Abstract
Background:
The prevalence of diabetes mellitus is increasing among Indian population over time. There are varying reports about the association of depression among type 2 diabetic individuals. However, there is limited data about this in India.
Aims:
To study the association of depression, demographic and socio-medical factors in type 2 diabetes patients.
Settings and Design:
Cross-sectional, epidemiological study.
Materials and Methods:
All the consenting type 2 diabetes mellitus patients attending to Medical OPD (n=210) were screened for symptoms of depression using beck depression inventory. All the participants were physically examined and a detailed psychiatric assessment were done. The relevant investigations were advised to identify comorbid conditions.
Statistical Analysis:
Chi-square test with odd's ratio.
Results:
One-fourth of the screened diabetic patients were found to be having depression. Females and overweight individuals were found to have features of depression. Patients with long duration of diabetes and on combination of antidiabetic drugs were significantly associated with depression. Among depressed diabetics 25.9% were having Ischemic heart disease as a comorbid medical illness.
Conclusions:
This study shows there is increased rate of depression among type 2 diabetic individuals. The interesting association of depression with several demographic and sociomedical factors have an important implication in type 2 diabetics.
Keywords: Association, beck depression inventory, depression, type 2 diabetes
INTRODUCTION
It is widely recognized that depression is more common among people with diabetes than in the general population.[1] A German study[2] that included 4,597 subjects and a Dutch study[3] that included 4,747 participants found no association between type 2 diabetes and depressive symptoms. In a general-practice setting study, that included 2,849 male and 3,160 female subjects, depression was not more prevalent in people with screen-detected diabetes or impaired glucose regulation than in people with normal glucose regulation.[4]
Contrary to these studies, within the Hertfordshire Cohort Study[5] there was a relationship between depression scores and diagnosed and previously undiagnosed diabetes. A recent meta-analysis of 27 studies found a statistically significant association between depression and hyperglycemia in both type 1 and type 2 diabetes.[6]
In 1992, it was stated about the relationship between depression and diabetes that “the etiology is unknown but is probably complex; and biological, genetic, and psychological factors remain as potential contributors. Several neuroendocrine and neurotransmitter abnormalities common to both depression and diabetes have been identified, adding to etiological speculations”.[7] It has been suggested that stress-induced activation of the hypothalamic-pituitary-adrenal axis may result in the development of metabolic abnormalities and depression.[8]
In addition to these biological factors, the observed association between diabetes and depressive symptoms could be a reflection of the burden of diabetes and comorbidities.
In the present study, our aim was to analyze the prevalence of depressive symptoms in people with previously known type 2 diabetes. Furthermore, our aim was to study the association between type 2 diabetes mellitus and depressive symptoms, taking into account potential confounding demographic and biological factors as well as comorbidity.
MATERIALS AND METHODS
This study was conducted in a tertiary care hospital (Sri Chamarajendra hospital) attached to a Government medical college, Hassan, Karnataka. The total study sample consisted of 210 cases who were previously known type 2 diabetes patients, selected by means of simple random sampling method from the medical out patient department. This study was conducted during period from January 2011 till April 2011. All subjects gave written informed consent and also clearance from ethical committee was taken. Information about age and sex was assessed by means of a questionnaire. Body mass index (BMI) and blood pressure were measured using standard methods. On the day of examination all patients were investigated for fasting and postprandial blood sugars. The detailed physical examination for all subjects was done by investigating physician. Depressive symptoms were assessed using the 21-item beck depression inventory (BDI-21).[9] The items in the BDI-21 are summed into a total score (0–63), with higher scores indicating more severe depressive symptoms. The applied cutoff score for depressive symptoms was ≥16 to increase specificity for depression.[10] The psychiatric assessment was done by co-investigator (psychiatrist).
RESULTS
Two hundred and ten completed questionnaires were analyzed. In our study all patients were type 2 diabetics. The prevalence of depression among the study participants according to BDI scale was 27.6%. The maximum number of patients (35.4%) were belonging to the range of the age group 51-60 (years). Female constituted of 65.7% of the study sample and 69% of which had BDI score more than or equal to 16, compared to males who had only 31%. However, the difference was not statistically significant (P value=0.54). Majority of the study sample, 82.9% were in the married category. The relationship between demographic and socioeconomic profile of the patients studied and BDI score is shown in [Tables 1 and 2], respectively.
