions (within 2 disc diameters of the ora serrata). The limited range of movement of the machines (anteroposterior only) considerably restricted the field of scanning. This was partially overcome by limited face turn or head tilt.
Discussion
Attempts have been made to study the retinal periphery with OCT in enucleated eyes.[2] Though more time consuming than macular scanning, satisfactory in vivo OCT imaging is possible for lesions in the retinal periphery.
With OCT, we could identify differences between the phenotypes of lattice degeneration. Pigmented lattices were found to have thinned retina and clinically unrecognized breaks, in contrast to the non-pigmented variety which had normal thickness. Whether pigmented lesions represent later stages of progressive degeneration with thinning and pigment hyperplasia remains to be investigated. Presence of dense attachment of vitreous at the ends of lattice degeneration could explain the curvilinear breaks in this location sometimes seen after a PVD. The configuration of peripheral retinal holes bore strong semblance to idiopathic macular holes and could possibly explain the similar innocuous nature.[3]
OCT demonstrated unequivocally the presence or absence, and extent of SRF, leading to better decision making and more complete treatment.
Imaging of suspicious naevi could be an important application of peripheral OCT. Features suggestive of malignancy such as thickness, SRF, and overlying retinal changes[4,5] could be picked up preclinically on serial monitoring and documented.
Shortcomings of our study include small sample size and diverse range of lesions presented. This novel study was conducted to assess the feasibility and applicability of peripheral OCT imaging with conventional systems. The study was able to establish the same and presents the first description of in vivo sectional features of peripheral retinal lesions. Even so, a larger sample size needs to be accumulated to enable generalization or conclusions on some findings. A larger study would also further elucidate the place and indications for peripheral OCT.
Conclusion
This first of its kind study demonstrates the use of conventional OCT for peripheral retinal imaging. It throws light on the OCT features of common peripheral lesions and illustrates possible clinical applications of such scanning.
References
- 1.Sehu KW, Lee WR. Retina: Vascular diseases. Degenerations and dystrophies. In: Sehu KW, Lee WR, editors. Ophthalmic pathology: An illustrated guide for clinicians. 1st ed. Victoria: Blackwell Publishing Ltd; 2005. pp. 233–4. [Google Scholar]
- 2.Ghazi NG, Dibernardo C, Ying H, Mori K, Gehlbach PL. Optical Coherence Tomography of peripheral retinal lesions in enucleated human eye specimens with histologic correlation. Am J Ophthalmol. 2006;141:740–2. doi: 10.1016/j.ajo.2005.10.058. [DOI] [PubMed] [Google Scholar]
- 3.Byer NE. Long-term natural history of lattice degeneration of the retina. Ophthalmology. 1989;96:1396–401. doi: 10.1016/s0161-6420(89)32713-8. [DOI] [PubMed] [Google Scholar]
- 4.Shields CL, Shields JA. Clinical features of small choroidal melanoma. Curr Opin Ophthalmol. 2002;13:135–41. doi: 10.1097/00055735-200206000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Muscat S, Parks S, Kemp E, Keating D. Secondary retinal changes associated with choroidal naevi and melanomas documented by optical coherence tomography. Br J Ophthalmol. 2004;88:120–4. doi: 10.1136/bjo.88.1.120. [DOI] [PMC free article] [PubMed] [Google Scholar]