Table 1.
Demographic characteristics of the study population
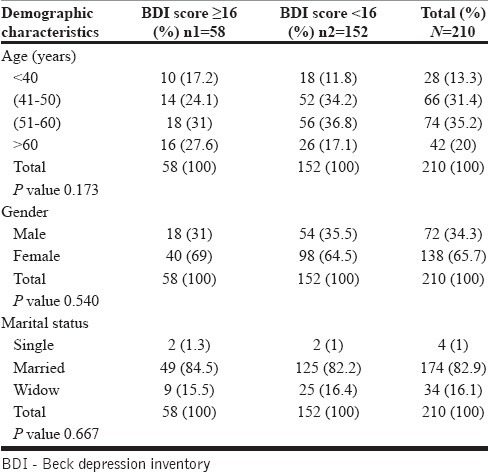
Table 2.
Relationship between socio-medical factors and BDI score
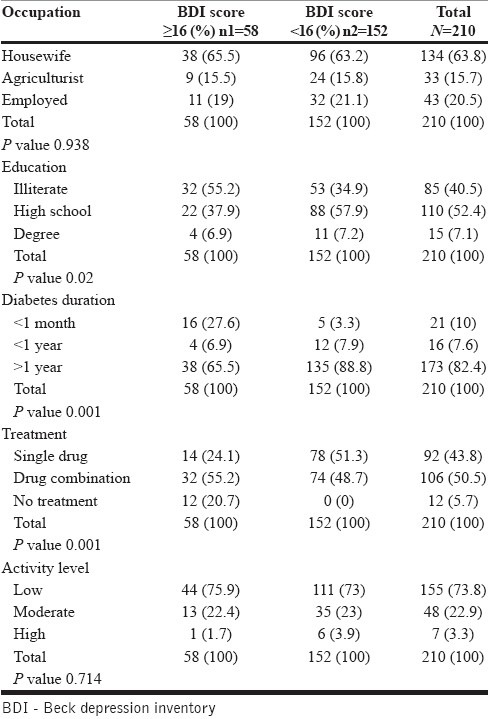
Table 2 shows the relationship between sociomedical factors and BDI score. The majority of our study population (55.2%) were illiterate. Among the study group 65.5% were suffering from depression, in those patients who had diabetes for more than a year which was statistically significant (P value=0.001).
The study group who were taking combination of drugs for treatment of diabetes were 55.2% who scored more than or equal to 16 in BDI, which was statistically significant (P value=0.001).
However, the occupational status and activity level of the study group were compared with the BDI score was found to be not significant statistically.
Among 51.7% diabetic patients who were suffering from depression also had hypertension as a comorbid factor, this was statistically significant P value=0.03) [Table 3].
Table 3.
Relationship between comorbid factors and BDI score

In diabetics, 25.9% of the depressive patient were having ischemic heart disease (IHD) as a comorbid medical illness. This difference was statistically significant (P value=0.008).
The obese (BMI ≥30 kg/m2) people with diabetes were only about 15.5% in the depressive group and there was no statistical difference observed.
The habit of consumption of tobacco was observed among 65.5% of depressive patients, which was statistically significant (P value=0.001).
DISCUSSION
The study showed the one-fourth of the screened patients are potential cases of depression. Most of them were females and 41% of the depressed patients were overweight. Patients with more than 1 year of duration of diabetes and patients were on combination of antidiabetic drug therapy were significantly associated with depression.
The demonstration of a consistent relationship is important because it lays the groundwork for exploring the pathways between depression as a psychological variable and complications as medical variables.
The relationship between diabetes and depression had been subject of many research and metaanalysis. There was a debate whether diabetes causes depression or not. Many studies even went further to investigate the possibility of depression as a risk factor for developing diabetes. However, the results are inconsistent. While most studies found that depression is highly prevalent among people with diabetes in different cultural settings when compared to non-diabetics; other large studies found that diabetes does not increase the risk or the risk is increased only in the presence of other complications.[11,12–21] In a recent meta-analysis type 2 diabetes was found to be associated with only modest increased risk of depression.[22] The prevalence rate in this study is comparable to a recent study, which used a similar scale and studies that used self reported questionnaires.[11,16]
It may be argued that the high prevalence rate found in this study is due to many patients having uncontrolled diabetes (70%), which is similar to what have been seen in previous studies.[23,24]
This study showed that more than 69% of those who scored ≥16 points were females. The predominance of depression among females is consistent with other studies. In a meta-analysis, Anderson et al. found that diabetes doubles the risk of depression and it is especially more among females 28.2% compared to 18% among males; this finding has been replicated in several recent studies.[11,25,15,16,26,27]
About 67% of the total sample was either overweight or obese which is expected in people with type 2 diabetes. However, the BDI score was much higher among obese patients; the difference was statistically not significant, see [Table 3].
CONCLUSIONS
Although about one-fourth of the screened patients were potential cases of depression, the great majority were under-recognized and undertreated. Hence, psychosocial assessment should be part of initial and ongoing evaluation of these patients to improve their quality of life and decrease adverse outcomes.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 2.Icks A, Kruse J, Dragano N, Broecker- Preuss M, Slomiany U, Mann K, et al. Heinz Nixdorf Recall Study Investigator Group. Are symptoms of depression more common in diabetes? Results from the Heinz Nixdorf Recall study. Diabet Med. 2008;25:1330–6. doi: 10.1111/j.1464-5491.2008.02585.x. [DOI] [PubMed] [Google Scholar]
- 3.Knol MJ, Heerdink ER, Egberts AC, Geerlings MI, Gorter KJ, Numans ME, et al. Depressive symptoms in subjects with diagnosed and undiagnosed type 2 diabetes. Psychosom Med. 2007;69:300–5. doi: 10.1097/PSY.0b013e31805f48b9. [DOI] [PubMed] [Google Scholar]
- 4.Aujla N, Abrams KR, Davies MJ, Taub N, Skinner TC, Khunti K. The prevalence of depression in white-European and Southasian people with impaired glucose regulation and screen-detected type 2 diabetes mellitus. PLoS One. 2009;4:e7755. doi: 10.1371/journal.pone.0007755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holt RI, Phillips DI, Jameson KA, Cooper C, Dennison EM, Peveler RC. The relationship between depression and diabetes mellitus: Findings from the Hertfordshire Cohort Study. Hertfordshire Cohort Study Group. Diabet Med. 2009;26:641–8. doi: 10.1111/j.1464-5491.2009.02742.x. [DOI] [PubMed] [Google Scholar]
- 6.Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM. Depression and poor glycemic control: A meta-analytic review of the literature. Diabetes Care. 2000;23:434–42. doi: 10.2337/diacare.23.7.934. [DOI] [PubMed] [Google Scholar]
- 7.Lustman PJ, Griffith LS, Gavard JA, Clouse RE. Depression in adults with diabetes. Diabetes Care. 1992;15:1631–9. doi: 10.2337/diacare.15.11.1631. [DOI] [PubMed] [Google Scholar]
- 8.Bjorntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2:73–86. doi: 10.1046/j.1467-789x.2001.00027.x. [DOI] [PubMed] [Google Scholar]
- 9.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 10.Lustman PJ, Clouse RE, Griffith LS, Car ney RM, Freedland KE. Screening for depression in diabetes using the Beck Depression Inventory. Psychosom Med. 1997;59:24–31. doi: 10.1097/00006842-199701000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Anderson RJ, Clouse RE, Freeland KE, Lustman PJ. The Prevalence of Comorbid Depression in Adults with Diabetes. A Meta-Analysis. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 12.Pibernik-Okanovic M, Peros K, Szabo S, Begic D, Metelko Z. Depression in Croatian Type 2 Diabetic Patients: Prevalence and Risk Factors. A Croatian Survey from the European Depression in Diabetes (EDID) Research Consortium. Diabet Med. 2005;22:942–5. doi: 10.1111/j.1464-5491.2005.01528.x. [DOI] [PubMed] [Google Scholar]
- 13.Chou KL, Chi I. Prevalence of Depression among Elderly Chinese with Diabetes. Int J Geriatr Psychiatry. 2005;20:570–5. doi: 10.1002/gps.1328. [DOI] [PubMed] [Google Scholar]
- 14.Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The Prevalence of Co-Morbid Depression in Adults with Type 2 Diabetes: A Systematic Review and Meta-Analysis. Diabet Med. 2006;23:1165–73. doi: 10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]
- 15.Asghar S, Hussain A, Ali SM, Khan AK, Magnusson A. Prevalence of Depression and Diabetes: A Population-Based Study From Rural Bangladesh. Diabet Med. 2007;24:872–7. doi: 10.1111/j.1464-5491.2007.02136.x. [DOI] [PubMed] [Google Scholar]
- 16.De Groot M, Doyle T, Hockman E, Wheeler C, Pinkerman B, Shubrook J, et al. Depression among Type 2 Diabetes Rural Appalachian Clinic Attendees. Diabetes Care. 2007;30:1602–4. doi: 10.2337/dc06-1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mansour A, Jabir M. The Prevalence of Comorbid Depression among Adults with Diabetes in Southern Iraq. Pakistan J Med Sci. 2007;23:185–7. [Google Scholar]
- 18.Li C, Ford ES, Strine TW, Mokdad AH. Prevalence of Depression among U.S. Adults with Diabetes. Diabetes Care. 2008;31:105–7. doi: 10.2337/dc07-1154. [DOI] [PubMed] [Google Scholar]
- 19.Brown LC, Majumdar SR, Newman SC, Johnson JA. Type 2 Diabetes Does Not Increase Risk of Depression. CMAJ. 2006;175:42–6. doi: 10.1503/cmaj.051429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pouwer F, Beekman AT, Nijpels G, Dekker JM, Snoek FJ, Kostense PJ, et al. Rates and Risks for Co-Morbid Depression in Patients with Type 2 Diabetes Mellitus: Results from a Community-Based Study. Diabetologia. 2003;46:892–8. doi: 10.1007/s00125-003-1124-6. [DOI] [PubMed] [Google Scholar]
- 21.Engum A, Mykletun A, Kristian K, Holen A, Dahl AA. Depression and Diabetes. A Large Population-Based Study of Sociodemographic, Lifestyle, and Clinical Factors Associated with Depression in Type 1 and Type 2 Diabetes. Diabetes Care. 2005;28:1904–9. doi: 10.2337/diacare.28.8.1904. [DOI] [PubMed] [Google Scholar]
- 22.Mezuk B, Eaton W, Albrecht S, Golden SH. Depression and Type 2 Diabetes over the Lifespan. Diabetes Care. 2008;31:2383–90. doi: 10.2337/dc08-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fikree M, Hanafi B, Hussain Z, Masuadi E. Glycemic Control of Type 2 Diabetes Mellitus. Bahrain Med Bull. 2006;28:105–7. [Google Scholar]
- 24.Nasser J. Evaluation of Diabetes Care in a Primary Care Setting. Bahrain Med Bull. 2007;29:45–9. [Google Scholar]
- 25.Egede LE, Zheng D, Simpson K. Comorbid Depression Is Associated with Increased Health Care Use and Expenditures in Individuals with Diabetes. Diabetes Care. 2002;25:464–70. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 26.De Groot M, Pinkerman B, Wagner J, Hockman E. Depression Treatment and Satisfaction in a Multicultural Sample of Type 1 and Type 2 Diabetic Patients. Diabetes Care. 2006;29:549–53. doi: 10.2337/diacare.29.03.06.dc05-1396. [DOI] [PubMed] [Google Scholar]
- 27.Nichols GA, Brown JB. Unadjusted and Adjusted Prevalence of Diagnosed Depression in Type 2 Diabetes. Diabetes Care. 2003;26:744–49. doi: 10.2337/diacare.26.3.744. [DOI] [PubMed] [Google Scholar]


